- 1Department of Clinical Medicine, UiT The Arctic University of Norway, Tromsø, Norway
- 2Norwegian Centre for E-Health Research, University Hospital of North Norway, Tromsø, Norway
Background: Reducing maternal mortality, neonatal mortality and under 5-year mortality are important targets addressed by the United Nations' Sustainable Development Goals. Despite studies reported an improvement in maternal and child health indicators, the progress achieved is not uniform across regions. Due to the increasing availability of mobile phones in low and middle-income countries, mHealth could impact considerably on reducing maternal and child mortality and maximizing women's access to quality care, from the antenatal stage to the post-natal period.
Methods: A systematic literature review of mHealth interventions aimed at reducing maternal and child mortality in Sub-Saharan Africa and Southern Asia. Primary outcomes were maternal mortality, neonatal mortality, and under-five mortality. Secondary outcomes were skilled birth attendance, antenatal care (ANC) and post-natal care (PNC) attendance, and vaccination/immunization coverage. We searched for articles published from January 2010 to December 2020 in Embase, Medline and Web of Science. Quantitative comparative studies were included. The protocol was developed according to the PRISMA Checklist and published in PROSPERO [CRD42019109434]. The Quality Assessment Tool for Quantitative Studies was used to assess the quality of the eligible studies.
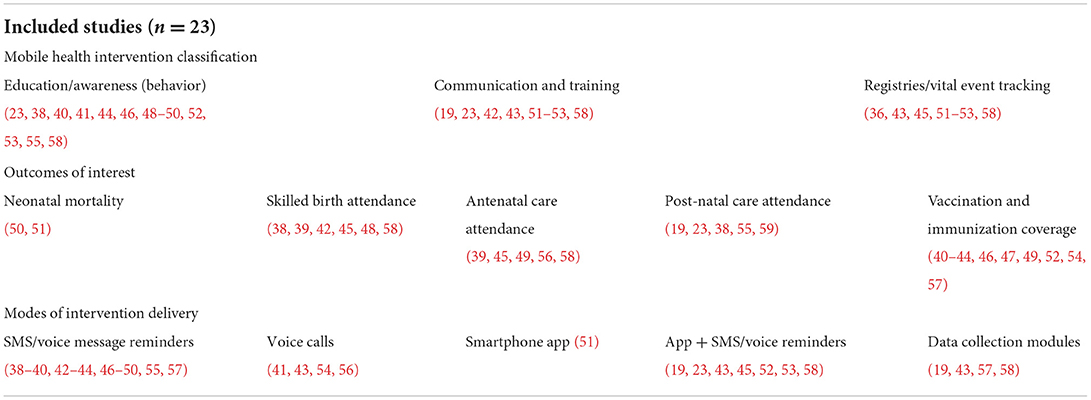
Results: 23 studies were included in the review, 16 undertaken in Sub-Saharan Africa and 7 in Southern Asia. Most studies used SMS or voice message reminders for education purposes. Only two studies reported outcomes on neonatal mortality, with positive results. None of the studies reported results on maternal mortality or under-five mortality. Outcomes on skilled birth attendance, ANC attendance, PNC attendance, and vaccination coverage were reported in six, six, five, and eleven studies, respectively. Most of these studies showed a positive impact of mHealth interventions on the secondary outcomes.
Conclusion: Simple mHealth educational interventions based on SMS and voice message reminders are effective at supporting behavior change of pregnant women and training of health workers, thus improving ANC and PNC attendance, vaccination coverage and skilled birth attendance. Higher quality studies addressing the role of mHealth in reducing maternal and child mortality in resource-limited settings are needed, especially in Southern Asia.
Systematic review registration: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42019109434, identifier CRD42019109434.
Introduction
The Millennium Development Goals (MDGs) were established in 2000 after the Millennium Summit of the United Nations (UN) (1, 2). Child and maternal mortality, addressed by MDG 4 and MDG 5, respectively, experienced a substantial decline from 2000 to 2015 (3–6). The global under 5-year mortality was reduced from 11.9 million deaths in 1990 to 7.7 million deaths in 2010 (7), with an accelerated decline reported during the second decade. Despite the target of decreasing maternal mortality by 75% was not achieved, all MDG regional groupings showed a significant improvement (4, 5). The end of the MDG era in 2015 marked the transition into the Sustainable Development Goals (SDGs), which encompassed global targets of further reducing maternal mortality, neonatal mortality and under 5-year mortality (8). The SDGs, implemented with another 15-year plan due by 2030, represent a comprehensive blueprint for sustainable development toward health and wellbeing. Over 50 indicators are defined by the SDGs to measure health outcomes and health service delivery (8). Reproductive, maternal, newborn and child health are among the main thematic areas.
Several studies reported an improvement in maternal and child health indicators (4, 7). Nevertheless, a UN report on the MDGs evaluations indicated that, regardless of the progress achieved, the reduction in maternal and child mortality across most regions was not uniform (2). This culminated in the inability to achieve the MDGs. According to Solow's growth model (9), a greater progress among low-income countries compared with high-income countries leads to convergence across the world countries. On the contrary, a greater progress among high-income countries widens the gaps, leading to overall divergence among countries (2, 9). There is therefore a call for a strong program of action and interventions to bring equity and eliminate the divergent progress on maternal and child health between high-income and low-income countries. Interventions aimed at eradicating preventable maternal and child mortality are required in resource-limited settings, such as Sub-Saharan Africa and Southern Asia, to ensure convergent progress worldwide.
Since most people in low and middle-income countries have a mobile phone (10), interventions based on mobile technologies represent a very promising tool to increase efficiency in health care and enhance service utilization (11–14). Mobile health (mHealth) is defined as medical and public health practice supported by mobile devices, such as mobile phones, patient monitoring devices, personal digital assistants, and other wireless devices (15). Such solutions enable the provision of healthcare anytime and anywhere, overcoming organizational and geographical barriers. mHealth has the potential to address the health challenges and needs of the Global South, particularly in Sub-Saharan Africa and Southern Asia (16–18). The introduction of mHealth interventions could impact considerably on reducing maternal mortality (11) and maximizing women's access to quality care (19), from the antenatal stage (20, 21) to the post-natal period (11, 22–24). mHealth might support the global effort in addressing the SDG 3 and achieving the SDG Target 3.1 and 3.2 on maternal and neonatal/child health, respectively (25, 26).
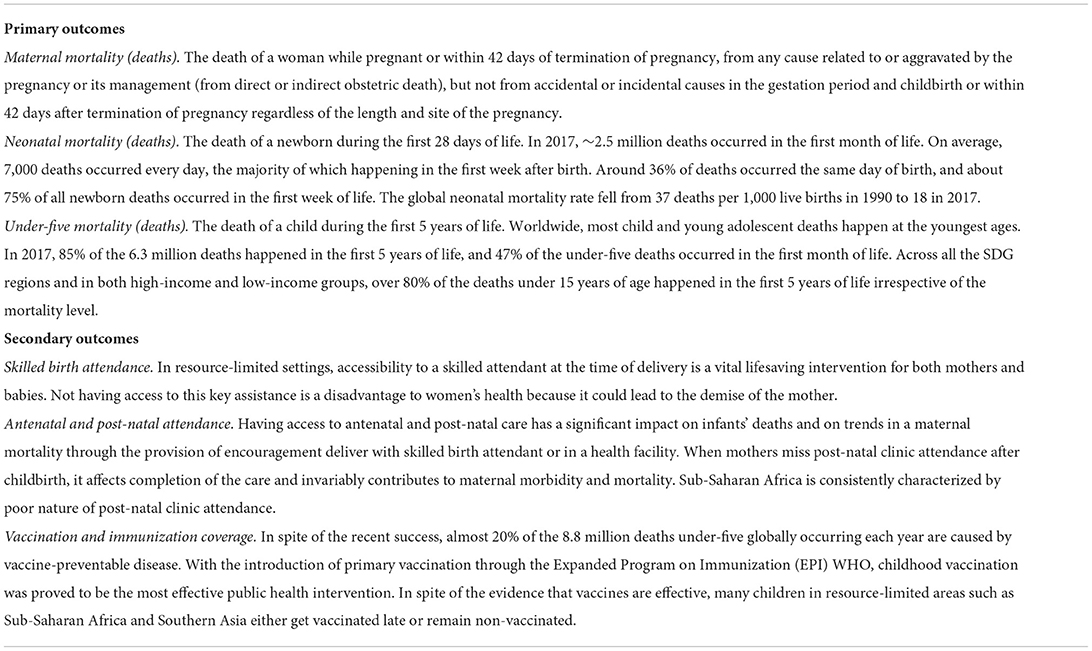
This study aimed to evaluate the impact of mHealth interventions on maternal and child health in resource-limited settings. The primary outcomes directly related to SDG Target 3.1 and 3.2 were: (1) maternal mortality (SDG Indicator 3.1.1), (2) neonatal mortality (SDG Indicator 3.2.2), (3) under-five mortality (SDG Indicator 3.2.1). Secondary outcomes selected by the authors due to their impact on maternal and child mortality included: skilled birth attendance (SDG Indicator 3.1.2), antenatal care (ANC) and post-natal care (PNC) attendance, vaccination/immunization coverage. The identification of effective mHealth interventions could contribute to an accelerated progress toward achieving the SDG 3 by 2030.
