- 1Harar Health Science College, Harar, Ethiopia
- 2School of Nursing and Midwifery, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
Background: Obstetric emergencies are life-threatening medical problems that develop during pregnancy, labor, or delivery. There are a number of pregnancy-related illnesses and disorders that can endanger both the mother's and the child's health. During active labor and after delivery, obstetrical crises can arise (postpartum). While the vast majority of pregnancies and births proceed without a hitch, all pregnancies are not without risk. Pregnancy can bring joy and excitement, but it can also bring anxiety and concern. Preterm birth, stillbirth, and low birth weight are all adverse pregnancy outcomes, leading causes of infant illness, mortality, and long-term physical and psychological disorders.
Purpose: The purpose of this study is to assess the magnitude and association of obstetric emergencies and adverse maternal-perinatal outcomes in Ethiopia.
Method: We used four databases to locate the article: PUBMED, HINARI, SCIENCE DIRECT, and Google Scholar. Afterward, a search of the reference lists of the identified studies was done to retrieve additional articles. For this review, the PEO (population, exposure, and outcomes) search strategy was used. Population: women who had obstetric emergencies in Ethiopia. Exposure: predictors of obstetric emergencies. Outcome: Women who had an adverse perinatal outcome. Ethiopian women were the object of interest. The primary outcome was the prevalence of adverse maternal and perinatal outcomes among Ethiopian women. Obstetrical emergencies are life-threatening obstetrical conditions that occur during pregnancy or during or after labor and delivery. The Joanna Briggs Institute quality assessment tool was used to critically appraise the methodological quality of studies. Two authors abstracted the data by study year, study design, sample size, data collection method, and study outcome. Individual studies were synthesized using comprehensive meta-analysis software and STATA version 16. Statistical heterogeneity was checked using the Cochran Q test, and its level was quantified using the I2 statistics. Summary statistics (pooled effect sizes) in an odd ratio with 95% confidence intervals were calculated.
Result: A total of 35 studies were used for determining the pooled prevalence of adverse maternal and perinatal outcomes; twenty-seven were included in determining the odd with 95% CI in the meta-analysis, from which 14 were cross-sectional, nine were unmatched case-control studies, and 14 were conducted in the south nation and nationality Peoples' Region, and eight were from Amhara regional states, including 40,139 women who had an obstetric emergency. The magnitude of adverse maternal and perinatal outcomes following obstetric emergencies in Ethiopia was 15.9 and 37.1%, respectively. The adverse maternal outcome increased by 95% in women having obstetric emergencies (OR 2.29,95% CI 2.43–3.52), and perinatal deaths also increased by 95% in women having obstetric emergencies (OR 3.84,95% CI 3.03–4.65) as compared with normotensive women.
Conclusion: This review demonstrated the high prevalence of perinatal mortality among pregnant women with one of the obstetric emergencies in Ethiopia. Adverse maternal and perinatal outcomes following obstetric emergencies such as ICU admission, development of PPH, giving birth via CS, maternal death, NICU admission, LBW, and perinatal death were commonly reported in this study.
Introduction
Obstetric emergencies are life-threatening medical problems that develop during pregnancy, labor, or delivery. There are a number of pregnancy-related illnesses and disorders that can endanger both the mother's and the child's health. Obstetrical emergencies may also occur during active labor and after delivery (postpartum) (1).
While the vast majority of pregnancies and births proceed without a hitch, all pregnancies are not without risk. Pregnancy can be a time of happiness and anticipation, but it can also be a period of anxiety and concern (2).
For a smooth transition from life in the womb to life outside the womb, a delicate balance between the mother's health, the course of the pregnancy, the delivery method, and early postoperative care is essential. Pregnancy and the neonatal period significantly impact maternal and child survival outcomes (3).
Adverse pregnancy outcomes are those pregnancy outcomes other than normal live birth, which mostly include preterm birth, stillbirth, and low birth weight, which are the major causes of neonatal morbidity, mortality, and long-term physical and psychological problems (4).
In both developing and developed countries, adverse birth outcomes such as prematurity, low birth weight, and stillbirth are major issues. Around 15 million babies are born prematurely worldwide, accounting for more than one in every ten births. More than one million newborns die soon after birth, and countless others are left with lifelong physical, neurological, or educational problems, frequently at a high cost to families and societies. Moreover, women also die as a result of complications during and after pregnancy and childbirth (5).
The majority of these problems emerge during pregnancy and can be avoided or treated. Other problems may be present before pregnancy, but they will increase during the pregnancy if they are not treated as part of the woman's therapy. Severe bleeding (typically after childbirth), infections (usually after childbirth), high blood pressure throughout pregnancy (pre-eclampsia and eclampsia), complications following delivery, and unsafe abortion are the leading causes of maternal death (6). As a result, the purpose of this study is to determine the magnitude of adverse maternal and perinatal outcomes following an obstetric emergency, as well as to describe the relationship between an obstetric emergency and adverse maternal-perinatal outcomes in women who have obstetric emergencies during pregnancy or labor.
Methods
The review flow was based on the established Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guidelines.
Inclusion criteria
The participants in this study were pregnant mothers who had an obstetric emergency and had a poor maternal-perinatal outcome. The studies were published in English from January 2010 to March 2022.
All published and unpublished observational (cross-sectional, case-control, prospective, and retrospective cohort studies) studies conducted in Ethiopia were included in this search.
Pregnant women who had obstetric emergencies were the study subjects, and the consequence was a negative maternal-perinatal outcome.
Data source, study selection, and search strategy
We used four databases to locate the article: PUBMED, HINARI, SCIENCE DIRECT, and Google Scholar. Onwards, a search of the reference lists of the identified studies was done to retrieve additional articles. For this review, the PEO (population, exposure, and outcomes) search strategy was used. Population: women who had obstetric emergencies in Ethiopia. Exposure: predictors of an obstetric emergency. Outcome: women who had adverse perinatal outcomes. Ethiopian women were the object of interest. The primary outcome was the prevalence of adverse maternal and perinatal outcomes among Ethiopian women. Obstetrical emergencies are life-threatening conditions that occur during pregnancy or after labor (7).
The secondary outcomes were: the predictors of obstetric emergencies such as maternal age, place of residence, ANC visit, gravidity, etc. For each selected PEO component, the electronic databases were searched using keywords and the medical subject heading [MeSH] terms. The keyword was “emergency obstetric OR PIH OR APH OR obstructed labor OR premature rupture of membranes (PROM) OR prolapsed umbilical cord OR placenta accreta OR rupture of the uterus OR amniotic fluid embolism AND adverse maternal outcomes OR ICU admission OR PPH OR hysterectomy OR distractive delivery OR CS OR long hospital stay OR blood transfusion OR maternal death OR adverse perinatal outcomes OR NICU admission OR birth asphyxia OR low APGAR score OR low birth weight OR premature birth OR RDS OR long hospital stay OR stillbirth OR neonatal death.” To address unpublished literature, the searches include literature from Google and Google scholar. The search was limited to papers published in English from January 2010 to March 2022 in Ethiopia.
