- 1Department of Environmental and Occupational Health, Colorado School of Public Health, University of Colorado Anschutz Campus, Aurora, CO, United States
- 2Department of Cardiology, University of Colorado School of Medicine, University of Colorado Anschutz Campus, Aurora, CO, United States
- 3Division of Electrophysiology, Emory University, Atlanta, GA, United States
Introduction: Emerging risk factors for atrial fibrillation (AF) incidence and episodes (exacerbation), the most common and clinically significant cardiac arrhythmia, include air and noise pollution, both of which are emitted during oil and natural gas (O&G) well site development.
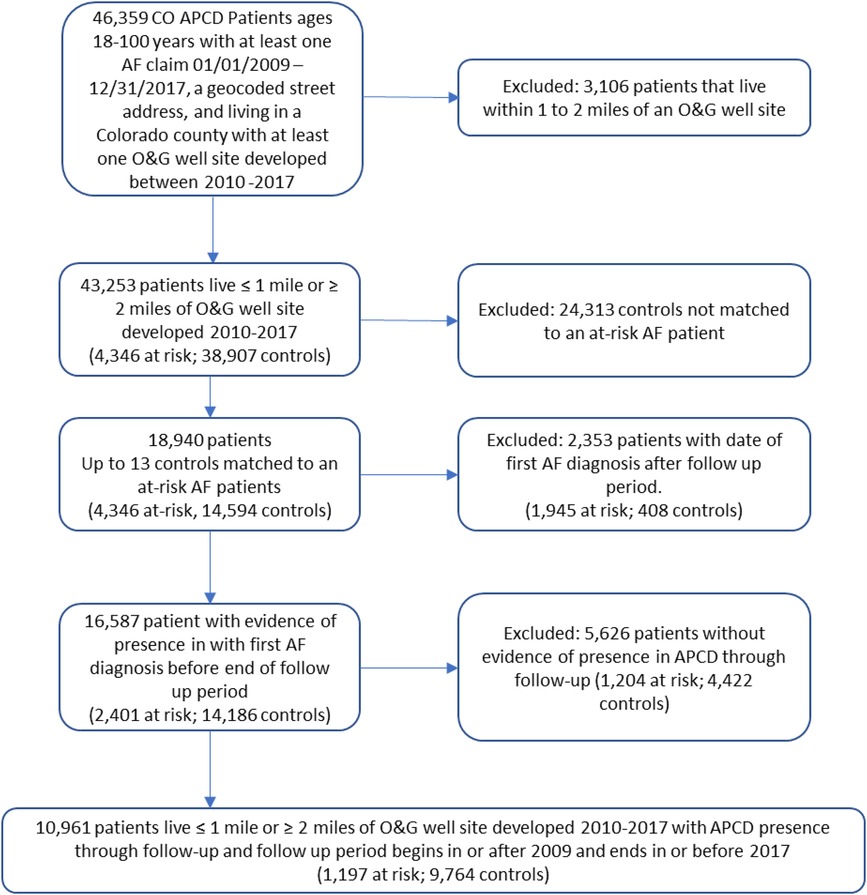
Methods: We evaluated AF exacerbation risk and proximity to O&G well site development by employing a novel data source and interrupted time-series design. We retrospectively followed 1,197 AF patients living within 1-mile of an O&G well site (at-risk of exposure) and 9,764 patients living >2 miles from any O&G well site (unexposed) for AF claims in Colorado's All Payer Claims Dataset before, during, and after O&G well site development. We calculated AF exacerbation risk with multi-failure survival analysis.
