- 1Department of Psychiatry, Dilla University, Dilla, Ethiopia
- 2Department of Nursing, Wolkite University, Wolkite, Ethiopia
- 3Department of Comprehensive Nursing, Wachemo University, Hossana, Ethiopia
- 4Department of Psychiatry, Injibara University, Injibara, Ethiopia
- 5Research and Training Department, Amanuel Mental Specialized Hospital, Addis Ababa, Ethiopia
- 6School of Public Health, Curtin University, Perth, WA, Australia
- 7Department of Psychiatry, College of Medicine and Health Science, Wollo University, Dessie, Ethiopia
Introduction: Cognition is defined as the mental activity or process of learning information and understanding through reason, experience, and the senses. In Sub-Saharan African nations like Ethiopia, such assessments of a pregnant mother's mental health during antenatal care are uncommon procedures. Instead, there is a greater focus on the physical well-being of the woman and her fetus. As a result, this study aimed to evaluate the cognitive deficits and related factors in a pregnant women attending an antenatal care service.
Methods: This hospital-based cross-sectional study included 415 pregnant women who were receiving antenatal care at Dilla University Referral Hospital in Dilla, Gedeo Zone, Ethiopia. In this study, respondents were chosen using systematic random sampling, and study participants were interviewed using administered questions to gather pertinent data. This study used the OSLO Social Support Scale, the Alcohol, Smoking, and Substance Involvement Screening Test, and the Mini-Mental Status Examination to assess the social support, cognitive status, and current substance use history of a respondent. Descriptive statistics including frequencies, graphs, and percentages were used to describe the results. A logistic regression analysis was conducted to determine the connection between independent factors and the outcome variable at a 95 percent confidence level and p < 0.05.
Result: Among all respondents who came for antenatal care visits, only 24 (5.8%) were unmarried (single, divorced, widowed). The mean age of respondents was 26 years old and 155 (37.3%) had attended secondary school. Variables such as strong social support [0.11 (0.03–0.23), p < 0.02], being a follower of orthodox religion [0.24 (0.12–0.39), p < 0.04], ≥5,000 Ethiopian birr monthly income [0.28 (0.17–0.48), p < 0.02], age >26 years old [1.23 (1.14–2.54), p < 0.04], unplanned pregnancy [2.78 (1.45–4.32), p < 0.02], and rural residence [3.90 (2.23–7.34), p < 0.04] were significantly associated with cognitive impairment at 95% confidence interval and a p-value <0.05.
Conclusion: This study found that pregnant women who attended antenatal care experienced a significant reduction in cognitive disorders. Additionally, this study revealed adjustable factors such as unwanted pregnancy, social support, and religiosity. It is preferable to check a pregnant woman's cognitive condition at antenatal services and to follow-up on each additional visit.
Introduction
The term “cognition” identifies a set of mental functions that are included in the receiving, processing, interpreting, and retrieving of information (1). Cognitive abilities are essential to a person's entire development because they involve many of the brain's fundamental processes, including thinking, reading, learning, retaining knowledge, and paying attention. These processes are used to solve problems, recall tasks, and make judgments (2). Globally, the prevalence of cognitive impairment ranges from 5.1% to 41%, with a median of 19.0%, and the incidence of cognitive impairment ranges from 22% to 76.8%, with a median of 53.97 per 1,000 person-year (3).
The term “pregnancy” is used to describe the time when a fetus develops inside a woman's uterus or womb from the last menstrual cycle to delivery. The average pregnancy lasts roughly 40 weeks, or just over 9 months (4). Worldwide, approximately one-fourth of adolescent women have become pregnant and in Africa, the percentage of adolescent pregnancy is 18.8%, with 19.3% of reported cases in Sub-Saharan Africa and 21.5% in Eastern Africa (5).
Many women go through a period of cognitive shift known as the “pregnancy brain” during pregnancy and the postpartum period. Mental fogginess and memory issues are the symptoms that women at these reproductive stages report experiencing the most (6). Additionally, it involves a general lack of emotional stability and self-control as well as an aggravating loss of declarative memory, which includes forgetting names and important faces (7).
