- 1Department of Public Health, College of Health Sciences, Assosa University, Assosa, Ethiopia
- 2Department of Reproductive Health and Health Services Management, School of Public Health, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia
- 3Department of Biostatistics and Epidemiology, School of Public Health, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia
- 4Department of Population and Family Health, Institute of Health, Jimma University, Jimma, Ethiopia
Introduction: Adverse pregnancy outcomes are a personal and social crisis caused by easily preventable pregnancy-related problems. Despite that, studies on the effectiveness of adherence to the continuity of antenatal care (ANC) services are scarce. Therefore, this study aims to determine the effectiveness of the continuity of ANC services and the determinants of adverse pregnancy outcomes.
Methods: A prospective follow-up study design was conducted from March 2020 to January 2021 in Northwest Ethiopia among randomly selected study subjects. Data were collected by trained data collectors using pre-tested structured questionnaires and analyzed using STATA Software version 14. A multilevel regression model was used to identify determinant factors, whereas the propensity score matching (PSM) model was used to look at the effectiveness of adherence to ANC services on adverse pregnancy outcomes.
Results: Among 2,198 study participants, 26.8% had adverse pregnancy outcomes, with 95% CI: 24.9–28.7 [abortion (6.1%; 95% CI: 5.1–7.1), low birth weight (11.5%; 95% CI: 10.2–12.9), and preterm birth (10.9; 95% CI: 9.6–12.3)]. Determinant factors were iron-folic acid supplementation (AOR = 0.52; 95% CI: 0.41, 0.68), delayed initiation of ANC visits at 4–6 months (AOR = 0.5; 95% CI: 0.32, 0.8), initiation of ANC visits after 6 months (AOR = 0.2; 95% CI: 0.06, 0.66), received four ANC visits (AOR = 0.36; 95% CI: 0.24, 0.49), an average time of rupture of the amniotic membrane of between 1 and 12 h (AOR = 0.66; 95% CI: 0.45, 0.97), and pregnancy-related problems (AOR = 1.89; 95% CI: 1.24, 2.9). As a treatment effect, completion of a continuum of visit-based ANC (ATET; β = −0.1, 95% CI: −0.15, −0.05), and continuum of care via space dimension (ATET; β = −0.11, 95% CI: −0.15, −0.07) were statistically significant on the reduction of adverse pregnancy outcomes.
Conclusion: In the study area, the rate of adverse pregnancy outcomes was high. Even though adherence to the continuity of ANC services via time and space dimensions is effective in the prevention of adverse pregnancy outcomes, programmatically important factors were also detected. Therefore, key strategies for promoting the uptake of antenatal services and strengthening iron-folic acid supplementation are strongly recommended.
Introduction
Pregnancy is a fruitful and joyful experience in human life that results in pregnancy outcome, the final result of the fertilization event (1). One of the best strategies to ensure a healthy birth is to have a healthy pregnancy. Early antenatal care (ANC) increases the odds of a healthy pregnancy (2, 3), but despite this, pregnancy may result in adverse pregnancy outcomes (abortion, preterm birth and low birth weight) and pregnancy complications (high blood pressure, gestational diabetes, iron deficiency anemia, and severe nausea and vomiting) (4, 5). Adverse pregnancy outcomes are any pregnancy outcomes other than normal live birth, which prominently encompasses preterm birth, stillbirth, and low birth weight. These are the major causes of neonatal morbidity, mortality, and long-term physical and psychological problems, which are critical public health problems in developing and developed countries (3, 6). Similarly, adverse pregnancy outcomes including birth asphyxia and trauma, prematurity, infections, congenital malformations, and disorders related to the perinatal period are the major leading causes of early neonatal mortality and contribute to 75% of early neonatal death (7, 8). Approximately 45% of early neonatal mortality occurs within 24 h after delivery; 19% occurs on the second day, and 16% occurs on the third day. The major causes of stillbirth are infection (37%), prolonged labor (11%), antepartum hemorrhage (10%), preterm birth delivery (7%), cord complications (6%), and accidents (5%) (8).
Globally, 213 million pregnancies occurred in 2012, 89% of which were in developing countries and 11% were in developed countries (9). In 2016, pregnancy-related complications caused approximately 230,600 maternal deaths (4, 5). The common causes of maternal death are bleeding, infection, hypertensive diseases during pregnancy, obstructed labor, miscarriage, abortion, and ectopic pregnancy, which are easily preventable and treatable (4, 5).
In Ethiopia, the prevalence of adverse pregnancy outcomes is high. In 2014, an estimated 620,300 pregnant women ended up having abortions. This implies that the annual abortion rate was 28 per 1,000 pregnancies, and the abortion rate was highest in urban areas (10, 11). The low birth weight in Ethiopia was 13.2% (12), whereas the preterm birth rate was 33.3% in Amhara (13), the low birth weight rate was 27.76% in South Gondar (14) and 24% in North Wolla (15). According to EDHS 2016, the low birth weight rate was 26.2% in Afar, 22.2% in Amhara, and 9.9% in Benishangul Gumuz (12).
Besides these, a variety of factors have been found to worsen the high prevalence of adverse pregnancy outcomes in Ethiopia. Many studies have found that socio-demographic and economic factors including maternal age (13, 15, 16), educational status (13, 15), place of residence (13), marital status and gender (15), occupational status (17), and family monthly income (15) could lead to adverse pregnancy outcomes. Moreover, obstetric factors and other related factors such as short birth interval (13, 16, 18), multipara and multigravidas (15, 16), pregnancy-induced hypertension, premature rupture of membrane, emergency obstetric complications during pregnancy and labor, and a history of adverse pregnancy outcomes (abortion, stillbirth, and preterm birth) (3, 11, 13, 15, 16) could be associated with adverse birth outcomes.
Similarly, other health-related factors were found to be determinant factors of adverse pregnancy outcomes, including maternal nutrition and anemia (3, 15, 16, 18), HIV infection, urinary tract infection, vaginal discharge and malaria (13, 16), public health sectors, legal issues of abortion, abortion procedures and skills of health care providers (11), delivery without induction of labor (17), dietary counseling during ANC follow-up and family planning methods (18), alcohol use (15), women being referred from other health facilities, and multiple pregnancies (3).
However, pregnancy-related complications and adverse pregnancy outcomes could be reduced by improving ANC service utilization and dietary counseling during pregnancy (18). Some limited evidence with weak study design and analysis suggests that the completion of ANC visits reduces preterm birth and low birth weight by 52% and 46% respectively (3, 13, 16, 18, 19). Moreover, receiving recommended ANC visits has a significant impact on preventing adverse pregnancy outcomes (abortion, preterm birth, and LBW) (3, 13–15, 18, 20).
