- 1Department of Psychology, Institute of Population Health, University of Liverpool, Liverpool, United Kingdom
- 2Department of Women & Children’s Health, School of Life Course & Population Sciences, King’s College London, London, United Kingdom
- 3Department of Nutritional Sciences, School of Life Course & Population Sciences, King’s College London, London, United Kingdom
Introduction: Infant and maternal breastfeeding benefits are well documented, globally. Despite efforts to increase global breastfeeding rates, the majority of high-income settings fall short of recommended targets. Breastfeeding rates in the UK are especially poor, and physiological difficulties (e.g., inverted nipples), fail to account for the observed breastfeeding intention-behaviour gap.
Method: The current online study sought to investigate the infant feeding experiences of 624 UK formula feeding mothers, through open text survey responses.
Results: A content analysis identified the following clusters of reasons for formula feeding: Feeding Attitudes, Feeding Problems, Mental Health, and Sharing the Load.
Discussion: Feeding Attitudes explained a large percentage of reasons given for formula feeding. Recommendations are made to improve antenatal breastfeeding education and to develop an intervention with an aim to improve maternal breastfeeding attitudes and subsequent practice. Feeding Problems also explained a large portion of combination feeding and started but stopped infant feeding accounts. The current paper calls for more comprehensive and tailored antenatal breastfeeding education to refine practical breastfeeding skills necessary for successful breastfeeding establishment and maintenance. Mental Health explained relatively small coverage. Suggestions are therefore made to train mental health practitioners on infant feeding with an aim to provide more extensive support, which may serve to disrupt the bidirectional relationship between poor mental health and poor breastfeeding outcomes. Finally, Sharing the Load explained moderate coverage across never breastfed, combination fed, and started but stopped feeding groups. Recommendations are made, in light of these findings, to tighten workplace legislation to protect breastfeeding women.
1. Introduction
Infant and maternal breastfeeding benefits are well documented, globally (1, 2). Breastfeeding also has wide-reaching benefits at economic, social, and environmental levels within a community, creating significant national economic savings (3). The World Health Organization (WHO) draw on this extensive evidence base in recommending exclusive breastfeeding for the first six months following birth, and continued breastfeeding to two years of age and beyond (4). Ambitions have been posed to increase global six-month exclusive breastfeeding rates to 50% by 2025 (5). Currently, UK rates severely fall below official recommendations, at fewer than 1% (6). Physiological difficulties e.g., hypoplastic breasts, are unable to account for this intention-behaviour gap (7). Infant feeding decision-making is complex and determined by structural, setting, and individual level determinants (2), which will be considered in turn.
Public breastfeeding attitudes are contradictory in the UK: pro-public breastfeeding discourse is widespread across UK healthcare settings, parenting forums, and in media portrayals of infant feeding (8, 9), while simultaneously only being supported when discrete (9). Formula milk manufacturers can take advantage of maternal insecurities and proliferate misinformation with an aim to increase formula milk purchasing, which also undermines breastfeeding confidence (10). Currently, advertisement of infant foods and drinks is ineffectively regulated in the UK, allowing for aggressive formula milk marketing strategies to remain widespread in the UK (10) which has a unilateral effect on infant feeding decision-making postpartum.
Quality of health services and antenatal care influence infant feeding decision-making at a community level (2). Women who receive antenatal guidance about breastfeeding benefits were more likely to initiate breastfeeding after birth (6). Although, protective services e.g., the Healthy Child Programme (which delivers five mandatory health checks between the 28th week of pregnancy to five years postpartum (11); have suffered from reduced capacity, resourcing, and financial investment in recent years (12). Of mothers experiencing breastfeeding difficulties, 20% did not receive advice from their healthcare team, which elevated risks of early breastfeeding cessation (12). Positive breastfeeding attitudes of relatives and romantic partners facilitate breastfeeding continuation (13), while insufficient support increases the risk of early breastfeeding cessation (14). Vicarious exposure to breastfeeding within one's friendship group, too, increases likelihood of breastfeeding for an individual (6).
Personal attributes and quality of the mother-infant relationship determine postpartum infant feeding choice (2). Higher breastfeeding self-efficacy and more positively held attitudes towards breastfeeding were significantly, positively associated with breastfeeding intention and continuation (15, 16). Breastfeeding challenges are, on the other hand, notable deterrents against breastfeeding continuation (14). Most frequently reported breastfeeding challenges included: perception of poor infant feeding technique, fear of infant not receiving enough breastmilk, excessive vomiting/reflux, perceived insufficient milk-supply, positioning and latching problems, infant rejection of the breast, and painful breasts/nipples (17, 18). Perinatal mental health problems are prevalent (10%–20%) and too can negatively impact breastfeeding outcomes (19). Postnatal depression has been significantly associated with poorer breastfeeding self-efficacy, any breastfeeding status or continuation (20). The relationship between postnatal anxiety and breastfeeding outcomes follows a similar trend (21).
Nevertheless, UK breastfeeding rates have been slowly increasing in recent decades (22). Rising trends are concurrent with increasing efforts to implement Baby Friendly Initiative (BFI) standards (23). BFI adoption has been linked with improved initiation and continuation rates in international, observational studies (24). However, the mid- and long-term impacts of BFI implementation on child health outcomes in high income settings are more contested (25). BFI-informed care has been criticised for overlooking sociocultural and structural barriers (26) and for promoting unrealistic breastfeeding expectations which manifest feelings of guilt and disappointment (26).
