
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Gastroenterol. , 15 December 2022
Sec. Gastrointestinal Infection
Volume 1 - 2022 | https://doi.org/10.3389/fgstr.2022.1063325
This article is part of the Research Topic Exploring the Interplay Between Clinical and Non-Clinical Outcomes for Children and Adults with Inflammatory Bowel Disease View all 6 articles
 Marco Vincenzo Lenti1,2*†
Marco Vincenzo Lenti1,2*† Giacomo Broglio1,2†
Giacomo Broglio1,2† Caterina Mengoli2
Caterina Mengoli2 Sara Cococcia1,2
Sara Cococcia1,2 Federica Borrelli de Andreis1,2
Federica Borrelli de Andreis1,2 Marta Vernero1,2
Marta Vernero1,2 Lavinia Pitotti1,2
Lavinia Pitotti1,2 Lucia Padovini1,2
Lucia Padovini1,2 Matteo Secco1,2
Matteo Secco1,2 Mariangela Delliponti2
Mariangela Delliponti2 Gino Roberto Corazza1,2
Gino Roberto Corazza1,2 Catherine Klersy3
Catherine Klersy3 Antonio Di Sabatino1,2
Antonio Di Sabatino1,2Introduction: Inflammatory bowel disease (IBD), namely ulcerative colitis and Crohn’s disease, is a chronic relapsing immune-mediated condition that may cause an impairment of social functions due to stigmatisation. Resilience instead is associated with an improvement in coping with adversities and thus may counteract the detrimental effects of stigmatisation. We herein sought to determine the fluctuation of stigmatisation and resilience in a cohort of patients with IBD at 1-year follow-up.
Methods: This is a prospective, monocentric study conducted in a tertiary referral centre. All patients with IBD were assessed at enrolment and at oneyear follow-up. Several clinical and demographic variables were collected. Stigmatisation was assessed through a validated Italian version of the Perceived Stigma Scale for IBD (PSS-IBD), while resilience was assessed through the 25-item Connor Davidson Resilience Scale (CD-RISC25). Also, self-efficacy (SEF) and self-esteem (SES) scales were assessed.
Results: In this study, 105 patients were included (46 Crohn’s disease, 59 ulcerative colitis; overall mean age 47 years ±11, M:F ratio 1:1.2). None of the 4 scales showed a statistically significant variation at one year compared to baseline (median CD-RISC25 64 at baseline vs 61 at follow-up; SEF 31 vs 30; SES 32.5 vs 32; PSS-IBD 0.45 vs 0.45). A statistically significant and inverse correlation was found between CD-RISC25 and PSS-IBD (rho -0.222, p=0.01), SEF and PSS-IBD (rho -0.219, p= 0.01), SES and PSS-IBD (-0.316, p=0.003). CD-RISC25 was found to be positively associated with inactive IBD (p=0.05).
Discussion: In this prospective study we have shown for the first time that stigmatisation, resilience, SEF and SEM did not change over a one-year time span, suggesting that, based on the information gathered, these characteristics may be independent from IBD severity or IBD flares. Furthermore, we found an inverse correlation of stigma with resilience, SEF and SES, suggesting an important role that these variables may have on preventing stigmatisation.
Inflammatory bowel disease (IBD), namely Crohn’s disease (CD), ulcerative colitis (UC), and IBD unclassified (1), is an immune-mediated chronic condition characterized by periods of relapse and remission (2), that has a deep impact on the patients’ health, quality of life, and psychological dimension. This is the consequence of a) pervasive symptoms (3) experienced by patients with IBD, such as chronic abdominal pain, diarrhoea, rectal bleeding, and fatigue; b) the risk of receiving surgical treatment (4) and; c) the marked impact of IBD on sexual life (4). Another cause of psychological burden in patients with IBD is social stigma (5, 6) which is defined as the feeling or fear that other people may have a negative attitude towards someone due to specific attributes (6–8), leading to a loss of status quo and to discrimination (7). In a clinical setting, stigma can be categorized into perceived stigma (when a negative attitude is felt by an individual), enacted stigma (discriminating acts), and internalized, self-stigma (8). Stigma is known to have a detrimental impact on several chronic diseases, such as psychiatric disorders (9), HIV (10, 11), and epilepsy (12). Stigma may be experienced by up to 84% of patients with IBD, regardless of disease activity (13); moreover, stigma is also associated with a higher prevalence of depression, social withdrawal, and poorer quality of life (14–16). Stigmatisation can be measured in patients with BID with a scale adapted from patients with irritable bowel syndrome (IBS), known as Perceived Stigma Scale (PSS) (17, 18).
