- 1Department of Neurology, Xiangya Hospital, Central South University, Changsha, China
- 2Hunan Provincial Key Laboratory of Medical Genetics, School of Life Sciences, Central South University, Changsha, China
- 3Key Laboratory of Hunan Province in Neurodegenerative Disorders, Central South University, Changsha, China
- 4National Clinical Research Center for Geriatric Diseases, Changsha, China
- 5Key Laboratory of Organ Injury, Aging and Regenerative Medicine of Hunan Province, Changsha, China
- 6Department of Geriatrics Neurology, Xiangya Hospital, Central South University, Changsha, China
- 7Department of Orthopedics, Xiangya Hospital, Central South University, Changsha, China
Background: Vitamin D insufficiency has been considered a risk factor for Alzheimer's disease (AD) in several studies. Recently, four single-nucleotide polymorphisms (SNPs) to be genome-wide significant for 25-hydroxyvitamin D [25(OH)D] were identified to have an association with the risk of AD. These include GC rs2282679 A>C, CYP2R1 rs10741657 T>C, DHCR7 rs12785878 T>C, and CYP24A1 rs6013897 T>A. However, the association between these polymorphisms and AD susceptibility in the Chinese population remains unclear.
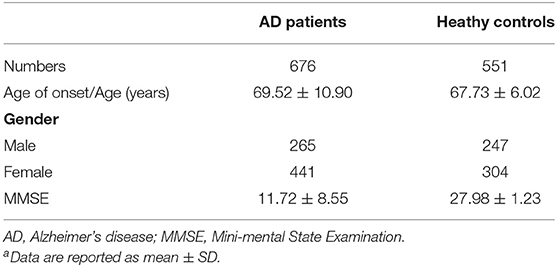
Methods: A case-control cohort study was conducted in 676 AD patients (mean age at onset was 69.52 ± 10.90 years, male: 39.2%) and 551 healthy controls (mean age was 67.73 ± 6.02 years, male: 44.8%). Genotyping was determined by PCR and SNaPshot sequencing. To determine whether the four SNPs account for risks in AD in Chinese population, multivariate logistic regression models were performed. Stratified analysis was performed based on gender and age of onset of AD, separately. Statistical significance was set at 0.0125 (0.05/4) based on Bonferroni correction.
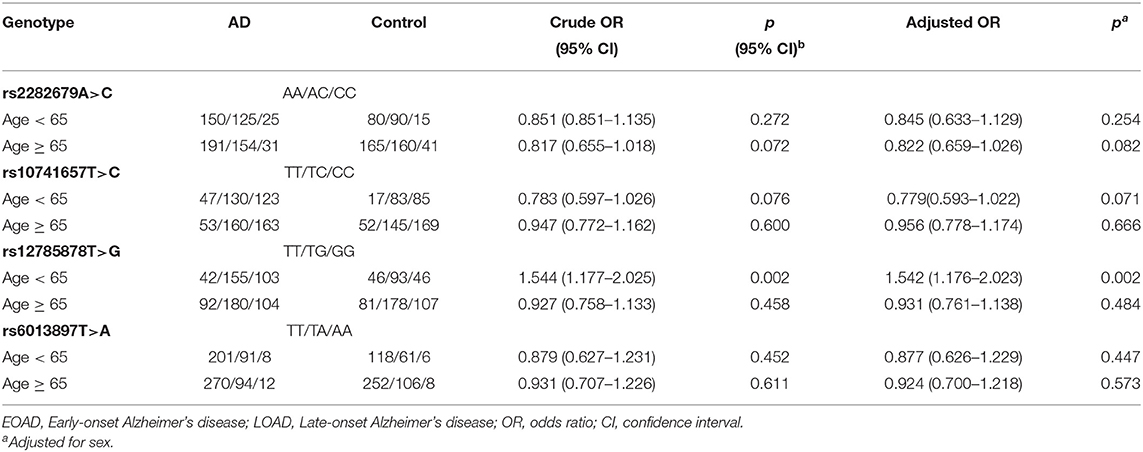
Findings: DHCR7 rs12785878 T>C was found to be significantly associated with an increased risk of early-onset Alzheimer's disease (EOAD) (n = 300, risk allele C, adjusted OR = 1.542, adjusted 95% CI = 1.176–2.023, p = 0.002). There was no statistical significance of the other three SNPs between the two groups.
