- 1School of Nursing and Midwifery, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
- 2School of Public Health, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
- 3School of Nursing and Midwifery, College of Health and Medical Sciences, Ambo University, Ambo, Ethiopia
Background: Episiotomy is an intentional surgical incision made on the perineum with the aim of enlarging the introits during the second stage of labor or just before delivery of the baby. It sometimes also interferes with the mother's comfort during the postpartum period and has associated complications especially when it is done without indication. However, there is limited information regarding episiotomy practice in the study area.
Objective: This study aimed to determine the magnitude of episiotomy practice and associated factors among women who gave birth at the Hiwot Fana Specialized University Hospital, Eastern Ethiopia, 2021.
Methods: A facility-based cross-sectional study was conducted among 408 systematically selected mothers who gave birth at the Hiwot Fana Specialized University Hospital, from 1 January to 30 December 2021. Datas were collected from delivery medical records using a pretested checklist. The extracted data were checked, coded, and entered into the Epi-data version 3.1 and exported to the STATA version 16 software for analysis. Binary logistic regression was fitted to identify factors associated with episiotomy practice. P-values < 0.05 were considered to declare the presence of statistical significance.
Results: The overall prevalence of episiotomy practice was found to be 43.4 % (95% CI: 38.7, 48.9), and mediolateral was the most commonly practiced episiotomy type (41.4%). Parity [AOR: 6.2; 95% CI (3.8–17.6)], 1st min Apgar score [AOR: 1.6; 95% CI (1.04–2.67)], presence of maternal medical disease [AOR: 3.3; 95% CI (1.09–6.9)], and induced labor [AOR: 1.6; 95%CI (1.12, 4.13)] were significantly associated with the episiotomy practice.
Conclusion: The prevalence of episiotomy practice in the study area was high. Parity, presence of maternal medical disease, induction of labor, and 1st min APGAR score were significant factors associated with episiotomy practice. Considering the presence of appropriate indications or preventing unjustifiable indications, can help to reduce the current high practice rates.
Introduction
An episiotomy is one of the widely practiced obstetric interventions performed to minimize the risk of severe tears or to enlarge the birth outlet during childbirth at a time when the fetus's head descends (1, 2). It helps in avoiding potential intracranial damage to the infant, prevents low Apgar score, and avoids severe and irregular perineal tears. The procedure also helps to prevent the relaxation of pelvic floor muscles and the incidence of cystocele and rectocele (3).
Even though seven different types of episiotomy have been reported in works of literature, two major types are routinely used: median and mediolateral episiotomy (2, 4, 5). Mediolateral episiotomies are most commonly performed in Europe, whereas midline episiotomy is common in the USA (6). World Health Organization (WHO) expressed a lack of evidence to perform routine or liberal use of episiotomy for women undergoing spontaneous vaginal birth and recommended restrictive episiotomy, despite its particular rate not being suggested (7).
The practice of episiotomy is highest in Latin America and lowest in Europe. The prevalence ranges from 9.7% in Sweden to 100% in Taiwan. For nulliparous women, a range from 63.3% in South Africa to 100% in Guatemala has been recorded, indicating an overall greater likelihood for primiparous to receive an episiotomy at birth (8). In Africa, the rates of episiotomy also varied: Rwanda reported 80.1% of episiotomy practice among primiparous women (9), and Ethiopia listed among the highest (10–14). In Ethiopia, findings from studies conducted in different parts of the country revealed that the magnitude of episiotomy is over 30%, and the practice was reported to increase up to 2.3-folds more in rural parts of Ethiopia (10, 14).
Most of the consequences of episiotomy affect the laboring mothers, greatly impacting their quality of life and leaving them with an unpleasant childbirth memory. A report showed that episiotomy alone had caused around 9 and 8% of primary postpartum hemorrhage and maternal sepsis, respectively (15). Findings also indicated that the procedure has increased the risk of subsequent pelvic floor dysfunction, fecal and urinary incontinence, spontaneous perineal tear, sexual dysfunction, and fetal head injury (16–18). Episiotomy is also associated with a higher incidence of perineal pain in the immediate postpartum period, which predisposes them to a risk of psychological morbidity and stress urinary incontinence at 6 weeks postpartum (19, 20). Studies also indicate routine episiotomy practice has undue adverse effects, such as extreme perineal trauma, or prolapse of the pelvic organ compared to restrictive episiotomy usage (21–23).
In addition, episiotomy is done to prevent severe perineal tears, even though it has been related to an increased risk of severe bleeding, wound hematoma, dyspareunia, increased discomfort, anal postpartum incontinence, and infection, implying minimal practice (23, 24). Therefore, indications for routine episiotomy are not well-supported or restrictive use of episiotomy is advocated (25, 26).
