- Department of Midwifery, College of Medicine and Health Sciences, Salale University, Fitche, Ethiopia
Background: Cervical cancer screening is a means of detecting cervical cancer early, before it develops, in order to reduce disease mortality and morbidity. When women are screened for cervical cancer between the ages of 30 and 40 years at least one time in their life, their risk of cancer could be decreased by 25–36%. Despite this advantage, cervical cancer screening coverage in Ethiopia is still <2%. As a result, we wanted to see how ready women in the Girar Jarso district, Ethiopia, were to get a cervical cancer test.
Methodology: Community-based cross-sectional study was done using a stratified cluster sampling technique among 855 women aged 30–65 years in the Girar Jarso district, Ethiopia, from 1 June 2021 to 1 September 2021. A pretested and semi-structured interviewer-administered questionnaire was used to collect the data. EpiData management version 4.6 was used to enter data, which was then exported to SPSS version 23 for analysis. Logistic regression analysis was performed, and variables with a p-value of <0.05 were taken as statistically significant predictors of the willingness to utilize cervical cancer screening.
Results: Of the 855 women, only 315 (46.7%, CI = 43–50.3) women were willing to be checked for cervical cancer, with 181 (21.2%) women having been screened at least one time in their life. Age of 30–39 years [AOR = 2.80 (95% CI: 1.05, 7.48)], urban resident [AOR = 2.12 (95% CI: 1.06, 4.48)], positive attitude [AOR = 1.68 (95% CI: 1.11, 2.53)], wealth status, awareness of cervical cancer, and low perceived barriers were independent predictors of the willingness to utilize cervical cancer screening.
Conclusion and recommendation: The willingness to utilize cervical cancer screening services is low in the Girar Jarso district. To improve community awareness and attitude, continued and sustainable advocacy on the value of cervical cancer screening should be offered through mass media and health extension workers.
Introduction
Approximately 570,000 cases and 311,000 deaths from cervical cancer are reported each year worldwide, making it the leading cause of death and illness among women (1). Global trends show that, in developing countries going through rapid societal and economic changes, the shift toward lifestyles like that of industrialized countries leads to a rising burden of any type of cancer (2). There is a large difference between developing and developed countries, where cervical cancer cases have been significantly reduced since the implementation of effective screening programs (3). China's cervical cancer screening rate and willingness were found to be 35.1 and 82.22%, respectively (4).
In Africa, cervical cancer is the second highest type of cancer occurring among women with an estimated 119,284 new cases and 81,687 fatalities each year, showing an increasing trend (5). In developed countries, programs exist that allow girls to be vaccinated against HPV and women to get screened regularly and treated appropriately on a regular basis, whereas in low- and middle-income countries (LMICs), access to these preventative measures is limited, and the disease is often unappreciated until it has progressed to its final stage (6). Although there was a high level of readiness to have a cervical cancer screening, the rate of screening is still low. Sub-Saharan Africa, for instance, has a strong propensity to use screening (7, 8).
In Ethiopia, over 6,294 new cases and 4,884 deaths occur each year, making it the second greatest cause of mortality following breast cancer, and the lion's share was among women aged 30–65 years, accounting for 79% of new cases and 65.8% of deaths per year (5). The prevalence and fatality rate in Ethiopia could probably be significantly higher than what was reported in a meta-analysis study given the sparse amount of data currently available (9). HPV vaccination and cytological screening programs can prevent cervical cancer, but these services are insufficient in LMICs, particularly in sub-Saharan Africa, including Ethiopia, where the issues are still devastating due to a lack of resources and a weak healthcare system, making cervical cancer screening opportunistic rather than planned. The chance of developing cancer can be decreased by 25–36% in women between the ages of 30 and 40 years who undergo a cervical cancer evaluation one time in their life (2–4). According to a study conducted in several regions of Ethiopia, women in the Ethiopian army (43.4%), Debre Berhan Town (45.3%) (6), and Addis Ababa (62.7%) (7) expressed a willingness to get a cervical cancer screening.
According to research, Ethiopia's prevalence of cervical cancer screening for disease prevention is low, at around 2% nationwide (4). The Federal Ministry of Health launched visual inspection with acetic acid (VIA) screening in conjunction with access to cryotherapy (7) at 800 healthcare facilities in order to increase the screening coverage by more than 80%. Furthermore, not only was a cancer registry established in several areas of the country, including the study area, to lessen the effects of cervical cancer, to promote cancer surveillance, and to register and research cervical cancer but also media campaign was made many times and is still in progress. As a result, a total of 22,818 women between the ages of 30–49 years underwent cervical cancer screening in 2015 (4, 8).
Despite the efforts made to increase cervical cancer screening, the rate of screening is still low. As a result, the purpose of this research is to learn about the community's willingness in the study area. To the best of our knowledge, no research has been done on the willingness to utilize cervical cancer screening among women aged 30–65 years, where the disease is most prevalent. This study is the first in the Girar Jarso district to assess the prevalence of willingness to utilize cervical cancer screening among women aged 30–65 years and to identify factors associated with the discovered prevalence.
