
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Genet., 16 August 2021
Sec. Applied Genetic Epidemiology
Volume 12 - 2021 | https://doi.org/10.3389/fgene.2021.717533
A correction has been applied to this article in:
Corrigendum: Genetic Polymorphism of Vitamin D Family Genes CYP2R1, CYP24A1, and CYP27B1 Are Associated With a High Risk of Non-alcoholic Fatty Liver Disease: A Case-Control Study
 Minxian Wang1†
Minxian Wang1† Ru Zhang1†
Ru Zhang1† Min Wang1
Min Wang1 Liuxin Zhang2
Liuxin Zhang2 Yajie Ding1
Yajie Ding1 Zongzhe Tang1
Zongzhe Tang1 Hongliang Wang3
Hongliang Wang3 Wei Zhang4
Wei Zhang4 Yue Chen1
Yue Chen1 Jie Wang1*
Jie Wang1*Background: Previous studies have highlighted the important role of vitamin D and calcium pathway genes in immune modulation, cell differentiation and proliferation, and inflammation regulation, all closely implicated in the pathogenesis of non-alcoholic fatty liver disease (NAFLD).
Objective: This study aims to investigate whether 11 candidate single nucleotide polymorphisms (SNPs) in vitamin D and calcium pathway genes (CYP2R1, CYP24A1, and CYP27B1) are associated with the risk of NAFLD.
Methods: In this case-control study, a total of 3,023 subjects were enrolled, including 1,114 NAFLD cases and 1,909 controls. Eleven genetic variants in CYP2R1, CYP24A1, and CYP27B1 genes were genotyped. Logistic regression analysis was used to assess the effects of these variants on NAFLD risk. The functional annotations of positive SNPs were further evaluated by bioinformatics analysis.
Results: After adjusting for age, gender, and metabolic measures, we identified that CYP24A1 rs2296241 variant genotypes (recessive model: OR, 1.316; 95% CI, 1.048–1.653; p = 0.018), rs2248359 variant genotypes (recessive model: OR, 1.315; 95% CI, 1.033–1.674; p = 0.026), and CYP27B1 rs4646536 variant genotypes (additive model: OR, 1.147; 95% CI, 1.005–1.310; p = 0.042) were associated with an elevated risk of NAFLD. In combined effects analysis, we found that NAFLD risk significantly increased among patients carrying more rs2296241-A, rs2248359-T, and rs4646536-T alleles (ptrend = 0.049). Multivariate stepwise analysis indicated that age, visceral obesity, ALT, γ-GT, hypertriglyceridemia, hypertension, low HDL-C, hyperglycemia, and unfavorable alleles were independent predictors of NAFLD (all p < 0.05). The area under the receiver operating characteristic curve was 0.789 for all the above factors.
Conclusion: The polymorphisms of vitamin family genes CYP24A1 (rs2296241, CYP24A1, and rs2248359) and CYP27B1 (rs4646536) were associated with NAFLD risk in Chinese Han population, which might provide new insight into NAFLD pathogenesis and tools for screening high-risk population.
Non-alcoholic fatty liver disease (NAFLD) has emerged as a major chronic liver disease, afflicting more than one-quarter of adults worldwide (Younossi et al., 2016). Previous studies have shown that NAFLD cannot only cause liver-related complications, such as non-alcoholic steatohepatitis (NASH), cirrhosis, hepatocellular carcinoma (HCC) (Lindenmeyer and McCullough, 2018) but also increase the risk of other extrahepatic diseases, such as cardiovascular disease (CVD) (Targher et al., 2010), type 2 diabetes mellitus (T2DM) (Tilg et al., 2017), and chronic kidney disease (Byrne and Targher, 2020). Its high global prevalence and poor prognosis have made NAFLD a serious public health threat.
The mechanisms underlying NAFLD are far from clear (Tarantino et al., 2019). Previous studies have indicated that NAFLD is a multi-factorial disease associated with a high frequency of metabolic comorbidities (Italian Association for the Study of the Liver (Aisf), 2017). Experts have reached a consensus on suggesting to rename NAFLD as metabolic-associated fatty liver disease (MAFLD), a more appropriate overarching term (Eslam et al., 2020). Dynamic interactions among insulin resistance, lipid metabolism, genetic variation, and other environmental factors shape the susceptibility and progression of this disease (Buzzetti et al., 2016; Eslam and George, 2016).
Vitamin D mediates immune-inflammatory and metabolic processes (Charoenngam and Holick, 2020; Szymczak-Pajor et al., 2020). Numerous studies have found that vitamin D deficiency is closely associated to the occurrence or development of insulin resistance-related diseases, such as T2DM, metabolic syndrome, and NAFLD (Cimini et al., 2017; Dawson-Hughes et al., 2020), despite its well-established roles in calcium homeostasis and bone mineralization (Reid et al., 2014; Borel et al., 2015). The local activated form of vitamin D is 1,25-dihydroxy vitamin D3 [1,25(OH)2D3]. Many diseases arise from low serum level of 25-hydroxyvitamin D3 [25(OH)D3], rather than vitamin D (Gandini et al., 2011).
The activation of 1,25(OH)2D3 requires two sets of hydroxylation. Vitamin D hydroxylases play a prominent role in this process (Höbaus et al., 2013). Vitamin D3 (cholecalciferol) is formed by cholesterol in the skin after exposure to sunlight. On the one hand, vitamin D3 is first hydrolyzed and synthesized into 25(OH)D3 and further catalyzed by 25-hydroxylase encoded by cytochrome P450 family 2 subfamily R member 1 (CYP2R1) and cytochrome P450 family 27 subfamily A member 1 (CYP27A1) genes. 25(OH)D3 is then hydroxylated in the kidney and synthesized into 1,25(OH)2D3 in other organs, which is catalyzed by the 1α-hydroxylase encoded by cytochrome P450 family 27 subfamily B member 1 (CYP27B1) gene. On the other hand, 1,25(OH)2D3 can be decomposed by 1,25-hydroxyvitamin-D3-24-hydroxylase encoded by cytochrome P450 family 24 subfamily A member 1 (CYP24A1) gene, maintaining the balance of vitamin D metabolism in vivo. Several genetic studies have reported that common single nucleotide polymorphisms (SNPs) in vitamin D pathway genes are associated with low-level serum 25(OH)D, including vitamin D receptor (VDR), vitamin D-binding protein (VDBP), CYP2R1, CYP24A1, and CYP27B1 (Bedogni et al., 2006; Angulo et al., 2007; Wang et al., 2010; Boyle et al., 2012; Visscher et al., 2012; Zhu and DeLuca, 2012; Dastani et al., 2013; Braithwaite et al., 2015; Hibler et al., 2015; Woods et al., 2015; Jolliffe et al., 2016; Jung and Shin, 2016; Cheng et al., 2017; Thacher and Levine, 2017; Gibson et al., 2018; National Workshop on Fatty Liver and Alcoholic Liver Disease, Chinese Society of Hepatology, Association et al., 2018; Arai et al., 2019; Cho et al., 2019; Younossi, 2019; Zhang et al., 2019; Liu et al., 2020; Ma et al., 2020; Qian et al., 2020; Torkko et al., 2020; Yu et al., 2020). Genome-wide association studies (GWAS) have also identified that variants near these genes are associated with vitamin D status (Wang et al., 2010; Visscher et al., 2012). Moreover, previous studies have suggested a role of VDR, VDBP gene polymorphisms in the progression of liver diseases such as inflammation, liver fibrosis (Jung and Shin, 2016; Arai et al., 2019). Therefore, we hypothesized that the polymorphisms of these hydroxylase gene might regulate serum VD level and related biological processes. However, limited evidence can prove the influence of vitamin D family genes (CYP2R1, CYP24A1, CYP27B1) polymorphisms on NAFLD susceptibility.