Collectively, one-dimensional promotional models appear ineffective for optimising breastfeeding outcomes, when compared with individualised initiatives and multicomponent interventional efforts (25, 27, 28). Pre-existing promotional strategies have also been ineffective in supporting breastfeeding continuation in line with WHO guidelines.
2. Materials and methods
The current study sought to understand, in greater depth, the infant feeding experiences and difficulties of women in the United Kingdom, in their first six months postpartum. The online survey was advertised via social media and online parenting forums and was completed by mothers (N = 624, MAge = 29.44 years) of infants (MAge = 17.96 weeks) who: Never Breastfed (NB, n = 158); Started, But Stopped Breastfeeding (SBS, n = 278); and who Combination Fed (CF, n = 188). We used mothers' qualitative responses to the question: “What were the main reasons you chose to formula feed your baby?” to address the following aims: (a) To investigate reasons given for not breastfeeding; and (b) To illuminate commonalities in reasoning across feeding groups.
The study received ethical approval from the University of Liverpool Institute of Psychology, Health and Society Research Ethics Committee (ref:- IPH/2047). All participants provided consent to participate on the first page of the on-line survey.
We utilised a qualitative content analysis (29) to allow for the content of this heterogenous textual data to be codified using a systematic process of categorisation, to produce thematic clusters derived from the text which can then be interpreted.
In the first organising phase: open coding, classification, and abstraction were undertaken, where two researchers were responsible for the creation of possible thematic clusters. These were labelled and categories were organised into these thematic clusters. This was followed by the coding phase, where the textual excerpts were read numerous times before being assigned to the appropriate thematic cluster, and coding were then categorised (i.e., all codes were assigned to thematic clusters). Finally, thematic clusters were assessed for thematic overlap and those clusters which were similar were made into broader clusters to minimise the number of overall thematic clusters. The presentation of results is always the final step in content analysis, which we have provided in a tabular format.
Coding and analysis were consultative whereby if different coding was identified, comparisons were made and researchers worked to compromise over nuance and semantic differences. Another researcher would arbitrate if agreement could not be reached.
The final sample of this qualitative analysis included 624 mothers. Frequencies were calculated to provide the number of occurrences of a particular code within the responses across all thematic clusters, and results were stratified by the three participant groups (NB; SBS; CF) to allow for comparison and observation of results across all participants. A proportion of our final sample (12.55%) did not provide open text responses or gave illegible responses e.g.,: “choose”, which were excluded from analysis.
3. Results
All themes identified during the analysis of 624 respondents are presented in Table 1. Infant feeding experiences and difficulties reported by respondents were sorted in to four thematic clusters: Feeding Problems; Mental Health; Feeding Attitudes; and Sharing the Load. Thematic clusters were split by infant feeding method: Never Breastfed (NB); Started but Stopped Breastfeeding (SBS); and Combination Feeding (CF).
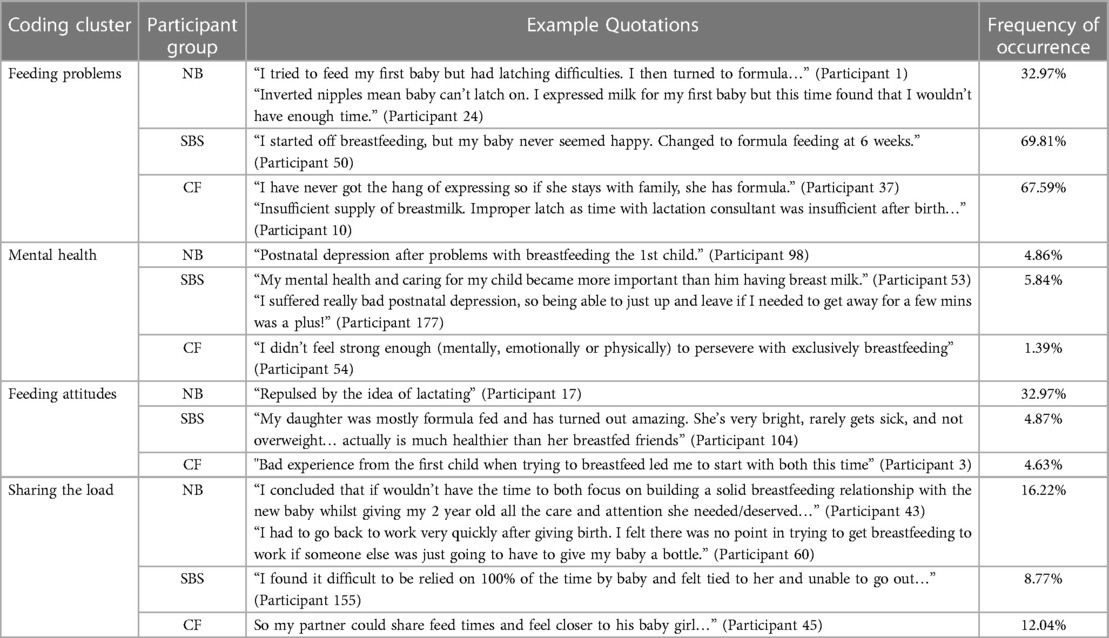
Table 1. Clusters of themes identified from content analysis, with provided examples in the form of statements and percentages.
