- 1Department of Anorectal Surgery, Baoshan District Integrated Traditional Chinese and Western Medicine Hospital, Shanghai, China
- 2Department of Traditional Chinese Medicine, Juquan Xincheng Community Health Service Center, Shanghai, China
- 3Department of Anorectal Surgery, Shuguang Hospital Affiliated to Shanghai University of Traditional Chinese Medicine, Shanghai, China
Background: Significant evidence has been documented regarding the intricate connection between the development of anal fistula (AF) and the composition of Body Mass Index (BMI). Nevertheless, due to the inherent limitations of reverse causality and confounders inherent in observational studies, this relationship remains unclarified. Our study aims to reveal the causal impact between BMI and AF, as well as identify its associated risk factors, thereby providing a more comprehensive understanding of this complex interaction.
Methods: Single nucleotide polymorphisms (SNPs) identified through genome-wide association study (GWAS) databases were used as instrumental variables for analysis. BMI served as the exposure variable, with six pooled GWAS datasets included. AF was the outcome variable. The Inverse Variance Weighted (IVW) method was used as the primary analytical technique, with MR-Egger regression, Weighted Median (WME) estimation, and Multiplicity Residual Sum and Outlier (MR-PRESSO) tests serving as secondary validations of the IVW results. Odds ratios (OR) were utilized as indicators to evaluate the causal relationship between BMI and AF.
Results: A total of 738 SNPs strongly associated with the exposure were identified as instrumental variables. The IVW results demonstrated a positive correlation between BMI and the risk of AF. The MR-Egger analysis yielded p-values greater than 0.05, indicating no pleiotropic effects among the selected SNPs. Cochran’s Q test also resulted in p-values greater than 0.05, suggesting no significant heterogeneity among the instrumental variables. The MR-PRESSO analysis revealed no horizontal pleiotropy or outliers potentially violating the causal assumption (p > 0.05).
Conclusion: High BMI is positively associated with the risk of AF, and correcting BMI levels may have a preventive effect on the incidence of AF.
Introduction
Anal fistula (AF) is primarily characterized by persistent or intermittent purulent, bloody, or mucinous secretions at the external orifice of the fistula, along with local symptoms of redness, swelling, heat, and pain. The severity of symptoms can vary significantly, often necessitating surgical intervention (Limura and Giordano, 2015; Hwang, 2022). Obesity, a slow-paced metabolic disease caused by multiple factors, refers to a pathological state of excessive accumulation of body fat, particularly triglycerides, resulting in a certain degree of overweight and excessive fat layer thickness (Pigeyre et al., 2016). A diagnosis of obesity is typically made when the body mass index (BMI) is ≥ 30 kg/m2. Epidemiological studies have shown that the prevalence of AF is 12.3 cases per 100,000 men and 5.6 cases per 100,000 women (Sainio, 1984). Over the past 40 years, the prevalence of obesity has increased from 3.2% to 10.8% among young and middle-aged men, and from 6.4% to 14.9% among women, while AF commonly occurs in individuals aged 20–40 years (NCD Risk Factor Collaboration NCD-RisC, 2016). Previous studies have found that obesity can promote inflammatory responses, metabolic dysfunction, and cancer risks (Iyengar et al., 2016; Kawai et al., 2021). Additionally, obesity will lead abnormalities in cell-mediated immune and phagocytic functions, resulting in anal fistula (Liu et al., 2011). Another meta-analysis found that an elevated BMI in patients with AF may be a potential factor for the high recurrence rate after AF surgery (Mei et al., 2019).