Interpretation: Our results suggested that DHCR7 rs12785878 T>C might be associated with an increased risk of EOAD in the Chinese population, while other polymorphisms related to vitamin D insufficiency might not be. However, due to the limited data in this study, replication studies in a larger sample are required.
Introduction
Vitamin D, a steroid hormone, is crucial for maintaining musculoskeletal health and mineral metabolism. Its insufficiency has been linked to several skeletal or extra-skeletal disorders, including bone fracture, osteoporosis, diabetes, cancer, and cardiovascular disease (Martinez et al., 1996; Wang et al., 2008; Zipitis and Akobeng, 2008; Rizzoli et al., 2014). Recently, large-scale cohort studies and cross-sectional studies suggested that a decreased 25-hydroxyvitamin D [25(OH)D] level is associated with an increased risk of Alzheimer's disease (AD) (Balion et al., 2012; Afzal et al., 2014; Littlejohns et al., 2014). AD is the most common neurodegenerative disease characterized by progressive impairments in cognition, memory, language, behavior, and motor functions (Reitz et al., 2011). The pathogenetic hallmarks of AD are cerebral extracellular amyloid plaques and intracellular neurofibrillary tangles followed by oxidative damage and inflammation, leading to localized synaptic failure, and neuronal loss (Querfurth and LaFerla, 2010). Vitamin D status has shown links with AD tightly. Several longitudinal studies have observed an association of reduced plasma 25(OH)D with an increased risk of AD (Afzal et al., 2014; Littlejohns et al., 2014). Other researchers found vitamin D supplementation could improve cognitive function in elderly patients with AD (Chaves et al., 2014; Jia et al., 2019). It has been proved that vitamin D increases the phagocytic clearance of amyloid plaques and reduces amyloid-induced cytotoxicity and apoptosis (Masoumi et al., 2009; Dursun et al., 2011; Mizwicki et al., 2012). Furthermore, the hormonally active form of vitamin D−1,25-dihydroxy vitamin D [1,25-(OH)2-vitD]—has been shown to improve intracellular Ca2+ homeostasis dysregulated in AD (Brewer et al., 2001, 2006; Gezen-Ak et al., 2011) and to upregulate neurotrophic factors (Saporito et al., 1994; Musiol and Feldman, 1997; Gezen-Ak et al., 2011).
However, reverse causation may also exist, as the onset of dementia may limit outdoor physical activity, reduce actual sunlight exposure of patients, and subsequently cause vitamin D deficiency. Therefore, some confounding factors may influence the accuracy of the results. In some studies, the researchers used Mendelian randomization (MR), a method that minimizes bias due to confounding or reverse causation (Smith and Ebrahim, 2003), to assess the contribution of 25(OH)D in the occurrence of AD (Mokry et al., 2016). They found four single-nucleotide polymorphisms (SNPs) related to vitamin D insufficiency [described 2.44% of the variance in 25(OH)D], including GC rs2282679 A>C, CYP2R1 rs10741657 T>C, DHCR7 rs12785878 T>C, and CYP24A1 rs6013897 T>A, were associated with an increased risk of developing AD [data from International Genomics of Alzheimer's Project (IGAP)] (Wang et al., 2010; Lambert et al., 2013), and all these four SNPs together can increase the odds of AD by 25%. This result provides evidence supporting the decrease of 25(OH)D as a causal risk factor for AD. To further test whether these SNPs associated with vitamin D insufficiency increase the risk of AD in the Chinese population, we conducted a case-control study to investigate the possible association between these four SNPs and AD in a Chinese cohort.