Study selection
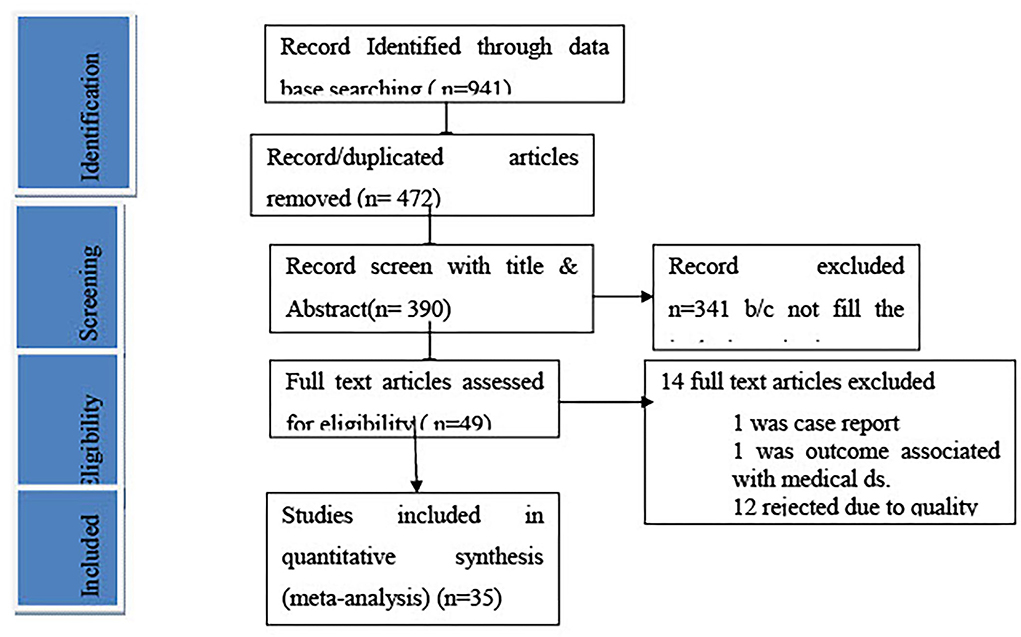
We include all observational studies published in English that show the relationship between obstetric emergencies and adverse maternal or perinatal outcomes, which were done in primary, general, or referral facilities, by excluding community-based studies, case series, and case report studies. The studies conducted outside of Ethiopia do not consider the WHO definition of an obstetric emergency. Studies on adverse outcomes with medical diseases and studies describe neither maternal nor perinatal outcomes. Thirty-two studies were finally identified, and the detailed data searching strategy was presented in the PRISMA flowchart (Figure 1).
Study selection procedure: Screening
In two phases, two authors (M.L. and N.A.) independently assessed the eligibility of chosen studies. To determine eligibility for the second step, which comprises full-text screening, the titles and abstracts of the retrieved literature were first assessed. During this phase, the authors conducted additional screening to determine whether or not the participants were eligible to participate in the study. Disagreements between the two reviewers were resolved by a conversation with the third review author and/or by consensus (M.T).
Data collection process
The data were retrieved from the eligible studies by the first review author (M.L.), which were then kept on a data extraction sheet and reviewed by the second review author (N.A.). Disagreements between the two reviewers were settled through conversation; otherwise, the third review author (M.T.) made the final decision. Based on the authors' names, sample size, outcomes, and study location, the studies were examined for duplication. Data were extracted from the year of the study, the region in which it was conducted, the study design, the type of obstetric emergency, the sample size, and the extent of the unfavorable outcome. During data extraction, adverse maternal outcomes (destructive delivery, CS, extended hospital stay, and maternal mortality) are classified as maternal outcomes. In contrast, perinatal outcomes (stillbirth, NICU admission, sepsis, and low birth weight) are classified as perinatal outcomes.
Assessment of methodological quality
The authors independently assessed all included studies for methodological validity using the JBI (Joanna Briggs Institute). The inclusion criteria, the randomness of participant selection, identification of research participants, the precision of measurement of outcomes of interest, use of proper statistical analysis methods, and documentation of sources of bias or confounding were all given special attention.
Statistical analysis
Using studies that reported pregnancy outcomes, an unadjusted odds ratio (OR) with a 95% confidence interval (CI) was calculated using both STATA version 16 (for adverse perinatal outcome) and comprehensive meta-analysis version 2 package (for adverse maternal outcome). In addition to the overall pooled prevalence of perinatal death, subgroup and sensitivity analyses were also performed. Considering the “synthesis of results,” the raw proportion was transformed into a suitable unit for meta-analysis using the logit transformation. To produce an overall summary estimate of the prevalence across studies and pooled study-specific estimates, a random effects model was employed to account for probable heterogeneity between studies, which defaults to the fixed effects model method in the absence of heterogeneity (8). The meta-analysis results were graphically shown using forest plots. The Chi2 test (Cochran Q test) was used to examine for statistical heterogeneity with a p-value of 0.05. The I2 statistic/s were used to determine the degree of heterogeneity among the studies, with an I2 value of <50% implying substantial heterogeneity. An obstetric emergency can be considered an exposure throughout the study, while unfavorable maternal and perinatal outcomes can be considered an outcome.
Risk of bias across studies
The study assessed the possibility of publication bias using Egger's linear regression test as a formal statistical test for publication bias (9). The Egger's test resulted in a P-value of <0.10, indicating statistically significant publication bias.
Additional analyses
Subgroup analysis was carried out based on publication year, study design, and Ethiopian regions. Furthermore, the sensitivity analysis investigated the extent to which modifications in the techniques or data utilized in specific studies influenced the overall findings of a review. The outliers and inliers were also considered in the sensitivity analysis.
Results
Description of the studies
We found 941 studies through searching the electronic medical database and other essential sources. Of those identified studies, 472 articles were removed due to duplication, and the remaining 390 articles screened by topic and abstract of these 341 studies were excluded because the content in the title and abstract did not match with the recent study. The remaining 49 full-text studies were reviewed to assess eligibility, and 14 studies were excluded due to duplication, an inconsistent study outcome, and a different study population from our study. The last 35 studies were critically appraised, and the studies that got higher scores were included in the study: 14 cross-sectional, nine unmatched case-control, five retrospective, five case-control, and two prospective cohorts.
Almost all studies adjusted for confounding variables, such as adverse outcomes resulting from other than obstetric emergencies and twin pregnancies.
