- 1Department of Psychiatry, College of Health and Medical Sciences, Haramaya University, Haramaya, Ethiopia
- 2Department of Epidemiology and Biostatistics, School of Public Health, College of Health and Medical Sciences, Haramaya University, Haramaya, Ethiopia
- 3Department of Public Health and Health Policy, School of Public Health, College of Health and Medical Sciences, Haramaya University, Haramaya, Ethiopia
Background: In Ethiopia, the magnitude of antenatal care (ANC) practice and institutional delivery is low as compared with developed countries. The majority of the pregnant women have not completed their ANC follow-up and only 43% of women have reached the four and above ANC. This study was conducted to determine the magnitude of ANC dropout and associated factors among pregnant women in Ethiopia.
Methods: Secondary data analysis was conducted using the 2019 Ethiopia Mini Demographic and Health Survey 2019 (2019 EMDHS). The sample was selected using a stratified, two-stage cluster sampling design and the data were analyzed using the binary logistic regression model to identify factors associated with ANC dropout. Adjusted odds ratio (AOR) with 95% CI was reported to declare significance and strength of association. A total weighted sample of 2,143 women who had antenatal care follow-up during pregnancy was included. In the multivariate logistic regression analysis, variables having a p-value < 0.05 were considered to have a significant association with ANC dropout.
Result: The magnitude of ANC dropout was 39.12% (95% CI: 37.07 and 41.20%) among women who had ANC follow-up in Ethiopia. Aged 30–49 years [AOR = 0.71; 95% CI: (0.54, 0.94)], attended primary [AOR = 0.79; 95% CI: (0.62, 0.99)], secondary [AOR = 0.63; 95% CI: (0.44, 0.87)], and higher education [AOR = 0.39; 95% CI: (0.25, 0.62)], were in first trimesters [AOR = 0.49; 95% CI: (0.40, 0.60)] at the time of first ANC visit, and had access to laboratory service [AOR = 0.25; 95% CI: (0.13, 0.51)] were found to be a negative significant associated factors of ANC dropouts, whereas being rural resident [AOR = 1.53; 95% CI: (1.11, 2.10)] has a positive significant association with ANC dropouts.
Conclusion: More than one-third of the pregnant women in Ethiopia had dropped out from their ANC follow-up in the study period. Being old-aged, educated, urban resident, having a first ANC visit in the first trimester, and having access to laboratory service were negatively associated with ANC dropouts. Therefore, we recommended encouraging women to have ANC visit at an early stage of pregnancy and conducting basic laboratory investigations during their visit. When undertaking that, due attention should be given to young, uneducated, and rural dweller women.
Background
Antenatal care (ANC) is the care provided by skilled healthcare professionals to pregnant women and adolescent girls in order to ensure the best health conditions for both the mother and baby during pregnancy (1). Since the introduction of focused antenatal care in 2002 by the WHO, there is a stunning change in the utilization of ANC follow-up in low- and middle-income countries and it was then recommended at least four ANC visits for pregnant women (2–4). ANC is one of the strategies designed to reduce neonatal mortality and maintain maternal health by teaching women to have more access to maternal health services and get ready for their newborns (5).
In low-income countries, the number of women attending antenatal care has gradually increased from 64% in 1990 to about 81% in 2009. However, only 39% of pregnant women attended four times or more antenatal care during 2000–2010. Maternal mortality was estimated at 216 globally and almost all (95%) happened in developing countries (6) and the rate was 412 in Ethiopia (7). Although the country has registered the dramatic change in reducing maternal and child mortality, the health of pregnant women and their children has remained a public health problem (8).
The health authority and governmental and nongovernmental organizations are paying attention and working toward reducing maternal and child mortality by providing a roadmap for ending preventable deaths of women, children, and adolescents by 2030 and helping them achieve their potential for and rights to health and wellbeing in all the settings (9). These strategies have three main objectives: ending preventable deaths, ensuring health and wellbeing, and expanding enabling environments, which were aligned with 17 targets within nine of the Sustainable Development Goals (10).
