
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Glob. Womens Health , 16 August 2023
Sec. Maternal Health
Volume 4 - 2023 | https://doi.org/10.3389/fgwh.2023.1187916
This article is part of the Research Topic Cervical Cancer Awareness – Volume I: Screening, Vaccines, and Prevention View all 8 articles
Background: Cervical cancer is the most prevalent gynecologic cancer in women and the second leading cause of cancer death worldwide. Africa's southern, eastern, and western regions have the highest rates of cervical cancer. Cervical cancer is treatable and curable when detected early, but it is nonetheless fatal in low- and middle-income (LMIC) nations where screening and early detection are not widely accessible.
Objective: The objective of this study is to assess the magnitude of precancerous cervical lesions and their associated factor among women screened for cervical cancer at a referral center in southern Ethiopia, in 2021.
Methods: A retrospective institution-based cross-sectional study was conducted from February 21 to April 14, 2022, among randomly selected 372 records of women screened for cervical cancer at Hawassa University Specialized Hospital. Data were extracted from clients' charts using a data extraction checklist. Statistical Package for Social Sciences version 26 and logistic regression analysis were applied to determine the association between dependent and independent variables, and significance was declared at p-value <0.05.
Results: The magnitude of abnormal cervical dysplasia in this study was 18.3% of which 14% were precancerous cervical lesions and 4.3% were cervical cancer. Early coitarche: Adjusted odds ratio (AOR) = 5.6 [95% (confidence interval) CI = 1.87–16.78], having more than one sexual partner: AOR = 2.6 [95% CI = 1.2–5.68], being HIV positive: AOR = 3.56 [95% CI = 1.53–8.29], and having sexually transmitted infections: AOR = 4.64 [95% CI = 2.08–10.35] were independent predictors of precancerous cervical lesions.
Conclusion: The magnitude of precancerous cervical lesions in the study setting is 18% and the magnitude of cervical cancer is 14%, which is higher than the pooled prevalence of precancerous cervical lesions in Ethiopia. Having multiple sexual partners, being HIV positive, having sexual intercourse before 21 years, and new STI diagnosis was independently associated with abnormal precancerous cervical lesions.
Columnar cells undergo modifications in a precancerous stage of the cervix, increasing their propensity to develop into cancer. Although this stage has not yet developed into cancer, if it is not treated quickly, it is quite likely to do so in 10 years or more (1, 2). The area of the cervix that contains epithelium that has undergone a squamous metaplastic transition is known as the transformation zone. There is an area of squamous metaplasia between the ectocervix and the squamocolumnar junction. The majority of anomalies are assumed to start in this region (3).
Cervical cancer is the most common gynecologic cancer in women. The human papillomavirus is the primary cause of the majority of these malignancies, while other hosts and behavioral variables also play a role in the development of the tumors after the first infection. Serology is also inconsistent and unable to differentiate between past and present infections. Consequently, the only way to be certain of a diagnosis is through the direct detection of HPV DNA or cytologic examination. The absence of routine pap smear screening is the biggest risk factor for cervical cancer (2).
Sub-Saharan Africa has the highest global incidence and mortality rates for cervical cancer, with rates particularly high in Eastern Africa (Malawi has the highest incidence and mortality rate in the world), Southern Africa, and Middle Africa. In Northern America, Australia/New Zealand, and Western Asia (Saudi Arabia and Iraq), mortality rates can vary by up to 18 times, while incidence rates are 7–10 times lower (4, 5).
Africa's southern, eastern, and western regions have the greatest rates of cervical cancer. Cervical cancer is still fatal in low- and middle-income countries (LMIC), where screening and early detection are not easily accessible although it is a preventable illness that can be cured when discovered early. Almost 90% of cervical cancer fatalities occur in LMICs. LMICs frequently struggle with a lack of resources and funds to offer proper treatment (4–6).
Cervical cancer is thought to be a concern for 29 million Ethiopian women, with 7,095 new cases and 4,752 fatalities reported annually. Cervical cancer is the main cause of cancer-related deaths among women aged 15–44 in the nation and the second most common malignancy among all women (7, 8).
