- Department of Midwifery, Asrat Woldeyes Health Science Campus, Debre Berhan University, Debre Berhan, Ethiopia
Background: Family planning integration in areas where women contact the healthcare system routinely is essential for addressing the high unmet need for family planning among postpartum women and reducing the risk of short interpregnancies. Immediate postpartum family planning (IPPFP) is an integrated service, and opportunities exist for women by providing family planning (FP) counseling and contraceptives as part of care following childbirth within 48 h. Therefore, this review aimed to assess the pooled estimate of immediate postpartum family planning utilization and its associated factors in Ethiopia.
Method: Electronic databases were used to conduct an extensive search of all published studies, and the digital library was used to identify any unpublished studies. An observational study that reports the prevalence/magnitude and/or associated factors/predictors/determinants of IPPFP utilization in Ethiopia was included. Data were extracted on the Microsoft Excel spreadsheet and analyzed using STATA Version 11. A random-effects model was applied to determine the pooled prevalence of immediate postpartum family planning utilization with a 95% confidence interval (CI). Inverse variance (I2) was used to identify the presence of heterogeneity, and a funnel plot and Egger's test were used to check the presence of publication bias. Subgroup analysis was conducted based on the sample size, region, and year of study to identify the source of heterogeneity.
Result: Of 15 primary studies, the overall pooled prevalence of immediate postpartum family planning utilization among postpartum women in Ethiopia was 21.04% (95% CI: 13.08, 29.00). Received counseling on FP [OR: 3.59; 95% CI (1.84, 7.01; P < 0.001), having a positive attitude toward FP [OR: 3.2; 95% CI (1.23, 8.35); P = 0.017], and partner support to use FP [OR: 5.85; 95% CI (1.12, 30.54; P = 0.036) were significant predictors of immediate postpartum family planning utilization.
Conclusion: Generally, IPPFP utilization in Ethiopia was insufficient. Therefore, to enhance the utilization, integrating FP counseling at all maternal service care points, strengthening community awareness to develop a favorable attitude toward family planning, and promoting partner involvement in family planning counseling are essential.
Systematic Review Registration: https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=239053, identifier: CRD42021239053.
Introduction
Improving the availability of contraceptives is essential to achieving the 2030's Sustainable Development Goals (SDGs) (1) and universal access to reproductive health services during pregnancy, childbirth, and the first year after delivery (2), which helps in decreasing the risk of premature birth, low birth weight, fetal and neonatal death, and adverse maternal health outcomes (3).
Postpartum family planning (PPFP) integration in areas where women contact the healthcare system routinely, such as during antenatal care, labor and delivery, postnatal care, immunization, and child healthcare, is essential for addressing the high unmet need for family planning (FP) among postpartum women and reducing the risk of short interpregnancies (4). Immediate postpartum family planning (IPPFP) is an integrated service, and opportunities exist for women by providing FP counseling and contraceptive as part of care following childbirth within 48 h (5, 6).
According to the World Health Organization (WHO) technical consultation committee for better maternal and child health outcomes, an interval of at least 2 years following a live birth is recommended before attempting another pregnancy (7). Infant and under-five child mortality would decrease by 10% and 21%, respectively, in those women who waited 2 years between giving birth and getting pregnant again (8).
Postpartum women have a greater unmet need for contraceptives than nonpostpartum women (6). Globally, 225 million women desire modern contraception to delay or prevent future pregnancy, but they do not have access (9). The demographic health survey data from 57 countries indicated that 62% of women in the first year after birth have an unmet need for FP (10). A study conducted in low- and middle-income countries showed that the unmet need for FP among postpartum women ranged from 25% to 96% (11). Pregnancies that happened within the first year of the delivery were mostly unplanned (12) and associated with increased risk of adverse maternal, perinatal, infant, and child health outcomes, ranging from stillbirth, small-for-gestational-age, low birthweight to neonatal and maternal morbidity and mortality (13, 14).
Maternal health problems related to pregnancy and childbirth remain a major global concern and leading causes of morbidity and mortality among reproductive-age women (9). As WHO's 2019 report, 810 women die every day from preventable causes related to pregnancy and childbirth, of which 94% of all maternal mortality occurs in low- and lower-middle-income countries (15). The prevalence of unintended pregnancy is still high and the most challenging issue within the domain of maternal and child health and women's reproductive health globally (16, 17). According to the WHO report from the estimated 210 million pregnancies worldwide, 44% of pregnancies were unintended and around 59% of pregnancies ended by abortion (18).
Although there are some fragmented primary studies on family planning utilization during the immediate postpartum period, most of them focused only on the postpartum intrauterine contraceptive device utilization in Ethiopia. Also, the determinants were variable among these studies. However, the pooled national level by addressing all options of IPPFP utilization was unknown. Therefore, this meta-analysis aimed to estimate the pooled prevalence of immediate postpartum family planning utilization and its associated factors in Ethiopia by considering the WHO Medical eligibility criteria for contraceptives-2015 for postpartum during the immediate postpartum period. The result of this study will provide important input for policymakers and healthcare providers about IPPFP utilization and will enforce them to design evidence-based strategies for improving IPPFP utilization in Ethiopia.
Objectives of the review
• To determine the pooled prevalence of immediate postpartum family planning uptake in Ethiopia
• To identify the predictors of immediate postpartum family planning uptake in Ethiopia
Methods
Study design, data source, and search strategy
This systematic review and meta-analysis was conducted to estimate the pooled prevalence of IPPFP utilization and its associated factors in Ethiopia under the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement (19, 20). We checked to see whether there were any similar ongoing systematic reviews and meta-analyses in the PROSPERO database, but no such studies had been conducted before. Then, the review protocol was registered on the PROSPERO database with registration number CRD42021239053. Finally, a standard systematic review and meta-analysis reporting PRISMA checklist was used to present the findings.