In Ethiopia, the magnitude of antenatal care practice and institutional delivery was low as compared with the ones in developed countries. The majority of the pregnant women have not completed their ANC follow-up and only 43% of women have reached the four and above ANC. Around 48% of the pregnant women had institutional delivery (11). Ongoing rates of dropout from their ANC follow-up have a negative impact on the pregnant women's health status and take the lion's share of high morbidity and mortality (11, 12).
The ANC dropout rate was more common in developing countries, particularly in sub-Saharan African countries where the ANC dropout rate was high (13, 14). Different scholars thought that various factors hindering the pregnant women make ANC dropout rate. Several studies suggested that socioeconomic factors such as poverty, accessibility of the health centers, lack of information about ANC, service quality, age at first birth, educational background, place of living, sociocultural, and individual factors directly affected the utilization of antenatal care follow-up services (15–19). Adequate utilization of the recommended antenatal care visits is a key to protecting both the mother and newborn from the adverse complications of pregnancy and childbirth. Despite this fact, there is a paucity of evidence on ANC dropout and associated factors at the national level in Ethiopia. Meanwhile, this study was conducted to find out about the magnitude of ANC dropout and its factors among pregnant women in Ethiopia using the 2019 Ethiopia Mini Demographic and Health Survey (2019 EMDHS) data.
Methods
Study Design and Setting
In the 2019 Ethiopia Mini Demographic and Health Survey (2019 EMDHS), a community-based cross-sectional study was carried out from 21 March 2019 to 28 June 2019. Nine regional states [Afar, Tigray, Amhara, Oromia, Somali, Southern Nations, Nationalities, and Peoples' Region (SNNPR), Benishangul Gumuz, Gambella, and Harari] and two city administrations (Addis Ababa and Dire Dawa) are found in the country.
Data Source
The Ethiopia Mini Demographic and Health Survey (EMDHS) data were used as a secondary data source for this study. A stratified two-stage cluster sampling was taken as the data source. Randomly, the enumeration areas (EAs) were selected in the first stage and then households were selected in the second stage. The target population for this study was all women who had any antenatal care in Ethiopia and those women in the selected enumeration areas (EAs) were the study population. Accordingly, a total weighted sample of 2,143 women who had antenatal care follow-up during their pregnancy was taken for this study.
Study Variables
In this study, antenatal care (ANC) dropout was taken as the outcome variable. Those women who did not complete the recommended visits during their pregnancy (a minimum of four visits for normal pregnancy) were considered “Yes” for ANC dropout unless it was coded as “No” for the outcome variable. Age, religion, marital status, educational level, place of residence, region, wealth index, sex of head of household, age of head of household, the timing of 1st antenatal check, and getting laboratory investigation were considered expiratory variables in this study.
Data Processing and Statistical Analysis
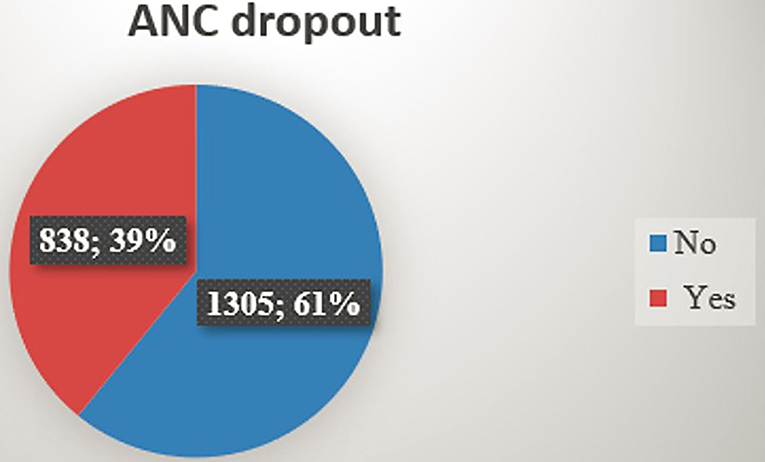
After data were extracted, editing, coding, and cleaning were done using Stata software version 16.0. The data were weighted using sampling weight (women's sample weight), primary sampling unit, and strata. Descriptive statistics and summary statistics were shown in the form of text, figures, and tables. Besides, the proportion of ANC dropout was presented using a pie chart.