The prevalence of cognitive impairment among pregnant women has been reported in several countries including northern India (23.73 ± 4.69) (8), Indonesia (81%) (9), and Nigeria (58.3%) (10). The contributing factors for cognitive problems during pregnancy are a maternal occupation, a change in thyroid functions (hypothyroxinemia) (11), second and third-trimester gestational age (12), incomplete pregnancy (13), co-morbid medical conditions (14), physical exercise (15), and personality characteristics differences (16). The health of the mother and the unborn child may suffer as a result of cognitive impairment during pregnancy, which could lead to an undesirable pregnancy and unhealthy offspring. Experiencing a cognitive disorder while pregnant causes changes to hormones such as cortisol, which have a direct impact on the baby's normal brain development (17). According to imaging studies, a pregnant woman's mental changes are also responsible for a baby having an active amygdala in the womb, which is connected to emotional problems like anxiety and sadness (18). Furthermore, mental instability during pregnancy has an impact on a baby's hippocampal growth and brain chemistry, both of which are crucial for learning and emotional expression (19). Managing cognitive changes during pregnancy requires regular eating habits and physical activity, maintaining stable relationships with friends and family, and abstaining from the use of narcotics and psychoactive substances (20).
Despite the importance of the health of a mother and her fetus, there are insufficient studies done in East Africa, including Ethiopia. As a consequence, the purpose of this study is to determine the prevalence of cognitive impairment and its factors among pregnant women who would get ANC follow-up service at Dilla University Referral Hospital. This study aims to identify knowledge gaps, demonstrate the severity of the issue in research areas, assist in creating plans and interventions that are appropriate for pregnant women and the cognitively impaired, and provide knowledge to health professionals so they can develop efficient strategies.
Methods and materials
Study area
The study was conducted at Dilla University Referral Hospital (DURH). DURH has five wards, namely medical (39 beds), surgical (26 beds), obstetrics/gynecology (9 beds), pediatrics (18 beds), and psychiatry (12 beds). The hospital has one psychiatry outpatient department, three medical outpatient departments, one surgical outpatient department, one pediatric outpatient department, and one antenatal care (ANC) follow-up service. ANC is a maternal healthcare service provided by skilled healthcare professionals aimed at risk identification, prevention, management of pregnancy-related or concurrent disease, and health education and health promotion.
Study design and period
An institutional-based cross-sectional study was conducted from May 12 to June 30, 2022.
Study populations
This study enrolled all pregnant women who were attending antenatal follow-up at DURH in Dilla Town Public Health Institution. All pregnant mothers who came to DURH for an ANC follow-up visit during the time of the data collection period were the study population.
Eligibility criteria
All pregnant women aged 18 years and above were included in this study, whereas participants who were critically ill or had difficulty communicating were excluded from the study.
Sample size determination
The sample size was determined using a single population proportion formula by an assumption of p = 50%, based on assumptions of unknown proportion with 95% confidence interval and 5% margin of error. By assuming a 10% non-response rate, the total sample size was computed to be (1.96)2 × 0.5(1–0.5)/(0.5)2 = 384 + 38(10%) = 422.
Sampling procedure
All eligible pregnant women attending at Dilla University were eligible to participate. A systematic random sampling technique was used to select the study participants. On average, a total of 1,100 participants came for ANC visits in each month. A regular interval (K) was calculated as 1100 ÷ 422 = 2.60–3. Therefore, every 3rd patient from the list of appointments was selected.
Data collection procedures and instruments
After the data was gathered utilizing the interview-administered data collection method, the data was recorded using the epi-collect software. Socio-demographic data, obstetric and maternal factors, substance-related factors, clinical issues, social factors, and cognitive impairment were all questioned by the data collectors. The information was gathered from participants using a questionnaire that was translated into Amharic and Gedeoffa language.
Standard Mini-Mental State Exam (SMMSE–30) is a tool used to assess cognitive impairment and includes components for orientation, attention, registration, computation, recall, and language. The administration time is between 10 and 15 min. The Mini-Mental State Examination (MMSE) is graded on a scale of 0–30, with 0–9 indicating severe cognitive impairment, 10–19 indicating moderate cognitive impairment, 20–24 indicating mild cognitive impairment, and >24 indicating no cognitive impairment. The patient's native language, educational attainment, and culture are considered when calculating the results of the mental status evaluation (25.26.27). A score of 22/30 was deemed to indicate cognitive impairment for participants with the educational levels of being unable to read or write and having not completed grade 8. Participants with an educational level of grade 9 were regarded to have cognitive impairment if their scores were less than 24/30. The MMSE had a sensitivity of 81% (95% CI, 78%–84%) and specificity of 89% (95% CI, 87%–92%) (17).
The Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST-3.0) was used to evaluate individuals' current use of alcohol, tobacco, chewing khat, and cannabis. It was created by the World Health Organization (WHO) to identify the use of psychoactive substances and associated issues in patients receiving primary care. Participants were classified as current substance users if they had used any psychoactive substance in the last three months (18).
The Oslo Social Support Scale (OSS-3) is a quick test of social functioning, regarded as one of the finest indicators of mental health. It includes several social support fields such a counting a number of helping groups. It measures other closeness, interest, and concern, and assistance in the real day-to-day activities. The OSS-3 results ranged from 3 to 14 on a scale; 3–8 is considered poor, 9–11 indicates moderate support; 12–14 indicates strong support (19).
Measurement
The outcome variable (dependent variable) was “cognitive impairment” among pregnant women. Thus, the independent variables used for multiple logistic regression analysis were age, religion, marital status, educational status, number of family members, residence, income, and occupation. Clinical factors in this study were previous history of mental illness, physical and psychological factors, abortion, stillbirth, live birth, neonatal death, pregnancy planned, total number of pregnancies, gestational age, number of antenatal care visits, current use of khat chewing, alcohol intake, and cigarette smoking.
Data quality assurance
The pretest was done on participants with 5% of the sample size in Yirgga Cheffe hospital. Data collectors and supervisors were trained on the data collection tool and sampling techniques. Supervision was held regularly during the data collection period by both the researcher and supervisors. Written informed consent was taken from all respondents before the actual data collection period. The wholeness and consistency of the data were cross-checked and cleaned manually.
Statistical analysis and processing
Epi-collect software was used to enter the data, which was then transferred to SPSS version 20 for additional analysis and cleaning. The results were presented using frequency, proportion, and descriptive techniques. To identify independently associated factors for cognitive impairment, binary logistic regression was used to determine the association between different factors and the outcome variable, and then all independent variables with a p-value of <0.25 were entered in the final model (multivariable logistic regression). The model fitness was examined using the Hosmer and Lemeshow goodness-of-fit test. At the appropriate 95% confidence interval, factors with a p-value of 0.05 or lower were statistically significantly associated with cognitive impairment.
Results
Socio-demographic data
This study included a respondents with 98% response rate. Among all respondents who came for antenatal visits, 24 (5.8%) were unmarried (single, divorced, widowed). The median income of the respondents was 5,000 Ethiopian birr and 155 (37.3%) had attended secondary school. Out of all respondents, 396 (95.4%) were from a rural area and 87 (20.9%) had government worker husbands (Table 1).
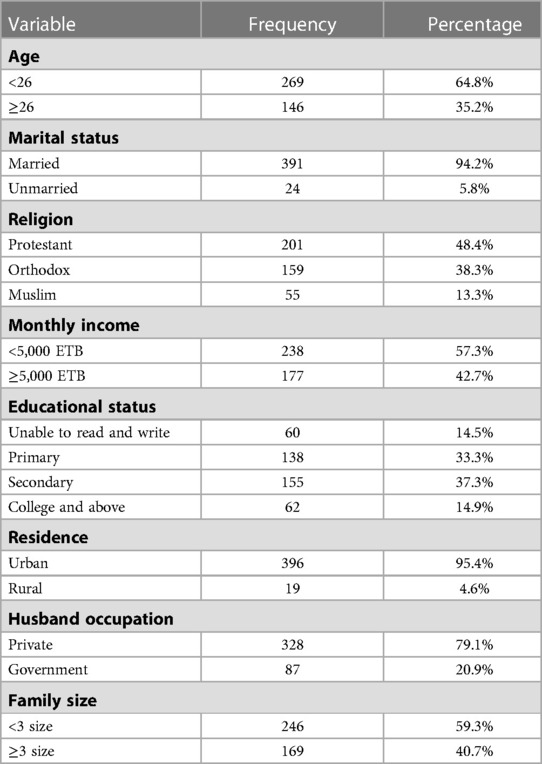
Table 1. Socio-demographic characteristics of respondents attending antenatal services at Dilla University Referral Hospital, Dilla, 2022, (N = 415).