3.1. Feeding problems
For CF mothers, 67.59% reported feeding difficulties. Infant feeding difficulties centred around perceived insufficient milk supply, poor latching technique, and practical difficulties expressing breastmilk. For SBS mothers, 69.81% also articulated feeding problems, though for these women difficulties were more infant-focused, describing infant as being dissatisfied with breastmilk which led to early breastfeeding cessation. Feeding difficulties were reported by 32.97% of NB mothers, also.
3.2. Mental health
Coverage for mental health difficulties among SBS mothers was minimal with only 5.84% reporting data coded within this thematic cluster. For these women, postnatal depression ensued following experience of stubborn breastfeeding challenges. 4.86% of NB mothers reported mental health difficulties. For these women, the convenience and flexibility which formula milk provided with regards to allowing the mother to engage in self-care activities and to care for her infant outweighed the benefits of breastfeeding. Mental health difficulties were reported by 1.39% of CF mothers, also.
3.3. Feeding attitudes
There was minimal coverage of feeding attitudes by CF mothers with just 4.63% reporting, and likewise for SBS mothers who had 4.87% reporting frequency. Reasons provided for poor feeding attitudes included negative experiences of breastfeeding attempts with older children and holding positive attitudes about the development of the mother's older, formula fed children, respectively. However, NB mothers reported more negative attitudes towards breastfeeding with 32.97% recalling data covered by this thematic cluster. For these women attitudes were held more strongly about the idea of breastfeeding, conceptually.
3.4. Sharing the load
CF and SBS mothers expressed sharing the load as reasons for their infant feeding method, with 12.04% and 8.77% reporting data, respectively. More NB mothers reported on this theme, at 16.22%. NB mothers noted formula feeding allowed the mother to balance infant care responsibilities more easily with parenting responsibilities for older children and with employment-based responsibilities.
4. Discussion
4.1. Summary of findings
A content analysis was conducted on open text, online survey responses collected from 624 from NB, SBS, and CF mothers. The content analysis identified four themes pertaining to reasons given for formula feeding method, which were: feeding problems, mental health, feeding attitudes, and sharing the load.
Feeding problems had comparatively large percentage coverage in reasons provided for formula feeding method. This was observed across CF and SBS groups, with mothers specifically commenting on difficulties establishing a successful breastfeeding latch. These findings parallel previous literature, which also reports practical breastfeeding difficulties, such as unsuccessful latching, to be a primary reason given for early breastfeeding cessation (17, 30–33). Previous literature has shown that professional prenatal breastfeeding education can increase latch skills, reduce nipple damage during breastfeeds (34), and extend breastfeeding duration (though methodological heterogeneity and poor research quality contribute towards mixed findings, and limits the ability to form firm conclusions (35). This suggests that specialised maternal support may serve to acknowledge and address breastfeeding issues, reinforcing calls for action reported in pre-existing infant feeding literature (36).
Unsurprisingly, those who NB did not disclose feeding problems. Formula feeding is an attractive infant feeding option for mothers with busy lifestyles (37). However, current findings demonstrate that a proclivity to breastfeed may be sourced in insufficient knowledge, supporting the notion that breastfeeding is a learned skill (38). Feeding problems are inherently linked with poorer understanding and refinement of breastfeeding skills (39, 40). Comprehensive and tailored education and support throughout pregnancy and the postpartum might deem breastfeeding a more viable option for new mothers.
Mental health was an underlying reason for formula feeding among all infant feeding groups. Specifically, formula feeding alleviated depressive symptoms for mothers in the current and in previous studies (41). This finding is concurrent with previous trends identifying a relationship between postnatal depression and poor breastfeeding exclusivity and duration (20, 42). Depressive symptoms disrupt the production of hormones involved in breastfeeding e.g., milk ejection reflex (43–45). Conversely, breastfeeding significantly increases levels of oxytocin and subsequent emotional recognition (46), which is important for emotional processing of stress, anxiety, and for sensitivity to infant affect (47). Improving accessibility to postnatal mental health support could act as a circuit break in the bidirectional relationship between maternal mental ill-health and poor breastfeeding outcomes (48–50), and may serve to improve both maternal emotional wellbeing and breastfeeding outcomes. Providing mental health providers with infant feeding education results in the provision of better tailored psychological support (49), which is a key recommendation of this paper.
Feeding attitudes were also proportionately large predictors of formula feeding status among all three groups. Positive breastfeeding attitudes being held by relatives and partners of the mother facilitate breastfeeding continuation (51), whereas negatively held attitudes can pose as notable barriers to successful breastfeeding practice (52). Infant feeding attitude held during pregnancy has shown stability over time, predicting breastfeeding initiation, duration, and exclusivity (53). In the current study, negative breastfeeding experiences with previous children averted mothers from attempting breastfeeding with their youngest infant, consistent with previous literature (54).
