- 1Latvian Biomedical Research and Study Centre, Riga, Latvia
- 2Department of Clinical Genetics, Institute of Clinical Medicine, Faculty of Medicine, University of Tartu, Tartu, Estonia
- 3Department of Clinical Genetics, United Laboratories, Tartu University Hospital, Tartu, Estonia
- 4Cleft, Lip and Palate Center, Institute of Stomatology, Riga Stradins’University, Riga, Latvia
- 5Medical Genetics Clinic, Children’s Clinical University Hospital, Riga, Latvia
Craniofacial morphogenesis is highly complex, as is the anatomical region involved. Errors during this process, resulting in orofacial clefts, occur in more than 400 genetic syndromes. Some cases of cleft lip and/or palate (CLP) are caused by mutations in single genes; however, complex interactions between genetic and environmental factors are considered to be responsible for the majority of non-syndromic CLP development. The aim of the current study was to identify genetic risk factors in patients with isolated cleft palate (CP) by whole genome sequencing. Patients with isolated CP (n = 30) recruited from the Riga Cleft Lip and Palate Centre, Institute of Stomatology, Riga, were analyzed by whole genome sequencing. Pathogenic or likely pathogenic variants were discovered in genes associated with CP (TBX22, COL2A1, FBN1, PCGF2, and KMT2D) in five patients; hence, rare disease variants were identified in 17% of patients with non-syndromic isolated CP. Our results were relevant to routine genetic counselling practice and genetic testing recommendations. Based on our data, we propose that all newborns with orofacial clefts should be offered genetic testing, at least for a panel of known CLP genes. Only if the results are negative and there is no suggestive family history or additional clinical symptoms (which would support additional exome or genome-wide investigation), should multifactorial empiric recurrence risk prediction tools be applied for families.
Introduction
Craniofacial morphogenesis is a highly complex process, reflecting the sophistication of the anatomical region it concerns. Impairment of this process, resulting in orofacial clefts, occurs in more than 400 genetic syndromes, with various modes of inheritance (OMIM, 2020). Some cases of cleft lip and/or palate (CLP) are caused by mutations in single genes, including COL11A1, GRHL3, IRF6, MSX1, TBX22, or TP63, with 30–40 genes typically screened in CLP clinical diagnosis gene panels (ConcertGenetics, 2021).
In 2008, it was reported that mutation screening of >20 candidate CLP genes resulted in identification of potential syndromic CLP-causing mutations in <10% of screened individuals (Vieira, 2008). Further, complex interactions between genetic and environmental factors mediate non-syndromic CLP development and are responsible for the majority of non-syndromic CLP cases (Fogh-Andersen, 1971).
Mechanisms leading to the development of isolated cleft palate (CP) are thought to differ from those leading to CLP, as a median defect; this classification was proposed in 1971 and remains valid to date (Fogh-Andersen, 1971). Isolated cleft palate is a congenital anomaly caused by the failure of secondary palate fusion process, which is anatomically distinct from the primary palate development. Formation of secondary palate starts around seventh gestational week and continues up to the 12th gestational week, meanwhile, primary palate formation is already finished by seventh/8 weeks (Mossey et al., 2009). CP is less frequent developmental defects compared to CLP. CP prevalence is 1.3–25.3 per 10,000 births and it differs between countries. Higher prevalence registered in Canada and some parts of Northern Europe, lower prevalence in South America and Africa. CLP prevalence is 3.4–22.9 per 10,000 births and it is higher in South America and Asia, thus emphasizing the difference in population genetics. CP is more common in females contrary to CLP, which is more frequent in males, and this aspect is constant across all populations (Mossey and Modell 2012). The manifestation of CP severity varies, it can be classified as unilateral or bilateral, complete, or incomplete, and a submucous form of cleft palate. European congenital anomaly registry EUROCAT study revealed that in 18% cases cleft palate was associated with other congenital anomalies, and in 27% cases CP is one of the symptoms in recognized genetic syndromes. CP and CLP accompanying other major congenital anomalies are referred as syndromic forms, and, similarly, CP and CLP not connected with major congenital anomalies are non-syndromic types (Calzolari et al., 2007). Human Phenotype Ontology database currently lists 857 disease associations with a cleft palate, which includes monogenic diseases with known or unknown etiology, chromosomal aberrations, imprinting disorders and embryofetopathies. CP caused by teratogenic exposure includes use of certain medications during pregnancy, like aminopterin, hydantoin and isotretinoin, or maternal abuse of alcohol, as well as pregnancies complicated by gestational diabetes (Köhler et al., 2021). By far the most common genetic syndrome associated with orofacial cleft is van der Woude syndrome type 1 and 2, caused by pathogenic variants in IRF6 and GRHL3 genes, accordingly. Van der Woude syndrome, however, is a rare exception, as both forms CLP and CP can be present in this syndrome, along with the lip pits (Online Mendelian Inheritance in Man, 1960).