The aim of this study was to investigate the correlation of candidate SNPs in vitamin D and calcium pathway genes (CYP2R1, CYP24A1, and CYP27B1) with the risk of NAFLD among Chinese Han population. Our findings may deepen our understanding of NAFLD and provide strategies for the screening, prevention, and individualized treatment of NAFLD patients.
The participants of this case-control study were recruited from a community (Nanjing, Jiangsu, China) from July to September 2018. NAFLD was diagnosed based on Guideline of prevention and treatment for non-alcoholic fatty liver disease: a 2018 update (National Workshop on Fatty Liver and Alcoholic Liver Disease, Chinese Society of Hepatology, Association et al., 2018). Diagnostic guidelines: (1) no history of drinking or overdose drinking (less than 210 g/week ethanol for men and 140 g/week for women in the past 12 months); (2) absence of drug hepatitis, hepatitis C virus genotype 3 infection, hepatolenticular degeneration, and other specific diseases that could result in fatty liver; (3) mildly to moderately increased serum levels of transaminase and γ-glutamyl transpeptidase (γ-GT) (<5 times above the upper normal limit), usually presenting as an increase in alanine aminotransferase (ALT); (4) metabolic syndrome constituents, such as visceral obesity, hyperglycemia, blood lipid disorder, and hypertension; (5) imaging results meeting the diagnostic criteria of diffuse fatty liver; and (6) histological findings of liver biopsy meeting the pathological diagnostic criteria of fatty liver disease. Since liver biopsy was difficult to obtain, we used the liver imaging methods mentioned in the guideline. NAFLD was diagnosed if criteria 1–4 coexist with criterion 5. The hepatic ultrasound examination was performed using a LOGIQ-E9 ultrasound system (General Electric Healthcare, Milwaukee, WI, United States).
Those patients diagnosed with NAFLD were grouped. The non-NAFLD controls were collected from the same community during the study period and randomly assigned to the control group. The constituent ratios of gender and age between case and control groups were considered similar, according to the result of frequency matching. Included were patients (1) signing informed consent; (2) aged between 18 and 60 years. Excluded were those: (1) taking antihypertensive, antidiabetic, lipid-lowering, or hypouricemic agents within 24-h before physical examination; (2) with infection, acute or chronic gastrointestinal diseases, autoimmune diseases, or malignant tumors; (3) with history of other viral hepatitis, alcoholic liver disease, or primary liver cancer; (4) having excessive alcohol consumption (alcohol consumption ≥ 30 g/day in males and ≥ 20 g/day in females); (5) receiving a liver transplant within the previous year or had complications of advanced liver disease (varicose veins, ascites, etc.); (6) with drug-induced fatty hepatitis; or (7) with a history of psychiatric disorders.
After literature review, we assumed that the frequency of gene mutation in the general population was 10–30%, odds ratio (OR) was 1.5, two-sided test α was 0.05, and power of test (1-β) was 80%. Sample size was estimated by NCSS-PASS 11.0 software (Dawson edition; Kaysville, UT, United States). The sample size of 1,114 NAFLD cases and 1,909 controls in this study was large enough to guarantee the production of reliable results.
The study was performed in accordance with the World Medical Association Declaration of Helsinki on ethical principles in medical research involving human subjects and was approved by the Institutional Ethics Review Committee of Nanjing Medical University (Nanjing, China). Written informed consent was obtained before blood test and genetic analysis.
The demographic and clinical characteristics of all participants were collected from self-designed questionnaires and electronic medical records. All participants underwent abdominal ultrasound and blood biochemical tests. Five-milliliter ethylenediaminetetraacetic acid (EDTA) anticoagulant venous blood was collected from the fasting participants via the antecubital vein in the morning. The serum and blood cells in each blood sample were separated and frozen at −80°C within 2 h, until further serological tests and genotyping assays.
We searched for target SNPs with potential biological function in three candidate genes (CYP2R1, CYP24A1, and CYP27B1). The selection processes were as follows: (1) downloading the genotype databases of CYP2R1, CYP24A1, and CYP27B1 in Han Chinese in Beijing (CHB) from the 1,000 Genomes Project database1; (2) importing the genotype databases into the Haploview software (version 4.2; Broad Institute, Cambridge, MA, United States). Parameters: Hardy-Weinberg (H-W) p-Value cutoff = 0.05; minor allele frequency (MAF) = 0.05; r2 ≥ 0.8. At this point, 41 tagging SNPs (tagSNPs) were generated; (3) searching for related studies, including (I) relevant research in the Chinese population; (II) studies on NAFLD, hypertension, type 2 diabetes, hyperlipidemia, metabolic syndrome, etc. Definitively, 11 candidate SNPs (CYP2R1-rs10741657, rs12794714, rs2060793, and rs1993116; CYP24A1-rs2296241, rs2248359, rs927650, and rs6068816; and CYP27B1-rs703842, rs10877012, and rs4646536) were selected for further genotyping.
We used magnetic bead method (blood genomic extraction kit; Pangu Genome Nanotechnology Co., Ltd.; Nanjing, China) for isolating genomic DNA from EDTA-anticoagulated blood samples. Genotyping assay was performed with a TaqMan allelic discrimination assay on the Light Cycler 480 II Real-Time PCR System (Roche, Switzerland). Detailed information on primers and probes was shown in Supplementary Table 1. Some measures were implemented to control the data quality as follows: (1) blind methods were adopted in genotyping, so that all technicians were unclear about the clinical data of the participants; and (2) repeated experiments were conducted in 10% of random samples with a repeatability of 100%. Genotyping success rate of all SNPs was above 95%. All tests were carried out in accordance with the manufacturer’s instructions.
