
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CURRICULUM, INSTRUCTION, AND PEDAGOGY article
Front. Glob. Womens Health , 05 April 2022
Sec. Maternal Health
Volume 3 - 2022 | https://doi.org/10.3389/fgwh.2022.880615
 Alexandra C. Viner1*
Alexandra C. Viner1* Gladys Membe-Gadama2
Gladys Membe-Gadama2 Sonia Whyte3
Sonia Whyte3 Doris Kayambo4
Doris Kayambo4 Martha Masamba2
Martha Masamba2 Enita Makwakwa5
Enita Makwakwa5 David Lissauer6,7
David Lissauer6,7 Sarah J. Stock8
Sarah J. Stock8 Jane E. Norman9
Jane E. Norman9 Rebecca M. Reynolds10
Rebecca M. Reynolds10 Brian Magowan11
Brian Magowan11 Bridget Freyne12
Bridget Freyne12 Luis Gadama2 on behalf of the DIPLOMATIC Collaboration
Luis Gadama2 on behalf of the DIPLOMATIC CollaborationIntroduction: Although ultrasound to determine gestational age is fundamental to the optimum management of pregnancy and is recommended for all women by the World Health Organisation, it remains unavailable to many women in low-income countries where trained practitioners are scarce. This study aimed to evaluate a novel, context-specific education package to teach midwives basic obstetric ultrasound, including the determination of gestational age by measurement of fetal femur length.
Methods: The study was conducted across six sites in Malawi in January 2021. Following a virtual “training of the trainers”, local teams delivered a 10-day programme encompassing both didactic and “hands on” components. Matched pre and post course tests assessed participants' knowledge of key concepts, with Objective Structured Clinical Examinations used to evaluate practical skills. To achieve a pass, trainees were required to establish the gestational age to within ±7 days of an experienced practitioner and achieve an overall score of >65% on five consecutive occasions. A matched pre and post course survey explored participants' attitudes and confidence in performing ultrasound examinations.
Results: Of the 29 midwives who participated, 28 finished the programme and met the criteria specified to pass. 22 midwives completed the matched knowledge tests, with the mean (SD) score increasing from 10.2 (3.3) to 18 (2.5) after training (P <0.0001). Mean difference 7.9, 95% CI 6.5–9.2. Midwives passed 87% of the Observed Structured Clinical Examinations, establishing the gestational age to within ±7 days of an experienced practitioner in 89% of assessments. Beliefs regarding the importance of antenatal ultrasound increased post course (p = 0.02), as did confidence in performing ultrasound examinations (p <0.0001).
Conclusion: This study demonstrates not only that ultrasound-naive practitioners can be taught to perform basic obstetric ultrasound dating scans, confidently and competently, after 10 days of training, but also that local teams can be orientated to successfully deliver the programme virtually. Previous ultrasound training initiatives, while often more comprehensive in their syllabus, have been of considerably longer duration and this is likely to be a barrier to upscaling opportunities. We propose that this focused training increases the potential for widescale and sustainable implementation.
As a fundamental component of obstetric and neonatal care, the World Health Organisation (WHO) has regularly cited the need for improved estimates of gestational age in low- and middle- income countries (LMICs) as a public health priority (1–3), not only to enhance clinical care but also to strengthen the global reporting of pregnancy complications and to facilitate the evaluation of context-specific interventions to improve outcomes.
There are a number of different ways to determine gestational age but early pregnancy ultrasound is considered the most precise (4–7). Despite WHO guidance recommending that all women receive an ultrasound scan prior to 24 weeks to “estimate gestational age, improve detection of fetal anomalies and multiple pregnancies and reduce induction of labor for post term pregnancy” (8), this remains unavailable to many women living in LMICs. In these settings, gestational age is derived from either the last menstrual period (LMP) or by abdominal palpation, both of which are substantially less accurate than ultrasound (9–11). Scaled provision of ultrasound is challenging for a number of reasons (12–17) ranging from economical and geographical, to human factors and healthcare infrastructures (18). Indeed, one of the most frequently cited barriers is the lack of trained practitioners (14, 15). Despite a number of previous programmes demonstrating success in training healthcare workers to perform obstetric ultrasound, the length and complexity of many programmes has been prohibitive, with practitioners struggling to secure cover for their clinical duties in order to provide or attend training (14, 15, 19).
This study evaluated a novel training programme designed to teach ultrasound-naive healthcare practitioners' basic obstetric ultrasound, using fetal femur length to determine gestational age. We explored the ability of midwives to perform and interpret ultrasound examinations. We assessed the accuracy of their fetal measurements compared to experienced practitioners and evaluated post course changes in their knowledge and confidence. Our hypothesis was that midwives could be trained to competency within 2 weeks. We also reviewed the quality of images obtained over the following 3 months and evaluated skill retention by repeating written and practical assessments at the end of this period.