By 2020, the Federal Ministry of Health in Ethiopia aimed to have at least 80% of the eligible target groups screened and treated for cases of pre-invasive cervical cancer. Yet, a community-based cross-sectional survey of nine districts and two city administrations in Ethiopia (Addis Ababa and Dire Dawa) reveals a shockingly low percentage of cervical screening (2.9%), and only 10% of patients had visited the cancer center in the early stages of their illness (7, 8).
Though several studies concentrating on north and central Ethiopia are conducted, most of these studies are conducted focusing on women with HIV. Besides assessing all women screened for cervical cancer, this study is conducted in the biggest referral center in southern Ethiopia which encompasses not only urban but also women from rural and pastoral areas of the south. Therefore, this study aimed to determine the magnitude of precancerous cervical lesions and their predictors among women screened for cervical cancer in Hawassa University Comprehensive Specialized Hospital Southern Ethiopia.
After identifying the prevalence of precancerous cervical lesions and associated factors in the study area, this study aims to provide the finding of the study to Sidama, SNNPR, and Oromia regional health bureaus to enact strategies helpful for reducing contributors of the infection.
The Sidama area, one of the three densely populated coffee-producing regions in the nation, has Hawassa as its capital. HUCSH is a teaching hospital in Hawassa that has been providing health services since 2006. It provides services for more than 20 million people from all over southern Ethiopia. Currently, it has over 450 beds and cares for clients in a broad range of services to over 90,200 outpatients, 181,116 inpatients, and 1,092 emergency cases annually. The hospital gives cervical cancer screening services with VIA for women aged 30–49 years.
A retrospective institution-based cross-sectional method was employed from February 21 to April 14, 2022, to determine the magnitude of cervical cancer and its associated factors among women screened for cervical cancer at HUCSH in 2021.
Medical records of all women who were screened for cervical cancer in the gynecologic department of HUCSH in 2021.
Medical records of women who were screened for cervical cancer available during the study period with complete information were recruited into the study including date of VIA examination, HIV status, and result of the VIA examination.
From the total number of 454 women screened for cervical cancer in 2021 at Hawassa University Comprehensive Specialized Hospital, 42 medical records were unavailable at the record center and 40 had incomplete information which resulted in the reduction of the sample size of the study to 372 charts of women screened for cervical cancer.
The prevalence of precancerous cervical lesions.
Socio-demographic characteristics (age, marital status, occupation, and educational status), sexual activity (number of sexual partners), age at first sexual intercourse, parity, status of HIV infection, STI status, use of contraceptives, and history of smoking.
Women who have been screened using visual inspection with acetic acid (VIA) and tested positive.
Data was collected by investigators from the HUCSH pre-cervical cancer screening unit of the client assessment form and the registry book as a form of the checklist. It contains means of identification (age, educational status, and other sociodemographic statuses like marital status and occupation), reproductive history (marital status, parity, contraceptive use, age at first intercourse, and pregnancy), menstrual bleeding pattern (regularity and postcoital bleeding), risk factors (history of smoking, number of sexual partners, previous abnormal pap smear, chronic corticosteroid use, and HIV status), examination result, VIA result, and intervention done, if any.
Statistical Package for Social Science (SPSS) Version 26 was used to code, enter, clean up, and update the data before analysis. The statistical relationship between each independent variable and the result variable was examined using a logistic regression model. Variables with a p-value of 0.25 or less were added to the multivariable logistic regression model. Tables and texts were used to display the results. Using adjusted odds ratios (AOR) with a 95% confidence interval, the strength of associations was evaluated, and significance was determined at a p-value of 0.05.
Training and orientation were provided for data collectors and supervisors for 2 days on the objective of the study, confidentiality of information, and data collection tools. Day-to-day supervision was carried out by the principal investigator and trained supervisor for the entire length of the data collection period.
Using the variance inflation factor and standard error, multi-collinearity was examined to determine whether there was a linear correlation between the independent variables. The multivariate analysis excluded variables having a standard error of >2 and a variance inflation factor >10 from consideration. To assess the model's fitness, a Hosmer-Lemeshow test was conducted. The test yielded a value >0.05, and the fit was assumed.
Ethical approval was obtained from the institutional review board (IRB) of Hawassa University College of Medicine and Health Sciences. A formal letter was written to Hawassa University's comprehensive specialized hospital to access data of women screened for cervical cancer during the study period. Data were kept confidential, the anonymity of the respondents was assured, and data were used only for research purposes.