To further explore the potential functions of gene variants, we performed bioinformatics analysis using some online database as follows: (1) determining the genetic variation-specific location sites on the chromosome and transcriptional regulation information with NCBI dbSNP2; (2) viewing the scores of all genetic variation sites in the Regulome DB database,3 and SNP scoring 1–3 might act in transcriptional regulation; (3) checking whether the genetic variation sites were located on the histone modification peak through the UCSC Genome Browser database4; and (4) using the RNA fold Web Server5 to predict the effect of genetic variation of positive SNP on the secondary structure.
All data analyses were performed using IBM SPSS Statistics for Windows 23.0 (IBM Corp, Armonk, NY, United States) and R software v3.4.3.6 Distributions of demographic and clinical characteristics among case and control groups were compared by the Chi-square (χ2) test (for categorical variables), Student’s t-test, or Mann-Whitney U-test (for continuous variables). Logistic regression analysis with adjustment for gender, age, aspartate aminotransferase (AST), ALT, γ-GT, triglyceride (TG), total cholesterol (TC), and high-density lipoprotein cholesterol (HDL-C) was used to calculate odds ratio (OR) and 95% confidence interval (95% CI) for assessing the associations of genotypes with the risk of NAFLD. Each SNP was analyzed using codominant model (mutant homozygous type vs. wild type and heterozygous type vs. wild type, respectively), dominant model (mutant homozygous type + heterozygous type vs. wild type), recessive model (mutant homozygous type vs. heterozygous type + wild type), and additive models (mutant homozygous type vs. heterozygous type vs. wild type). False discovery rate (FDR) corrections were used for multiple comparisons, considering the pFDR-value ≤ 0.25 as modest confidence that the correlation represented a positive result (Woods et al., 2015). The combined effect of three independent SNPs (CYP24A1-rs2296241, CYP24A1-rs2248359, and CYP27B1-rs4646536) was analyzed using the Cochran-Armitage trend test. Subgroup analysis was performed for positive SNPs, and Q-test was performed to calculate the heterogeneity between subgroups. Multivariate stepwise logistic regression analysis was used to determine the independent predictive factors for NAFLD. A receiver-operating characteristic curve (ROC) was used to represent the risk prediction model for NAFLD, with the area under the receiver operating characteristic curve (AUROC) indicating its predictive power. A two-tailed test with a p-value < 0.05 was regarded as statistically significant in all analyses.
A total of 3,023 participants were enrolled in our study, including 1,114 NAFLD cases and 1,909 controls. The distribution of demographic and clinical characteristics in two study groups is summarized in Table 1. No significant differences were observed in age and gender between the control and NAFLD groups (all p > 0.05). However, there were significant differences in body mass index (BMI), waist circumference (WC), systolic blood pressure (SBP), diastolic blood pressure (DBP), TG, TC, HDL-C, low-density lipoprotein cholesterol (LDL-C), glucose (GLU), γ-GT, ALT, AST, direct bilirubin (DBIL), and total bilirubin (TBIL) (all p < 0.001).
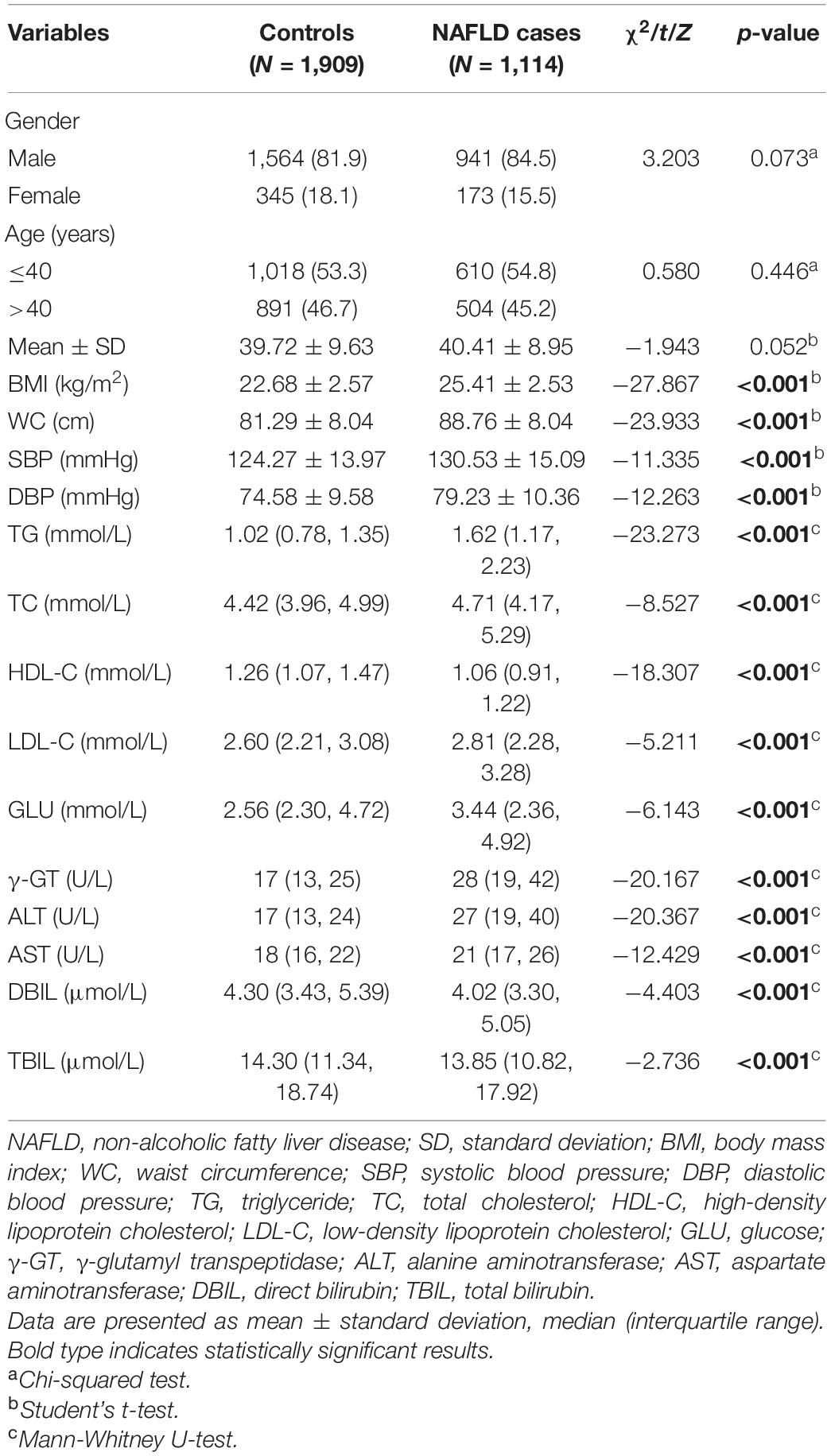
Table 1. Distributions and comparisons of demographic and clinical characteristics between NAFLD case and control groups.