Reducing the non-evidence-based practice of episiotomy is a global target in improving maternal health and their birthing experiences (27, 28). A number of strategies have been suggested by international leading associations and communities. Continuous quality improvement programs, obstetric interventions, including choosing different positions of birth, and setting an acceptable rate of episiotomy (10%) for normal deliveries were some of them (29–31).
Factors like obstetric procedure, maternal and fetal conditions, increase in age of women, prim-parity, malposition of fetus, instrumental delivery, and vaginal breech delivery have shown an association with why usually episiotomy is practiced (32–34). Despite plenty of research evidencing against liberal use of episiotomy and its related complications, the rate continues to rise in many developing nations. Epidemiologically reliable prevalence and associated factors of episiotomy practice are not well-studied in the study area. Therefore, this study aimed to determine the magnitude of episiotomy and factors associated with women who gave birth in HFSUH, Eastern Ethiopia, which might help reduce the non-evidence-based practice of episiotomy and associated complications in lower-income settings.
Method and materials
Study design, setting, and period
A facility-based quantitative cross-sectional study was conducted at HFSUH, a tertiary referral center affiliated with the College of Health and Medical Sciences, Haramaya University, Ethiopia. The hospital provides both general and specialist services for about 3.8 million populations in Eastern Ethiopia with more than 4,000 deliveries per annum. During the study period, the unit was run by seven consultants, 29 residents, and 43 midwives. A neonatal intensive care unit (NICU) equipped with essential equipment for caring neonates with special care needs is available. The study recruits women who gave birth from 1 January 1 to 30 December 2021.
Population
Women who gave birth through vaginal delivery at the Hiwot Fana Specialized University Hospital were the source population. Women who gave birth through vaginal delivery at the Hiwot Fana Specialized University hospital from 1 January to 30 December 2021 were the study population. The study excluded records with incomplete information.
Sample size determination
The minimum sample size required for this study was determined using a single population proportion formula with assumptions of confidence level at 95% = 1.96, a margin of error (d) = 0.05, and a reasonable proportion of episiotomy practice (41.4%) from the previous study in conducted Tigray (12).
Then, after adding contingency for incompleteness (10%), the total sample size calculated for this study was 408.
Sampling technique
The unique medical record number of women who gave birth by vaginal delivery obtained from the registration book was used to create the sampling frame. The total number of women who gave birth by vaginal delivery (2,548) during the study period was divided by the total sample size (408) to obtain the fixed periodic interval value (K-value) of approximately 6 (6th). A systematic random sampling technique was utilized to select a medical record by the determined K-value.
Data collection
Data were collected using the data extraction checklist developed after reviewing relevant literature (10, 14, 35). The extraction sheet addressed the socio-demographics, pregnancy, labor and delivery, and postnatal characteristics. Data were collected by six BSc holder midwives and supervised by two public health specialists (MPH).
Variables
The outcome variable of the study was episiotomy practice. The independent variables included socio-demographic factors, pregnancy, labor, delivery, and postnatal characteristics.
Data quality control
To assure the quality of data, training was given to data collectors and supervisors on the objective of the study for 2 days. A pre-test was done on 5% of the sample size before the actual data collection. The checklists were modified based on the pretest result, repetitive ideas, and ambiguous questions were corrected, and the modified checklists were used for the final data collection. Data were checked for completeness, accuracy, clarity, and consistency by the principal investigator and supervisors before data entry into the software. Double data entry was done for its validity and compared to the original data. Simple frequencies and cross-tabulation were done to check for missing values and variables.
Data processing and analysis
The collected datas were checked for completeness, cleaned, edited, coded, and entered into the Epi data version 3.1 to minimize logical errors and design skipping patterns. Then, the datas were exported to STATA version 16 for analysis. The assumptions for binary logistic regression were checked. Bivariate and multivariable logistic regression analyses were done to check the association between the practice of episiotomy and each independent variable. All variables with P-value < 0.2 in the bivariate analysis were included in the final model of multivariate analysis to control all possible confounders and the variables were selected by step-wise selection. The goodness of fit was tested by the Hosmer-Lemeshow test (P-value = 0.561). The multi-co-linearity test was carried out to see the correlation between independent variables by using standard error and variance inflation factor (VIF). Adjusted odds ratio along with 95% CI was estimated to identify factors associated with episiotomy practice. A P-value < 0.05 was considered to declare the presence of a statistically significant association.
Ethics approval and consent to participate
Ethical approval was obtained from Haramaya University, College of Health and Medical Sciences, Institutional Health Research Ethics Review Committee (IHRERC). Data collection began after obtaining informed, voluntary written consent from the head of the institution. Throughout the study period, the confidentiality of the data was strictly maintained through a collection of anonymized record only.
