- 1College of Natural and Health Sciences, Zayed University, Abu Dhabi, United Arab Emirates
- 2Abu Dhabi Public Health Centre, Abu Dhabi, United Arab Emirates
Pre-pregnancy obesity is a risk factor for several health problems such as gestational diabetes, preeclampsia, labor induction, postpartum hemorrhage, and neonatal hypoglycemia. Being underweight is a risk factor for fetal growth restriction. Despite the negative impact of abnormal pre-pregnancy body mass index (BMI) (over and underweight) on pregnancy outcomes, a limited amount of studies has been conducted on the prevalence of pre-pregnancy over and underweight and associated factors in the United Arab Emirates (UAE). Thus, the aim of this study was to investigate the prevalence and factors associated with underweight, overweight, and obesity among mothers with children under the age of 2 years in Abu Dhabi, the UAE. A cross-sectional multicenter study was conducted in 2017 and included data from seven government health care centers in Abu Dhabi. Maternal pre-pregnancy BMI was calculated as the weight in kilograms (kg) divided by the square of the height in meters (m), (kg/m2). A total of 1,622 mother–child pairs were included in this study. Out of the 1,622 mothers, 43 (2.7%) were underweight, 1,068 (65.8%) were normal weight, 412 (25.4%) were overweight, and 99 (6.1%) were obese. Mothers with advanced maternal age (AMA) (≥35 years) were more likely to be overweight, odds ratio [OR] = 1.93, (95% confidence interval [CI] 1.52–2.3), p ≤ 0.001, and obese OR = 2.15 (95% CI 1.32–3.39), p = 0.001. Mothers with lower family income were more likely to be obese OR = 2.72 (95% CI 1.44–5.93), p = 0.002. Mothers with high parity (≥2) were more likely to be overweight OR = 1.91 (95% CI 1.49–2.50), p ≤ 0.001; obese OR = 1.76 (95% CI 1.06–2.92), p = 0.024; and less likely to be underweight OR = 0.52 (95% CI 0.27–0.94), p = 0.037. Obese mothers were more likely to deliver via cesarean section (CS) OR = 1.95 (95% CI 1.27–2.96), p = 0.002. This study provides valuable baseline information on the epidemiology of pre-pregnancy BMI in the UAE. The sociodemographic factors identified in the study can be used to target at-risk women. The study findings can also be used to develop contextualized strategies to prevent and manage complications associated with abnormal pre-pregnancy BMI in Emirati women.
Introduction
In recent years, the prevalence of overweight and obesity has been dramatically increasing worldwide, including women of reproductive age as well as pregnant mothers (1). In the United Arab Emirates (UAE), a systematic review assessing the prevalence of overweight and obesity prevalence reported a 2–3-fold increase between 1989 and 2017 (2). These results should be considered alarming because the obesity rates were higher among women, including women of reproductive age and pregnant women (42%) (3).
A previous study has documented that pre-pregnancy BMI has a more significant impact on pregnancy outcomes than weight gain during pregnancy (4, 5). Several studies addressed the effects of maternal pre-pregnancy obesity on pregnancy outcomes, including maternal and newborn health, such as gestational diabetes, gestational hypertension, macrosomia (6–8), preterm delivery (9–11), delayed initiation of breastfeeding, and a shortened duration of exclusive breastfeeding (12).
Before pregnancy, being underweight was also found to be associated with adverse health issues related to newborn health, such as the delivery of low birth weight (LBW) infants (13, 14). In addition, obesity, as well as overweight, may also affect the mode of delivery, which ultimately may have an impact on healthcare costs and maternity services (15). Concurrent with the rise in obesity prevalence, the rate of cesarean section (CS) has increased in the UAE from 10% in 1995 (16) to 24% in 2014 (17). A recent study reported a higher CS rate in Abu Dhabi at 30.2% (18). These rates are significantly higher than those suggested by the World Health Organization (WHO), of 10–15% of all live births (19). They are alarming when their impact on maternal and infant health is considered. Several studies reported an increased risk of CS in obese women (20–22).
In view of the abovementioned health problems, an important research area should also consider the sociodemographic characteristics that affect pre-pregnancy body mass index (BMI). Identifying the sociodemographic factors associated with pre-pregnancy BMI and maternal obesity is useful for implementing targeted preventive actions and improving their efficacy. However, the results appear inconsistent across the studies that have already investigated the relationship between sociodemographic factors and pre-pregnancy BMI. For example, some studies identified poor socioeconomic conditions, based on the level of the family income as low or living in deprived conditions to be significantly associated with maternal obesity (5, 23, 24). Other researchers of low-income countries found that maternal underweight in early pregnancy is most probably related to pre-pregnancy underweight as a leading risk factor for adverse birth outcomes, including LBW, preterm birth, and small for gestational age (25, 26).
However, there have been inconsistent findings for other sociodemographic factors such as maternal age and education level (5, 23, 27). An understanding of the sociodemographic factors associated with abnormal pre-pregnancy BMI can be useful in designing appropriate measures. There is not only a lack of studies from the UAE on the epidemiology of pre-pregnancy BMI but also on associated sociodemographic factors. Therefore, we undertook this study to understand the prevalence of abnormal pre-pregnancy BMI and the associated sociodemographic factors.