Methods and materials
Study design and setting
A community-based cross-sectional study was conducted in the Girar Jarso district of North Shoa zone, Oromia region, Ethiopia, from 1 June 2021 to 1 September 2021. All women between the ages of 30 and 65 years who lived in specified kebeles for at least 6 months were included in this study. Individuals who were seriously ill (unable to provide correct and required information) were not allowed to participate.
Sample size and sampling technique
The sample size was calculated using the proportion of women willing to be screen for cervical cancer (62.7%) (7), a standard score of 95% CI and a 5% margin of error, and a 10% nonresponse rate. After adding the design effect, a total sample size of 790 was determined. A stratified cluster sampling technique was employed. The Girar Jarso district is divided into two sections, namely, urban and rural. Five rural clusters and one urban cluster were chosen at random from 21 kebeles, and all households within those clusters were included in the study. Finally, each home in each of the selected kebeles was interviewed consequently. When there was more than one eligible woman in a home, one was chosen at random using the lottery technique. Women between the ages of 30 and 65 years were interviewed in the selected kebeles. When an eligible participant was not at home, data collectors returned to the household at different time intervals or used a different method (i.e., phone calls after his/her first journey if available), and interviewers were given the option of collecting data after working hours and on weekends if they were unable to locate the eligible participant. If interviewers were unable to locate the eligible participant, the household was marked as a nonresponse.
Data collection tools and procedures
Data were collected using an interviewer-administered questionnaire. A questionnaire was adopted from related literature (7, 8, 10), and it was translated into Afaan Oromo and then back to English to ensure consistency. Before real data collection, the translated questionnaires were pretested, and a few questions were modified after discussion with the study teams. Age, residence, marital status, religion, education status, occupation, income, and health insurance were among the sociodemographic data. Contraceptive use, history of STIs, sero-HIV status, age of sexual intercourse, parity, duration of the marriage, and history of gynecologic examination are among the reproductive-related factors. Cervical cancer screening attitudes, knowledge, and barriers to utilize were also included.
Willingness to be screened for cervical cancer is defined as a woman who is willing to be tested and has decided to be screened in the coming year but has never been screened previously (10). Those who had never screened for cervical cancer over their lives were regarded as never screened, while those who had screened at least one time were considered as screened. Eight attitude questions about cervical cancer and screening were presented and measured on a Likert scale (1 = “Strongly disagree”; 2 = “Disagree”; 3 = “Neutral”; 4 = “Agree”; and 5 = “Strongly agree”). Then, those who scored mean and above were categorized as having a “positive attitude” and those who scored below the mean were categorized as having a “negative attitude.” Eighteen knowledge questions about cervical cancer and screening were presented, and the correct answer scored 1 and the incorrect answer scored 0. The total points to be scored were 18, and the minimum was 0. Then, those who scored mean and above were categorized as having “good knowledge” and those who scored below the mean were categorized as having “poor knowledge.” Nineteen perceived barriers questions about cervical cancer and screening were presented and measured on a Likert scale (1 = “Strongly disagree”; 2 = “Disagree”; 3 = “Neutral”; 4 = “Agree”; and 5 = “Strongly agree”). Then, those who scored mean and above were categorized as having a “high perceived barrier” and those who scored below the mean were categorized as having a “low perceived barrier” (9). To examine the internal consistency of distinct items, Cronbach's alpha coefficients were calculated. Nineteen items with a Cronbach's alpha of 0.95 were used to assess perceived barriers. Attitudes were also measured by eight items with Cronbach's alpha of 0.800 and 0.76 for knowledge of cervical cancer and screening.
Data processing and analysis
Data were double-checked, coded, and entered into EpiData version 4.6 before being exported to SPSS (Statistical Package for Social science) version 23 for analysis. Tables, graphs, and frequency were utilized to portray the data in the descriptive statistics tables. Binary logistic regression was fitted to identify factors associated with the willingness to utilize cervical cancer screening. Variables with a p-value of <0.25 were identified and fitted to multivariable logistic regression. Variables scoring a p-value of <0.05 at 95% CI were considered significant. Variance inflation factors (VIF) were utilized to screen for multicollinearity, and a VIF of <10 was employed as a cutoff point to diagnose multicollinearity. A p-value of >0.05 was used to indicate the model fit using the Hosmer and Lemeshow model's goodness-of-fit test.
Results
Background characteristics
In this study, 855 participants were involved; among them, 597 (60.9%) participants were from rural areas, and 383 (48.8%) participants were between the ages of 30 and 39 years. Approximately 643 (75%) respondents practiced the orthodox religion. Of the participants in the interview, seven hundred forty-seven (87.4%) were married, and among them, 443 (51.8%) were housewives. In total, four hundred ninety-six (58%) participants had health insurance. Of the female participants, two hundred eighty-six (33.5%), or roughly one-third of them, attended primary school. Among all respondents, 200 (23.4%) households were in the middle quintile in terms of wealth (Table 1).