Study characteristics
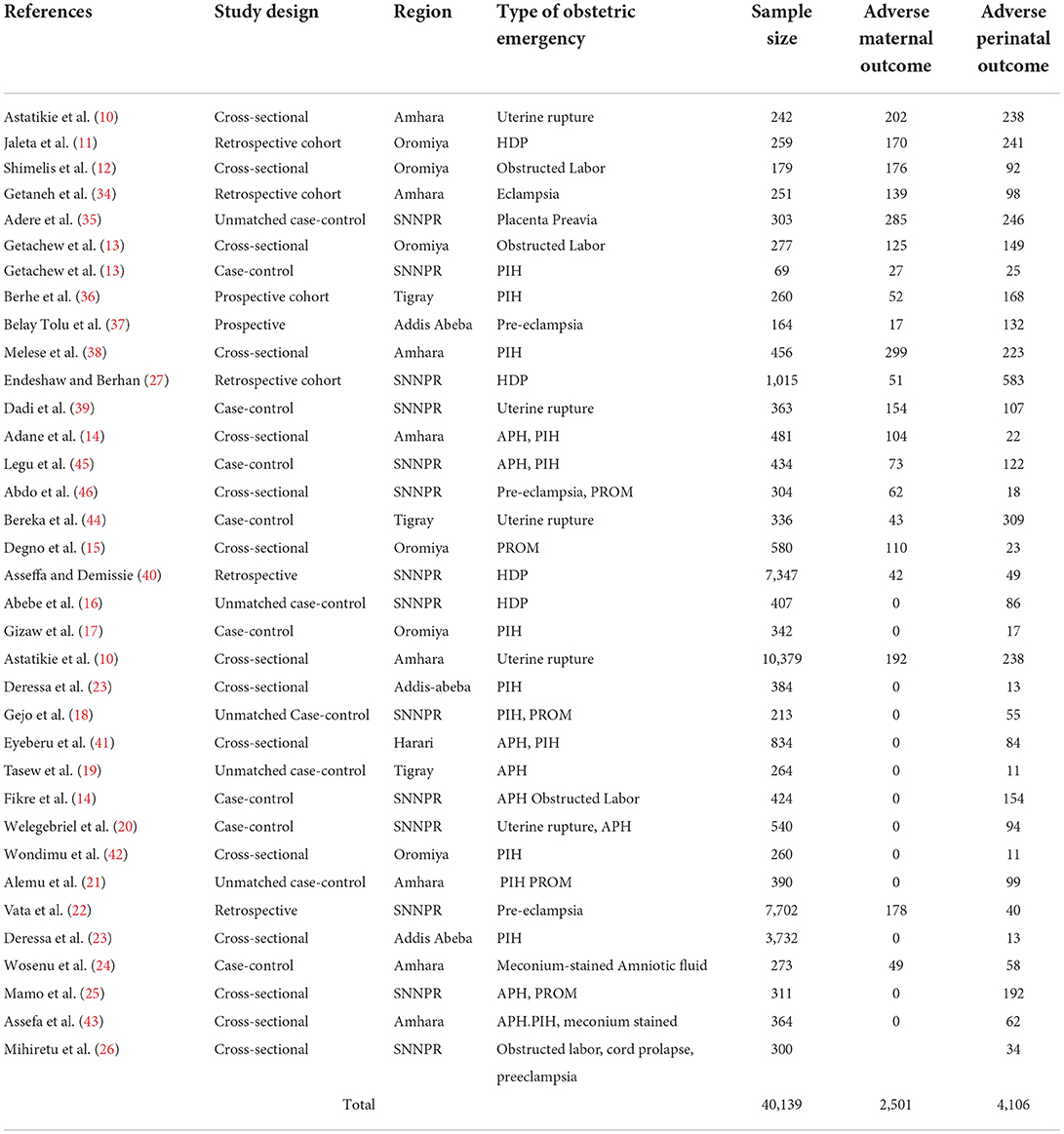
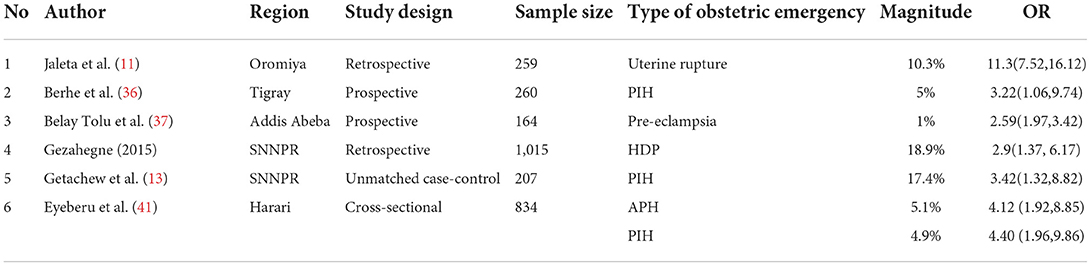
The characteristics of the cross-sectional [1,024] prospective or retrospective cohort [2,531] and case-control studies [3,244] included in this review from 6 regional states of Ethiopia are summarized in Table 1. The majority of studies were conducted in SNNPR, Amhara, and Oromiya regional states, which are 14, 8, and 6, respectively.
The sample size of the studies ranged from 69 in SNNPR to 10,379 in Amhara regional state, 38 with a total of 40,139 participants. Overall, 2,501 pregnant women and 4,106 infants were recorded as suffering from disorders due to obstetric emergencies during the antepartum and/or intrapartum and/or postpartum period.
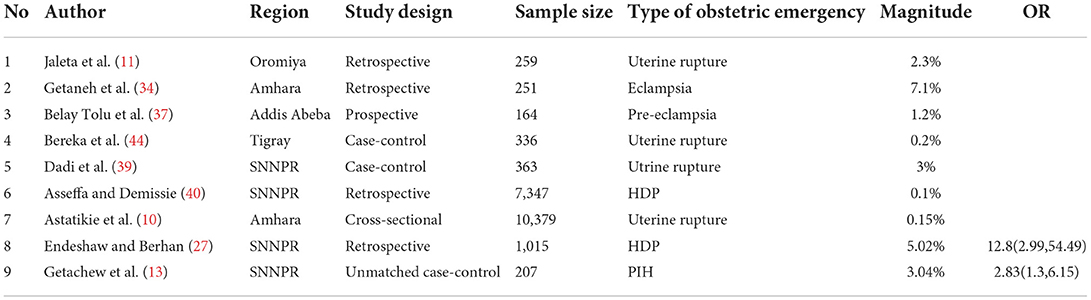
Association between obstetric emergencies and adverse maternal outcome
Sixteen studies have reported a significant relationship between the exposure variable and the intended outcome, and the magnitude of maternal mortality ranges from 0.1 to 8%. From these, two studies described the association between obstetric emergencies and maternal death. 12.8 (2.99, 54.49) (27) and 2.83 (1.3, 6.15) (13). According to the reviewed studies, maternal mortality is 3–13 times more prevalent in women having obstetric emergencies than in normotensive women (Table 2).
Association between obstetric emergencies and adverse perinatal outcome
Twenty-two studies have reported a significant relationship between obstetric emergencies and adverse perinatal outcomes. Of those studies, 11 showed the association of obstetric emergency with adverse outcomes of stillbirth, six studies with EOND, five studies with NICU admission, seven studies with preterm birth, and two with perinatal deaths. Six studies indicated the occurrence of EOND in relation to obstetric emergencies.
According to reviewed studies, the magnitude of EOND ranges from 0.2 to 19%. The risk of EOND is 1.5–12 times more likely to occur in women having obstetric emergencies than in normotensive women. Eleven studies also examined the onset of stillbirth with maternal obstetric complications. The magnitude of stillbirth ranged from 0.027 to 81% in women with obstetric emergency problems. The risk of stillbirth is 2.35–24 times more likely to occur in women with obstetric emergency problems than in normotensive women. In addition to this, seven studies indicated that the association of preterm birth with obstetric emergencies and the magnitude of preterm birth in Ethiopia ranged from 3.2 to 50% in women having obstetric complications, as well as the risk of preterm birth was increased by 0.182–40% in women having obstetric complications than normotensive women. Nevertheless, five studies were reviewed and showed a significant association between obstetric emergencies and the rate of NICU admission. The magnitude of NICU admission is 0.2–31 times higher in neonates delivered from mothers having obstetric emergency problems, and the risk of being admitted to NICU is 2–34 times higher in neonates born from mothers with obstetric complications.