The genotype distributions of the 11 SNPs between the two study groups and the results of the logistic regression analysis are shown in Table 2. After adjusting for gender, age, AST, ALT, γ-GT, TG, TC, and HDL-C, logistic regression analyses showed that CYP24A1-rs2296241-A allele (AA vs. GG: adjusted OR = 1.337, 95% CI = 1.035–1.726, p = 0.026; recessive model: adjusted OR = 1.316, 95% CI = 1.048–1.653, p = 0.018; additive model: adjusted OR = 1.135, 95% CI = 1.002–1.287, p = 0.047), CYP24A1-rs2248359-T allele (TT vs. CC: adjusted OR = 1.348, 95% CI = 1.037–1.753, p = 0.026; recessive model: adjusted OR = 1.315, 95% CI = 1.033–1.674, p = 0.026; additive model: adjusted OR = 1.137, 95% CI = 1.002–1.289, p = 00.047), and CYP27B1-rs4646536-T variant (TT vs. CC: adjusted OR = 1.359, 95% CI = 1.021–1.808, p = 0.035; additive model: adjusted OR = 1.147, 95% CI = 1.005–1.310, p = 0.042) significantly improved the risk of NAFLD. They were also significant after FDR correcting for multiple comparisons (all pFDR ≤ 0.25, Supplementary Table 1). However, no significant association was observed between CYP2R1-rs10741657, CYP2R1-rs12794714, CYP2R1-rs2060793, CYP2R1-rs1993116, CYP24A1-rs927650, CYP24A1-rs6068816, CYP27B1-rs703842, and CYP27B1-rs10877012 variants (all p > 0.05).
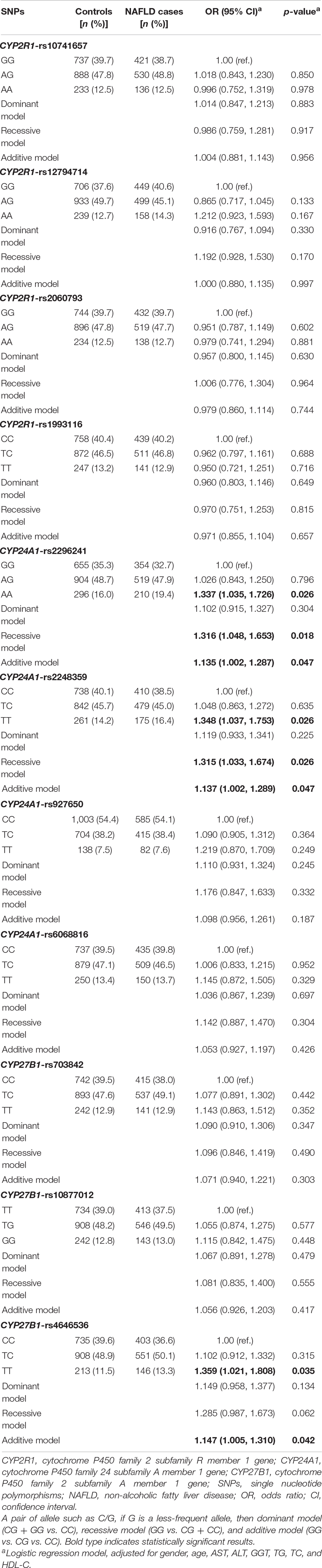
Table 2. Genotype distributions among the two study groups and association analyses of these 11 SNPs and NAFLD.
The combined effects of rs2296241-A, rs2248359-T, and rs4646536-T on susceptibility to NAFLD were evaluated by counting the number of unfavorable alleles from these three SNPs, as shown in Table 3. The results showed that NAFLD prevalence was increased in people carrying more unfavorable alleles. Compared with those who had “0” unfavorable alleles, participants with “1–3” or “4–6” unfavorable alleles had significantly increased risk of NAFLD (adjusted OR = 1.348, 95% CI = 1.016–1.788, p = 0.039; adjusted OR = 1.438, 95% CI = 1.038–1.993, p = 0.029, respectively). The more unfavorable alleles, the higher NAFLD risk, suggesting a significant locus-dosage effect of combined alleles on NAFLD risk (ptrend = 0.049). Moreover, participants carrying more than one unfavorable allele of relevant SNPs had a 36.8% higher risk of NAFLD, compared with people without an unfavorable allele (p = 0.028).
Afterward, stratified analysis was conducted to further evaluate the combined effects of rs2296241-A, rs2248359-T, and rs4646536-T (Supplementary Table 2). We found that the association between unfavorable genotypes and NAFLD risk was still significant in men (adjusted OR = 1.223, 95% CI = 1.029–1.454, p = 00.022), γ-GT ≤ 50 U/L (adjusted OR = 1.189, 95% CI = 1.007–1.404, p = 0.042), non-low HDL-C (adjusted OR = 1.287, 95% CI = 1.058–1.565, p = 0.012). Moreover, heterogeneity test discovered no statistical significance in all the subgroups (all p > 0.05).
A stepwise regression model was established comprising gender, age, visceral obesity, ALT, γ-GT, hypertriglyceridemia, hypertension, low HDL-C, hyperglycemia, and combined unfavorable alleles (CYP24A1 rs2296241-A, CYP24A1 rs2248359-T, and CYP27B1 rs4646536-T). The result showed that age (OR = 0.785, 95% CI = 0.646–0.954, p = 0.015), visceral obesity (OR = 4.400, 95% CI = 3.511–5.515, p < 0.001), ALT (OR = 2.240, 95% CI = 1.689–2.970, p < 0.001), γ-GT (OR = 1.414, 95% CI = 1.031–1.938, p = 0.031), hypertriglyceridemia (OR = 3.497, 95% CI = 2.806–4.360, p < 0.001), hypertension (OR = 1.723, 95% CI = 1.374–2.160, p < 0.001), low HDL-C (OR = 1.722, 95% CI = 1.404–2.111, p < 0.001), hyperglycemia (OR = 1.515, 95% CI = 1.016–2.260, p = 0.042), and unfavorable alleles (OR = 1.459, 95% CI = 1.093–1.948, p = 0.010) were independent influencing predictors of NAFLD in Table 4. Subsequently, we constructed a combined factor model based on the above nine variables for assessing NAFLD risk. The combined model achieved an AUROC of 0.789 (95% CI = 0.773–0.805) (Figure 1). At a cutoff value of −0.85, the sensitivity and specificity of this novel model were 69.6% (66.7–72.4) and 78.1% (76.0–80.0), respectively. The positive likelihood ratio and negative likelihood ratio were 3.18 and 0.39, respectively.