Methods
Study design
We performed a systematic literature review (27) on mHealth interventions aimed at reducing preventable maternal, neonatal and under-five mortality in Sub-Saharan Africa and Southern Asia. The review was conducted in accordance with the Preferred Reporting Items for Systematic review and Meta-Analysis Protocols (PRISMA-P) (28, 29) to ensure a transparent and complete reporting of the study. The study protocol was developed a priori and published in the International Prospective Register of Systematic Reviews (PROSPERO) [registration number CRD42019109434] (30).
Eligibility criteria
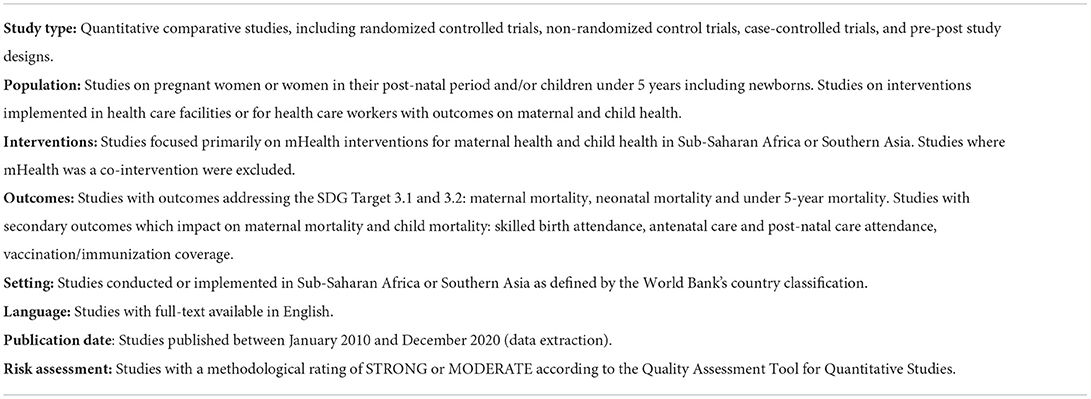
The scope of the review and eligibility criteria were formulated using the PICOS framework (participants, interventions, comparisons, outcomes, study type) (31) (Table 1).
Data sources and search strategy
Relevant articles were searched in Medline, Embase and Web of Science. The search strategy was based on the PICOS framework and developed using selected keywords as well as thesaurus terms of each database. The search strategy (Supplementary Table 1) included terms relating to or describing mHealth interventions according to the eligibility criteria. The search strategy was tested before starting the formal screening. The results of each database search were stored into a single reference database (Endnote). Duplicate references were removed. The electronic search was performed by one review team member (EB).
Study selection and data extraction
Titles and abstracts were screened, and studies which did not meet the inclusion criteria were excluded. The full texts of the selected studies were then retrieved and independently assessed for eligibility by two review team members (EB, PZ). Any disagreement over the eligibility of particular studies was resolved through discussion and the involvement of another reviewer (MJ). A standardized data extraction form was developed, piloted and used to extract information from the full texts for evidence synthesis (Supplementary Table 2). For each article, results were extracted for the primary and secondary outcomes (Table 2).
Methodological quality assessment
The overall quality related to the conduction of quantitative studies and reporting of the results is not always satisfactory (32). Studies of low methodological quality typically tend to report better treatment effects than studies of high quality (33–35). The Effective Public Health Practice Project (EPHPP) Quality Assessment Tool for Quantitative Studies was used to assess the quality of the eligible studies (36), since the EPHPP tool has proven to have a higher inter-rate agreement compared to the Cochrane Collaboration Risk of Bias tool when evaluating quantitative studies (37). The quality of each study was assessed in terms of selection bias, study design, confounders, blinding, data collection methods, and withdrawal and dropouts. A rating is assigned to each of the six components, and a final global rating (strong, moderate, weak) was then assigned. Studies with weak ratings were defined by the quality assessment tool as those with more than three weak component ratings. According to the recommendations by the Cochrane handbook (31) and the EPHPP Quality Assessment Tool for Quantitative Studies (36), studies of weak methodological quality were excluded from the final analysis to improve the quality of the results of this systematic literature review.
Synthesis of the results
Data extracted on the characteristics and findings of the included studies were structured in form of a tabular summary. The findings were analyzed and organized according to study types, mHealth interventions and outcomes.
Results
Search results
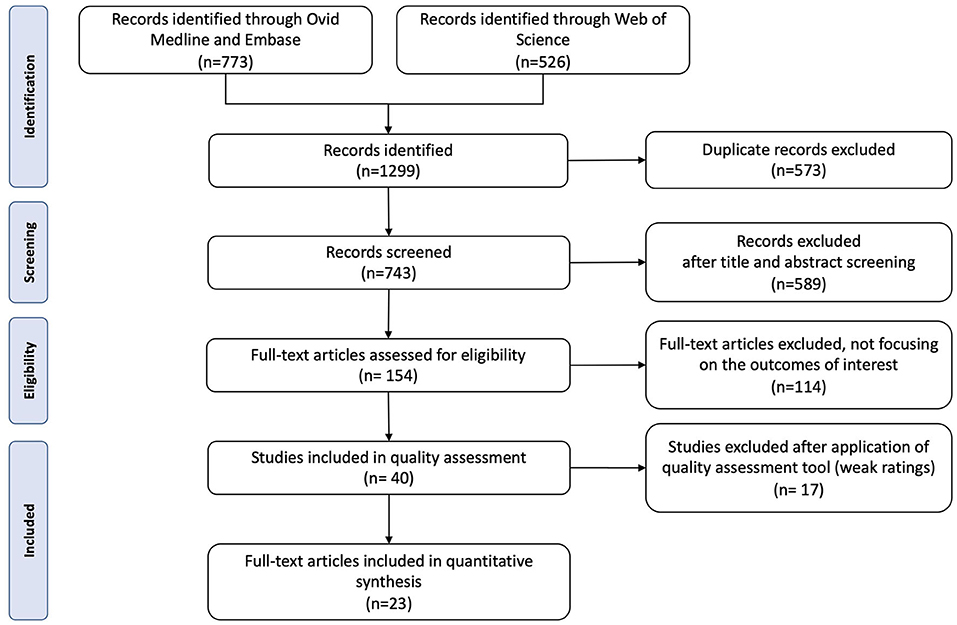
A total of 1,299 articles were identified from the search strategy (Figure 1). After removing duplicates and initial screening, 154 full-text articles were assessed for eligibility. Following further inspection and quality assessment (Supplementary Table 3), 23 articles were included in this review (19, 23, 38–58).