Materials and methods
Participants and data collection
This study was a multicenter cross-sectional study where mothers of children were recruited from the community and healthcare centers in Abu Dhabi from March to September 2017. The study sample included Emirati and non-Emirati families. Seven governmental clinics providing maternal and child health services were approved for data collection. Mothers with young children visiting the healthcare centers with their children were approached by trained female research assistants who provided oral and written information about the study in Arabic and English. The inclusion criteria for recruiting participants had at least one child under 2 years of age. The research assistants interviewed the mothers using a structured questionnaire for data collection. The original project from which these data were extracted was approved (ZU17_006_F) by the Research Ethics Committee at Zayed University, the UAE. Also, clearance was obtained from the Abu Dhabi Health Services Company.
Study instrument
The primary study tool was a questionnaire validated by conducting a pilot study where necessary corrections were done before the distribution to collect the data. The questionnaire was first designed in English and then interpreted in Arabic, using a cross-translation strategy, where a local Arabic speaker translated the English document into Arabic. After that, another local Arabic speaker blinded to the original translation and converted the document back to English. The questionnaire included family demographics (e.g., parent education, age, nationality, and occupation, maternal and paternal education, occupation, maternal age, family financial status), child's information, health indicators (e.g., child gender, birth weight, delivery mode, parity), and infant feeding practices (e.g., breastfeeding initiation).
More information about the study methodology was described in the previous study (28).
Variables
The primary variable of this study is pre-pregnancy BMI (underweight, normal weight, overweight, and obese). The secondary variables are sociodemographic characteristics such as maternal age in years, parity, parent education, occupation; pregnancy outcomes such as gestational age at delivery (term vs. preterm), birth weight at delivery (normal birth weight vs. LBW), and mode of delivery (vaginal vs. CS). These variables are selected based on previous studies (5, 23–27). For each variable, odds ratio (OR) and 95% CI was calculated, and any variable with a p < 0.05 was considered significant.
Definitions
Education
Education is categorized into less than secondary and secondary and above, i.e., < secondary education is considered primary education, unlike ≥ secondary education level.
Body mass index (BMI)
BMI is defined as the weight in kilograms divided by the square of the height in meters (kg/m2). Both pre-pregnancy maternal weight and height were provided from the maternal health cards. The BMI was categorized into subgroups using the WHO classification (29) as follows: underweight (BMI <18.5 kg/m2), normal weight (BMI 18.5–24.9 kg/m2), overweight (BMI 25–29.9 kg/m2), and obese (BMI ≥ 30 kg/m2).
Parity
Number of times that a woman had given birth to a fetus with a gestational age of 24 weeks or more, regardless of whether the child was born alive or was stillborn.
Gestational age (GA) at delivery
A measure of the age of a pregnancy in weeks, which is taken from the beginning of the woman's last menstrual period. Term birth was defined as the birth of a baby at ≥37 weeks GA. Preterm birth was defined as the birth of a baby at <37 weeks GA.
Birth weight at delivery
Refers to the baby's weight in grams immediately after delivery; any baby delivered with a weight <2,500 grams was considered as LBW and ≥2,500 grams as normal weight.
Arab nationality
All Emirati mothers and other Arab nationalities.
Non-Arab nationality
Asian mothers and other non-Arab nationalities.
Family income
Based on the mother's answer to the following question, “Considering your monthly family income, how would you rate your and your family's overall financial well-being?” < good or ≥good.
Data analysis
Data were analyzed using Statistical Package for the Social Science (IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp.). Descriptive statistics were applied to estimate the prevalence with a 95% confidence interval (CI) among different pre-pregnancy BMI groups. Means and proportions for the sociodemographic characteristics were compared between the four subgroups of the pre-pregnancy BMI (underweight, normal, overweight, and obese) by ANOVA and Chi-square tests, respectively. Continuous variables, such as maternal age, parity, gestational age, and birth weight at delivery, were also analyzed as continuous and categorical variables. As the dependent variable (pre-pregnancy BMI) comprised four subgroups, multi-nominal logistic regression was applied. In the ANOVA and Chi-square tests, significant variables (p < 0.05) were further analyzed by logistic regression.