Out of 454 women screened for a precancerous lesion at HUCSH by VIA in the year 2021, a total of 372 medical records were reviewed in this study. The mean age of the participants was 38.68 (SD ± 9.07) years. Nearly 46.8% of participants had an educational level of elementary school and the majority of the participants were married (317) (85.2%) (Table 1).
The participants' average starting age for sexual activity was 19.64 years (SD: 2.95). The majority of participants, 363 (97.6%), had at least one child, and 193 (51.8%) of them had more than three. A history of STI was present in nearly one-fifth of the individuals [73 (19.6%)], and 82 (22.04%) had several partners. More than a fourth-fifth of the participants 308 (82.79%) had been tested for HIV and forty-seven (12.6%) of them were reactive of which 44 (93.6%) were on highly active antiretroviral therapy (HAART) (Table 2).
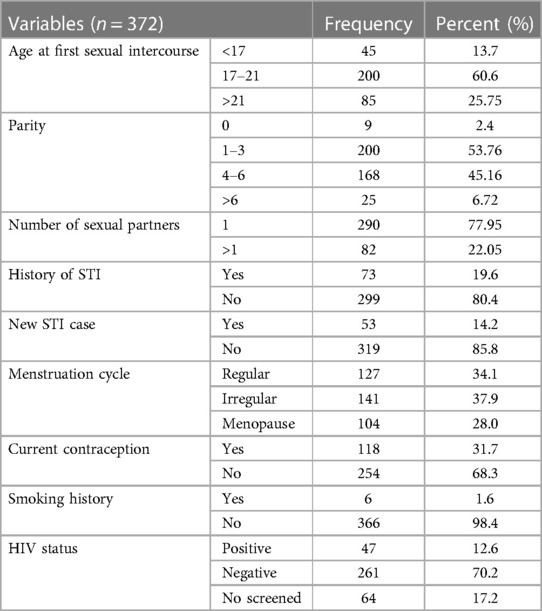
Table 2. Reproductive health history and related characteristics of women screened for cervical cancer at HUCSH, 2021.
Among 372 women's medical records, 18.3% of participants had abnormal cervical lesions, of which 14% were found to be positive and 4.3% had lesions suspected to be cervical cancer (Figure 1).
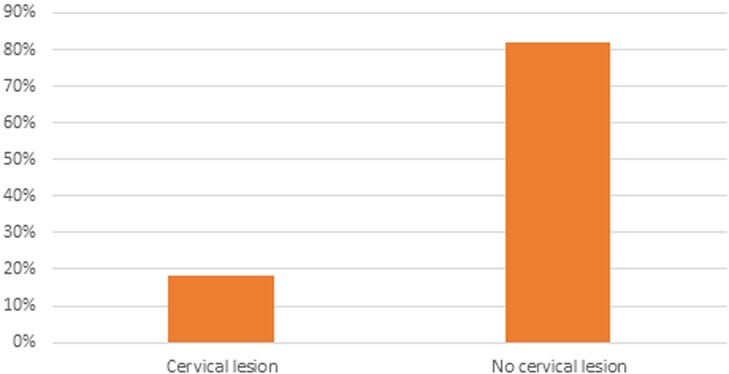
Figure 1. The magnitude of precancerous cervical lesions by VIA screening among women screened for cervical cancer at HUCSH, 2021.
Of the 372 women screened for cervical cancer in the duration of the study, 96.8% had a normal pelvic exam, 86.3% were screened for the first time, 4.6% had a suspicious lesion upon examination, 14% had a positive VIA result, and 13.7% received cryotherapy (Table 3).
The multivariable logistic regression analysis showed that early age coitarche, having more than one sexual partner, being HIV positive, and new STI history were independently associated with abnormal cervical lesions. The odds of the abnormal cervical lesion were 5.6 times higher among women whose age at first sexual intercourse was <21 years old, AOR = 5.6 [95% CI = 1.87–16.78]. Women who had more than one sexual partner were 2.6 times more likely than women who had only one partner to acquire abnormal cervical lesions, AOR = 2.6 [95% CI = 1.2–5.68]. Those who were HIV+ had a higher chance of developing atypical cervical lesions, AOR = 3.56 [95% CI = 1.53–8.29]. The odds of the abnormal cervical lesion were 4.64 times higher among women who had new sexually transmitted infections (STI) AOR = 4.64 [95% CI = 2.08–10.35] (Table 4).