Results
Socio-demographic characteristics
In this study, 408 records of mothers who gave birth have been reviewed. Among the majority of the study participants, 216 (52.9%) were between 15 and 24 years old and the mean age was 25.1(+/−4.3 SD). Most of them were urban residents (57.1%). About 235 (57.6%) of the study participants were Muslims by their religion. Only 26 (6.4%) mothers had medical conditions, including hypertensive, metabolic, cardiac, and respiratory disorders (Table 1).
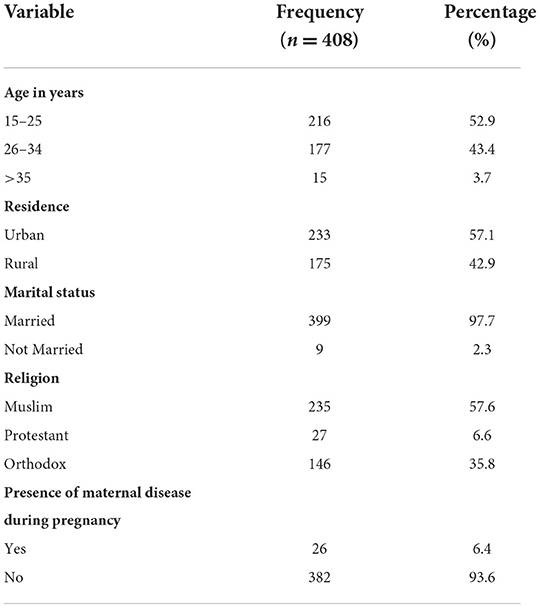
Table 1. Socio-demographic characteristics of women who gave birth in the Hiwot Fana Specialized University Hospital, Eastern Ethiopia, 2021.
Pregnancy, labor, and delivery related characteristics
From the total reviewed mothers' records, 274 (67.2%) had antenatal care (ANC) follow-up on index pregnancy. Regarding birth experience, 76 (18.6%) mothers were pregnant for the first time. In addition, 292 (71.6) had given birth through SVD previously. Among mothers who had previous vaginal births, 99 (24.2%) had previous episiotomy experiences. About 328 (80.4%) had spontaneous labor onset (Table 2).
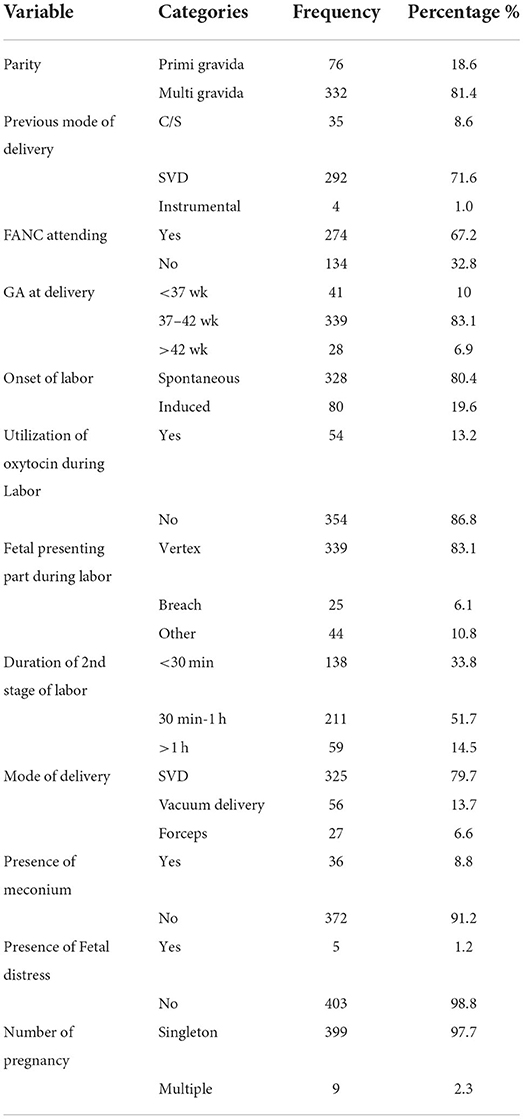
Table 2. Pregnancy, labor, and delivery characteristics of women who gave birth in the Hiwot Fana Specialized University Hospital, Eastern Ethiopia, 2021.
Birth outcome and postnatal characteristics
This study showed that 142 (34.8%) have the 1st min Apgar score of <6. The presence of meconium was identified in 36 (8.8%) newborns. Furthermore, around 88.2% have birth weights of 2,500−3,999 g.
Episiotomy practice
The overall prevalence of episiotomy practice was 43.4% (95%CI; 38.7, 48.9). About 101 (24.7%) indicated secondary to tight perineum, while 31 (7.5%) indicated a prolonged second stage of labor. The most commonly practiced type of episiotomy was mediolateral that accounted for around 41.4% (169) and 95.4% of all episiotomies done.