Pregnancy-related variables
Out of the respondents who came for antenatal care, 344 (82.9%) of them had planned pregnancy, and 29 (7%) had current pregnancy complications. The majority of the participants 183 (44.1%) were the second trimester and 47 (11.3%) of them had a history of abortion (Table 2).
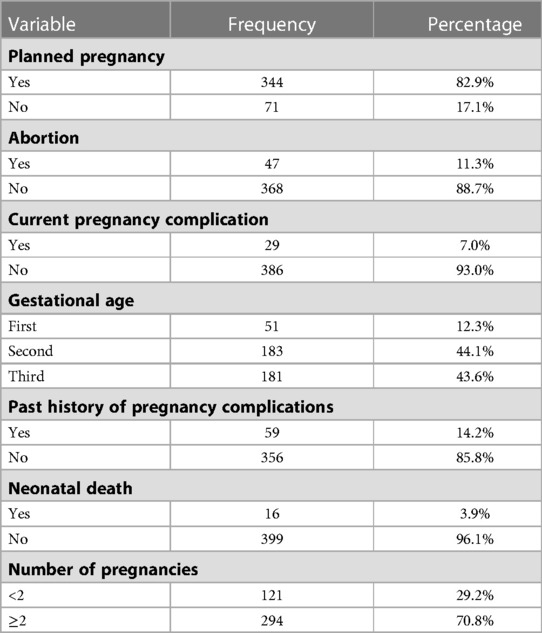
Table 2. Pregnancy-related characteristics of respondents attending antenatal service at Dilla University Referral Hospital, Dilla, 2022, (N = 415).
Psychosocial variables
Out of the total respondents, 4 (1%) had a history of rape and 52 (12.5%) had a history of the loss of a loved one. Only 24 (5.8%) of respondents had reported a history of physical, psychological, or sexual violence and 2 (0.5%) had been diagnosed with mental illness (Table 3).
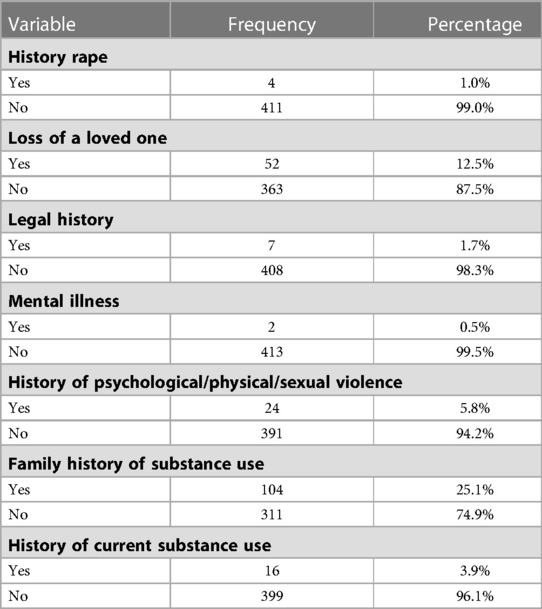
Table 3. Psychosocial characteristics of respondents attending antenatal service at Dilla University Referral Hospital, Dilla, 2022, (N = 415).
Cognitive disorder
The mean score of the Mini-Mental State Exam among pregnant women is (26 ± 2), 95% (SD = 25.8–26.5). Out of all respondents enrolled in this study, 112 (27%) of them had a cognitive impairment and scored (<24/30).
The logistic regression analysis result
According to this study result, variables such as strong social support [0.11 (0.03–0.23), p < 0.02], orthodox religion followers [0.24 (0.12–0.39), p < 0.04], >5,000 Ethiopian birr monthly income [0.28 (0.17–0.48), p < 0.02], age >26 years old [1.23 (1.14–2.54), p < 0.04], unplanned pregnancy [2.78 (1.45–4.32), p < 0.02] and rural residence [3.90 (2.23–7.34), p < 0.04] were significantly associated with cognitive impairment at 95% confidence interval and p < 0.05 (Table 4).