Furthermore, four authors (MS, TD, GW, and TM) explored all relevant studies were searched in the following databases; PubMed, Google Scholar, African Journal of Online (AJOL), HINARI, Scopus, Science Direct, Excerpta Medica database (EMBASE), DOAJ, and Web of Science. Google and the organization's website were used to search the gray literature and unpublished research studies. Studies were searched by using the full title (immediate postpartum family planning utilization and associated factors in Ethiopia) and the following searching keywords or terms; “Immediate postpartum Family planning,” “Postpartum family planning,” “Postpartum Intrauterine Contraceptive Device,” “Postpartum Intrauterine Device,” “PPIUCD,” “PPIUD,” “Uptake,” “Utilization,” “Use,” “Determinants,” “Predictors,” “associated factors,” “immediate postpartum period,” and “Ethiopia.” To find any further missed studies, the reference lists of all included published and unpublished studies were reviewed. All fields and MeSH (Medical Subject Headings) terms with Boolean operators (“OR” and/or “AND”) were used to search studies in the advanced PubMed search engine (Additional File S1).
Eligibility criteria
Both published and unpublished observational studies (cross-sectional and case–control), which report the prevalence/magnitude and/or associated factors/predictors/determinants of IPPFP utilization in Ethiopia, were included. Also, this review included studies done until July 30,2022. Studies with a different outcome of interest/operational definitions and inaccessibility of full text were excluded.
Outcome measurement, study selection, and quality assessment
IPPFP utilization was considered when a postpartum woman was using any of the postpartum contraceptive options (progesterone-only pills, implant, intrauterine devices, and permanent FP method) within 48 h of delivery. After studies were searched from different international databases and organization's websites, studies were screened by using the following criteria (duplication, relevancy, accessibility of full text, and outcomes of interest). Finally, the quality of each study was assessed using the standard quality assessment tool [Newcastle–Ottawa scale (NOS)] (21) and by four authors (MS, SA, BTT, and MSC) independently using the following components: selection, comparability, and outcome, which were graded by five, two, and three, respectively. Any disagreements between the four authors during quality appraisal were resolved by the other two authors (FK and TLD) through discussion and re-evaluation of selected studies. For analysis, only the primary studies with a medium score (fulfilling 50% of the quality evaluation criteria) and above were included (22) (Additional File S2).
Data extraction process
Data were extracted using a data extraction format prepared in a Microsoft Excel 2010 spreadsheet by three authors (MS, BTT, and MSC). This form includes the first author's name, study year, study area, region, study design, sample size, prevalence of IPPFP utilization, and AOR with a 95% CI for factors associated with the utilization of IPPFP. By involving a fourth author (TLD), differences at the time of data extraction were solved through discussion and consensus.
Data synthesis and statistical analysis
Data were extracted using Microsoft Excel 2010 spreadsheet and analyzed using STATA Version 11 software. Because high heterogeneity across studies was identified using inverse variance (I2) statistics with its corresponding P-value (I2 = 98.6%, P < 0.001) (23–25), a random-effects model was applied to determine the pooled prevalence of IPPFP utilization. Also, subgroup analysis was performed based on the sample size, year of study, and region to identify the source of heterogeneity across studies. A funnel plot and Egger's test were used to check publication bias (26). A P-value of less than 0.05 was used to declare the statistical significance of publication bias (27). Due to this, the publication bias for meta-analysis results was addressed using the Duval and Tweedie nonparametric trim and fill analysis by random-effects analysis (28, 29). A factor associated with IPPFP uptake in at least two primary studies was included in the meta-analysis. The results were presented using texts, tables, and forest plots with effect and 95% CI measures.
Results
Study selection
A total of 1,198 studies were searched from different international databases and Ethiopian universities' institutional repositories using different searching strategies. The EndNote 7 reference manager was used to screen all retrieved studies. As a result, 412 studies were removed due to duplication. Then, 771 studies were excluded due to unrelated titles, abstract inaccessibility of full text, and different outcomes of interest. Finally, 15 studies that met the inclusion criteria were considered for the meta-analysis (Figure 1).
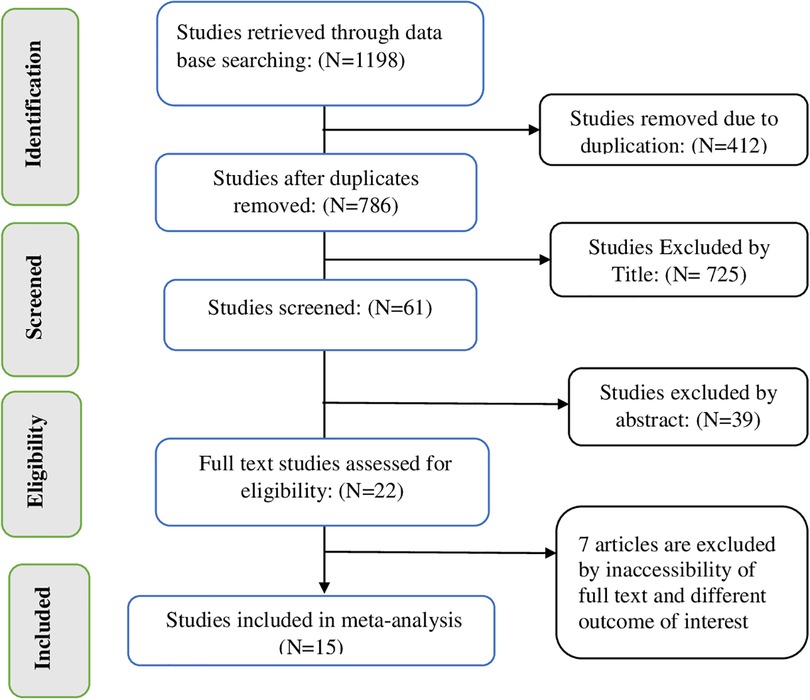
Figure 1. PRISMA flow diagram of included studies to estimate the pooled prevalence of immediate postpartum family planning utilization and its associated factors among women in Ethiopia, 2022.
Characteristics of included studies
Fifteen primary studies were included in this systematic review and meta-analysis, of which 13 were cross-sectional studies, while two were case–control studies with a sample size ranging from 182 to 884 (30, 31). Regarding the region in which the study was conducted, four articles were from Amhara (31–34), five from SNNP (35–39), four from Addis Ababa (31, 40–42), and two from the Oromia (43, 44) region with the year of study ranging from 2016 to 2020. The highest prevalence of IPPFP utilization was reported by Arero et al. (53.2%) (44), which was done in the Oromia region, while the lowest IPPFP utilization was reported in the Amhara region by Hagos et al. (3.3%) (30) (Table 1).