Factors associated with episiotomy practice
On bi-variate analysis, variables like age, the onset of labor, presence of maternal medical disease, duration of the second stage of labor, use of oxytocin during labor, Hx of the previous episiotomy, gravidity, and the Apgar score at the 1st min had p-value score of <0.2 and entered into the multivariable regression analysis. In the multivariable logistic regression analysis, parity, 1st min APGAR score, the presence of maternal medical disease, and induction of labor were significantly associated with episiotomy practice at a p-value of < 0.05 (Table 3).
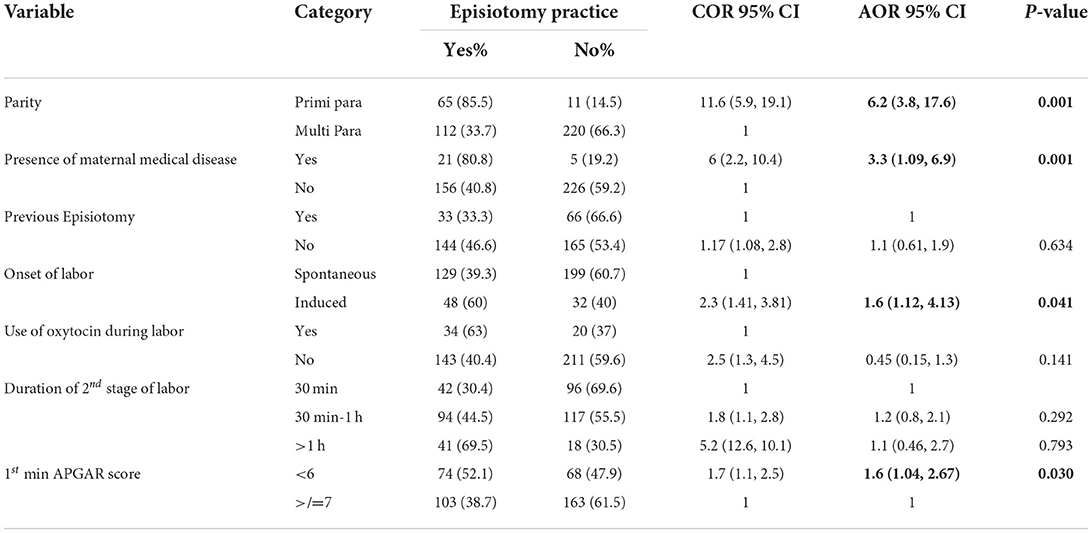
Table 3. Factors associated with episiotomy practice among mothers who gave birth at the HFSUH, 2021.
Discussion
More than two-fifth of women incurred episiotomy during delivery, and mediolateral was the most commonly (41.4%) practiced episiotomy type. In addition, being primigravida, 1st min Apgar score <6, presence of maternal medical disease, and induction of labor increased the odds of episiotomy practice.
The prevalence of 43.4% (95%CI; 38.7, 48.9) episiotomy practice in the current study is consistent with other findings found in Northwest Ethiopia 44.5% (11), Shire, Ethiopia 41.4% (12), Addis Ababa, Ethiopia, 40% (35), Kano, Nigeria 41.4% (36), Iran 41.5% (37), and studies conducted in developing countries, 36–40% (38).
On the other hand, the current finding is found to be lower than studies conducted in Addis Ababa, Ethiopia (65%) (39), Arbaminch, Ethiopia (68%) (14), Uganda (73%) (40), and in northern Nigeria (89.3%) (41). Similarly, several studies done in different hospitals expose a higher prevalence of episiotomy between 69.2 and 96.2% among primigravid women (18, 42, 43). However, the current result of the prevalence of episiotomy was found higher than study conducted in Jimma 25% (44), Vietnamese-born women (29.9%) (45), Nigeria (21%) (16), Brazil 29.1% (46), Nepal 22% (47), East African women 30% (48), and Mizan Aman 30.6% (33). This difference might happen due to the dissimilarity in settings of the study participants, study period, different sample sizes, sampling techniques, and characteristics of the study population. The elevated prevalence in the current study might be due to the characteristics of the study participant at a specialized University Hospital. The majority of the pregnant mothers who gave birth here were from the category of high risk, complicated cases, and had to go through various obstetric interventions, which might increase the jeopardy of episiotomy.
In congruent with facility-based studies conducted in Addis Ababa, Ethiopia (35, 39), Brazil (49), Nigeria (50), and Uganda (40), primigravid women were more likely to have episiotomy than multiparous women. The study conducted in Uganda indicated that a primigravid mother was four times more likely to have an episiotomy than a multiparas mother (40). This may be due to the perineum muscle of the primigravid mothers being tighter than multiparas women, and due to this, the birth attendant tends to perform a liberal episiotomy.