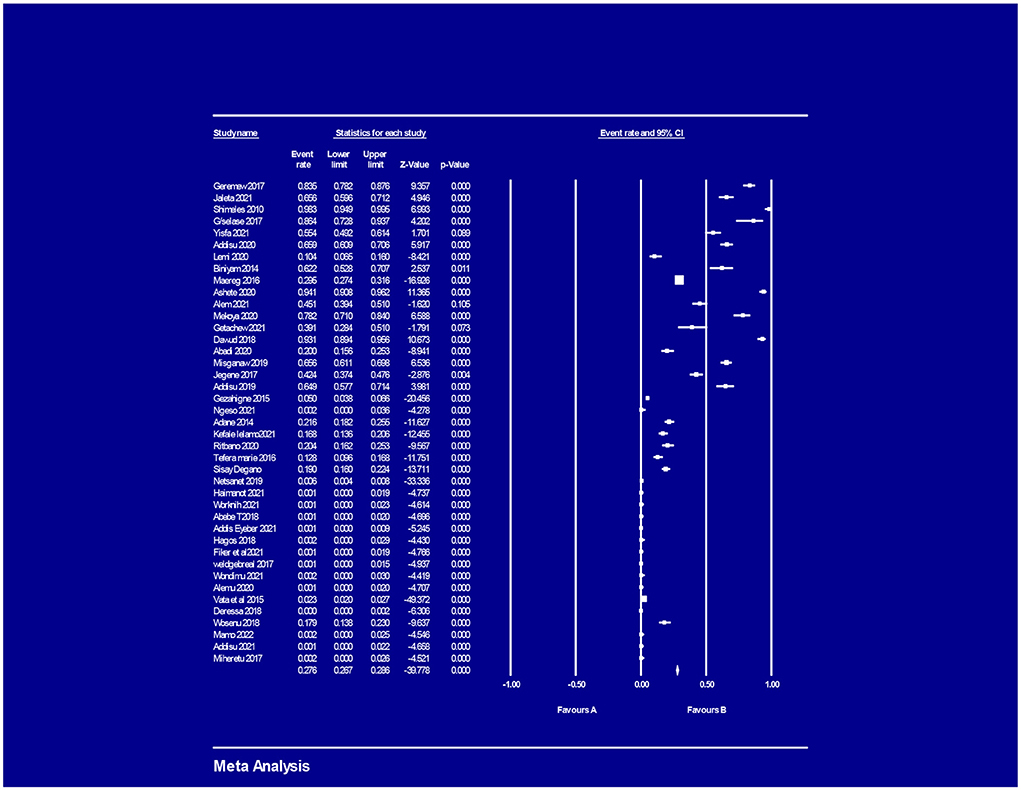
The magnitude of adverse maternal and perinatal outcome
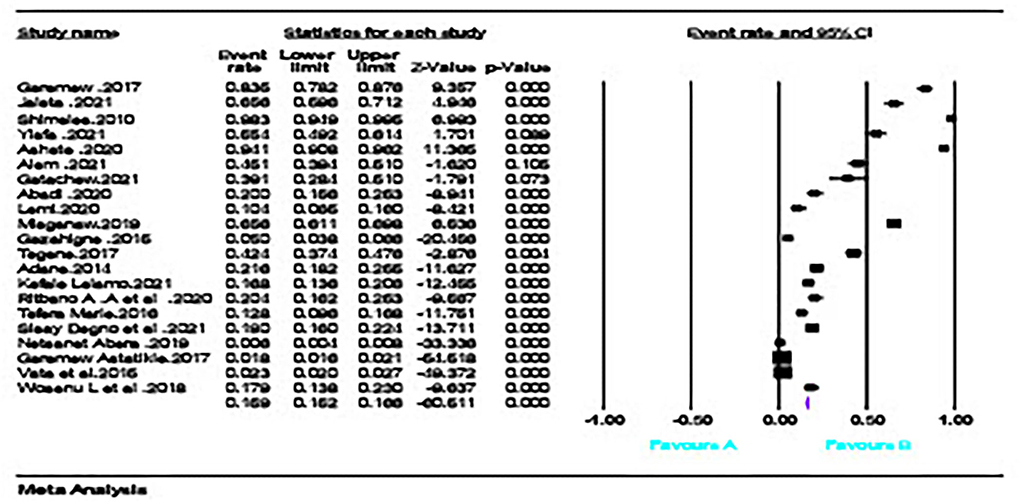
The pooled prevalence of adverse maternal outcomes following obstetric emergencies in Ethiopia was 15.9% (95% CI = [0.152, 0.166]); (Figure 2), whereas the pooled prevalence of adverse perinatal outcomes following obstetric emergencies in Ethiopia was 37.1% (95% CI = [0.362, 0.381]) (Figure 3).
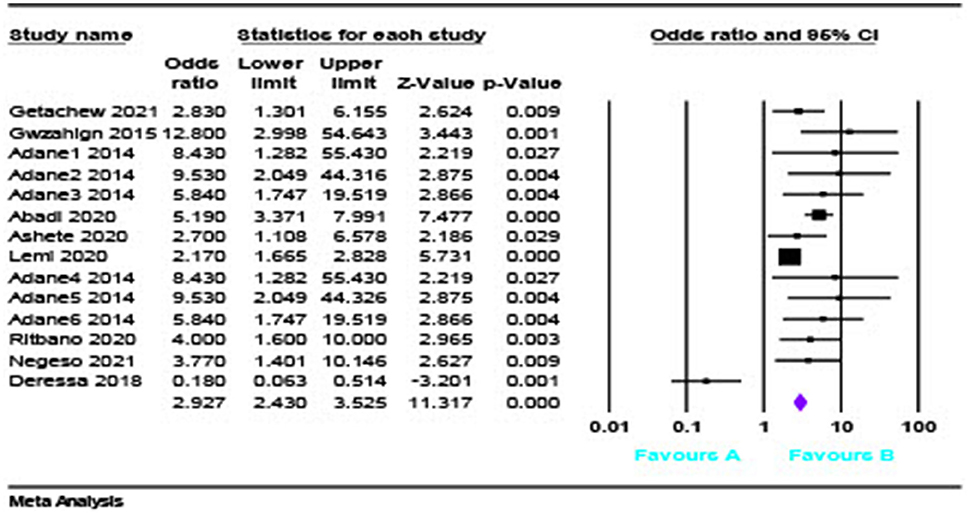
Obstetric emergencies and adverse maternal outcomes
The pooled analysis showed that the risk of adverse maternal outcome was 2.92 times OR = 2.927(95% CI = [2.43, 3.52]) (Figure 4) more likely to occur in women having obstetric emergencies than normotensive women.
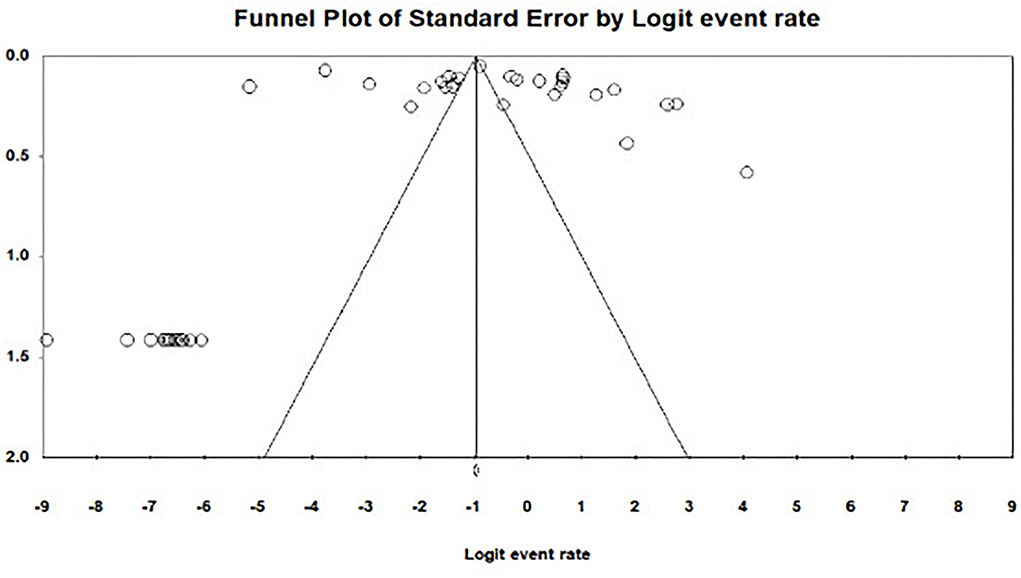
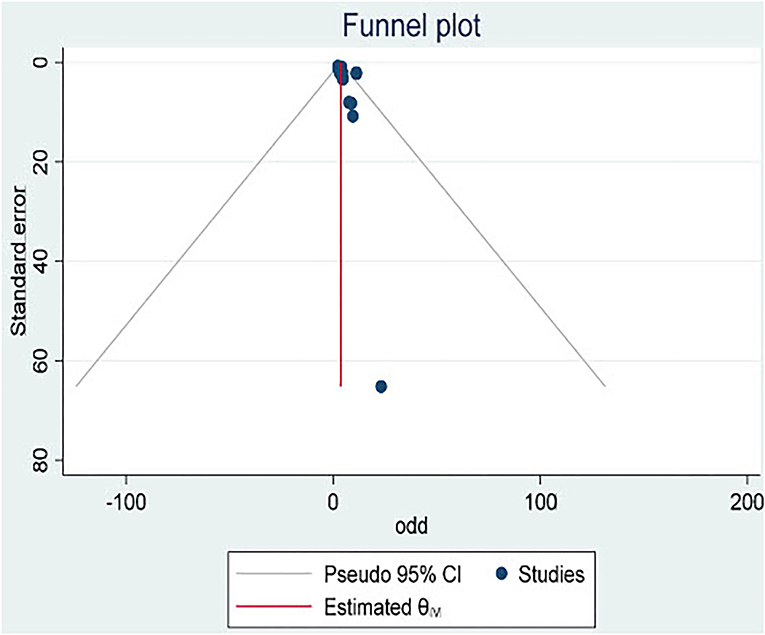
Publication bias
There was evidence of publication bias across studies reporting on adverse maternal outcomes following obstetric emergencies. Egger's test for bias gave a p-value of 0.41 and a funnel plot of asymmetry in shape (Figure 5).