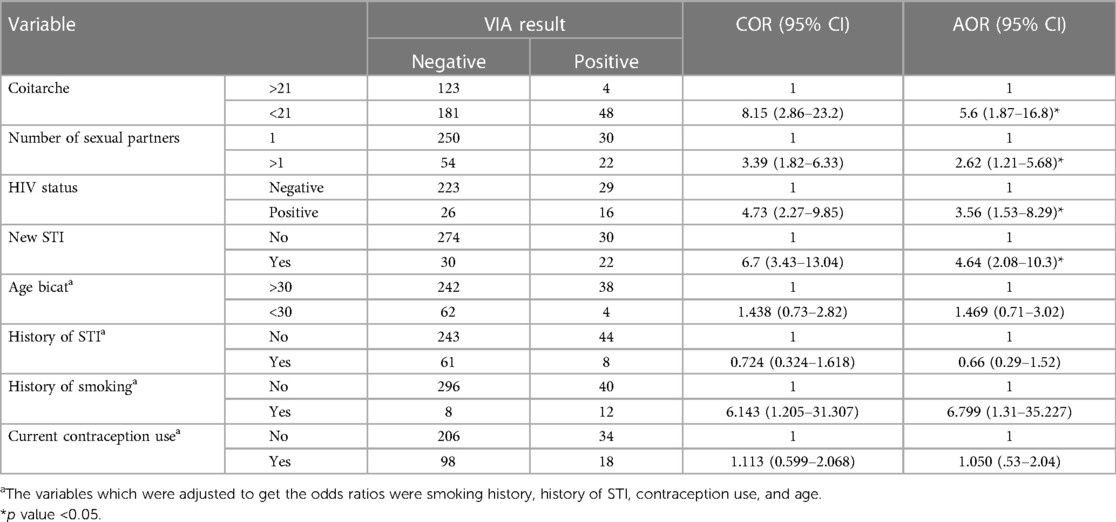
Table 4. Bivariable and multivariable logistic regression analysis of factors associated with precancerous cervical lesions among women screened for cervical cancer at HUCSH, 2021.
This study assessed the prevalence of precancerous cervical lesions and associated factors among women screened for cervical cancer at HUCSH in 2021. In this study, women were screened with visual inspection with acetic acid (VIA) for precancerous cervical lesions. Because VIA is less expensive and uses resources that are readily available locally, it is preferred in low-resource nations like Ethiopia. In this study, 18% had a suspicious precancerous cervical lesion, 14% were positive for precancerous cervical lesions tested by visual inspection with acetic acid, and 4.3% had lesions suspected to be cervical cancer.
The magnitude of precancerous cervical lesions in this study (14%) is consistent with the finding of a study in the Amhara region of northern Ethiopia (13.1%), and a systematic review and meta-analysis pooled the prevalence of cervical precancerous lesions among women in Ethiopia (13.4%) (9, 10).
Compared to other previous studies, the finding of the study is less than what was reported in a study conducted at Gandhi memorial hospital, Ethiopia, (23.5%) and a study conducted among women greater than 30 years of age in southern Ethiopia (27.7%) (11, 12). The discrepancy between our study and the one conducted in Addis Ababa can be due to the nature of the center in Addis Ababa where the study was conducted. Which is one of the main referral centers in the country for screening for cervical cancer for suspected cases from different parts of the country. On the other hand, the discrepancy with the findings of the second study can be attributed to the fact that the study was conducted among women older than 30 years of age in the urban areas of southern Ethiopia, whereas our study encompasses women from both rural and pastoral areas of the region.
On the other hand, this study's outcome is higher than studies from Cameroon (3.33%), Ghana (3.7%), India (1%), and Northeast Ethiopia (6.9%) (3, 13–15). This difference in the magnitude of the condition can be attributed to the fact that these studies are done among a large population in the community, including women not screened for cervical cancer, and over extended years.