Our programme was designed to teach ultrasound-naive midwives in LMIC settings to perform the basics of obstetric ultrasound, including:
- The safe and appropriate use of an ultrasound machine
- The identification of number of fetuses
- The confirmation of fetal viability
- The confirmation of fetal presentation
- The determination of gestational age and estimated date of delivery by measurement of the fetal femur length (FL)
- The upkeep and secure storage of the ultrasound machines
The training programme was based on pilot work undertaken in Malawi in early 2020 and included both didactic and practical components. The first day and a half comprised of intense “classroom based” sessions, followed by eight and a half days of practical “hands on” experience. Details of these sessions are shown in Table 1. Simulation sessions using bespoke low-cost phantoms were incorporated into the “classroom” component, not only to help familiarize trainees with the machines, but also to help them develop confidence with probe manipulation prior to scanning volunteers. Small group sessions were intended to encourage discussion and team problem solving, as well as to encourage trainees to take ownership of the service and to anticipate and troubleshoot what they envisaged may be barriers to the implementation of ultrasound in their facilities.
The “hands on” sessions were conducted at the individual facilities, during which trainees had the opportunity to perform directly supervised ultrasound examinations on client volunteers. Feedback was provided in real-time and, as their skills evolved, trainees were supported to perform their scans with increasing independence. To complement the training, trainees were provided with a comprehensive printed handbook containing all of the information relayed in the lectures. Laminated sheets encompassing key concepts were also made available with each of the ultrasound machines as aide memoires.
In the absence of a universally accepted definition of what constitutes competency in obstetric ultrasound, our group reached a consensus agreement based on previous initiatives (20–24). Trainees were evaluated by way of Observed Structured Clinical Examinations (OSCEs) and their ability to determine the gestational age of clients to within ±7 days of the trainers. The OSCE comprised of 17 components mapped to the curriculum, with five tasks considered “essential”. To pass, the trainee was required to achieve an overall score of 11 (65%) or greater, correctly perform all 5 of the “essential” tasks and determine gestational age to within ±7 days of the gestational age assessed by their trainer. Both trainers and trainees were blinded to the measurements and gestational age until the end of the examination. Once trainees performed five consecutive examinations fulfilling these criteria, they were deemed competent to perform these basic ultrasound scans independently. Details of the OSCE components are shown in Table 2, with the “essential” tasks depicted in bold. A flowchart illustrating the protocol for assessment of competency is shown in Figure 1.
The training was conducted in January-February 2021 as part of a “parent” study exploring what factors may influence the upscale of basic antenatal ultrasound in LMIC settings (PACTR202010788566263). The project ran across 6 health facilities in Malawi, selected to encompass both urban and rural facilities. These included 3 sites in Blantyre, 1 in Lilongwe and 2 in the northern district of Karonga.
Fifteen local trainers were recruited to facilitate the course based on the following predefined criteria, kept intentionally broad to reflect the general paucity of trained practitioners in many LMIC settings. They should be an obstetrician (trainee or consultant), radiologist, sonographer, midwife or clinical officer, who has received training in basic obstetric ultrasound (via a formal or apprenticeship model) and who has performed independent obstetric ultrasound for a minimum of 1 year. They must also be capable and confident to troubleshoot any problems the trainees may encounter performing scans.
Nine of the trainers were doctors in obstetrics and gynecology, four were clinical officers, one a radiographer and one a clinical associate. Eleven had received formal training in obstetric ultrasound, with the remaining three taught “on the job”. They had an average of 5.9 years' experience in performing obstetric ultrasound, ranging from 1.5 to 16 years. All trainers attended a “training of the trainers” session, held virtually as a result of COVID-19 restrictions. All were provided with a detailed training manual and complied with the same standard operating procedures. A ratio of 1:4 trainers to trainees was maintained for all “hands on” sessions.
Twenty-nine midwives were selected to participate by their local District Nursing Officer (DNO), based on their role as a key provider of antenatal care to women at the participating facilities and their engagement in service improvement. In order to preserve the continuity of subsequent scanning services, we sought to train a minimum of four midwives per site. Unfortunately, in order to ensure the ongoing provision of routine clinical care at the facilities during the training period, not all midwives at each site were able to participate. All held either a Degree or Diploma in Nursing and Midwifery and none had any previous experience of using ultrasound. They had an average of 10.5 years of experience, ranging from 1 to 30 years, representative of the skill mix working within the participating facilities.
“Hands on” sessions were made possible thanks to client volunteers, eligible to participate if they were over 18 years old, thought to be over 14 weeks gestation and able to provide informed written consent. They were provided with a small allowance to cover their travel expenses, and each was allocated a unique identification number to maintain their confidentiality.