Globally and nationally, attention and priority have been given to maternal health services, specifically ANC services, which is an entry point for maternal health services. The rate of adverse pregnancy outcomes in Ethiopia, especially in the study region, is the highest in the world. Adverse pregnancy outcomes are personal and social crises caused by easily manageable and preventable pregnancy-related problems. Studies on the effectiveness of ANC visits on the prevention of adverse pregnancy outcomes (abortion, preterm birth, and low birth weight) are extremely scarce. Therefore, this study aims to determine the effect of the continuity of ANC services on adverse pregnancy outcomes and the determinant factors that affect adverse pregnancy outcomes at the individual level (level–1) and the community level (level–2). Moreover, the treatment effect of adherence to the continuity of ANC services on adverse pregnancy outcomes was determined using propensity score matching model (PSM).
Methods and materials
Study area
The study was conducted in Benishangul-Gumuz Regional State (BGRS). The region is one of the eleven regions that make up Ethiopia’s Federal Democratic Republic of Ethiopia. Assosa town is the capital city of the region, located 670 km west of Addis Ababa, the capital city of Ethiopia. The region has three zones, three town administrative cities, 21 districts/Woredas, one special district/Woreda, and 475 clusters/Kebeles (439 rural and 36 urban clusters/Kebeles).
The region has an estimated area of 51,381 square kilometers, which represents approximately 4.6% of the total land area of Ethiopia, and is located between 9° 17 N–12° 06 N latitude and 34° 04 E–37° 04 E longitude (21). Based on the 2007 national population and household census, the 2018 population projection revealed that the total population of the region was 1,127,001, consisting of 571,960 (50.75%) men and 555,041 (49.25%) women (with a men-to-women ratio of 1.03) and the total number of households was 246,570 (22); this covers 1.1% of the national population.
Study design and period
A community and health facility-linked prospective follow-up study design was conducted from March 2020 to January 2021.
Population
The source population consisted of pregnant women within the community during the time of the baseline survey who were permanent residents of the region (having lived there for more than 6 months). The study participants were all pregnant women within the selected kebeles/ketenas, which were selected by sampling technique.
Sample size determination
The sample size was calculated using STATA/MP 13.0 software by considering two population proportion formulas based on the following assumption. The outcome variable was adverse pregnancy outcome (abortion, low birth, and preterm birth) and the predictor variable was continuity of ANC visits. Since no study has been conducted in Ethiopia to determine the sample size, a study from other developing countries was used to determine the sample size. A study done in rural Uganda found that the proportion of adverse pregnancy outcomes (“abortion”) among mothers who completed the recommended ANC visits was 8.2% (P1 = 0.082) and the proportion of adverse pregnancy outcomes (“abortion”) among mothers who could not access ANC services was 18% (P2 = 0.18) (23). A 95% confidence level and 80% power were used to detect a 9.8% difference or a 54.4% increment among exposed and non-exposed groups. Hence, r = ratio of exposure to non-exposure pregnant women equal to 1:1 for the population allocation ratio; was calculated (P = 0.13); considering a design effect 2 and a non-response rate of 10%. As a result, the final sample consisted of 823 pregnant women. However, this study was part of extensive research in which 2,402 pregnant women received follow-up care to determine the effects of a continuum of care in maternal health services on adverse birth outcomes (24), which was used as the final sample size for this study.
Sampling procedures and techniques
A multistage sampling technique was employed to select pregnant women for the study. This study was conducted at the regional level. Initially, two zones and one town administrative were selected by simple random sampling (SRS). Then, four districts/“woredas” from Assoa Zone, two districts/“woredas” from Metekel Zone, and two districts/"woredas” from the Assosa town administration were selected using simple random sampling (SRS) techniques. In the third stage, seven kebeles from each district (except the Assosa district/“woreda”, from which 10 kebeles were selected) and five ketenas from each district/“woreda” of town administration were selected and included in the study. Consequently, from the seven kebeles from each district/“woreda”, the 10 kebeles from the Assosa district/“woreda”, and the five ketenas from each district/“woreda” of the town administration, pregnant women were enumerated via house-to-house visits, and all those registered were included in the study. All women who reported having a pregnancy of 8 weeks or above were considered eligible study subjects and enrolled in the study then followed up for 11 months. Assuming that every household that hosted pregnant women hosted at least one pregnant woman, households that hosted pregnant women were taken as a final sampling unit (FSU). Besides the baseline survey, all health facilities found within the catchment area were listed and considered candidates for the health facility survey. As a result, 46 health facilities (3 hospitals, 12 health centers, and 31 health posts) were found within the catchment areas and included in the study.
Data collection instruments and quality assurance
Before data collection, research instruments were formulated in English from different sources: EDHS 2016 (25), National Technical Guidance for MPDSR 2017 (26), MCH Program Indicator Survey 2013 (27), survey tools conducted in Jimma Zone, Southwest Ethiopia (28), survey tools conducted in Rural South Ethiopia (29), and other relevant literature. Then, the instruments were translated into the local language, training was provided for both data collectors and supervisors, and pre-testing was conducted to maintain the quality of the data. During data collection, supervisors and principal investigators checked the work of each of the data collectors for the completeness and relevance of the data.
Data collection process
Before the data collection process, health extension workers (HEWs) were assigned to conduct a census or enumerate pregnant women in each of the clusters/“kebeles” via home visits. Then, the data collection at the baseline as well as during the follow-up phase was conducted by agricultural extension workers, elementary teachers, and health workers (particularly Health workers (HWs) for health facility registration and confirmation of events only). During baseline registration, basic information on the pregnant women was gathered and recorded, including socioeconomic characteristics, household assets to compute wealth index, obstetric characteristics (present and past), and medical history (present and past).
Following that, the selected pregnant women were monitored, and any event that was associated with the use of maternal health services and the outcome of pregnancy and neonatal health conditions was recorded. The data were collected via house-to-house interviews, and the recorded or registered documents were reviewed in the health facility.