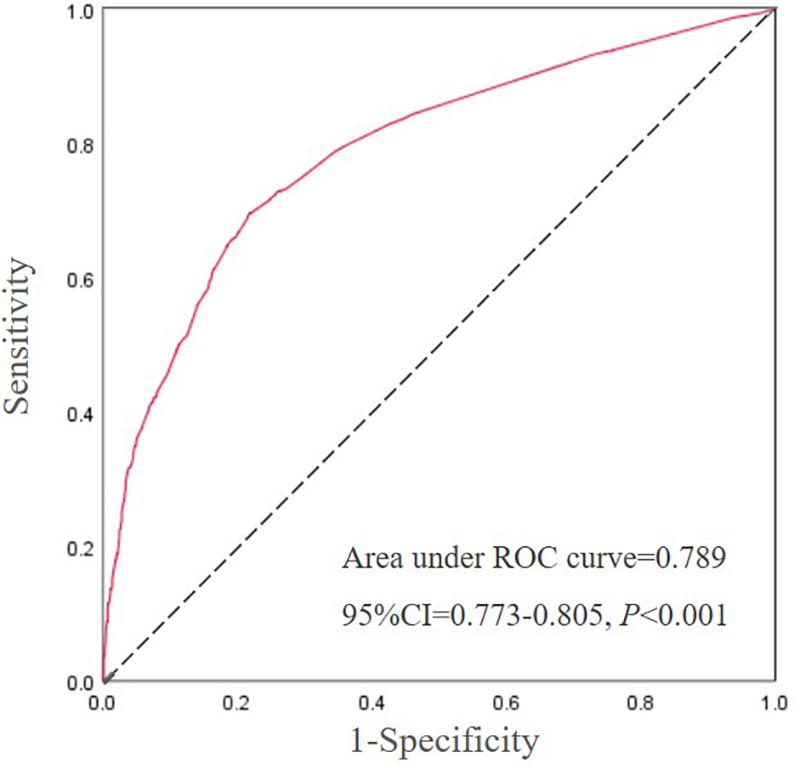
Figure 1. The ROC curve for the influence factors of Table 4. Abbreviations: NAFLD, non-alcoholic fatty liver disease; AUROC, area under the receiver operating curve. The response variable is NAFLD risk and the diagnostic test variable is a combination of age, visceral obesity, ALT, γ-GT, hypertriglyceridemia, hypertension, low HDL-C, hyperglycemia, and unfavorable alleles with the coefficients taken from the regression analysis.
The Regulome DB score for the CYP24A1-rs2296241, CYP24A1-rs2248359, and CYP27B1-rs4646536 were 4, 4, and 1d, respectively.7 The UCSC prediction showed that rs2296241, rs2248359, and rs4646536 were all enriched near the H3K4Me1 marker (Figure 2). The effect of rs2296241, rs2248359, and rs4646536 predicted by RNA fold Web Server on the secondary structure of CYP24A1 and CYP27B1 mRNA is shown in Figure 2. The arrows indicated the position of the mutation (50 bases upstream and 50 bases downstream of the mutation). The minimum free energy (MFE) of G and A alleles of CYP24A1-rs2296241 were estimated at −10.9 and −7.5 kcal/mol, respectively. The MFE of C and T alleles of CYP24A1-rs2248359 were estimated at −21.5 and −18.6 kcal/mol, respectively. The MFE of A and T alleles of CYP27B1-rs4646536 were all estimated at −30.5 kcal/mol.
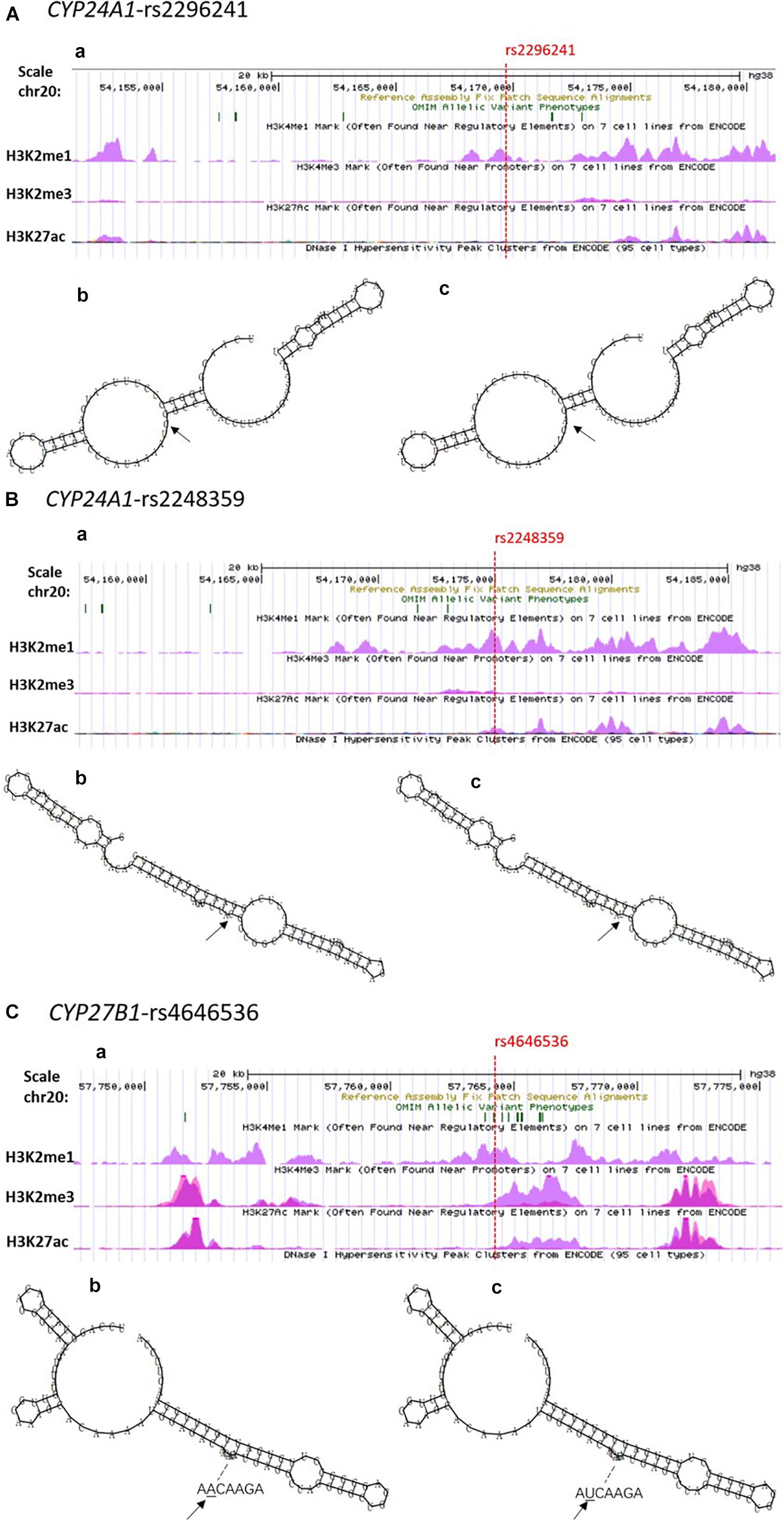
Figure 2. Functional prediction of positive SNPs in CYP24A1 and CYP27B1. Notes. (A) CYP24A1-rs2296241; (B) CYP24A1-rs2248359; (C) CYP27B1-rs4646536. (a) USCS functional annotations of SNPs, respectively. The red dotted line indicated the position of target SNPs (available at http://genome.ucsc.edu/). (b,c) Influence of SNPs on the mRNA secondary structures. (b) Wild-type sequence; (c) mutant-type sequence. The arrows indicate the position of the mutation (50 bases upstream and 50 bases downstream of the mutation). The minimum free energies (MFE) for the G and A allele of rs2296241 were estimated at −10.9 and −7.5 kcal/mol, respectively. The MFE for the C and T allele of rs2248359 were estimated at −21.5 and −18.6 kcal/mol, respectively. The MFE for the A and T alleles of rs4646536 were all estimated at −30.5 kcal/mol by RNA fold Wed Server.