All training was complete by the end of February 2021, with remote supervision and image review provided for the following 3 months. To assess the ongoing quality of the ultrasound examinations, trainees were required to submit images for regular review. Images were assessed by two independent reviewers who were experienced in obstetric ultrasound and blinded to the midwife submitting the image. If the reviewer was confident that the image was that of a femur, they went on to assess the quality of the image using the following criteria;
- The femur should be displayed horizontally at an angle <45 degrees
- Both ends of the femur should be clearly visible
- The femur should fill >50% of the ultrasound images
- If depicted, the calipers should be correctly placed
If the reviewer did not consider the image to be clearly that of a femur, the image was deemed unacceptable, and no further assessment of that image was performed. Of those that were rated, a score of 2 out 3 was deemed acceptable for those without calipers and 3 out of 4 if calipers were shown. Scores and comments were fed back to the trainees weekly.
Prior to the training, each trainee undertook a 24-question multiple choice knowledge test to assess their theoretical understanding of ultrasound, scanning technique and basic fetal anatomy. They also completed a questionnaire using a 5-point Likert scale (1 = Strongly Disagree, 5 = Strongly Agree) to assess their attitude toward and confidence using ultrasound. Both assessments were repeated immediately after completion of the training and again 3 months later.
Data was analyzed using SPSS (IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY: IBM Corp). Matched pre and post course knowledge tests were analyzed using paired t-tests, with a Bland Altman plot used to assess the level of agreement between the gestational ages assigned by the trainees vs. those obtained by the trainers. Within the pre and post course questionnaires, questions evaluating similar concepts, for example confidence, were allocated into four groups for analysis, with the reliability of these groupings tested using Cronbach's alpha. If scoring >0.8, these were then analyzed as a group using a Wilcoxon signed rank test. If a group did not demonstrate adequate reliability, scoring <0.8, the statements were analyzed as single items. Intraclass correlation coefficients (ICC) were used to assess the inter-rater reliability of the reviewers assessing the follow up scans. A p-value <0.05 was considered statistically significant.
All participants (trainees and client volunteers) provided informed written consent, with participant information leaflets and consent forms available in both Chichewa and Tumbuka, as well as in English. As key stakeholders, the Ministry of Health in Malawi and the District Health Officers of the participating sites were involved in the conception of the project and supportive of its implementation. This study was approved by the University of Edinburgh and the University of Malawi—College of Medicine Research and Ethics Committee (COMREC) P08/19/2768.
At the end of the 10-day programme, 28 trainees had completed the training and all were certified as competent. The remaining trainee was unable to finish the course due to illness. Three hundred and ninety-five clients participated across the six sites, all of whom had a viable intrauterine pregnancy. No woman required referral for any suspected complication or anomaly, however 1 client was referred for high risk care following the identification of multiple pregnancy (twins). Two clients were found to be <14 weeks gestation and therefore ineligible to participate. Two hundred and twelve clients were unable to recall their LMP (54%) and 153 (39%) presented prior to 24 weeks gestation.
Twenty-two of the 28 trainees completed matched pre and post course knowledge tests. All improved on their original score, with the mean (SD) score rising from 10.2 (3.3) to 18 (2.5) following training (p <0.0001). The mean difference was 7.9, 95% CI 6.5–9.2.
Cronbach's alpha confirmed “good” reliability within groups 1–3, as depicted in Table 3, therefore the responses to these questions were analyzed as a group. The questions allocated into group 4 however, were found to demonstrate “poor” reliability and therefore were analyzed as single statements. Twenty-three of the 28 trainees completed matched pre and post course questionnaires, the results of which are summarized in Table 3. Prior to training, most disagreed with the suggestion that ultrasound posed risks for the mother and baby, however the overall strength of this conviction increased following the programme (p = 0.027). Trainees' confidence in performing ultrasound examinations also increased after training (p <0.0001), as did their perceived ability to incorporate ultrasound into their routine work (p = 0.016). Their belief regarding the importance of ultrasound in antenatal care and their interest in performing scans also increased, however these results did not reach significance.
Of the 405 OSCE assessments that were undertaken, 351 (86.7%) were considered a pass. Every assessment scored the required 11 or more, with 277 (56%) achieving the top mark of 17. Of the 54 assessments marked as a fail, eight were due to an inability to complete one of the “essential” tasks, 41 due to insufficient accuracy in the determination of gestational age and five on account of both. Aside from the accurate determination of gestational age, the most common problem encountered within the OSCE was the inability to correctly determine fetal presentation. Trainees were able to determine gestational age to within ±7 days in 359 (89%) of cases, with Bland Altman analysis approximating the overall level of agreement as ±9.6 days as shown in Figure 2.