Resilience is a positive psychological resource that may potentially counteract the detrimental effects of stigma on quality of life (19). Resilience can be found in three main dimensions, namely personality traits (the innate ability to address negative situations), outcomes (the positive impact that resilience has on the disease’s impact), and processes (the dynamic process, namely coping with a chronic condition) (20). Interestingly, resilience in IBD has been found to be associated with a more favourable outcome (21–23), and it is linked to some individual characteristics, including age, sex, employment status (24, 25). Additionally, it can be trained via resilience-enhancing programs and the development of mindfulness (26–28). Resilience can be measured with objective scales, and one of the most used worldwide is the Connor-Davidson Resilience Scale (CD-RISC25) (29).
Finally, self-efficacy (SEF) and self-esteem (SES) may also play an important role in relation to stigma and resilience. SEF is defined as the confidence to independently manage the disease without needing a caregiver (30) and it has been found to favourably affect the outcome of chronic diseases (31), though being a task-specific skill (31–33) and therefore a non-transferable skill from other aspects of life; furthermore, self-efficacy can predict health promoting behaviour in chronic ill patients, regardless of disease activity and severity (34). SES instead plays an important role in mental health, as a lack of it has been linked to a higher rate of depression and anxiety (35, 36); notably, in the IBD setting, it can be measured by a scale developed by Rosenberg et al. (36, 37).
Because of limited data on stigma in IBD and because of the absence of a validated scale for PSS-IBD in the Italian language, we previously performed a study for validating an Italian version of the PSS-IBD (29). By using a three-step method, the validation showed acceptable translation and psychometric properties, with an excellent item internal consistency (Cronbach alpha 0.87). Additionally, we assessed stigmatisation, resilience, SEF, and SES at baseline; we found that resilience negatively correlated with perceived stigma. In the present paper we report the one-year follow-up results of the aforementioned prospective study (29), as well as other important outcomes, including the associations between stigma, resilience, SEF, and SES in relation to IBD activity.
IBD patients followed-up at the IBD Clinical & Research Centre of the San Matteo Hospital Foundation were consecutively enrolled between December 2018 and September 2019 and we originally planned to follow them up after 12 months. However, due to the occurrence of the SARS-CoV-2 pandemic, the follow-up period was extended until July 2021. The initial sample consisted of 126 IBD patients, though 24 dropped out at the follow-up evaluation. Briefly, all IBD diagnoses followed the international guidelines (1, 38). Patients were eligible for inclusion if they had at least a 3-month history of IBD, were aged ≥18, were able to complete a questionnaire, and were willing to provide written informed consent; patients with an inconclusive or uncertain diagnosis of IBD, those diagnosed less than 3 months before or unwilling to provide informed consent were excluded. Demographic and clinical characteristics were gathered, including IBD type, disease activity and duration, comorbidities, and previous IBD-related surgery.
We evaluated disease activity in CD with the Harvey-Bradshaw index (HBI) (39), while using the Partial Mayo Index for UC (40). HBI is a score that considers many factors, spacing from general well-being, abdominal pain, number of liquid or soft stools, the presence of abdominal mass and complications, if any (namely arthralgia, uveitis, erythema nodosum and others). An HBI of <5 defines disease remission, an HBI of 5-7 a mild disease, an HBI of 8-16 a moderate disease, and an HBI of >16 a severe disease. The Partial Mayo Score evaluates stool frequency, rectal bleeding, and the physician rating of disease activity. A Partial Mayo Score of <2 defines disease remission, a score of 2-4 a mild disease severity, a score of 5-7 a moderate disease severity, and a score of >7 a severe disease severity. By active disease, we considered either a Partial Mayo Score of ≥5 for UC or an HBI of ≥ 8 for CD.