In this case-control study, we explored the associations of vitamin D family genes CYP2R1, CYP24A1, and CYP27B1 genetic polymorphism with the risk of NAFLD among Chinese Hans. Our result showed that CYP24A1 rs2296241-A, rs2248359-T, and CYP27B1 rs4646536-T as unfavorable alleles were associated with the increased risk of NAFLD. The combination of clinical factors and unfavorable alleles exhibited a desirable predictive value for the risk of NAFLD.
NAFLD is a complex metabolic disorder closely associated with obesity, T2DM, and metabolic syndrome (Younossi, 2019). Vitamin D is a pleiotropic hormone definitively involved in immune-inflammatory and metabolic processes (Charoenngam and Holick, 2020). Accumulative previous studies have suggested vitamin D deficiency highly prevalent among the general Asian population (Cheng et al., 2017; Cho et al., 2019). Several recent meta-analyses have suggested that low vitamin D level may impact disease progression of NAFLD, while in chronic liver diseases, enzymatic conversion (hydroxylation) is disrupted in the liver through a variety of mechanisms, leading to low serum vitamin D levels (Zhu and DeLuca, 2012; Zhang et al., 2019; Liu et al., 2020). SNPs in genes involved in the vitamin D metabolic process could affect vitamin D status. The associations of CYP2R1, CYP24A1, and CYP27B1 gene polymorphisms with vitamin D deficiency in multiple population have been reported (Gibson et al., 2018; Arai et al., 2019). In this study, we genotyped three target genes (CYP2R1, CYP24A1, and CYP27B1) encoding hydroxylase in the vitamin D metabolic pathway. No relationship was found between CYP2R1 and NAFLD. Similar negative results were found in previous studies among different populations (Gibson et al., 2018). However, positive results have shown that genetic variants of CYP24A1 and CYP27B1 can increase the risk of NAFLD. To our knowledge, this is the first study revealing a relationship between CYP24A1 and CYP27B1 SNPs and NAFLD risk.
Although no studies have shown a relationship between the polymorphisms of CYP24A1, CYP27B1, and NAFLD, these variants have been extensively investigated in other diseases, such as organ-specific autoimmune endocrine diseases (Ma et al., 2020), CVD (Qian et al., 2020), metabolic diseases (Yu et al., 2020), and multiple cancers (Hibler et al., 2015; Torkko et al., 2020). Our results also confirmed that NAFLD patients with a combined load of unfavorable alleles (rs2296241-A, rs2248359-T, and rs4646536-T) exhibited an association with the increase in NAFLD risk, and this association was also in a dose-dependent manner. These findings would provide useful information of risk assessment or possible diagnostic markers for NAFLD.
In the model of combined unfavorable alleles with other clinical factors (binary age, visceral obesity, ALT, γ-GT, hypertriglyceridemia, hypertension, low HDL-C, hyperglycemia), gender was not significant, but the remaining nine were independent risk factors of NAFLD. These results are almost consistent with NAFLD guidelines and some previous studies. Abnormal ALT and γ-GT levels, hypertriglyceridemia, hypertension, low HDL-C levels, and hyperglycemia have been recognized as predictors of metabolic syndrome (National Workshop on Fatty Liver and Alcoholic Liver Disease, Chinese Society of Hepatology, Association et al., 2018). Age and BMI are established predictors of liver fibrosis and have been included in the NAFLD fibrosis score formula (Angulo et al., 2007). WC and γ-GT are included in the non-invasive model Fatty Liver Index (FLI) for risk prediction of NAFLD (Bedogni et al., 2006). Moreover, the AUROC of our model combining the above nine variables was 0.789, indicating that it had a desirable predictive value. Given its potential predictive value, the predictive model combining clinical and genetic factors might provide new avenue for early screening in high-risk population. Cost-benefit analysis should be considered in future studies.
In this study, we used multiple bioinformatics databases to predict the function of positive SNPs. The Regulome DB score for the CYP24A1-rs2296241, CYP24A1-rs2248359, and CYP27B1-rs4646536 were 4, 4, and 1 days, respectively, which indicated that these loci have strong potential functions, regulate the expression of CYP24A1 and CYP27B1 by changing multiple regulatory motifs, and interfere with protein-binding activity (Boyle et al., 2012). The performances of UCSC showed that rs2296241, rs2248359, and rs4646536 were involved in promoter and enhancer modification in different cell lines, especially in the vicinity of enhancer elements (H3K2me1 marker) of multiple cell lines. Moreover, they were also related to the change of transcription factor-binding module. In addition, the MFEs of rs2296241 G and A alleles (−10.9 vs. −7.5 kcal/mol) and rs2248359 C and T alleles (−21.5 vs. −18.6 kcal/mol) were different, suggesting that mutation of rs2296241 and rs2248359 may affect the transcription of CYP24A1. Further research is warranted to identify the function of these polymorphisms in vitamin D metabolic pathway.
Several potential limitations need to be considered. Firstly, this is a single-center study, and population selection is under-represented. In response, gender and age were matched in the design stage, and multivariate analysis and stratified analysis were carried out to control the influence of the confounding factors. Secondly, we only chose three hydroxylase genes in the vitamin D metabolic pathway, which may not fully analyze the relationship between genetic variants and NAFLD risk. More genetic loci are needed to confirm the effect of genetic variation on the risk of NAFLD. It is necessary to further explore the impact of polygenic loci and their combination with other environmental factors on NAFLD risk in a multicenter population of different races.