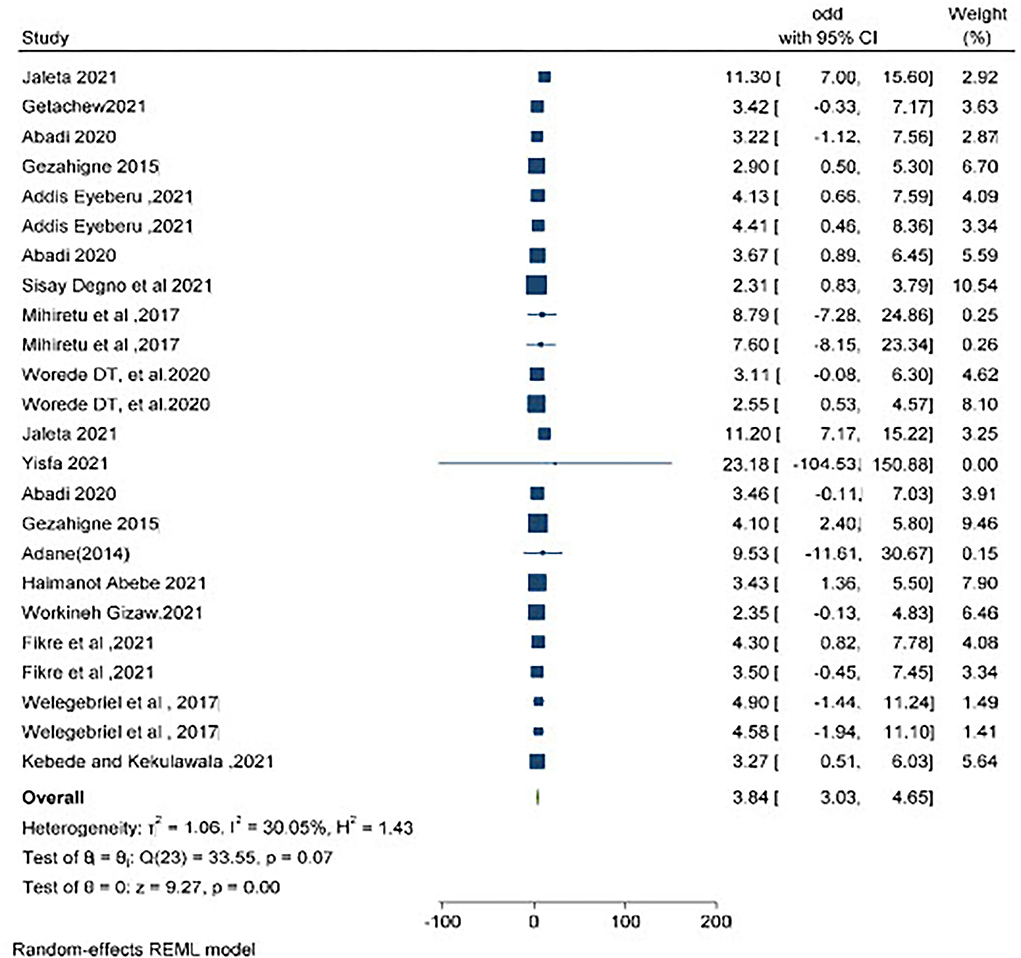
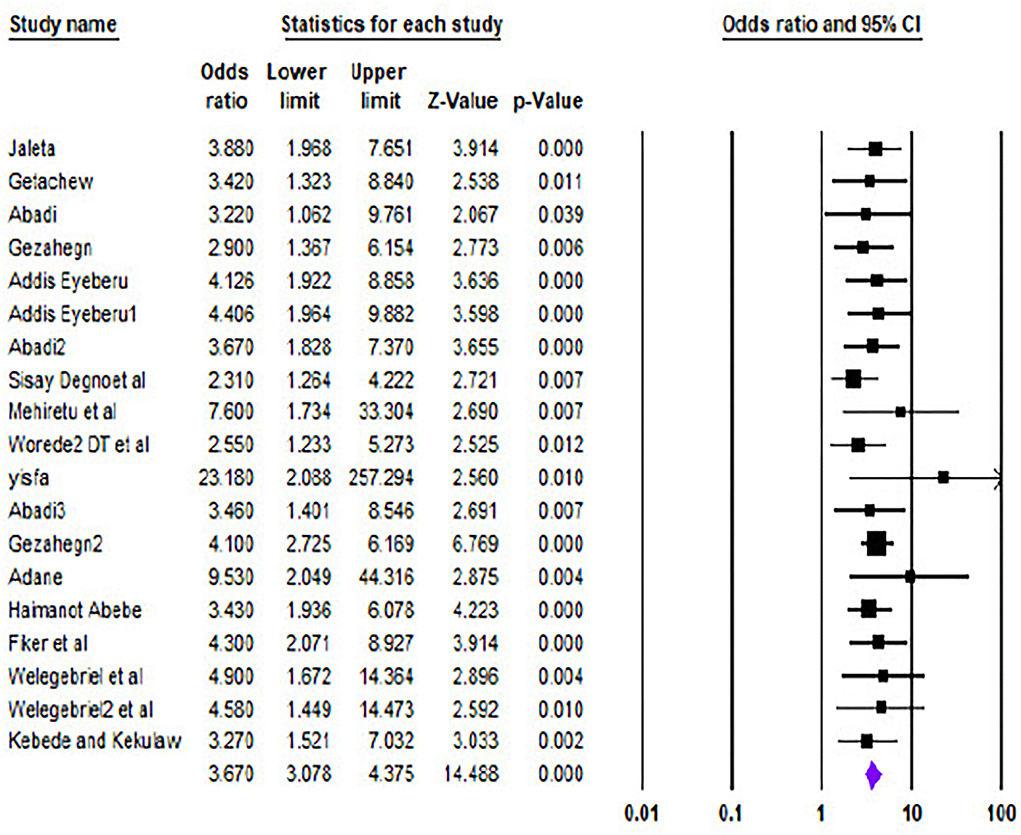
Obstetric emergencies and perinatal deaths
Twelve studies described the association between obstetric emergencies and perinatal deaths. The pooled analysis showed both soft wares (i.e., STATA and CMA) (Figures 6, 7, respectively) that the likelihood of perinatal death was significantly increased by 3.84 (OR = 3.84, 95% CI 3.03–4.65) I2 = 30.05% p = 0.07) and 3.67 (OR = 3.67.95% CI 3.078–4.375) times more in a mother having obstetric emergencies than normotensive women, respectively.