Results: The analysis of the total study population does not provide strong evidence of an association between AF exacerbation and proximity to O&G wells sites during (HR = 1.07, 95% CI: 0.94, 1.22) or after (HR = 1.01, 95% CI: 0.88, 1.16) development. However, AF exacerbation risk differed by patient age and sex. In patients >80 years living within 0.39 miles (2,059 feet) of O&G well site development, AF exacerbation risk increased by 83% (HR = 1.83, 95% CI: 1.25, 2.66) and emergency room visits for an AF event doubled (HR = 2.55, 95% CI: 1.50, 4.36) during development, with risk increasing with proximity. In female patients living within 0.39 miles of O&G well site development, AF exacerbation risk increased by 56% percent (95% CI: 1.13, 2.15) during development. AF exacerbation risk did not persist past the well development period. We did not observe increased AF exacerbation risk in younger or male patients.
Discussion: The prospect that proximity to O&G well site development, a significant noise and air pollution source, may increase AF exacerbation risk in older and female AF patients requires attention. These findings support appropriate patient education to help mitigate risk and development of mitigation strategies and regulations to protect the health of populations in O&G development regions.
Introduction
Atrial fibrillation (AF), the most common and clinically significant cardiac arrhythmia, impairs quality of life and substantially elevates stroke, systemic thromboembolism and heart failure risk (1, 2). The incidence and prevalence of AF are increasing (1–5). Adults aged >40 years of age have a 25% lifetime risk of developing AF (1). There are 9.3 million American's living with this chronic, dangerous, and costly condition contributing to an estimated 130,000 deaths and $6 billion in health care costs per year (6).
While knowledge on AF etiology is sparse, there are several known AF risk factors, including biological sex, advancing age, and co-morbidities (1), as well as emerging environmental risk factors including air and noise pollution (7–11). Several epidemiological studies have indicated that the risk of AF incidence increases with increasing levels of air pollutants, including particulate matter ≤2.5 micrometers, (PM2.5), nitrogen oxides (NOx), and ozone (8, 12–18), as well as higher exposure to traffic and railway noise (9, 19, 20). Additionally, studies have observed the risk of AF episodes (exascerbation) increases with increasing levels of air pollutants and noise (13, 14, 21, 22). In general, adverse cardiovascular effects are observed when audible noise levels exceed 50 A-weighted decibels (dBA) (23). Studies also suggest that nocturnal noise, which disrupts the normal sleep cycle, may be associated with greater health consequences than daytime noise (24–26). Clinically, chronic sleep deprivation is associated hypertension (27) and cardiovascular disease (28) which are firmly established and modifiable risk factors for AF (1).
One significant source of both air and noise pollution is the development of oil and natural gas (O&G) well sites. Between 2011 and 2014, 25,000–35,000 O&G well sites were developed annually in the United States (US) exceeding 150,000 total new well sites as of 2019 (29). This resulted in an extensive dispersion of O&G well sites across populated areas, with over 17 million people living within one mile of an O&G well (30). In Colorado, more than 378,000 people live within 1-mile of an O&G well site, with the densest development northeast of Denver (31). Air and noise pollution emitted during development of O&G well sites potentially impact all individuals residing near the sites (32).
As described elsewhere, modern O&G well site development is a complex, industrial process (33). Diesel-powered equipment, trucks, and generators continuously emit air pollutants and noise; on-site storage tanks, valves and pipes also emit air pollutants (34–36). Audible noise levels of 69 dBA and low frequency noise of 80 C-weighted decibels (dBC) have been reported during O&G well site development (35, 37). During development of 22-well O&G site in Colorado, 1–16 diesel trucks per hour travelled to and from the site, concentrations of PM2.5 more than doubled, and noise measurements exceeded 50 dBA day and night, within1,288 feet of the site (36).
It is not known if noise and air pollution emitted from O&G well site development exacerbates AF in the large and growing population living near these sites. We are not aware of any studies on this topic. However, studies indicate that living near O&G well sites may impact cardiac conditions associated with AF. Proximity to O&G well sites may affect in-utero heart development (38–42), increase hospitalizations for heart failure (43) in acute myocardial infarction patients (44), and increase augmentation index and blood pressure (45). Our objective is to determine if the burden of AF increases in AF patients living near O&G well site development and identify susceptible subpopulations by employing a novel time-series design and data source in a large population of AF patients using specific O&G metrics. Because air pollution and noise emissions persist in the production period following well site development, we also determine AF exacerbation increases (or persists) after the well site is developed.