Results
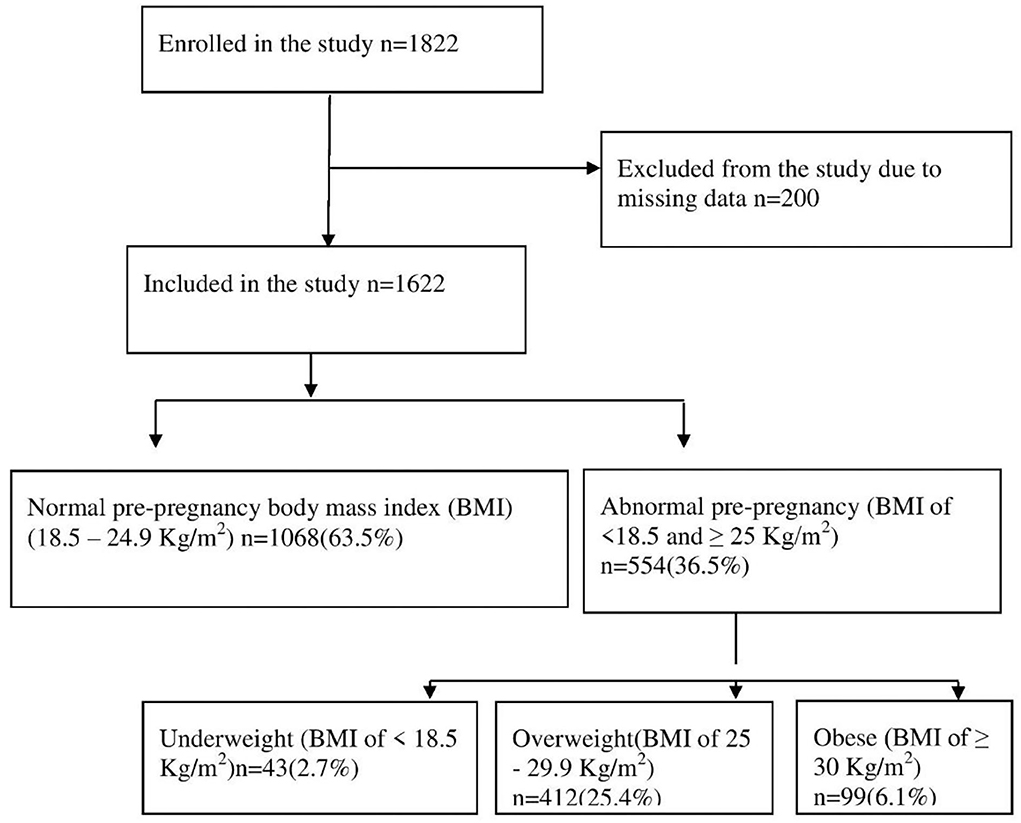
A total of 1,622 mother–child pairs were included in this work from the original sample (N = 1,822). The remaining 200 participants were excluded due to missing data such as maternal education, gestational age, and mode of delivery (Figure 1).
The mean (SD) of maternal age and parity was 30.1 (5.2) years and 2.2 (1.2), respectively. Out of 1,622 mothers, 43 (2.7%) (95% CI 2.5–2.9) were underweight (BMI <18.5 kg/m2), 1,068 (65.8%) (95% CI 63.5–68.1) were normal weight (BMI 18.5–24.9 kg/m2), 412 (25.4%) (95% confidence interval [CI] 23.3–27.5) were overweight (BMI 25–29.9 kg/m2) and 99 (6.1%) (95% CI 5.9–6.3) were obese (BMI ≥ 30 kg/m2). Among 1,622 mothers, 95.9% of women had secondary education or higher. About 4 out of 10 mothers were employed (37.5%). As for nationality, there was no difference in pre-pregnancy BMI between Arab mothers, including Emarati, and other non-Arab mothers. About one-third of the mothers gave birth via CS (30.5%). Of the 1,622 children, 6.7% and 9.6% were preterm births and LBW, respectively (Table 1).
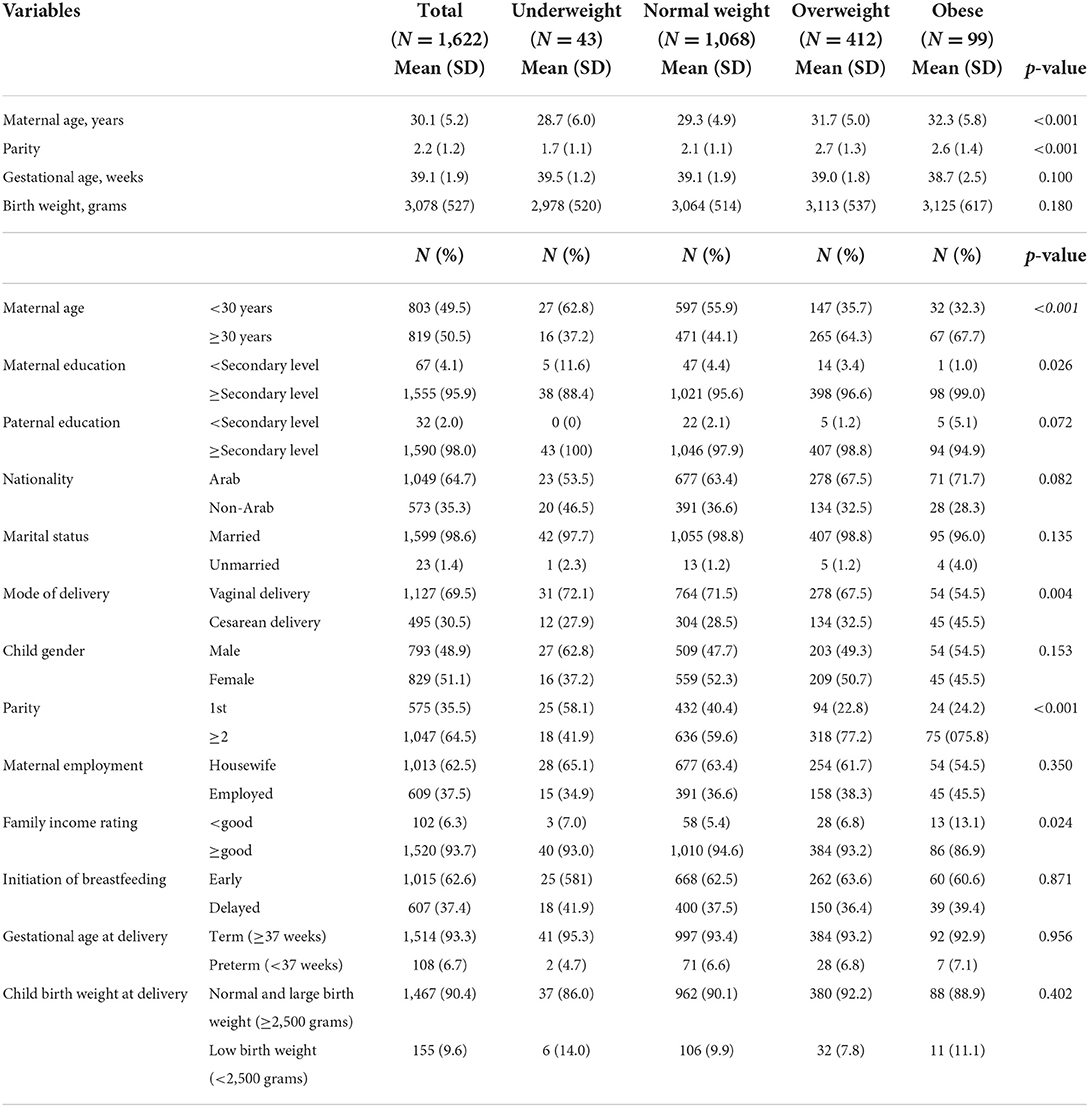
Table 1. Sociodemographic characteristics of the studied participants in the different pre-pregnancy BMI subgroups in Abu Dhabi, the United Arab Emirates.