Feeding attitudes were an especially notable predictor for NB mothers. Pro-formula feeding attitudes predict exclusivity more so than knowledge of breastfeeding benefits (55), and evidence suggests that formula feeding women commonly hold misconceptions about breastfeeding (56). Among formula feeding women, previous breastfeeding experiences significantly predicted breastfeeding initiation and duration in subsequent births (57) and more positive formula feeding attitudes predicted formula feeding intention during pregnancy (56). Feeding attitudes are malleable (53), and intervention-based studies have shown utility in improving breastfeeding attitudes and postpartum outcomes (58).
On the topic of intervention research—morally charged promotional breastfeeding discourse can unintentionally cultivate feelings of guilt and shame for those who cannot, or do not breastfeed (59, 60). It is therefore important for intervention efforts to remain mindful of potential ramifications of “breast is best” discourse, and to adopt an incremental goal setting approach to behaviour change (61). Current findings also support the notion that formula feeding attitudes and breastfeeding attitudes are not antagonistic, but rather independent (62). Positive formula feeding attitudes are predictive of breastfeeding cessation (63). Targeting positively held attitudes towards formula milk, over promoting positive attitudes towards breastmilk, is a potential avenue for intervention (10).
The final major theme, sharing the load, was cited by mothers across all feeding methods, but was especially pronounced among NB mothers. Breastfeeding is a resource-taxing infant feeding method which places sole caregiving responsibility on the mother (64). Breastfeeding, therefore, can be especially difficult for mothers balancing conflicting social identities e.g., balancing childcare and work responsibilities (2, 65). Practical support from one's maternal grandmother (66), romantic partner (67), and from one's employer (68, 69) can ease the perceived demands of breastfeeding. Consequently, sharing the load may reflect perceived insufficient support from one's social support network and/or insufficient advocation of one's needs early postpartum. In the current study, sharing the load encompassed difficulties in finding private space(s) to breastfeed and struggling to manage infant feeding demands and work responsibilities (70). Although workplace protection exists for breastfeeding women (71) which positively impacts breastfeeding outcomes for working mothers (72), employer adherence to these guidelines is mixed (2, 73). Greater adherence to the WHO code on Marketing of Breastmilk Substitutes (10), which, among other legislative forms of protection, mandates breastfeeding employers are reasonably supported in returning to work while nursing e.g., flexible working hours, implementation of expression rooms, might serve to improve breastfeeding outcomes for working mothers.
4.2. Strengths limitations, and future research
The methodological framework adopted in the current study allowed for formula feeding participants to share candid responses regarding the often ‘taboo’ subject of breastfeeding cessation (59, 60). It was important that this element of social desirability was controlled, in a demographic where feeling inadequate and dejected socially is commonplace (74). A sampling bias exists in perinatal literature, whereby the majority of participants tend to be exclusive or partial breastfeeders (59). Online data collection enabled a large sample of formula feeding women to be recruited, comparable to previously published infant feeding quantitative works (75). However, the open text response format in the survey lacked control over quality of respondent answers, with some participants providing vagaries. In the current study, women self-identified their formula feeding status. Reliance on self-identification in some instances led to discrepancies with researcher understanding of infant feeding categories, which may have led to misclassification e.g., a proportion of our sample self-identified as NB, while in-text they reported having given one breastfeed postpartum. Self-identification is, however, paramount in one's interpretation of events (76). Gaining the insights and perceptions of these women was essential for addressing study aims, warranting the self-reported data collection method. Furthermore, due to the self-selecting nature of the research, it could be possible that participants with negative experiences presented to the research, whereas those with neutral or positive experiences of breastfeeding may have chosen not to participate. Within the current methodological design, reasons for breastfeeding cessation were recorded retrospectively, meaning that may have increased chances of response bias.
4.3. Conclusions
The current study used content analysis on open text, online survey responses collected from 624 NB, SBS, and CF mothers to address the following aims: (a) To investigate reasons given for not breastfeeding, and (b) To illuminate commonalities in reasoning across feeding groups. Feeding problems explained a large percentage coverage in reasons for formula feeding. The current study recommends comprehensive prenatal breastfeeding educational programmes to address feeding difficulties commonly experienced during the early postpartum and to encourage those with formula feeding intent to consider breastfeeding as a viable infant feeding option. Improving accessibility to and quality of perinatal mental health support services may serve as a circuit break for the bidirectional relationship between maternal mental ill health and poor breastfeeding outcomes. Interventions are proposed, which adopt an incremental goal setting approach to breastfeeding, and are recommended to alter breastfeeding attitudes more favourably for formula feeding mothers. Finally, tighter legislation on workplace protection of lactating mothers and active encouragement of the maternal family unit's support and advocation of breastfeeding practice are recommended to support women who wish to breastfeed.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The study received ethical approval from the University of Liverpool Institute of Psychology, Health and Society Research Ethics Committee (ref:- IPH/2047). The participants provided their informed consent to participate in this study.