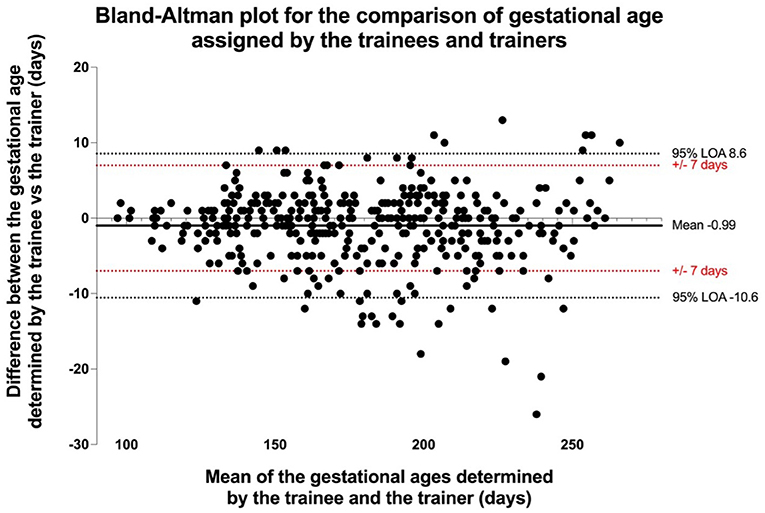
Figure 2. Bland Altman plot of comparison between the gestational ages assigned by the trainees vs the trainers.
Due to illness and competing clinical duties, repeat assessments after 3 months were only obtained for nine trainees. Within this group, the mean score of 19 obtained at the end of the training was maintained (p = 0.772). Trainees maintained their beliefs regarding the importance of ultrasound within antenatal care and continued to report high levels of confidence in performing independent ultrasound examinations (p = 0.916 and p = 0.670, respectively).
Twenty-seven repeat OSCE examinations were undertaken by nine trainees. Twenty-three of the assessments met the criteria to pass with all nine trainees demonstrating retention of their practical skills. The mean (SD) OSCE score was 16.8 (0.5), with all five “essential” tasks completed successfully for every assessment. Trainees were able to determine the gestational age to within ±7 days of the trainers on 24 (86%) occasions.
A total of 130 images were submitted for review in the 3 months following the training. Of these, one reviewer marked 17 (13%) as unacceptable and the other 13 (10%). In 9 (6%) cases this was because the reviewers did not consider the image to be that of a femur. One reviewer awarded 67 (52%) of the images the top score, the other 57 (44%). The most common source of error was that the femur did not fill >50% of the image. Levels of agreement between the reviewers were high, as demonstrated by an ICC of 0.962 (p <0.0001).
The total cost of delivering this programme across six sites was £55,182, including the provision of six Mindray DP-10 ultrasound machines.
We have demonstrated that it is possible to train ultrasound-naive practitioners to perform basic obstetric ultrasound scans, confidently and competently, after just 10 days of training, with skills retained after 3 months of independent practice. Despite having no prior experience in using ultrasound, all trainees displayed significant increases in their knowledge, confidence, and practical skills. These were sustained in the group available for follow up, however as this was only a third of participants this result should be interpreted with caution. Furthermore, in contrast to many other programs that have been developed in collaboration with groups from high income countries (25–31), our training was delivered exclusively by local faculty who were orientated to the programme virtually. This not only improved the immediate success of the programme, as the local team were much better placed to navigate the intricacies of the setting and troubleshoot any unexpected issues, but also makes this a more sustainable model.
This package was differentiated from previous programs described in the literature by applying a simplified approach to a similar baseline pedagogical framework (21, 23–25, 28, 31). Firstly, we chose to date pregnancies using FL as a single parameter. Compared with the conventional, more complex circumferential measurements of abdominal circumference (AC) and head circumference (HC), measurement of the FL requires only an image of a straight bone, making it a much easier measurement to obtain (6, 32). The reported difference in the gestational age assigned by FL alone is only ±2.4 days at <24 + 0 weeks, ±1.7 days at 24–29 + 6 days and ±1.8 days at >30 + 0 weeks (33). We believe that utilizing this approach has the potential to maximize the sustainability and implementation of this US training program without compromising clinical care. Secondly, in contrast to other programs (21, 30, 34–37), we purposefully excluded items such as the identification of fetal anomaly or measurement of cervical length and covered only the fundamentals of basic obstetric ultrasound. This was agreed with local stakeholders as an appropriate approach, which minimized training time and thus time away from work, while maximizing the possibility for accurate gestational age assessment in the community in line with WHO guidance.