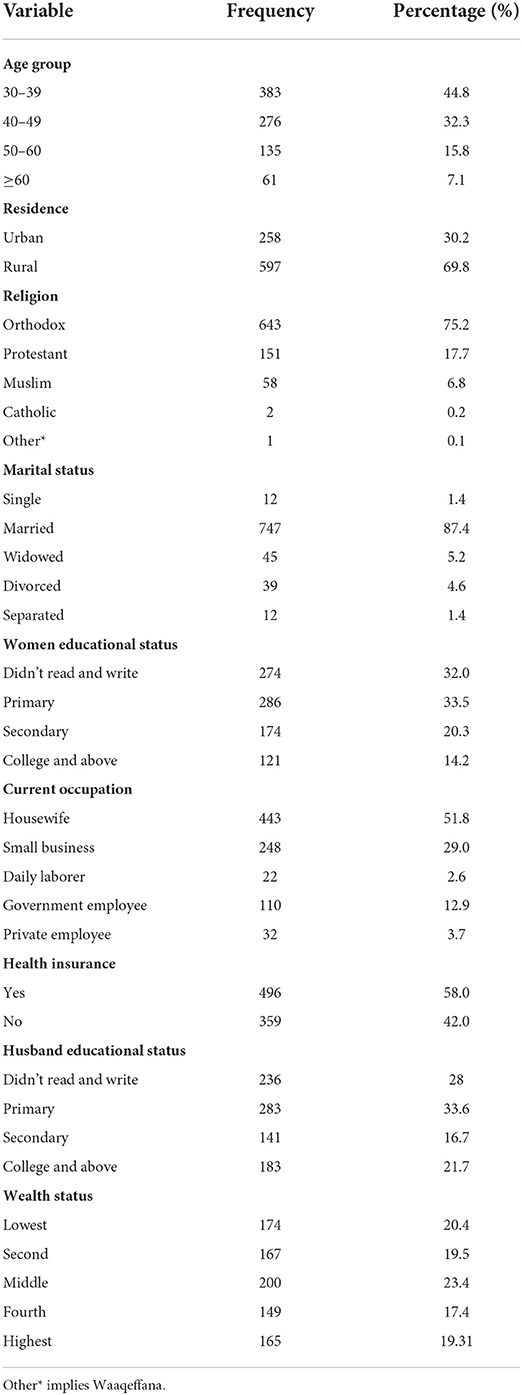
Table 1. Sociodemographic characteristics of women aged 30–65 years in the Girar Jarso district, Ethiopia (N = 855) during January 2022.
Reproductive characteristics
Of the 855 respondents, 485 (56.7%) got married before the age of 20 years, and 531 (63.5%) had at least one child, with 457 (55.6%) respondents using a modern form of contraception. An HIV test was administered to more than 800 people (87.5%), and 684 of them (81.5%) received a negative result; 591 (69%) participants had their first sexual experience before turning 20 years of age (Table 2).
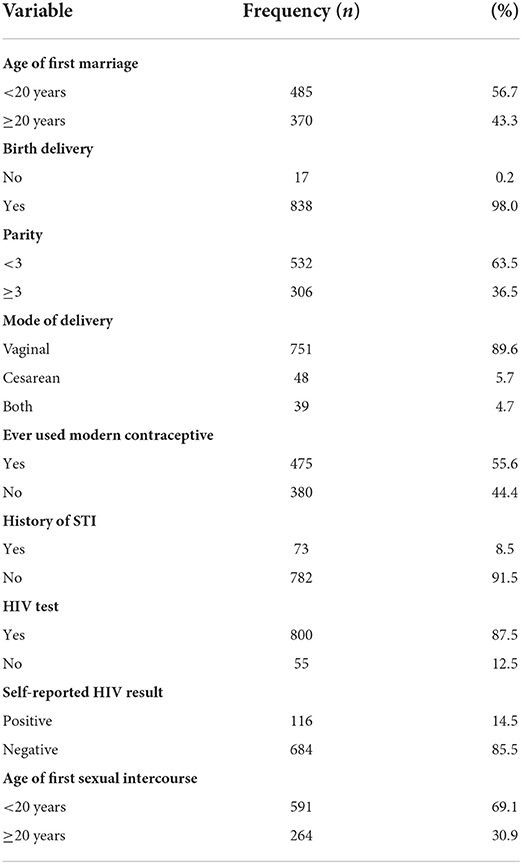
Table 2. Reproductive characteristics among women aged 30–65 years in the Girar Jarso district, Ethiopia (N = 855) during January 2022.
Awareness of cervical cancer screening
Of the respondents, four hundred fifty-nine (53.7%) had heard about cervical cancer. Among those participants who heard about cervical cancer, half (459, 53.7%) of them responded that cervical cancer is preventable and one-fourth (247, 28.9%) of them reported that it is a communicable disease, whereas only 381 (44.6%) of the participants had heard about cervical cancer screening and only 289 (33.8%) of the participants knew where the screening center is located (Table 3). The primary source of information for the respondents was health workers (216, 48.9%), followed by television (203, 46.9%) (Figure 1).