Materials and Methods
Participants
This study recruited 676 AD patients (mean age at onset was 69.52 ± 10.90 years, male: 39.2%) from mainland China. The diagnoses of probable or possible AD according to the NINCDS-ADRDA criteria (Dubois et al., 2007) were made by two or more experienced neurologists in Xiangya Hospital, Central South University. Early-onset Alzheimer's disease (EOAD) was defined as AD with an age at onset <65 years (300 subjects). Late-onset Alzheimer's disease (LOAD) was defined as AD with an age at onset more than 65 years (376 subjects). Five hundred and fifty-one healthy unrelated Chinese individuals (mean age was 67.73 ± 6.02 years, male: 44.8%) without a history of neurodegenerative diseases were recruited from the Xiangya Wellness Center as a control group. Neurocognitive assessment was performed on all AD patients, including Mini-Mental State Examination (MMSE), Clinical Dementia Rating Scale (CDR), and Activity of Daily Living Scale (ADL). MMSE was also conducted with healthy controls in this study. Informed consent for participation in the study was obtained from all subjects. This study was approved by the Ethical Review Board at Xiangya Hospital of Central South University in China.
DNA Isolation and Genotyping Methods
Genomic DNA was extracted from peripheral blood leukocytes from all patients and controls. The quality and quantity of DNA were assessed with a fluorometer. The genotype was detected by SNaPshot, a single-base extension (SBE) assay, using ABI SNaPshot Multiplex Kit and 3730xl DNA analyzer (Applied Biosystems). Positive controls and negative controls are set for each sequencing test. All sequencing results are interpreted by two researchers using Peak Scanner-V2.0 software separately. For quality control, we randomly selected about 5% of all samples for Sanger sequencing testing, and the coincidence rate was 100%. Primers and amplification conditions required in polymerase chain reaction (PCR) are listed in Supplementary Tables 1, 2.