Mothers of babies with a 1st min Apgar score of <6 were 1.6 times more likely to experienced episiotomy than babies with ≥7 Apgar score. A similar finding was reported from the study conducted at Petrolane, Brazil, which found newborns with lower Apgar scores were two times more likely to happen in the episiotomy group (51). Another study in Ethiopia found that episiotomy happened 5 times more likely among mothers who had low Apgar score bay than those with normal Apgar scores (12). A study conducted in Iran showed a significant mean difference in the 1st-min Apgar score (8.21 ± 0.77) in the episiotomy group and (8.86 ± 1.09) in the non-episiotomy group (37). Additionally, another study result indicated that 21.7% of infants in the episiotomy group and 15.1% in the non-episiotomy group had Apgar scores <7, with a significant difference between them (52).
This study indicated that mothers who had medical diseases were 3.3 times more likely to experience episiotomy than mothers who have no medical disease. This finding is similar to the study done so far in Ethiopia (34). However, a study conducted in Brazil revealed that maternal disease specifically hypertensive syndrome showed a significant association with episiotomy performance (49). This is probably because the birth attendant might think that performing an episiotomy will decrease the duration of labor and delivery particularly in mothers with medical diseases, who are at higher risk for post-partum complications (53).
Furthermore, our study revealed that mothers who gave birth by induced labor had higher odds of episiotomy exposure than those who gave birth by spontaneous onset. This is similar to findings from other studies conducted in Latin America (1), Brazil (18), Iran (37), Northwest Ethiopia (11), and Shire town Ethiopia (34). The possible ground may be if labor does not begin and advance spontaneously, it may not bring perineal muscle's physiological lessening and this could call for perineal intervention (54). Induced labor can also be high in strength and frequency of uterine contractions that may result in non-reassurance fetal heart rate patterns that may need an episiotomy to be applied by the birth attendant in an attempt to decrease the length of labor (55).
Limitations of the study
This study has some limitations to consider while interpreting the findings. The cross-sectional nature of the study design prevents temporal relationship inference. In addition, the use of records hinders complete information.
Conclusion
The practice of episiotomy is high in the study area. More than two-fifth of women who gave birth incurred episiotomy during delivery. Parity, 1st min Apgar score, presence of maternal medical disease, and the induced onset of labor were significantly associated with the practice of episiotomy. It is imperative to reduce the rate of episiotomy to improve the well-being and quality of life of women. Considering the presence of appropriate indication or preventing unjustifiable case selection, especially on nulliparous mothers, and induction of labor may help reduce the current high practice rates. In addition, designing programs that improve maternal health conditions to prevent medical diseases, which may complicate pregnancy, would be beneficial.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Haramaya University, College of Health and Medical Sciences, Institutional Health Research Ethics Review Committee (IHRERC). The head of institution provided written informed consent to allow data collection for this study.
Author contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Funding
This study was funded by Haramaya University. The funding body has no role in the design of the study and collection, analysis and interpretation of data, and in writing the manuscript.
Acknowledgments
The authors would like to thank the Haramaya University College of Health and Medical Science for providing opportunities and technical support throughout the study. The authors are also grateful to the Hiwot Fana Specialized University Hospital and study participants in the region for their valuable support during the data collection.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ANC, Antenatal care; AOR, Adjusted Odds Ratio; C/S, Cesarean Section; COR, Crude Odds Ratio; EFW, Estimated fetal weight; HFSUH, Hiwot Fana Specialized University Hospital; IHRERC, Institutional Health Research Ethics Review Committee; NICU, Neonatal Intensive Care Unit; SVD, Spontaneous Vaginal Delivery; VIF, variance inflation factor; WHO, World health organization.
References
1. Ballesteros-Meseguer C, Carrillo-García C, Meseguer-de-Pedro M, Canteras-Jordana M, Martínez-Roche M. Episiotomy and its relationship to various clinical variables that influence its performance. Revista latino-americana de enfermagem. (2016) 24:2686. doi: 10.1590/1518-8345.0334.2686
2. Hinshaw K, Arulkumaran S. Malpresentation, malposition, cephalopelvic disproportion and obstetric procedures. Dewhurst's Textbook Obst Gynaecol. (2018) 4:354. doi: 10.1002/9781119211457.ch26
3. Boujenah J, Tigaizin A, Fermaut M, Murtada R, Benbara A, Benchimol M, et al. Is episiotomy worthwile to prevent obstetric anal sphincter injury during operative vaginal delivery in nulliparous women? Eu J Obst Gynecol Reproduct Biol. (2019) 232:60–4. doi: 10.1016/j.ejogrb.2018.11.014
4. Cunningham F, MacDonald P, Gant N, Leveno K, Gilstrap III L, Hankins G. Anatomy of the reproductive tract. Williams Obst. (2001) 5:31–61.