Our program was further strengthened by the robust approach to assessment. There is a lack of consensus on the assessment of competency in obstetric ultrasound and a number of previous programs have omitted practical assessment completely (27, 31, 35, 38–40). The OSCE approach to “hands-on” assessment is well-established (24, 26, 28, 30, 41), as is the concept of comparing trainee measurements with those obtained by the faculty (20, 22, 23, 33, 42). By combining these, we sought to ensure that all aspects of our curriculum were assessed, with trainees demonstrating their ability to explain and document their findings as well as obtain accurate results. The need to achieve this on five consecutive occasions is more demanding than any previous program, but we felt that it was important to ensure trainees were able to perform consistently prior to independent practice.
Local faculty, training midwives in their own health facilities was also an important strength, not only because it supported unbroken scanning experience, but also because the faculty were familiar and trusted colleagues, from whom the midwives were comfortable seeking help. This helped to foster a supportive learning environment, exemplified by the midwives continuing to seek clarification regarding their scans when unsure, predominantly via a designated WhatsApp group (43). The local training team were also able to visit the sites intermittently to provide in person support.
Despite delivering successful training, there were some unanticipated challenges, namely power outages, transport strikes and a pandemic. Problems arising as a result of strike action were easily mitigated by adopting a pragmatic approach and moving “hands on” sessions to alternative days, although this did result in some of the post-course responses being overlooked, thus limiting our matched pairs. Although a little disruptive, this ensured adequate numbers of pregnant volunteers were available to undergo ultrasound scans. Delayed timelines as a result of COVID-19 impacted our ability to obtain follow up data for all participants and restrictions not only prevented the UK faculty from traveling to participate, but also necessitated a virtual orientation of the local team members who had not been present for the pilot training. Initially perceived as a set-back, this subsequently emerged as an important strength. Not only was virtual orientation both straightforward and effective, but the training enhanced by the exclusively local faculty, able to build on their pre-existing rapport with the midwives. Crucially, this also demonstrates that the programme can be delivered successfully by local teams out with those who developed it, a strong predictor of success in other settings.
Collating the trainees' images for remote review was also found to be an unexpected challenge. Having initially developed a bespoke mobile application to facilitate this, we found that users with non-android devices were unable to download it and were therefore unable to submit or review images. As a result, trainees were required to print a subset of their anonymized images, which were then collected in person with feedback provided a few days later. Although ultimately effective, this approach resulted in delays to feedback and entailed the ongoing provision of various consumables. Had it been possible under our ethics approval, a pragmatic approach to overcome this issue might have been to facilitate follow up via WhatsApp. Cheap and readily available, the use of WhatsApp in healthcare projects is well-established (44, 45). and this approach would be well-aligned with the concept of embedding initiatives into pre-existing systems.
Following the success of this training program, it is being evaluated as part of a mixed methods quasi-experimental trial with the primary outcome of proportion of women with accurate gestational age assessment at six health centers in Malawi. The results of this program and progress of the trial have been endorsed by the Reproductive Health Directorate of the Ministry of Health of Malawi, the Association of Malawian Midwives and the Society of Obstetricians and Gynecologists of Malawi. In addition, we have identified one trainee per site (n = 6) with an aptitude for scanning who will be mentored to become the next generation of trainers. Finally, in collaboration with regulatory bodies in Malawi, we are discussing a how to incorporate basic obstetric ultrasound into the nursing and midwifery curriculum in Malawi, demonstrating the ongoing local commitment to upscale this service. Although ours was an experienced group, with an average of 10.5 years clinical experience, we believe that by integrating this programme into midwifery training ultrasound skills could be made accessible to midwives at all professional levels.
The TUDA training program is an effective method of training midwives in basic obstetric ultrasound in a 2 week period, thus overcoming a major barrier cited by previous initiatives (12, 14, 15, 19, 46). This program has the potential to contribute to efforts to achieve coverage of current WHO recommended guidance for basic obstetric ultrasound in LMICS. By empowering developing local faculty to provide supportive supervision in the trainees primary place of work, local acceptability was increased and basic implementation hurdles overcome during the training phase facilitating progression to independence and retention of skills.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by University of Edinburgh and the University of Malawi—College of Medicine Research and Ethics Committee (COMREC) P08/19/2768. The patients/participants provided their written informed consent to participate in this study.
Catherine Bamuya, Esmie Banda, James Boardman, Effie Chipeta, Mia Crampin, Sarah Cunningham Burley, Jean Desire Kabamba, Elizabeth Grant, Caroline Hollins Martin, Aisha Holloway, Khondwhani Kawaza, Corrine Love, Monica Malata, Fadhila Mazanderani, Catherine Mkandawire, Patrica Munthali, Peter Mwaba, Shakira Namisengo, Everist Njelesani, Linda Nyondo-Mipando, Hilary Pinnock, Muriel Syacumpi, Frank Taulo.