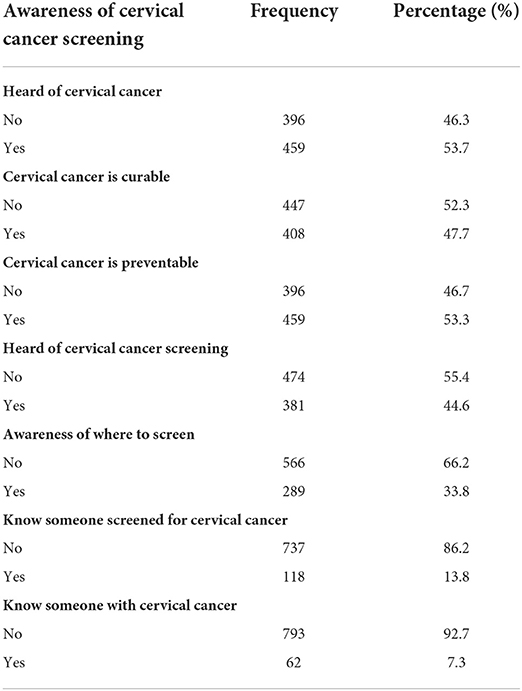
Table 3. Awareness of cervical cancer screening among women aged 30–65 years in the Girar Jarso district, Ethiopia (N = 855) during January 2022.
Knowledge of cervical cancer and screening
Among those who ever heard about cervical cancer, only 353 (41.3%) participants had good knowledge. Only 125 (33%) and 123 (24.5%) of those with good knowledge were willing to use and had utilized cervical cancer screening at least one time in their lives, respectively (Figure 2).
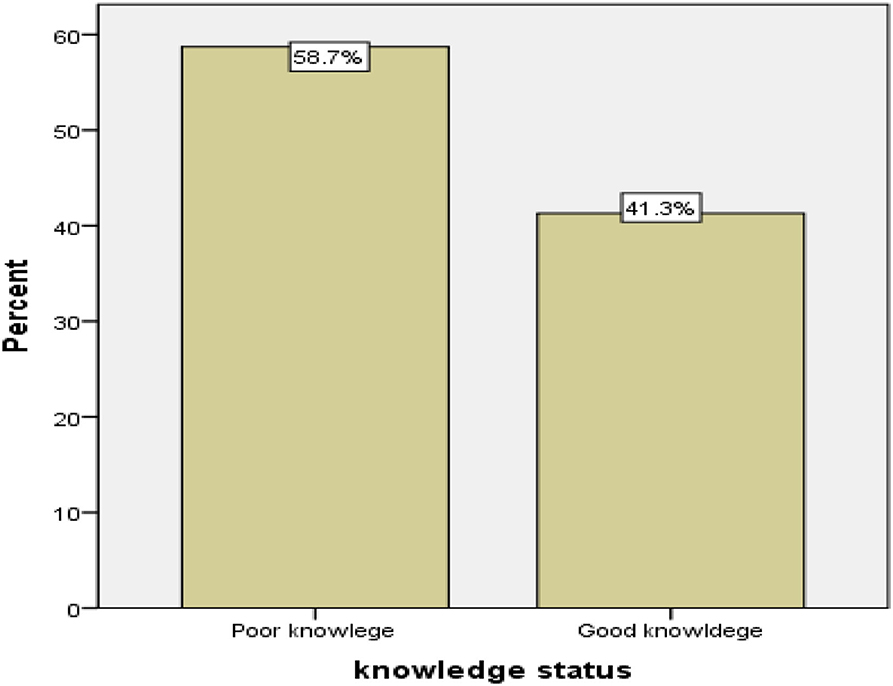
Figure 2. Knowledge of cervical cancer and screening service utilization among women aged 30–36 years in the Girar Jarso district, Ehiopia during January 2022.
Attitude and barriers toward cervical cancer screening
Of the current respondents, four hundred seventy-four (55.4%) had a positive attitude, and two-thirds (65.4%) of those who had a good attitude were willing to be examined for cervical cancer. Of all the study participants, 455 (53.2%) had low perceived barriers, and nearly two-thirds (65.1%) of those respondents were willing to uptake cervical cancer screening.
The prevalence of willingness to utilize cervical cancer screening
Only 315 (46.7%) respondents who had never screened for cervical cancer were willing to do so, whereas only 181 (21.2%) respondents had been screened for cervical cancer at least one time in their lives. Women were unwilling to be examined for cervical cancer because they felt healthy (73.7%), were shy, were afraid of a positive result, did not know about the service, believed that screening was expensive, and did not have permission from their husbands.
Factors associated with the willingness to utilize cervical cancer screening
The results of the bivariable and multivariable logistic regressions are documented in Table 4. In a b-ivariable analysis, place of residence; age; current occupation of women; husband's educational status; having health insurance; the age of first marriage; parity; modern contraceptive use; duration of contraceptive use; self-reported HIV test; the age of first sexual intercourse; aware that cervical cancer is preventable, communicable, and killer; perceived barriers; wealth status of the respondent; attitude; knowledge about cervical cancer; and screening were found to be associated with the willingness to utilize cervical cancer screening (p < 0.25).