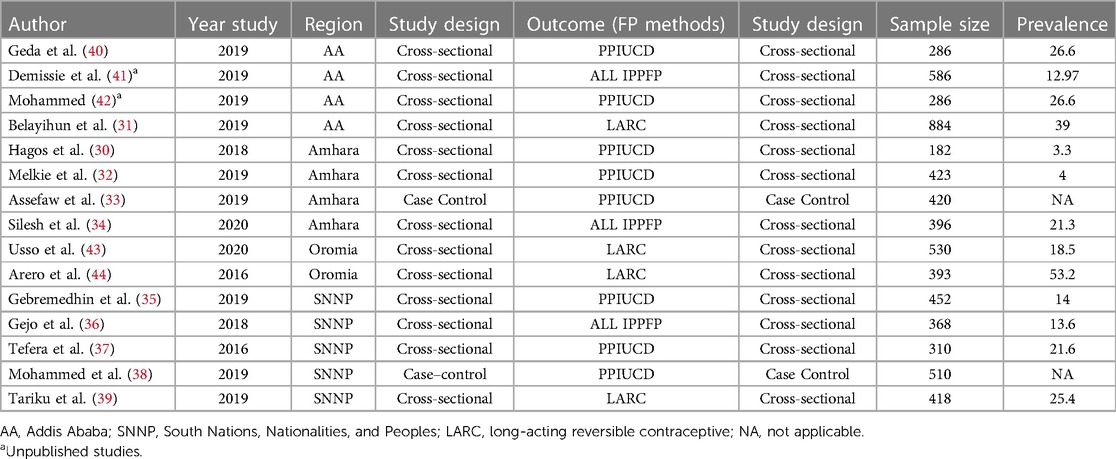
Table 1. Descriptive summary of 15 studies included to estimate the pooled prevalence of immediate postpartum family planning utilization in Ethiopia.
Prevalence of immediate postpartum family planning uptake
A total of 13 (11 published and two unpublished) studies with 5,514 postpartum women were included in this review to estimate the pooled prevalence of IPPFP uptake. Accordingly, this study revealed high heterogeneity across the studies, as evidenced by I2 statistics (I2 = 98.43%, P < 0.001); the random-effects model was applied to estimate the pooled prevalence of IPPFP utilization. Therefore, the pooled prevalence of IPPFP utilization among postpartum women in Ethiopia was 21.45% (95% CI: 14.07, 28.83) (Figure 2).
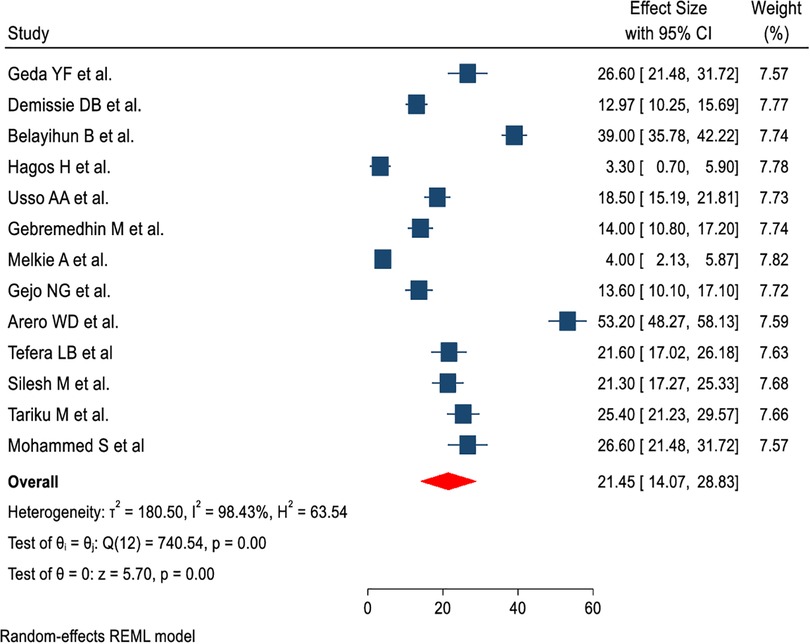
Figure 2. Forest plot of pooled prevalence of immediate postpartum family planning utilization among postpartum women in Ethiopia.
Publication bias and heterogeneity
A funnel plot and Egger's test (26) were used to check publication bias. A P-value of less than 0.05 was used to declare the statistical significance of publication bias (27). Accordingly, the funnel plots' results revealed an asymmetrical pattern, which suggests that the included studies have a publishing bias (Figure 3A). In addition, Egger's regression test revealed that studies had publication bias (P-value = 0.001 (Figure 3B). Therefore, the Duval and Tweedie nonparametric trim and fill analysis using the random-effects method was conducted to deal with the publication bias for meta-analysis results (28, 29). As a result, after 6 studies were filled, 19 studies were included to resolve the publication bias across studies by trim and fill analysis to produce the pooled estimate of IPPFP utilization of 2.05 (1.24, 2.85) (Figure 3C).