In this study, women who had more than one sexual partner were found to have a 2.6 times higher risk for cervical precancerous lesion than those who reported having one sexual partner. This finding is supported by a result from a study conducted in Addis Ababa, Ethiopia, Northeast Ethiopia, southern Ethiopia, Addis Ababa, and other African countries (11, 12, 15–20). Sexual contact is the primary method of transmission for the human papillomavirus, which causes precancerous cervical lesions. As with other sexually transmitted diseases, the risk of acquiring the virus increases with having sexual intercourse with multiple partners as it increases the chance of having more frequent and unprotected coitus (1, 2).
In the study, women who were HIV positive were found to have 3.56 times greater odds of having precancerous cervical lesions than women who were HIV negative. This finding is supported by a study on the global burden of the disease and a study in northeast Ethiopia which shows that the pooled risk of cervical cancer was increased by sixfold in women living with HIV (15, 21). HIV and cervical cancer are inextricably linked. HIV-positive women are commonly assumed to have more risky sexual behavior than their counterparts. The immune system is crucial for eliminating cancer cells and reducing their development and dissemination. HIV-infected women have impaired cell-mediated immunity that makes them more prone to the cancerous effect of HPV; this sequence of risks exposes them to having a precancerous cervical lesion more easily than HIV-negative women (2, 22).
The study found that women who started having sexual intercourse before the age of 21 had 5.6 times higher odds of acquiring precancerous cervical lesions than those whose first sexual intercourse was above the age of 21 years. This result is in line with research conducted in Addis Ababa, southern Ethiopia, and the northeast of Ethiopia (12, 15, 17, 23). Because of the biological tendency of the young cervix during adolescence that may be more sensitive to chronic HPV infection, first sexual contact at an early age exposes one to the early acquisition of the HPV virus (24). Having sex at a younger age increases the chance of having sex for longer years in life, which, in turn, can raise the risk of acquiring cervical cancer (25).
In this study, women having new STI cases were found to have 4.64 times higher odds of being VIA positive for cervical cancer than those who had no STI at the time of screening. This finding is consistent with a study conducted in northeast Ethiopia, Amhara region in northern Ethiopia, and Gojjam in northwest Ethiopia (10, 15, 20, 26). The most prevalent sexually transmitted infection is the human papillomavirus (HPV), of which two types—HPV-16 and HPV-18—are responsible for approximately 50% of high-grade cervical pre-cancers (27). According to studies, Chlamydia bacteria and other STIs enable HPV to multiply and survive in the cervix, which may raise the risk of cervical cancer (3, 28). Furthermore, the fact that STIs and the virus that causes cervical cancer share a common route of transmission and risk factors can be linked to the high prevalence of cervical cancer among women with STIs (2).
In conclusion, this study found that the prevalence of precancerous cervical lesions in this study is higher than the pooled prevalence of precancerous cervical lesions in Ethiopia. To lower the prevalence of abnormal cervical lesions in the study area, the Federal Ministry of Health should concentrate on the primary prevention strategy (HPV vaccine) at an earlier stage. Many sexual partners, HIV positivity, having had sex before the age of 21, and a recent STI diagnosis were all separately linked to atypical precancerous cervical lesions.
Because our data is secondary, we were not able to find some of the medical records. Some information from the checklist which was important for our study was missing. Since it was an already prepared checklist and the participants could not be addressed at the time of the study, some additional associated factors were not assessed. Hence, the study can be generalized to women screened at this University hospital.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Institutional review board of Hawass University College of Medicine and Health Sciences. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
LT and WJ Conceived and designed the study and analyzed the data. AM and TY prepared the manuscript. All authors contributed to the article and approved the submitted version.
We would like to express our gratitude to the data collectors and record officers of HUCSH.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgwh.2023.1187916/full#supplementary-material.
HIV, human immunodeficiency virus; HPV, human papilloma virus; HUCSH, Hawassa University comprehensive specialized hospital; LMIC, low to middle-income countries; SCJ, squamocolumnar junction; STI, sexually transmitted infections; VIA, visual inspection with acetate; WHO, World Health Organization.
1. FMOH. Guideline for Cervical Cancer Prevention and Control in Ethiopia (2015). Addis Ababa: Federal Democratic Republic of Ethiopia Ministry of Health. https://www.iccp-portal.org/system/files/plans/Guideline%20Eth%20Final.pdf (Accessed February 7, 2023).