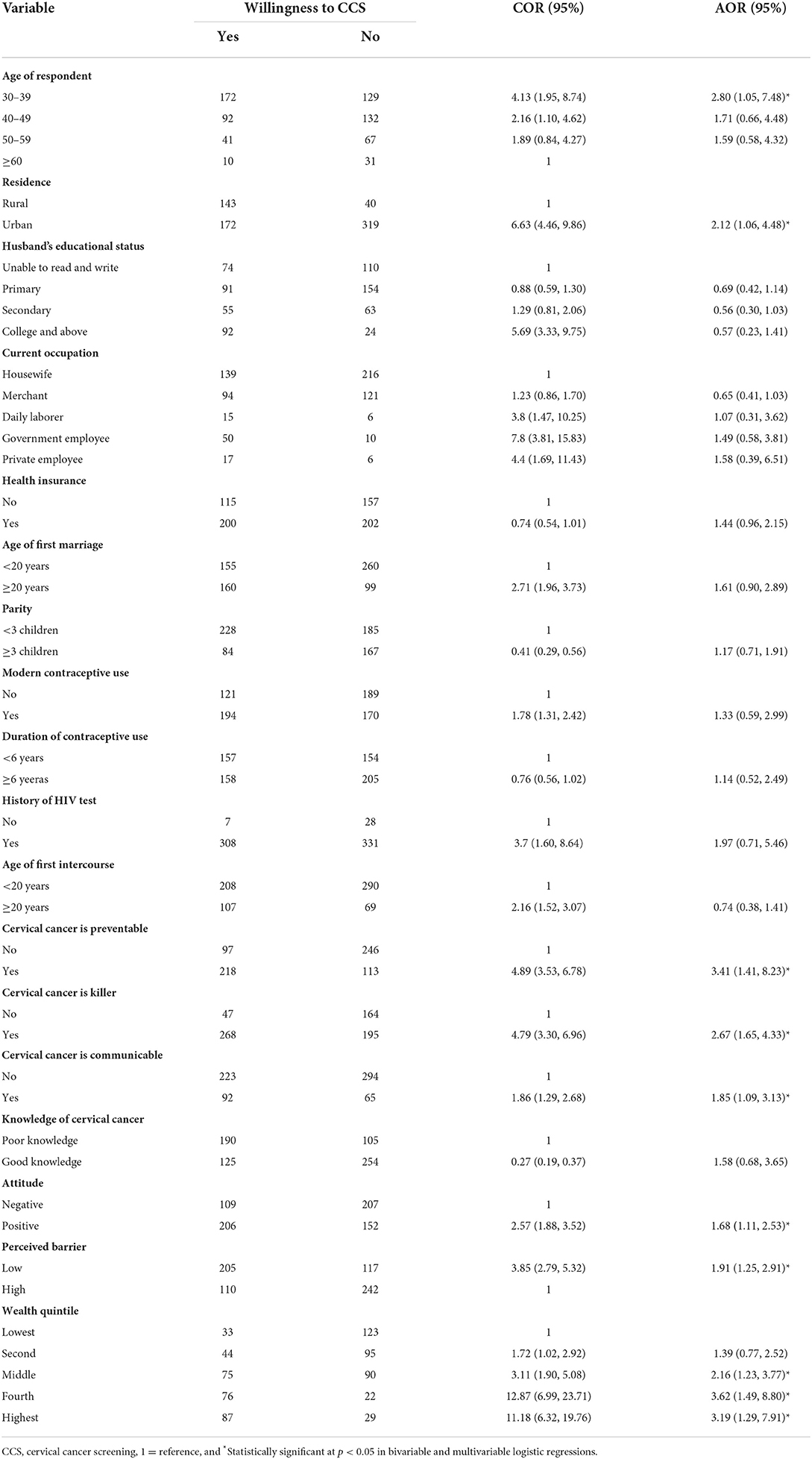
Table 4. Factors associated with the willingness to utilize cervical cancer screening service among women aged 30–65 years in the Girar Jarso district, Ethiopia during January 2022.
In a multivariable analysis, women's age, residence, attitude, awareness of cervical cancer, perceived barrier, and wealth status of the respondent were found to be independently significant. All women aged 30–49 years were 2.8 times more willing to be screened for cervical cancer as compared with those ≥60 years (AOR = 2.80; 95% CI: 1.05, 7.48). Urban residents were 2.12 times more willing for cervical screening compared with rural residents (AOR = 2.12; 95% CI: 1.06, 4.48). Women who were aware that cervical cancer is preventable had an AOR of 3.41; 95% CI: 1.41, 8.23, women who were aware that cervical cancer is a killer had an AOR of 2.67; 95% CI: 1.65, 4.33, and women who were aware that cervical cancer is communicable had an AOR of 1.85; 95% CI: 1.09, 3.13. Women who had a positive attitude toward the willingness to utilize cervical cancer screening were 1.68 times more likely compared with those who had a negative attitude (AOR = 1.68; 95% CI: 1.11, 2.53). Women who had low perceived barriers toward cervical cancer screening were two timesmore willing compared with those who had high perceived barriers (AOR = 1.91; 95% CI: 1.25, 2.91). Finally, factors such as women who were in the middle (AOR = 2.16; 95% CI: 1.23, 3.77), fourth (AOR = 3.62;95%CI:1.49,8.80), and high estquintile (wealthiest) [AOR = 3.19;95%CI:(1.29,7.91)] were found to increase willingness to utilize cervical cancer screening.