Statistical Analysis
The chi-squared test was used to test for the Hardy–Weinberg equilibrium (HWE) of the genotypes. A p-value < 0.05 using a two-tailed test was considered statistically significant. To estimate the strength of the association between the SNPs and AD risk, multivariate logistic regression models with gender and age as covariates were performed, and the correlation strength was presented with odds ratio (OR) and 95% confidence interval (CI). For statistical significance in the association analysis, we used the Bonferroni correction to adjust the p-value from 0.05 to (0.05 / k), where k is the number of SNPs tested in each independent association test (k = 4 in our study). Therefore, a p-value of < 0.0125 demonstrates a significant association in statistics. Stratified analysis was performed based on gender and age of onset of AD, separately. Statistical analysis was carried out using SPSS26.0 software.
Results
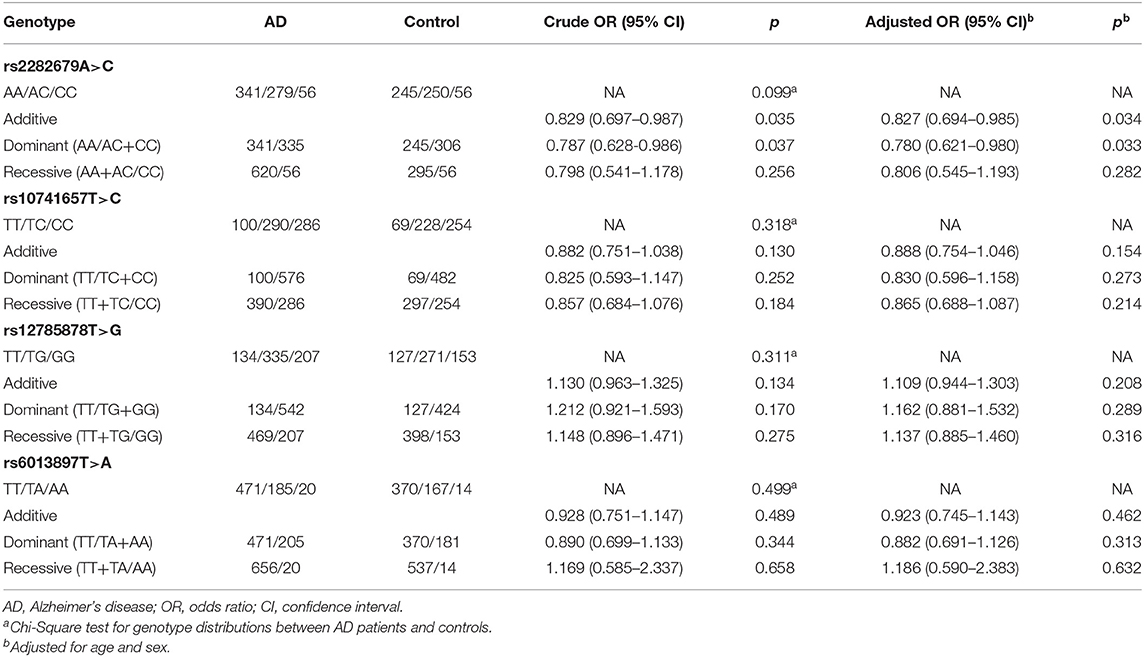
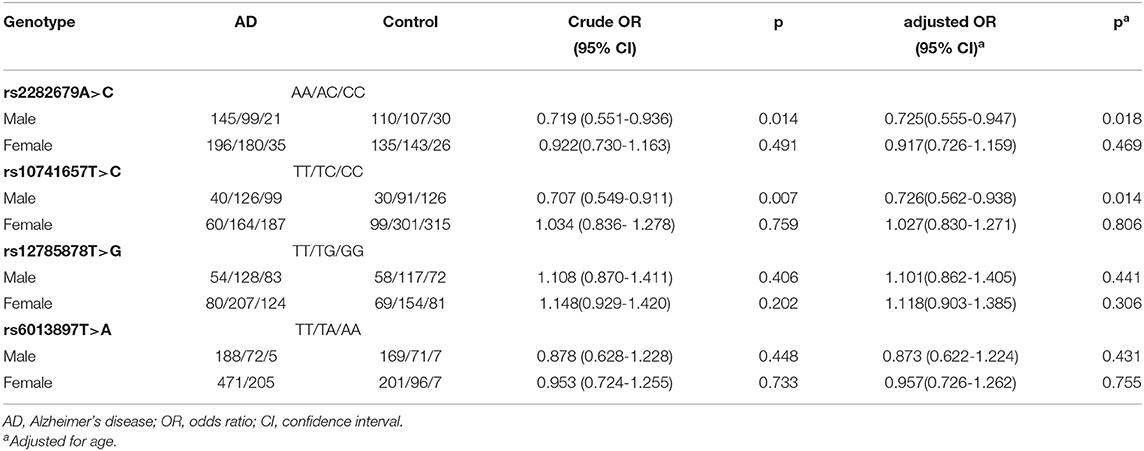
The basic information of all 1,127 subjects (676 patients and 551 healthy controls) are shown in Table 1. The genotype frequencies of the four SNPs in all controls followed HWE (p > 0.05). There was no statistical significance of these four SNPs in genotype or allele frequencies between the two groups (Table 2). Stratification analysis showed CYP2R1 rs10741657 T>C was associated with decreased risk of male AD patients (p = 0.007, OR = 0.707); however, after being adjusted for age, the adjusted p-value was > 0.0125 (Table 3). We also found DHCR7 rs12785878 T>C to be significantly associated with an increased risk of EOAD (p = 0.002, OR = 1.544, 95% CI = 1.177–2.025) (Table 4), and after being adjusted for sex, the difference was still significant (p = 0.002, adjusted OR = 1.542, adjusted 95% CI = 1.176–2.023).