5. Carroli G, Mignini L. Episiotomy for vaginal birth. Cochrane Database Sys Rev. (2009) 3:Cd000081. doi: 10.1002/14651858.CD000081.pub2
6. Räisänen S, Vehviläinen-Julkunen K, Heinonen S. Need for and consequences of episiotomy in vaginal birth: a critical approach. Midwifery. (2010) 26:348–56. doi: 10.1016/j.midw.2008.07.007
7. Intrapartum care for a positive childbirth experience. Geneva: World Health Organization; Evidence and recommendations. (2018). Available online at: https://www.ncbi.nlm.nih.gov/books/NBK513805/ (accessed February 02, 2022).
8. Ogunyemi D, Manigat B, Marquis J, Bazargan M. Demographic variations and clinical associations of episiotomy and severe perineal lacerations in vaginal delivery. J Natl Med Assoc. (2006) 98:1874.
9. Mbukani R, Kakoma J. Is nulliparity a risk factor for poor obstetrical and neonatal outcomes in rwandan district hospitals? A Prosp Observ Study Muhima Dist Hos. (2012) 69:50–53.
10. Beyene F, Nigussie AA, Limenih SK, Tesfu AA, Wudineh KG. Factors associated with episiotomy practices in Bahirdar city, Ethiopia: a cross-sectional study. Risk Manag Healthc Policy. (2020) 13:2281. doi: 10.2147/RMHP.S277657
11. Woretaw E, Teshome M, Alene M. Episiotomy practice and associated factors among mothers who gave birth at public health facilities in Metema district, northwest Ethiopia. Reprod Health. (2021) 18:142. doi: 10.1186/s12978-021-01194-9
12. Yemaneh Y, Sahile E, Alehegn A, Girma A, Robles C. Assessment of the proportion and associated factors of episiotomy at public health institutions of Axum town, Tigray region, North Ethiopia, 2016. Crit Care Obstetrics Gynecol. (2017) 3:11. doi: 10.21767/2471-9803.1000152
13. Worku S, Mitku Y, Getahun S. Episiotomy practice and its associated factor among women who gave birth at Public Health Institutions of Akaki Kality in Addis Ababa, Ethiopia. Clin Mother Child Health. (2019) 16:2. doi: 10.4172/2090-7214.1000318
14. Fikadu K, Boti N, Tadesse B, Mesele D, Aschenaki E, Toka E, et al. Magnitude of episiotomy and associated factors among mothers who give birth in arba minch general hospital, southern ethiopia: observation-based cross-sectional study. J Preg. (2020) 2020:5142. doi: 10.1155/2020/8395142
15. Chang SR, Chen KH, Lin HH, Chao YMY, Lai YH. Comparison of the effects of episiotomy and no episiotomy on pain, urinary incontinence, and sexual function 3 months postpartum: a prospective follow-up study. Int J Nurs Stud. (2011) 48:409–18. doi: 10.1016/j.ijnurstu.2010.07.017
16. Inyang-Etoh E, Umoiyoho A. The practice of episiotomy in a university teaching hospital in Nigeria: how satisfactory? Int J Med Biomed Rese. (2012) 1:68–72. doi: 10.14194/ijmbr.1111
17. Ahmed HM. Midwives' Clinical Reasons for Performing Episiotomies in the Kurdistan Region: Are they evidence-based? Sultan Qaboos Univ Med J. (2014) 14:e369–74.
18. Braga GC, Clementino STP. Luz PFNd, Scavuzzi A, Noronha Neto C, Amorim MMR. Fatores de risco para a episiotomia: um estudo de caso-controle. Revista da Associação Médica Brasileira. (2014) 60:465–72. doi: 10.1590/1806-9282.60.05.015
19. Albers LL, Sedler KD, Bedrick EJ, Teaf D, Peralta P. Factors related to genital tract trauma in normal spontaneous vaginal births. Birth. (2006) 33:94–100. doi: 10.1111/j.0730-7659.2006.00085.x
20. Islam A, Hanif A, Ehsan A, Arif S, Niazi SK, Niazi AK. Morbidity from episiotomy. J Pak Med Assoc. (2013) 63:696–701.
