- 1Higher Institute of Health Sciences, Nazi Boni University, Bobo-Dioulasso, Burkina Faso
- 2Department of Gynecology, Obstetrics and Reproductive Medicine, Sourô Sanou University Hospital Center, Bobo-Dioulasso, Burkina Faso
- 3Health Science Training and Research Unit, Joseph Ki-Zerbo University, Ouagadougou, Burkina Faso
- 4Department of Gynecology-Obstetrics, Yalgado Ouedraogo Teaching Hospital, Ouagadougou, Burkina Faso
- 5Research Institute of Health Sciences (IRSS), Ouagadougou, Burkina Faso
- 6Obstetrics Gynecology Department, Regional Teaching Hospital of Ouahygouya, Ouahigouya, Burkina Faso
- 7Department of Gynecology-Obstetrics, Regional Hospital Center of Koudougou, Koudougou, Burkina Faso
Introduction: Intrapartum stillbirth is an indicator of health and community development.
Objective: To identify the risk factors associated with intrapartum stillbirth in a tertiary teaching hospital in Burkina Faso.
Patients and methods: A case-control study conducted from January 1 to August 30, 2019. Cases were defined as patients admitted to Yalgado Ouedraogo teaching hospital (YOTH) with a live fetus of at least 28 weeks’ gestation and who gave birth to an intrapartum stillborn, a fetus delivered without any signs of life in the first minute postpartum. Controls were defined as patients who delivered a live newborn. Study controls were gradually recruited and matched to cases. For each case, two controls were recruited and matched according to criteria such as delivery route and day of delivery. Data were cleaned in Epidata and exported to Stata for analysis. Variables with a p < 0.05 significance level in the multivariable regression were retained. Odds ratio (OR) and 95% confidence intervals are reported.
Results: Eighty-three intrapartum stillbirths were documented among a total of 4,122 deliveries, a stillbirth rate of 20.1 per 1,000 births. There was a statistically significant association between intrapartum stillbirth and prior caesarean section (p = 0.045), multiparity (p = 0.03), the receipt of antenatal care (ANC) by a nurse (p = 0.005) and the disuse of the partogram (p = 0.004). We did not find a significant association between the number of ANC consultations performed (p = 0.3), whether membranes were ruptured at admission (p = 0.6), the duration of labor (p = 0.6) and intrapartum fetal death. Multivariate analysis showed that patient referral to another heath facility (OR: 3.33; 95% IC: 1.56, 7.10), no obstetric ultrasound performed (OR: 3.16; 95% IC: 2.11, 4.73), birth weight less than 2,500 g (OR: 7.49; 95% IC: 6.40, 8.76) were significantly associated with intrapartum stillbirth.
Conclusion: Specific interventions must be taken to identify these risk factors of intrapartum stillbirth in order to ensure better and appropriate management.
1. Introduction
Stillbirths are an indicator of the health and development of a community (1). In the worldwide, the intrapartum mortality rate varies from region to region. Stillbirth has decreased significantly in developed countries due to the per partum component, likely a result of better access to care (2). This rate seems higher when the socio-economic level of the community is low. In 2006, according to the World Health Organization (WHO), in Africa 7.5% of fetuses die during the perinatal period, including 4.1% in the intrapartum period and 3.4% in the early neonatal period. This is a reflection of the low level of health (3). Significant progress remains to be made because the figures are still high in Sub-Saharan Africa (4, 5). These rates are the indicators that best reflect the quality of prenatal consultations and labor monitoring (6). There is very little data on stillbirths in Burkina Faso, like many countries in sub-Saharan Africa, but has high rates of intrapartum deaths (7–10) and the intrapartum stillbirth rate is disparate from one region to another. In 2018, according to data from the Department of Health and Family, the per partum death rate was very high in the Centre (41.4%), Centre-Ouest (48.1%) and Haut-Bassins regions (43.7%) (11). It was the ratio of fresh stillbirths to the total number of stillbirths in these regions. In the obstetrics department of Yalgado Ouedraogo teaching hospital in Ouagadougou (YOTH), the intrapartum stillbirth rate remains high (63.4% of all stillbirths) (11). It was the ratio of fresh stillbirths to the total. In order to prevent future death, the present study aims to identify the factors associated with intrapartum stillbirth at YOTH.