Discussion
In this study, we investigated the association of SNPs related to vitamin D insufficiency and the risk of AD in a cohort of Chinese subjects with AD and healthy controls. No statistically significant differences were observed in these SNPs between cases and controls. However, stratification analysis found the DHCR7 rs12785878 T>C involved in the synthesis of vitamin D to be associated with the risk of EOAD, providing supporting evidence for the association between vitamin D insufficiency and EOAD.
Despite the detailed information about molecular pathogenic events that research has provided, little is known about the cause of AD, and no curative treatments are available. Many factors could be involved in the incidence of AD, like vitamin D insufficiency, which previous studies have found to be associated with an increased risk of AD. This is an important discovery since vitamin D repletion can be achieved safely and inexpensively through supplementation, which might reduce the occurrence of AD. However, whether vitamin D insufficiency is the cause or the result of AD remains unclear. One of the main reasons is that observational studies are susceptible to confounding factors. For example, the actual sunlight exposure of patients could not be measured accurately, and their lifestyle changes over time. Genetic background can be an entry point to solve this issue since it's not affected by factors like behavior and lifestyle that may confound observational studies.
The four SNPs associated with vitamin D insufficiency were confirmed to be related to the risk of AD, and all of these four SNPs map to genes within the vitamin D metabolic pathway (Mokry et al., 2016). GC rs2282679 A>C and CYP24A1 rs6013897 T>A are associated with the metabolism of vitamin D, while DHCR7 rs12785878 T>C and CYP2R1 rs10741657 T>C are related to the synthesis of vitamin D. Additionally, GC rs2282679 A>C and DHCR7 rs12785878 T>C may also have pleiotropic effects. GC encodes vitamin D-binding protein (DBP), and it is responsible for transporting most of 25(OH)D in the body (Bikle et al., 1985; White and Cooke, 2000; Verboven et al., 2002). The level of DBP has been found to increase in cerebrospinal fluid in AD patients (Zhang et al., 2008), and it can also interact with Aβ and suppress Aβ-mediated pathology (Moon et al., 2013). A recent MR study found GC rs2282679 A>C variant was not only associated with 25(OH)D levels but also associated with DBP levels, which indicated that GC rs2282679 A>C might be a pleiotropic variant (Zhang et al., 2020). DHCR7 encodes an enzyme responsible for transforming 7-dehydrocholesterol to cholesterol, and DHCR7 rs12785878 T>C was found to be associated with cholesterol according to a study in the Global Lipids Genetics Consortium (Willer et al., 2013). A recent analysis provided strong evidence indicating total cholesterol, low-density lipoprotein cholesterol, and high-density lipoprotein cholesterol levels as causal susceptibility factors for AD (Ostergaard et al., 2015). This provides possible evidence that this SNP may have other effects on AD. However, proofs are insufficient whether this SNP is associated with other factors that can increase the risk of AD.
Our results showed that DHCR7 rs12785878 T>C is associated with increased risk of EOAD rather than the more common LOAD, indicating that genetic background has a more significant impact on EOAD. We did not find significant differences between cases and controls on the other three SNPs. There are several possible explanations for our negative results. Firstly, the previous study did not include the Chinese population, which means the results based on these data sources might not apply to the Chinese community even though they have included another Asian group like Indian. Since the ethnic or geographic origin of subjects can affect the frequency of SNP, this can partly explain why positive results were not replicated in our Chinese cohort. Secondly, considering our sample size is relatively small for association studies, more samples should be included to provide more substantial evidence. Although there is no strong connection between the other three SNPs associated with vitamin D insufficiency and risk of AD in our study, using genotype or allele frequency to measure the role of a risk factor in disease etiology is still useful. Since these four SNPs only explain little heritability of vitamin D, further investigation of other variations that might be associated with vitamin D and MR analysis between genetically decreased vitamin D and risk of AD in the Chinese population are needed.