Genetic studies focused on case (or patient parent trio)-control association studies, and facilitated identification of CLP candidate genes, supporting the theory of predominantly multifactorial inheritance patterns in such patients. Complex disease research requires high statistical power, therefore frequently genetic studies included CLP and CP cases as a one sample group. Selected examples of genes whose minor effect variants contribute to CLP development include TGFA (Letra et al., 2012), IRF6 (Murray et al., 1990), TGFB2, MSX1, and TGFB3 (Lidral and Shiang 1997), TBX22 (Marçano et al., 2004), GRHL3 (Peyrard-Janvid et al., 2014) CTNND1, PLEKHA7, PLEKHA5 (L. L. Cox et al., 2018) and GDF11 and FST (T. C. Cox et al., 2019). Further, some association studies identified only risk loci lacking known genes, namely chromosomes 9q21 and 2q32 (Marazita et al., 2004), 19q13 (Warrington et al., 2006) and 8p11 (Riley et al., 2007). Ludwig et al. conducted a large meta-analysis of informative cohorts, leading to detection of seven new loci, in addition to those already known, as follows: chromosomes 1p36, 2p21, 3p11.1, 8q21.3, 13q31.1, 8q24, and 15q22 (Ludwig et al., 2012).
More affordable genetic technologies have transformed CLP research; most association studies are now genome-wide, and three large studies employing whole exome and whole genome approaches have been conducted. Whole exome sequencing (WES) of 57 multinational families was conducted with the precise aim of identifying novel copy number variations in known genes and risk loci, and detected five informative deletions in the CDH1, FGF8, FGFR4, TRPS1, and FTCD genes (Bureau et al., 2014). To date, the largest study conducted involved whole genome sequencing (WGS) of 315 European and 265 Latin American trios, all having offspring with CLP, resulting in genome-wide association data confirming previous findings and adding a new locus, chromosome 21q22.3 (Mukhopadhyay et al., 2020).
Despite massive WGS studies, it has always been presumed that some patients with non-syndromic CLP have rare variants in disease-causing genes. This hypothesis was confirmed by Basha et al., who conducted a WES study demonstrating that approximately 10% of cases previously described as non-syndromic CLP were patients with rare genetic syndromes. Further, patients were first screened for IRF6 mutations, and positive cases were excluded from the study; therefore, the actual percentage with genetic syndromes may have been higher (Basha et al., 2018).
Our aim in the current project was to identify genetic risk factors by WGS in patients with isolated CP. We hypothesized that we would identify rare variants causing monogenic syndromes, as well as new copy number variations, in a well-described group of patients with isolated CP.
Materials and Methods
Recruitment of Families and Ethics Statement
Patients were recruited in 2000–2020 from the Riga Cleft Lip and Palate Centre, Institute of Stomatology, Riga Stradins University as described previously (Lace et al., 2006). All patients with orofacial clefts were evaluated by clinical geneticist and initial investigations of syndromic forms were performed. 56 probands with isolated cleft palate and both of their parents were included in the study, of them 21 cases were rejected due to insufficient DNA quality because of long term storage and multiple episodes of thaw and re-freezing. Five patients with known pathogenic variants in IRF6 and GRHL3 genes were excluded from the study as syndromic forms of cleft palate cases. In the families with identified de novo variants DNA profiling was performed.
This study was approved by the Central Medical ethics committee of Latvia. The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments. All participants and/or their legal guardians provided written informed consent prior to enrolment.
Library Preparation and Whole Genome Sequencing
Libraries were prepared from 300 ng of high-quality genomic DNA using a MGIEasy Universal DNA Library Prep Set (MGI Tech Co., Shenzhen, China), according to the manufacturer’s instructions. Libraries were sequenced at a mean coverage of 30× on the MGI MGISEQ-2000RS platform, using a nanoball approach, to generate 150 bp paired-end reads.