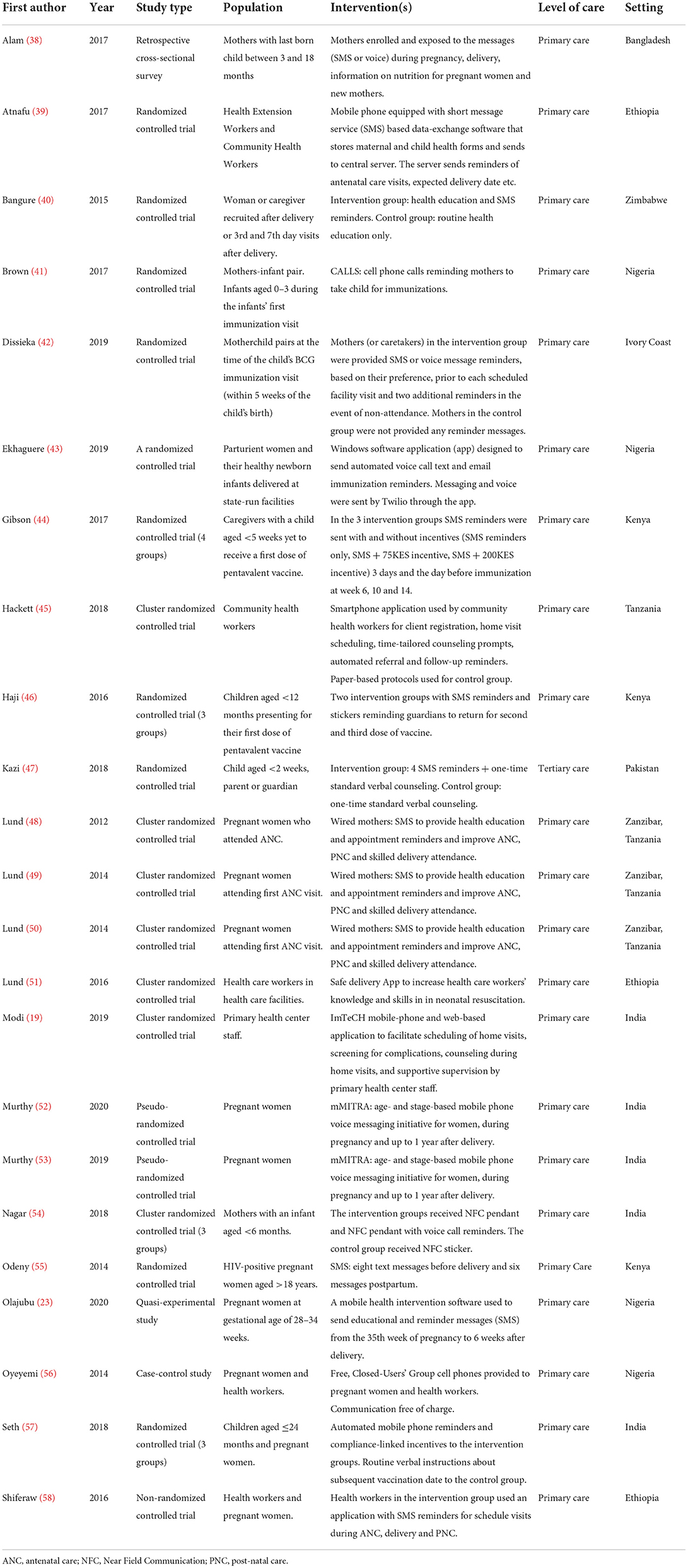
Characteristics of the included studies
The characteristics of the included studies, including study type, population, interventions, level of care, and setting, were structured in a tabular summary (Table 3). There were 20 randomized controlled trials (RCTs), one non-randomized controlled trial, one quasi-experimental study and one retrospective cross-sectional survey. Sixteen studies were undertaken in Sub-Saharan Africa, while only seven were undertaken in Southern Asia. All studies except one were conducted in primary care settings.
The vast majority of the studies reported mHealth interventions used for educational purposes. The most common form of delivery was SMS, used either alone as reminders or in combination with a mobile application (Table 4).
Synthesis of the study outcomes
Primary outcomes
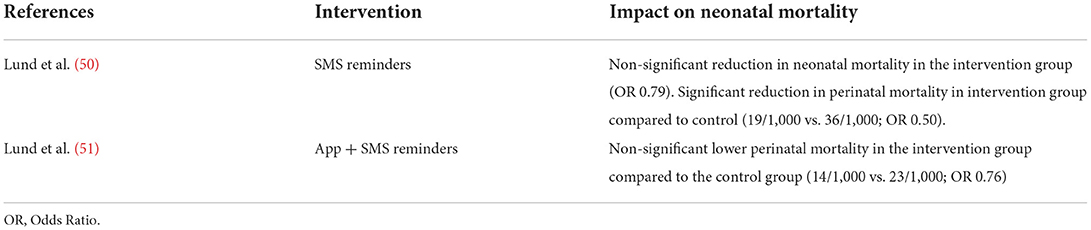
Neonatal mortality
Only two studies reported neonatal mortality outcomes (Table 5). In a cluster RCT conducted in primary health care facilities in Zanzibar, the Wired Mothers intervention, consisting of a text message and free call voucher system linking women to the health system throughout their pregnancy, childbirth, and postpartum period, was associated with a significant reduction in perinatal mortality and a non-significant reduction in neonatal mortality (Odds Ratio (OR) 0.79) (50). In a RCT conducted on 73 primary healthcare facilities in Ethiopia, the use of a safe delivery app was associated with a non-significant decline in perinatal mortality (OR 0.76) (51).
Maternal mortality and under-five mortality
None of the studies included in this review reported results on maternal mortality and under-five mortality. No study from Southern Asia reported results on the primary outcomes.
Secondary outcomes
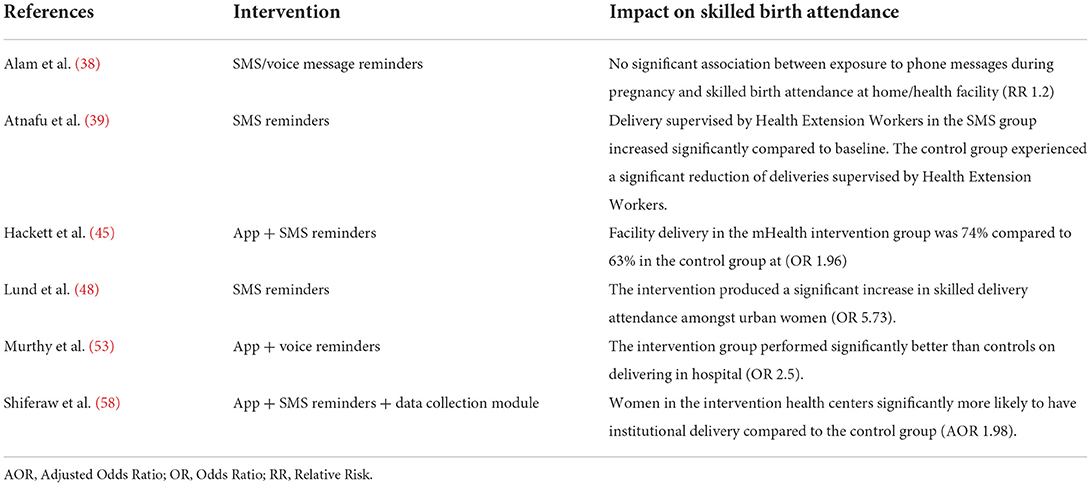
Skilled birth attendance
Six studies reported outcomes on skilled birth attendance (Table 6), which is a vital lifesaving intervention for both mothers and babies. Three studies delivering mHealth interventions based on SMS/voice message reminders only (38, 39, 48) demonstrated a positive impact on skilled birth attendance. In the Wired Mothers study, the intervention group receiving SMS reminders had a significantly higher percentage of women delivering with skilled birth personnel (60%) compared to the control group (47%) (48). The use of apps in combination with SMS or voice reminders has also been proven to significantly increase supervised institutional deliveries in three studies (45, 53, 58).