Data processing and analysis
To develop skipping patterns and avoid logical mistakes, the collected data were coded and entered into Epi Info version 7.2.2.6. The data were then cleaned, edited, and analyzed using SPSS version 22 and STATA Software version 14. All variables were computed for descriptive statistics. Analyses with only one predictor variable were performed using the crude odds ratio and 95% confidence interval, which help to select candidate variables for multivariable analysis (where p < 0.25). At the level of significance (p < 0.05), a maximum likelihood estimate of the independent effects on the adverse pregnancy outcome was calculated. The Principal Component Analysis (PCA) was used to calculate and categorize the household wealth index. Before running the full model, effect modification at p < 0.1 and multi-collinearity effect between independent variables using variance inflation factors (VIF > 10%) were assessed. All independent variables included in the model had VIF < 10 and the coefficient of the interaction terms was p ≥ 0.1. Thus, interaction and multi-collinearity effects did not exist. Due to cluster variability in this study, a multilevel regression model was employed to identify individual- and community-level factors of adverse pregnancy outcomes (abortion, low birth weight, and preterm birth). In this study, “Kebeles/Ketenas” were considered clusters, and access to the hospital was categorized as a level-2 factor. Individual-level variables, namely socio-demographic characteristics, obstetric characteristics, information on maternal health services, and newborn health services, were taken as level-1 factors. The goodness of fit for the multilevel model was assessed using the log-likelihood ratio (LR) test and intra-class correlation coefficient test. It was found to be statistically significant (p < 0.0001) such as dataset was fitting the multilevel regression. Finally, the average treatment of adherence to the continuity of ANC visit-based services and a continuum of care in maternal health care services via space dimension on adverse pregnancy outcomes was estimated by propensity score matching. The effect was measured by β 95% CI at p < 0.05.
Measurement and operational definition
Abortion: Termination of pregnancy before 28 weeks of GA or at less than 1,000 gm weight of conception.
Antenatal care: Pregnancy-related health care checkups that a pregnant woman receives at a health facility.
Content of ANC package: Pregnant women receive a minimum ANC package, which includes information on signs of danger in pregnancy, blood pressure measurement, iron and folic acid supplementation, nutritional counseling services, urine tests, blood tests, and protection against tetanus.
Preterm birth: Babies born alive before 37 weeks of gestational age.
Low birth weight: Defined by the World Health Organization (WHO) as weight at birth of <2,500 grams.
Results
The rate of adverse pregnancy outcomes and related issues
The rate of adverse pregnancy outcomes among the participants was 26.8% (95% CI: 24.9%, 28.7%). A total of 133 (6.1%) were reported as abortion with 95% CI (5.1%–7.1%), 253 (11.5%) newborns were considered low birth weight (<2.5 kg) with 95% CI (10.2%–12.9%), and 240 (10.9%) newborns were preterm birth (born before 37 weeks of GA) with 95% CI (9.6%–12.3%).
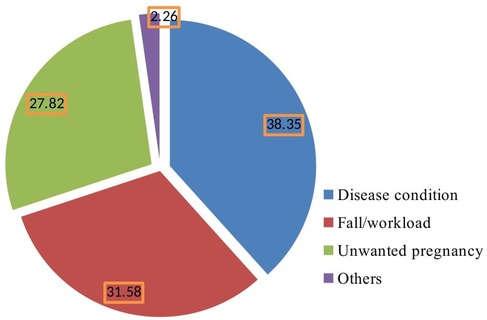
Among the abortion cases detected, there were 57 cases of spontaneous abortion (42.9%) and 39 cases of threatened abortion (29.3%) in the study area. Of them, 29 (21.8%) women had a desire to terminate the pregnancy and 10 (7.5%) had attempted to terminate the pregnancy. Around one-third (46 cases, 34.7%) were unsafe abortions that occurred in unhygienic places. The pregnancy-related problems during pregnancy before the event occurred were excessive vaginal bleeding (78 cases, 58.6%) and severe headache (58 cases, 43.6%). The most common illnesses women encountered during pregnancy before the occurrence of abortion were malaria (40 cases, 30.1%), high blood pressure (35 cases, 26.3%), and heart disease (23 cases, 17.3%) (Table 1). The main possible causes of abortion were disease condition of the mother (51 cases, 38.35%), falls and workload during pregnancy (42 cases, 31.58%), and unwanted pregnancy (37 cases, 27.82%) (Figure 1).
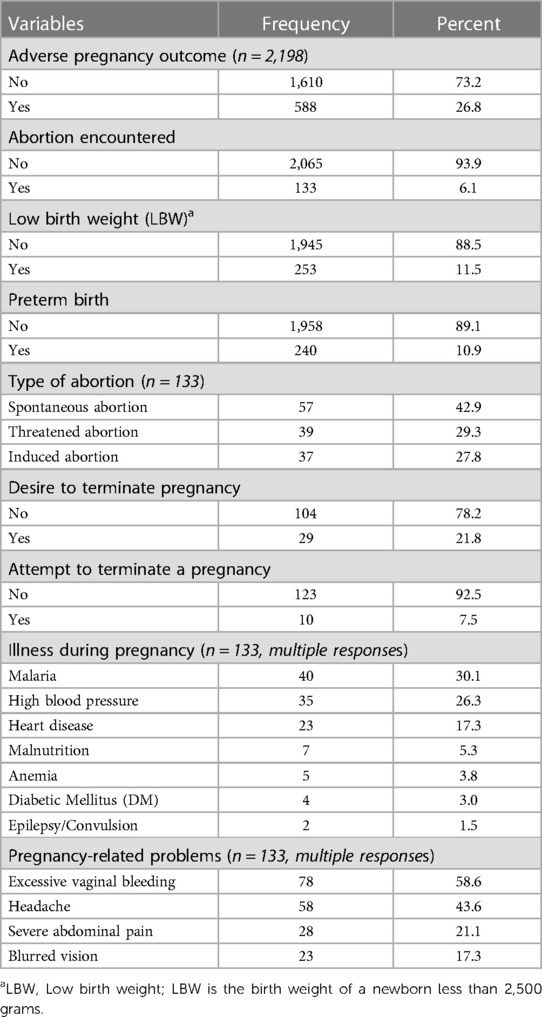
Table 1. Rate and type of adverse pregnancy outcomes and related factors among the study subjects in Benishangul Gumuz Region, Northwestern Ethiopia, March 2020–January 2021.
Determinants of adverse pregnancy outcomes
A multilevel regression model was used to identify individual- and community-level determinant factors of adverse pregnancy outcomes. Before running the full model, the ICC (ρ) for the outcome was determined in the empty model to see if the data fitted a multilevel regression model or not. Then, ICC (ρ) was calculated as a full model for the outcome to detect the variability attributed to clusters after controlling the individual level factors.
Then, ICC (ρ) was calculated in the empty model and it was found to be 0.22, indicating that 22% of the variation was contributed by cluster variations. The test of preference for log-likelihood vs. logistic regression was also statistically significant (P < 0.0001). Following that, the full model was run by considering both the cluster-level and individual-level variables, and the ICC (ρ) was increased to 0.30. This indicates that 30% of the variation was attributed to cluster-level variables. The preference for log-likelihood vs logistic regression was statistically significant (P < 0.0001), suggesting that there was a preference for using a multilevel analysis model (Table 2).