CYP24A1 (rs2296241, rs2248359) and CYP27B1 (rs4646536) variants are associated with a high risk of NAFLD in the Chinese Han population. The combination of unfavorable SNPs and metabolic-related indicators shows high efficiency in predicting the risk of NAFLD. These findings might provide new insight into NAFLD pathogenesis and a new tool for early screening of high-risk population.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by the Institutional Ethics Review Committee of Nanjing Medical University (Nanjing, China). The patients/participants provided their written informed consent to participate in this study.
JW designed and organized the study. MXW, RZ, MW, LZ, YD, ZT, HLW, WZ, and YC contributed to the planning, designing, and analyses of the data collection and quality control. MW, RZ, MW, LZ, YD, and ZT performed data reduction and statistical analysis. HLW and WZ provided materials and analysis tools. MXW, RZ, and JW wrote and critically revised the manuscript. All authors read and approved the final manuscript.
This work was supported by the Natural Science Foundation of Jiangsu Province, China (Grant No. BK20181369), the Priority Academic Program Development of Jiangsu Higher Education Institutions [Grant No. PAPD (2018) 87], and the Six Talent Peaks project in Jiangsu Province, China (Grant No. 2019-WSN-049).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We thank all the students, doctors, and nurses who participated in this work.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgene.2021.717533/full#supplementary-material
Angulo, P., Hui, J. M., Marchesini, G., Bugianesi, E., George, J., Farrell, G. C., et al. (2007). The NAFLD fibrosis score: a noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology 45, 846–854. doi: 10.1002/hep.21496
Arai, T., Atsukawa, M., Tsubota, A., Koeda, M., Yoshida, Y., Okubo, T., et al. (2019). Association of vitamin D levels and vitamin D-related gene polymorphisms with liver fibrosis in patients with biopsy-proven nonalcoholic fatty liver disease. Dig. Liver Dis. 51, 1036–1042. doi: 10.1016/j.dld.2018.12.022
Bedogni, G., Bellentani, S., Miglioli, L., Masutti, F., Passalacqua, M., Castiglione, A., et al. (2006). The fatty liver index: a simple and accurate predictor of hepatic steatosis in the general population. BMC Gastroenterol. 6:33. doi: 10.1186/1471-230X-6-33
Borel, P., Caillaud, D., and Cano, N. J. (2015). Vitamin D bioavailability: state of the art. Crit. Rev. Food Sci. Nutr. 55, 1193–1205. doi: 10.1080/10408398.2012.688897
Boyle, A. P., Hong, E. L., Hariharan, M., Cheng, Y., Schaub, M. A., Kasowski, M., et al. (2012). Annotation of functional variation in personal genomes using RegulomeDB. Genome Res. 22, 1790–1797. doi: 10.1101/gr.137323.112
Braithwaite, V. S., Jones, K. S., Schoenmakers, I., Silver, M., Prentice, A., and Hennig, B. J. (2015). Vitamin D binding protein genotype is associated with plasma 25OHD concentration in West African children. Bone 74, 166–170. doi: 10.1016/j.bone.2014.12.068
Buzzetti, E., Pinzani, M., and Tsochatzis, E. A. (2016). The multiple-hit pathogenesis of non-alcoholic fatty liver disease (NAFLD). Metabolism 65, 1038–1048. doi: 10.1016/j.metabol.2015.12.012
Byrne, C. D., and Targher, G. (2020). NAFLD as a driver of chronic kidney disease. J. Hepatol. 72, 785–801. doi: 10.1016/j.jhep.2020.01.013
Charoenngam, N., and Holick, M. F. (2020). Immunologic effects of vitamin D on human health and disease. Nutrients 12:2097. doi: 10.3390/nu12072097
Cheng, Q., Du, Y., Hong, W., Tang, W., Li, H., Chen, M., et al. (2017). Factors associated to serum 25-hydroxyvitamin D levels among older adult populations in urban and suburban communities in Shanghai, China. BMC Geriatr. 17:246. doi: 10.1186/s12877-017-0632-z
Cho, Y. H., Kim, J. W., Shim, J. O., Yang, H. R., Chang, J. Y., Moon, J. S., et al. (2019). Association between vitamin D deficiency and suspected nonalcoholic fatty liver disease in an adolescent population. Pediatr. Gastroenterol. Hepatol. Nutr. 22, 233–241. doi: 10.5223/pghn.2019.22.3.233
Cimini, F. A., Barchetta, I., Carotti, S., Bertoccini, L., Baroni, M. G., Vespasiani-Gentilucci, U., et al. (2017). Relationship between adipose tissue dysfunction, vitamin D deficiency and the pathogenesis of non-alcoholic fatty liver disease. World J. Gastroenterol. 23, 3407–3417. doi: 10.3748/wjg.v23.i19.3407
Dastani, Z., Li, R., and Richards, B. (2013). Genetic regulation of vitamin D levels. Calcif. Tissue Int. 92, 106–117. doi: 10.1007/s00223-012-9660-z
Dawson-Hughes, B., Staten, M. A., Knowler, W. C., Nelson, J., Vickery, E. M., LeBlanc, E. S., et al. (2020). Intratrial exposure to vitamin D and new-onset diabetes among adults with prediabetes: a secondary analysis from the vitamin D and type 2 diabetes (D2d) study. Diabetes Care 43, 2916–2922. doi: 10.2337/dc20-1765
Eslam, M., and George, J. (2016). Genetic and epigenetic mechanisms of NASH. Hepatol. Int. 10, 394–406. doi: 10.1007/s12072-015-9689-y
Eslam, M., Sanyal, A. J., and George, J. (2020). International consensus panel. MAFLD: a consensus-driven proposed nomenclature for metabolic associated fatty liver disease. Gastroenterology 158, 1999–2014.e1.