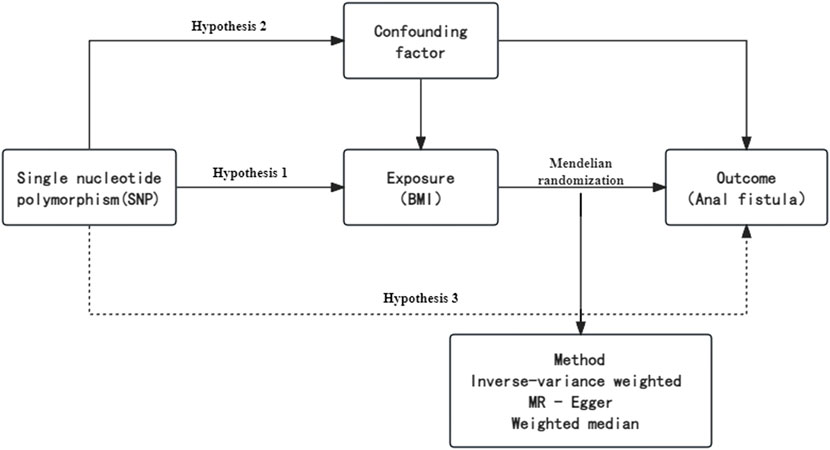
Currently, multiple studies suggest a positive correlation between BMI and the risk of AF occurrence. However, previous observational studies have been subject to biases such as confounding factors and reverse causality. Mendelian randomization (MR) is an epidemiological research method that can infer potential causal relationships and has been widely used in recent years for causality research in genome-wide association study (GWAS) data (Smith and Ebrahim, 2003; Evans and Davey Smith, 2015). This method uses single nucleotide polymorphisms (SNPs) as instrumental variables to infer the causal relationship between exposure factors and outcomes (Wang, 2020). Since the alleles of specific SNPs are randomly assigned at conception, and genetic variations precede the development of diseases, genetic variations are not influenced by potential confounding factors, thus avoiding the possibility of reverse causality. The aim of this study is to explore the causal impact of obesity on the risk of AF occurrence using a two-sample Mendelian randomization analysis approach.
Materials and methods
Analysis methods and data sources
In this study, BMI was treated as the exposure factor, and SNPs significantly associated with BMI were used as Instrumental Variables (IVs), with AF as the outcome variable. After eliminating outliers, the causal analysis was performed by using two sample MR analysis method, followed by heterogeneity test and pleiotropy test, and finally the reliability of the results was tested. IVs in MR study should meet three core assumptions (Greenland, 2000; Lawlor et al., 2008; Burgess et al., 2013): (1) The IVs are strongly correlated with the exposure factor; (2) The IVs affect the outcome only through the exposure factor and are not directly or indirectly related to the outcome through other pathways; (3) The IVs are unrelated to confounding factors in the “exposure-outcome” relationship. All data on the association between exposure factor variables BMI and outcome variable AF were sourced from the IEU Open GWAS project database. SNPs significantly associated with BMI were screened as IVs based on GWAS, and different MR methods were used to analyze the causal relationship between BMI and AF. The data population consisted of Europeans and did not include gender stratification. By reading the original literature, no sample overlap problems between the two groups of data were found. Ethical review and informed consent had been obtained in all original studies.
Selection of IVs
To avoid bias in the analysis that may be introduced by strong linkage disequilibrium (LD) relationships among SNPs, this study selected SNPs that were independent of each other and had a genome-wide association with AF from the database, with selection criteria including (Noyce et al., 2017): (1) Selecting IVs highly correlated with the exposure factor (BMI) as SNP sites (p < 5 × 10^-8); (2) Physical distance between genes >10,000 kb, and maintaining an r^2 value of <0.001 for LD between retained SNPs; (3) Removing SNPs with a minor allele frequency (MAF) ≤0.01; (4) Ensuring that the effect of SNPs on the exposure corresponds to the same allele as their effect on the outcome. A combined dataset of exposure and outcome was merged, containing the above IVs and their relationship with both the outcome and exposure factors, and palindromic SNPs were deleted. The remaining SNPs were the final IVs representing the exposure. The Weighted Median Estimate (WME) is a weighted empirical distribution function of ratio estimate values for all SNPs within the research range, which can reduce bias in the estimation of causal effects. A flowchart briefly presents the whole procedure in Figure 1.
Two-sample MR analysis
This study used 3 MR methods to analyze the causal estimate of BMI on AF, mainly using Inverse Variance Weighted (IVW) analysis (Liu et al., 2011; Burgess et al., 2013), supplemented by WME (Bowden et al., 2015), and MR-Egger regression (Bowden et al., 2016). The IVW method was used as the main analysis method to assess the causal effect of BMI on AF. The IVW method combines the Wald ratio estimates of each IV in a meta-analysis into a weighted linear regression model for the association between the instrument and the result. When there is no pleiotropy of IVs, the IVW method has higher test efficiency and precision and can obtain the smallest effect estimate with minimal bias. Further, the intercept term of the MR-Egger regression was used to test whether there is genetic pleiotropy in the BMI-related IVs with AF, with P > 0.05 indicating that there is no pleiotropy between the instrumental and the outcome variables, and rejecting the null hypothesis indicates the presence of pleiotropy (Burgess and Thompson, 2017). The Cochran’s Q test was used to test the heterogeneity of the IVs, with P < 0.05 indicating heterogeneity (Burgess et al., 2016). The MR Pleiotropy Residual Sum and Outlier (MR-PRESSO) test was used to exclude outliers (Verbanck et al., 2018). A leave-one-out sensitivity analysis method was used to perform sensitivity analysis, examining the impact of each SNP on the results (Skrivankova et al., 2021). Stability of the results was checked by observing asymmetry in the funnel plot. This study conducted statistical analysis using the TwoSampleMR and MR-PRESSO software packages in R (version 4.3.1), with a significance level of α = 0.05.