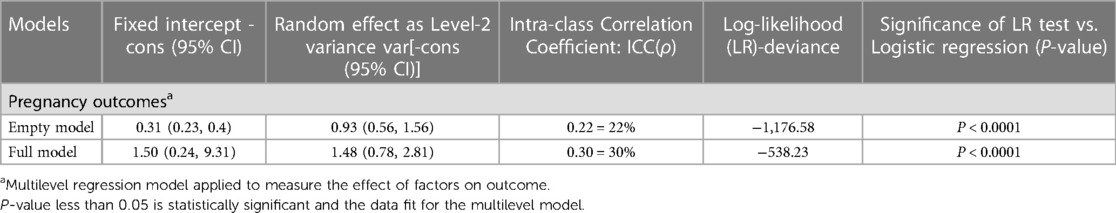
Table 2. Parameters of odds ratio and test of goodness-of-fit of the mixed-effects models, Benishangul Gumuz Region, Northwest Ethiopia, 2021.
After adjusting for a confounding effect in the final two-level mixed-effects model, cluster-level variables did not predict adverse pregnancy outcomes. The association with the expected outcomes was found to be not statistically significant. Among the lower-level variables, different factors were identified as important determinant factors of adverse pregnancy outcomes.
Besides these, the odds of having adverse pregnancy outcomes among women who started ANC after 6 months of gestational age (AOR = 0.20; 95% CI: 0.06, 0.66) and within 4–6 months of gestational age (AOR = 0.50; 95% CI: 0.32, 0.80) were, respectively, 80% and 50% lower than among women who started ANC visits within 3 months. Similarly, the odds of the occurrence of adverse pregnancy outcomes among women who received the recommended ANC visits (≥4 visits) (AOR = 0.32; 95% CI: 0.24, 0.52) and iron-folic acid supplementation during pregnancy (AOR = 0.52; 95% CI: 0.28, 0.0.93) were, respectively, 68% and 48% lower than their counterpart.
Moreover, the odds of encountering adverse pregnancy outcomes among women who had pregnancy-related problems during pregnancy (AOR = 1.89; 95% CI: 1.24, 2.90) were two times higher than among women who didn't have pregnancy-related problems. The odds of having an abortion, low birth weight, and preterm birth among women who had an average time of rupture of amniotic membranes of between 1 and 12 h before labor (AOR = 0.66; 95% CI: 0.45, 0.97) were 44% lower than among those who had an average time of rapture of amniotic membranes of less than 1 h before labor (Table 3).
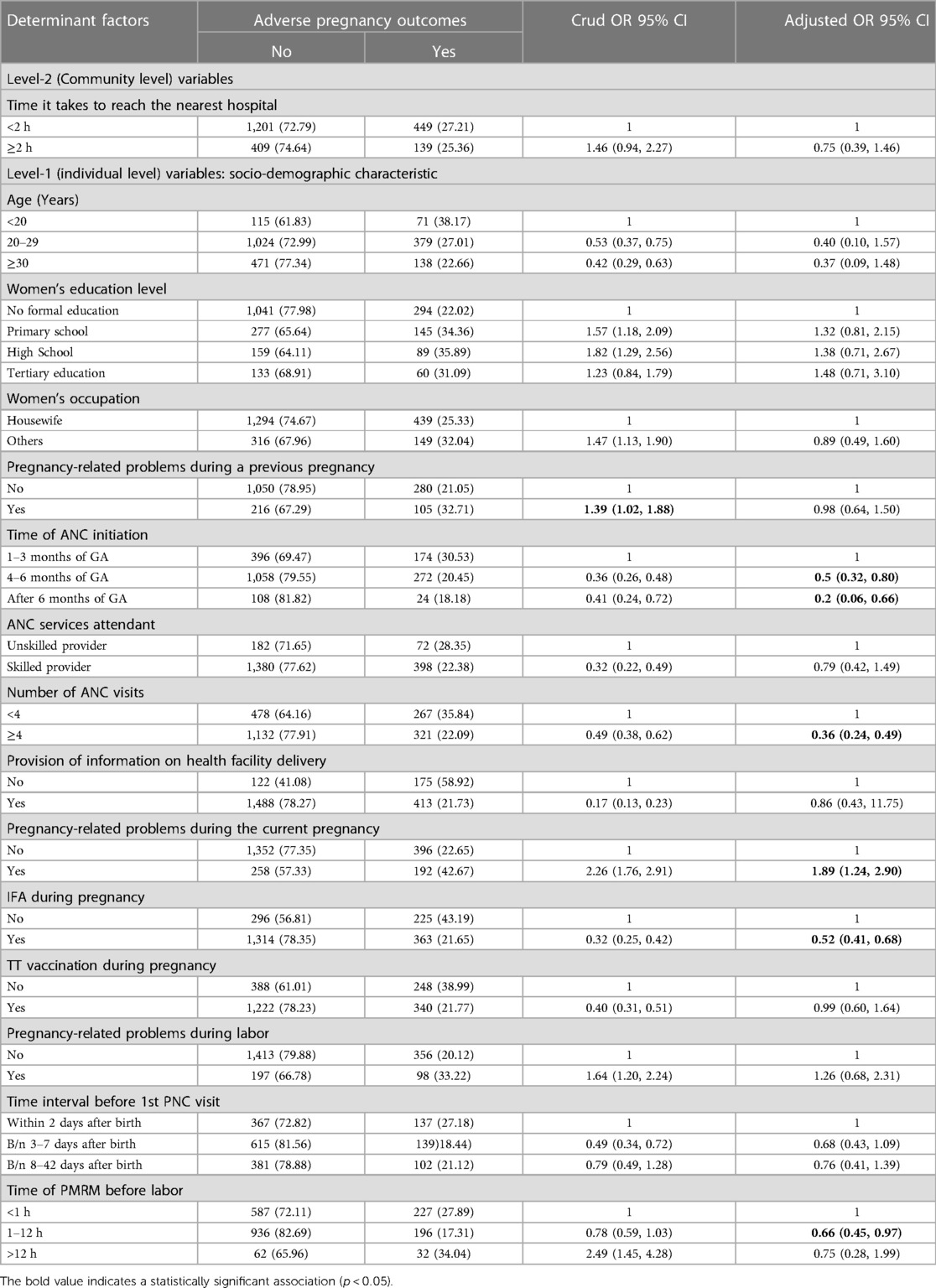
Table 3. Multilevel regression models analysis on determinants of pregnancy outcomes, Benishangul Gumuz Region, Northwest Ethiopia, 2021.
The effect of the continuity of ANC packages on adverse pregnancy outcomes
Propensity score matching (PSM) approaches were used to compare women who adhered to the continuity of ANC visits and received their key intervention packages to those who discontinued ANC visits and key interventions. These models were used to limit the risk of confounding effects. Of the five different approaches to propensity score matching (PSM), one-to-one matching was used to estimate the effect of interventions on adverse pregnancy outcomes. After matching treated and controlled individuals, the effects of the continuity of ANC visits and their key interventions and the continuum of care via the space dimension on adverse pregnancy outcomes (abortion, low birth weight, and preterm birth) were determined.