Stigma was assessed by using the Italian validated version of the PSS-IBD (41) scale, a self-administered questionnaire composed of 10 items and scoring the perceived stigma from 0 (never) to 4 (always) points, with the higher ranking meaning a higher level of stigma. The score was performed both for the patient’s “significant others” (SO) (i.e., the social background, family, friends) and for the “healthcare professional” (HP), leading to a total of 20 overall evaluated items. Both evaluations are important, as are part of the original PSS-IBS. The distinction between SO and HP was deemed important as patients with IBS may be more likely to be considered as having a psychosomatic disorder, thus increasing stigma. Also, measuring the perceived stigma from patients is pivotal because it can have an impact on the patients’ trust on HP. The final stigma score was then obtained by calculating all the values and mean of all values of the items (SO+HP).
Resilience was evaluated using the Italian-translated version of the Connor-Davidson Resilience Scale (CD-RISC25) (29) which consists of a self-administered questionnaire composed of 25 items on a five-point Likert scale, where 0 stands for strongly disagree and 4 for strongly agree, and the final score is obtained with the sum of all the individual scores, with a higher score underlying a higher resilience (42).
The Rosenberg SES scale, is a 10-item scale. Scoring involves combined ratings from 1 to 4 points; low SES answers are “disagree” or “strongly disagree” on items 1, 3, 4, 7, 10, and, conversely, “strongly agree” or “agree” on items 2, 5, 6, 8, 9 (35, 36, 43) with higher scores underlying a higher level of SES.
SEF is the ability to cope with the needs and the medical adherence in a chronic disease. In IBD this skill was measured with a scale developed by Keefer et al. in 2011 (41) and it consists in an interview with 29 items that explore various disease-related areas with item scores varying from 1 (not at all) to 10 (totally). The 4 areas that were evaluated were as floow: managing stress and emotions, managing medical care, managing symptoms and diseases, maintaining remission (44), with the higher the score, the higher the SEF.
We used the Stata software (release 17, StataCorp, College Station, TX, USA) for computations. A 2-sided p-value <0.05 was considered as statistically significant. We described continuous variables with the mean and standard deviation (SD) or the median and quartiles (IQR), if skewed; we described categorical variables as counts and percent. We used the signed rank test for comparisons of questionnaire scores and the exact McNemar test to compare disease activity over time. We used the Mann Whitney U test to compare scores between patients with active or inactive disease at time 0; we used the Spearman R and 95% confidence interval (95% CI) to measure the correlation of scores at time 0. The study was approved by the local Ethics Committee (Protocol #20190003611), and all participants gave their informed written consent to take part to the study and for the anonymized publication of data.
In our study, 105 patients of the previously 125 enrolled (84%) completed the follow-up. The demographic and clinical characteristics are summarized in Table 1. Of the overall 105 patients, 45.2% had Crohn’s disease and 54.8% had ulcerative colitis. Regarding therapy, 14 (13.5%) of patients were under biological therapy, with infliximab being the most prescribed (7 patients; 50%) and 38 (36%) were given 5-aminosalycilic drugs. Finally, five (4%) patients were not taking medications.
At one-year follow-up, 4 questionnaires were assessed, namely CD-RISC 25, PSS, SES and SEF scales (Table 2). No statistically significant difference was found between baseline and follow-up for all questionnaires. The CD-RISC25 values were 64 at baseline (IQR 54-79 and 61 at follow-up (IQR 51-73; p=0.12); the SEF values were 31 at baseline (IQR 28-34) and 30 at follow-up (IQR 27-33; p=0.12); the SES values were 32.5 at baseline (IQR 28-34) and 32 at follow-up (IQR 29-34,5; p=0.17). We also evaluated the PSS-IBD scale that showed higher values for the significant others (PSS-SO) stigma versus the healthcare (PSS-HP) one, with no statistically significant difference between baseline and follow-up. PSS-SO was 0.7 (IQR 0.4-1.4) at baseline and 0.7 (IQR 0.4-1.3) at follow-up (p=0.54); PSS-HP was 0.1 both at baseline and at follow-up (p=0.96) and PSS-SUM, obtained by adding the scores of HP and SO, was 0.45 at baseline (IQR 0.25-0.9) and 0.45 (IQR 0.2-0.85) at follow-up (p=0.8).