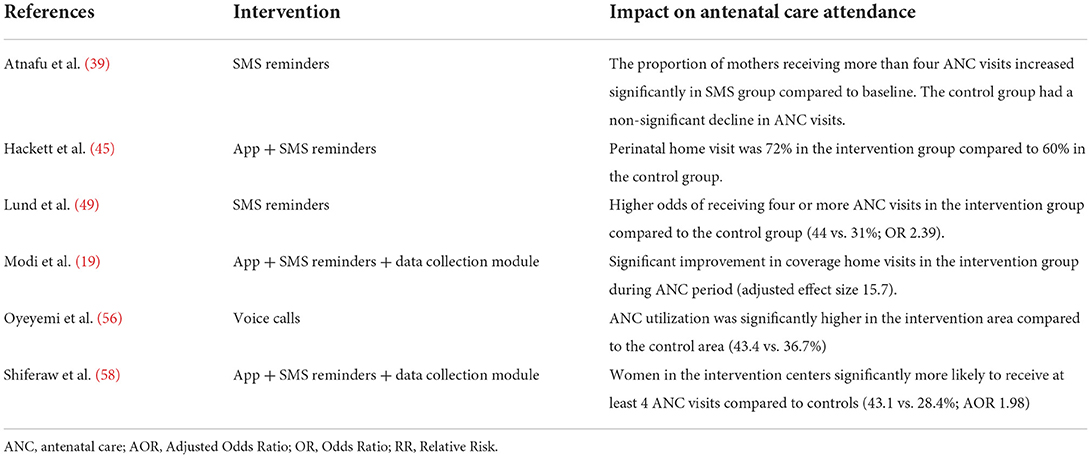
Antenatal and post-natal care attendance
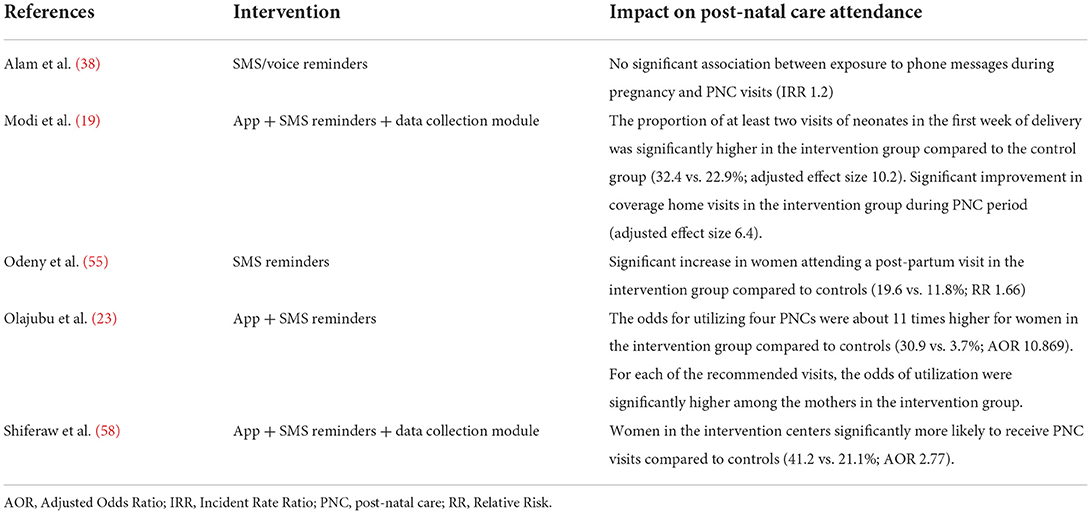
Outcomes on ANC attendance (Table 7) and PNC attendance (Table 8) were reported in six studies (19, 39, 45, 49, 56, 58) and five studies (19, 23, 38, 55, 58), respectively. These studies showed that a variety of mHealth interventions delivered through simple mobile phone voice calls (56), SMS/voice reminders (38, 39, 49, 55) or apps/data collection modules (19, 23, 45, 58) can lead to improved access to ANC and PNC services. A study conducted in Ethiopia where SMS reminders for scheduled visits were sent to health workers demonstrated that women in the intervention health centers were more likely to attend at least four ANC visits (58). Attendance to four ANC visits was also associated with higher odds of PNC and delivery in a health facility where there is a greater chance of having access to a skilled birth attendant (58). Similarly, results from the SUSTAIN-MNCH study, where a smartphone-based application was designed to assist community health workers in Tanzania, showed that the uptake of ANC was a strong predictor of facility delivery (45).
Vaccination/immunization coverage
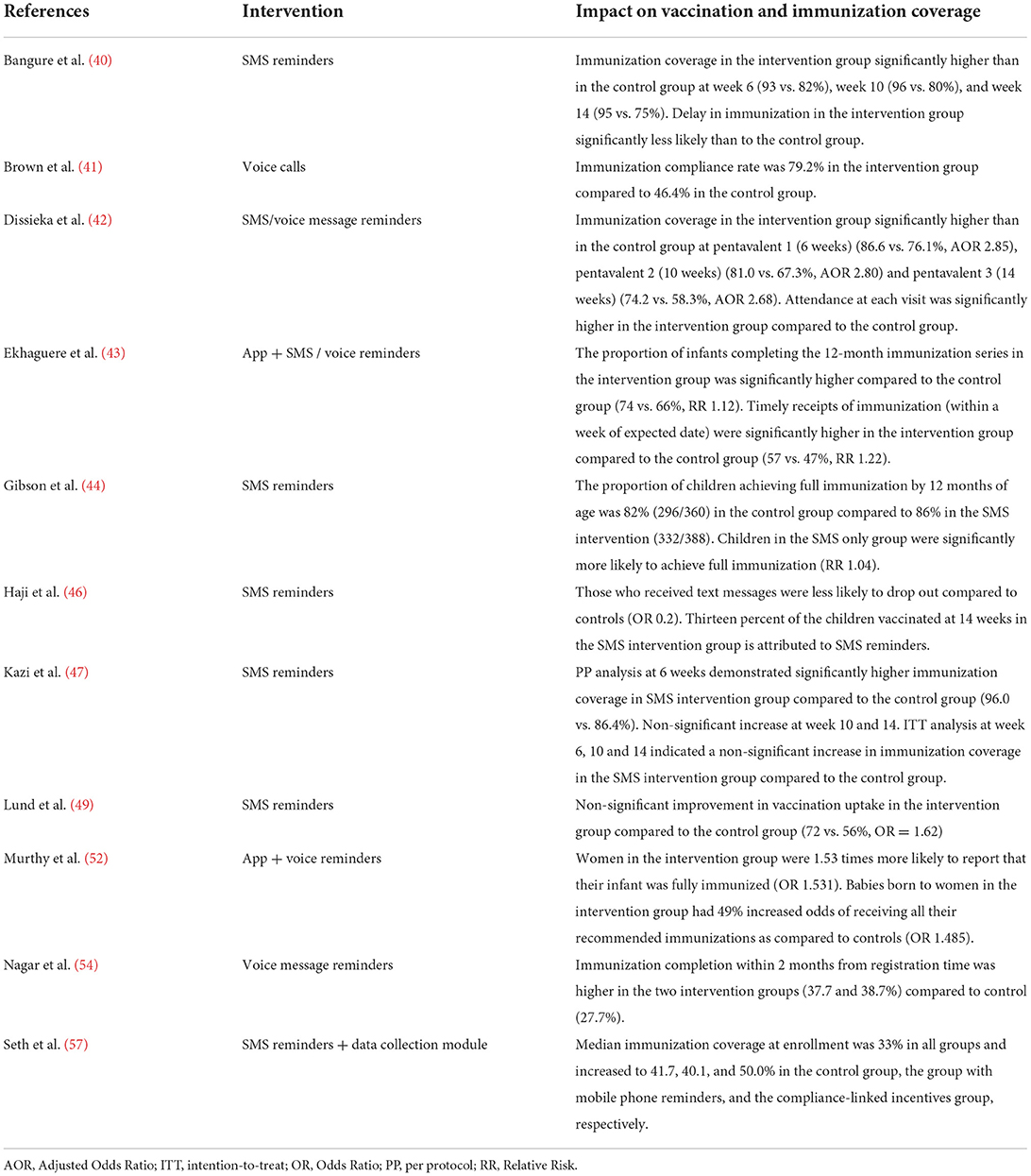
Eleven studies had outcomes related to vaccination coverage (Table 9) (40–44, 46, 47, 49, 52, 54, 58). The vast majority of these studies delivered simple interventions consisting of SMS/voice message reminders (40, 42, 44–47, 54, 57) or voice calls (41). One study found that the intervention group receiving SMS reminders had a significantly lower vaccination dropout rate compared to the control group receiving routine reminders (OR 0.2) and a significantly higher vaccination coverage (46). In another study evaluating a cellphone-based reminder/recall strategy to improve childhood routine immunization, immunization compliance rate was 79.2% among the children in intervention group and 46.4% in the control group (41).