In multi-nominal logistic regression analysis, mothers with advanced maternal age (AMA) (≥35 years) were more likely to be overweight odds ratio [OR] = 1.93 (95% CI 1.52–2.3) and obese OR = 2.15 (95% CI 1.32–3.39). Mothers with lower family income were more likely to be obese OR = 2.72 (95% CI 1.44–5.93). Mothers with high parity (≥2) were more likely to be overweight OR = 1.91 (95% CI 1.49–2.50) and obese OR = 1.76 (95% CI 1.06–2.92) and less likely to be underweight OR = 0.52 (95% CI 0.27–0.94). Obese mothers were more likely to deliver via CS OR = 1.95 (95% CI 1.27–2.96). Other adverse pregnancy outcomes such as preterm birth and LBW were not associated with abnormal BMI (i.e., underweight, overweight, and obesity).
Maternal education among the studied participants was not associated with BMI abnormality (Table 2).
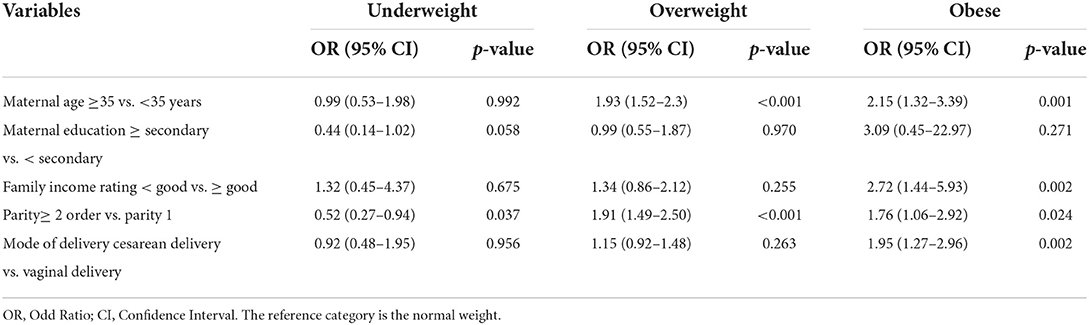
Table 2. Factors associated with underweight, overweight and obesity among studied participants in Abu Dhabi, the United Arab Emirates using multinomial logistic analysis.
Discussion
To the best of the authors' knowledge, this is the first comprehensive study on the epidemiology of pre-pregnancy BMI in Abu Dhabi, the UAE. Therefore, this work will be considered as an additional value to the few existing data published regarding pre-pregnancy BMI in the UAE (30). The main findings of current works were estimating the prevalence of pre-pregnancy BMI subgroups and exploring the possible associated factors (e.g., age, family income, parity, and CS) with abnormal pre-pregnancy BMI subgroups. More than one-third (34.2%) of the total participants (1,622) had abnormal pre-pregnancy BMI, i.e., underweight (2.7%), overweight (25.7%), and obesity (6.1%).