Discussion
This study aimed to assess the willingness to utilize cervical cancer screening among women aged 30–65 years in the Girar Jarso district, Ethiopia. Accordingly, the prevalence of willingness to utilize cervical cancer screening was found to be 46.7% (95% CI: 43, 50.3).
Our results were consistent with the research done among Ethiopian army women (43.4%) (11) and among women in Debre Berhan town (45.3%) (6), where screening for cervical cancer was offered to participants. However, this result was lower than that of studies conducted in Addis Ababa, Ethiopia (62.7%) (7); Nigeria [three studies−73.6% (10), 86.7% (12), and 88.9% (13), respectively]; Mozambique (86%) (14); and South America (88.9%) (15) among Latino immigrants. This discrepancy may be explained by a number of sociodemographic factors, including a person's perception of their own health or their ignorance of the services offered by a health facility. In fact, nearly a third of our respondents (73.7%) expressed feeling healthy and their reluctance to get an examination. Additionally, 58.7% of participants had inadequate knowledge, and 18.9% of women were unaware of the service. The outcome of this study, however, was higher than those of two studies done in India [32% (16) and 20% (17), respectively]. This discrepancy may be attributed to varying study populations, study periods, and cultural variables that make it challenging for the community to accept cervical cancer screening.
Women aged 30–39 years were found to be more willing to be screened for cervical cancer than women aged ≥60 years. This conclusion was consistent with a Tanzanian study that found younger age (30–39 years) was substantially associated with the willingness to screen (11) when compared with other age groups. This could be related to the high-level of education attainment. In fact, those aged 30–39 years had a higher educational attainment level (21.1%) than those aged 60 and above years (7.1%). As the 30–39 age group represents the reproductive age for most women in a resource-constrained environment, the high readiness to screen for cervical cancer may be attributable to more frequent exposure to reproductive services and care than women in other age groups. Furthermore, the cervical cancer screening guideline in Ethiopia encourages women aged 30–49 years to be screened for cervical cancer, and women in this age group may have better knowledge and intention to be screened than women in other age groups (12). Moreover, this age group is a productive age with the possibility of receiving more gynecological examinations, giving birth, and receiving more health information about reproductive health, including cervical cancer, which promotes screening services and may give more readiness to receive screening.
To rule out the contribution of the current address on the willingness to screen for cervical cancer, we included sociodemographic characteristics in our model. According to our findings, participants in the urban area were 2.12 times more willing to be examined than in the rural area. Our findings were compared with those reported in a Tanzanian study (11). One possible explanation is that women who live in cities have easy access to information from various sources such as the media and health centers. This argument was reinforced by a Ugandan study that found that women who lived in urban areas had a higher knowledge of cervical cancer (13). Women who live in cities have easier access to healthcare than women who live in rural areas. Residing in a rural area is a risk factor because cervical cancer screening in Ethiopia is done by a few public hospitals that are mainly located in urban areas.
The wealth status of the study participants was also another strong predictor of the willingness to utilize cervical cancer screening services. In comparison with those in the lowest quintile, women in the middle, fourth, and highest quintiles were substantially related to their willingness to get screened for cervical cancer. This report was consistent with the study report from Ethiopia (14), Tanzania (15), and two studies from China (4, 16). These findings might be unsurprising because people of high socioeconomic class are likely to be concerned about their health even before they show signs and symptoms and they are unconcerned about the cost of screening. They can also travel long distances for screening by transportation. This may be because those having more income have additional money to allocate for the promotion of their health in addition to meeting their basic needs. Studies conducted in Addis Ababa (17), Malaysia (18), Iran (19), and Korea (20) for different healthcare services support this conclusion. There was a result that people with a higher income were more aware of cervical cancer, implying that there was a link (21).
According to a study from Addis Ababa, Ethiopia (7), and Nigeria (10), there was a substantial link between cervical cancer awareness and the willingness to utilize cervical cancer screening. Similarly, in this study, participants who were aware that cervical cancer is communicable, killer, and preventable were found to be substantial predictors of the willingness to utilize cervical cancer screening compared with those who were unaware. This could be explained by participants who were aware of cervical cancer in general, meaning that those who reported cervical cancer as a killer, communicable disease, and preventable disease were concerned, fearful, and wanted to be screened. Another possible explanation is that a respondent who is aware is more likely to be aware of the benefits and choose it. It is possible that public awareness is being raised as a result of a mass media campaign focusing on a certain component of the problem.