Discussion
Summary of evidence
This study provides a comprehensive overview of mHealth interventions implemented in Sub-Saharan Africa and Southern Asia with outcomes addressing, directly or indirectly, the Target 3.1 and 3.2 of the SDG 3. We identified 23 relevant studies published from 2010 to 2020, which demonstrate a growing effort in evaluating the effects of mHealth interventions on maternal and child health outcomes. Low access to maternal health services, including skilled birth attendance at delivery, ANC attendance, PNC attendance, and vaccination and immunization coverage, represents a major cause of maternal and neonatal mortality. Interventions aimed at addressing those outcomes can therefore contribute to alleviate the burden of maternal and neonatal deaths targeted by the SDG 3. Despite few studies addressed mortality outcomes directly, the results from this systematic review showed that mHealth interventions are effective at changing the behavior of pregnant women, caretakers and health workers, and at increasing ANC attendance, PNC attendance, childhood vaccination/immunization rates, and skilled delivery attendance. Most of the mHealth interventions covered by this review were delivered with minimal resources and consisted of simple SMS or voice message reminders which are particularly suitable for resource-limited settings.
mHealth impact on maternal, neonatal and under-five mortality
Only two studies (50, 51) reported results on neonatal mortality, while none of the included studies reported results on maternal and under-5 year mortality. The two studies with results on neonatal mortality found that SMS reminders for pregnant women and smartphone-based applications for education of health workers can be effective in reducing neonatal deaths in resource-limited countries. The evidence of the impact of mHealth interventions on neonatal mortality is, however, limited since it is based on two studies only, both conducted in the Eastern part of Sub-Saharan Africa. More studies conducted in the two SDG regions covered by this review, and especially in Southern Asia, are still needed to support the evidence of the effects on neonatal mortality. This is also necessary to avoid any divergence in the progress toward the SDGs between the two regions. Overall, only seven of the 23 studies included in this review were conducted in Southern Asia. A number of studies from Southern Asia were excluded from this review since they obtained a weak rating in the quality assessment (Supplementary Table 3).
mHealth impact on skilled birth attendance
Skilled birth attendance is recognized as a crucial intervention to avert preventable obstetric complications, which are one of the main causes of maternal and perinatal mortality (59). The proportion of births or deliveries attended by skilled birth personnel is a vital indicator for harnessing the SDG Target 3.1. Access to skilled birth attendance is also addressed by the Global Strategy for Women's, Children's and Adolescents' Health 2016–2030 and by the framework for ending preventable maternal mortality 2015–2030 (60). The coverage of skilled birth attendants in Sub-Saharan Africa is lower compared to all other regions in the world (61). Moreover, the MDG tracking report (62) stated that the proportion of births in the presence of a skilled attendant in Sub-Saharan Africa increased only by 7% between 1990 (41%) and 2008 (48%).
Evidence from this systematic review demonstrated that mHealth interventions, such as the Wired Mothers, have the potential to support skilled birth attendance which, in turn, can contribute to reduce the global maternal mortality (48). Other studies concluded that mHealth interventions can support behavioral change and influence women's choice of delivery attendance (63, 64). The Safe Delivery Application study conducted in Ethiopia demonstrated that mHealth interventions can improve knowledge and skill acquisition of healthcare workers as well as quality care during emergencies in child birth (51). Such findings are instrumental in addressing the challenges in the provision of quality care due to the absence of continuing education programs. Findings from another study conducted in Ethiopia on the use of a mHealth intervention to improve delivery and PNC (58) supported an earlier study conducted in Zanzibar testing the ability of SMS reminders to improve skilled birth delivery at births (48).
mHealth impact on antenatal and post-natal care attendance
Having access to ANC and PNC has a significant impact on neonatal mortality as well as an indirect role in reducing maternal mortality by encouraging women to deliver with assistance of a skilled birth attendant or in a health facility (65). Interventions encouraging frequent ANC contacts allow pregnant women to prepare for delivery and be acquainted with educational information on the warning signs of poor maternal or infant health during pregnancy and childbirth. Likewise, interventions aimed at promoting PNC allow mothers and babies to be assessed during visits and can mitigate the risks of maternal and infant morbidity and mortality, which are highest in the days and weeks following childbirth (66–68). mHealth interventions have the potential to support the uptake of these maternal and child health services, thus contributing to reduce regional differences in infant and maternal mortality.
The Wired Mothers (48) and the SUSTAIN-MNCH (45) studies indicated that mHealth interventions delivered through smartphones can contribute to attain the World Health Organization's (WHO) recommendation of four ANC visits in the course of pregnancy (at weeks 14, 24, 30, and 36) and delivery at a health facility (69, 70). Such interventions are especially useful in disadvantaged settings burdened with poverty and low rates of facility delivery. Additionally, the SUSTAIN-MNCH intervention and the Safe Delivery Application confirmed the importance of training of health workers through smartphone applications to enhance uptake of health facility delivery and skills improvement on newborn resuscitation, thus supporting the global effort in reducing neonatal mortality. The results from the Safe Delivery Application support the findings from a review showing that neonatal resuscitation reduces neonatal and perinatal mortality (71). Moreover, ensuring that every child delivery is done in the presence of skilled health personnel is a key to reduce the global maternal deaths (72). The current systematic review showed that access to skilled birth delivery and health facility delivery, as part of mHealth interventional strategies in the continuum of care, can contribute to reduce mortality rates as addressed by the SDG Target 3.1 and 3.2.
mHealth impact on vaccination and immunization coverage
A UNICEF report in 2015 acknowledges childhood diseases as the cause of most neonatal and under-five deaths in Sub-Saharan Africa (73). A simple and effective way of protecting children and minimizing the spread of diseases is immunization. The main target of the immunization agenda 2030 is to make immunization achievable for everyone, everywhere, at every age, by 2030. A number of studies have confirmed that immunization is a cost-effective public health intervention capable of contributing significantly to the SDG 3.2 (i.e., end avoidable deaths of newborns and children under five) (74–76).
The results from this review are indicative of how simple mHealth interventions, including SMS reminders (40, 44, 46), voice message reminders (42, 52, 54) and voice calls (41), are effective at improving vaccination and immunization coverage in resource-limited settings where coverage is low, such as Sub-Saharan Africa and Southern Asia. The available evidence also shows that mHealth interventions can contribute to reduce delays in immunization and improve immunization compliance rate (40, 41), thus increasing adherence to timely receipts of immunization and immunization completeness (43, 54). This will ultimately contribute to the Global Vaccine Action Plan (GVAP), which aims to achieve at least 90% national vaccination coverage and herd immunity level of immunization coverage where the chain of disease transmission is broken. Improved vaccination and immunization coverage will, in turn, support the SDG Target 3.2 of ending avoiding deaths of newborns and children under-5 years of age.