Bioinformatics Analyses of Genome Data and Variant Filtering
Bioinformatics data processing was carried out at the High Performance Computing Center of the University of Tartu (University of Tartu 2018). Output Fastq files were processed and variants were called using WDL scripts and the Cromwell workflow management system (Van der Auwera and O’Connor, 2020), adhering to GATK v4 best practice guidelines. In brief, raw sequencing reads were mapped to the hg38 human reference genome using the BWA MEM algorithm (v0.7.17) (Li and Durbin 2010), followed by processing using GATK (v4.1.4.0), including flagging of duplicate reads and recalibration of base quality scores. Variants were first called for individual samples using the GATK HaplotypeCaller before multi-sample joint aggregation and re-annotation using GATK GenotypeGVCFs. The variant call set was annotated using hail .2 (Hail Team, Hail .2: https://github.com/hail-is/hail) and then uploaded to the Seqr platform (https://github.com/broadinstitute/seqr) for collaborative variant analysis. Variant filtration focused on rare variants in coding regions and splice-sites predicted to affect protein function and following the known inheritance pattern for the 198 CP associated genes (Supplementary Table S1), followed by pathogenic/likely pathogenic variants in OMIM genes, and 67 actionable genes, according to American College of Medical Genetics (ACMG) recommendations. Reported variants were validated by direct sequencing using 10 pm of each primer (primer sequences are available upon request), BigDye™ Terminator v3.1 Cycle Sequencing Kit (ThermoFisher Scientific, USA), and an ABI PRISM 3100 sequencer (Applied Biosystems, USA).
Copy number variants (CNVs) were assessed using WGS reads by two approaches. First, large CNVs and aneuploidies were screened using indexcov (Pedersen et al., 2017). Second, structural variants, including CNVs, inversions, and translocations, were called using Manta (Chen et al., 2016).
Results
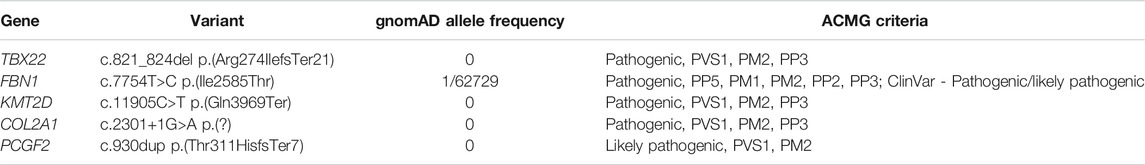
A total of 30 patients with isolated CP were analyzed by WGS, and pathogenic or likely pathogenic variants were discovered in genes associated with CP (TBX22, COL2A1, FBN1, PCGF2, KMT2D) in five of these patients, as detailed below. Summary of identified variants in Table 1. Here and further LAHSHAL classification was used (Kriens, 1989), where letters itself specifies anatomical site (L -lip, A—alveolus, H—hard palate, S—soft palate), capital letters identify total cleft in the anatomical site, small letter means partial cleft and star means submucous cleft.
A male, age 21 years (identification no (ID): 0901) presented with a cleft soft-hard palate (HSH; LAHSHAL classification), velopharyngeal incompetence, speech disorder, and conductive deafness. An X-linked variant, NM_001109879.2 TBX22 c.821_824del p.(Arg274IlefsTer21), was identified in the proband in a hemizygous state; his unaffected mother was a heterozygous carrier. This variant is absent from the gnomAD v3 genomes database (Karczewski et al., 2020) and classified as likely pathogenic according to the ACMG guidelines.
A 17-year-old female (ID: 13401) with maxillary hypoplasia and cleft in the soft palate was found to be a heterozygous carrier of the disease-associated variant, NM_000138.5 FBN1 c.7754T>C p.(Ile2585Thr), inherited from her mother. This variant was previously reported in patients with Marfan syndrome (Loeys, 2001; Arnaud et al., 2019), and is listed in ClinVar as pathogenic/likely pathogenic (Landrum et al., 2018).
A female of 13-years-old (ID: 24701) with isolated CP (hSh, LAHSHAL) presented with global developmental delay, language delay, astigmatism, strabismus, and recent tension headaches. She had a history of chronic otitis media, treated by tympanoplasty. Brain MRI did not reveal any abnormalities besides vertebral artery development variation. A de novo disease-causing variant, NM_003482.4 KMT2D c.11905C>T p.(Gln3969Ter), was identified and classified as pathogenic by ACMG criteria. The variant was absent from the gnomAD v3 database (Karczewski et al., 2020). Parentity was confirmed.
A male, age 28 years, (ID: 11801) with isolated CP (hSh, LAHSHAL) was found to have a paternally inherited variant, NM_001844.5 COL2A1 c.2301+1G>A p.(?), absent from the gnomAD v3. database and previously reported as a disease-causing alteration (Korkko et al., 2000).