2. Hoffman B, Schorge J, Schaffer J, Halvorson L, Bradshaw K, Cunningham F. Williams Gynecology. 2nd ed. McGraw-Hill Professional (2012). 1401 p.
3. Nkfusai NC, Mubah TM, Yankam BM, Tambe TA, Cumber SN. Prevalence of precancerous cervical lesions in women attending Mezam Polyclinic Bamenda, Cameroon. Pan Afr Med J. (2019) 32:174. doi: 10.11604/pamj.2019.32.174.16895
4. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2021) 71(3):209–49. doi: 10.3322/caac.21660
5. De Martel C, Plummer M, Vignat J, Franceschi S. Worldwide burden of cancer attributable to HPV by site, country and HPV type. Int J Cancer. (2017) 141(4):664–70. doi: 10.1002/ijc.30716
6. Burt LM, McCormak M, Lecuru F, Kanyike DM, Bvochora-Nsingo M, Ndlovu N, et al. Cervix cancer in sub-Saharan Africa: an assessment of cervical cancer management. JCO Glob Oncol. (2021) 7:173–82. doi: 10.1200/GO.20.00079
7. Assefa AA, Astawesegn FH, Eshetu B. Cervical cancer screening service utilization and associated factors among HIV positive women attending adult ART clinic in public health facilities, Hawassa town, Ethiopia: a cross-sectional study. BMC Health Serv Res. (2019) 19:1. doi: 10.1186/s12913-018-3827-x
8. Gemeda EY, Kare BB, Negera DG, Bona LG, Derese BD, Akale NB, et al. Prevalence and predictor of cervical cancer screening service uptake among women aged 25 years and above in Sidama zone, Southern Ethiopia, using health belief model. Cancer Control. (2020) 27(1):1073274820954460. doi: 10.1177/1073274820954460
9. Zena D, Elfu B, Mulatu K. Prevalence and associated factors of precancerous cervical lesions among women in Ethiopia: a systematic review and meta-analysis. Ethiop J Health Sci. (2021) 31(1):189–200.34158766
10. Temesgen MM, Alemu T, Shiferaw B, Legesse S, Zeru T, Haile M, et al. Prevalence of oncogenic human papillomavirus (HPV 16/18) infection, cervical lesions and its associated factors among women aged 21–49 years in Amhara region, northern Ethiopia. Plos One. (2021) 16(3) e0248949.33760866
11. Mekuria M, Edosa K, Endashaw M, Bala ET, Chaka EE, Deriba BS, et al. Prevalence of cervical cancer and associated factors among women who attended cervical cancer screening center at Gahandi memorial hospital, Ethiopia. Cancer Inform. (2021) 20:11769351211068431. doi: 10.1177/11769351211068431
12. Teka T, Kote M, Kejela G, Getachew T. Magnitude and factors associated with precervical cancer among screened women in southern Ethiopia. Adv Public Health. (2019) 2019. doi: 10.1155/2019/5049752
13. Donkoh ET, Agyemang-Yeboah F, Asmah RH, Wiredu EK. Prevalence of cervical cancer and pre-cancerous lesions among unscreened women in Kumasi, Ghana. Medicine (Baltimore). (2019) 98(13):e14600. doi: 10.1097/MD.0000000000014600
14. Kalavathy MC, Mathew A, Krishna KJ, Saritha VN, Sujathan K. Risk factors and prevalence of cervical squamous intraepithelial lesions among women in south India: a community-based cross-sectional study. Indian J Cancer. (2022) 59(1):95–100. doi: 10.4103/ijc.IJC_699_19
15. Temesgen K, Workie A, Dilnessa T, Abate M. Proportions of pre-cancerous cervical lesions and its associated factors among women clients in the age group of 30−49yrs in gynecology ward of dessie referral hospital and FGAE, north-east Ethiopia, 2016. J Cancer Tumor Int. (2019) 9(2):1–15. doi: 10.9734/jcti/2019/v9i230105
16. World Health Organization and International Agency for Research on Cancer. Prevention of cervical cancer through screening using visual inspection with acetic acid (VIA) and treatment with cryotherapy. A demonstration project in six African countries: Malawi, Madagascar, Nigeria, Uganda, the United Republic of Tanzania, and Zambia (2012). Available at: https://www.who.int/publications/i/item/9789241503860 (Accessed February 5, 2023).