The results indicate that receiving a first ANC visit (ATET; β = −0.18; 95% CI: −0.26, −0.11; p < 0.001); receiving a fourth ANC visit (ATET; β = −0.1; 95% CI: −0.15, −0.05; p < 0.001); receiving ANC services conducted by a skilled attendant (ATET; β = −0.17; 95% CI: −0.24, −0.11; p < 0.001); and completing the continuum of care via space dimension (ATET; β = −0.11; 95% CI: −0.15, −0.07; p < 0.001) are associated with a significant reduction in the likelihood of adverse pregnancy outcomes (abortion, low birth weight, and preterm birth) (Table 4).
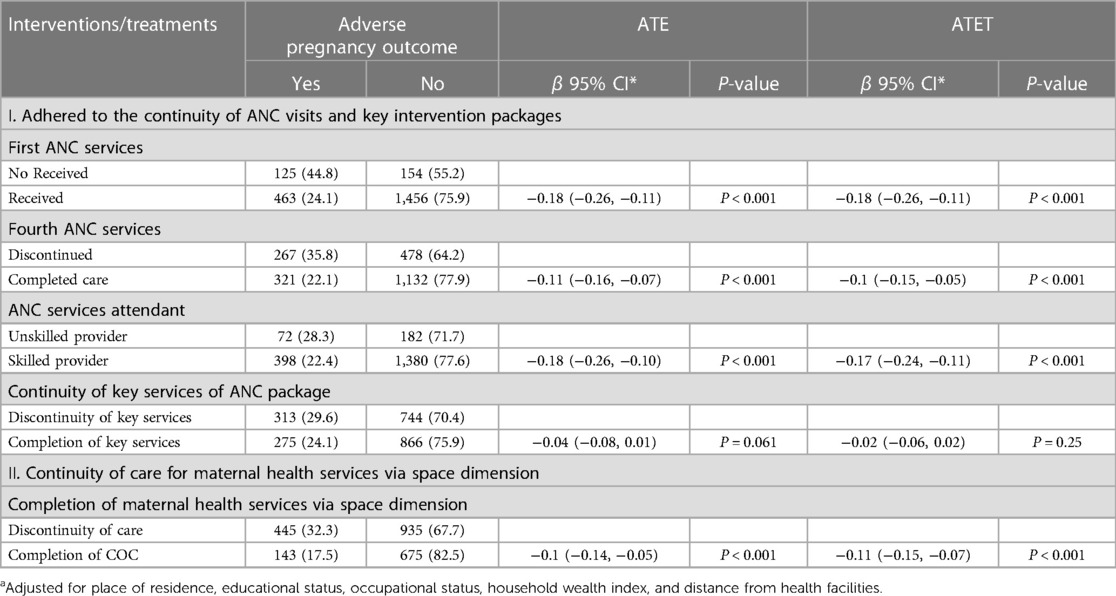
Table 4. Propensity score matching analysis on the effect of adherence to the continuity of ANC services on pregnancy outcomes in Benishangul Gumuz Region, Northwest Ethiopia, March 2020–January 2021.
Discussion
Generally, this study aims to assess the rate of adverse pregnancy outcomes and their determinant factors and to measure the effectiveness of adherence to the continuity of ANC visit-based and content-based services on adverse pregnancy outcomes.
The rate of adverse pregnancy outcomes
Abortion, preterm birth, and low birth weight are common adverse pregnancy outcomes that are attributed to poor maternal health conditions and poor utilization of maternal health services. This study found that the rate of adverse pregnancy outcomes was 26.8%. This finding is higher than that of a study in Rural southwest Uganda (10.8%) (23) but lower than that of a study in Southwest Nigeria (37.05%) (17). This discrepancy is due to variation in socio-demographic and economic factors, cultural influences and beliefs, knowledge and attitudes of the community, and accessibility of health facilities and medical equipment.
In the year 2014, an estimated 620,300 pregnancies resulted in abortion, implying that the annual abortion rate was 28 per 1,000 pregnancies in Ethiopia (10, 11). Besides this, this study found that the rate of abortion was 6.1%, occurring in 61 per 1,000 pregnancies, which is far higher than the annual abortion rate in Ethiopia (10, 11). Despite the various efforts made in Ethiopia, including in the study areas, to improve maternal health services and strengthen family planning services, there is no reduction in the rate of abortion. However, this finding is lower than those of studies conducted in rural northwest Bangladesh (35.7%) (30), Rural Uganda (8.4%) (23), and Rural South Western Uganda (8.6%) (23). The reason might be the variability of legal issues on abortion procedures in Ethiopia and other countries worsening and/or reducing the occurrence of adverse pregnancy outcomes. However, this finding is much higher than those of studies in other countries and across the nation. This discrepancy may be because the study area is highly remote, with poor infrastructure and roads, and the community has low awareness and a lack of knowledge on the advantages of early detection and management of adverse pregnancy outcomes, particularly abortion.
In Ethiopia, unsafe abortion was the leading cause of maternal mortality and morbidity. In this study, more than one-third of the abortion cases constituted unsafe abortion, occurring in an unhygienic place. Furthermore, we found that women encountered severe vaginal bleeding and severe headache prior to the occurrence of abortion. Women also encountered illnesses during pregnancy before the occurrence of abortion, namely malaria, high blood pressure, and heart disease. However, the main possible causes of abortion were disease condition of the mother, falls, workload during pregnancy, and unwanted pregnancy.
Preterm birth can cause lifelong effects such as cerebral palsy, intellectual disability, visual and hearing impairments, growth retardation, and poor health outcomes. In line with these, this study found that the rate of preterm birth was 10.9%, which is consistent with a study in Gondar University Hospital, which reported the rate at 14.2% (31), whereas it is lower than evidence from Amhara (33.3%) (13) and Southwest Nigeria (22.08%) (17) but higher than the rate reported in Hawassa town health facility (3.6%) (32). This discrepancy may be due to the variation of socio-demographic, cultural, and custom differences and the issue of study time and design.
Low birth weight exposes newborns to a variety of negative health consequences: fetal and neonatal mortality and morbidity, stunted growth, cognitive development, and chronic disorders. In this study, the prevalence of low birth weight was 11.5%, which is consistent with evidence from Gondar University Hospital (11.2%) (31) and Hawassa town health facility (11.6%) (32). This finding is higher than the result from Bahar Dar administrative city (7.8%) (33), Tigray (7.5%) (19), and Benishangul Gumuz region (9.9%) (12) but it is lower than the findings of studies in Ethiopia (13.2%) (12), Amhara region (22.2%) (12), South Gondar (27.76%) (14); North Wolla (24%) (15), Afar (26.2%) (12), Northern Nigeria (20%) (34), Southwest Nigeria (14.98) (17), and Eastern Uganda (13.4%) (35). This discrepancy can be explained by the variability of access to health facilities, availability of medical supplies, and societal awareness of nutritional requirements during pregnancy.