2. Patients and method
The study took place in the Obstetrics department of the Yalgado Ouedraogo University Hospital Center in Ouagadougou (YOTH), Burkina Faso. A prospective case-control study was conducted of intrapartum stillbirth over a period of 8 months from January 1 to August 30, 2019. Women in labor carrying an active pregnancy of at least 28 weeks’ gestation were eligible for the study. All patients who delivered an intrapartum stillborn during the study period were included. Cases were defined as patients admitted to CHU-YO with a live fetus of at least 28 weeks’ gestation and who gave birth to an intrapartum stillborn, a fetus delivered without any signs of life in the first minute postpartum. Controls were defined as patients who delivered a live newborn. Study controls were gradually recruited and matched to cases. For each case, two controls were recruited and matched according to criteria such as delivery route and day of delivery. Antepartum stillbirths as well as live births with present cardiac activity, yet who died afterwards were excluded from the study. In addition, patients who delivered at home or in route to the health facility were not included. Pre-existing health conditions of women during pregnancy were taken into account in the exclusion criteria.
Interviews with patients and register and record review were conducted using individual data collection forms. Data collection was carried out by students specializing in the said department. The mothers of stillbirths were informed that this was a study and their consent was taken before the administration of the questionnaire. This was a prospective collection and informed consent was obtained before the administration of the questionnaire. The anonymity of the respondents was respected. The study had the approval of the ethics committee of Burkina Faso by deliberation number 2018-03-54. Data were collected in the postpartum.
Data was entered using Epi Data software and imported into Stata software for analysis. Logistic regression was conducted to assess bivariate associations between stillbirth and risk factors. Multivariable logistic regression using a bottom-up step-by-step method was employed to assess the relationship between stillbirth and risk factors; all variables with a p-value less than 0.2 during the univariate analysis were gradually included in the multivariate model. Variables with a p < 0.05 significance level in the multivariable regression were retained. The Hosmer and Lemeshow test was conducted to assess goodness of fit. The value of the area under the Receiver Operating Characteristic (ROC) curve was also used to assess the model's level of prediction. Taking into account the matching criteria of day of delivery, analyses corrected for a possible cluster effect. Odds ratio (OR) and 95% confidence intervals are reported.