Compared to the recently published work in the UAE reporting a 59.4% pre-pregnancy BMI ≥25 kg/m2 (30), this study revealed less prevalence of overweight/obesity (31.8%). The discrepancies in the prevalence could be attributed to many reasons, such as the small sample size of the former study, which included only Emirates and Arab mothers' nationalities (30), unlike this study. A similar prevalence of normal pre-pregnancy BMI (63.5%) was reported by several studies, e.g., in Canada (65.8%) (15) and in France (64.2%) (23); however, the difference is within the abnormal pre-pregnancy BMI subcategories. A study in Saudi Arabia reported 29.7% normal BMI and a very high prevalence of pre-pregnancy overweight and obesity (31). Similar results of a high prevalence of pre-pregnancy overweight were observed in Qatar and Lebanon (32).
In this work, maternal education was positively associated with pre-pregnancy BMI in the univariate analysis. However, this association was not identified in the logistic regression analysis. The literature is contradictory regarding the association between maternal education and abnormal pre-pregnancy BMI (33, 34). For example, high maternal education was associated with overweight/obesity in Bangladesh (33). Whereas in Taiwan, it was the opposite (34). The influence of education on pre-pregnancy BMI could be attributed to the quality of education more than the class attended (< secondary or ≥secondary level).
In addition, mothers with lower family income were more likely to be obese OR = 2.72 (95% 1.44–5.93).
The literature results vary regarding the association between family income and obesity, some results go with high family income associated with obesity (32), and others (34) oppose this results. In support of this results, the strong correlation between lower-income and the risk of obesity was revealed in the literature even by meta-analysis (35). Besides, the coexistence of malnutrition, undernutrition, and over-nutrition, and its huge negative impact on the health and economy is common in low- and middle-income countries (36, 37).
Mothers with high parity (≥2) were also more likely to be overweight OR = 1.91 (95% 1.49–2.50), obese OR = 1.76 (95% 1.06–2.92), and less likely to be underweight OR = 0.52 (95% 0.27–0.94). Many studies, including the studied country, documented the strong correlation between higher parity and obesity (30, 34, 38, 39). A study in Denmark estimated that the average gained 0.62 BMI units after every additional birth (38). Therefore, increasing parity will be associated with increased overweight/obesity. Even the factors related to abnormal pre-pregnancy BMI are correlated, i.e., AMA with high parity (40) and AMA with CS (18). This results showed among mothers with high birth order, 1,047, 640 (61.1%) were older and high parity. Interestingly, high parity influences the mode of delivery in many ways. For example, high parity was reported to be associated with anemia (41) and CS (42).
The study revealed that obese mothers were almost twice as likely to deliver via cesarean section OR = 1.95 (95% 1.27–2.96). Furthermore, obesity decreased the chance of successful vaginal birth after cesarean section (VBAC) (43, 44). Many authors have documented the negative impact of obesity on pregnancy outcomes, including CS (34, 45–47). Besides, CS is correlated with adverse effects such as maternal mortality, perinatal morbidity, and mortality (48). In many settings, including the UAE, pre-pregnancy BMI was a common denominator in the etiology of excessive gestational weight gain (30, 34). In addition, pre-pregnancy obesity and greater weight gain independently increase the risk of CS (34, 49). Therefore, programs to reduce pre-pregnancy obesity might reduce the high rates of CS and good pregnancy outcomes. For instance, a study in Italy documented reducing the most adverse pregnancy outcomes when decreasing pre-pregnancy BMI (50).
Unlike this results, abnormal pre-pregnancy BMI, such as obesity and underweight, was found to be associated with some poor perinatal outcomes, e.g., LBW (13, 46), preterm birth (34, 46, 51), and poor breastfeeding practices, e.g., breastfeeding initiation and duration (52, 53), and gestational diabetes mellitus (GDM) (54). The variations between the current and previous results indicate the complexity of influencing abnormal pre-pregnancy BMI on maternal and perinatal and early child health. Such variations should encourage researchers to conduct more research to explore this complexity by estimating the magnitude of these abnormal BMI groups, finding the associated impacts, and motivating the involved parties to take appropriate actions to improve maternal and child health.
To our knowledge, this is the first comprehensive study tackling pre-pregnancy BMI epidemiology in Abu Dhabi, the UAE. This study revealed valuable information from a large sample of the community, which healthcare planners can use to improve maternal and child health by addressing the maintenance of a healthy BMI before, during, and after delivery to achieve good pregnancy outcomes. Hence, the results will help the health authorities in the UAE to ensure that they are providing the best guidance and care for pregnant women. In addition, the results underscore the need for culture-specific intervention programs to promote healthy body weight in women of childbearing age. More accurate and precise policies would be formulated on weight gain recommendations and weight monitoring during pregnancy.
However, our study has some limitations which are (a) the recall bias as the data collection included children up to 2 years old, (b) possible bias on these results due to missing data, and (c) not including the possible impact of BMI on maternal and child morbidity and mortality.
Conclusions
This study provides valuable information that can be used by policymakers as a tool to improve maternal and child health in order to maintain a normal BMI for a healthy pregnancy outcome. Additionally, there is a need to strengthen the available healthcare system for the overall prevention of obesity through primary care as a leading system and establish a structured network of specialized obesity centers. Moreover, developing guidelines on weight gain for optimizing pregnancy and neonatal outcomes will provide an excellent communication tool for healthcare experts, mothers, and children. Finally, additional intervention research is needed, including designed lifestyle programs to improve pregnancy outcomes.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by (ZU17_006_F) the Research Ethics Committee at Zayed University, the UAE. The patients/participants provided their written informed consent to participate in this study.