Since the data had hierarchical and clustering nature, the mixed effect logistic model (multilevel model) was fitted to identify factors associated with ANC dropout. Due to the fact that the rate of ANC dropout varies from cluster to cluster, a cluster-level random intercept was introduced in the mixed effect logistic model. The within-cluster correlation was measured using the intracluster correlation coefficient (ICC), which is expected to be ≥10% to use the model. But, the ICC value was 7.77, which told us to select a fixed model (binary logistic regression model) over the mixed model. Variables having a p-value < 0.05 were considered as having a significant association with the ANC dropout. Model adequacy was also checked using Hosmer–Lemeshow test, which is expected to be ≥ 0.05 to say that the model is adequate.
Results
Characteristics of the Study Participants
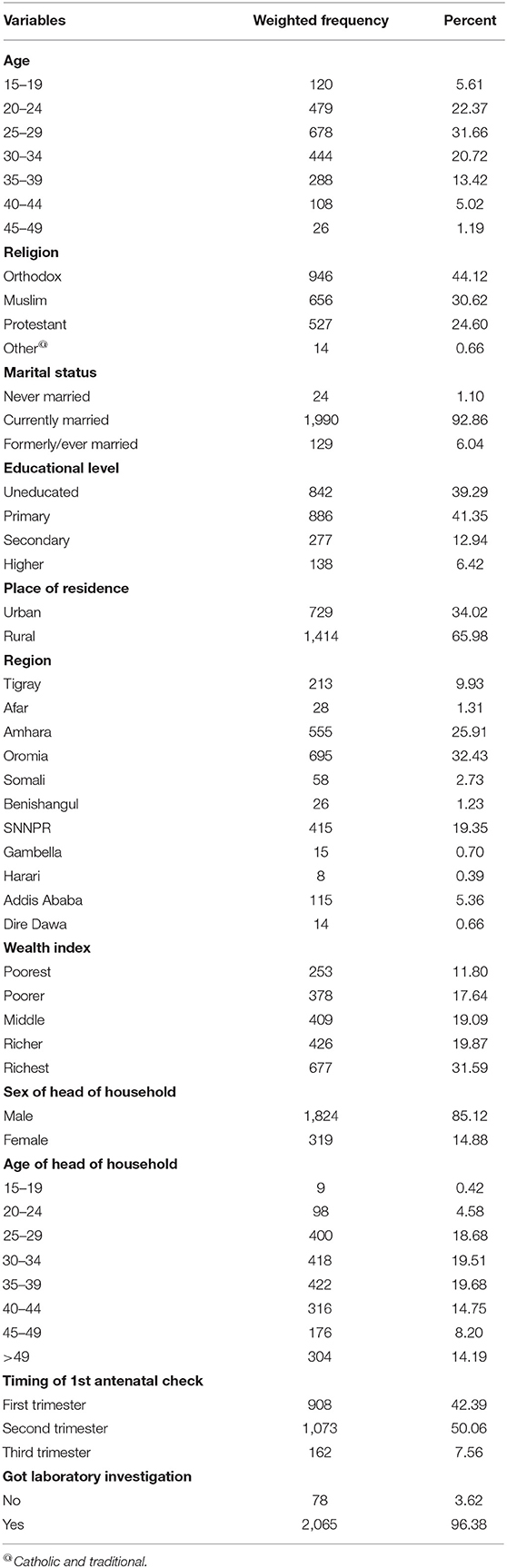
The mean age of women who attended ANC follow-up in Ethiopia was 28.21 (±6.31 SD) and the average number of living children was 3.00 (±2.06). The majority of the mothers (91%) were married and 44.12% of them were orthodox. Nearly two-thirds (65.98%) of the respondents were from the rural areas. Eighty-five percentage of heads of the households were male and their mean age was 37.54 years (±12.6 SD). Nearly one-third (29.44%) of the mothers were from poor wealth index and 40.1% of the mothers were uneducated. Regarding the ANC follow-up, 50.05 and 7.56% of the respondents got their first visit in the second and third trimesters, respectively. Moreover, 96.38% of the mothers were sent to the laboratory during the ANC visits (Table 1).