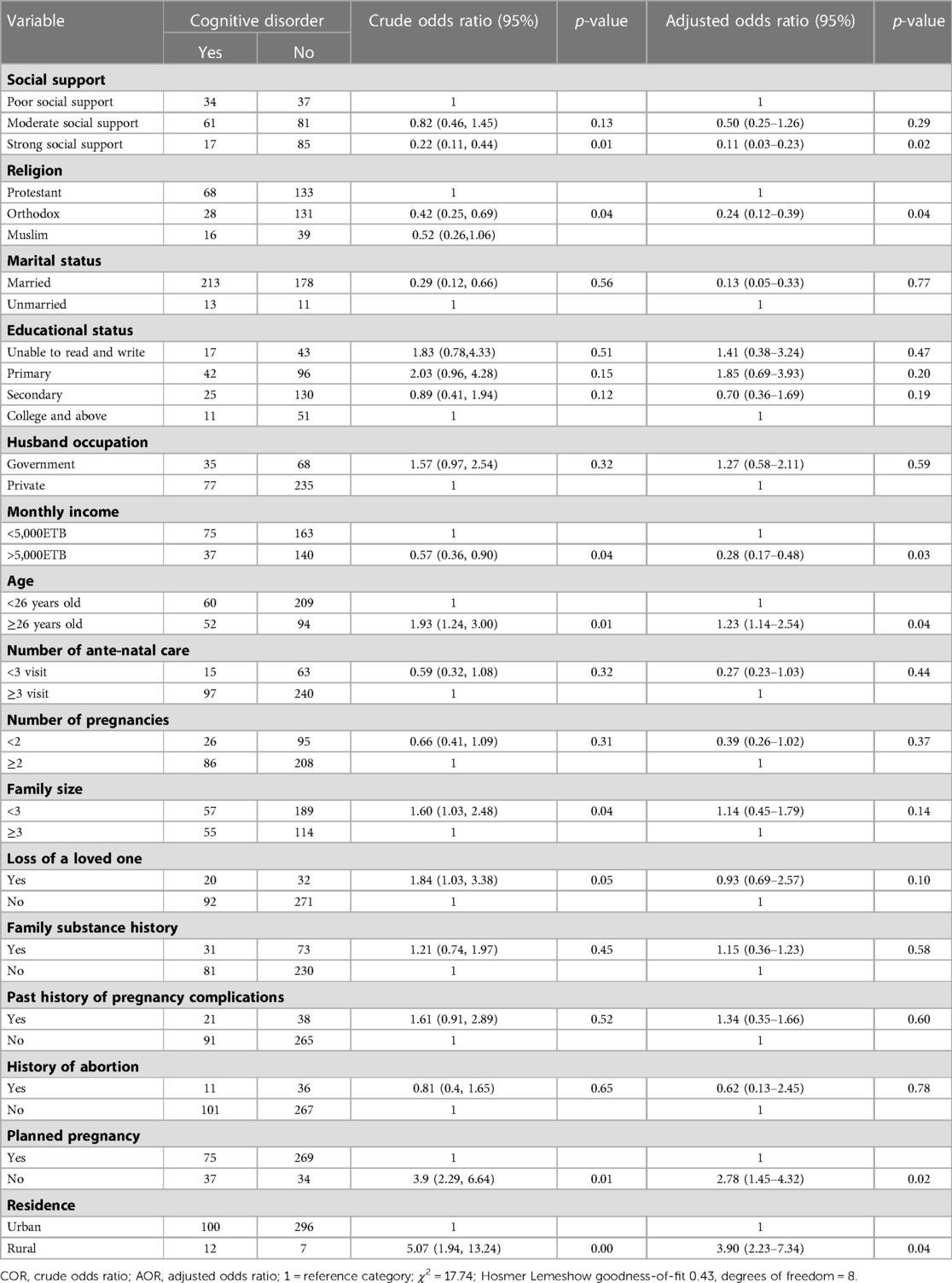
Table 4. Bivariate and multivariate logistic regression analysis of respondents attending antenatal service at Dilla University Referral Hospital, Dilla, 2022 (N = 415).