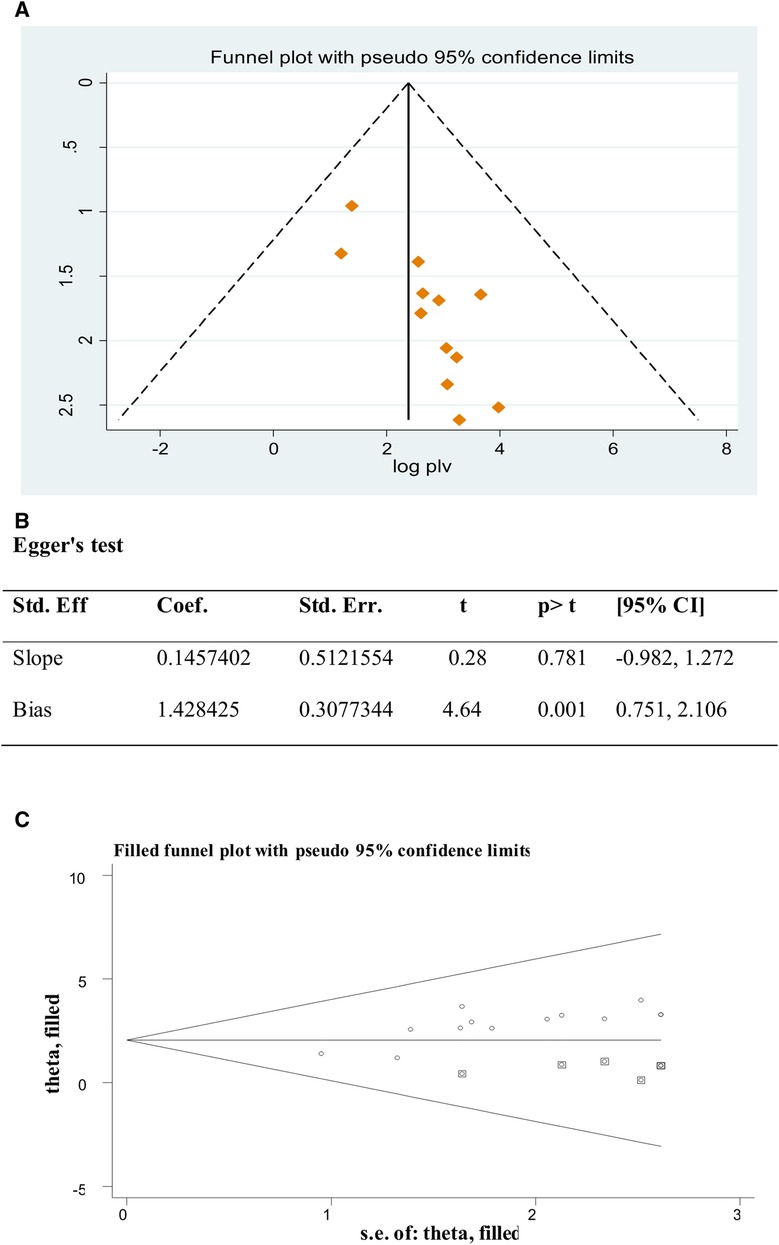
Figure 3. (A) Funnel plot to test publication bias of 13 studies. (B) Egger’s test, (C) result of the trim and fill analysis.
Subgroup analysis and sensitivity analysis
Significant heterogeneity was observed among included primary studies. Therefore, subgroup analysis was conducted based on the sample size, region, and year of study to identify the source of heterogeneity. Accordingly, the overall prevalence of IPPFP uptake was found to be high among studies conducted with <400 sample size [23.52 (11.84, 35.20)], in the Oromia region [35.75 (1.74, 69.75)], and in the year 2016 [37.3 (6.33, 68.27)] (Table 2).
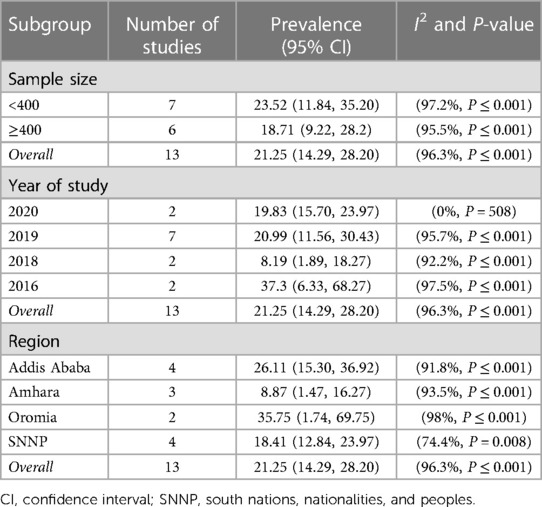
Table 2. Subgroup analysis of immediate postpartum family planning utilization in Ethiopia (n = 13).
A leave-one-out sensitivity analysis was performed to check the effect of individual studies on the pooled estimate of IPPFP utilization. In the sensitivity analysis, the pooled prevalence of IPPFP utilization was observed to be low at 10.02% (3.90%, 25.72%) and high at 15.28% (5.43%, 42.98%) when the studies of Belayihun et al. and Melkie et al. were omitted, respectively (Table 3).
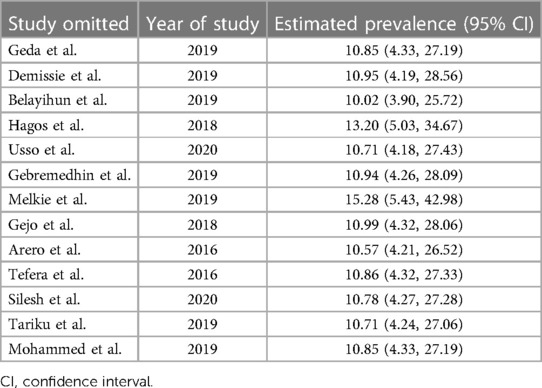
Table 3. Sensitivity analysis of immediate postpartum family planning utilization in Ethiopia (n = 13).
Determinants of immediate postpartum family planning uptake
From the nine identified factors from primary studies, counseling on FP, attitude toward FP, and having partner support to use FP showed statistically significant associations with IPPFP utilization in this meta-analysis. However, the age of women, ever heard about FP, knowledge of FP, discussion with the partner, planned status of the pregnancy, and plan to have another child showed no statistically significant association with IPPFP utilization (Additional File S3).
The pooled effect of attitude toward FP on IPPFP utilization among women during the immediate postpartum period was evaluated using two primary studies (34, 41). The result of this study revealed that women's attitude toward FP was significantly associated with IPPFP utilization, and the likelihood of utilizing IPPFP was 3.2 times higher among those women who had a positive attitude toward FP than their counterparts [OR: 3.2; 95% CI (1.23, 8.35); P = 0.017], with heterogeneity (I2 = 85.5%, P-value = 0.009) (Figure 4).