Associated factors of adverse pregnancy outcomes
Early initiation and adherence to the recommended schedule of ANC visits help in the early diagnosis, prevention, and treatment of pregnancy-related problems and complications, which minimize the occurrence of adverse pregnancy outcomes (36). In contrast, this study found that the odds of having adverse pregnancy outcomes among women who started ANC after 6 months of gestational age (AOR = 0.20) and within 4–6 months of gestational age (AOR = 0.50) were lower than among women who started ANC visits within 3 months. This can be explained by pregnant women attending a health facility as early as possible when they suffer pregnancy-related problems and abnormal indications being identified. The probability of the occurrence of adverse pregnancy outcomes among women who have pregnancy-related complications is high.
The World Health Organization recommends the use of ANC services that can help overcome pregnancy-related complications and avoid adverse pregnancy outcomes. In line with this, this study found that the odds of the occurrence of adverse pregnancy outcomes among women who received the recommended ANC visits were 76% lower than their counterparts. This finding is supported by studies conducted in other parts of the country, namely Northwest Ethiopia (20), South Gondar (14), Amhara region (13), and Jimma University Specialized Hospital (3), and also in other countries, such as Eastern Uganda (35), rural Uganda (23), Southwest Nigeria (17), and Northern Nigeria (34). This is because during ANC visits, any pregnancy-related problems are detected and appropriate treatments are provided to overcome complications that could increase the risk of the occurrence of abortion, premature birth, and low birth weight. The recommended ANC visits create an opportunity to receive good care during pregnancy, which is significantly important for the health of the mother and the development of the fetus within the womb, and promotes healthy behaviors that enhance the chances of good pregnancy outcomes.
Maternal nutrition and dietary counseling during pregnancy are significantly important interventions to reduce the occurrence of adverse pregnancy outcomes. Hence, this study depicts that the odds of the occurrence of adverse pregnancy outcomes among women who received iron-folic acid supplementation during pregnancy were 48% lower than among women who did not receive iron-folic acid supplementation. This finding is supported by the findings of studies in South Gondar (6) and Bahar Dar administrative city (33). This is because of the direct effect of the maternal nutritional status on placental size, the strength of the membrane, and the fetus. As a result, providing iron-folic acid supplementation and increasing the frequency of the provision of nutritional advice for pregnant women contribute to the increased birth weight of newborns and the maturity of the fetus within the womb (33).
In this study, women who had pregnancy-related problems during pregnancy were found to be two times more likely to have adverse pregnancy outcomes. This finding is consistent with a study conducted in South Gondar (6), Amhara region (13), Hawassa town HF (32), and Jimma University Hospital (3). This implies that a history of abnormal birth outcomes, pregnancy and childbirth-related complications, chronic illness, current pregnancy-related complications, and illness are risk factors for the occurrence of abnormal pregnancy outcomes in subsequent pregnancies and in the current pregnancy outcomes. This could be related to a decrease in placental blood flow caused by endothelial cell damage and blood vessel constriction. This disorder disrupts the mother-fetus interaction of nutrients and oxygen, resulting in abnormal pregnancy outcomes, such as abortion, low birth weight, preterm birth, and stillbirth.
Effect of adherence to ANC services on adverse pregnancy outcomes
The continuity of maternal health services has been recognized as a strategy for minimizing gaps in adverse pregnancy outcomes by connecting pregnant women to health-promoting resources, avoiding the duplication of effort, improving communication between families and health providers (37), and retaining pregnant women within the pathway of maternal health services visits (38–40). In line with this, this study found that for women who received a first ANC visit; received a fourth ANC visit; received ANC services conducted by a skilled attendant; received key services of the ANC package, and completed the continuum of care via space dimension, the rate of adverse pregnancy outcomes was reduced by 18%, 11%, 18%, 4%, and 10%, respectively, compared with their counterparts. This finding is consistent with the results of prior studies in Northwest Ethiopia (20), Bahar Dar administrative city (33), Tigray (19), Hawassa town health facility (32), Ghana (41), and North Carolina (37). This implies that high-quality ANC can improve pregnancy outcomes in two dimensions: directly through preventative measures and indirectly by encouraging deliveries in healthcare settings, where difficulties can be better addressed (41). Moreover, primary health care services, particularly focusing on maternal health services and social support, reduce adverse pregnancy outcomes (2). Evidence in the UK suggests that continuity of care is a core intervention in the health system used to reduce preterm births and improve the survival of neonates (42).
Conclusion
This study found that more than a quarter of the women involved experienced adverse pregnancy outcomes. Before the occurrence of abortion, women encountered excessive vaginal bleeding and severe bleeding. The common illnesses women frequently suffered during pregnancy were malaria, blood pressure, and heart disease. Iron-folic acid supplementation during pregnancy, early ANC initiation, and completion of the recommended ANC services were found to be major protective interventions against adverse pregnancy outcomes, whereas pregnancy-related problems during pregnancy and premature rupture of the membrane were found to be determinant factors of adverse pregnancy outcomes. As a treatment effect, the completion of ANC visits and receipt of the key content of ANC services via time and space dimensions significantly reduce adverse pregnancy outcomes. Therefore, key strategies for promoting the uptake of antenatal services and strengthening iron-folic acid supplementation are strongly recommended, alongside increasing utilization of key packages of antenatal services and conducting awareness creation campaigns on maximizing the benefits of prenatal care.
Data availability statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the Research Review and Ethics Committee (REC) of School of Public Health, Addis Ababa University with protocol number SPH/3089/011. Then, Ethical approval was acquired from the Institutional Review Board (IRB) of the College of Health Science, Addis Ababa University with protocol number 048/19/SPH. The Regional Health Bureau provided formal approval letters to their respective local administrative offices. Before any data collection begins, each respondent provided verbal consent to participate in the study. By deleting any identities from the questionnaire, confidentiality was maintained. The patients/participants provided their written informed consent to participate in this study.
Author contributions
All authors contributed to the conception, design, and execution of the study and the acquisition, analysis, and interpretation of the data; prepared and commented on the manuscript; gave final approval of the version to be published, agreed to submit to the journal, and agreed to be accountable for all aspects of the work. All authors contributed to the article and approved the submitted version.