When compared with women who had a negative attitude toward cervical cancer screening, those who had a positive attitude were found to be substantially related. Similarly, we observed that attitudes regarding cervical cancer screening were important determinants affecting willingness in reports from the United States (22), Canada (23), and Ethiopia (6). The likely rationale is that participants with a favorable attitude regarding cervical cancer screening may be able to change thoughts and minimize or discard reluctance of their own beliefs, increasing the likelihood of being willing to utilize cervical cancer screening.
Another variable that predicted the willingness to utilize cervical cancer screening was the perceived barrier. Women who thought there were low barriers to cervical cancer screening were more likely to use it than those who thought there were many. This finding is compared with a recent study in China (24) and Uganda (25), which found that a personal barrier, such as feeling apprehensive if the screening revealed discomfort, could be a negative inducement for screening attendance. Other barriers include social barriers such as fear of being screened because it is considered immoral, not being recommended by family to undergo screening, of fear of others learning their results, and husband's refusal to allow, as well as facility barriers such as preferring female doctors, not having a health facility close to home, and having to wait a long time to have screening. Low barrier denotes that there is a low facility barrier or a high density of health institutions, and satisfactory outreach activities are held in the district. This could be explained by women's view of their own vulnerability to illness, and if they perceived that they are prone to cancer of the cervix, they seek screening and medical care to protect themselves.
Strengths and limitations of the study
We identified different factors associated with the willingness to utilize cervical cancer screening, including the rural community, which makes it the first study of its kind because most previous studies focused on urban institutions and making population inferences. On the contrary, some factors may be subject to social desirability bias; however, we trained female data collectors to eliminate this as much as possible. Due to its cross-sectional character, it does not show a causal relationship.
Conclusion
The willingness of women aged 30–65 years to utilize cervical cancer screening was found to be low in this study. Age; residing in a city; knowing that cervical cancer is preventable, killer, and communicable; having a positive attitude; having a low perceived barrier; and being in the middle, fourth, or highest quintile were all predictors of the willingness to utilize cervical cancer screening programs. As a result, through various media and health extension workers, efforts should be made to raise community awareness and attitude. Furthermore, to influence community beliefs about cervical cancer screening, a community-based screening program should be established and implemented with the help of key national partners and organizations.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics statement
Letter of ethical clearance and approval was obtained from Salale University Ethical Review Committee. The patients/participants provided their written informed consent to participate in this study.
Author contributions
All authors made a significant contribution to the conception, study design, execution, acquisition of data, analysis, and interpretation. All authors were involved in drafting, revising, or critically reviewing the article, gave final approval of the version to be published, have agreed on the journal to which the article has been submitted, and agreed to be accountable for all aspects of the work.
Acknowledgments
We would like to acknowledge Salale University for giving the chance to conduct this study. We want to express our appreciation to the Girar Jarso District Health Bureau, data collectors, supervisors, and participants of this study for their help and willingness.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AOR, adjusted odds ratio; CCS, cervical cancer screening; COR, crude odds ratio; HIV, human immunodeficiency virus; HPV, human papillomavirus; LMICs, low and middle-income countries; STI, sexually transmitted infection; VIA, visual inspection with acetic acid; VIF, variance of inflation factor.
References
1. WHO. Cervical Cancer. (2020). Available from: https://www.who.int/news-room/fact-sheets/detail/human-papillomavirus-(hpv)-and-cervical-cancer (accessed January 28, 2022).
3. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2021) 71:209–49. doi: 10.3322/caac.21660
4. Lin W, Chen B, Wu B, Yuan S, Zhong C, Huang W, et al. Cervical cancer screening rate and willingness among female migrants in Shenzhen, China: three-year changes in citywide surveys. Cancer Res Treat. (2020) 53:212–22. doi: 10.4143/crt.2020.219
5. Bruni L, Albero G, Serrano B, Mena M, Gómez D, Muñoz J, et al. ICO/IARC. Human Papillomavirus Related Diseases in Africa: Summary Report 17 June 2019. (2019). Available from: https://hpvcentre.net/statistics/reports/XFX.pdf (accessed December 30, 2019).