A 12-year-old female patient (ID: 24801) with CP (*S*, LAHSHAL) and a history of intrauterine growth retardation, followed by developmental delay, expressive language delay, and behavioral issues, was found to have the variant NM_001136498.2 PCGF2 c.930dup p.(Thr311HisfsTer7), also present in her affected father. This variant is absent from the gnomAD v3 database (Karczewski et al., 2020), and likely pathogenic, according to ACMG criteria. The patient had been under genetic investigation from the age of 4 years.
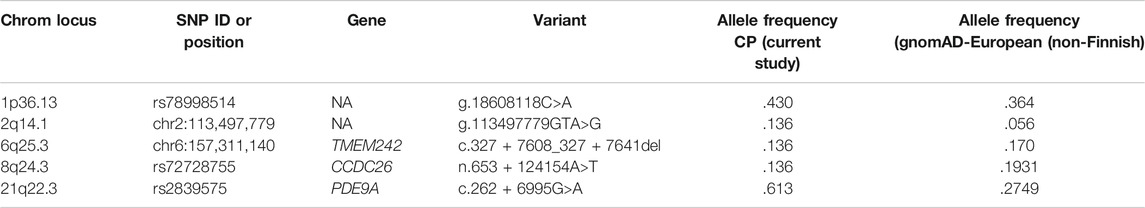
With the consent of patients/parents, information about identified variants was transferred to the clinical geneticist in charge. There were no other variants actionable by ACMG criteria to report back to families. Pathogenic copy number variations were not identified. In addition, 20 nucleotide polymorphisms (SNP) (Supplementary Table S2) were screened in the remaining 25 samples. SNPs included in the analysis were chosen based on a WGS study published in 2020 (Mukhopadhyay et al., 2020), and five of them were identified in our cohort; however, their allelic frequencies were not significantly different relative to gnomAD data (Karczewski et al., 2020), likely due to limited statistical power because of our small sample size (Table 2).
Discussion
Clinically available genetic tests for infants born with CLP could offer rapid and relatively inexpensive precision diagnosis, prognosis prediction, and family counselling. Arguments that some of those syndromes can be diagnosed clinically are not valid, since some of the main clinical presentations of syndromes may only emerge at a later age (e.g., Stickler syndrome); therefore, routine genetic testing is a powerful tool available for practicing clinical specialists.
One of the families included in this study had an X-linked disease-associated variant in the TBX22 gene, which has never been described before and was inherited from the unaffected mother. TBX22 has been described in several previous studies (Braybrook et al., 2001; Marçano et al., 2004; Demeer et al., 2018) as a cause of X-linked semi-dominant CP and ankyloglossia (CPX) (OMIM). Further, variants in TBX22 were identified in 2.5% of isolated non-syndromic CP cases (n = 200) (Marçano et al., 2004), and in 16% of cases in a smaller WES study of 12 non-syndromic patients with CLP and CP (Demeer et al., 2018). Ankyloglossia is the most frequent disease presentation associated with TBX22 gene variants and is a minor anomaly, rarely considered important to report in patients or their family members (Braybrook et al., 2001). The role of TBX22 during palatogenesis was confirmed in experiments using Tbx22null mice, which presented with submucous CP, ankyloglossia, severely underdeveloped vomer, and choanal atresia, caused by reduced bone formation in the posterior hard palate due to impaired ossification (Pauws et al., 2009). The recurrence risk calculation for our family changed because of the results of genetic testing. The mother is a carrier of this X-linked variant; therefore, the recurrence risk in the family is as high as 25%–50%, rather than the 3% empiric risk established for isolated CP. Risk of CP development in males hemizygous for the pathogenic variant is 96%, whereas in heterozygous females, the risk is only 6% (Marçano et al., 2004).
Kabuki syndrome with a de novo pathogenic nonsense KMT2D c.11905C>T, p.Gln3969Ter variant was identified in one of the probands who had global developmental delay. Cleft lip and or palate is among the structural findings in 30% of such cases (Paik and Lim 2016). The recurrence risk for the family is 1%, based on theoretical gonadal mosaicism.
A somewhat surprising finding was the identification of a patient with Marfan syndrome in our cohort. According to the Ghent criteria (Loeys et al., 2010) (Loeys et al., 2010), malar hypoplasia and a high arched palate, as present in our patient, are minor criteria for skeletal involvement. For children and young adults <20 years old, the clinical presentation of Marfan syndrome can be vague, in the absence of early cardiovascular or ocular symptoms, which explains the lack of earlier investigation for Marfan syndrome in our patient. The recurrence risk in the family is 50%.