Results
Selection of IVs
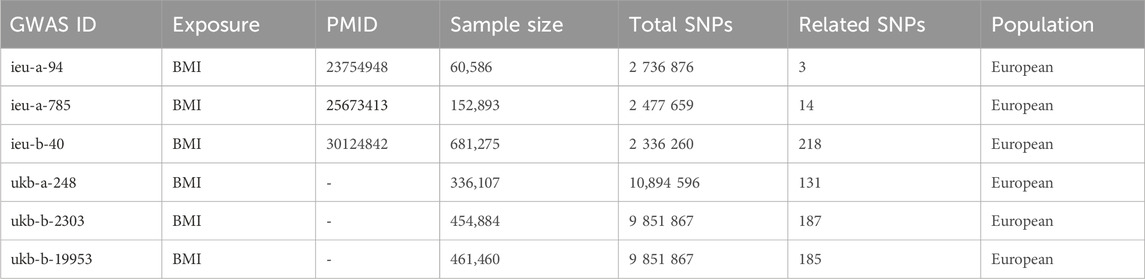
According to the instrumental variable screening standards, six highly relevant BMI exposure datasets with AF were selected from GWAS, and after excluding linkage disequilibrium, 738 SNPs from the GWAS database were used as IVs for two-sample Mendelian randomization analysis. Among them, six groups of BMI IVs contained 2,147,205 participants. The genetic correlation data of AF came from a GWAS of 463,010 participants in the United Kingdom Biobank, including 1,003 cases of AF. The population sources of both groups of data were European and included both males and females. Specific information about GWAS can be found in Table 1.
Causal effect analysis results of BMI and AF
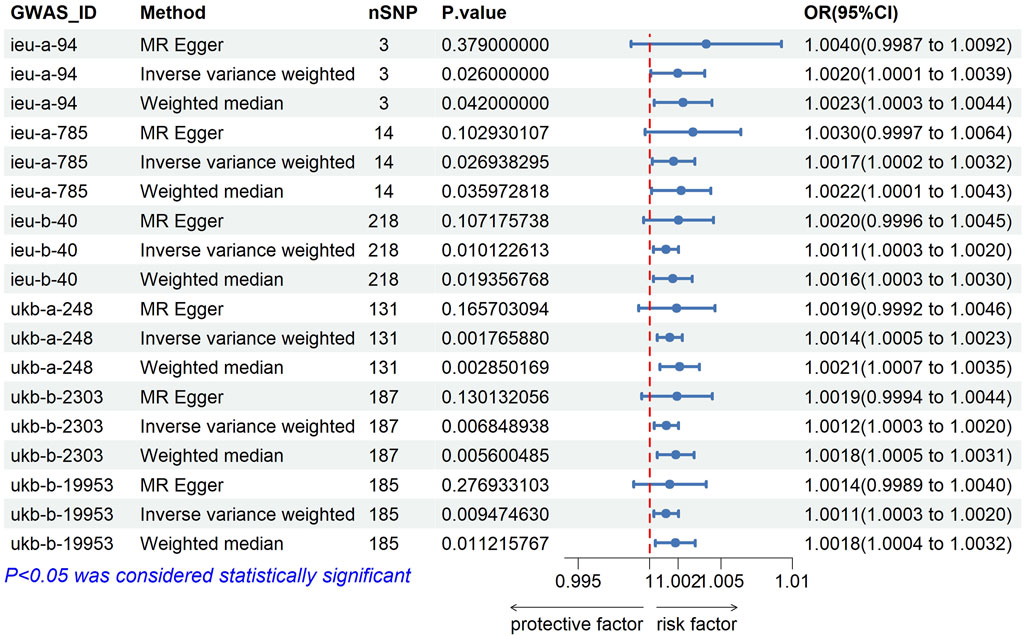
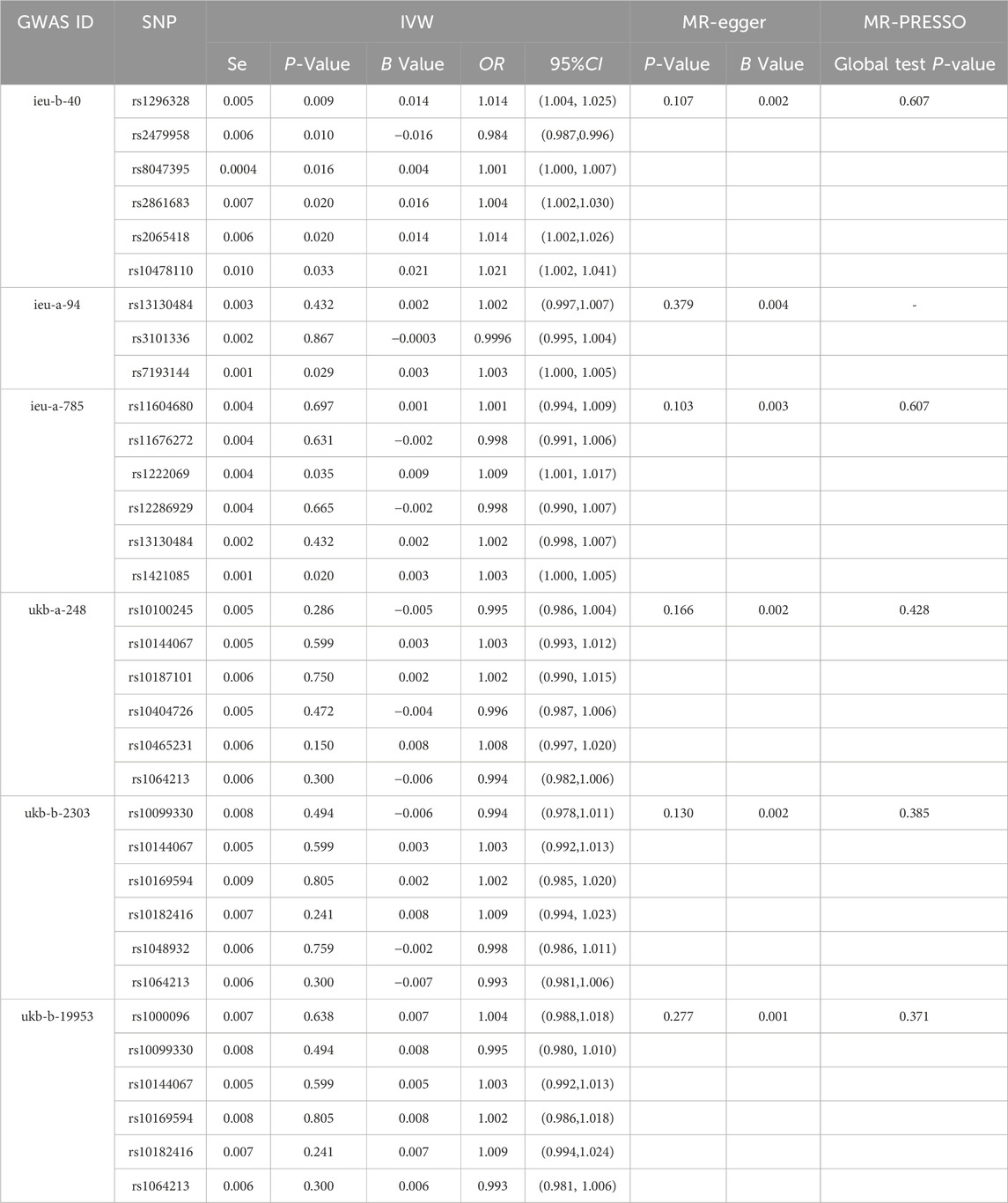
After analysis, the F values of all six groups of BMI-related IVs were greater than 10, suggesting that the influencing factors of BMI were related to the risk of developing AF. The IVW method showed that the increase in genetic predicted BMI IVs ieug-a-94 (OR = 1.002, 95%CI 1.000–1.004, p = 0.026), ieug-a-785 (OR = 1.0017, 95%CI 1.001–1.004, p = 0.027), ieub-40 (OR = 1.001, 95%CI 1.000–1.003, p = 0.010), ukb-a-248 (OR = 1.001, 95%CI 1.001–1.002, p = 0.002), ukb-b-2303 (OR = 1.001, 95%CI 1.000–1.002, p = 0.007), and ukb-b-19953 (OR = 1.001, 95%CI 1.000–1.002, p = 0.009) was associated with an increased risk of AF, see Figures 1, 2. Table 2 lists the IVW results of some SNPs, OR values, and 95%CI. The β values of MR-egger regression and WME showed the same direction as the β values of the IVW method, indicating that the direction of causal effects obtained by the three methods was consistent (Table 2; Figures 2, 3).