AV prepared the protocol for this study, with input and guidance from all authors. The education package was developed by AV, GM-G, DK, MM, BM, and LG, with GM-G, MM, EM, and LG co-ordinating the delivery of the training in Malawi. Data was analyzed by AV, who also prepared the first draft of the manuscript, under the guidance of SW, SJS, JN, DL, BM, BF, and LG. All authors provided critical insight for the manuscript.
This research was funded by the National Institute for Health Research (NIHR) (GHR Project: 17/63/08 DIPLOMATIC collaboration) using UK aid from the UK Government to support global health research. We acknowledge the support of the Medical Research Council Centre for Reproductive Health (MRC CRH) Grant MR/N022556/1 and the support of the British Heart Foundation (RE/18/5/34216). SJS was supported by Wellcome Trust Clinical Career Development Fellowship 209560/Z/17/Z.
The views expressed in this publication are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
On behalf of the DIPLOMATIC collaborators we would like to thank Patricia Munthali Khomani, Chifundo Kondoni, Shakira Namisengo and Lorraine Adamson for their administrative assistance in supporting this programme and Thokozani Ganiza for her help with data collection. We would also like to thank the Ministry of Health in Malawi who supported this work and the practitioners who gave up their time to participate. We are also extremely grateful to all the participants who volunteered during our pilot training courses.
AC, Abdominal circumference; EDD, Estimated date of delivery; FL, Femur length; HC, Head circumference; ICC, Intraclass correlation coefficients; LMICs, Low- and middle- income countries; LMP, Last menstrual period; OSCE, Observed Structured Clinical Examinations; WHO, World Health Organization.
1. Vogel JP, Oladapo OT, Manu A, Gülmezoglu AM, Bahl R. New WHO recommendations to improve the outcomes of preterm birth. Lancet Glob Heal. (2015) 3:e589–90. doi: 10.1016/S2214-109X(15)00183-7
2. Lee ACC, Blencowe H, Lawn JE. Small babies, big numbers: global estimates of preterm birth. Lancet. (2019) 7:e2–3. doi: 10.1016/S2214-109X(18)30484-4
4. Pettker CM, Goldberg JD, El-Sayed YY. Methods for Estimating the Due Date. Washington, DC: American College of Obstetricians and Gynecologists. Committee Opinion (2017).
5. Loughna P, Chitty L, Evans T, Chudleigh T. Fetal size and dating: charts recommended for clinical obstetric practice. Ultrasound. (2009) 17:161–7. doi: 10.1179/174313409X448543
6. Butt K, Lim K. Determination of gestational age by ultrasound. J Obstet Gynaecol Canada. (2014) 36:171–81. doi: 10.1016/S1701-2163(15)30664-2
9. Treloar A, Boynton R., Behn B., Brown B. Variation of the human menstrual cycle through reproductive life. Int J Fertil. (1967) 12:77–126.
10. Baskett TF, Nagele F. Naegele's rule: a reappraisal. BJOG. (2000) 107:1433–5. doi: 10.1111/j.1471-0528.2000.tb11661.x
11. Lee ACC, Whelan R, Bably NN, Schaeffer LE, Rahman S, Ahmed S, et al. Prediction of gestational age with symphysis-fundal height and estimated uterine volume in a pregnancy cohort in Sylhet, Bangladesh. BMJ Open. (2020) 10:1–10. doi: 10.1136/bmjopen-2019-034942
12. Wanyonyi S, Mariara C., Vinayak S, Stones W. Opportunities and challenges in realizing universal access to obstetric ultrasound in Sub-Saharan Africa. Ultrasound Int Open. (2017) 3:E52–9. doi: 10.1055/s-0043-103948
13. Seffah JD, Adanu RMK. Obstetric ultrasonography in low-income countries. Clin Obstet Gynecol. (2009) 52:250–5. doi: 10.1097/GRF.0b013e3181a4c2d5
14. Shah S, Bellows BA, Adedipe AA, Totten JE, Backlund BH, Sajed D. Perceived barriers in the use of ultrasound in developing countries. Crit Ultrasound J. (2015) 7:3–7. doi: 10.1186/s13089-015-0028-2
15. Kim ET, Singh K, Moran A, Armbruster D, Kozuki N. Obstetric ultrasound use in low and middle income countries: a narrative review. Reprod Health. (2018) 15:1–26. doi: 10.1186/s12978-018-0571-y