6. Getahun T, Kaba M, Derseh BT. Intention to screen for cervical cancer in Debre Berhan Town, Amhara Regional State, Ethiopia: application of theory of planned behavior. J Cancer Epidemiol. (2020) 2020:e3024578. doi: 10.1155/2020/3024578
7. Belete N, Tsige Y, Mellie H. Willingness and acceptability of cervical cancer screening among women living with HIV/AIDS in Addis Ababa, Ethiopia: a cross sectional study. Gynecol Oncol Res Pract. (2015) 2:6. doi: 10.1186/s40661-015-0012-3
8. Cunningham MS, Skrastins E, Fitzpatrick R, Jindal P, Oneko O, Yeates K, et al. Cervical cancer screening and HPV vaccine acceptability among rural and urban women in Kilimanjaro Region, Tanzania. BMJ Open. (2015) 5:e005828–e005828. doi: 10.1136/bmjopen-2014-005828
9. Nigussie T, Admassu B, Nigussie A. Cervical cancer screening service utilization and associated factors among age-eligible women in Jimma town using health belief model, South West Ethiopia. BMC Womens Health. (2019) 19:127. doi: 10.1186/s12905-019-0826-y
10. Ndikom C. Willingness to utilize cervical cancer screening services among, antenatal clinic attendees in selected hospitals in Ibadan, Nigeria. J Womens Health Issues Care. (2014) 3:3. doi: 10.4172/2325-9795.1000149
11. New-Aaron M, Meza JL, Goedert MH, Kibusi SM, Mkhoi ML, Mayengo CD, et al. Cervical cancer screening among women receiving antiretroviral therapy in a resource-limited environment. Asian Pac J Cancer Prev. (2020) 21:2035–45. doi: 10.31557/APJCP.2020.21.7.2035
13. Ndejjo R, Mukama T, Musabyimana A, Musoke D. Uptake of cervical cancer screening and associated factors among women in rural Uganda: a cross sectional study. PLOS ONE. (2016) 11:149696. doi: 10.1371/journal.pone.0149696
14. Tsegay A, Araya T, Amare K. Knowledge, attitude, and practice on cervical cancer screening and associated factors among women aged 15–49 years in Adigrat Town, Northern Ethiopia, 2019: a community-based cross-sectional study. Int J Womens Health. (2021) 12:1283–98. doi: 10.2147/IJWH.S261204
15. Weng Q, Jiang J, Haji FM, Nondo LH, Zhou H. Women's knowledge of and attitudes toward cervical cancer and cervical cancer screening in Zanzibar, Tanzania: a cross-sectional study. BMC Cancer. (2020) 20:63. doi: 10.1186/s12885-020-6528-x
16. Bai Y, Liu Q, Chen X, Gao Y, Gong H, Tan X, et al. Protection motivation theory in predicting intention to receive cervical cancer screening in rural Chinese women. Psychooncology. (2018) 27:442–9. doi: 10.1002/pon.4510
17. Abate K, Worku A, Hussien S, Aklilu A. Association between socioeconomic status and willingness to pay for medical care among government school teachers in Addis Ababa. Sci J Pub Health. (2015) 3:677–85. doi: 10.11648/j.sjph.20150305.23
18. Noor Aizuddin A, Sulong S, Aljunid SM. Factors influencing willingness to pay for healthcare. BMC Public Health. (2012) 12:1–1. doi: 10.1186/1471-2458-12-S2-A37
19. Javan N, Zahra K, Ahmad F, Mohammad K. Identification determinant factors on willingness to pay for health services in Iran. Health Econ Rev. (2017) 7:40. doi: 10.1186/s13561-017-0179-x
20. Son KM, Young SN, Hee YJ, Cheol PE, KuiSon C. Women's willingness to pay for cancer screening. J Prev Med Public Health. (2006) 39:331–8.
21. Somdatta P, Upadhyay M, Chhabra P. Awareness of cervical cancer and willingness to participate in screening program: public health policy implications. J Cancer Res Ther. (2017) 13:318. doi: 10.4103/0973-1482.187279
22. Thompson EL, Galvin AM, Daley EM, Tatar O, Zimet GD, Rosberger Z. Recent changes in cervical cancer screening guidelines: US women's willingness for HPV testing instead of Pap testing. Prev Med. (2020) 130:105928. doi: 10.1016/j.ypmed.2019.105928
23. Ogilvie GS, Smith LW, van Niekerk DJ, Khurshed F, Krajden M, Saraiya M, et al. Women's intentions to receive cervical cancer screening with primary human papillomavirus testing. Int J Cancer. (2015) 133:2934–43.
24. Jia Y, Li S, Yang R, Zhou H, Xiang Q, Hu T, et al. Knowledge about cervical cancer and barriers of screening program among women in Wufeng County, a high-incidence region of cervical cancer in China. PLoS ONE. (2013) 8:e67005. doi: 10.1371/journal.pone.0067005
Keywords: willingness, cervical cancer screening, Girar Jarso, Ethiopia, North Shoa zone
Citation: Desta AA, Alemu FT, Gudeta MB, Dirirsa DE and Kebede AG (2022) Willingness to utilize cervical cancer screening among Ethiopian women aged 30–65 years. Front. Glob. Womens Health 3:939639. doi: 10.3389/fgwh.2022.939639
Received: 09 May 2022; Accepted: 01 August 2022;
Published: 30 August 2022.
Edited by:
Blami Dao, Jhpiego, United StatesReviewed by:
Elissa Z. Faro, University of Iowa Health Care, United StatesAli-Asghar Kolahi, Shahid Beheshti University of Medical Sciences, Iran
Copyright © 2022 Desta, Alemu, Gudeta, Dirirsa and Kebede. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Adugna Alemu Desta, YWR1Z25hMjEyM0BnbWFpbC5jb20=
 Adugna Alemu Desta
Adugna Alemu Desta Fikadu Tolesa Alemu
Fikadu Tolesa Alemu Moges Beya Gudeta
Moges Beya Gudeta Dejene Edosa Dirirsa
Dejene Edosa Dirirsa Andualem Gezahegn Kebede
Andualem Gezahegn Kebede