Magnitude of Antenatal Care Dropout
The magnitude of ANC dropout was 39.12% (95% CI: 37.07 and 41.20%) among women who had antenatal care follow-up in Ethiopia (Figure 1).
Factors Associated With Antenatal Care Dropout Among Pregnant Mothers in Ethiopia
In the multivariate logistic regression model, age, educational status, place of residence, the region where the mothers lived, gestational age at the time of 1st antenatal care visit, and access to laboratory service were found to be the significant associated factors of ANC dropout after controlling the confounder effect (Table 2).
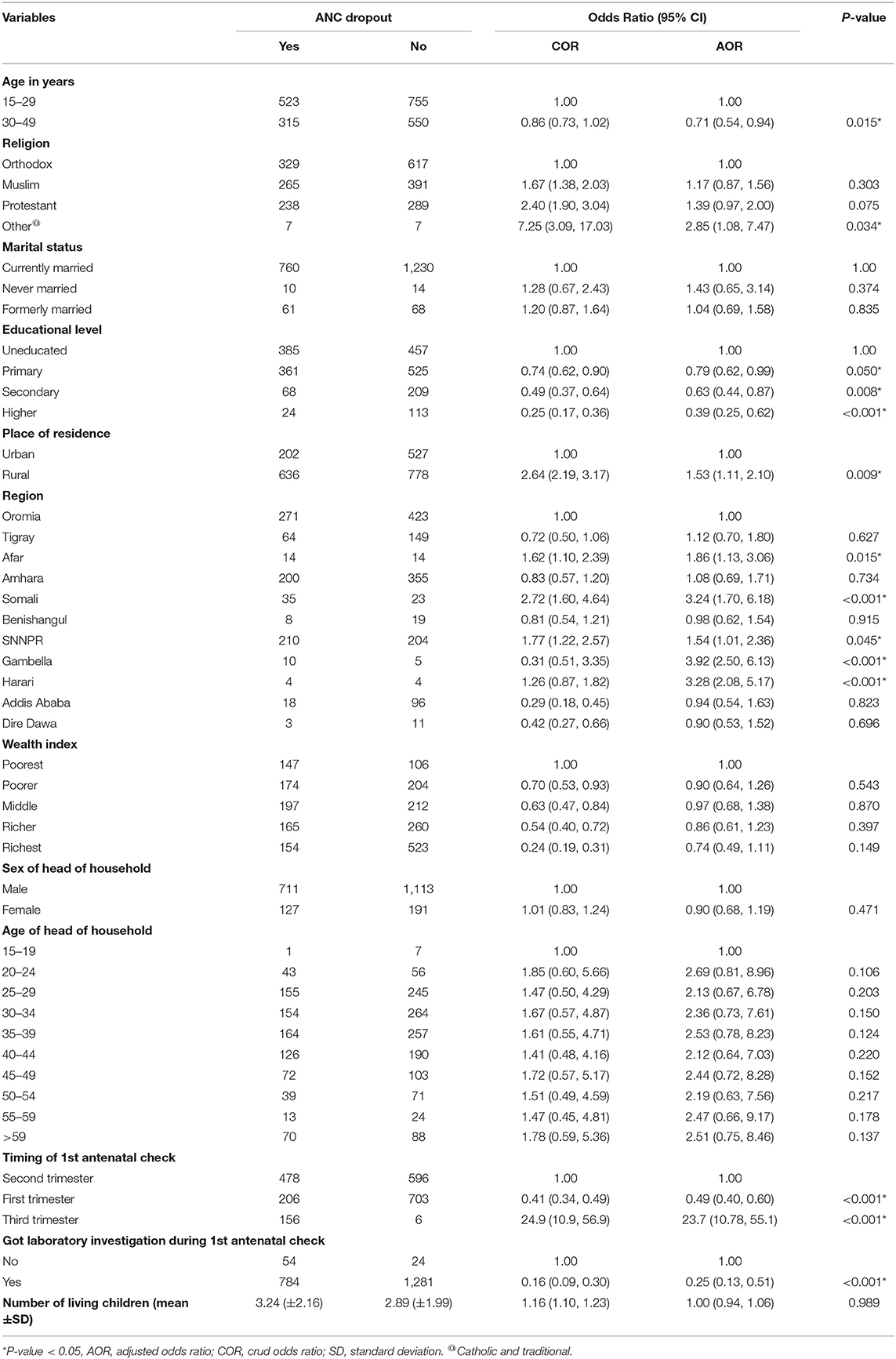
Table 2. The bivariate and multivariate logistic regression analysis of ANC dropout among pregnant women in Ethiopia in 2021.
The odds of ANC dropout decreased by 21% [adjusted odds ratio (AOR) = 0.79 (0.62, 0.99)], 37% [AOR = 0.63 (9.44, 0.87)], and 61% [AOR = 0.39 (0.25, 0.62)] among pregnant mothers who were on ANC follow-up and who had primary, secondary, and higher education, respectively, as compared to pregnant mothers with no formal education. The likelihood of ANC dropout was 1.53 times [AOR = 1.53 (1.11, 2.10)] higher among the pregnant mothers who lived in rural areas as compared with the pregnant mothers who lived in urban areas.