Publication bias
There was evidence of publication bias across studies reporting on the occurrence of perinatal death following an obstetric emergency, with Egger's test for bias giving a p-value of 0.014 and the asymmetry shape of the funnel plot (Figure 8).
Sensitive analysis
Sensitivity analysis was done by removing outliers and inliers, and no significant difference was investigated. While removing outliers, we noticed that the pooled analysis revealed OR 3.69 (95% CI 3.08–4.42), and after removing inliers, the pooled analysis was OR 3.67 (95% CI 3.07–4.40), so we can say this meta-analysis result is not sensitive.
Subgroup analysis
Subgroup analysis of perinatal death by design, region, and publication year revealed little heterogeneity (I2 = 57.41 and 20.15% based on areas) and substantial homogeneity (I2 = 0.00% based on publication year and study design)across the studies in terms of risk of perinatal death.
Subgroup analysis of prenatal death prevalence by region across Ethiopia showed a significantly higher pooled prevalence in Amhara regional state (5.89%; 95% CI = [1.64, 21.18]) and Harari regional state (4.25%; 95% CI = [2.44, 7.41] (Table 3). The subgroup analysis by study design also revealed a high pooled prevalence in retrospective study (3.92%, 95% CI = [2.86, 5.38] as well as cross-sectional (3.64%, 95% CI = [2.48, 5.33] study designs (Table 4). Subgroup analysis of prenatal death prevalence by publication year showed a significantly higher pooled prevalence than a study conducted in 2014 (9.53%; 95% CI = [2.04, 44.31]) and 2017 (5.26%; 95% CI = [2.63, 10.54]) (Table 5).
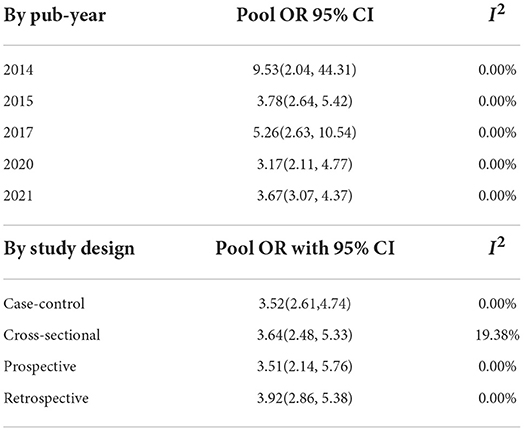
Table 3. Sub group analysis of obstetrics emergency based on publication year of studies in Ethiopia from 2010 to 2022.
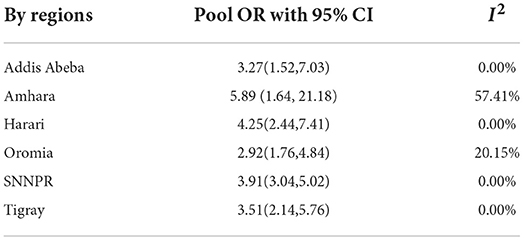
Table 5. Sub-group analysis of obstetrics emergency based on region of studies in Ethiopia from 2010 to 2022.
The meta-regression indicates that the number of publications on obstetric emergencies is on the rise, which shows that perinatal death following obstetric emergencies is currently receiving attention (Figure 7). Our finding indicated that every unit increment of obstetric emergencies leads to the risk of perinatal death also increasing by a unit (Figure 8).
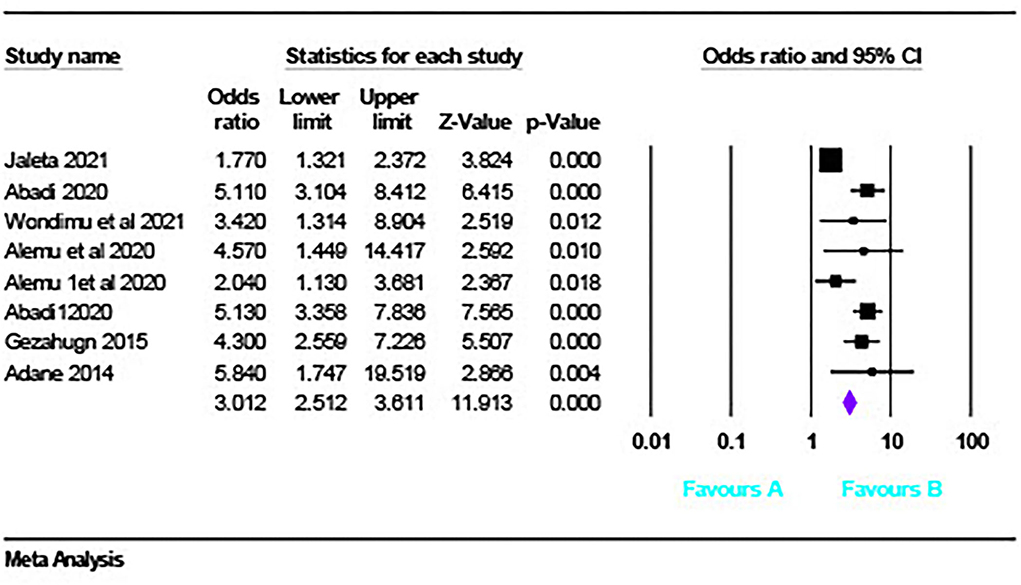
Obstetric emergencies and adverse perinatal outcomes
Six studies described the association between obstetric emergencies and adverse perinatal outcomes (LBW, NICU admission). The pooled analysis showed that the risk of adverse perinatal outcome was three times (OR = 3.012, 95% CI [2.51 – 3.61] p < 0.001, I2 = 75.24%) (Figure 9) more likely to occur in women having obstetric emergencies than normotensive women.
Discussion
Our findings demonstrated that women with obstetrical difficulties had higher maternal and perinatal morbidity and mortality, which is consistent with a study conducted in Sub-Saharan African nations but slightly higher than a survey conducted in China and the WHO multi-country prevalence. This could be attributed to poor health-seeking behavior, as women are more likely to present late and with severe diseases. This study's preterm birth rate was comparable to that of a study conducted in Sub-Saharan African countries (44%). Our findings suggested that the risk of neonatal death was higher than that suggested by Latin American adverse outcome research following Vasa-preavia (1.19–2.05%), which could be attributed to the fact that in our nation, the three delays contributed to 40% of bad pregnancy outcomes (28). The unfavorable maternal outcome following an obstetric emergency was 15.9%, according to our findings. This conclusion was more significant than a multi-country study finding of 4.31% among women with pre-eclampsia but lower than the 18.06 % among women with eclampsia.This could be related to the study area, sample size, and variance in inclusion criteria. Our findings also revealed that the adverse perinatal outcome following an obstetric emergency in Ethiopia is 37.1 %, which is higher than the global average of 30.89 % (women with pre-eclampsia). This could be due to differences in inclusion criteria (29).
Obstetric emergencies and adverse maternal outcomes
An obstetric emergency is a potentially fatal obstetrical condition that causes considerable maternal and fetal morbidity and mortality. Furthermore, our findings revealed that maternal and neonatal morbidity and mortality were common among women who had experienced obstetrical difficulties. According to the meta-analysis, the probability of a negative maternal outcome is 2.9 times higher in mothers with an obstetric emergency than in normotensive women. This finding was in line with a study conducted in SSA, which found that pregnant women with hypertension were 3.1 times more likely than normotensive pregnant women to have a cesarean section. However, this result is lower than that of a Pakistani study, which found that women with hypertension were 6.23 times more likely to have a negative outcome. (30).This could be related to the difference in the number of papers included in the meta-analysis, which varies from 0 to 1.8 times in high-income nations. Because of variations in the incidence and quality of obstetric treatment provided to emergency obstetric patients, there is such a large disparity (31).