Correlations among the various questionnaires were assessed via the Spearman’s Rho (Table 3). Notably, an inverse correlation between PSS (and its subgroups) and CD-RISC25 was noticed in almost all cases, as well as for SES or SEF and PSS (and its subgroups).
Lastly, we evaluated disease activity and its correlation with CD-RISC25 and PSS, and the effect that reaching disease remission at one year could have on these two variables (Table 4). Of the 126 patients, at baseline 86% were in remission and 14% (n=15) had an active disease (Partial Mayo Score ≥5 for UC or HBI ≥8 for CD). Disease remission was defined as for all the patients who had active disease on baseline and had partial mayo scores <5 and HBI <8 at follow-up. Of note, CD-RISC25 was inversely and significantly associated with disease activity. Disease remission at follow-up was achieved in 14 (92%) patients who had active disease at baseline, and this had no impact on both stigma and resilience.
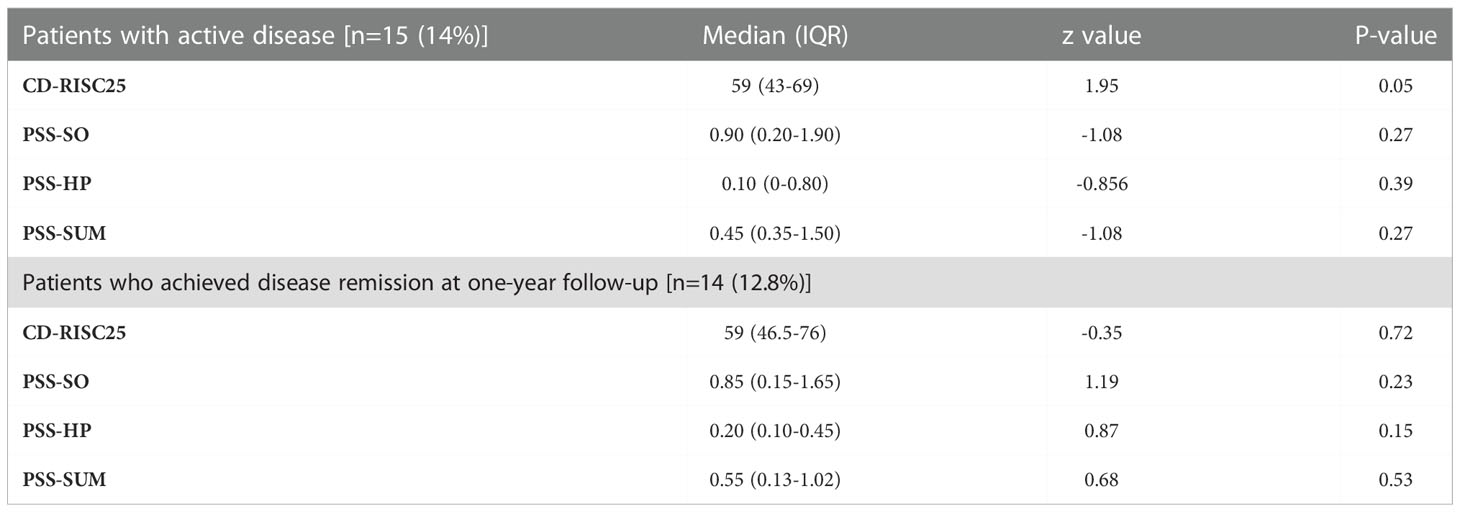
Table 4 Correlation between disease activity and questionnaire scores, and between those who reached disease remission at one-year follow-up and questionnaire scores.
In this prospective study we have shown for the first time that stigmatisation, resilience, SEF and SEM did not change over a one-year time span, suggesting that, based on the information gathered, these characteristics may be independent from IBD severity or IBD flares. Furthermore, we found an inverse correlation of stigma with resilience, SEF and SES, suggesting an important role that these variables may have on preventing stigmatisation.