Limitations
According to the scope of this systematic literature review and its eligibility criteria, only papers published in peer-reviewed journals were included. As a consequence, other sources which might include useful results on maternal and child mortality, such as reports from non-profit organizations or white or gray literature, were excluded. Moreover, the study included only papers published in English. It is possible that studies reporting results of mHealth interventions conducted in Sub-Saharan Africa and Southern Asia were published in another language than English. It is also worth noting that there was an overlap among some of the studies included in this review. In particular, three papers reporting on use of SMS reminders were linked to the same program in Zanzibar, Tanzania (48–50). The generalizability of the findings from this review is affected by the variety of the mHealth interventions described in the included studies.
Policy implications
This systematic literature review provides a useful contribution toward the role of mHealth interventions in achieving the UN's SDG 3. The results showed an increasing number of evidence-based interventions aimed to make pregnancy and childbirth safer for both mother and child by alleviating the burden of maternal and neonatal deaths. The findings from this study can inform policy makers and serve as a basis to provide recommendations on the implementation of mHealth interventions in resource-limited settings, including SMS messages to improve maternal health-seeking behavior and reminders to caretakers in the health delivery structure.
With most maternal, neonatal and child deaths taking place in Sub-Saharan Africa and Southern Asia, a need for action is required to achieve the SDG Target 3.1 and 3.2. If innovative interventions supporting maternal, neonatal and child health are implemented in the healthcare delivery system, more than half of the global 56 million deaths under-5 year could potentially be prevented between 2018 and 2030 in Sub-Saharan Africa and Southern Asia (77). The potential presented by mHealth interventions is promising and offers new hope for the future. The progress demonstrated in the two SDG regions included in this systematic review shows that the maternal and child health can be improved through mHealth interventions aimed to increase access to skilled delivery attendance, vaccination coverage, immunization uptake, ANC and PNC. Increasing women's access to quality care, from the antenatal stage to the post-natal period, also contribute to improving equity and reducing health disparities between high-income and low-income countries. This ultimately contributes to a growing evidence that mHealth can support the SDG 3 (78) by reducing maternal and neonatal mortality in the post 2015 agenda of the UN.
Conclusions
The results from this systematic review are indicative of how simple mHealth educational interventions based on SMS and voice message reminders, used either alone or in combination with a mobile application, can support behavior change of pregnant women and training of health workers and are effective at improving skilled birth attendance, ANC and PNC attendance, and vaccination coverage. At the primary health care level, mHealth interventions can play a pivotal role in increasing access to quality care in a decentralized health care system. This is especially important in resource-limited settings, such as Sub-Saharan Africa and Southern Asia, where an acceleration of progress is needed to address the burden of maternal mortality and neonatal mortality. Higher quality studies addressing the role of mHealth in reducing maternal and child mortality in resource-limited settings are needed, especially in Southern Asia.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
Author contributions
Conceptualization, methodology, validation, and writing—review and editing: EB, MJ, and PZ. Data curation, visualization, and writing—original draft: EB. Investigation: EB and PZ. Supervision: MJ and PZ. All authors contributed to the article and approved the submitted version.
Funding
This study was initiated and managed by UiT The Arctic University of Norway as part of a master's degree program in Telemedicine and E-health. Access to commercial databases was granted through the UiT library.
Acknowledgments
We thank librarian Eirik Reierth at the UiT The Arctic University of Norway, who helped in developing the search strings for the review, and Karianne Lind at the Norwegian Centre for E-health Research who helped in conducting the search on the selected databases.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgwh.2022.942146/full#supplementary-material
References
1. Power C. Addressing the UN millennium development goals. Int Educ J Compar Perspect. (2011) 10:3–19.
2. Goli S, Arokiasamy P. Maternal and child mortality indicators across 187 countries of the world: converging or diverging. Glob Public Health. (2014) 9:342–60. doi: 10.1080/17441692.2014.890237
3. Melamed C, Sumner A. A Post-2015 global development agreement: why, what, who. In: Workshop on Post-2015 Global Development Agreement. Cairo (2011). Available online at: https://cdn.odi.org/media/documents/7369.pdf
4. Alkema L, Chou D, Hogan D, Zhang S, Moller A-B, Gemmill A, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet. (2016) 387:462–74. doi: 10.1016/S0140-6736(15)00838-7
5. WHO. Trends in Maternal Mortality: 1990-2015: Estimates From WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Geneva: World Health Organization (2015).
6. Hug L, Sharrow D, You D. Levels & trends in child mortality: report 2017. In: Estimates Developed by the UN Inter-agency Group for Child Mortality Estimation. New York, NY: United Nations Children's Fund (2017).
7. Rajaratnam JK, Marcus JR, Flaxman AD, Wang H, Levin-Rector A, Dwyer L, et al. Neonatal, postneonatal, childhood, and under-5 mortality for 187 countries, 1970–2010: a systematic analysis of progress towards Millennium Development Goal 4. Lancet. (2010) 375:1988–2008. doi: 10.1016/S0140-6736(10)60703-9
8. WHO. World Health Statistics 2017: Monitoring Health for the SDGs. Sustainable Development Goals. Geneva: WHO (2017).
9. Barro RJ, Sala-i-Martin X, Blanchard OJ, Hall RE. Convergence across states and regions. Brookings Papers Econ Activity. (1991) 1:107–82. doi: 10.2307/2534639
10. Betjeman TJ, Soghoian SE, Foran MP. mHealth in sub-Saharan Africa. Int J Telemed Applic. (2013) 2013:6. doi: 10.1155/2013/482324
11. mHealth Alliance. Leveraging Mobile Technologies to Promote Maternal and New Born Health: The Current Landscape and Opportunities for Advancement in Low Resource Settings. Oakland, CA: Center for Technology & Innovation in Public Health (2012).
12. Oyeyemi SO, Wynn R. The use of cell phones and radio communication systems to reduce delays in getting help for pregnant women in low-and middle-income countries: a scoping review. Glob Health Action. (2015) 8:28887. doi: 10.3402/gha.v8.28887
13. Jo Y, LeFevre AE, Healy K, Singh N, Alland K, Mehra S, et al. Costs and cost-effectiveness analyses of mCARE strategies for promoting care seeking of maternal and newborn health services in rural Bangladesh. PLoS ONE. (2019) 14:e0223004. doi: 10.1371/journal.pone.0223004
14. Linde DS, Korsholm M, Katanga J, Rasch V, Lundh A, Andersen MS. One-way SMS and healthcare outcomes in Africa: systematic review of randomised trials with meta-analysis. PLoS ONE. (2019) 14:e0217485. doi: 10.1371/journal.pone.0217485