The odds of ANC dropout were 1.86 [AOR = 1.86 (1.13, 3.06)], 3.24 [AOR = 3.24 (1.70, 6.18)], 1.54 [AOR = 1.54 (1.01, 2.36)], 3.92 [AOR = 3.92 (2.50, 6.13)], and 3.28 times [AOR = 3.28 (2.08, 5.17)] higher in Afar, Somali, SNNPR, Gambella, and Harari among pregnant mothers as compared to the mothers who lived in Oromia at the time of the survey. The likelihoods of defaulting the ANC services were 39% [AOR = 0.71; 95% CI: (0.54, 0.94)] lower among the pregnant mothers aged between 30 and 49 years as compared with the pregnant mothers aged between 15 and 29 years.
The gestational age at the time of the visit was another significant associated factor for ANC dropout. The odds of ANC dropout decreased by 51% [AOR = 0.49 (0.40, 0.60)] for the mothers who started ANC visit in the first trimester of their pregnancy as compared with the mothers who started ANC visit in the second trimester of their pregnancy. However, the odds of ANC dropout were 23.7 times [AOR = 23.7 (10.78, 55.1)] higher for the pregnant mothers who had their first ANC visit in the third trimester as compared with the pregnant mothers who had their first ANC visit in the second trimester.
The likelihood of defaulting from ANC service decreased by 75% [AOR = 0.25 (0.13, 0.51)] for the mothers who have received laboratory service at the time of the survey as compared with the mothers who did not receive laboratory service at the time of the survey.