A very rare novel disease-associated variant, c.930dup p.(Thr311HisfsTer7), in PCGF2 was discovered in a female patient with positive family history. To date, 13 cases with pathogenic variants in the PCGF2 gene have been described (Turnpenny et al., 2018), with prevalent features including intellectual disability, impaired growth (including intrauterine), and a range of cardiovascular and skeletal anomalies. High palate and bifid uvula have been described in two of the 13 reported patients. Our patient had a history of pre- and postnatal growth retardation, mild intellectual disability, expressive language delay, and a cleft soft palate. The PCGF2 gene has roles in cell proliferation and differentiation and, due its dominant negative effect on histone binding during embryogenesis, it is associated with a recognizable syndrome (Turnpenny et al., 2018).
In 2010, we conducted a case-control association study of the same patient cohort with isolated CP and concluded that COL2A1 and COL11A2 contribute to the risk of non-syndromic CP (Nikopensius et al., 2010). Further, we hypothesized that confirmed association could also be explained by COL11A2 and COL2A1 disease-associated variants in some patients. The current WGS analysis confirmed the presence of a pathogenic COL2A1 variant in a patient with CP in our study group, supporting our hypothesis that patients with monogenic disease were likely present among previously analyzed cohorts of patients with CLP. Therefore, the COL2A1 and COL11A2 genes are unlikely to be associated with non-syndromic forms of CP via complex interactions among common minor effect gene variants and environmental factors. The pathogenic variant in our case was inherited from the affected father; hence the recurrence risk for the family is 50%.
Additionally, we analyzed 20 variants identified by previous WGS association studies of individuals from Europe with CLP. Variants in the chromosomal loci 2q14.1 and 21q22.3 were more frequent in our CP patient group than in data from the general European population. Interestingly, one of these variants (c.262 + 6995G>A) is localized in the PDE9A gene, and haploinsufficiency of this gene and others in the 21q22.3 locus, within deletions of 1–10 Mb, is reportedly associated with a CP phenotype in 12.5% cases; however, duplications of this region of any size were never associated with cleft formation (Firth et al., 2009).
We identified rare disease variants in 17% of patients with non-syndromic isolated CP. Applications of these results in routine practice altered genetic counselling and recommendations for genetic testing. Based on our results, we propose that all newborns with orofacial clefts should undergo genetic testing, at least with an appropriate gene panel for CLP; only after negative results, and where there is no suggestive family history or additional clinical symptoms (which validate the requirement for additional exome or genome-wide investigations), should a multifactorial risk prediction percentage be provided for families.
Data Availability Statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: https://www.lovd.nl, 0000816624, 0000816623, 0000816622. Accession: E-MTAB-11360. https://www.ebi.ac.uk/arrayexpress/experiments/E-MTAB-11360.
Ethics Statement
The studies involving human participants were reviewed and approved by the Central Medical Ethics Committee of Latvia. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author Contributions
BL: drafted the manuscript, interpreted variants, and secured funding for the project; SP: conducted bioinformatics data processing, variant calling, and interpretation; DL: conducted WGS analysis and Sanger sequencing; IG: described patient and family phenotypes; IA: recruited patients and drafted the manuscript; IM: recruited patients and drafted the manuscript; BB: recruited patients and drafted the manuscript; JS: selected and prepared samples, and drafted the manuscript; II: drafted the manuscript, and conducted WGS analysis and Sanger sequencing.