Author contributions
ZT designed the study and recruited the participants. ZT and AH analyzed the data and wrote the manuscript. DP contributed to the design of the study, data collection, and manuscript writing. All authors read, critically revised, and approved the final manuscript.
Funding
This research was funded by the research incentive fund (R17042) from the Research Office at Zayed University.
Acknowledgments
The authors would like to thank all of the mothers and children who participated in the study. Our gratitude is extended to the research assistants for their efforts.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
OR, Odds Ratios; BMI, Body Mass Index; CI, Confidence Interval; LBW, Low Birth Weight; CS, Cesarean Section; SD, Standard Deviation; SPSS, Statistical Package for Social Science; UAE, United Arab Emirates; WHO, World Health Organization.
References
1. Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. (2013) 382:427–51. doi: 10.1016/S0140-6736(13)60937-X
2. Radwan H, Ballout RA, Hasan H, Lessan N, Karavetian M, Rizk R. The epidemiology and economic burden of obesity and related cardiometabolic disorders in the United Arab emirates: a systematic review and qualitative synthesis. J Obes. (2018) 2018:2185942. doi: 10.1155/2018/2185942
3. Jahan F. Obesity in women: a challenge in Arab world. J Women's Health Care. (2016) 5:e116. doi: 10.4172/2167-0420.1000e116
4. Chen C-N, Chen H-S, Hsu H-C. Maternal prepregnancy body mass index, gestational weight gain, and risk of adverse perinatal outcomes in Taiwan: a population-based birth cohort study. Int J Environ Res Public Health. (2020) 17:1221. doi: 10.3390/ijerph17041221
5. Gaillard R, Durmuş B, Hofman A, Mackenbach JP, Steegers EA, Jaddoe VW. Risk factors and outcomes of maternal obesity and excessive weight gain during pregnancy. Obesity. (2013) 21:1046–55. doi: 10.1002/oby.20088
6. Begum KS, Sachchithanantham K, De Somsubhra S. Maternal obesity and pregnancy outcome. Clin Exp Obstet Gynecol. (2011) 38:14–20.
7. Robinson HE, O'Connell CM, Joseph KS, McLeod NL. Maternal outcomes in pregnancies complicated by obesity. Obstet Gynecol. (2005) 106:1357–64. doi: 10.1097/01.AOG.0000188387.88032.41
8. Lim CC, Mahmood T. Obesity in pregnancy. Best Pract Res Clin Obstet Gynaecol. (2015) 29:309–19. doi: 10.1016/j.bpobgyn.2014.10.008
9. Braun RD, Cnattingius S, Bergstrom R, Lipworth L, Kramer MS. Pre-pregnancy weight and the risk of adverse pregnancy outcome. New Eng J Med. (2009) 338:147–52. doi: 10.1080/00016340802303349
10. Cnattingius S, Villamor E, Johansson S, Bonamy A-KE, Persson M, Wikström A-K, et al. Maternal obesity and risk of preterm delivery. Jama. (2013) 309:2362–70. doi: 10.1001/jama.2013.6295
11. Mayor S. Being obese before conception triples odds of obese or overweight offspring, review finds. Br Med J Publ Group. (2019) 8:4187. doi: 10.1136/bmj.l4187
12. Amir LH, Donath S A. systematic review of maternal obesity and breastfeeding intention, initiation and duration. BMC Preg Childbirth. (2007) 7:1–14. doi: 10.1186/1471-2393-7-9
13. Murai U, Nomura K, Kido M, Takeuchi T, Sugimoto M, Rahman M. Prepregnancy body mass index as a predictor of low birth weight infants in Japan. Asia Pac J Clin Nutr. (2017) 26:434–7. doi: 10.6133/apjcn.032016.11
14. Han Z, Mulla S, Beyene J, Liao G, McDonald SD. Maternal underweight and the risk of preterm birth and low birth weight: a systematic review and meta-analyses. Int J Epidemiol. (2011) 40:65–101. doi: 10.1093/ije/dyq195
15. Vinturache A, Moledina N, McDonald S, Slater D, Tough S. Pre-pregnancy body mass index (BMI) and delivery outcomes in a Canadian population. BMC Preg- Childbirth. (2014) 14:1–10. doi: 10.1186/s12884-014-0422-y
16. World Health Organization. The World Health Report 2005, Statistical Annex. Geneva: World Health Organization (2005).