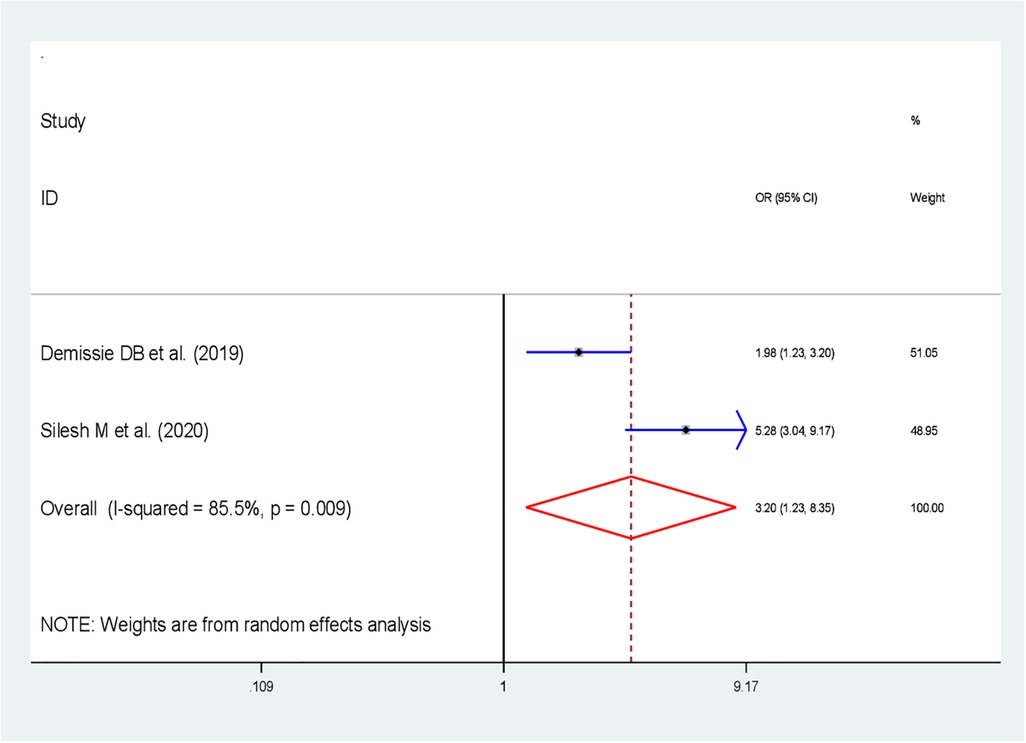
Figure 4. Forest plot showing the association between attitudes toward FP employed status and immediate postpartum family planning utilization in Ethiopia.
Eleven studies were included in determining the pooled effects of FP counseling status on IPPFP utilization (31, 32, 44, 33, 35, 37, 39–43). The findings revealed that FP counseling status was significantly associated with the utilization of IPPFP; those women who received FP counseling were 3.6 times more likely to utilize IPPFP than women who were not counseled on FP [OR: 3.59; 95% CI (1.84, 7.01; P < 0.001)] with heterogeneity (I2 = 91.9%, P-value <0.001) (Figure 5).
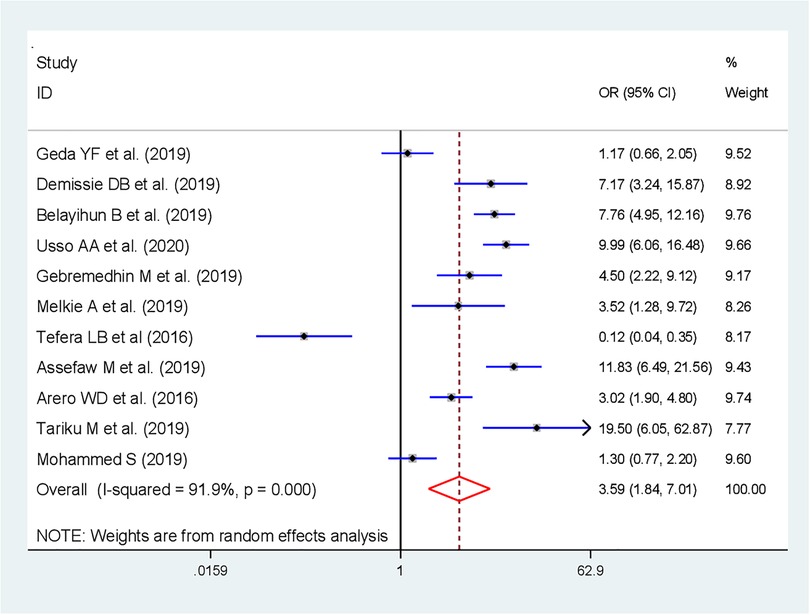
Figure 5. Forest plot showing the association between counseling on FP and immediate postpartum family planning utilization in Ethiopia.
Furthermore, the effect of partner support to use FP on IPPFP utilization was assessed by using three studies (34, 38, 40). The finding of this study revealed that the pooled effect of having partner support to use FP was significantly associated with the utilization of IPPFP; postpartum women who had partner support to use FP were almost six times more likely to use IPPFP than their counterparts [OR: 5.85; 95% CI (1.12, 30.54; P = 0.036)], with heterogeneity (I2 = 96.1%, P-value <0.001) (Figure 6).
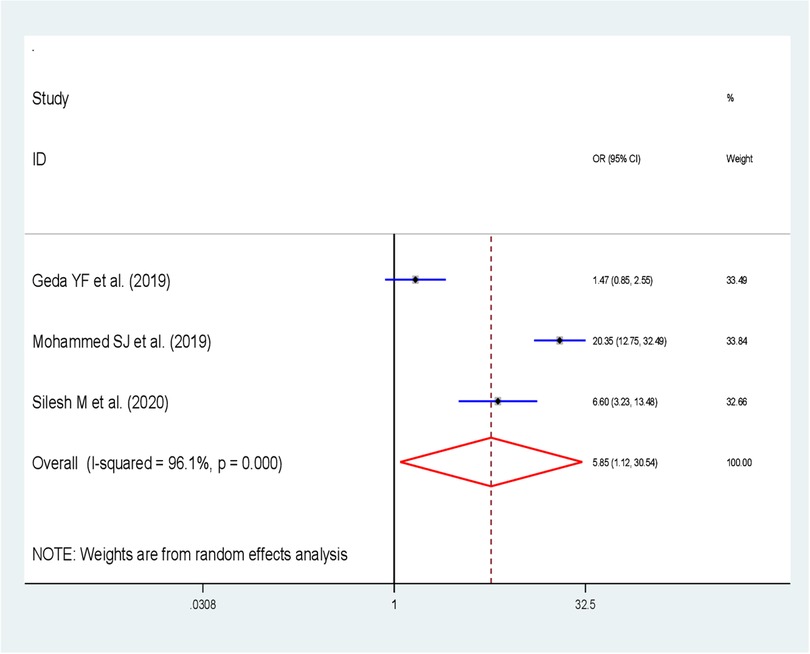
Figure 6. Forest plot showing the association between partner support and immediate postpartum family planning utilization in Ethiopia.