Funding
This project was funded by the Latvian Research Council, Grant no: lzp-2020/2-0374 “Deciphering the genetic mechanisms of the individuals with isolated cleft palate by whole genome sequencing”. SP was supported by an Estonian Research Council grant (MOBTP175).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgene.2022.828534/full#supplementary-material
References
Arnaud, P., Hanna, N., Benarroch, L., Aubart, M., Bal, L., Bouvagnet, P., et al. (2019). Genetic Diversity and Pathogenic Variants as Possible Predictors of Severity in a French Sample of Nonsyndromic Heritable Thoracic Aortic Aneurysms and Dissections (NshTAAD). Genet. Med. 21 (9), 2015–2024. doi:10.1038/s41436-019-0444-y
Basha, M., Demeer, B., Revencu, N., Helaers, R., Theys, S., Bou Saba, S., et al. (2018). Whole Exome Sequencing Identifies Mutations in 10% of Patients with Familial Non-syndromic Cleft Lip And/or Palate in Genes Mutated in Well-Known Syndromes. J. Med. Genet. 55 (7), 449–458. doi:10.1136/jmedgenet-2017-105110
Braybrook, C., Doudney, K., Marçano, A. C. B., Arnason, A., Bjornsson, A., Patton, M. A., et al. (2001). The T-Box Transcription Factor Gene TBX22 Is Mutated in X-Linked Cleft Palate and Ankyloglossia. Nat. Genet. 29 (2), 179–183. doi:10.1038/ng730
Bureau, A., Parker, M. M., Ruczinski, I., Taub, M. A., Marazita, M. L., Murray, J. C., et al. (2014). Whole Exome Sequencing of Distant Relatives in Multiplex Families Implicates Rare Variants in Candidate Genes for Oral Clefts. Genetics 197 (3), 1039–1044. doi:10.1534/genetics.114.165225
Calzolari, E., Pierini, A., Astolfi, G., Bianchi, F., Neville, A. J., and Rivieri, F. (2007). Associated Anomalies in Multi-Malformed Infants with Cleft Lip and Palate: An Epidemiologic Study of Nearly 6 Million Births in 23 EUROCAT Registries. Am. J. Med. Genet.A. 143A (6), 528–537. doi:10.1002/ajmg.a.31447
Chen, X., Schulz-Trieglaff, O., Shaw, R., Barnes, B., Schlesinger, F., Källberg, M., et al. (2016). Manta: Rapid Detection of Structural Variants and Indels for Germline and Cancer Sequencing Applications. Bioinformatics 32 (8), 1220–1222. doi:10.1093/bioinformatics/btv710
ConcertGenetics (2021). Precision Medicine Is the Most Exciting Frontier in Healthcare. Available at: https://www.concertgenetics.com (Accessed 0212, 2021).
Cox, L. L., Cox, T. C., Uribe, L. M. M., Zhu, Y., Richter, C. T., Nidey, N., et al. (2018). Mutations in the Epithelial Cadherin-P120-Catenin Complex Cause Mendelian Non-syndromic Cleft Lip with or without Cleft Palate. Am. J. Hum. Genet. 102 (6), 1143–1157. doi:10.1016/j.ajhg.2018.04.009
Cox, T. C., Lidral, A. C., McCoy, J. C., Liu, H., Cox, L. L., Zhu, Y., et al. (2019). Mutations in GDF11 and the Extracellular Antagonist, Follistatin, as a Likely Cause of Mendelian Forms of Orofacial Clefting in Humans. Hum. Mutat. 40 (10), 1813–1825. doi:10.1002/humu.23793
Demeer, B., Revencu, N., Helaers, R., Devauchelle, B., François, G., Bayet, B., et al. (2018). Unmasking Familial CPX by WES and Identification of Novel Clinical Signs. Am. J. Med. Genet. 176 (12), 2661–2667. doi:10.1002/ajmg.a.40630
Firth, H. V., Richards, S. M., Bevan, A. P., Clayton, S., Corpas, M., Rajan, D., et al. (2009). DECIPHER: Database of Chromosomal Imbalance and Phenotype in Humans Using Ensembl Resources. Am. J. Hum. Genet. 84 (4), 524–533. doi:10.1016/j.ajhg.2009.03.010
Fogh-Andersen, P. (1971). Epidemiology and Etiology of Clefts. Birth Defects Orig Artic Ser. 7 (7), 50–53.
Karczewski, K. J., Francioli, L. C., Tiao, G., Cummings, B. B., Alföldi, J., Wang, Q., et al. (2020). The Mutational Constraint Spectrum Quantified from Variation in 141,456 Humans. Nature 581 (7809), 434–443. doi:10.1038/s41586-020-2308-7
Köhler, S., Gargano, M., Matentzoglu, N., Carmody, L. C., Lewis-Smith, D., Vasilevsky, N. A., et al. (2021). The Human Phenotype Ontology in 2021. Nucleic Acids Res. 49 (D1), D1207–D1217. doi:10.1093/nar/gkaa1043
Korkko, J., Cohn, D. H., and Ala-Kokko, L. (2000). Deborah Krakow, and Darwin J. ProckopWidely Distributed Mutations in the COL2A1 Gene Produce Achondrogenesis Type II/Hypochondrogenesis. Am. J. Med. Genet. 92 (2), 95–100. doi:10.1002/(SICI)1096-8628(20000515)92:2<95:AID-AJMG3>3.0.CO;2-9
Kriens, O. (1989). What Is a Cleft Lip and Palate? : A Multidisciplinary Update : Proceedings of an Advanced Workshop. Stuttgart: Thieme.