Discussion
Cognitive dysfunction is characterized by deficiencies in motor functioning, linguistic and nonverbal learning, short-term and working memory, visual and auditory processing, problem-solving, and attention (16). According to previous reports, the stress of pregnancy and the influence of hormonal changes during pregnancy may be to blame for reported cognitive impairment (4). This study found that 112 (27%) of respondents had cognitive impairment and variables such as strong social support, orthodox religion follower, unable to read and write, >5,000 Ethiopian birr monthly income, age >26 years old, unplanned pregnancy, and rural residence were significantly associated with cognitive impairment. This study revealed that 27% with 95% CI (22.9%–31.6%) respondents had cognitive impairment which was in line with a study done in northern India, (23.73 ± 4.69) (8). However, this study finding was lower than the studies done in Indonesia (81%) (9), and Nigeria (58.3%) (10). This might be attributed to the difference in the study setting, socio-demographic characteristics, and nutritional status of respondents. This study also revealed that respondents who were orthodox religion followers were 0.24 (0.12–0.39), p < 0.04) times less likely to develop cognitive impairment which is consistent with the results of study completed in Australia (20). Perhaps religious activities such as singing, praying, worshipping, attending sermons, bible reading, and socializing with other believers can maintain abundant neocortical brain synapses and minimize cognitive impairment.
Pregnant women who had an income ≥5,000 ETB were 0.28 (0.17–0.48) times less likely to have cognitive impairment than their referent group. This result finding is consistent with the results of other research conducted in Ethiopia (21). An increased monthly income can make it possible for the fulfillment of provisions such as food, shelter, and other necessities that are vital for cognitive development. This study also found that those respondents with age ≥26 years old were 1.23 (1.14–2.54) times more likely to confront cognitive impairment. This is also supported by another study done in Ethiopia (22). Effectiveness on mental tasks, such as tests of processing speed, working memory, and executive cognitive function, which call for one to quickly analyze or change information in order to make a choice, declines with age (23). This study also found that respondents with unplanned pregnancy status were 2.78 (1.45–4.32) times more likely to experience cognitive impairment. Unwanted pregnancies result in psychological ill-preparedness, a lack of interest in the pregnancy period, a lack of motivation to work, excessive worry about the future, and poor assertiveness, all of which are linked to the cognitive deficit (24). This study also found that respondents with rural residence were 3.90 (2.23–7.34) times more likely to encounter cognitive decline as compared with their counterparts. This study finding is consistent with a study done that attributed the impact of living in rural area to a lack of exploring calendars, urban environments, hospitals, and other locations that are necessary for cognitive assessment (25). The final predictor variable associated with cognitive decline was strong social support and this study revealed that respondents with strong social support were 0.11 (0.03–0.23) times less likely to have scores associated with cognitive decline as compared with those with poor social support. Good social support helps with physical health, food, psychological wellbeing, maintaining relationships, practical assistance, emotional support, and confirmation of values and attitudes (26).
Conclusion
This study found that nearly one-fourth of respondents had developed cognitive impairment during pregnancy. Predictors associated with a higher chance of cognitive impairment were strong social support, following orthodox religion, ≥5,000 Ethiopian birr monthly income, age >26 years old, unplanned pregnancy, and rural residence. In addition, strengthening social support and having a wanted pregnancy is also important good mental state. It is crucial to assess respondents' cognitive capacities in order to provide better psychological antenatal care and to strive to increase social acceptance of their pregnancy. The routine assessment of cognitive function and integrating mental health services with antenatal care service is vital for the overall wellbeing of a pregnant mother.
Data availability statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by The research ethics approval was obtained from the institutional review board (IRB) of Dilla University College of medicine and health science (duirb877/22/06). The procedures used in this inquiry were in accordance with the values indicated in the Declaration of Helsinki. Each respondent supplied written informed consent prior to the survey's implementation. The patients/participants provided their written informed consent to participate in this study. Written informed consent was not obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
All authors contributed significantly to the work that was published, whether it is in the generation of ideas, study design, execution, data collection, analysis, and interpretation, or in all of these areas. TA and CK: prepared the manuscript for publication. They also all participated in writing, revising, or critically evaluating the article, gave their final approval for the version that would be published, agreed on the journal to which the article would be submitted, and agreed to be held responsible for all aspects of the work. All authors contributed to the article and approved the submitted version.