The first endpoint of our study consisted in the follow-up evaluation of the CD-RISC25, the PSS-IBD, and the SEF and SES scales in order to assess how they changed over time. Interestingly, for all of these scales, no statistical difference emerged, suggesting that stigma and resilience are stable over time in IBD, at least over one year, differently to what is seen for IBS (35, 37). Furthermore, a strong “floor effect” was evident with regard to stigmatisation; this was, in fact, particularly low, especially the HP sub-score, probably because these patients were accessing a tertiary referral centre for IBD management, with well-trained doctors and nurses having a long lasting experience, as we postulated in our previous paper (29). Even considering this explanation, the levels of stigmatisation experienced by our patients were even lower than those reported in a similar, previously published, paper (18). We may speculate that the patients included in our study had, on average, a longstanding disease, and hence they had more time to cope and adapt to IBD. There may also be other factors, namely cultural and behavioural, that were not specifically addressed in this study. To note, the follow-up period coincided with the outbreak of the COVID-19 pandemic that may have played an independent role in determining stigma and resilience levels.
Interestingly, what emerged from our second endpoint was that stigma and resilience have an inverse correlation, as well as SES and SEF, with regard to stigma. We noted that CD-RISC25 was inversely related to the PSS-SO, PSS-HP (although at the limit of significance), and PSS-SUM. Stigma, SEF and SES had a similar trend. This suggests that interventions aimed at improving resilience, SES, and SEF may potentially counteract the perceived stigmatisation; therefore, interventional studies are needed to clarify this topic, as there is no available evidence.
Finally, in the third endpoint of our study we noted that resilience was inversely associated with an active disease, while stigma was inversely correlated with disease activity, although not significantly. Lastly, reaching disease remission at one year did not have any statistically significant correlation with the CD-RISC25 or the PSS-IBD. These results may be related to the small sample size of patients with an active disease who reached remission in our cohort. Nonetheless, various results can be found in previously published papers (13, 14, 29) in this regard, although with a small sample size. In our previously published paper, only for UC patients, disease activity correlated with higher PSS-SO, while no other associations among PSS and disease activity in CD were noticed (29). In another study, disease activity was found to worsen quality of life, but a formal correlation between stigma and disease activity was not made (13). Finally, in a study looking at stigma and depressive symptoms in young IBD patients, there were too few patients with an active disease for drawing firm conclusions (14). Hence, further larger studies are needed to better address this issue.
Our study certainly has some limits. First, our cohort had a consistent floor effect both on perceived stigma and disease activity, and the follow-up period was affected by the COVID-19 outbreak. The sample size was relatively small, therefore, further studies with larger cohorts are needed to better assess these topics. Our study has some strengths as well, as it was the first prospective, clinical study that evaluated how stigma and resilience changed over time in in an Italian cohort of IBD patients, demonstrating not only that these two characteristics are stable over one year, but even that SEF and SES are stable as well. Furthermore, we noticed that stigma is inversely correlated with resilience, SES and SEF, and this finding paves the way for a more holistic approach that should include a psychological assessment and support in IBD patients.
IBD patients are complex patients who may be burdened by psychological and physical issues that need to be recognised and correctly assessed by their treating physicians, in order to offer to these patients a higher quality of life. A more holistically-driven approach, with the intervention of a multidisciplinary team may help bringing a special focus on reducing stigma and improving resilience, SEF, and SES in this population. Other factors potentially affecting stigma and resilience in IBD should be investigated.
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by San Matteo Hospital Foundation. The patients/participants provided their written informed consent to participate in this study.
All authors participated in the drafting of the manuscript or critical revision of the manuscript for important intellectual content and provided approval of the final submitted version. All authors contributed to collect data, writing the manuscript, and reviewing the paper.
We thank the “Rete Aging” project - Italian Ministry of Health, for supporting research focusing on diseases and conditions affecting the elderly.
ML and GB are grateful to the University of Pavia and for supporting their research projects.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Magro F, Gionchetti P, Eliakim R, Ardizzone S, Armuzzi A, Barreiro-de Acosta M, et al. European Crohn’s and colitis organisation [ECCO]. third European evidence-based consensus on diagnosis and management of ulcerative colitis. part 1: Definitions, diagnosis, extra-intestinal manifestations, pregnancy, cancer surveillance, surgery, and ileo-anal pouch disorders. J Crohns Colitis. (2017) 11(6):649–70. doi: 10.1093/ecco-jcc/jjx008. Erratum in: J Crohns Colitis. 2022.