Lace, B., Vasiljeva, I., Dundure, I., Barkane, B., Akota, I., and Krumina, A. (2006). Mutation Analysis of the MSX1 Gene Exons and Intron in Patients with Nonsyndromic Cleft Lip and Palate. Stomatologija 8 (1), 21–24.
Landrum, M. J., LeeLee, J. M., Benson, M., Brown, G. R., Chao, C., Chitipiralla, S., et al. (2018). ClinVar: Improving Access to Variant Interpretations and Supporting Evidence. Nucleic Acids Res. 46 (D1), D1062–D1067. doi:10.1093/nar/gkx1153
Letra, A., Fakhouri, W., Fonseca, R. F., Menezes, R., Kempa, I., Prasad, J. L., et al. (2012). Interaction between IRF6 and TGFA Genes Contribute to the Risk of Nonsyndromic Cleft Lip/Palate. PLoS ONE 7 (9), e45441. doi:10.1371/journal.pone.0045441
Li, H., and Durbin, R. (2010). Fast and Accurate Long-Read Alignment with Burrows-Wheeler Transform. Bioinformatics 26 (5), 589–595. doi:10.1093/bioinformatics/btp698
Lidral, A. C., Murray, J. C., Buetow, K. H., Basart, A. M., Schearer, H., Shiang, R., et al. (1997). Studies of the Candidate Genes TGFB2, MSX1,TGFA, and TGFB3 in the Etiology of Cleft Lip and Palate in the Philippines. Cleft Palate-Craniofacial J. 34 (1), 1–6. doi:10.1597/1545-1569_1997_034_0001_sotcgt_2.3.co_2
Loeys, B. (2001). Genotype and Phenotype Analysis of 171 Patients Referred for Molecular Study of the Fibrillin-1 Gene FBN1 Because of Suspected Marfan Syndrome. Arch. Intern. Med. 161 (20), 2447–2454. doi:10.1001/archinte.161.20.2447
Loeys, B. L., Dietz, H. C., Braverman, A. C., Callewaert, B. L., De Backer, J., Devereux, R. B., et al. (2010). The Revised Ghent Nosology for the Marfan Syndrome. J. Med. Genet. 47 (7), 476–485. doi:10.1136/jmg.2009.072785
Ludwig, K. U., Mangold, E., Herms, S., Nowak, S., Reutter, H., Paul, A., et al. (2012). Genome-Wide Meta-Analyses of Nonsyndromic Cleft Lip with or without Cleft Palate Identify Six New Risk Loci. Nat. Genet. 44 (9), 968–971. doi:10.1038/ng.2360
Marazita, M. L., Murray, J. C., Lidral, A. C., Arcos-Burgos, M., Cooper, M. E., Goldstein, T., et al. (2004). Meta-Analysis of 13 Genome Scans Reveals Multiple Cleft Lip/Palate Genes with Novel Loci on 9q21 and 2q32-35. Am. J. Hum. Genet. 75 (2), 161–173. doi:10.1086/422475
Marcano, A. C. B., Doudney, K., Braybrook, C., Squires, R., Patton, M. A., Lees, M. M., et al. (2004). TBX22 Mutations Are a Frequent Cause of Cleft Palate. J. Med. Genet. 41 (1), 68–74. doi:10.1136/jmg.2003.010868
Mossey, P. A., Little, J., Munger, R. G., Dixon, M. J., and Shaw, W. C. (2009). Cleft Lip and Palate. The Lancet 374 (9703), 1773–1785. doi:10.1016/S0140-6736(09)60695-4
Mossey, P. A., and Modell, B. (2012). Epidemiology of Oral Clefts 2012: An International Perspective. Front. Oral Biol. 16, 1–18. doi:10.1159/000337464
Mukhopadhyay, N., Bishop, M., Mortillo, M., Chopra, P., Hetmanski, J. B., Taub, M. A., et al. (2020). Whole Genome Sequencing of Orofacial Cleft Trios from the Gabriella Miller Kids First Pediatric Research Consortium Identifies a New Locus on Chromosome 21. Hum. Genet. 139 (2), 215–226. doi:10.1007/s00439-019-02099-1
Murray, J. C., Nishimura, D. Y., Buetow, K. H., Ardinger, H. H., Spence, M. A., Sparkes, R. S., et al. (1990). Linkage of an autosomal dominant clefting syndrome (Van der Woude) to loci on chromosome Iq. Am. J. Hum. Genet. 46 (3), 486–491.