Gandini, S., Boniol, M., Haukka, J., Byrnes, G., Cox, B., Sneyd, M. J., et al. (2011). Meta-analysis of observational studies of serum 25-hydroxyvitamin D levels and colorectal, breast and prostate cancer and colorectal adenoma. Int. J. Cancer 128, 1414–1424. doi: 10.1002/ijc.25439
Gibson, P. S., Quaglia, A., Dhawan, A., Wu, H., Lanham-New, S., Hart, K. H., et al. (2018). Vitamin D status and associated genetic polymorphisms in a cohort of UK children with non-alcoholic fatty liver disease. Pediatr. Obes. 13, 433–441. doi: 10.1111/ijpo.12293
Hibler, E. A., Klimentidis, Y. C., Jurutka, P. W., Kohler, L. N., Lance, P., Roe, D. J., et al. (2015). CYP24A1 and CYP27B1 polymorphisms, concentrations of vitamin D metabolites, and odds of colorectal adenoma recurrence. Nutr. Cancer 67, 1131–1141. doi: 10.1080/01635581.2015.1068818
Höbaus, J., Thiem, U., Hummel, D. M., and Kallay, E. (2013). Role of calcium, vitamin D, and the extrarenal vitamin D hydroxylases in carcinogenesis. Anticancer Agents Med. Chem. 13, 20–35. doi: 10.2174/1871520611307010020
Italian Association for the Study of the Liver (Aisf) (2017). AISF position paper on nonalcoholic fatty liver disease (NAFLD): updates and future directions. Dig. Liver Dis. 49, 471–483. doi: 10.1016/j.dld.2017.01.147
Jolliffe, D. A., Walton, R. T., Griffiths, C. J., and Martineau, A. R. (2016). Single nucleotide polymorphisms in the vitamin D pathway associating with circulating concentrations of vitamin D metabolites and non-skeletal health outcomes: review of genetic association studies. J. Steroid Biochem. Mol. Biol. 164, 18–29. doi: 10.1016/j.jsbmb.2015.12.007
Jung, M. K., and Shin, E. C. (2016). Regulatory T cells in Hepatitis B and C virus infections. Immune Netw. 16, 330–336. doi: 10.4110/in.2016.16.6.330
Lindenmeyer, C. C., and McCullough, A. J. (2018). The natural history of nonalcoholic fatty liver disease-an evolving view. Clin. Liver Dis. 22, 11–21. doi: 10.1016/j.cld.2017.08.003
Liu, T., Xu, L., Chen, F. H., and Zhou, Y. B. (2020). Association of serum vitamin D level and nonalcoholic fatty liver disease: a meta-analysis. Eur. J. Gastroenterol. Hepatol. 32, 140–147. doi: 10.1097/meg.0000000000001486
Ma, X., Xie, Z., Qin, J., Luo, S., and Zhou, Z. (2020). Association of vitamin D pathway gene CYP27B1 and CYP2R1 polymorphisms with autoimmune endocrine disorders: a meta-analysis. J. Clin. Endocrinol. Metab. 105:dgaa 525.
National Workshop on Fatty Liver and Alcoholic Liver Disease, Chinese Society of Hepatology, Association, C. M. Fatty Liver Expert Committee, and Chinese Medical Doctor Association (2018). Guidelines of prevention and treatment for alcoholic liver disease: a 2018 update. Zhonghua Gan Zang Bing Za Zhi 26, 188–194.
Qian, P., Cao, X., Xu, X., Duan, M., Zhang, Q., and Huang, G. (2020). Contribution of CYP24A1 variants in coronary heart disease among the Chinese population. Lipids Health Dis. 19:181.
Reid, I. R., Bolland, M. J., and Grey, A. (2014). Effects of vitamin D supplements on bone mineral density: a systematic review and meta-analysis. Lancet 383, 146–155. doi: 10.1016/s0140-6736(13)61647-5
Szymczak-Pajor, I., Drzewoski, J., and Śliwińska, A. (2020). The molecular mechanisms by which vitamin d prevents insulin resistance and associated disorders. Int. J. Mol. Sci. 21:6644. doi: 10.3390/ijms21186644
Tarantino, G., Citro, V., and Capone, D. (2019). Nonalcoholic fatty liver disease: a challenge from mechanisms to therapy. J. Clin. Med. 9:15. doi: 10.3390/jcm9010015
Targher, G., Day, C. P., and Bonora, E. (2010). Risk of cardiovascular disease in patients with nonalcoholic fatty liver disease. N. Engl. J. Med. 363, 1341–1350.
Thacher, T. D., and Levine, M. A. (2017). CYP2R1 mutations causing vitamin D-deficiency rickets. J. Steroid Biochem. Mol. Biol. 173, 333–336. doi: 10.1016/j.jsbmb.2016.07.014
Tilg, H., Moschen, A. R., and Roden, M. (2017). NAFLD and diabetes mellitus. Nat. Rev. Gastroenterol. Hepatol. 14, 32–42.
Torkko, K., Till, C., Tangen, C. M., Goodman, P. J., Song, X., Schenk, J. M., et al. (2020). Vitamin D pathway and other related polymorphisms and risk of prostate cancer: results from the prostate cancer prevention trial. Cancer Prev. Res. (Phila) 13, 521–530. doi: 10.1158/1940-6207.capr-19-0413
Visscher, P. M., Brown, M. A., McCarthy, M. I., and Yang, J. (2012). Five years of GWAS discovery. Am. J. Hum. Genet. 90, 7–24. doi: 10.1016/j.ajhg.2011.11.029
Wang, T. J., Zhang, F., Richards, J. B., Kestenbaum, B., van Meurs, J. B., Berry, D., et al. (2010). Common genetic determinants of vitamin D insufficiency: a genome-wide association study. Lancet 376, 180–188.
Woods, N. T., Monteiro, A. N., Thompson, Z. J., Amankwah, E. K., Naas, N., Haura, E. B., et al. (2015). Interleukin polymorphisms associated with overall survival, disease-free survival, and recurrence in non-small cell lung cancer patients. Mol. Carcinog. 54(Suppl. 1) E172–E184.
Younossi, Z. M. (2019). Non-alcoholic fatty liver disease–a global public health perspective. J. Hepatol. 70, 531–544. doi: 10.1016/j.jhep.2018.10.033
Younossi, Z. M., Koenig, A. B., Abdelatif, D., Fazel, Y., Henry, L., and Wymer, M. (2016). Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 64, 73–84. doi: 10.1002/hep.28431
Yu, S., Feng, Y., Qu, C., Huo, W., Mao, Z., Wang, C., et al. (2020). CYP27B1 as an instrument gene to investigate the causal relationship between vitamin D deficiency and obesity: a family-based study. Eur. J. Clin. Nutr. 74, 806–810. doi: 10.1038/s41430-020-0594-7
Zhang, Z., Thorne, J. L., and Moore, J. B. (2019). Vitamin D and nonalcoholic fatty liver disease. Curr. Opin. Clin. Nutr. Metab. Care 22, 449–458.
Keywords: non-alcoholic fatty liver disease, cytochrome P450 family 24 subfamily A member 1 gene, cytochrome P450 family 27 subfamily B member 1 gene, polymorphism, risk
Citation: Wang M, Zhang R, Wang M, Zhang L, Ding Y, Tang Z, Wang H, Zhang W, Chen Y and Wang J (2021) Genetic Polymorphism of Vitamin D Family Genes CYP2R1, CYP24A1, and CYP27B1 Are Associated With a High Risk of Non-alcoholic Fatty Liver Disease: A Case-Control Study. Front. Genet. 12:717533. doi: 10.3389/fgene.2021.717533
Received: 31 May 2021; Accepted: 13 July 2021;
Published: 16 August 2021.
Edited by:
Gary T. Hardiman, Queen’s University Belfast, United KingdomReviewed by:
Giovanni Tarantino, University of Naples Federico II, ItalyCopyright © 2021 Wang, Zhang, Wang, Zhang, Ding, Tang, Wang, Zhang, Chen and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jie Wang, d2FuZ2ppZW5qbXVAMTI2LmNvbQ==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.