Conclusion
In conclusion, our results suggest that DHCR7 rs12785878 T>C might be associated with risk of EOAD in the Chinese population, while other SNPs related to vitamin D insufficiency might not be. However, due to the limited data in this study, replication studies in larger samples are required.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethical Review Board at Xiangya Hospital of Central South University in China. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
XLiu, LS, PW, and ZL participated in the design of the study, statistical analysis, and manuscript drafting. HW and JP collected the samples and performed experiments. BJ, LS, and ZL instructed and supervised the whole study. BJ and XLia helped to draft the manuscript and in the statistical analysis. All authors read and approved the final manuscript.
Funding
This work was funded by the National Natural Science Foundation of China (No. 81671075 to LS) and the Science and Technology Institute Foundation of Hunan Province (No. 2018JJ2650 to ZL).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgene.2021.583695/full#supplementary-material
References
Afzal, S., Bojesen, S. E., and Nordestgaard, B. G. (2014). Reduced 25-hydroxyvitamin D and risk of Alzheimer's disease and vascular dementia. Alzheimers Dement. 10, 296–302. doi: 10.1016/j.jalz.2013.05.1765
Balion, C., Griffith, L. E., Strifler, L., Henderson, M., Patterson, C., and Heckman, G., et al. (2012). Vitamin D, cognition, and dementia: a systematic review and meta-analysis. Neurology 79, 1397–1405. doi: 10.1212/WNL.0b013e31826c197f
Bikle, D. D., Siiteri, P. K., Ryzen, E., and Haddad, J. G. (1985). Serum protein binding of 1,25-dihydroxyvitamin D: a reevaluation by direct measurement of free metabolite levels. J. Clin. Endocrinol. Metab. 61, 969–975. doi: 10.1210/jcem-61-5-969
Brewer, L. D., Porter, N. M., Kerr, D. S., Landfield, P. W., and Thibault, O. (2006). Chronic 1alpha,25-(OH)2 vitamin D3 treatment reduces Ca2+ -mediated hippocampal biomarkers of aging. Cell Calcium 40, 277–286. doi: 10.1016/j.ceca.2006.04.001
Brewer, L. D., Thibault, V., Chen, K. C., Langub, M. C., Landfield, P. W., and Porter, N. M. (2001). Vitamin D hormone confers neuroprotection in parallel with downregulation of L-type calcium channel expression in hippocampal neurons. J. Neurosci. 21, 98–108. doi: 10.1523/JNEUROSCI.21-01-00098.2001
Chaves, M., Toral, A., Bisonni, A., Rojas, J. I., Fernandez, C., and Garcia, B. M., et al. (2014). Treatment with vitamin D and slowing of progression to severe stage of Alzheimer's disease. Vertex 25, 85–91.
Dubois, B., Feldman, H. H., Jacova, C., Dekosky, S. T., Barberger-Gateau, P., and Cummings, J., et al. (2007). Research criteria for the diagnosis of Alzheimer's disease: revising the NINCDS-ADRDA criteria. Lancet Neurol. 6, 734–746. doi: 10.1016/S1474-4422(07)70178-3
Dursun, E., Gezen-Ak, D., and Yilmazer, S. (2011). A novel perspective for Alzheimer's disease: vitamin D receptor suppression by amyloid-beta and preventing the amyloid-beta induced alterations by vitamin D in cortical neurons. J. Alzheimers Dis. 23, 207–219. doi: 10.3233/JAD-2010-101377