Discussion
This systematic review and meta-analysis aimed to assess the pooled prevalence and associated factors of IPPFP utilization in Ethiopia. To the best of our knowledge, this meta-analysis is a first of its kind in determining the national prevalence and significant factors of IPPFP utilization in Ethiopia, which is used as input for policymakers, healthcare providers, and other stakeholders to design evidence-based strategies to strengthen IPPFP utilization.
The overall pooled prevalence of IPPFP uptake among postpartum women in Ethiopia was 21.04% (95% CI: 13.08, 29.00). This finding is comparable with a study done in Ethiopia on PPIUCD (21.63%) (22) but lower than a systematic review and meta-analysis conducted in low- and middle-income countries (41.2%) (45) and Ethiopia (45.44%–45.79%) (46, 47). The possible reason for this variation could be attributed to variations in the study setting, study period, and accessibility of health facilities. In addition to this, variation in sociocultural and women's health-seeking behavior between the studies settings might contribute to this difference.
In the present review and meta-analysis, subgroup analysis was done based on the region and year of study, indicating no variations in the uptake of IPPFP among the region and year of study in Ethiopia. Accordingly, the highest utilization of PPIUCD was observed in Oromia at 35.75% (1.74, 69.75) (43, 44) and the studies conducted in 2016 at 37.29% (6.33, 68.27) based on the region, study population, and year of study, respectively. The observed variation could be due to regional religious and cultural differences. In addition, IPPFP uptake improved from time to time; the difference in residence and inclusion criteria of primary studies on information exposure could be the possible reason for the discrepancies in the uptake of IPPFP by year of study.
In this meta-analysis, counseling status was positively associated with IPPFP utilization. Women who received counseling on FP were four times more likely to utilize IPPFP compared to their counterparts. This is consistent with studies conducted in four countries (India, Nepal, Sri Lanka, and Tanzania) (48) and Ethiopia (47). Also, a study done in Ethiopia revealed that women who had been counseled were 3.05 times more likely to utilize PPIUCD than those who had not been counseled about PPIUCD (22). This might be because counseling could significantly help women to have accurate information about family planning, which further changes the negative attitudes of women toward family planning and minimize myths and misconceptions related to family planning.
The odds of uptake of IPPFP were three times higher among women who have a positive attitude toward FP than women who have a negative attitude toward FP. This might be because one's attitude toward a particular activity is crucial to how something will be carried out in practical situations.
Moreover, the finding of this study revealed that women who had partner support to use FP were six times more likely to utilize IPPFP than women who have not had partner support. A similar finding was also reported by the study conducted in Ethiopia; PPIUD uptake was 11.48 times higher in those women who had husband/partner support than those who had no support (22).
This study has some limitations. The lack of studies from most regions may affect the generalizability of this study. Furthermore, significant heterogeneity was detected across studies, which undermines the pooled estimate of IPPFP utilization. Subgroup analysis was done based on the sample size, region, and year of study. However, the possible source of heterogeneity was not identified.
Conclusion
The overall prevalence of IPPFP utilization was low in Ethiopia. Being counseled on FP, having a positive attitude toward FP, and having partner support to use FP were significantly associated with IPPFP utilization. Therefore, to enhance immediate postpartum family planning utilization, integrating FP counseling at all maternal service care points, strengthening community awareness to develop a favorable attitude toward family planning, and promoting partner involvement in family planning counseling are essential. Furthermore, for the researchers, it is better to assess the factors related to health facilities and healthcare providers on IPPFP utilization.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary Material.
Author contributions
MS conceived and designed the review and was the guarantor of the review. MS, GW, BTT, SA, TM, and MSC developed the search strings and screened, selected, and evaluated the quality of the studies. MS, BTT, MSC, and TLD extracted the data from selected studies, carried out analysis and interpretation, and rigorously reviewed the manuscript. MS carried out the draft of the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgwh.2023.1095804/full#supplementary-material
References
1. Starbird E, Norton M, Marcus R. Investing in family planning: key to achieving the sustainable development goals. Glob Health Sci Pract. (2016) 4:191–210. doi: 10.9745/GHSP-D-15-00374
2. United Nations Department of Economic and Social Affairs, Division SAP. Family Planning and the 2030 Agenda for Sustainable Development (2019). Available at: https://www.un.org/en/development/desa/population/publications/pdf/family/familyPlanning_DataBooklet_2019.pdf.
3. WHO. WHO Programming Strategies for Postpartum Family Planning (2013). Geneva. Available at: http://www.who.int/reproduc¬tivehealth/publications/family_planning/ppfp_strategies/en/.