Obstetric emergencies and perinatal deaths
In terms of perinatal deaths, the pooled analysis revealed that the risk of perinatal death was significantly increased by 3.84 times, and the meta-analysis revealed medium heterogeneity in women having obstetric emergencies compared to normotensive women, and this finding was lower than a study conducted in SSA, which revealed that perinatal mortality was 8.2 times more significantly associated with HDP, and the meta-analysis revealed large heterogeneity, I2 = 96.9%, p < 0.0001 (32). This could be due to differences in geography, sample error, and the methodology of each study.
Obstetric emergencies and LBW
The pooled analysis of our findings showed that the risk of LBW was significantly increased by 4.77 times greater in women having obstetric emergencies than in normotensive women. This finding was almost similar to a study finding of SSA; the likelihood of LBW was 3.23 times greater in women having PIH (32).
Obstetric emergencies and NICU admission
The pooled analysis of our findings revealed that the risk of NICU admission was five times higher in women giving birth while having obstetric emergencies than in normotensive women. Our finding was higher than a study conducted in Georgia, shows that newborns whose mothers received intensive care due to obstetric emergencies had 1.16 times increased odds of being admitted to NICU (33). This might be due to care management differences and differences in the study area.
Strengths and weaknesses of the study
Studies were carefully chosen using a rigorous search technique to ensure that retrospective and prospective cohorts and cross-sectional studies were included unbiasedly. Despite carefully selecting relevant and well-conducted research, there was a wide range of reported obstetric emergency magnitudes. Because of the small number of studies evaluating outcomes, particularly negative maternal outcomes, it was impossible to draw firm conclusions. The research was only conducted in six regions of the country, which may have diminished its representativeness. Additionally, several included studies had small sample sizes, which may affect the estimation of the results. Most of the included studies have been predominantly conducted in tertiary health institutions, and the findings may not reflect outcomes in low-level facilities. This study hadn't addressed factors for the occurrence of obstetric emergencies.
Conclusion
This review demonstrated the high prevalence of perinatal mortality among pregnant women with one of the obstetric emergencies in Ethiopia. Adverse maternal and perinatal outcomes following obstetric emergencies such as ICU admission, development of PPH, giving birth via CS, maternal death, NICU admission, LBW, and perinatal death were commonly reported in this study.
Recommendations
Because three delays in our country (delay in diagnosis, delay in early referral, and delay in providing quality of care) contributed to 40% of adverse pregnancy outcomes, it is recommended to intervene at three levels to improve the maternal and fetal outcomes of obstetric emergencies in Ethiopia; this helps to ensure the safety of pregnant women and their babies.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Acknowledgments
We would like to thank all of the authors of the studies included in our review.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
2. Lawn JE, Gravett MG, Nunes TM, Rubens CE, Stanton C, Global report on preterm birth and stillbirth (1 of 7): definitions, description of the burden and opportunities to improve data. BMC Pregnancy Childbirth. (2015). 10:S1. doi: 10.1186/1471-2393-10-S1-S1
3. Filippi V, Ronsmans C, Campbell OM, Graham WJ, Mills A, Borghi J et al. Maternal healthin poor countries: the broader context and a call for action. Lancet. (2006) 368:1535–41. doi: 10.1016/S0140-6736(06)69384-7
4. Chaibva BV. Determinants of adverse pregnancy outcomes in Mutare district clinics, Manicaland Province, Zimbabwe (MSc Dissertion). Faculty of Health Sciences, University of Pretoria, Pretoria, South Africa. Available online at: https://repository.up.ac.za/bitstream/handle/2263/46131/Chaibva_Determinants_2015.pdf?sequence=1
6. Say L, Chou D, Gemmill A, Tunçalp Ö, Moller AB, Daniels J, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Global Health. (2014) 2:e323–33. doi: 10.1016/S2214-109X(14)70227-X
7. Chamberlain G, Steer P. Obstetric emergencies. Br Med J. (1999) 318:1342. doi: 10.1136/bmj.318.7194.1342
8. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. (1986) 7:177–88. doi: 10.1016/0197-2456(86)90046-2
9. Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
10. Astatikie G, Limenih MA, Kebede M, Maternal and fetal outcomes of uterine rupture and factors associated with maternal death secondary to uterine rupture. BMC Pregnancy Childbirth. (2017). 17:117. doi: 10.1186/s12884-017-1302-z
11. Jaleta DD, Gebremedhin T, Jebena MG, Jebena MG Perinatal outcomes of women with hypertensive disorders of pregnancy in Jimma Medical Center southwest Ethiopia Retrospective cohort study. PLoS ONE. (2021) 16:e0256520. doi: 10.1371/journal.pone.0256520
12. Shimelis F, Segni H, Fessahaye A. Incidence, causes and outcome of obstructed labor in jimma university specialized hospital. Ethiop J Health Sci. (2010) 20:145–51. doi: 10.4314/ejhs.v20i3.69443
13. Getachew A, Wakgari N, Gishille T. Feto-maternal outcomes of obstructed labor and associated factors among mothers who gave birth in public hospitals of West Shoa Zone, Central Ethiopia: cross-sectional study. Ethiop J Health Sci. (2021) 31:467–74. doi: 10.4314/ejhs.v31i3.3
14. Adane AA, Ayele TA, Ararsa LG, Bitew BD, Zeleke BM. Adverse birth outcomes among deliveries at Gondar University Hospital, Northwest Ethiopia. Pregnancy Childbirth. (2014). 14:90. doi: 10.1186/1471-2393-14-90
15. Degno S, Lencha B, Aman R, Atlaw D, Mekonnen A, Woldeyohannes D et al. Adverse birth outcomes and associated factors among mothers who delivered in Bale zone hospitals, Oromia Region, Southeast Ethiopia. J Int Med Res. (2021) 49:1–12. doi: 10.1177/03000605211013209
16. Abebe H, Shitu S, Workye H, Mose A Predictors of stillbirth among women who had given birth in Southern Ethiopia. PLoS ONE. (2021) 16:e0249865. doi: 10.1371/journal.pone.0249865
17. Gizaw W, Feyisa M, Hailu D, Nigussie T. Determinants of stillbirth in hospitals of North Shoa Zone, Oromia region, Central Ethiopia: A case control study. Heliyon. (2021) 7:e07070. doi: 10.1016/j.heliyon.2021.e07070
18. Gejo NG, Kebede BA, Abdo RA, Anshebo AA, Halil HM, Woldu BF et al. Factors associated with preterm birth at Wachemo University Nigist Eleni Mohammed memorial hospital, southern Ethiopia: case-control study. BMC Pregnancy Childbirth. (2021) 21:35. doi: 10.1186/s12884-020-03503-9
19. Tasew H, Zemicheal M, Teklay G, Mariye T, Ayele E, Risk factors of birth asphyxia among newborns in public hospitals of Central Zone Tigray Ethiopia. BMC Res Notes. (2018). 11:496. doi: 10.1186/s13104-018-3611-3
20. Welegebriel TK, Dadi TL, Mihrete KM, Determinants of stillbirth in Bonga General and Mizan Tepi University Teaching Hospitals southwestern Ethiopia: a case– control study. BMC Res Notes. (2017) 10:713. doi: 10.1186/s13104-017-3058-y