3. Results
During the study period, eligibility was assessed among 4,122 deliveries. In total, data was collected on 83 cases of intrapartum stillbirth and 163 controls. Among a total of 4,122 deliveries, the reported intrapartum stillbirth rate was 20.1 per 1,000 births.
The mean age of the patients was 26.9 years. Patients under the age of 20 accounted for 19.3% (16) in the case group vs. 14% (23) in the control group.
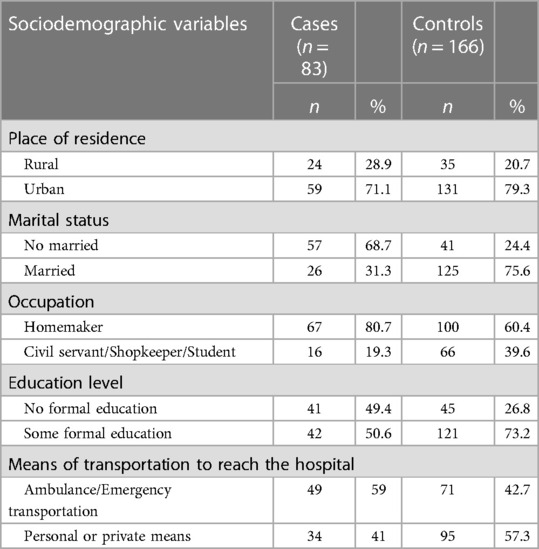
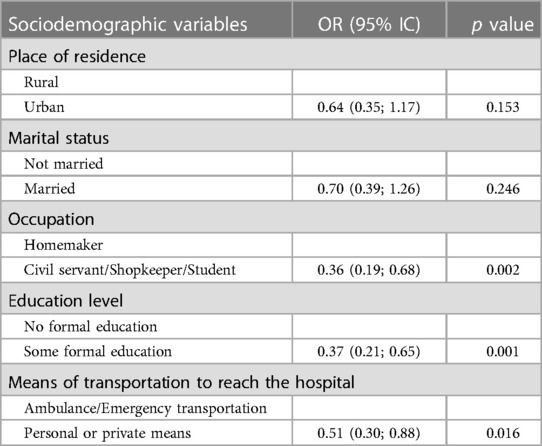
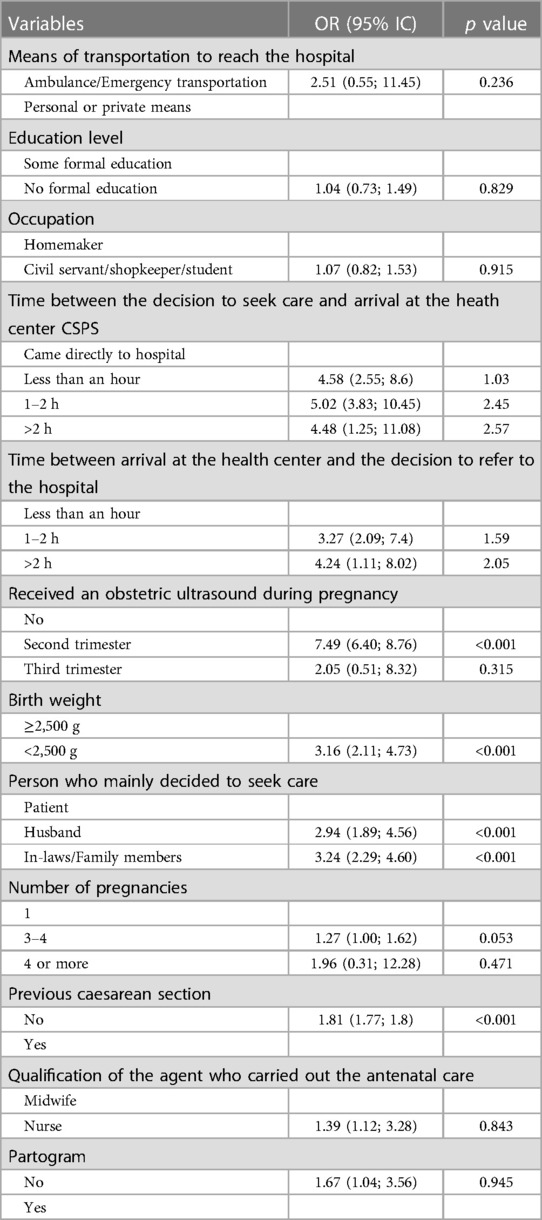
Table 1 presents the sociodemographic factors associated with intrapartum stillbirth and Table 2 with logistic regression.
There was a statistically significant association between intrapartum stillbirth and prior caesarean section (p = 0.045) and multiparity (p = 0.03). However, there was not a statistically significant association between the use of contraceptives and intrapartum stillbirth (p = 0.6). There was a statistically significant association between intrapartum fetal death and the receipt of antenatal care (ANC) by a nurse (p = 0.005) and the disuse of the partogram (p = 0.004). We did not find a significant association between the number of ANC consultations performed (p = 0.3), whether membranes were ruptured at admission (p = 0.6), the duration of labor (p = 0.6) and intrapartum fetal death.
There was a statistically significant association between fetal weight of less than 2,500 grams and intrapartum fetal death (p < 0.001). However, there was no statistically significant association between fetal presentation or position, other than the vertex presentation, and intrapartum fetal death (p = 0.47).
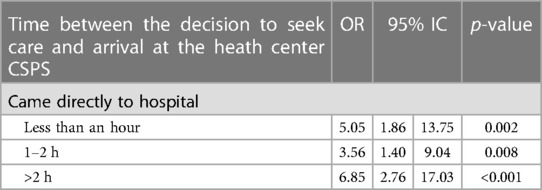
There was a statistical association between the person who decided on the consultation (in-laws/ancestors, spouse) and stillbirths (p < 0.001). Table 3 presents the association between the delay in making the decision to consult and intrapartum stillbirth.
3.1. Delay between decision to refer and arrival at YOTH
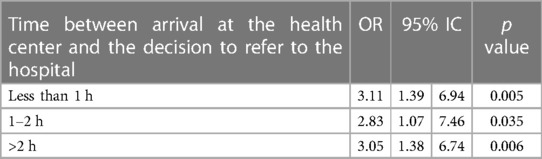
There was a statistical link between the delay in decision to refer and intrapartum stillbirth.