17. World Health Organization. World Health Statistics 2015. Geneva: World Health Organization (2015).
18. Taha Z, Ali Hassan A, Wikkeling-Scott L, Papandreou D. Prevalence and associated factors of caesarean section and its impact on early initiation of breastfeeding in Abu Dhabi, United Arab Emirates. Nutrients. (2019) 11:2723. doi: 10.3390/nu11112723
19. World Health Organization WHO. Statement on Caesarean Section Rates. Geneva: World Health Organization (2015).
20. O'Dwyer V, Farah N, Fattah C, O'Connor N, Kennelly MM, Turner MJ. The risk of caesarean section in obese women analysed by parity. Eu J Obst Gynecol Reprod Biol. (2011) 158:28–32. doi: 10.1016/j.ejogrb.2011.04.007
21. El-Chaar D, Finkelstein SA, Tu X, Fell DB, Gaudet L, Sylvain J, et al. The impact of increasing obesity class on obstetrical outcomes. J Obste Gynaecol Canada. (2013) 35:224–33. doi: 10.1016/S1701-2163(15)30994-4
22. Saadia Z. Association between maternal obesity and cesarean delivery complications. Cureus. (2020) 12:7163. doi: 10.7759/cureus.7163
23. Boudet-Berquier J, Salanave B, Desenclos J-C, Castetbon K. Sociodemographic factors and pregnancy outcomes associated with prepregnancy obesity: effect modification of parity in the nationwide Epifane birth-cohort. BMC Pregnancy Childbirth. (2017) 17:1–13. doi: 10.1186/s12884-017-1456-8
24. Kim SY, Dietz PM, England L, Morrow B, Callaghan WM. Trends in prepregnancy obesity in nine states, 1993-2003. Obesity. (2007) 15:986–93. doi: 10.1038/oby.2007.621
25. He Z, Bishwajit G, Yaya S, Cheng Z, Zou D, Zhou Y. Prevalence of low birth weight and its association with maternal body weight status in selected countries in Africa: a cross-sectional study. BMJ Open. (2018) 8:e020410. doi: 10.1136/bmjopen-2017-020410
26. de Alencar Britto RP, Florêncio TMT, Silva AAB, Sesso R, Cavalcante JC, Sawaya AL. Influence of maternal height and weight on low birth weight: a cross-sectional study in poor communities of northeastern Brazil. PLoS ONE. (2013) 8:e80159. doi: 10.1371/journal.pone.0080159
27. Heslehurst N, Ells LJ, Simpson H, Batterham A, Wilkinson J, Summerbell CD. Trends in maternal obesity incidence rates, demographic predictors, and health inequalities in 36,821 women over a 15-year period. BJOG: An Int J Obstet Gynaecol. (2007) 114:187–94. doi: 10.1111/j.1471-0528.2006.01180.x
28. Taha Z, Garemo M, Nanda J. Patterns of breastfeeding practices among infants and young children in Abu Dhabi, United Arab Emirates. Int Breastfeed J. (2018) 13:1–10. doi: 10.1186/s13006-018-0192-7
29. Organization WH. WHO : Global Database on Body Mass Index. Geneva: World Health Organization (2018).
30. Hashim M, Radwan H, Hasan H, Obaid RS, Al Ghazal H, Al Hilali M, et al. Gestational weight gain and gestational diabetes among Emirati and Arab women in the United Arab Emirates: results from the MISC cohort. BMC Preg Childbirth. (2019) 19:1–11. doi: 10.1186/s12884-019-2621-z
31. Wahabi H, Esmaeil S, Fayed A. maternal prepregnancy weight and pregnancy outcomes in Saudi women: subgroup analysis from Riyadh mother and baby cohort study (RAHMA). BioMed Res Int. (2021) 2021:5942. doi: 10.1155/2021/6655942
32. Abdulmalik MA, Ayoub JJ, Mahmoud A. collaborators M, Nasreddine L, Naja F. Pre-pregnancy BMI, gestational weight gain and birth outcomes in Lebanon and Qatar. Results of the MINA cohort. PLoS ONE. (2019) 14:e0219248. doi: 10.1371/journal.pone.0219248
33. Hashan MR, Gupta RD, Day B, Al Kibria GM. Differences in prevalence and associated factors of underweight and overweight/obesity according to rural–urban residence strata among women of reproductive age in Bangladesh: evidence from a cross-sectional national survey. BMJ Open. (2020) 10:4321. doi: 10.1136/bmjopen-2019-034321
34. Liang C-C, Chao M, Chang S-D, Chiu SY-H. Impact of prepregnancy body mass index on pregnancy outcomes, incidence of urinary incontinence and quality of life during pregnancy-An observational cohort study. Biomed J. (2020). doi: 10.1016/j.bj.2019.11.001
35. Kim TJ, von dem Knesebeck O. Income and obesity: what is the direction of the relationship? A systematic review and meta-analysis. BMJ open. (2018) 8:e019862. doi: 10.1136/bmjopen-2017-019862
36. Winichagoon P, Margetts BM. The Double Burden of Malnutrition in Low-and Middle-Income Countries. Energy Balance and Obesity. Lyon, FR: International Agency for Research on Cancer (2017).