15. WHO. mHealth: New Horizons for Health Through Mobile Technologies. Geneva: World Health Organization (2011).
16. Jo Y, Labrique AB, Lefevre AE, Mehl G, Pfaff T, Walker N, et al. Using the lives saved tool (LiST) to model mHealth impact on neonatal survival in resource-limited settings. PLoS ONE. (2014) 9:e102224. doi: 10.1371/journal.pone.0102224
17. Akter S, Ray P. mHealth-an ultimate platform to serve the unserved. Yearb Med Inform. (2010) 2010:94–100. doi: 10.1055/s-0038-1638697
18. Curioso WH, Mechael PN. Enhancing ‘M-health'with south-to-south collaborations. Health Affairs. (2010) 29:264–7. doi: 10.1377/hlthaff.2009.1057
19. Modi D, Dholakia N, Gopalan R, Venkatraman S, Dave K, Shah S, et al. mHealth intervention “ImTeCHO” to improve delivery of maternal, neonatal, and child care services-A cluster-randomized trial in tribal areas of Gujarat, India. PLoS Med. (2019) 16:e1002939. doi: 10.1371/journal.pmed.1002939
20. Tang S, Ghose B, Hoque MR, Hao G, Yaya S. Women using mobile phones for health communication are more likely to use prenatal and post-natal services in Bangladesh: cross-sectional study. Jmir Mhealth and Uhealth. (2019) 7:e10645. doi: 10.2196/10645
21. Benski AC, Schmidt NC, Viviano M, Stancanelli G, Soaroby A, Reich MR. Improving the quality of antenatal care using mobile health in Madagascar: five-year cross-sectional study. Jmir Mhealth and Uhealth. (2020) 8:e18543. doi: 10.2196/18543
22. Adanikin AI, Awoleke JO, Adeyiolu A. Role of reminder by text message in enhancing postnatal clinic attendance. Int J Gynaecol Obstet. (2014) 126:179–80. doi: 10.1016/j.ijgo.2014.02.009
23. Olajubu AO, Fajemilehin BR, Olajubu TO, Afolabi BS. Effectiveness of a mobile health intervention on uptake of recommended postnatal care services in Nigeria. PLoS ONE. (2020) 15:e0238911. doi: 10.1371/journal.pone.0238911
24. Kebede AS, Ajayi IO, Arowojolu AO. Effect of enhanced reminders on postnatal clinic attendance in Addis Ababa, Ethiopia: a cluster randomized controlled trial. Global Health Action. (2019) 12:1609297. doi: 10.1080/16549716.2019.1609297
25. Sondaal SFV, Browne JL, Amoakoh-Coleman M, Borgstein A, Miltenburg AS, Verwijs M, et al. Assessing the effect of mHealth interventions in improving maternal and neonatal care in low-and middle-income countries: a systematic review. PLoS ONE. (2016) 11:e0154664. doi: 10.1371/journal.pone.0154664
26. Amoakoh HB, Klipstein-Grobusch K, Amoakoh-Coleman M, Agyepong IA, Kayode GA, Sarpong C, et al. The effect of a clinical decision-making mHealth support system on maternal and neonatal mortality and morbidity in Ghana: study protocol for a cluster randomized controlled trial. Trials. (2017) 18:157. doi: 10.1186/s13063-017-1897-4
27. Smith V, Devane D, Begley CM, Clarke M. Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Med Res Methodol. (2011) 11:15. doi: 10.1186/1471-2288-11-15
28. Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. (2015) 4:1. doi: 10.1186/2046-4053-4-1
29. Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. (2015) 349:g7647. doi: 10.1136/bmj.g7647
30. Bossman E, Zanaboni P, Johansen M. The post-2015 development agenda: progress towards sustainable development goal target on maternal mortality and child mortality in limited resource settings with mHealth interventions: a systematic review in Sub-Saharan Africa and Southern Asia. PROSPERO. (2019) CRD42019109434. Available online at: https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=109434
31. Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane Handbook for Systematic Reviews of Interventions. 2nd ed. Chichester: John Wiley & Sons (2019). doi: 10.1002/9781119536604
32. Augestad KM, Berntsen G, Lassen K, Bellika JG, Wootton R, Lindsetmo RO, et al. Standards for reporting randomized controlled trials in medical informatics: a systematic review of CONSORT adherence in RCTs on clinical decision support. J Am Med Inform Assoc. (2012) 19:13–21. doi: 10.1136/amiajnl-2011-000411
33. Moher D, Pham B, Jones A, Cook DJ, Jadad AR, Moher M, Tugwell P, Klassen TP. Does quality of reports of randomised trials affect estimates of intervention efficacy reported in meta-analyses? Lancet. (1998) 352:609–13. doi: 10.1016/S0140-6736(98)01085-X
34. Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA. (1995) 273:408–12. doi: 10.1001/jama.273.5.408
35. Colditz GA, Miller JN, Mosteller F. How study design affects outcomes in comparisons of therapy. I: medical. Stat Med. (1989) 8:441–54. doi: 10.1002/sim.4780080408
36. Armijo-Olivo S, Stiles CR, Hagen NA, Biondo PD, Cummings GG. Assessment of study quality for systematic reviews: a comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool: methodological research. J Eval Clin Pract. (2012) 18:12–8. doi: 10.1111/j.1365-2753.2010.01516.x
37. Thomas BH, Ciliska D, Dobbins M, Micucci S. A process for systematically reviewing the literature: providing the research evidence for public health nursing interventions. Worldviews Evid Based Nurs. (2004) 1:176–84. doi: 10.1111/j.1524-475X.2004.04006.x
38. Alam M, D'Este C, Banwell C, Lokuge K. The impact of mobile phone based messages on maternal and child healthcare behaviour: a retrospective cross-sectional survey in Bangladesh. BMC Health Serv Res. (2017) 17:434. doi: 10.1186/s12913-017-2361-6
39. Atnafu A, Otto K, Herbst CH. The role of mHealth intervention on maternal and child health service delivery: findings from a randomized controlled field trial in rural Ethiopia. Mhealth. (2017) 3:39. doi: 10.21037/mhealth.2017.08.04
40. Bangure D, Chirundu D, Gombe N, Marufu T, Mandozana G, Tshimanga M, et al. Effectiveness of short message services reminder on childhood immunization programme in Kadoma, Zimbabwe - a randomized controlled trial, 2013. BMC Public Health. (2015) 15:137. doi: 10.1186/s12889-015-1470-6
41. Brown VB, Oluwatosin OA. Feasibility of implementing a cellphone-based reminder/recall strategy to improve childhood routine immunization in a low-resource setting: a descriptive report. BMC Health Serv Res. (2017) 17(Suppl. 2):703. doi: 10.1186/s12913-017-2639-8
42. Dissieka R, Soohoo M, Janmohamed A, Doledec D. Providing mothers with mobile phone message reminders increases childhood immunization and vitamin A supplementation coverage in Côte d'Ivoire: a randomized controlled trial. J Public Health Afr. (2019) 10:1032. doi: 10.4081/jphia.2019.1032
43. Ekhaguere OA, Oluwafemi RO, Badejoko B, Oyeneyin LO, Butali A, Lowenthal ED, et al. Automated phone call and text reminders for childhood immunisations (PRIMM): a randomised controlled trial in Nigeria. BMJ Glob Health. (2019) 4:e001232. doi: 10.1136/bmjgh-2018-001232
44. Gibson DG, Ochieng B, Kagucia EW, Were J, Hayford K, Moulton LH, et al. Mobile phone-delivered reminders and incentives to improve childhood immunisation coverage and timeliness in Kenya (M-SIMU): a cluster randomised controlled trial. Lancet Glob Health. (2017) 5:E428–38. doi: 10.1016/S2214-109X(17)30072-4
45. Hackett K, Lafleur C, Nyella P, Ginsburg O, Lou W, Sellen D. Impact of smartphone-assisted prenatal home visits on women's use of facility delivery: results from a cluster-randomized trial in rural Tanzania. PLoS ONE. (2018) 13:e0199400. doi: 10.1371/journal.pone.0199400
46. Haji A, Lowther S, Ngan'ga Z, Gura Z, Tabu C, Sandhu H, et al. Reducing routine vaccination dropout rates: evaluating two interventions in three Kenyan districts, 2014. BMC Public Health. (2016) 16:152. doi: 10.1186/s12889-016-2823-5
47. Kazi AM, Ali M, Zubair K, Kalimuddin H, Kazi AN, Iqbal SP, et al. Effect of mobile phone text message reminders on routine immunization uptake in pakistan: randomized controlled trial. JMIR Public Health Surveill. (2018) 4:e20. doi: 10.2196/publichealth.7026