2. Di Sabatino A, Rovedatti L, Vidali F, Macdonald TT, Corazza GR. Recent advances in understanding crohn’s disease. Intern Emerg Med (2013) 8(2):101–13. doi: 10.1007/s11739-011-0599-2
3. Bączyk G, Kozłowska KA, Formanowicz D, Białas E, Karoń J, Krokowicz P. The relationship between the symptom of fatigue and the functioning of patients with inflammatory bowel diseases after surgery. Prz Gastroenterol (2019) 14(4):242–9. doi: 10.5114/pg.2019.90251
4. Häuser W, Janke KH, Klump B, Hinz A. Anxiety and depression in patients with inflammatory bowel disease: comparisons with chronic liver disease patients and the general population. Inflammation Bowel Dis (2011) 17(2):621–32. doi: 10.1002/ibd.21346
5. Lenti MV, Cococcia S, Ghorayeb J, Di Sabatino A, Selinger CP. Stigmatisation and resilience in inflammatory bowel disease. Intern Emerg Med (2020) 15(2):211–23. doi: 10.1007/s11739-019-02268-0
6. Taft TH, Keefer L. A systematic review of disease-related stigmatization in patients living with inflammatory bowel disease. Clin Exp Gastroenterol (2016) 9:49–58. doi: 10.2147/CEG.S83533
7. Corrigan PW, Watson AC. Understanding the impact of stigma on people with mental illness. World Psychiatry (2002) 1(1):16–20.
8. Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol (2001) 27:363–85. doi: 10.1146/annurev.soc.27.1.363
9. Degnan A, Berry K, Humphrey C, Bucci S. The relationship between stigma and subjective quality of life in psychosis: A systematic review and meta-analysis. Clin Psychol Rev (2021) 85:102003. doi: 10.1016/j.cpr.2021.102003
10. Wu X, Chen J, Huang H, Liu Z, Li X. Perceived stigma, medical social support and quality of life among people living with HIV/AIDS in hunan, China. Appl Nurs Res (2015) 28(2):169–74. doi: 10.1016/j.apnr.2014.09.011
11. Ammirati RJ, Lamis DA, Campos PE, Farber EW. Optimism, well-being, and perceived stigma in individuals living with HIV. AIDS Care (2015) 27(7):926–33. doi: 10.1080/09540121.2015.1018863
12. Shi Y, Wang S, Ying J, Zhang M, Liu P, Zhang H, et al. Correlates of perceived stigma for people living with epilepsy: A meta-analysis. Epilepsy Behav (2017) 70(Pt A):198–203. doi: 10.1016/j.yebeh.2017.02.022
13. Taft TH, Keefer L, Leonhard C, Nealon-Woods M. Impact of perceived stigma on inflammatory bowel disease patient outcomes. Inflammation Bowel Dis (2009) 15(8):1224–32. doi: 10.1002/ibd.20864
14. Gamwell KL, Baudino MN, Bakula DM, Sharkey CM, Roberts CM, Grunow JE, et al. Perceived illness stigma, thwarted belongingness, and depressive symptoms in youth with inflammatory bowel disease (IBD). Inflammation Bowel Dis (2018) 24(5):960–5. doi: 10.1093/ibd/izy011
15. Barned C, Stinzi A, Mack D, O’Doherty KC. To tell or not to tell: A qualitative interview study on disclosure decisions among children with inflammatory bowel disease. Soc Sci Med (2016) 162:115–23. doi: 10.1016/j.socscimed.2016.06.023
16. Guo L, Rohde J, Farraye FA. Stigma and disclosure in patients with inflammatory bowel disease. Inflammation Bowel Dis (2020) 26(7):1010–6. doi: 10.1093/ibd/izz260
17. Jones MP, Keefer L, Bratten J, Taft TH, Crowell MD, Levy R, et al. Development and initial validation of a measure of perceived stigma in irritable bowel syndrome. Psychol Health Med (2009) 14(3):367–74. doi: 10.1080/13548500902865956
18. Taft TH, Keefer L, Artz C, Bratten J, Jones MP. Perceptions of illness stigma in patients with inflammatory bowel disease and irritable bowel syndrome. Qual Life Res (2011) 20(9):1391–9. doi: 10.1007/s11136-011-9883-x
19. Luo D, Zhou M, Sun L, Lin Z, Bian Q, Liu M, et al. Resilience as a mediator of the association between perceived stigma and quality of life among people with inflammatory bowel disease. Front Psychiatry (2021) 12:709295. doi: 10.3389/fpsyt.2021.709295