Nikopensius, T., Jagomägi, T., Krjutškov, K., Tammekivi, V., Saag, M., Prane, I., et al. (2010). Genetic Variants in COL2A1, COL11A2, and IRF6 Contribute Risk to Nonsyndromic Cleft Palate. Birth Defects Res. A: Clin. Mol. Teratology 88 (9), 748–756. doi:10.1002/bdra.20700
Online Mendelian Inheritance in Man (1960). An Online Catalog of Human Genes and Genetic Disorders. Baltimore, MD: McKusick-Nathans Institute of Genetic Medicine, Johns Hopkins University. Available at: https://omim.org/.
Paik, J. M., and Lim, S. Y. (2016). Kabuki Syndrome with Cleft Palate. Arch. Plast. Surg. 43 (5), 474–476. doi:10.5999/aps.2016.43.5.474
Pauws, E., Hoshino, A., Bentley, L., Prajapati, S., Keller, C., Hammond, P., et al. (2009). Tbx22 Null Mice Have a Submucous Cleft Palate Due to Reduced Palatal Bone Formation and Also Display Ankyloglossia and Choanal Atresia Phenotypes. Hum. Mol. Genet. 18 (21), 4171–4179. doi:10.1093/hmg/ddp368
Pedersen, B. S., Collins, R. L., Quinlan, M. E., and au, A. R. (2017). Indexcov: Fast Coverage Quality Control for Whole-Genome Sequencing. GigaScience 6 (11), 1–6. doi:10.1093/gigascience/gix090
Peyrard-Janvid, M., Leslie, E. J., Kousa, Y. A., Smith, T. L., Dunnwald, M., Magnusson, M., et al. (2014). Dominant Mutations in GRHL3 Cause Van Der Woude Syndrome and Disrupt Oral Periderm Development. Am. J. Hum. Genet. 94 (1), 23–32. doi:10.1016/j.ajhg.2013.11.009
Riley, B. M., Schultz, R. E., Cooper, M. E., Goldstein-McHenry, T., Daack-Hirsch, S., Lee, K. T., et al. (2007). A Genome-wide Linkage Scan for Cleft Lip and Cleft Palate Identifies a Novel Locus on 8p11-23. Am. J. Med. Genet. 143A (8), 846–852. doi:10.1002/ajmg.a.31673
Turnpenny, P. D., Wright, M. J., Sloman, M., Caswell, R., van Essen, A. J., Gerkes, E., et al. (2018). Missense Mutations of the Pro65 Residue of PCGF2 Cause a Recognizable Syndrome Associated with Craniofacial, Neurological, Cardiovascular, and Skeletal Features. Am. J. Hum. Genet. 103 (5), 786–793. doi:10.1016/j.ajhg.2018.09.012
Van der Auwera, G. A., and O'Connor, B. (2020). Genomics in the Cloud: Using Docker, GATK, and WDL in Terra. 1st ed. Newton, Massachusetts, United States: O’Reilly Media.
Vieira, A. R. (2008). Unraveling Human Cleft Lip and Palate Research. J. Dent Res. 87 (2), 119–125. doi:10.1177/154405910808700202
Keywords: isolated cleft palate, whole genome sequencing, rare monogenic diseases, recurrence risk, PCGF2
Citation: Lace B, Pajusalu S, Livcane D, Grinfelde I, Akota I, Mauliņa I, Barkāne B, Stavusis J and Inashkina I (2022) Monogenic Versus Multifactorial Inheritance in the Development of Isolated Cleft Palate: A Whole Genome Sequencing Study. Front. Genet. 13:828534. doi: 10.3389/fgene.2022.828534
Received: 03 December 2021; Accepted: 25 January 2022;
Published: 24 February 2022.
Edited by:
Gerson Shigeru Kobayashi, University of São Paulo, BrazilReviewed by:
Xiaoming Liu, University of South Florida, United StatesGeorges Nemer, Hamad Bin Khalifa University, Qatar
Alexandre Rezende Vieira, University of Pittsburgh, United States
Copyright © 2022 Lace, Pajusalu, Livcane, Grinfelde, Akota, Mauliņa, Barkāne, Stavusis and Inashkina. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Baiba Lace, QmFpYmEubGFjZUBiaW9tZWQubHUubHY=, b3JjaWQub3JnLzAwMDAtMDAwMS01MzcxLTY3NTY=
 Baiba Lace
Baiba Lace Sander Pajusalu
Sander Pajusalu Diana Livcane1
Diana Livcane1 Inna Inashkina
Inna Inashkina