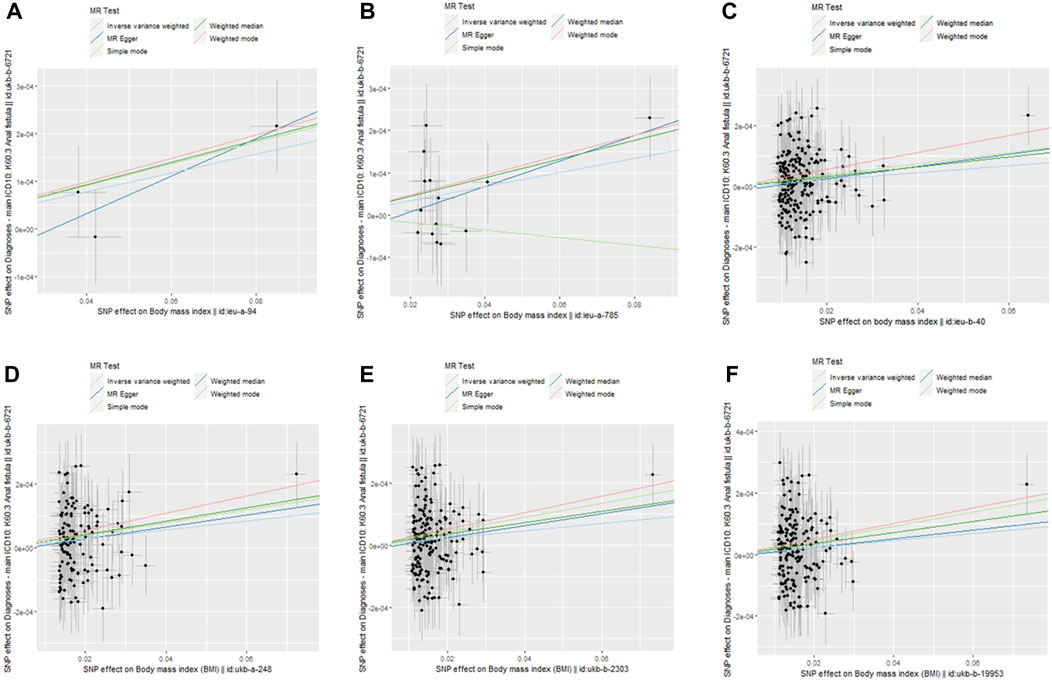
Figure 3. Scatter plots of the 5 MR tests in six causal associations from BMI features to anal fistula. SNP effects were plotted into lines for the inverse-variance weighted test (light blue line), weighted median estimator (green line), MR-Egger regression (blue line), weight median estimator (red line) and simple mode estimator (light green line). The slope of the line corresponded to the causal estimation.
In the sensitivity analysis, the MR-egger result indicated that there was no horizontal pleiotropy among the six instrumental variables (p > 0.05). The results of Cochran’s Q test were all p > 0.05, indicating that there was no significant heterogeneity among the instrumental variables. The MR-PRESSO result showed no horizontal pleiotropy and possible violations of causal effects in the IVs (p > 0.05, Table 2). Using the leave-one-out method, the results obtained after removing each SNP one by one were all p < 0.05, consistent with the results of the causal effect analysis using the IVW method, indicating that there were no non-specific SNPs affecting the causal estimation results.
Discussion
This study employed the MR methodology to analyze the potential causal association between BMI and AF using genome-wide association study (GWAS) data. The results showed that all six groups of IVs associated with BMI consistently indicated a significant role of obesity in the pathogenesis of AF.