Table 4 presents the association between the decision-making time to refer to YOTH and intrapartum stillbirth.
3.2. Time between the arrival of the patient at hospital YOTH and the first examination
There was no statistical association between the time to first examination at hospital and intrapartum stillbirth with p = 0.8.
3.3. Factors associated with intrapartum stillbirth in multivariate analysis
Table 5 presents the multivariate analysis of intrapartum stillbirth variables.
4. Discussion
4.1. Limits and constraints of the study
The major difficulty of our study was the collection of information by interview with patients in emotional shock at the loss of the newborn.
4.2. Intrapartum stillbirth rate
The hospital intrapartum stillbirth rate was 20.1 per 1,000 births. This result is close to that of Sandjong et al. (12) in 2,009 in Cameroon who had found a rate of 18 per 1,000 births. On the other hand, it is clearly lower than that of Chigbu et al. (13) in 2009 in Nigeria who reported an intrapartum stillbirth rate of 52.1 per 1,000 births. In the United States of America, Fretts et al. (14) found an intrapartum stillbirth rate of 6.4‰ in 2005. In India, the intrapartum stillbirth rate was 16 per 1,000 births in 2014 (15). In view of these results, there is a disparity in intrapartum stillbirth rates from one country to another. The organization of care and the quality of the technical platform are explanatory elements.
4.3. Factors associated with socio-demographic characteristics
Patients under the age of 20 accounted for 19.3% (16) in the case group, a result similar to Foumane et al.'s study in Cameroon (16) and Getahun et al.'s study in Missouri (17) who found 18.9% and 19.5% of patients aged under 20, respectively, were victims of stillbirth. These findings suggest that young maternal age is a risk factor for intrapartum mortality. In fact, lack of reproductive experience is known to be associated with poor pregnancy outcomes (18, 19). Adolescents have been associated with adverse pregnancy outcomes with a decreasing risk of intrapartum stillbirth as maternal age decreases (19).
We found a predominance of intrapartum stillbirth in unmarried women similar to Foumane and colleagues (16). The intolerance of pregnancies outside of marriage in traditional African society causes these women to have hidden, unmonitored, high-risk pregnancies, and explains the maternal and fetal tragedy linked to these pregnancies. Nonetheless, marital status was not statistically related to the occurrence of intrapartum stillbirth. Wang (20) in his study also found no statistical link between marital status and stillbirth.
There was a statistically significant association between intrapartum stillbirth and patients with no financial income and no schooling. Lack of regular income and low level of education were identified as risk factors for intrapartum stillbirth by Foumane et al. in Cameroon. The poor are most at risk and have the lowest coverage of skilled birth care (1). Improving the socio-economic and educational status of women in developing countries could be a strategy to reduce the intrapartum stillbirth rate.
On univariate and multivariate analysis, there is a statistical link between intrapartum stillbirth and the decision to consult was either made by the spouse or the in-laws. Indeed, in a traditional African society woman have limited agency and decision-making power, especially within family dynamics. This can lead to a delay in the consultation.
4.4. Factors associated with clinical data
There was a statistical association (univariate analysis) between being referred and intrapartum stillbirth with a p = 0.016 with an OR of 0.51 (0.30; 0.88): patients that were referred for care at hospital were 3 times as likely to have intrapartum stillbirth. In multivariate analysis no statistical link was found (p = 0.236). This result corroborates that of Sandjong et al. in Cameroon (8). where the risk of stillbirth was high when the patient is referred by another health facility; [OR = 4.81, 95% CI (2.39–9.91); p < 0.001]. In Burkina Faso the problem lies in the inadequate evacuation conditions. Patients are referred when the conditions of the mother or the fetus are critical. Even more serious is the fact that the shortage of certain consumables in free care contributes to delaying the treatment of patients.
Antenatal consultations (ANC) were mainly carried out by midwives or gynecologists. The odds of intrapartum stillbirth was statistically significant when ANC consultations were performed by other health workers with p = 0.005 OR of 4.86 with a CI (1.63–14.50): patients who had ANC consultations were performed by other agents were four times as likely to have an intrapartum stillbirth. ANC consultations should be carried out by agents trained to meet the objectives. The unavailability of midwives at all times in peripheral health facilities could explain why ANC consultations are carried out by other agents (nurses, itinerant health agents).