Gezen-Ak, D., Dursun, E., and Yilmazer, S. (2011). The effects of vitamin D receptor silencing on the expression of LVSCC-A1C and LVSCC-A1D and the release of NGF in cortical neurons. PLoS ONE 6:e17553. doi: 10.1371/journal.pone.0017553
Jia, J., Hu, J., Huo, X., Miao, R., Zhang, Y., and Ma, F. (2019). Effects of vitamin D supplementation on cognitive function and blood Abeta-related biomarkers in older adults with Alzheimer's disease: a randomised, double-blind, placebo-controlled trial. J. Neurol. Neurosurg. Psychiatry 90, 1347–1352. doi: 10.1136/jnnp-2018-320199
Lambert, J. C., Ibrahim-Verbaas, C. A., Harold, D., Naj, A. C., Sims, R., Bellenguez, C., et al. (2013). Meta-analysis of 74,046 individuals identifies 11 new susceptibility loci for Alzheimer's disease. Nat. Genet. 45, 1452–1458. doi: 10.1038/ng.2802
Littlejohns, T. J., Henley, W. E., Lang, I. A., Annweiler, C., Beauchet, O., Chaves, P. H., et al. (2014). Vitamin D and the risk of dementia and Alzheimer disease. Neurology 83, 920–928. doi: 10.1212/WNL.0000000000000755
Martinez, M. E., Giovannucci, E. L., Colditz, G. A., Stampfer, M. J., Hunter, D. J., and Speizer, F. E., et al. (1996). Calcium, vitamin D, and the occurrence of colorectal cancer among women. J. Natl. Cancer Inst. 88, 1375–1382. doi: 10.1093/jnci/88.19.1375
Masoumi, A., Goldenson, B., Ghirmai, S., Avagyan, H., Zaghi, J., Abel, K., et al. (2009). 1alpha,25-dihydroxyvitamin D3 interacts with curcuminoids to stimulate amyloid-beta clearance by macrophages of Alzheimer's disease patients. J. Alzheimers Dis. 17, 703–717. doi: 10.3233/JAD-2009-1080
Mizwicki, M. T., Menegaz, D., Zhang, J., Barrientos-Duran, A., Tse, S., and Cashman, J. R., et al. (2012). Genomic and nongenomic signaling induced by 1alpha,25(OH)2-vitamin D3 promotes the recovery of amyloid-beta phagocytosis by Alzheimer's disease macrophages. J. Alzheimers Dis. 29, 51–62. doi: 10.3233/JAD-2012-110560
Mokry, L. E., Ross, S., Morris, J. A., Manousaki, D., Forgetta, V., and Richards, J. B. (2016). Genetically decreased vitamin D and risk of Alzheimer disease. Neurology 87, 2567–2574. doi: 10.1212/WNL.0000000000003430
Moon, M., Song, H., Hong, H. J., Nam, D. W., Cha, M., and Oh, M. S., et al. (2013). Vitamin D-binding protein interacts with Aβ and suppresses Aβ-mediated pathology. Cell Death Differentiat. 20, 630–638. doi: 10.1038/cdd.2012.161
Musiol, I. M., and Feldman, D. (1997). 1,25-dihydroxyvitamin D3 induction of nerve growth factor in L929 mouse fibroblasts: effect of vitamin D receptor regulation and potency of vitamin D3 analogs. Endocrinology 138, 12–18. doi: 10.1210/endo.138.1.4858
Ostergaard, S. D., Mukherjee, S., Sharp, S. J., Proitsi, P., Lotta, L. A., Day, F., et al. (2015). Associations between potentially modifiable risk factors and Alzheimer disease: a mendelian randomization study. PLoS Med. 12:e1001841. doi: 10.1371/journal.pmed.1001841
Querfurth, H. W., and LaFerla, F. M. (2010). Alzheimer's disease. N. Engl. J. Med. 362, 329–344. doi: 10.1056/NEJMra0909142
Reitz, C., Brayne, C., and Mayeux, R. (2011). Epidemiology of Alzheimer disease. Nat. Rev. Neurol. 7, 137–152. doi: 10.1038/nrneurol.2011.2
Rizzoli, R., Stevenson, J. C., Bauer, J. M., van Loon, L. J., Walrand, S., and Kanis, J. A., et al. (2014). The role of dietary protein and vitamin D in maintaining musculoskeletal health in postmenopausal women: a consensus statement from the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO). Maturitas 79, 122–132. doi: 10.1016/j.maturitas.2014.07.005