Previous observational studies have explored the correlation between BMI and the incidence of AF. Bayrak et al. (Bayrak and Altintas, 2022) found a positive association between obesity and recurrence after AF surgery. Lu et al. (Lu et al., 2019) conducted a retrospective study of 790 patients with AF and observed a positive correlation between high BMI and both the high incidence and recurrence rate of AF. Similarly, Schwandner et al. (Schwandner, 2011) observed in a prospective cohort study that the recurrence rate of AF was significantly lower in non-obese patients compared to obese patients. Additionally, the reoperation rate for recurrent abscesses requiring drainage was significantly higher in obese patients. These findings are consistent with the results of our study (OR = 1.002, 95% CI 1.000–1.004). The main symptom of AF is periodic purulent discharge and pain, which can be cured by surgical removal of the infected focus and epithelialized fistula. Obesity or overweight is a major risk factor for the development of comorbid conditions such as cardiovascular disease, type 2 diabetes mellitus, malignancy, asthma, osteoarthritis, chronic back pain, obstructive sleep apnea, non-alcoholic fatty liver disease, and gallbladder diseases (Mulita et al., 2021). Additionally, adipose tissue has high metabolic activity and can secrete pro-inflammatory cytokines such as interleukin (IL)-6 and tumor necrosis factor (TNF)-α, which may promote inflammatory responses and tumorigenesis (Wei et al., 2015; Ying et al., 2020). Physical exercise not only effectively reduces body fat but also improves cardiopulmonary function. Unick et al. (Unick et al., 2017) found that 150–250 min of physical activity per week is sufficient to maintain weight loss. Adults and older adults should engage in at least 150 min per week of moderate-to-vigorous physical activity to prevent significant weight gain and reduce the risk of chronic diseases, while also incorporating muscle-strengthening activities on at least 2 days per week (World Health Organization, 2020).
Despite numerous clinical studies indicating a correlation between BMI and AF, these findings may only reflect the clinical signs of AF patients and do not necessarily establish a causal link between BMI and AF. As previously mentioned, RCTs may be influenced by confounding factors and reverse causality. In contrast to previous observational studies, this study is the first to systematically explore the potential causal association between obesity and AF pathogenesis from a genetic perspective, effectively avoiding the confounding biases and reverse causality issues inherent in traditional observational studies. On one hand, Mendelian randomization studies, leveraging genetic approaches, employed various statistical methods such as IVW, WME, MR-Egger regression analysis, and MR-PRESSO to validate the stability of the causal relationship between exposure factors and outcomes. On the other hand, the data used in this study originated from a European population, ensuring that all study participants were of European ancestry, which minimized biases resulting from differences in environment, ethnicity, and dietary structure. Most importantly, the genetic variants associated with BMI in the six groups were derived from large-scale GWAS meta-analyses, ensuring the strength of IVs in the MR analysis and the accuracy of the study results.
However, this study also has some limitations. Firstly, the inclusion of only European individuals reduces population stratification bias but may limit the reliability of the evidence for the association between BMI and AF in other ethnic groups. Therefore, further studies are needed to investigate the relationship between BMI and AF in other ethnic populations. Secondly, AF exhibits multiple clinical subtypes, necessitating subsequent subgroup studies, including exploring the relationship between normal weight, overweight and obese people on the formation and postoperative healing of AF, complex AF and high AF. Thirdly, this study solely explored the causal relationship between BMI and AF without delving into the underlying mechanisms. Adjusting or maintaining normal BMI may be a potential treatment for alleviating the clinical symptoms of anal fistula and improving the postoperative recovery of anal fistula surgery. Meantime, future studies should be conducted across different ethnic groups and include stratified analyses based on gender and age to further explore the impact of BMI on the occurrence and development of AF. Additionally, BMI changes over time, and while the aim of MR analysis is to estimate the lifelong impact of exposure factors on outcomes, the genetic instruments used here are associated with BMI at specific age intervals, potentially affecting the validity of the results. Although Mendelian randomization is a commonly used experimental design, it also has its limitations. In practical applications, it is crucial to consider multiple factors comprehensively and in light of specific circumstances to ensure the reliability of experimental results. Given that AF can also result from multiple factors, including rectovaginal fistulas caused by perineal colostomy, it is crucial to be mindful of this complication. Additionally, since the GWAS database does not track the formation of AF, it is important to consider possible exposures (Mulita et al., 2022).
In summary, this study employed a two-sample MR approach to systematically investigate the potential causal association between BMI and the occurrence of AF. The results indicate a positive correlation between BMI and the risk of AF, suggesting that correcting obesity may have a preventive role in the occurrence and development of AF. However, further multicenter clinical studies with larger sample sizes and additional MR studies are needed to validate the causal relationship between obesity and AF pathogenesis.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
BC: Conceptualization, Data curation, Methodology, Software, Writing–original draft, Writing–review and editing. YL: Data curation, Methodology, Software, Writing–original draft. YW: Data curation, Formal Analysis, Validation, Writing–original draft. QW: Funding acquisition, Resources, Supervision, Writing–review and editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Shanghai Municipal Commission of Science and Technology (No. 23Y11921800) and the Shanghai Municipal Health Commission (No. ZYTSZK1-8).