There was a statistically significant association between patient's lack of obstetric ultrasound during pregnancy and intrapartum stillbirth (OR: 7.49; CI: 6.40, 8.76). Obstetric ultrasounds are a key intervention which can detect pregnancy complications and determining the prognosis for childbirth. Sandjong et al. have shown that a single ultrasound performed between the 28th and 32nd week of gestation would reduce intrapartum stillbirth (12).
4.5. Factors associated with delays
Bivariate analyses determined a statistical association between the delay in the decision to seek care at a health center and intrapartum stillbirth. Similarly, there was a statistical association between intrapartum stillbirth and delayed referral to hospital (greater than 2 h). On the other hand, we did not find a statistical association but this link disappears in the multivariate analysis. Chigbu et al.'s study in Nigeria found that all delays were associated with intrapartum stillbirth in both univariate and multivariate analysis (13).
5. Conclusion
The intrapartum stillbirth rate in our study remains high. Factors such as referral from a health facility, no obstetric ultrasound during pregnancy, low neonatal birth weight, and delay in decision-making to seek care were significantly associated with intrapartum stillbirth. Regular and effective follow-up of all pregnant women is essential through quality ANC and active labor and delivery monitoring using a partograph. Specific actions are necessary to enable rapid recognition of the risk factors for intrapartum stillbirth and to ensure rapid and effective management.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the authorization of the ethics committee of the Yalgado Ouédraogo hospital has been obtained. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author contributions
BEK and HZ prepared the manuscript, MT collected the data, AC analyzed the data, SRS and BT provided a useful review of this manuscript. All authors contributed to the article and approved the submitted version.
Acknowledgments
The authors would like to thank all patients for their consent obtained. The authors also thank all the staff who contributed to the care of the patients. They would also like to thank Meighan Mary for her contributions to the writing in English.
Conflict of interest
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. The handling editor EAKJ declared a past co-authorship with the author BEK.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ANC, antenatal care; OR, odds ratio; ROC, receiver operating characteristic.
References
1. Liu LC, Wang YC, Yu MH, Su HY. Major risk factors for stillbirth in different trimesters of pregnancy—a systematic review. Taiwan J Obstet Gynecol. (2014) 53(2):141–5. doi: 10.1016/j.tjog.2014.04.003
2. Craig ED, Stewart AW, Mitchell EA. Causes of late fetal death in New Zealand 1980-1999. Aust N Z J Obstet Gynaecol. (2004) 44(5):441–8. doi: 10.1111/j.1479-828X.2004.00284.x
3. WHO. Neonatal and Perinatal Mortality: Country, Regional and Global Estimates (2006) World Health Organization: Geneva, Switzerland. pp.14. Available at: https://apps.who.int/iris/handle/10665/43444 (Accessed July 9, 2022).
4. McCaw-Binns A, Greenwood R, Ashley D, Golding J. Antenatal and perinatal care in Jamaica: do they reduce perinatal death rates? Paediatr Perinat Epidemiol. (1994) 8(s1):86–97. doi: 10.1111/j.1365-3016.1994.tb00493.x
5. Darmstadt GL, Yakoob M, Haws RA, Menezes EV, Soomro T, Bhutta ZA. Reducing stillbirths: interventions during labour. BMC Pregnancy Childbirth. (2009) 9(Suppl 1):S6. doi: 10.1186/1471-2393-9-S1-S6
6. Künzel W, Herrero J, Onwuhafua P, Staub T, Hornung C. Maternal and perinatal health in Mali, Togo and Nigeria. Eur J Obstet Gynecol Reprod Biol. (1996) 69(1):11–7. doi: 10.1016/0301-2115(95)02528-6
7. Millogo T, Ouédraogo GH, Baguiya A, Meda IB, Kouanda S, Sondo B. Factors associated with fresh stillbirths: a hospital-based, matched, case-control study in Burkina Faso. Int J Gynaecol Obstet. (2016) 135(S1):S98–102. doi: 10.1016/j.ijgo.2016.08.012
8. Kiondo P, Nakimuli A, Ononge S, Wandabwa JN, Musaba MW. Predictors of intrapartum stillbirths among women delivering at Mulago Hospital, Kampala, Uganda. Int J MCH AIDS. (2021) 10(2):156–65. doi: 10.21106/ijma.409
9. Maaløe N, Housseine N, Bygbjerg IC, Meguid T, Khamis RS, Mohamed AG, et al. Stillbirths and quality of care during labour at the low resource referral hospital of Zanzibar: a case-control study. BMC Pregnancy Childbirth. (2016) 16(1):351. doi: 10.1186/s12884-016-1142-2
10. Lawn JE, Blencowe H, Waiswa P, Amouzou A, Mathers C, Hogan D, et al. Stillbirths: rates, risk factors, and acceleration towards 2030. Lancet. (2016) 387(10018):587–603. doi: 10.1016/S0140-6736(15)00837-5
11. Ministère de la santé. Annuaire Statistique 2018. (2019) Available at: http://cns.bf/IMG/pdf/annuaire_ms_2018.pdf (Accessed February 24, 2021).