4. Gaffield ME, Egan S, Temmerman M. It’s about time: WHO and partners release programming strategies for postpartum family planning. Glob Health Sci Pract. (2014) 2:4–9. doi: 10.9745/GHSP-D-13-00156
5. High Impact Practices in Family Planning (HIPs). Family planning high impact practices list. Washington, DC: The High Impact Practices Partnership (2022). Available at: https://www.fphighimpactpractices.org/briefs/family-planning-high-impact-practices-list/
6. Glasier A, Baird D, Blumenthal P, Cameron S, Alison Fiander AG. Best practice paper in postpartum family planning. R Coll Obstet Gynaecol. (2015) 1(1):1–13. Available at: https://www.glowm.com/pdf/best-practice-paper-1---postpartum-family-planning.pdf
7. Tran NT, Gaffield ME, Seuc A, Landoulsi S, Yamaego WME, Cuzin-Kihl A, et al. Effectiveness of a package of postpartum family planning interventions on the uptake of contraceptive methods until twelve months postpartum in Burkina Faso and the Democratic Republic of Congo: the YAM DAABO study protocol. BMC Health Serv Res. (2018) 18:439. doi: 10.1186/s12913-018-3199-2
8. Cleland J, Conde-Agudelo A, Peterson H, Ross J, Tsui A. Contraception and health. Lancet. (2012) 380(9837):149–56. doi: 10.1016/S0140-6736(12)60609-6
9. WHO. WHO updates fact sheet on Family Planning_ Contraception (14 December 2016) _ communitymedicine4asses. Community Medicine for All Seeking Simple Explanations (2016). Available at: https://communitymedicine4asses.wordpress.com/2016/12/16/who-updates-fact-sheet-on-family-planning-contraception-14-december-2016/.
10. Rossier C, Bradley SEK, Ross J, Winfrey W. Reassessing unmet need for family planning in the postpartum period. Stud Fam Plann. (2015) 46(4):355–67. doi: 10.1111/j.1728-4465.2015.00037.x
11. Pasha O, Goudar SS, Patel A, Garces A, Esamai F, Chomba E, et al. Postpartum contraceptive use and unmet need for family planning in five low-income countries. Reprod Health. (2015) 12(Supplement.2):1–7. Available at: http://ecommons.aku.edu/pakistan_fhs_mc_chs_chs/25425561377
12. Ahmed S, Norton M, Williams E, Ahmed S, Shah R, Begum N, et al. Operations research to add postpartum family planning to maternal and neonatal health to improve birth spacing in Sylhet district, Bangladesh. Glob Heal Sci Pract. (2013) 1(2):262–76. doi: 10.9745/GHSP-D-13-00002
13. Lyell DJ. Official reprint from UpToDate. Interpregnancy interval and obstetrical complications. www.uptodate.com. (2017). Available at: https://enjoypregnancyclub.com/wp-content/uploads/2017/06/Interpregnancy%20interval%20and%20obstetrical%20complications.pdf
14. Ekin A, Gezer C, Taner CE, Ozeren M, Mat E, Solmaz U. Impact of interpregnancy interval on the subsequent risk of adverse perinatal outcomes. J Obstet Gynaecol Res. (2015) 41(11):1744–51. doi: 10.1111/jog.12783
15. Trends in maternal mortality 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Geneva: World Health Organization (2019). Available at: https://www.who.int/publications/i/item/9789241516488
16. Bishwajit G, Tang S, Yaya S, Feng Z. Unmet need for contraception and its association with unintended pregnancy in Bangladesh. BMC Pregnancy Childbirth. (2017) 17(1):1–9. doi: 10.1186/s12884-017-1379-4
17. Horvath S, Schreiber CA. Unintended pregnancy, induced abortion, and mental health. Curr Psychiatry Rep. (2017) 19(11):77. doi: 10.1007/s11920-017-0832-4
18. Bearak J, Popinchalk A, Alkema L, Sedgh G. Global, regional, and subregional trends in unintended pregnancy and its outcomes from 1990 to 2014: estimates from a Bayesian hierarchical model. Lancet Glob Heal. (2018) 6(4):e380–9. doi: 10.1016/S2214-109X(18)30029-9
19. Moher D, Liberati A, Tetzlaff J, Altman DG. The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6(7):e1000097. doi: 10.1371/journal.pmed.1000097
20. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. (2009) 62:1–34. doi: 10.1016/j.jclinepi.2009.06.006
21. Modesti PA, Reboldi G, Cappuccio FP, Agyemang C, Remuzzi G, Rapi S, et al. Cross sectional study Newcastle–Ottawa quality assessment scale. PLoS One. (2016) 11(1):1–2. doi: 10.1371/journal.pone.0147601
22. Kassa BG, Ayele AD, Belay HG, Tefera AG, Tiruneh GA, Ayenew NT, et al. Postpartum intrauterine contraceptive device use and its associated factors in Ethiopia: systematic review and meta-analysis. Reprod Health. (2021) 18(1):1–12. doi: 10.1186/s12978-021-01273-x
23. Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327(7414):557–60. doi: 10.1136/bmj.327.7414.557
24. Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. (2010) 1(2):97–111. doi: 10.1002/jrsm.12
25. DerSimonian R, Kacker R. Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials. (2007) 28(2):105–14. doi: 10.1016/j.cct.2006.04.004
26. Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. Comparison of two methods to detect publication bias in meta-analysis. JAMA. (2006) 295(6):676–80. doi: 10.1001/jama.295.6.676
27. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. (1994) 50(4):1088. doi: 10.2307/2533446
28. Pal BK, Rahman MS. Sensitive spectrofluorimetric determination of ruthenium at nanotrace levels using 2-(α-pyridyl) thioquinaldinamide [PTQA]. Talanta. (1999) 48(5):1075–84. doi: 10.1016/S0039-9140(98)00318-X
29. Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315(7109):629–34. doi: 10.1136/bmj.315.7109.629
30. Hagos H, Tiruneh D, Necho W, Biru S. Postpartum intra-uterine contraceptive device utilization among mothers who delivered at Debre Tabor general hospital: cross sectional study design. Int J Fam Community Med. (2020) 4(5):139–44. doi: 10.15406/ijfcm.2020.04.00203