Author contributions
Conceptualisation: VF; Methodology: SAS; Validation: PD; Formal Analysis: DR, LJ; Investigation: VF, SAS, PD; Resources: VF; Data Curation: DR; Writing—Original Draft: DR, LJ, CZ; Writing—Review & Editing: SAS, VF, JAH, PD; Visualization: DR, LJ; Supervision: VF, SAS; Project Administration: VF, SAS. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Victora CG, Bahl R, Barros AJD, França GVA, Horton S, Krasevec J, et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. (2016) 3879(10017):475–90. doi: 10.1016/S0140-6736(15)01024-7
2. Rollins NC, Bhandari N, Hajeebhoy N, Horton S, Lutter CK, Martines JC, et al. Why invest, and what it will take to improve breastfeeding practices? Lancet. (2016) 387(10017):491–504. doi: 10.1016/S0140-6736(15)01044-2
3. Pokhrel S, Quigley MA, Fox-Rushby J, McCormick F, Williams A, Trueman P, et al. Potential economic impacts from improving breastfeeding rates in the UK. Arch Dis Child. (2015) 100(4):334–40. doi: 10.1136/archdischild-2014-306701
4. WHO. Infant and young child feeding. Accessed on 20 Dec 2022: https://www.who.int/news-room/fact-sheets/detail/infant-and-young-child-feeding (2020).
5. WHO/UNICEF. Global nutrition targets 2025: breastfeeding policy brief. Accessed on 18 Dec 2022: https://apps.who.int/iris/handle/10665/149022 (2014).
6. McAndrew F, Thompson J, Fellows L, Large A, Speed M, Renfrew MJ. Infant Feeding Survey 2010: Summary. Accessed on 19 Dec 2022: https://files.digital.nhs.uk/publicationimport/pub08xxx/pub08694/ifs-uk-2010-sum.pdf (2012).
7. Brown A. Breastfeeding as a public health responsibility: a review of the evidence. J Hum Nutr Diet. (2017) 30(6):759–70. doi: 10.1111/jhn.12496
8. Merritt R, Vogel M, Ladbury P, Johnson S. A qualitative study to explore fathers’ attitudes towards breastfeeding in south west England. Prim Health Care Res Dev. (2019) 20:1–7. doi: 10.1017/S1463423618000877
9. Morris C, De La Fuente GAZ, Williams CET, Hirst C. UK Views toward breastfeeding in public: an analysis of the public’s response to the claridge’s incident. J Hum Lact. (2016) 32(3):472–80. doi: 10.1177/0890334416648934
10. WHO. How the marketing of formula milk influences our decisions on infant feeding. Accessed 19 Dec 2022: https://www.who.int/teams/maternal-newborn-child-adolescent-health-andageing/formula-milk-industry (2022).
11. Department of Health. Healthy child programme: Pregnancy and the first five years of life. Accessed on 20 Dec 2022: https://www.gov.uk/government/publications/healthy-child-programme-pregnancy-and-the-first-5-years-of-life (2009).
12. UNICEF UK. Removing the barriers to breastfeeding: A call to action how removing barriers can give babies across the UK the best start in life. Accessed on 20 Dec 2022: https://www.unicef.org.uk (2017).
13. Ingram J, Rosser J, Jackson D. Breastfeeding peer supporters and a community support group: evaluating their effectiveness. Matern Child Nutr. (2005) 1(2):111-8. doi: 10.1111/j.1740-8709.2005.00005.x
14. Mangrio E, Persson K, Bramhagen AC. Sociodemographic, physical, mental and social factors in the cessation of breastfeeding before 6 months: a systematic review. Scand J Caring Sci. (2018) 32(2):451–65. doi: 10.1111/scs.12489
15. Brockway M, Benzies K, Hayden KA. Interventions to improve breastfeeding self-efficacy and resultant breastfeeding rates: a systematic review and meta-analysis. J Hum Lact. (2017) 33(3):486-99. doi: 10.1177/0890334417707957
16. Hoddinott P, Allan K, Avenell A, Britten J. Group interventions to improve health outcomes: a framework for their design and delivery. BMC Public Health. (2010) 10:800. doi: 10.1186/1471-2458-10-800
17. Teich AS, Barnett J, Bonuck K. Women's perceptions of breastfeeding barriers in early postpartum period: a qualitative analysis nested in two randomized controlled trials. Breastfeed Med. (2014) 9(1):9–15. doi: 10.1089/bfm.2013.0063
18. PHE. New survey of mums reveals perceived barriers to breastfeeding. Accessed on 19 Dec 2022: https://www.gov.uk/government/news/new-survey-of-mums-reveals-perceived-barriers-to-breastfeeding (2017).
19. Bauer A, Parsonage M, Knapp M, Iemmi V, Adelaja B. The costs of perinatal mental health problems. Accessed on 20 Dec 2022: http://eprints.lse.ac.uk/59885/1/__lse.ac.uk_storage_LIBRARY_Secondary_libfile_shared_repository_Content_Bauer%2C%20M_Bauer_Costs_perinatal_%20mental_2014_Bauer_Costs_perinatal_mental_2014_author.pdf (2014).
20. Dennis CL, McQueen K. Does maternal postpartum depressive symptomatology influence infant feeding outcomes? Acta paediatrica. Int J Paediatr. (2007) 96(4):590–4. doi: 10.1111/j.1651-2227.2007.00184.x
21. Fallon V, Groves R, Halford JCG, Bennett KM, Harrold JA. Postpartum anxiety and infant-feeding outcomes: a systematic review. J Hum Lact. (2016) 32(4):740–58. doi: 10.1177/0890334416662241
22. PHE. Breastfeeding prevalence at 6-8 weeks after birth (Experimental Statistics) 2018/19 Annual Data Statistical Commentary. Accessed on 19 Dec 2022: http://www.gov.uk/phe (2019).