Discussion
This study assessed the magnitude and associated factors of ANC dropout using the 2019 EMDHS data. Accordingly, the magnitude of ANC dropout among women on ANC follow-up in Ethiopia was found to be 39.12% (95% CI: 37.07 and 41.20%). The finding is higher than previous studies conducted in Debre Markos (32.2%) (18) and Nigeria (16). This might be due to the difference in accessibility and quality of maternal health services. The Debre Markos study was conducted among urban women in Debre Markos where the accessibility and quality of maternal health services are better, whereas the current study was conducted among the general population of women in Ethiopia. Regarding the study in Nigeria, women tend to have higher access to maternity care and lower dropout due to higher socioeconomic status. This implies that though Ethiopian pregnant mothers have access to health institutions, there is a significant gap in keeping the continuum of maternal care.
The current study also identified factors associated with ANC dropout. Pregnant mothers who were on ANC follow-up and who had primary, secondary, and higher education were less likely to drop out from recommended ANC visits compared to those with no formal education. This finding is in line with previous studies carried out in the Enemay district of Ethiopia (20), Pakistan (17), and Egypt (21). This might be due to the positive association between women's education and ANC service. Those with better knowledge of the importance and adequacy of ANC services are more likely to utilize the recommended number of ANC visits (22). This might imply that educating women will increase the utilization of ANC services.
The likelihood of ANC dropout is higher among pregnant mothers from rural area. This finding is in agreement with previous studies in Nigeria (23, 24) and Indonesia (25) and this might be due to the low accessibility of ANC service in rural areas. The other reason might be being far away from health facilities and multiple responsibilities among most women in rural area that hinder them to get enough time for seeking the service.
Pregnant women in Afar, Somali, SNNPR, Gambella, and Harari regions had higher odds of ANC dropout compared to the women who lived in Oromia regional state. The reason for this discrepancy could be the difference in accessibility and quality of service across different geographical regions of Ethiopia. This could be evidenced by a higher number of health facilities in the region compared to other regions of Ethiopia (26).
The age of women was another variable significantly associated with ANC dropout. Pregnant women of higher age were at lower odds of ANC dropout. This finding is similar to the result from a previous study (27) and this might be explained by the fact that women of higher age are more likely to have the autonomy in healthcare decision-making that enables them to decide for receiving the care by themselves, which, in turn, increases the chance of pregnant women to use ANC services. This implies that early age at marriage also adversely affects ANC utilization.
This study revealed that the odds of ANC dropout is lower for the mothers who started ANC visit early in the first trimester of their pregnancy. This might be justified by early ANC visit that provides an opportunity for women to get information on the importance of ANC services and subsequent schedules and this could motivate and encourage them to have the recommended number of ANC visit (28, 29).
The likelihood of defaulting from ANC service was lower for the women who received laboratory service at the time of the survey as compared to those mothers who did not receive the laboratory service at the time of the survey. This result is in agreement with previous studies in Senegal (30) and this might be explained by the fact that those women who received laboratory service had a chance to get professional advice based on laboratory findings and this could increase women's understanding of the importance of ANC and their health condition, which, in turn, encourages women to complete their ANC follow-up.
The main limitation of the current study was that it was conducted based on secondary data; thus, we could not include information on some of the important variables such as the quality of ANC services and women's decision-making autonomy among others. The lack of sufficient literature on the topic was among the additional limitations faced for comparison of our findings with previous studies in the discussion part.
Conclusion
More than one-third of the pregnant women in Ethiopia have dropped out from their ANC follow-up in the study period. Being old-aged, educated and urban residents, having the first ANC visit in the first trimester, and having access to laboratory services were positively associated with ANC dropouts. Therefore, we recommended encouraging women to have ANC visit at an early stage of pregnancy and conducting basic laboratory investigations during their visit. When undertaking that, due attention should be given to the young, uneducated, and rural dweller women, particularly, in Afar, Somali, SNNPR, Gambella, and Harari regions.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author Contributions
The conception of the work, design of the work, acquisition of data, analysis, and interpretation of data were conducted by BT. Data curation, drafting the article, revising it critically for intellectual content, validation, and final approval of the version to be published were done by MW, BT, AW, NB, and DE. All authors have read and approved the final version of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We acknowledge the DHS for giving us the data for the study area.