Acknowledgments
We thank Dilla University, the data collectors, and the respondents who participated in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bayne T, Brainard D, Byrne RW, Chittka L, Clayton N, Heyes C, et al. What is cognition? Curr Biol. (2019) 29(13):R608–15. doi: 10.1016/j.cub.2019.05.044
2. Greenfield EA, Reynolds A, Moorman SM. Life course linkages between enriching early-life activities and later life cognition: evidence from the Wisconsin longitudinal study. Soc Sci Med. (2022) 294:114673. doi: 10.1016/j.socscimed.2021.114673
3. Pais R, Ruano L, Carvalho OP, Barros H. Global cognitive impairment prevalence and incidence in community dwelling older adults—a systematic review. Geriatrics. (2020) 5(4):84. doi: 10.3390/geriatrics5040084
4. Fishel Bartal M, Lindheimer MD, Sibai BM. Proteinuria during pregnancy: definition, pathophysiology, methodology, and clinical significance. Am J Obstet Gynecol. (2020) 226(2S):S819–S834. doi: 10.1016/j.ajog.2020.08.108. Epub 2020 Sep 1. 32882208.
5. Kassa GM, Arowojolu A, Odukogbe A, Yalew AW. Prevalence and determinants of adolescent pregnancy in Africa: a systematic review and meta-analysis. Reprod Health. (2018) 15(1):1–17. doi: 10.1186/s12978-018-0640-2
6. Brown E, Schaffir J. “Pregnancy brain”: a review of cognitive changes in pregnancy and postpartum. Obstet Gynecol Surv. (2019) 74(3):178–85. doi: 10.1097/OGX.0000000000000655
7. Kumari R. Baby brain or pregnancy brain or momnesia. Int J Nurs Educ ResResearch. (2019) 7(1):115–8. doi: 10.5958/2454-2660.2019.00023.1
8. Meena PS, Soni R, Jain M, Jilowa CS. Cognitive dysfunction and associated behaviour problems in postpartum women: a study from North India. East Asian Arch Psychiatry. (2016) 26(3):104–8.27703098
9. Mukhlis H, Putri RH, Puspita L, Wardani PK, Fitri NL. Variables associated to the decline of cognitive function in the third trimester of pregnancy. J Crit Rev. (2020) 7(14):1449–56. doi: 10.31838/jcr.07.14.328
10. Yarube IU, Friday J, Alhassan A, Saleh M. Cognitive dysfunction among primi gravidae attending an ante natal clinic in Kano, Northwest Nigeria. Niger J Physiol Sci. (2019) 34(1):43–8. https://pubmed.ncbi.nlm.nih.gov/31449270/31449270
11. Pop VJ, Ormindean V, Mocan A, Meems M, Broeren M, Denollet JK, et al. Maternal cognitive function during pregnancy in relation to hypo-and hyperthyroxinemia. Clin Endocrinol. (2019) 91(6):824–33. doi: 10.1111/cen.14107
12. Barda G, Mizrachi Y, Borokchovich I, Yair L, Kertesz DP, Dabby R. The effect of pregnancy on maternal cognition. Sci Rep. (2021) 11(1):1–6. doi: 10.1038/s41598-021-91504-9
13. Li F-D, He F, Chen T-R, Xiao Y-Y, Lin S-T, Shen W, et al. Reproductive history and risk of cognitive impairment in elderly women: a cross-sectional study in eastern China. J Alzheimers Dis. (2016) 49(1):139–47. doi: 10.3233/JAD-150444. 26444784.26444784
14. John CM, Mohamed Yusof NIS, Abdul Aziz SH, Mohd Fauzi F. Maternal cognitive impairment associated with gestational diabetes mellitus—a review of potential contributing mechanisms. Int J Mol Sci. (2018) 19(12):3894. doi: 10.3390/ijms19123894
15. Klein CP, Hoppe JB, Saccomori AB, Dos Santos BG, Sagini JP, Crestani MS, et al. Physical exercise during pregnancy prevents cognitive impairment induced by amyloid-β in adult offspring rats. Mol Neurobiol. (2019) 56(3):2022–38. doi: 10.1007/s12035-018-1210-x
16. Casey P. A longitudinal study of cognitive performance during pregnancy and new motherhood. Arch Womens Ment Health. (2000) 3(2):65–76. doi: 10.1007/s007370070008