23. Pound CM, Unger SL. The baby-friendly initiative: protecting, promoting, and supporting breastfeeding. Paediatr Child Health. (2012) 17(6):317–21. doi: 10.1093/pch/17.6.317
24. Cleminson J, Oddie S, Renfrew MJ, McGuire W. Being baby friendly: evidence-based breastfeeding support. Arch Dis Child. (2015) 100(2):173–8. doi: 10.1136/archdischild-2013-304873
25. Fallon VM, Harrold JA, Chisholm A. The impact of the UK baby friendly initiative on maternal and infant health outcomes: a mixed-methods systematic review. Matern Child Nutr. (2019) 15(3):1–22. doi: 10.1111/mcn.12778
26. Groleau D, Sigouin C, D'souza NA. Power to negotiate spatial barriers to breastfeeding in a western context: when motherhood meets poverty. Health Place. (2013) 24:250-9. doi: 10.1016/j.healthplace.2013.08.011
27. Schmied V, Beake S, Sheehan A, McCourt C, Dykes F. Women’s perceptions and experiences of breastfeeding support: a metasynthesis. Birth. (2011) 38(1):49–60. doi: 10.1111/j.1523-536X.2010.00446.x
28. Sinha B, Chowdhury R, Sankar MJ, Martines J, Taneja S, Mazumder S, et al. Interventions to improve breastfeeding outcomes: a systematic review and meta-analysis. Acta Paediatr. (2015) 104(467):114–34. doi: 10.1111/apa.13127
29. Hsieh HF, Shannon S. Three approaches to qualitative content analysis. Qual Health Res. (2005) 15:1277–88. doi: 10.1177/1049732305276687
30. Odom EC, Li R, Scanlon KS, Perrine CG, Grummer-Strawn L. Reasons for earlier than desired cessation of breastfeeding. Pediatrics. (2013) 131(3):726–32. doi: 10.1542/peds.2012-1295
31. Morrison AH, Gentry R, Anderson J. Mothers’ reasons for early breastfeeding cessation. MCN. The Am J Matern Child Nurs. (2019) 44(6):325–30. doi: 10.1097/NMC.0000000000000566
32. Davie P, Chilcot J, Jones L, Bick D, Silverio SA. Indicators of ‘good’ feeding, breastfeeding latch, and feeding experiences among healthy women with healthy infants: A qualitative pathway analysis using grounded theory. Women and Birt. (2021) 34(4):e357-e367. doi: 10.1016/j.wombi.2020.08.004
33. Davie P, Bick D, Silverio SA, Chilcot J. Easier, but not easy: Testing a grounded theory of breastfeeding experiences among women with larger birthweight infants. Psychology & Healt. (2023) 38(2):167-89. doi: 10.1080/08870446.2021.1956495
34. Gao H, Wang J, An J, Liu S, Li Y, Ding S, et al. Effects of prenatal professional breastfeeding education for the family. Sci Rep. (2022) 12(1):1–4. doi: 10.1038/s41598-022-09586-y
35. Wong KL, Tarrant M, Lok KYW. Group versus individual professional antenatal breastfeeding education for extending breastfeeding duration and exclusivity: a systematic review. J Hum Lact. (2015) 31(3):354–66. doi: 10.1177/0890334415583294
36. Gianni ML, Bettinelli ME, Manfra P, Sorrentino G, Bezze E, Plevani L, et al. Breastfeeding difficulties and risk for early breastfeeding cessation. Nutrients. (2019) 11(10):1–10. doi: 10.3390/nu11102266
37. Zhang K, Tang L, Wang H, Qiu L, Binns CW, Lee AH. Why do mothers of young infants choose to formula feed in China? Perceptions of mothers and hospital staff. Int J Environ Res Public Health. (2015) 12(5):4520–32. doi: 10.3390/ijerph120504520
38. Gavine A, MacGillivray S, Renfrew MJ, Siebelt L, Haggi H, McFadden A. Education and training of healthcare staff in the knowledge, attitudes and skills needed to work effectively with breastfeeding women: a systematic review. Int Breastfeed J. (2017) 12(6):1–10. doi: 10.1186/s13006-016-0097-2
39. Hilmiye A, Mert K, Gülergün D. The effect of postnatal breastfeeding education/support offered at home 3 days after delivery on breastfeeding duration and knowledge: a randomized trial. J Matern Fetal Neonatal Med. (2011) 24(2):354–61. doi: 10.3109/14767058.2010.497569
40. Wood N, Woods N, Blackburn S, Sanders EA. Interventions that enhance breastfeeding initiation, duration, and exclusivity: a systematic review. Am J Matern Child Nurs. (2016) 41(5):299–307. doi: 10.1097/NMC.0000000000000264
41. Wouk K, Stuebe AM, Meltzer-Brody S. Postpartum mental health and breastfeeding practices: an analysis using the 2010-2011 pregnancy risk assessment monitoring system. Matern Child Health J. (2017) 21(3):636–47. doi: 10.1007/s10995-016-2150-6