References
1. World Health Organization. WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience (2016).
3. World Health Organization. WHO Antenatal Care Randomized Trial: Manual for the Implementation of the New Model. Report No.: 9241546298 (2002).
4. Villar J, Bergsjo P. WHO Antenatal Care Randomized Trial: Manual for the Implementation of the New Model. Geneva: WHO (2002). 37 p.
5. Bergsj P. What is the evidence for the role of antenatal care strategies in the reduction of maternal mortality and morbidity. Safe Motherhood Strat Rev Evid. (2001) 35–54.
6. Howden-Chapman P, Siri J, Chisholm E, Chapman R, Doll CN, Capon A. SDG 3: Ensure Healthy Lives and Promote Wellbeing for All at All Ages. France: International Council for Science (2017). p. 81–126.
7. Csa I. Central Statistical Agency (CSA) [Ethiopia] and ICF. Addis Ababa; Calverton, MD: Ethiopia Demographic and Health Survey (2016).
9. Every Woman Every Child. The Global Strategy for Women's, Children's and Adolescents Health (2015).
10. Bexell M, Jönsson K (editors). Responsibility and the United Nations' Sustainable Development Goals. Forum for Development Studies. Taylor & Francis (2017).
11. Institute EPH ICF. Ethiopia Mini Demographic and Health Survey 2019: Key Indicators. Rockville, MD: EPHI, ICF (2019).
12. Shibre G, Idriss-Wheeler D, Yaya S. Inequalities and trends in neonatal mortality rate (NMR) in Ethiopia: evidence from the Ethiopia Demographic and Health Surveys, 2000–2016. PLoS ONE. (2020) 15:e0234483. doi: 10.1371/journal.pone.0234483
13. Okethwangu D, Opigo J, Atugonza S, Kizza CT, Nabatanzi M, Biribawa C, et al. Factors associated with uptake of optimal doses of intermittent preventive treatment for malaria among pregnant women in Uganda: analysis of data from the Uganda Demographic and Health Survey, 2016. Malar J. (2019) 18:1–8. doi: 10.1186/s12936-019-2883-y
14. Hakizimana D, Nisingizwe MP, Logan J, Wong R. Identifying risk factors of anemia among women of reproductive age in Rwanda–a cross-sectional study using secondary data from the Rwanda demographic and health survey 2014/2015. BMC Public Health. (2019) 19:1–11. doi: 10.1186/s12889-019-8019-z
15. Grodzinsky A, Florio K, Spertus JA, Daming T, Schmidt L, Lee J, et al. Maternal mortality in the United States and the HOPE Registry. Curr Treat Options Cardiovasc Med. (2019) 21:1–6. doi: 10.1007/s11936-019-0745-0
16. Akinyemi JO, Afolabi RF, Awolude OA. Patterns and determinants of dropout from maternity care continuum in Nigeria. BMC Pregn Childb. (2016) 16:1–11. doi: 10.1186/s12884-016-1083-9
17. Iqbal S, Maqsood S, Zakar R, Zakar MZ, Fischer F. Continuum of care in maternal, newborn and child health in Pakistan: analysis of trends and determinants from 2006 to 2012. BMC Health Serv Res. (2017) 17:189. doi: 10.1186/s12913-017-2111-9
18. Amare NS, Araya BM, Asaye MM. Dropout from maternity continuum of care and associated factors among women in Debre Markos town, Northwest Ethiopia. bioRxiv. (2019) 620120. doi: 10.1101/620120
19. Singh K, Story WT, Moran AC. Assessing the continuum of care pathway for maternal health in South Asia and sub-Saharan Africa. Matern Child Health J. (2016) 20:281–9. doi: 10.1007/s10995-015-1827-6
20. Shitie A, Assefa N, Dhressa M, Dilnessa T. Completion and factors associated with maternity continuum of care among mothers who gave birth in the last one year in Enemay District, Northwest Ethiopia. J Pregn. (2020) 2020. doi: 10.1155/2020/7019676
21. Hamed A, Mohamed E, Sabry M. Egyptian status of continuum of care for maternal, newborn, and child health: Sohag Governorate as an example. Int J Med Sci Public Health. (2018) 7:1. doi: 10.5455/ijmsph.2018.0102607032018
22. Ali SA, Dero AA, Ali S, Ali G. Factors affecting the utilization of antenatal care among pregnant women: a literature review. J Preg Neonatal Med. (2018) 2.