Saporito, M. S., Brown, E. R., Hartpence, K. C., Wilcox, H. M., Vaught, J. L., and Carswell, S. (1994). Chronic 1,25-dihydroxyvitamin D3-mediated induction of nerve growth factor mRNA and protein in L929 fibroblasts and in adult rat brain. Brain Res. 633, 189–196. doi: 10.1016/0006-8993(94)91539-3
Smith, G. D., and Ebrahim, S. (2003). 'Mendelian randomization': can genetic epidemiology contribute to understanding environmental determinants of disease? Int. J. Epidemiol. 32, 1–22. doi: 10.1093/ije/dyg070
Verboven, C., Rabijns, A., De Maeyer, M., Van Baelen, H., Bouillon, R., and De Ranter, C. (2002). A structural basis for the unique binding features of the human vitamin D-binding protein. Nat. Struct. Biol. 9, 131–136. doi: 10.1038/nsb754
Wang, T. J., Pencina, M. J., Booth, S. L., Jacques, P. F., Ingelsson, E., Lanier, K., et al. (2008). Vitamin D deficiency and risk of cardiovascular disease. Circulation 117, 503–511. doi: 10.1161/CIRCULATIONAHA.107.706127
Wang, T. J., Zhang, F., Richards, J. B., Kestenbaum, B., van Meurs, J. B., and Berry, D., et al. (2010). Common genetic determinants of vitamin D insufficiency: a genome-wide association study. Lancet 376, 180–188. doi: 10.1016/S0140-6736(10)60588-0
White, P., and Cooke, N. (2000). The multifunctional properties and characteristics of vitamin D-binding protein. Trends Endocrinol. Metab. 11, 320–327. doi: 10.1016/S1043-2760(00)00317-9
Willer, C. J., Schmidt, E. M., Sengupta, S., Peloso, G. M., Gustafsson, S., Kanoni, S., et al. (2013). Discovery and refinement of loci associated with lipid levels. Nat. Genet. 45, 1274–1283. doi: 10.1038/ng.2797
Zhang, H., Wang, T., Han, Z., Wang, L., Zhang, Y., and Wang, L., et al. (2020). Impact of vitamin D binding protein levels on Alzheimer's disease: a mendelian randomization study. J. Alzheimers Dis. 74, 991–998. doi: 10.3233/JAD-191051
Zhang, J., Sokal, I., Peskind, E. R., Quinn, J. F., Jankovic, J., and Kenney, C., et al. (2008). CSF multianalyte profile distinguishes Alzheimer and Parkinson diseases. Am. J. Clin. Pathol. 129, 526–529. doi: 10.1309/W01Y0B808EMEH12L
Keywords: vitamin D insufficiency, Alzheimer's disease, single neucleotide polymorphism, genetic association analysis, 25(OH)D
Citation: Liu X, Wu P, Shen L, Jiao B, Liao X, Wang H, Peng J and Lin Z (2021) DHCR7 rs12785878 T>C Polymorphism Is Associated With an Increased Risk of Early Onset of Alzheimer's Disease in Chinese Population. Front. Genet. 12:583695. doi: 10.3389/fgene.2021.583695
Received: 15 July 2020; Accepted: 08 January 2021;
Published: 22 February 2021.
Edited by:
Jordi Pérez-Tur, Superior Council of Scientific Investigations (CSIC), SpainReviewed by:
May A. Beydoun, National Institutes of Health (NIH), United StatesCarol D. SanMartín, Major University, Chile
Steven Estus, University of Kentucky, United States
Copyright © 2021 Liu, Wu, Shen, Jiao, Liao, Wang, Peng and Lin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhangyuan Lin, bGluemhhbmd5dWFuMjUwNSYjeDAwMDQwO3NpbmEuY29t
 Xixi Liu
Xixi Liu Pengfei Wu2
Pengfei Wu2 Lu Shen
Lu Shen Bin Jiao
Bin Jiao Xinxin Liao
Xinxin Liao Zhangyuan Lin
Zhangyuan Lin