42. Lewis CA, Kimmig AS, Zsido RG, Jank A, Derntl B, Sacher J. Effects of hormonal contraceptives on mood: a focus on emotion recognition and reactivity, reward processing, and stress response. Curr Psychiatry Rep. (2019) 21(11):115. doi: 10.1007/s11920-019-1095-z
43. Deif R, Burch EM, Azar J, Yonis N, Abou Gabal M, El Kramani N, et al. Dysphoric milk ejection reflex: the psychoneurobiology of the breastfeeding experience. Front Glob Womens Health. (2021) 2:669826. doi: 10.3389/fgwh.2021.669826
44. Golan Y, Assaraf YG. Genetic and physiological factors affecting human milk production and composition. Nutrients. (2020) 12(5):1–20. doi: 10.3390/nu12051500
45. Heise AM, Wiessinger D. Dysphoric milk ejection reflex: a case report. Int Breastfeed J. (2011) 6(1):1–7. doi: 10.1186/1746-4358-6-6
46. Matsunaga M, Kikusui T, Mogi K, Nagasawa M, Ooyama R, Myowa M. Breastfeeding dynamically changes endogenous oxytocin levels and emotion recognition in mothers. Biol Lett. (2020) 16(6):1–6. doi: 10.1098/rsbl.2020.0139
47. Seeley WW, Menon V, Schatzberg AF, Keller J, Glover GH, Kenna H, et al. Dissociable intrinsic connectivity networks for salience processing and executive control. J Neurosci. (2007) 27(9):49–56. doi: 10.1523/JNEUROSCI.5587-06.2007
48. Borra C, Iacovou M, Sevilla A. New evidence on breastfeeding and postpartum depression: the importance of understanding women's intentions. Matern Child Health J. (2015) 19(4):897–907. doi: 10.1007/s10995-014-1591-z
49. Rivi V, Petrilli G, Blom JMC. Mind the mother when considering breastfeeding. Front Global Women's Health. (2020) 1(3):1–5. doi: 10.3389/fgwh.2020.00003
50. Ystrom E. Breastfeeding cessation and symptoms of anxiety and depression: a longitudinal cohort study. BMC Pregnancy Childbirth. (2012) 12:1–6. doi: 10.1186/1471-2393-12-36
51. Davidson EL, Ollerton RL. Partner behaviours improving breastfeeding outcomes: An integrative review. Women Birth. (2020) 33(1):e15-e23. doi: 10.1016/j.wombi.2019.05.010
52. Morris C, Schofield P, Hirst C. Exploration of the factors influencing attitudes to reastfeeding in public. J Human Lact. (2020) 36(4):776–88. doi: 10.1177/0890334419878119
53. Hamze L, Carrick-Sen D, Zhang Z, Liu Y, Mao J. Maternal attitude towards breastfeeding: a concept analysis. Br J Midwifery. (2018) 26(7):462–9. doi: 10.12968/bjom.2018.26.7.462
54. Donnan PT, Dalzell J, Symon A, Rauchhaus P, Monteith-Hodge E, Kellett G, et al. Prediction of initiation and cessation of breastfeeding from late pregnancy to 16 weeks: the Feeding Your Baby (FYB) cohort study. BMJ Open. (2013) 3(8):e003274. doi: 10.1136/bmjopen-2013-003274
55. Radzyminski S, Callister LC. Mother's beliefs, attitudes, and decision making related to infant feeding choices. J Perinat Educ. (2016) 25(1):18–28. doi: 10.1891/1058-1243.25.1.18
56. Shaker I, Scott JA, Reid M. Infant feeding attitudes of expectant parents: breastfeeding and formula feeding. J Adv Nurs. (2004) 45(3):260–8. doi: 10.1046/j.1365-2648.2003.02887.xv
57. Huang Y, Ouyang YQ, Redding SR. Previous breastfeeding experience and its influence on breastfeeding outcomes in subsequent births: a systematic review. Women Birth. (2019) 32(4):303–9. doi: 10.1016/j.wombi.2018.09.003
58. Tseng JF, Chen SR, Au HK, Chipojola R, Lee GT, Lee PH, et al. Effectiveness of an integrated breastfeeding education program to improve self-efficacy and exclusive breastfeeding rate: a single-blind, randomised controlled study. Int J Nurs Stud. (2020) 111:1–10. doi: 10.1016/j.ijnurstu.2020.103770
59. Jackson L, De Pascalis L, Harrold J, Fallon V. Guilt, shame, and postpartum infant feeding outcomes: a systematic review. Matern Child Nutr. (2021a) 17(3):1–29. doi: 10.1111/mcn.13141
60. Jackson L, De Pascalis L, Harrold J, Fallon V. Maternal guilt and shame in the context of infant feeding: a concept analysis. Midwifery. (2021b) 105:1–11. doi: 10.1016/j.midw.2021.103205
61. Tedder J. The roadmap to breastfeeding success: teaching child evelopment to extend breastfeeding duration. J Perinat Educ. (2015) 24(4):239–48. doi: 10.1891/1058-1243.24.4.239
62. Richetin J, Conner M, Perugini M. Not doing is not the opposite of doing: implications for attitudinal models of behavioural prediction. Pers Soc Psychol Bull. (2011) 37(1):40–54. doi: 10.1177/0146167210390522