12. Sandjong TID, Tebeu PM, Mbu RE, Mboudou E, Guegang GE, Nkwabong E, et al. Mort fœtale intrapartum au Cameroun: une analyse de deux hôpitaux de référence de yaoundé, cameroun. Clin Mother Child Health. (2009) 6(2):1123–7.
13. Chigbu CO, Okezie OA, Odugu BU. Intrapartum stillbirth in a Nigerian tertiary hospital setting. Int J Gynaecol Obstet. (2009) 104(1):18–21. doi: 10.1016/j.ijgo.2008.08.011
14. Fretts RC. Etiology and prevention of stillbirth. Am J Obstet Gynecol. (2005) 193(6):1923–35. doi: 10.1016/j.ajog.2005.03.074
15. Newtonraj A, Kaur M, Gupta M, Kumar R. Level, causes, and risk factors of stillbirth: a population-based case control study from Chandigarh, India. BMC Pregnancy Childbirth. (2017) 17(1):371. doi: 10.1186/s12884-017-1557-4
16. Foumane P, Mounton AC, Sama JD, Nguefack S, Pisoh WD, Mboudou ET. Risk factors of intrapartal fetal death in a low-resource setting. Open J Obstet Gynecol. (2014) 4(101):4–15. doi: 10.4236/ojog.2014.43018
17. Getahun D, Ananth CV, Kinzler WL. Risk factors for antepartum and intrapartum stillbirth: a population-based study. Am J Obstet Gynecol. (2007) 196(6):499–507. doi: 10.1016/j.ajog.2006.09.017
18. Walsh CA, McMenamin MB, Foley ME, Daly SF, Robson MS, Geary MP. Trends in intrapartum fetal death, 1979-2003. Am J Obstet Gynecol. (2008) 198(1):47.e1-47. doi: 10.1016/j.ajog.2007.06.018
19. Wilson RE, Alio AP, Kirby RS, Salihu HM. Young maternal age and risk of intrapartum stillbirth. Arch Gynecol Obstet. (2008) 278(3):231–6. doi: 10.1007/s00404-007-0557-4
Keywords: stillbirths, risk factors, intrapartum, hospital, Burkina Faso
Citation: Komboigo BE, Zamane H, Coulibaly A, Sib SR, Thiombiano M and Thieba B (2023) Factors associated with intrapartum stillbirth in a tertiary teaching hospital in Burkina Faso. Front. Glob. Womens Health 4:1038817. doi: 10.3389/fgwh.2023.1038817
Received: 7 September 2022; Accepted: 20 March 2023;
Published: 3 April 2023.
Edited by:
Ermel Ameswué Kpogbé Johnson, Yackoley Institute, Burkina FasoReviewed by:
Mikaila Kabore, Regional Hospital of Ziniaré, Burkina FasoHadiza Mudi, Aliko Dangote College of Nursing Sciences Bauchi State Nigeria, Nigeria
Drucilla Jane Roberts, Massachusetts General Hospital and Harvard Medical School, United States
© 2023 Komboigo, Zamane, Coulibaly, Sib, Thiombiano and Thieba. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Komboigo Bewendin Evelyne ZXZlbHluZWtvbWJvaWdvQHlhaG9vLmZy
Specialty Section: This article was submitted to Maternal Health, a section of the journal Frontiers in Global Women's Health
 Bewendin Evelyne Komboigo
Bewendin Evelyne Komboigo Hyacinthe Zamane3,4
Hyacinthe Zamane3,4