Acknowledgments
We would like to thank Addis Ababa University, College of Health for providing ethical approval and partially sponsoring our work. The authors would also like to express their gratitude to all of the pregnant women, data collectors, supervisors, and other individuals who contributed directly or indirectly to the study’s success. Last but not least, the authors wish to express their gratitude to Miss Abebech Tefera, Miss Chaltu Argeta, Dr. Nigatu Disassa, and Assistant Professor Atnafu Morka for their unwavering assistance in the preparation, management, and duplication of the research questionnaires.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bahk J, Yun S-C, Kim Y-m, Khang Y-H. Impact of unintended pregnancy on maternal mental health: a causal analysis using follow up data of the panel study on Korean children (PSKC). BMC Pregnancy Childbirth. (2015) 15(1):85. doi: 10.1186/s12884-015-0505-4
2. Dunlop AL, Dubin C, Raynor BD, Bugg GW Jr, Schmotzer B, Brann AW Jr. Interpregnancy primary care and social support for African-American women at risk for recurrent very-low-birthweight delivery: a pilot evaluation. Matern Child Health J. (2008) 12(4):461–8. doi: 10.1007/s10995-007-0279-z
3. Yeshialem E, Abera M, Tesfay A. Determinants of adverse pregnancy outcomes among mothers who gave birth in jimma university specialized hospital, case control study, 2016. Ethiopian J Reprod Health. (2019) 11(1):10. Available at: https://ejrh.org/index.php/ejrh/article/view/235
4. GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980−2016: a systematic analysis for the global burden of disease study 2016. Lancet. (2017) 390(10100):1151–210. doi: 10.1016/S0140-6736(17)32152-9
5. Say L, Chou D, Gemmill A, Tunçalp Ö, Moller AB, Daniels J, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. (2014) 2(6):e323–33. doi: 10.1016/S2214-109X(14)70227-X
6. Addisu D, Biru S, Mekie M, Minuye B, Bezie M, Alebachew W, et al. Predictors of adverse pregnancy outcome at Hospitals in South Gondar Zone, North-central Ethiopia: a multicenter facility-based unmatched case-control study. Heliyon. (2021) 7(2):e06323-e. doi: 10.1016/j.heliyon.2021.e06323
7. Engmann C, Walega P, Aborigo RA, Adongo P, Moyer CA, Lavasani L, et al. Stillbirths and early neonatal mortality in rural Northern Ghana. Tropl Med Int Health. (2012) 17(3):272–82. doi: 10.1111/j.1365-3156.2011.02931.x
8. Engmann C, Garces A, Jehan I, Ditekemena J, Phiri M, Mazariegos M, et al. Causes of community stillbirths and early neonatal deaths in low-income countries using verbal autopsy: an international, multicenter study. J Perinatol. (2012) 32(8):585–92. doi: 10.1038/jp.2011.154
9. Sedgh G, Singh S, Hussain R. Intended and unintended pregnancies worldwide in 2012 and recent trends. Stud Fam Plann. (2014) 45(3):301–14. doi: 10.1111/j.1728-4465.2014.00393.x
10. Moore AM, Gebrehiwot Y, Fetters T, Wado YD, Bankole A, Singh S, et al. The estimated incidence of induced abortion in Ethiopia, 2014: changes in the provision of services since 2008. Int Perspect Sex Reprod Health. (2016) 42(3):111. doi: 10.1363/42e1816
11. Gebrehiwot Y, Fetters T, Gebreselassie H, Moore A, Hailemariam M, Dibaba Y, et al. Changes in morbidity and abortion care in Ethiopia after legal reform: national results from 2008 to 2014. Int Perspect Sex Reprod Health. (2016) 42(3):121. doi: 10.1363/42e1916
12. Ethiopia Central Statistical Agency (CSA) and ICF. Ethiopia demographic and health survey 2016. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF.: The DHS program ICF Rockville, Maryland, USA. (2017). Available at: https://dhsprogram.com/pubs/pdf/FR328/FR328.pdf
13. Woday A, Muluneh MD. Determinants of preterm birth among mothers who gave birth at public hospitals in the Amhara region, Ethiopia: a case-control study. PLoS ONE. (2019) 14(11):e0225060. doi: 10.1371/journal.pone.0225060
14. Mihretie G, Bisetegn T, Gelaye K, Ayele T. The effect of antenatal depression on birth weight among newborns in South Gondar zone, Northwest Ethiopia: a population-based prospective cohort study. Arch Public Health. (2021) 79:121. doi: 10.1186/s13690-021-00567-7
15. Wubetu AD, Amare YE. Newborn birth weight and associated factors among mother-neonate pairs in public hospitals, North Wollo, Ethiopia. Pediatric Health Med Ther. 2021;2021(11):111–8. doi: 10.2147/PHMT.S299202
16. Laelago T, Yohannes T, Tsige G. Determinants of preterm birth among mothers who gave birth in East Africa: systematic review and meta-analysis. Ital J Pediatr. (2020) 46(1):10. doi: 10.1186/s13052-020-0772-1
17. Awoleke JO, Olofinbiyi BA. Poor prenatal service utilization and pregnancy outcome in a tertiary health facility in Southwest Nigeria. Pan Afr Med J. (2020) 35:28. doi: 10.11604/pamj.2020.35.28.20426
18. Hailemichael HT, Debelew GT, Alema HB, Weldu MG, Misgina KH. Determinants of adverse birth outcome in Tigrai region, North Ethiopia: Hospital-based case-control study. BMC Pediatr. (2020) 20(1):10. doi: 10.1186/s12887-019-1835-6
19. Haftu A, Hagos H, Mehari MA, G/Her B. Pregnant women adherence level to antenatal care visit and its effect on perinatal outcome among mothers in tigray public health institutions, 2017: cohort study. BMC Res Notes. (2018) 11(1):872. doi: 10.1186/s13104-018-3987-0
20. Worku AG, Yalew AW, Afework MF. The contributions of maternity care to reducing adverse pregnancy outcomes: a cohort study in Dabat district, northwest Ethiopia. Matern Child Health J. (2014) 18(6):1336–44. doi: 10.1007/s10995-013-1367-x
21. United Nations Development Programme—Ethiopia (UNDP). The Benishangul Regional State is selected for design of model REDD program under the UNFCCC Warsaw framework. (2017). Available at: https://www.undp.org/sites/g/files/zskgke326/files/migration/et/564b2c04d28fb9d51671ff55a627808510ebfbc49cba774c343394c26fc46f3b.pdf