Acknowledgments
We are grateful to the volunteers who participated in this study, the researchers who shared their findings, the GWAS data platform, and the major research consortia, all of which provided leads and possibilities for subsequent studies.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Bayrak, M., and Altintas, Y. (2022). Predictive factors affecting recurrence of anal fistula after LIFT procedure. J. Coll. Physicians Surg. Pak 32 (11), 1470–1473. doi:10.29271/jcpsp.2022.11.1470
Bowden, J., Davey Smith, G., and Burgess, S. (2015). Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int. J. Epidemiol. 44 (2), 512–525. doi:10.1093/ije/dyv080
Bowden, J., Davey Smith, G., Haycock, P. C., and Burgess, S. (2016). Consistent estimation in mendelian randomization with some invalid instruments using a weighted median estimator. Genet. Epidemiol. 40 (4), 304–314. doi:10.1002/gepi.21965
Burgess, S., Butterworth, A., and Thompson, S. G. (2013). Mendelian randomization analysis with multiple genetic variants using summarized data. Genet. Epidemiol. 37 (7), 658–665. doi:10.1002/gepi.21758
Burgess, S., Dudbridge, F., and Thompson, S. G. (2016). Combining information on multiple instrumental variables in Mendelian randomization: comparison of allele score and summarized data methods. Stat. Med. 35 (11), 1880–1906. doi:10.1002/sim.6835
Burgess, S., and Thompson, S. G. (2017). Interpreting findings from Mendelian randomization using the MR-Egger method. Eur. J. Epidemiol. 32 (5), 377–389. doi:10.1007/s10654-017-0255-x
Evans, D. M., and Davey Smith, G. (2015). Mendelian randomization: new applications in the coming age of hypothesis-free causality. Annu. Rev. Genomics Hum. Genet. 16, 327–350. doi:10.1146/annurev-genom-090314-050016
Greenland, S. (2000). An introduction to instrumental variables for epidemiologists. Int. J. Epidemiol. 29 (4), 722–729. doi:10.1093/ije/29.4.722
Hwang, S. H. (2022). Trends in treatment for hemorrhoids, fistula, and anal fissure: go along the current trends. J. Anus Rectum Colon 6 (3), 150–158. doi:10.23922/jarc.2022-012
Iyengar, N. M., Gucalp, A., Dannenberg, A. J., and Hudis, C. A. (2016). Obesity and cancer mechanisms: tumor microenvironment and inflammation. J. Clin. Oncol. 34 (35), 4270–4276. doi:10.1200/JCO.2016.67.4283
Kawai, T., Autieri, M. V., and Scalia, R. (2021). Adipose tissue inflammation and metabolic dysfunction in obesity. Am. J. Physiol. Cell Physiol. 1 (3), C375–C391. doi:10.1152/ajpcell.00379.2020
Lawlor, D. A., Harbord, R. M., Sterne, J. A., Timpson, N., and Davey Smith, G. (2008). Mendelian randomization: using genes as instruments for making causal inferences in epidemiology. Stat. Med. 27 (8), 1133–1163. doi:10.1002/sim.3034
Limura, E., and Giordano, P. (2015). Modern management of anal fistula. World J. Gastroenterol. 21 (1), 12–20. doi:10.3748/wjg.v21.i1.12
Liu, C. K., Liu, C. P., Leung, C. H., and Sun, F. J. (2011). Clinical and microbiological analysis of adult perianal abscess. J. Microbiol. Immunol. Infect. 44 (3), 204–208. doi:10.1016/j.jmii.2011.01.024
Lu, D., Lu, L., Cao, B., Li, Y., Cao, Y., Li, Z., et al. (2019). Relationship between body mass index and recurrence/anal fistula formation following initial operation for anorectal abscess. Med. Sci. Monit. 23 (25), 7942–7950. doi:10.12659/MSM.917836
Mei, Z., Wang, Q., Zhang, Y., Liu, P., Ge, M., Du, P., et al. (2019). Risk Factors for Recurrence after anal fistula surgery: a meta-analysis. Int. J. Surg. 69, 153–164. doi:10.1016/j.ijsu.2019.08.003
Mulita, F., Lampropoulos, C., Kehagias, D., Verras, G. I., Tchabashvili, L., Kaplanis, C., et al. (2021). Long-term nutritional deficiencies following sleeve gastrectomy: a 6-year single-centre retrospective study. Prz. Menopauzalny 20 (4), 170–176. doi:10.5114/pm.2021.110954