21. Röckner G, Fianu-Jonasson A. Changed pattern in the use of episiotomy in Sweden. BJOG. (1999) 106:95–101. doi: 10.1111/j.1471-0528.1999.tb08207.x
22. Aasheim V, Nilsen ABV, Reinar LM, Lukasse M. Perineal techniques during the second stage of labour for reducing perineal trauma. Cochrane Database Sys Rev. (2017) 3:6672. doi: 10.1002/14651858.CD006672.pub3
23. Lurie S, Kedar D, Boaz M, Golan A, Sadan O. Need for episiotomy in a subsequent delivery following previous delivery with episiotomy. Arch Gynecol Obstet. (2013) 287:201–4. doi: 10.1007/s00404-012-2551-8
24. Chia C-C, Huang S-C. Third-and fourth-degree perineal laceration in vaginal delivery. Taiwan J Obstet Gynecol. (2012) 1:148–52. doi: 10.1016/j.tjog.2012.01.035
25. Jiang H, Qian X, Carroli G, Garner P. Selective versus routine use of episiotomy for vaginal birth. Cochrane Database Sys Rev. (2017) 2:Cd000081. doi: 10.1002/14651858.CD000081.pub3
26. Practice Bulletin No. 165 Summary: prevention and management of obstetric lacerations at vaginal delivery: correction. Obstet Gynecol. (2016) 128:411. doi: 10.1097/AOG.0000000000001578
27. ACOG. ACOG committee opinion no. 766: approaches to limit intervention during labor and birth. Obstet Gynecol. (2019) 133:e164–73. doi: 10.1097/AOG.0000000000003074
28. Hussein SAAA, Dahlen H, Schmied V. What makes episiotomy rates change? : a systematic review of the literature. Int J Childbirth. (2012) 2:29–39. doi: 10.1891/2156-5287.2.1.29
29. Lede RL, Belizán JM, Carroli G. Is routine use of episiotomy justified? Am J Obstet Gynecol. (1996) 174:1399–402. doi: 10.1016/S0002-9378(96)70579-3
30. Organization WH. WHO Recommendations for Prevention and Treatment of Maternal Peripartum Infections. Geneva: World Health Organization (2016).
31. Reynolds JL. Reducing the frequency of episiotomies through a continuous quality improvement program. Cmaj. (1995) 153:275–82.
32. Friedman AM, Ananth CV, Prendergast E, D'Alton ME, Wright JD. Variation in and factors associated with use of episiotomy. Jama. (2015) 313:197–9. doi: 10.1001/jama.2014.14774
33. Kumera MG, Ademe BW, Akessa GM. Assessment of episiotomy practice in Mizan Aman General Hospital, Ethiopia. Assessment. (2015) 20:12–20. doi: 10.7176/JHMN
34. Niguse K, Gidey G, Gebrehiwot H, Abay M, Getachew D, Worku T. Episiotomy Practice and its associated factors among mothers who gave birth vaginally at public health institutions of Shire Town, Northern Ethiopia. Infection. (2016) 8:9. doi: 10.37591/rrjohp.v6i1.850
35. Kiros K, Lakew Z. Magnitude of episiotomy in a teaching hospital in Addis Ababa, Ethiopia. Ethiop Med J. (2006) 44:205–9.
36. Garba I, Ozegya MS, Abubakar IS, Ayyuba R. Episiotomy at Aminu Kano teaching hospital, Kano, Nigeria: a 3-year review. Arch Int Surg. (2016) 6:17. doi: 10.4103/2278-9596.187202
37. Rasouli M, Keramat A, Khosravi A, Mohabatpour Z. Prevalence and factors associated with episiotomy in Shahroud City, northeast of Iran. Int J Womens Health Reprod Sci. (2016) 4:125–9. doi: 10.15296/ijwhr.2016.29
38. Maduma-Butshe A, Dyall A, Garner P. Routine episiotomy in developing countries: time to change a harmful practice. Br Med J Pub Group. (1998). doi: 10.1136/bmj.316.7139.1179
39. Tefera T, Kebede B, Mekonen T. Prevalence of episiotomy and factors associated with Practice of episiotomy at Saint Paul's Hospital Millennium Medical College: a cross sectional study. Ethi J Reprod Health. (2019) 11:8.
40. Pebolo F, Judith A, Dan KK. Prevalence and factors associated with episiotomy practice among primiparous women in Mulago national referral hospital Uganda. Int J Preg Child Birth. (2019) 5:197–201. doi: 10.15406/ipcb.2019.05.00176
41. Ocheke AN, Samuels E, Ocheke IE, Agaba PA, Ekere C, Bitrus J, et al. An audit of perineal trauma and vertical transmisson of HIV. Afr J Reprod Health. (2017) 21:67–72. doi: 10.29063/ajrh2017/v21i4.7
42. Shmueli A, Gabbay Benziv R, Hiersch L, Ashwal E, Aviram R, Yogev Y, et al. Episiotomy–risk factors and outcomes. J Maternal-Fetal Neonatal Med. (2017) 30:251–6. doi: 10.3109/14767058.2016.1169527
43. Owa OO, Eniowo AR, Ilesanmi OS. Factors associated with episiotomy among parturients delivering in a tertiary care centre in Nigeria. Int J Res Med Sci. (2015) 3:836–40. doi: 10.5455/2320-6012.ijrms20150403
44. Marai W, A. two years retrospective review of episiotomy at Jimma Teaching Hospital, southwestern Ethiopia. Ethiop Med J. (2002) 40:141–8.