22. Federal Democratic Republic of Ethiopia Central Statistical Agency (CSA). Population projection of Ethiopia for all regions at Wereda level from 2014 to 2017. Addis Ababa, Ethiopia. (2013). Available at: http://www.statsethiopia.gov.et/wp-content/uploads/2019/05/Population-Projection-At-Wereda-Level-from-2014-2017.pdf
23. Asiki G, Baisley K, Newton R, Marions L, Seeley J, Kamali A, et al. Adverse pregnancy outcomes in rural Uganda (1996–2013): trends and associated factors from serial cross sectional surveys. BMC Pregnancy Childbirth. (2015) 15:279. doi: 10.1186/s12884-015-0708-8
24. Zelka MA, Yalew AW, Debelew GT. The effects of completion of continuum of care in maternal health services on adverse birth outcomes in Northwestern Ethiopia: a prospective follow-up study. Reprod Health. (2022) 19(1):200. doi: 10.1186/s12978-022-01508-5
25. Ethiopia Central Statistical Agency (CSA) and ICF. Ethiopia demographic and health survey 2011. Addis Ababa: The DHS program ICF Rockville, Maryland, USA. (2012). Available at: https://dhsprogram.com/pubs/pdf/fr255/fr255.pdf
26. Ethiopian Minisry of Health (MoH). National technical guidance for maternal and perinatal death surveillance and response (MPDSR). Ethiopian Public Health Institue. (2017). Available at: https://www.ephi.gov.et/images/pictures/National-Maternal-and-Perinatal–Death-Surveillance-and-Response-guidance-2017.pdf
27. Agha S, Williams E. Maternal and child health program indicator survey 2013, Sindh Province. MNCH Services component, USAID/Pakistan MCH Program. Karachi, Pakistan: Jhpiego. (2013). Available at: https://www.mchip.net/sites/default/files/MCH%20Program%20Indicator%20Survey%20Report%202013%20Sindh%20Province.pdf
28. Debelew GT, Afework MF, Yalew AW. Determinants and causes of neonatal mortality in Jimma Zone, Southwest Ethiopia: a multilevel analysis of prospective follow up study. PLoS One. (2014) 9(9):e107184. doi: 10.1371/journal.pone.0107184
29. Balla YY, Data T, Lindtjorn B. Maternal and neonatal mortality in rural south Ethiopia: outcomes of community-based birth registration by health extension workers. PLoS ONE. (2015) 10(3). doi: 10.1371/journal.pone.0119321
30. Sikder SS, Labrique AB, Craig IM, Wakil MA, Shamim AA, Ali H, et al. Patterns and determinants of care seeking for obstetric complications in rural northwest Bangladesh: analysis from a prospective cohort study. BMC Health Serv Res. (2015) 15:166. doi: 10.1186/s12913-015-0832-1
31. Adane AA, Ayele TA, Ararsa LG, Bitew BD, Zeleke BM. Adverse birth outcomes among deliveries at Gondar University Hospital, Northwest Ethiopia. BMC Pregnancy Childbirth. (2014) 14:90. doi: 10.1186/1471-2393-14-90
32. Tsegaye B, Kassa A. Prevalence of adverse birth outcome and associated factors among women who delivered in Hawassa town governmental health institutions, south Ethiopia, in 2017. Reprod Health. (2018) 15(1):193. doi: 10.1186/s12978-018-0631-3
33. Tafere TE, Afework MF, Yalew AW. Providers adherence to essential contents of antenatal care services increases birth weight in Bahir Dar City Administration, North West Ethiopia: a prospective follow up study. Reprod Health. (2018) 15(1):163. doi: 10.1186/s12978-018-0610-8
34. Onwuhafua PI, Williams ICO, Kolawole AO, Adze JA. The effect of frequency of antenatal visits on pregnancy outcome in Kaduna, Northern Nigeria. Trop J Obstet Gynaecol. (2016) 33:317–21. doi: 10.4103/0189-5117.199813
35. Kananura RM, Wamala R, Ekirapa-Kiracho E, Tetui M, Kiwanuka SN, Waiswa P, et al. A structural equation analysis on the relationship between maternal health services utilization and newborn health outcomes: a cross-sectional study in Eastern Uganda. BMC Pregnancy Childbirth. (2017) 17(1):98. doi: 10.1186/s12884-017-1289-5
36. Sarker BK, Rahman M, Rahman T, Rahman T, Khalil JJ, Hasan M, et al. Status of the WHO recommended timing and frequency of antenatal care visits in Northern Bangladesh. PLoS ONE. (2020) 15(11):e0241185. doi: 10.1371/journal.pone.0241185
37. Hillemeier MM, Domino ME, Wells R, Goyal RK, Kum H-C, Cilenti D, et al. Effects of maternity care coordination on pregnancy outcomes: propensity-weighted analyses. Matern Child Health J. (2015) 19(1):121–7. doi: 10.1007/s10995-014-1502-3
38. Kikuchi K, Ansah EK, Okawa S, Enuameh Y, Yasuoka J, Nanishi K, et al. Effective linkages of continuum of care for improving neonatal, perinatal, and maternal mortality: a systematic review and meta-analysis. PLoS One. (2015) 10(9):e0139288. doi: 10.1371/journal.pone.0139288
39. Kikuchi K, Okawa S, Zamawe CO, Shibanuma A, Nanishi K, Iwamoto A, et al. Effectiveness of continuum of care-linking pre-pregnancy care and pregnancy care to improve neonatal and perinatal mortality: a systematic review and meta-analysis. PLoS One. (2016) 11(10):e0164965. doi: 10.1371/journal.pone.0164965
40. Emiru AA, Alene GD, Debelew GT. Women’s retention on the continuum of maternal care pathway in west Gojjam zone, Ethiopia: multilevel analysis. BMC Pregnancy Childbirth. (2020) 20(1):258. doi: 10.1186/s12884-020-02953-5
41. Afulani PA. Determinants of stillbirths in Ghana: does quality of antenatal care matter? BMC Pregnancy Childbirth. (2016) 16(1):132. doi: 10.1186/s12884-016-0925-9
Keywords: abortion, Benishangul Gumuz, continuity of ANC visits, low birth weight, preterm birth
Citation: Zelka MA, Yalew AW and Debelew GT (2023) The effects of adherence to recommended antenatal services on adverse pregnancy outcomes in Northwest Ethiopia: multilevel and propensity score matching (PSM) modeling. Front. Glob. Womens Health 4:1082405. doi: 10.3389/fgwh.2023.1082405
Received: 24 March 2023; Accepted: 12 June 2023;
Published: 26 June 2023.
Edited by:
Ramon Escuriet, Blanquerna Ramon Llull University, SpainReviewed by:
Diana Navarro Llobet, Granollers General Hospital, SpainFelipe Ojeda, Granollers General Hospital, Spain
© 2023 Zelka, Yalew and Debelew. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Muluwas Amentie Zelka bXVsdXdhczEyQGdtYWlsLmNvbQ==
 Muluwas Amentie Zelka
Muluwas Amentie Zelka Alemayehu Worku Yalew3
Alemayehu Worku Yalew3