48. Lund S, Hemed M, Nielsen BB, Said A, Said K, Makungu MH, et al. Mobile phones as a health communication tool to improve skilled attendance at delivery in Zanzibar: a cluster-randomised controlled trial. Bjog. (2012) 119:1256–64. doi: 10.1111/j.1471-0528.2012.03413.x
49. Lund S, Nielsen BB, Hemed M, Boas IM, Said A, Said K, et al. Mobile phones improve antenatal care attendance in Zanzibar: a cluster randomized controlled trial. BMC Pregn Childb. (2014) 14:29. doi: 10.1186/1471-2393-14-29
50. Lund S, Rasch V, Hemed M, Boas IM, Said A, Said K, et al. Mobile phone intervention reduces perinatal mortality in zanzibar: secondary outcomes of a cluster randomized controlled trial. JMIR Mhealth Uhealth. (2014) 2:e15. doi: 10.2196/mhealth.2941
51. Lund S, Boas IM, Bedesa T, Fekede W, Nielsen HS, Sorensen BL. Association between the safe delivery app and quality of care and perinatal survival in ethiopia: a randomized clinical trial. JAMA Pediatr. (2016) 170:765–71. doi: 10.1001/jamapediatrics.2016.0687
52. Murthy N, Chandrasekharan S, Prakash MP, Kaonga NN, Peter J, Ganju A, et al. The impact of an mHealth Voice Message Service (mMitra) on infant care knowledge, and practices among low-income women in india: findings from a pseudo-randomized controlled trial. Matern Child Health J. (2019) 23:1658–69. doi: 10.1007/s10995-019-02805-5
53. Murthy N, Chandrasekharan S, Prakash MP, Ganju A, Peter J, Kaonga N, et al. Effects of an mHealth voice message service (mMitra) on maternal health knowledge and practices of low-income women in India: findings from a pseudo-randomized controlled trial. BMC Public Health. (2020) 20:820. doi: 10.1186/s12889-020-08965-2
54. Nagar R, Venkat P, Stone LD, Engel KA, Sadda P, Shahnawaz M. A cluster randomized trial to determine the effectiveness of a novel, digital pendant and voice reminder platform on increasing infant immunization adherence in rural Udaipur, India. Vaccine. (2018) 36:6567–77. doi: 10.1016/j.vaccine.2017.11.023
55. Odeny TA, Bukusi EA, Cohen CR, Yuhas K, Camlin CS, McClelland RS. Texting improves testing: a randomized trial of two-way SMS to increase postpartum prevention of mother-to-child transmission retention and infant HIV testing. AIDS. (2014) 28:2307–12. doi: 10.1097/QAD.0000000000000409
56. Oyeyemi SO, Wynn R. Giving cell phones to pregnant women and improving services may increase primary health facility utilization: a case-control study of a Nigerian project. Reprod Health. (2014) 11:8. doi: 10.1186/1742-4755-11-8
57. Seth R, Akinboyo I, Chhabra A, Qaiyum Y, Shet A, Gupte N, et al. Mobile phone incentives for childhood immunizations in rural India. Pediatrics. (2018) 141:e20173455. doi: 10.1542/peds.2017-3455
58. Shiferaw S, Spigt M, Tekie M, Abdullah M, Fantahun M, Dinant G-J. The effects of a locally developed mHealth intervention on delivery and postnatal care utilization; a prospective controlled evaluation among health centres in Ethiopia. PLoS ONE. (2016) 11:e0158600. doi: 10.1371/journal.pone.0158600
59. Zegeye B, Ahinkorah BO, Ameyaw EK, Budu E, Seidu AA, Olorunsaiye CZ, et al. Disparities in use of skilled birth attendants and neonatal mortality rate in Guinea over two decades. BMC Pregn Childb. (2022) 22:56. doi: 10.1186/s12884-021-04370-8
60. World Health Organization. Definition of skilled health personnel providing care during childbirth: the 2018 joint statement by WHO, UNFPA, UNICEF, ICM, ICN, FIGO and IPA (No. WHO/RHR/18.14). World Health Organization (2018). Available online at: https://www.who.int/publications/i/item/WHO-RHR-18.14 (accessed August 10, 2022).
61. UNICEF. Global Delivery Care Coverage and Trends. Percentage of Births Assisted by a Skilled Birth Attendant, by Country, 2019. UNICEF (2014). Available online at: https://data.unicef.org/topic/maternal-health/delivery-care/
62. Ban K. United Nations. The Millennium Development Goals Report 2010. New York: United Nations; 2010. Contract No: Document Number.
63. Lester RT, Ritvo P, Mills EJ, Kariri A, Karanja S, Chung MH, et al. Effects of a mobile phone short message service on antiretroviral treatment adherence in Kenya (WelTel Kenya1): a randomised trial. Lancet. (2010) 376:1838–45. doi: 10.1016/S0140-6736(10)61997-6
64. Fjeldsoe BS, Marshall AL, Miller YD. Behavior change interventions delivered by mobile telephone short-message service. Am J Prev Med. (2009) 36:165–73. doi: 10.1016/j.amepre.2008.09.040
65. Regassa N. Antenatal and postnatal care service utilization in southern Ethiopia: A population-based study. Afr Health Sci. (2011) 11:390–7.
66. Darmstadt GL, Bhutta ZA, Cousens S, Adam T, Walker N, de Bernis L; Lancet Neonatal Survival Steering Team. Evidence-based, cost-effective interventions: how many newborn babies can we save? Lancet. (2005) 365:977–88. doi: 10.1016/S0140-6736(05)71088-6
67. Doku DT, Neupane S. Survival analysis of the association between antenatal care attendance and neonatal mortality in 57 low- and middle-income countries. Int J Epidemiol. (2017) 46:1668–77. doi: 10.1093/ije/dyx125
68. Arunda M, Emmelin A, Asamoah BO. Effectiveness of antenatal care services in reducing neonatal mortality in Kenya: analysis of national survey data. Glob Health Action. (2017) 10:1328796. doi: 10.1080/16549716.2017.1328796
70. WHO. WHO Recommended Interventions for Improving Maternal and Newborn Health: Integrated Management of Pregnancy and Childbirth. Geneva: World Health Organization (2007).
71. Patel A, Khatib MN, Kurhe K, Bhargava S, Bang A. Impact of neonatal resuscitation trainings on neonatal and perinatal mortality: a systematic review and meta-analysis. BMJ Paediatr Open. (2017) 1:e000183. doi: 10.1136/bmjpo-2017-000183
72. WHO. Proportion of Births Attended by a Skilled Attendant: 2008 Updates. Geneva: World Health Organization (2008).
73. Guerrera G. Neonatal and pediatric healthcare worldwide: a report from UNICEF. Clin Chim Acta. (2015) 451(Pt A):4–8. doi: 10.1016/j.cca.2015.03.004
74. United Nations Inter-agency Group for Child Mortality Estimation. Levels & Trends in Child Mortality: Report 2017. New York, NY: United Nations Children's Fund (2017).
75. Kc A, Nelin V, Raaijmakers H, Kim HJ, Singh C, Målqvist M. Increased immunization coverage addresses the equity gap in Nepal. Bull World Health Organ. (2017) 95:261–9. doi: 10.2471/BLT.16.178327
76. Jit M, Dang TT, Friberg I, Hoang VM, Pham Huy TK, Walker N, et al. Thirty years of vaccination in Vietnam: impact and cost-effectiveness of the national Expanded Programme on Immunization. Vaccine. (2015) 33(Suppl. 1):A233–9. doi: 10.1016/j.vaccine.2014.12.017
77. (UNIGME) UNI-aGfCME. ‘Levels & Trends in Child Mortality: Report 2018, Estimates developed by the United Nations Inter-agency Group for Child Mortality Estimation. New York, NY: United Nations Children's Fund (2018).
Keywords: mHealth, maternal health, child health, antenatal care, post-natal care, Sustainable Development Goals, low and middle-income countries
Citation: Bossman E, Johansen MA and Zanaboni P (2022) mHealth interventions to reduce maternal and child mortality in Sub-Saharan Africa and Southern Asia: A systematic literature review. Front. Glob. Womens Health 3:942146. doi: 10.3389/fgwh.2022.942146
Received: 18 May 2022; Accepted: 03 August 2022;
Published: 25 August 2022.
Edited by:
Tabassum Firoz, Yale New Haven Health System, United StatesReviewed by:
Elissa Z. Faro, University of Iowa Health Care, United StatesBeth Payne, University of British Columbia, Canada
Copyright © 2022 Bossman, Johansen and Zanaboni. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Paolo Zanaboni, cGFvbG8uemFuYWJvbmlAZWhlYWx0aHJlc2VhcmNoLm5v
 Elvis Bossman
Elvis Bossman Monika A. Johansen1,2
Monika A. Johansen1,2 Paolo Zanaboni
Paolo Zanaboni