16. Maraci MA, Yaqub M, Craik R, Beriwal S, Self A, von Dadelszen P, et al. Toward point-of-care ultrasound estimation of fetal gestational age from the trans-cerebellar diameter using CNN-based ultrasound image analysis. J Med Imaging. (2020) 7:1. doi: 10.1117/1.JMI.7.1.014501
17. Puchalski Ritchie LM, Khan S, Moore JE et al. Low- and middle-income countries face many common barriers to implementation of maternal health evidence products. J Clin Epidemiol. (2016) 76:229–37. doi: 10.1016/j.jclinepi.2016.02.017
18. Smith GC, Nakimuli A. Ultrasound estimation of gestational age in late pregnancy in low-income countries: made to measure or off-the-peg? Lancet Global Health. (2020) 8:e462–3. doi: 10.1016/S2214-109X(20)30081-4
19. Maw AM, Galvin B, Henri R, Yao M, Exame B, Fleshner M, et al. Stakeholder perceptions of point-of-care ultrasound implementation in resource-limited settings. Diagnostics. (2019) 9:1–11. doi: 10.3390/diagnostics9040153
20. Millar K, Patel S, Munson M, Vesel L, Subbiah S, Jones RM, et al. INTERGROWTH-21st gestational dating and fetal and newborn growth standards in peri-urban Nairobi, Kenya: quasi-experimental implementation study protocol. JMIR Res Protoc. (2018) 7:10. doi: 10.2196/10293
21. Nathan R, Swanson JO, Marks W, Goldsmith N, Vance C, Sserwanga NB, et al. Screening obstetric ultrasound training for a five-country cluster randomized controlled trial. Ultrasound Q. (2014) 30:262–6. doi: 10.1097/RUQ.0000000000000096
22. Neufeld LM, Wagatsuma Y, Hussain R, Begum M, Frongillo EA. Measurement error for ultrasound fetal biometry performed by paramedics in rural Bangladesh. Ultrasound Obstet Gynecol. (2009) 34:387–94. doi: 10.1002/uog.6385
23. Sarris I, Ioannou C, Ohuma EO, Altman DG, Hoch L, Cosgrove C, et al. Standardisation and quality control of ultrasound measurements taken in the INTERGROWTH-21st Project. BJOG. (2013) 120(Suppl. 2):33–7. doi: 10.1111/1471-0528.12315
24. Shah S, Santos N, Kisa R, Mike Maxwell O, Mulowooza J, Walker D, et al. Efficacy of an ultrasound training program for nurse midwives to assess high-risk conditions at labor triage in rural Uganda. PLoS ONE. (2020) 15:e0235269. doi: 10.1371/journal.pone.0235269
25. Wylie BJ, Kalilani-Phiri L, Madanitsa M, Membe G, Nyirenda O, Mawindo P, et al. Gestational age assessment in malaria pregnancy cohorts: a prospective ultrasound demonstration project in Malawi. Malar J. (2013) 12:183. doi: 10.1186/1475-2875-12-183
26. Wanjiku GW, Bell G, Wachira B. Assessing a novel point-of-care ultrasound training program for rural healthcare providers in Kenya. BMC Health Serv Res. (2018) 18:1–7. doi: 10.1186/s12913-018-3196-5
27. Shah S, Epino H, Bukhman G, Noble VE et al. Impact of the introduction of ultrasound services in a limited resource setting: Rural Rwanda. BMC Int Health Hum Rights. (2009) 9:1–6. doi: 10.1186/1472-698X-9-4
28. Kimberly HH, Murray A, Mennicke M, Liteplo A, Lew J, Bohan JS, et al. Focused maternal ultrasound by midwives in rural Zambia. Ultrasound Med Biol. (2010) 36:1267–72. doi: 10.1016/j.ultrasmedbio.2010.05.017
29. Greenwold N, Wallace S, Prost A, Jauniaux E. Implementing an obstetric ultrasound training program in rural Africa. Int J Gynecol Obstet. (2014) 124:274–7. doi: 10.1016/j.ijgo.2013.09.018
30. Bentley S, Hexom B, Nelson BP. Evaluation of an obstetric ultrasound curriculum for midwives in Liberia. J Ultrasound Med. (2015) 34:1563–8. doi: 10.7863/ultra.15.14.08017
31. Boamah EA, Asante KP, Wylie BJ. Gestational age assessment in the Ghana randomized air pollution and health study (GRAPHS): ultrasound capacity building, fetal biometry protocol development, and ongoing quality control background: the ghana randomized air pollution and health study (GRAPHS). JMIR Res Protoc. (2014) 3:e77–100. doi: 10.2196/resprot.3797
32. Salomon LJ, Alfirevic Z, Da Silva Costa F, Deter RL, Figueras F, Ghi T, et al. ISUOG practice guidelines: ultrasound assessment of fetal biometry and growth. Ultrasound Obstet Gynecol. (2019) 53:715–23. doi: 10.1002/uog.20272