20. Kim GM, Lim JY, Kim EJ, Park SM. Resilience of patients with chronic diseases: A systematic review. Health Soc Care Community. (2019) 27(4):797–807. doi: 10.1111/hsc.12620
21. Liu Z, Zhou X, Zhang W, Zhou L. Factors associated with quality of life early after ischemic stroke: the role of resilience. Top Stroke Rehabil. (2019) 26(5):335–41. doi: 10.1080/10749357.2019.1600285
22. Sehgal P, Ungaro RC, Foltz C, Iacoviello B, Dubinsky MC, Keefer L. High levels of psychological resilience associated with less disease activity, better quality of life, and fewer surgeries in inflammatory bowel disease. Inflammation Bowel Dis (2021) 27(6):791–6. doi: 10.1093/ibd/izaa196
23. Taylor K, Scruggs PW, Balemba OB, Wiest MM, Vella CA. Associations between physical activity, resilience, and quality of life in people with inflammatory bowel disease. Eur J Appl Physiol (2018) 118(4):829–36. doi: 10.1007/s00421-018-3817-z
24. Acciari AS, Leal RF, Coy CSR, Dias CC, Ayrizono MLS. Relationship among psychological well-being, resilience and coping with social and clinical features in crohn’s disease patients. Arq Gastroenterol (2019) 56(2):131–40. doi: 10.1590/S0004-2803.201900000-27
25. Ye ZJ, Liang MZ, Qiu HZ, Liu ML, Hu GY, Zhu YF, et al. Effect of a multidiscipline mentor-based program, be resilient to breast cancer (BRBC), on female breast cancer survivors in mainland China-a randomized, controlled, theoretically-derived intervention trial. Breast Cancer Res Treat (2016) 158(3):509–22. doi: 10.1007/s10549-016-3881-1
26. Kovacs AH, Bandyopadhyay M, Grace SL, Kentner AC, Nolan RP, Silversides CK, et al. Adult congenital heart disease-coping and REsilience (ACHD-CARE): Rationale and methodology of a pilot randomized controlled trial. Contemp Clin Trials. (2015) 45(Pt B):385–93. doi: 10.1016/j.cct.2015.11.002
27. Wang M, Lu X, Liu M. The mediating effect of psychological resilience on the level of mindfulness and general well-being in patients with inflammatory bowel disease. Ann Palliat Med (2021) 10(8):9215–22. doi: 10.21037/apm-21-2053
28. Connor KM, Davidson JR. Development of a new resilience scale: the connor-Davidson resilience scale (CD-RISC). Depress Anxiety. (2003) 18(2):76–82. doi: 10.1002/da.10113
29. Cococcia S, Lenti MV, Mengoli C, Klersy C, Borrelli de Andreis F, Secco M, et al. Validation of the Italian translation of the perceived stigma scale and resilience assessment in inflammatory bowel disease patients. World J Gastroenterol (2021) 27(39):6647–58. doi: 10.3748/wjg.v27.i39.6647
30. Carlsen K, Haddad N, Gordon J, Phan BL, Pittman N, Benkov K, et al. Self-efficacy and resilience are useful predictors of transition readiness scores in adolescents with inflammatory bowel diseases. Inflammation Bowel Dis (2017) 23(3):341–6. doi: 10.1097/MIB.0000000000001038
31. Johnston-Brooks CH, Lewis MA, Garg S. Self-efficacy impacts self-care and HbA1c in young adults with type I diabetes. Psychosom Med (2002) 64(1):43–51. doi: 10.1097/00006842-200201000-00007
32. Taal E, Rasker JJ, Seydel ER, Wiegman O. Health status, adherence with health recommendations, self-efficacy and social support in patients with rheumatoid arthritis. Patient Educ Couns. (1993) 20(2-3):63–76. doi: 10.1016/0738-3991(93)90122-d
34. Eindor-Abarbanel A, Naftali T, Ruhimovich N, Bar-Gil Shitrit A, Sklerovsky-Benjaminov F, Konikoff F, et al. Important relation between self-efficacy, sense of coherence, illness perceptions, depression and anxiety in patients with inflammatory bowel disease. Frontline Gastroenterol (2020) 12(7):601–7. doi: 10.1136/flgastro-2020-101412
35. Abdel-Khalek AM. Introduction to the psychology of self-esteem self-esteem: Perspectives, influences, and improvement strategies. Nova Science (2014) p. 1–23.