17. Lacy M, Kaemmerer T, Czipri S. Standardized mini-mental state examination scores and verbal memory performance at a memory center: implications for cognitive screening. Am J Alzheimer's Dis Other Dement®. (2015) 30(2):145–52. doi: 10.1177/1533317514539378
18. John WS, Zhu H, Greenblatt LH, Wu L-T. Recent and active problematic substance use among primary care patients: results from the alcohol, smoking, and substance involvement screening test in a multisite study. Subst Abus. (2021) 42(4):487–92. doi: 10.1080/08897077.2021.1901176
19. Kocalevent R-D, Berg L, Beutel ME, Hinz A, Zenger M, Härter M, et al. Social support in the general population: standardization of the Oslo social support scale (OSSS-3). BMC Psychol. (2018) 6(1):1–8. doi: 10.1186/s40359-017-0211-2
20. Hosseini S, Chaurasia A, Oremus M. The effect of religion and spirituality on cognitive function: a systematic review. Gerontologist. (2019) 59(2):e76–e85. doi: 10.1093/geront/gnx024
21. Wubetu AD, Asefa KK, Gebregiorgis BG. Prevalence of neurocognitive impairment and associated factors among people living with HIV on highly active antiretroviral treatment, Ethiopia. HIV/AIDS. (2021) 13:425. doi: 10.2147/HIV.S298141. 33889028; 8057951.
22. Salahuddin M, Manzar MD, Hassen HY, Unissa A, Hameed UA, Spence DW, et al. Prevalence and predictors of neurocognitive impairment in Ethiopian population living with HIV. HIV/AIDS. (2020) 12:559. doi: 10.2147/HIV.S260831. 33116918; 7568595.
23. Román G, Jackson R, Gadhia R, Román A, Reis J. Mediterranean diet: the role of long-chain ω-3 fatty acids in fish; polyphenols in fruits, vegetables, cereals, coffee, tea, cacao and wine; probiotics and vitamins in prevention of stroke, age-related cognitive decline, and Alzheimer disease. Rev Neurol. (2019) 175(10):724–41. doi: 10.1016/j.neurol.2019.08.005
24. Sharman LS, Douglas H, Price E, Sheeran N, Dingle GA. Associations between unintended pregnancy, domestic violence, and sexual assault in a population of Queensland women. Psychiatry. Psychol Law. (2019) 26(4):541–52. doi: 10.1080/13218719.2018.1510347
25. Ginja S, Jackson K, Newham JJ, Henderson EJ, Smart D, Lingam R. Rural-urban differences in the mental health of perinatal women: a UK-based cross-sectional study. BMC Pregnancy Childbirth. (2020) 20(1):1–11. doi: 10.1186/s12884-020-03132-2
Keywords: Antenatal Care, Cognitive, pregnancy, Dilla, Ethiopia
Citation: Kassaw C, Wale T, Negash M, Temesgen K, Mekuriaw B, Tolessa O, Abdisa EN, Chekol YA, Ayano G and Anbesaw T (2023) Cognitive disorder and associated factors among pregnant women attending antenatal service at Dilla University Referral Hospital, 2022. Front. Glob. Womens Health 4:1061626. doi: 10.3389/fgwh.2023.1061626
Received: 4 October 2022; Accepted: 4 May 2023;
Published: 19 May 2023.
Edited by:
Michaela Hynie, York University, CanadaReviewed by:
Sugarmaa Myagmarjav, Mongolian National University of Medical Sciences, MongoliaTungalagsuvd Altankhuu, Mongolian National University of Medical Sciences, Mongolia
© 2023 Kassaw, Wale, Negash, Temesgen, Mekuriaw, Tolessa, Abdisa, Chekol, Ayano and Anbesaw. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tamrat Anbesaw dGFtcmF0YW5iZXNhd0BnbWFpbC5jb20=
 Chalachew Kassaw
Chalachew Kassaw Tiruwork Wale1
Tiruwork Wale1 Birhanie Mekuriaw
Birhanie Mekuriaw Elias Nigusu Abdisa
Elias Nigusu Abdisa Yigrem Ali Chekol
Yigrem Ali Chekol Getinet Ayano
Getinet Ayano Tamrat Anbesaw
Tamrat Anbesaw