31. Belayihun B, Asnake M, Tilahun Y, Molla Y. Factors associated with long-acting reversible contraceptive use in the immediate postpartum period in Ethiopia. Ethiop J Heal Dev. (2021) 35(5):11–9. Available at: https://www.ajol.info/index.php/ejhd/article/view/219866
32. Melkie A, Addisu D, Mekie M, Dagnew E. Utilization of immediate postpartum intrauterine contraceptive device and associated factors among mothers who gave birth at selected hospitals in west Gojjam zone, Ethiopia, multi-level facility-based study, 2019. Heliyon. (2021) 7(1):e06034. doi: 10.1016/j.heliyon.2021.e06034
33. Assefaw M, Azanew G, Engida A, Tefera Z, Gashaw W. Determinants of postpartum intrauterine contraceptive device uptake among women delivering in public hospitals of south Gondar zone, northwest Ethiopia, 2019: an unmatched case-control study. Obstet Gynecol Int. (2021) 2021:1757401. doi: 10.1155/2021/1757401. PMID: 33688350; PMCID: 7920734
34. Silesh M, Lemma T, Abdu S, Fenta B, Tadese M, Taye BT. Utilisation of immediate postpartum family planning among postpartum women at public hospitals of North Shoa zone, Ethiopia: a cross-sectional study. BMJ Open. (2022) 12(2):1–10. doi: 10.1136/bmjopen-2021-051152
35. Gebremedhin M, Alemayehu A, Yihune M, Dessu S, Melis T, Nurahmed N. Acceptability and factors associated with immediate postpartum intrauterine contraceptive device use among women who gave birth at government hospitals of Gamo zone, Southern Ethiopia, 2019. Open Access J Contracept. (2021) 12:93-101. doi: 10.2147/OAJC.S291749
36. Gejo NG, Anshebo AA, Dinsa LH. Postpartum modern contraceptive use and associated factors in Hossana town. PLoS One. (2019) 14(5):1–10. doi: 10.1371/journal.pone.0217167
37. Tefera LB, Abera M, Fikru C, Tesfaye DJ. Utilization of immediate post-partum intra uterine contraceptive device and associated factors: a facility based cross sectional study among mothers delivered at public health facilities of Sidama zone, South Ethiopia. J Preg Child Heal. (2017) 4:326. doi: 10.4172/2376-127X.1000326
38. Jemal Mohammed S, Gebretsadik W, Endashaw G, Shigaz Shimbre M, Assfa Mossa K, Nuriye Metebo K, et al. Determinants of postpartum IUCD utilization among mothers who gave birth in Gamo zone public health facilities, Southern Ethiopia: a case-control study. Open Access J Contracept. (2020) 11:125–33. doi: 10.2147/OAJC.S257762
39. Tariku M, Legesse B, Tantu T, Duko B. Uptake of immediate postpartum LARCs and associated factors among mothers who gave birth at Hawassa University comprehensive specialized hospital, Hawassa, Ethiopia. Int J Reprod Med. (2022) 2022:1–8. doi: 10.1155/2022/1422094
40. Geda YF, Nejaga SM, Belete MA, Lemlem SB, Adamu AF. Immediate postpartum intrauterine contraceptive device utilization and influencing factors in Addis Ababa public hospitals: a cross-sectional study. Contracept Reprod Med. (2021) 6(1):1–10. doi: 10.1186/s40834-020-00145-2
41. Demissie DB, Dadi HW. Immediate postpartum modern family planning utilization and associated factors among women gave birth public health facilities, Addis Ababa, Ethiopia. Res Sq. (2021). doi: 10.21203/rs.3.rs-479663/v1
42. Mohammed S. Assessment of Knowledge, Attitude and Practice of Immediate Postpartum Intra Uterine Contraceptive Device and Associated Factors Among Postpartum Women at Selected Government Hospitals in Addis Ababa, Ethiopia (2019).
43. Usso AA, Adem HA, Dessie Y, Tura AK. Utilization of immediate postpartum long acting reversible contraceptives among women who gave birth in public health facilities in Eastern Ethiopia: a cross-sectional study. Int J Reprod Med. (2021) 2021:1–8. doi: 10.1155/2021/1307305
44. Arero W, Teka W, Jarso H. Prevalence, and pattern of LARC use in immediate postpartum period at Jimma University Medical Center, Ethiopia [18F]. Obstet Gynecol. (2018) 131(1):68S. doi: 10.1097/01.AOG.0000533328.55352.1b
45. Dev R, Kohler P, Feder M, Unger JA, Woods NF, Drake AL. A systematic review and meta-analysis of postpartum contraceptive use among women in low- and middle-income countries. Reprod Health. (2019) 16:1–17. doi: 10.1186/s12978-018-0662-9
46. Tesfu A, Beyene F, Sendeku F, Wudineh K, Azeze G. Uptake of postpartum modern family planning and its associated factors among postpartum women in Ethiopia: a systematic review and meta-analysis. Heliyon. (2022) 8(1):e08712. doi: 10.1016/j.heliyon.2021.e08712
47. Wakuma B, Mosisa G, Etafa W, Mulisa D, Tolossa T, Fetensa G, et al. Postpartum modern contraception utilization and its determinants in Ethiopia: a systematic review and meta-analysis. PLoS One. (2020) 15:1–21. doi: 10.1371/journal.pone.0243776
Keywords: immediate postpartum, family planning, postpartum, utilization, Ethiopia
Citation: Silesh M, Demisse TL, Taye BT, Moltot T, Chekole MS, Wogie G, Kasahun F and Adanew S (2023) Immediate postpartum family planning utilization and its associated factors among postpartum women in Ethiopia: a systematic review and meta-analysis. Front. Glob. Womens Health 4:1095804. doi: 10.3389/fgwh.2023.1095804
Received: 11 November 2022; Accepted: 2 August 2023;
Published: 22 August 2023.
Edited by:
Stephen Kennedy, University of Oxford, United KingdomReviewed by:
Theresa Hoke, Family Health International 360, United StatesEunice Toko Namuyenga, Maseno University, Kenya
© 2023 Silesh, Demisse, Taye, Moltot, Chekole, Wogie, Kasahun and Adanew. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mulualem Silesh c2lsZXNobXVsdWFsZW0yMkBnbWFpbC5jb20=
 Mulualem Silesh
Mulualem Silesh Tesfanesh Lemma Demisse
Tesfanesh Lemma Demisse Birhan Tsegaw Taye
Birhan Tsegaw Taye Tebabere Moltot
Tebabere Moltot Moges Sisay Chekole
Moges Sisay Chekole Girma Wogie
Girma Wogie Fetene Kasahun
Fetene Kasahun Solomon Adanew
Solomon Adanew