17. Teame H, Addissie A, Ayele W, Hirpa S, Gebremariam A, Gebreheat G, et al. Factors associated with cervical precancerous lesions among women screened for cervical cancer in Addis Ababa, Ethiopia: a case-control study. PloS One. (2018) 13(1):e0191506. doi: 10.1371/journal.pone.0191506
18. Weldegebreal F, Worku T. Precancerous cervical lesion among HIV-positive women in sub-Saharan Africa: a systematic review and meta-analysis. Cancer Control. (2019) 26(1):1073274819845872. doi: 10.1177/1073274819845872
19. Ali-Risasi C, Verdonck K, Padalko E, Vanden Broeck D, Praet M. Prevalence and risk factors for cancer of the uterine cervix among women living in Kinshasa, the democratic republic of the Congo: a cross-sectional study. Infect Agents Cancer. (2015) 10:1–11. doi: 10.1186/s13027-015-0015-z
20. Jolly PE, Mthethwa-Hleta S, Padilla LA, Pettis J, Winston S, Akinyemiju TF, et al. Screening, prevalence, and risk factors for cervical lesions among HIV positive and HIV negative women in Swaziland. BMC Public Health. (2017) 17(1):1–8. doi: 10.1186/s12889-017-4120-3
21. Stelzle D, Tanaka LF, Lee KK, Khalil AI, Baussano I, Shah AS, et al. Estimates of the global burden of cervical cancer associated with HIV. Lancet Glob Health. (2021) 9(2):e161–9. doi: 10.1016/S2214-109X(20)30459-9
22. Choudhury SA, Choudhury NA, Humphrey AD, Berthaud V, Ladson G, Tucker VA, et al. Higher prevalence of human papillomavirus-related cervical precancerous abnormalities in HIV-infected compared to HIV-uninfected women. J Natl Med Assoc. (2016) 108(1):19–23. doi: 10.1016/j.jnma.2015.12.003
23. Makuza JD, Nsanzimana S, Muhimpundu MA, Pace LE, Ntaganira J, Riedel DJ. Prevalence and risk factors for cervical cancer and pre-cancerous lesions in Rwanda. Pan Afr Med J. (2015) 22:1. doi: 10.11604/pamj.2015.22.26.7116
24. Abebe M, Eshetie S, Tessema B. Prevalence of sexually transmitted infections among cervical cancer suspected women at university of Gondar comprehensive specialized hospital, north-west Ethiopia. BMC Infect Dis. (2021) 21(1):1–7. doi: 10.1186/s12879-021-06074-y
25. Liu ZC, Liu WD, Liu YH, Ye XH, Chen SD. Multiple sexual partners as a potential independent risk factor for cervical cancer: a meta-analysis of epidemiological studies. Asian Pac J Cancer Prev. (2015) 16(9):3893–900. doi: 10.7314/APJCP.2015.16.9.3893
26. Getinet M, Taye M, Ayinalem A, Gitie M. Precancerous lesions of the cervix and associated factors among women of east Gojjam, northwest Ethiopia, 2020. Cancer Manag Res. (2021) 2021:9401–10. doi: 10.2147/CMAR.S338177
27. UN AIDS. HIV and cervical cancer. United Nations. (2022). Available at: https://www.unaids.org/en/resources/documents/2022/HIV-and-cervical-cancer (Accessed at 6 February 2023).
Keywords: magnitude, precancerous cervical lesion, cervical cancer, associated factors, southern Ethiopia
Citation: Tenkir L, Mamuye A, Jemebere W and Yeheyis T (2023) The magnitude of precancerous cervical lesions and its associated factors among women screened for cervical cancer at a referral center in southern Ethiopia, 2021: a cross-sectional study. Front. Glob. Womens Health 4:1187916. doi: 10.3389/fgwh.2023.1187916
Received: 16 March 2023; Accepted: 23 June 2023;
Published: 16 August 2023.
Edited by:
Mwansa Ketty Lubeya, University of Zambia, ZambiaReviewed by:
Masangu Mulongo, Wits Health Consortium (WHC), South Africa© 2023 Tenkir, Mamuye, Jemebere and Yeheyis. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tomas Yeheyis dHllaGV5aXNAZ21haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.