36. Opheim R, Moum B, Grimstad BT, Jahnsen J, Prytz Berset I, Hovde Ø, et al. Self-esteem in patients with inflammatory bowel disease. Qual Life Res (2020) 29(7):1839–46. doi: 10.1007/s11136-020-02467-9
38. Maaser C, Sturm A, Vavricka SR, Kucharzik T, Fiorino G, Annese V, et al. European Crohn’s and colitis organisation [ECCO] and the European society of gastrointestinal and abdominal radiology [ESGAR]. ECCO-ESGAR guideline for diagnostic assessment in IBD part 1: Initial diagnosis, monitoring of known IBD, detection of complications. J Crohns Colitis. (2019) 13(2):144–64. doi: 10.1093/ecco-jcc/jjy113
39. Harvey RF, Bradshaw JM. A simple index of crohn’s-disease activity. Lancet (1980) 1(8167):514. doi: 10.1016/s0140-6736(80)92767-1
40. Travis SP, Schnell D, Krzeski P, Abreu MT, Altman DG, Colombel JF, et al. Reliability and initial validation of the ulcerative colitis endoscopic index of severity. Gastroenterology (2013) 145(5):987–95. doi: 10.1053/j.gastro.2013.07.024
41. Keefer L, Kiebles JL, Taft TH. The role of self-efficacy in inflammatory bowel disease management: preliminary validation of a disease-specific measure. Inflammation Bowel Dis (2011) 17(2):614–20. doi: 10.1002/ibd.21314
42. Graff LA, Sexton KA, Walker JR, Clara I, Targownik LE, Bernstein CN, et al. Validating a measure of patient self-efficacy in disease self-management using a population-based IBD cohort: The IBD self-efficacy scale. Inflammation Bowel Dis (2016) 22(9):2165–72. doi: 10.1097/MIB.0000000000000856
43. Muse K, Johnson E, David AL. A feeling of otherness: A qualitative research synthesis exploring the lived experiences of stigma in individuals with inflammatory bowel disease. Int J Environ Res Public Health (2021) 18(15):8038. doi: 10.3390/ijerph18158038
Keywords: Connor-Davidson resilience scale, Crohn’s disease, inflammatory bowel disease, stigma, self-efficacy, self-esteem
Citation: Lenti MV, Broglio G, Mengoli C, Cococcia S, Borrelli de Andreis F, Vernero M, Pitotti L, Padovini L, Secco M, Delliponti M, Corazza GR, Klersy C and Di Sabatino A (2022) Stigmatization and resilience in inflammatory bowel disease patients at one-year follow-up. Front. Gastroenterol. 1:1063325. doi: 10.3389/fgstr.2022.1063325
Received: 06 October 2022; Accepted: 29 November 2022;
Published: 15 December 2022.
Edited by:
Tiffany Taft, Northwestern University, United StatesReviewed by:
Alexandra Fuss, Yale University, United StatesCopyright © 2022 Lenti, Broglio, Mengoli, Cococcia, Borrelli de Andreis, Vernero, Pitotti, Padovini, Secco, Delliponti, Corazza, Klersy and Di Sabatino. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marco Vincenzo Lenti, bWFyY28ubGVudGlAdW5pcHYuaXQ=
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.