Mulita, F., Tepetes, K., Verras, G. I., Liolis, E., Tchabashvili, L., Kaplanis, C., et al. (2022). Perineal colostomy: advantages and disadvantages. Prz. Gastroenterol. 17 (2), 89–95. doi:10.5114/pg.2021.109665
NCD Risk Factor Collaboration (NCD-RisC) (2016). Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet 2 (387), 1377–1396. doi:10.1016/S0140-6736(16)30054-X
Noyce, A. J., Kia, D. A., Hemani, G., Nicolas, A., Price, T. R., De Pablo-Fernandez, E., et al. (2017). Estimating the causal influence of body mass index on risk of Parkinson disease: a Mendelian randomisation study. PLoS Med. 14 (6), e1002314. doi:10.1371/journal.pmed.1002314
Pigeyre, M., Yazdi, F. T., Kaur, Y., and Meyre, D. (2016). Recent progress in genetics, epigenetics and metagenomics unveils the pathophysiology of human obesity. Clin. Sci. (Lond). 130 (12), 943–986. doi:10.1042/CS20160136
Sainio, P. (1984). Fistula-in-ano in a defined population. Incidence and epidemiological aspects. Ann. Chir. Gynaecol. 73, 219–224.
Schwandner, O. (2011). Obesity is a negative predictor of success after surgery for complex anal fistula. BMC Gastroenterol. 23 (11), 61. doi:10.1186/1471-230X-11-61
Skrivankova, V. W., Richmond, R. C., Woolf, B. A. R., Yarmolinsky, J., Davies, N. M., Swanson, S. A., et al. (2021). Strengthening the reporting of observational studies in epidemiology using mendelian randomization: the STROBE-MR statement. JAMA 326 (16), 1614–1621. doi:10.1001/jama.2021.18236
Smith, G. D., and Ebrahim, S. (2003). “Mendelian randomization”: can genetic epidemiology contribute to understanding environmental determinants of disease? Int. J. Epidemiol. 32, 1–22. doi:10.1093/ije/dyg070
Unick, J. L., Gaussoin, S. A., Hill, J. O., Jakicic, J. M., Bond, D. S., Hellgren, M., et al. (2017). Objectively assessed physical activity and weight loss maintenance among individuals enrolled in a lifestyle intervention. Obes. (Silver Spring) 25 (11), 1903–1909. doi:10.1002/oby.21971
Verbanck, M., Chen, C. Y., Neale, B., and Do, R. (2018). Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat. Genet. 50 (5), 693–698. doi:10.1038/s41588-018-0099-7
Wang, Y. (2020). Challenges and factors that influencing causal inference and interpretation, based on Mendelian randomization studies. Chin. J. Epidemiol. 41 (8), 1231–1236. doi:10.3760/cma.j.cn112338-20200521-00749
Wei, H. J., Zeng, R., Lu, J. H., Lai, W. F. T., Chen, W. H., Liu, H. Y., et al. (2015). Adipose-derived stem cells promote tumor initiation and accelerate tumor growth by interleukin-6 production. Oncotarget 10 (10), 7713–7726. doi:10.18632/oncotarget.3481
World Health Organization (2020). WHO guidelines on physical activity and sedentary behaviour. Geneva, Switzerland: World Health Organization.
Keywords: two sample Mendelian randomization, body mass index, BMI, anal fistula, causal relationship, incidence risk
Citation: Chen B, Liu Y, Wang Y and Wang Q (2024) Causal relationship between body mass index and anal fistula: a two-sample Mendelian randomization study. Front. Genet. 15:1406231. doi: 10.3389/fgene.2024.1406231
Received: 24 March 2024; Accepted: 10 July 2024;
Published: 25 July 2024.
Edited by:
Vincenzo Davide Palumbo, Euro-Mediterranean Institute of Science and Technology (IEMEST), ItalyReviewed by:
Marcos Edgar Herkenhoff, University of São Paulo, BrazilAndreas Antzoulas, General University Hospital of Patras, Greece
Francesk Mulita, General University Hospital of Patras, Greece
Copyright © 2024 Chen, Liu, Wang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qingming Wang, davidwqm@163.com
†These authors have contributed equally to this work and share first authorship
 Bo Chen
Bo Chen