33. The WHO Alliance for Maternal Newborn Health Improvement Late Pregnancy Dating Study Group. Performance of late pregnancy biometry for gestational age dating in low-income middle-income countries : a prospective, multicountry, population-based cohort study from the WHO Alliance for Maternal Newborn Health Improvement (AMANHI) Study Group. Lancet Glob Heal. (2020) 8:545–54. doi: 10.1016/S2214-109X(20)30034-6
34. Baj N, Dubbins P, Evans JA. Obstetric ultrasound education for the developing world: a learning partnership with the World Federation for Ultrasound in Medicine and Biology. Ultrasound. (2015) 23:53–8. doi: 10.1177/1742271X14566848
35. Enabudoso E, Adams OH. Organizing an international-standard obstetric ultrasonography training program in a low-resource setting. Int J Gynecol Obstet. (2017) 136:102–4. doi: 10.1002/ijgo.12016
36. Kim J, Shakya PR, Choi S, Park JS, Tamrakar SR, Heo J, et al. An evaluation of obstetric ultrasound education program in Nepal using the RE-AIM framework. BMC Med Educ. (2021) 21:1–13. doi: 10.1186/s12909-021-02484-3
37. Kinnevey C, Kawooya M, Tumwesigye T, Douglas D, Sams S. Addressing obstetrical challenges at 12 rural Ugandan health facilities: findings from an international ultrasound and skills development training for midwives in Uganda. Int J MCH AIDS. (2016) 5:46–52. doi: 10.21106/ijma.106
38. Adler D, Mgalula K, Price D, Taylor O. Introduction of a portable ultrasound unit into the health services of the Lugufu refugee camp, Kigoma District, Tanzania. Int J Emerg Med. (2008) 1:261–6. doi: 10.1007/s12245-008-0074-7
39. Ahmadzia H, Cigna S, Namagembe I, Macri C, Galerneau F, Magriples U. Teaching obstetric ultrasound at Mulago Hospital - Kampala, Uganda. Afr Health Sci. (2018) 18:166–71. doi: 10.4314/ahs.v18i1.21
40. Toscano M, Marini TJ, Drennan K, Baran TM, Kan J, Garra B, et al. Testing telediagnostic obstetric ultrasound in Peru: a new horizon in expanding access to prenatal ultrasound. BMC Pregn Childb. (2021) 21:328. doi: 10.1186/s12884-021-03720-w
41. Vinayak S, Sande J, Nisenbaum H, Nolsøe CP. Training midwives to perform basic obstetric point-of-care ultrasound in rural areas using a tablet platform and mobile phone transmission technology—A WFUMB COE project. Ultrasound Med Biol. (2017) 43:2125–32. doi: 10.1016/j.ultrasmedbio.2017.05.024
42. Rijken MJ, Lee SJ, Boel ME, Papageorghiou AT, Visser GHA, Dwell SLM, et al. Obstetric ultrasound scanning by local health workers in a refugee camp on the Thai-Burmese border. Ultrasound Obstet Gynecol. (2009) 34:395–403. doi: 10.1002/uog.7350
43. Facebook Inc. WhatsApp. (2020). Available online at: https://whatsapp.com (accessed February 2, 2022).
44. Mars M, Escott R. WhatsApp in clinical practice: a literature review. Stud Health Technol Inform. (2016) 231:82–90. doi: 10.3233/978-1-61499-712-2-82
45. Eke OF, Henwood PC, Wanjiku GW, Fasina A, Kharasch SJ, Shokoohi H. Global point-of-care ultrasound education and training in the age of COVID-19. Int J Emerg Med. (2021) 14:12–5. doi: 10.1186/s12245-021-00338-9
Keywords: gestational age, ultrasound, training, Malawi, midwives
Citation: Viner AC, Membe-Gadama G, Whyte S, Kayambo D, Masamba M, Makwakwa E, Lissauer D, Stock SJ, Norman JE, Reynolds RM, Magowan B, Freyne B and Gadama L (2022) Training in Ultrasound to Determine Gestational Age (TUDA): Evaluation of a Novel Education Package to Teach Ultrasound-Naive Midwives Basic Obstetric Ultrasound in Malawi. Front. Glob. Womens Health 3:880615. doi: 10.3389/fgwh.2022.880615
Received: 21 February 2022; Accepted: 11 March 2022;
Published: 05 April 2022.
Edited by:
Jane Elizabeth Hirst, University of Oxford, United KingdomReviewed by:
Orvalho Augusto, University of Washington, United StatesCopyright © 2022 Viner, Membe-Gadama, Whyte, Kayambo, Masamba, Makwakwa, Lissauer, Stock, Norman, Reynolds, Magowan, Freyne and Gadama. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alexandra C. Viner, YWxleHZpbmVyQGRvY3RvcnMub3JnLnVr
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.