23. Adewuyi EO, Auta A, Khanal V, Bamidele OD, Akuoko CP, Adefemi K, et al. Prevalence and factors associated with underutilization of antenatal care services in Nigeria: a comparative study of rural and urban residences based on the 2013 Nigeria demographic and health survey. PLoS ONE. (2018) 13:e0197324. doi: 10.1371/journal.pone.0197324
24. Babalola BI. Determinants of urban-rural differentials of antenatal care utilization in Nigeria. Afr Popul Stud. (2014) 28:1263–73. doi: 10.11564/0-0-614
25. Titaley CR, Dibley MJ, Roberts CL. Factors associated with underutilization of antenatal care services in Indonesia: results of Indonesia Demographic and Health Survey 2002/2003 and 2007. BMC Public Health. (2010) 10:1–10. doi: 10.1186/1471-2458-10-485
26. Brhane M, Kassahun G. Hospital Service in Ethiopia and Its Spatial Distribution Around the Ethiopia. Insight Medical Publishing Group (2021).
27. Worku D, Teshome D, Tiruneh C, Teshome A, Berihun G, Berhanu L, et al. Antenatal care dropout and associated factors among mothers delivering in public health facilities of Dire Dawa Town, Eastern Ethiopia. BMC Pregn Childb. (2021) 21:1–8. doi: 10.1186/s12884-021-04107-7
28. Tesfu AA, Aweke AM, Gela GB, Wudineh KG, Beyene FY. Factors associated with timely initiation of antenatal care among pregnant women in Bahir Dar city, Northwest Ethiopia: Cross-sectional study. Nursing Open. (2022) 9:1210–7. doi: 10.1002/nop2.1162
29. Belayneh T, Adefris M, Andargie G. Previous early antenatal service utilization improves timely booking: cross-sectional study at university of Gondar hospital, northwest Ethiopia. J Pregn. (2014) 2014. doi: 10.1155/2014/132494
Keywords: ANC dropout, pregnant women, Ethiopia, Demographic and Health Survey data, DHS
Citation: Tariku M, Tusa BS, Weldesenbet AB, Bahiru N and Enyew DB (2022) More Than One-Third of Pregnant Women in Ethiopia Had Dropped Out From Their ANC Follow-Up: Evidence From the 2019 Ethiopia Mini Demographic and Health Survey. Front. Glob. Womens Health 3:893322. doi: 10.3389/fgwh.2022.893322
Received: 02 April 2022; Accepted: 21 June 2022;
Published: 14 July 2022.
Edited by:
Patrick Musonda, University of Zambia, ZambiaReviewed by:
Choolwe Jacobs, University of Zambia, ZambiaGodfred O. Boateng, University of Texas at Arlington, United States
Copyright © 2022 Tariku, Tusa, Weldesenbet, Bahiru and Enyew. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Daniel Berhanie Enyew, YmVyaGFuaWVkQGdtYWlsLmNvbQ==
 Mandaras Tariku
Mandaras Tariku Biruk Shalmeno Tusa
Biruk Shalmeno Tusa Adisu Birhanu Weldesenbet
Adisu Birhanu Weldesenbet Nebiyu Bahiru
Nebiyu Bahiru Daniel Berhanie Enyew
Daniel Berhanie Enyew