45. Trinh AT, Khambalia A, Ampt A, Morris JM, Roberts CL. Episiotomy rate in Vietnamese-born women in Australia: support for a change in obstetric practice in Viet Nam. Bull World Health Organ. (2013) 91:350–6. doi: 10.2471/BLT.12.114314
46. Carvalho C, Souza A, Moraes Filho OB. Prevalence and factors associated with practice of episiotomy at a maternity school in Recife, Pernambuco, Brazil. Revista da Associacao Medica Brasileira. (1992). (2010) 56:333–9. doi: 10.1590/S0104-42302010000300020
47. Joshi A, Acharya R. Perineal outcome after restrictive use of episiotomy in primi-gravidas. JNMA J Nepal Med Assoc. (2009) 48:269–72. doi: 10.31729/jnma.286
48. Belihu FB, Small R, Davey M-A. Episiotomy and severe perineal trauma among eastern African immigrant women giving birth in public maternity care: a population based study in Victoria, Australia. Women Birth. (2017) 30:282–90. doi: 10.1016/j.wombi.2016.11.008
49. Carvalho CCM, Moraes Filho OB. Prevalence and factors associated with practice of episiotomy at a maternity school in Recife, Pernambuco, Brazil. Revista da Associação Médica Brasileira. (2010) 56:333–9. doi: 10.1590/s0104-42302010000300020
50. Chigbu B, Onwere S, Aluka C, Kamanu C, Adibe E. Factors influencing the use of episiotomy during vaginal delivery in South Eastern Nigeria. East Afr Med J. (2008) 85:240–3. doi: 10.4314/eamj.v85i5.9618
51. Al-Ghammari K, Al-Riyami Z, Al-Moqbali M, Al-Marjabi F, Al-Mahrouqi B, Al-Khatri A, et al. Predictors of routine episiotomy in primigravida women in Oman. App Nurs Res. (2016) 29:131–5. doi: 10.1016/j.apnr.2015.05.002
52. Izuka E, Dim C, Chigbu C, Obiora-Izuka C. Prevalence and predictors of episiotomy among women at first birth in Enugu, south east Nigeria. Ann Med Health Sci Res. (2014) 4:928–32. doi: 10.4103/2141-9248.144916
53. Souza ASRd, Noronha Neto C, Coutinho IC, Diniz CP, Lima MMdS. Pré-eclâmpsia. Femina. (2006) 5:499–507. doi: 10.4149/bll_2016_099
54. Kacvinska A, Drab M, Totka A, Holoman K, Gabor M. The effect of prostaglandin induced labor and selected factors on the occurrence and extent of birth-canal injuries. Bratisl Lek Listy. (2016) 117:511–4. doi: 10.4149/BLL_2016_099
Keywords: episiotomy, magnitude, parity, induced labor, medical conditions, Ethiopia
Citation: Bekele H, Tamiru D, Debella A, Getachew A, Yohannes E, Lami M, Negash A, Asfaw H, Ketema I, Eyeberu A, Habte S, Eshetu B, Getachew T, Mesfin S, Birhanu B, Heluf H, Kibret H, Negash B, Alemu A, Dessie Y and Balis B (2022) Magnitude of episiotomy practice and associated factors among women who gave birth at Hiwot Fana Specialized University Hospital, Eastern Ethiopia. Front. Glob. Womens Health 3:911449. doi: 10.3389/fgwh.2022.911449
Received: 02 April 2022; Accepted: 06 September 2022;
Published: 10 October 2022.
Edited by:
Dilly O. C. Anumba, The University of Sheffield, United KingdomReviewed by:
Addisu Alemu, Debre Markos University, EthiopiaDagne Addisu, Debre Tabor University, Ethiopia
Copyright © 2022 Bekele, Tamiru, Debella, Getachew, Yohannes, Lami, Negash, Asfaw, Ketema, Eyeberu, Habte, Eshetu, Getachew, Mesfin, Birhanu, Heluf, Kibret, Negash, Alemu, Dessie and Balis. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Habtamu Bekele, aGFidGkuYmVrZWxlQGdtYWlsLmNvbQ==; Dawit Tamiru, ZGF3aXR0YW1ydTVAZ21haWwuY29t
 Habtamu Bekele
Habtamu Bekele Dawit Tamiru
Dawit Tamiru Adera Debella
Adera Debella Alemeshet Getachew2
Alemeshet Getachew2 Ephrem Yohannes
Ephrem Yohannes Magarsa Lami
Magarsa Lami Abraham Negash
Abraham Negash Sisay Habte
Sisay Habte Bajrond Eshetu
Bajrond Eshetu Tamirat Getachew
Tamirat Getachew Sinetibeb Mesfin
Sinetibeb Mesfin Helina Heluf
Helina Heluf Belay Negash
Belay Negash Yadeta Dessie
Yadeta Dessie Bikila Balis
Bikila Balis