21. Alemu AY, Belay GM, Berhanu M, Minuye B. Determinants of neonatal mortality at neonatal intensive care unit in Northeast Ethiopia: unmatched case-control study. Trop Med Health. (2020) 48:40. doi: 10.1186/s41182-020-00232-9
22. Vata PK, Chauhan NM, Nallathambi A, Hussein F. Assessment of prevalence of preeclampsia from Dilla region of Ethiopia. BMC Res Notes. (2015) 8:816. doi: 10.1186/s13104-015-1821-5
23. Deressa AT, Cherie A, Belihu TM, Tasisa GG. Factors associated with spontaneous preterm birth in Addis Ababa public hospitals, Ethiopia: cross sectional study. BMC Preg Childbirth. (2018) 18:332. doi: 10.1186/s12884-018-1957-0
24. Wosenu L, Worku AG, Teshome DF, Gelagay AA Determinants of birth asphyxia among live birth newborns in University of Gondar referral hospital northwest Ethiopia: a case-control study. PLoS ONE. (2018) 13:e0203763. doi: 10.1371/journal.pone.0203763
25. Mamo SA, Teshome GS, Tesfaye T, Goshu AT Perinatal asphyxia and associated factors among neonates admitted to a specialized public hospital in South Central Ethiopia: a retrospective cross-sectional study. PLoS ONE. (2022) 17:e0262619. doi: 10.1371/journal.pone.0262619
26. Mihiretu A, Negash T, Elazar T Perinatal Death and Associated Factors in Wolaita Sodo Referral Hospital Southern Ethiopia: A Facility Based Cross-Sectional Study. Prim Health Care. (2017) 7:1–5. doi: 10.4172/2167-1079.1000269
27. Endeshaw G, Berhan Y. Perinatal outcome in women with hypertensive disorders of pregnancy: A retrospective cohort study. Int Sch Res Not. (2015) 2015:208043. doi: 10.1155/2015/208043
28. Musarandega R, Nyakura M, Machekano R, Pattinson R, Munjanja SP, Causes of maternal mortality in Sub-Saharan Africa: a systematic review of studies published from 2015 to 2020. J Glob Health. (2021) 11:04048. doi: 10.7189/jogh.11.04048
29. Abalos E, Cuesta C, Carroli G, Qureshi Z, Widmer M, Vogel JP et al. Pre-eclampsia, eclampsia and adverse maternal and perinatal outcomes: a secondary analysis of the World Health Organization Multicountry Survey on Maternal and Newborn Health. BJOG. (2014) 121:14–24. doi: 10.1111/1471-0528.12629
30. Hossain N, Shah N, Khan N, Lata S, Khan NH. Maternal and perinatal outcome of hypertensive disorders of pregnancy at a tertiary care hospital. J Dow Univ Health Sci Karachi. (2011) 5:12–6. doi: 10.1186/s12884-019-2617-8
31. Ronsmans C, Campbell O. Quantifying the fall in mortality associated withinterventions related to hypertensive diseases of pregnancy. BMC Public Health. (2011) 11:S8. doi: 10.1186/1471-2458-11-S3-S8
32. Gemechu KS, Assefa N, Mengistie B. Prevalence of hypertensive disorders of pregnancy and pregnancy outcomes in Sub-Saharan Africa: a systematic review and meta-analysis. SAGE Women's Health. (2020) 16:1–25. doi: 10.1177/1745506520973105
33. Manjavidze T, Rylander C, Skjeldestad FE, Kazakhashvili N, Anda EE. The impact of antenatal care utilization on admissions to neonatal intensive care units and perinatal mortality in Georgia. PLoS ONE. (2020) 15:e0242991. doi: 10.1371/journal.pone.0242991
34. Getaneh Y, Fekatu E, Jemere AT, Mengiste Z, Tarekegn GE, Oumer M. Incidence and determinants of adverse outcomes among women who were managed for eclampsia in the University of Gondar Comprehensive Specialized Hospital, Northwest Ethiopia. BMC Preg Childbirth. (2021) 21:734. doi: 10.1186/s12884-021-04199-1
35. Adere A, Mulu A, Temesgen F. Neonatal and maternal complications of placenta praevia and its risk factors in tikur anbessa specialized and gandhi memorial hospitals: Unmatched case-control study. J Pregnancy. (2020) 2020:5630296. doi: 10.1155/2020/5630296
36. Berhe AK, Ilesanmi AO, Aimakhu CO, Mulugeta A. Effect of pregnancy induced hypertension on adverse perinatal outcomes in Tigray regional state, Ethiopia: A prospective cohort study. BMC Preg Childbirth. (2020) 20:7. doi: 10.1186/s12884-019-2708-6
37. Belay Tolu L, Yigezu E, Urgie T, Feyissa GT. Maternal and perinatal outcome of preeclampsia without severe feature among pregnant women managed at a tertiary referral hospital in urban Ethiopia. PLoS ONE. (2020) 15:e0230638. doi: 10.1371/journal.pone.0230638
38. Melese MF, Badi MB, Aynalem GK. Perinatal outcomes of severe preeclampsia/ eclampsia and associated factors among mothers admitted in Amhara Region referral hospitals, North West Ethiopia. BMC Res Notes. (2019) 12:147. doi: 10.1186/s13104-019-4161-z
39. Dadi TL, Mihirete KM, Welegebrial TK. Causes and timing of maternal death in mizan - tepi university teaching and bonga general hospital from 2011–2015: A case control study and using propensity score matching analysis. Open Public Health J. (2017) 10:98–105. doi: 10.2174/1874944501710010098
40. Asseffa NA, Demissie BW. Perinatal outcomes of hypertensive disorders in pregnancy at a referral hospital, Southern Ethiopia. PLoS ONE. (2019) 14:e0213240. doi: 10.1371/journal.pone.0213240
41. Eyeberu A, Shore H, Getachew T, Atnafe G, Dheresa M. Neonatal mortality among neonates admitted to NICU of Hiwot Fana specialized university hospital, eastern Ethiopia, 2020: A cross-sectional study design. BMC Pediatr. (2021) 21:125. doi: 10.1186/s12887-021-02598-z
42. Wondimu M, Balcha F, Bacha G, Habte A. The magnitude of neonatal near miss and associated factors among live births in public hospitals of Jimma Zone, Southwest Ethiopia, 2020: A facility-based cross-sectional study. PLoS ONE. (2021) 16:e0251609. doi: 10.1371/journal.pone.0251609
43. Assefa A, Fantahun Y, Mesfin E. Maternal and perinatal outcome of antepartum hemorrhage at three teaching hospitals in Addis Ababa, Ethiopia. Ethiopian J Reprod Health. (2020) 12:12–9. Available online at: https://ejrh.org/index.php/ejrh/article/view/395/128
44. Bereka TM, Aweke AM, Wondie TE. Associated factors and outcome of uterine rupture at Suhul General Hospital, Shire Town, North West Tigray, Ethiopia 2016: A case-control study. Obstet Gynecol Int. (2017) 2017:8272786. doi: 10.1155/2017/8272786
45. Legu KL, Debiso AT, Rodamo KM. The magnitude of perinatal mortality rate and associated risk factors among deliveries at Dilla University Referral Hospital, Southern Ethiopia: A case-control study. Health Care-Low Resour. (2021) 9:9960. Available online at: https://www.pagepressjournals.org/index.php/hls/article/view/9960/9836
Keywords: adverse outcome, perinatal death, maternal death, adverse, obstetrics emergency
Citation: Leta M, Assefa N and Tefera M (2022) Obstetric emergencies and adverse maternal-perinatal outcomes in Ethiopia; A systematic review and meta-analysis. Front. Glob. Womens Health 3:942668. doi: 10.3389/fgwh.2022.942668
Received: 12 May 2022; Accepted: 25 August 2022;
Published: 26 October 2022.
Edited by:
Adebola Emmanuel Orimadegun, University of Ibadan, NigeriaReviewed by:
Kehinde Adesokan, University of Ibadan, NigeriaChristopher Yilgwan, University of Jos, Nigeria
Copyright © 2022 Leta, Assefa and Tefera. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Masresha Leta, bWFzcmVzaGFsZXRhMyYjeDAwMDQwO2dtYWlsLmNvbQ==
 Masresha Leta
Masresha Leta Nega Assefa2
Nega Assefa2 Maleda Tefera
Maleda Tefera