37. Félix-Beltrán L, Macinko J, Kuhn R. Maternal height and double-burden of malnutrition households in Mexico: stunted children with overweight or obese mothers. Public Health Nutr. (2021) 24:106–16. doi: 10.1017/S136898002000292X
38. Li W, Wang Y, Shen L, Song L, Li H, Liu B, et al. association between parity and obesity patterns in a middle-aged and older Chinese population: a cross-sectional analysis in the Tongji-Dongfeng cohort study. Nutr Metab. (2016) 13:1–8. doi: 10.1186/s12986-016-0133-7
39. Taghdir M, Alimohamadi Y, Sepandi M, Rezaianzadeh A, Abbaszadeh S, Mahmud FM. Association between parity and obesity: a cross sectional study on 6,447 Iranian females. J Prev Med Hyg. (2020) 61:E476. doi: 10.15167/2421-4248/jpmh2020.61.3.1430
40. Ndiaye K, Portillo E, Ouedraogo D, Mobley A, Babalola S. High-risk advanced maternal age and high parity pregnancy: tackling a neglected need through formative research and action. GlobHealth: Sci Pract. (2018) 6:372–83. doi: 10.9745/GHSP-D-17-00417
41. Al-Farsi YM, Brooks DR, Werler MM, Cabral HJ, Al-Shafei MA, Wallenburg HC. Effect of high parity on occurrence of anemia in pregnancy: a cohort study. BMC Preg Child. (2011) 11:1–7. doi: 10.1186/1471-2393-11-7
42. Adam I, Kheiri S, Sharif ME, Ahmed AB, Rayis DA. Anaemia is associated with an increased risk for caesarean delivery. Int J Gynecol Obstet. (2019) 147:202–5. doi: 10.1002/ijgo.12946
43. Wilson E, Sivanesan K, Veerasingham M. Rates of vaginal birth after caesarean section: What chance do obese women have? Au New Zealand J Obstet Gynaecol. (2020) 60:88–92. doi: 10.1111/ajo.13003
44. Juhasz G, Gyamfi C, Gyamfi P, Tocce K, Stone JL. Effect of body mass index and excessive weight gain on success of vaginal birth after cesarean delivery. Obstet Gynecol. (2005) 106:741–6. doi: 10.1097/01.AOG.0000177972.32941.65
45. Al-Kubaisy W, Al-Rubaey M, Al-Naggar RA, Karim B, Noor NAM. Maternal obesity and its relation with the cesarean section: A hospital based cross sectional study in Iraq. BMC Preg Childbirth. (2014) 14:1–5. doi: 10.1186/1471-2393-14-235
46. Ratnasiri AW, Lee HC, Lakshminrusimha S, Parry SS, Arief VN, DeLacy IH, et al. Trends in maternal prepregnancy body mass index (BMI) and its association with birth and maternal outcomes in California, 2007–2016: a retrospective cohort study. PLoS ONE. (2019) 14:e0222458. doi: 10.1371/journal.pone.0222458
47. Wang X, Zhang X, Zhou M, Juan J, Wang X. Association of prepregnancy body mass index, rate of gestational weight gain with pregnancy outcomes in Chinese urban women. Nutr Metab. (2019) 16:1–9. doi: 10.1186/s12986-019-0386-z
48. Betran AP, Torloni MR, Zhang J, Ye J, Mikolajczyk R, Deneux-Tharaux C, et al. What is the optimal rate of caesarean section at population level? A systematic review of ecologic studies. Reproduct Health. (2015) 12:1–10. doi: 10.1186/s12978-015-0043-6
49. Seligman LC, Duncan BB, Branchtein L, Gaio DSM, Mengue SS, Schmidt MI. Obesity and gestational weight gain: cesarean delivery and labor complications. Rev Saude Publica. (2006) 40:457–65. doi: 10.1590/S0034-89102006000300014
50. Masturzo B, Franzè V, Germano C, Attini R, Gennarelli G, Lezo A, et al. Risk of adverse pregnancy outcomes by prepregnancy Body Mass Index among Italian population: a retrospective population-based cohort study on 27,807 deliveries. Arch Gynecol Obstet. (2019) 299:983–91. doi: 10.1007/s00404-019-05093-0
51. Vinturache A, McKeating A, Daly N, Sheehan S, Turner M. Maternal body mass index and the prevalence of spontaneous and elective preterm deliveries in an Irish obstetric population: a retrospective cohort study. BMJ Open. (2017) 7:e015258. doi: 10.1136/bmjopen-2016-015258
52. Masho SW, Cha S, Morris MR. Prepregnancy obesity and breastfeeding noninitiation in the United States: an examination of racial and ethnic differences. Breastfeed Med. (2015) 10:253–62. doi: 10.1089/bfm.2015.0006
53. Wojcicki JM. Maternal prepregnancy body mass index and initiation and duration of breastfeeding: a review of the literature. J Women's Health. (2011) 20:341–7. doi: 10.1089/jwh.2010.2248
Keywords: pre-pregnancy BMI, overweight, obesity, cesarean section, birth order, United Arab Emirates
Citation: Taha Z, Hassan AA and Papandreou D (2022) Epidemiology of pre-pregnancy body mass index (BMI) among mothers in Abu Dhabi, the United Arab Emirates. Front. Glob. Womens Health 3:893808. doi: 10.3389/fgwh.2022.893808
Received: 10 March 2022; Accepted: 08 August 2022;
Published: 13 September 2022.
Edited by:
Tabassum Firoz, Yale New Haven Health System, United StatesReviewed by:
Zacharoula Karabouta, University General Hospital of Thessaloniki AHEPA, GreeceEleni Andreou, University of Nicosia, Cyprus
Copyright © 2022 Taha, Hassan and Papandreou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zainab Taha, WmFpbmFiLlRhaGFAenUuYWMuYWU=
 Zainab Taha1*
Zainab Taha1* Dimitrios Papandreou
Dimitrios Papandreou