63. Ertem IO, Votto N, Leventhal JM. The timing and predictors of the early termination of breastfeeding. Pediatrics. (2001) 107(3):543–8. doi: 10.1542/peds.107.3.543
64. Brown A, Raynor P, Lee M. Healthcare professionals’ and mothers’ perceptions of factors that influence decisions to breastfeed or formula feed infants: a comparative study. J Adv Nurs. (2011) 67(9):1993–2002. doi: 10.1111/j.1365-2648.2011.05647.x
65. Ahmad RS, Sulaiman Z, Nik Hussain NH, Mohd Noor N. Working mothers’ breastfeeding experience: a phenomenology qualitative approach. BMC Pregnancy Childbirth. (2022) 22(85):1–8. doi: 10.1186/s12884-021-04304-4
66. Negin J, Coffman J, Vizintin P, Raynes-Greenow C. The influence of grandmothers on breastfeeding rates: a systematic review. BMC Pregnancy Childbirth. (2016) 16:1–10. doi: 10.1186/s12884-016-0880-5
67. Wolfberg AJ, Michels KB, Shields W, O'Campo P, Bronner Y, Bienstock J. Dads as breastfeeding advocates: results from a randomized controlled trial of an educational intervention. Am J Obstet Gynecol. (2004) 191(3):708-12. doi: 10.1016/j.ajog.2004.05.019
68. Stewart-Glenn J. Knowledge, perceptions, and attitudes of managers, coworkers, and employed breastfeeding mothers. AAOHN J. (2008) 56(10):423–31. doi: 10.3928/08910162-20081001-02
69. Tsai SY. Employee perception of breastfeeding-friendly support and benefits of breastfeeding as a predictor of intention to use breast-pumping breaks after returning to work among employed mothers. Breastfeed Med. (2014) 9(1):16–23. doi: 10.1089/bfm.2013.0082
70. Kinshella MW, Prasad S, Hiwa T, Vidler M, Nyondo-Mipando AL, Dube Q, et al. Barriers and facilitators for early and exclusive breastfeeding in health facilities in Sub-Saharan Africa: a systematic review. Global Health Res Policy. (2021) 6(1):21. doi: 10.1186/s41256-021-00206-2
71. Advisory, Conciliation and Arbitration Service (ACAS). Accommodating breastfeeding employees in the workplace. Accessed on 02 August 2021: https://www.acas.org.uk/sites/default/files/2021-03/acas-guide-on-accommodatingbreastfeeding-in-the-workplace.pdf (2014).
72. Scott VC, Taylor YJ, Basquin C, Venkitsubramanian K. Impact of key workplace breastfeeding support characteristics on job satisfaction, breastfeeding 72 duration, and exclusive breastfeeding among health care employees. Breastfeed Med. (2019) 14(6):416–23. doi: 10.1089/bfm.2018.0202
73. Snyder K, Hansen K, Brown S, Portratz A, White K, Dinkel D. Workplace breastfeeding support varies by employment type: the service workplace disadvantage. Breastfeed Med. (2018) 13(1):23–8. doi: 10.1089/bfm.2017.0074
74. Tosun LP, Öztürk A, Özdemir G. Mother to mother: mothers’ social comparison-based emotions on social networking sites. Eur J Psychol. (2020) 16(4):602–18. doi: 10.5964/ejop.v16i4.2159
75. Komninou S, Fallon V, Halford JCG, Harrold JA. Differences in the emotional and practical experiences of exclusively breastfeeding and combination feeding mothers. Matern Child Nutr. (2016) 13:1–11. doi: 10.1111/mcn.12364
Keywords: postpartum, breastfeeding, formula feeding, bottle feeding, combination feeding, social support
Citation: Roberts D, Jackson L, Davie P, Zhao C, Harrold JA, Fallon V and Silverio SA (2023) Exploring the reasons why mothers do not breastfeed, to inform and enable better support. Front. Glob. Womens Health 4:1148719. doi: 10.3389/fgwh.2023.1148719
Received: 24 January 2023; Accepted: 20 March 2023;
Published: 12 April 2023.
Edited by:
Sarah Earle, The Open University, United KingdomReviewed by:
Kadidiatou Kadio, Institut de Recherche en Sciences de la Santé (IRSS), Burkina FasoYolanda Contreras-García, University of Concepcion, Chile
© 2023 Roberts, Jackson, Davie, Zhao, Harrold, Fallon and Silverio. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Leanne Jackson TGVhbm5lLkphY2tzb25AbGl2ZXJwb29sLmFjLnVr
†These authors share first authorship
‡These authors share senior authorship
Specialty Section: This article was submitted to Women's Mental Health, a section of the journal Frontiers in Global Women's Health
 Dean Roberts
Dean Roberts Leanne Jackson
Leanne Jackson Philippa Davie
Philippa Davie Catherine Zhao
Catherine Zhao Joanne A. Harrold
Joanne A. Harrold Victoria Fallon
Victoria Fallon Sergio A. Silverio
Sergio A. Silverio