Methods
We retrospectively followed 10,961 AF patients in Colorado's All Payer Claims Dataset (COAPCD) before, during, and after development of O&G well sites. Using both an interrupted time series (ITS) and controlled interrupted time series (CTIS) design (Figure 1) (46, 47), we evaluated if living near O&G well site during development exacerbates AF and if AF exacerbation persists after development of the site. We selected an ITS design because of the limited co-variate information available in Colorado's All Payer Claims Dataset (APCD). Because ITS is based on observation of a single population over time, it accounts for between group differences, such as unmeasured confounding, as well as within group characteristics that change slowly over time, secular changes, random fluctuations from one point to the next and regression to mean (46). To control for time-varying trends which do not form part of the underlying trend (e.g., seasonal, regional scale environmental events, and natural progression of AF), we also performed a CITS by adding an unexposed group as recommended by Bernal et al. (47) Per these recommendations, we included and reported results from both the ITS and CITS to provide a greater degree of confidence that an observed association between proximity to development of an O&G well site and AF exacerbation is causal (47). For example, if the CITS analysis indicates an association, but the ITS does not, then there may have been an event affecting AF in the control population that did not affect the population living within one mile. The Colorado Multiple Institutional Review Board approved our study (IRB Protocol Number 17–0692).
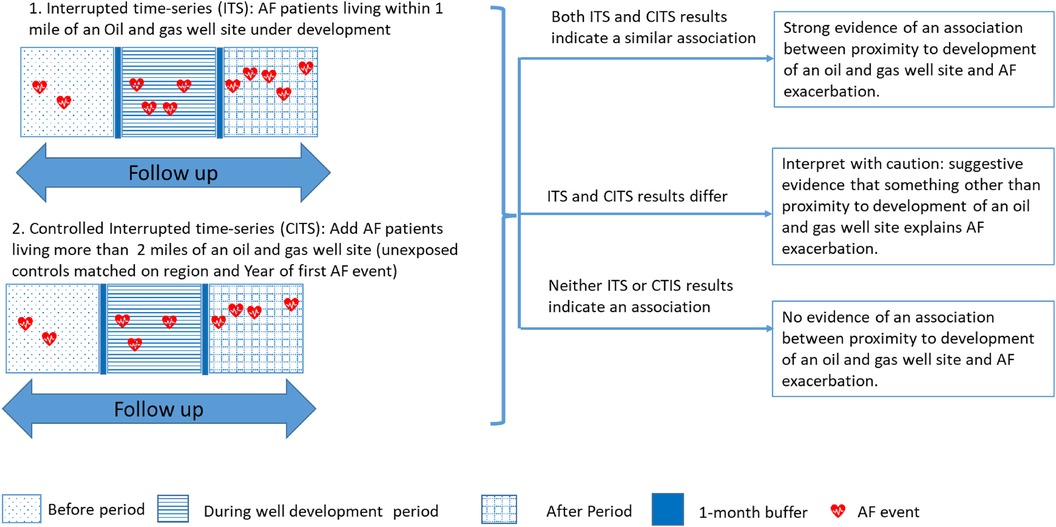
Figure 1 Interrupted time-series study design and assignment of before, during, and after oil and gas well site development period. AF, atrial fibrillation [adapted from Bernal et al. (47)].
Study population
We selected our cohort from the COAPCD, administered by The Center for Improving Value in Health Care. The COAPCD represents approximately 65% of Colorado's fully insured population including claims data from commercial health plans (large group, small group, and individual), Medicare, and Colorado's Medicaid Program beginning in 2009. We included patients in the COAPCD aged 18–100 years with a complete street address that we could geocode, living in a Colorado county with at least one O&G well site developed between 2010 and 2017, and at least one principal diagnosis code for AF or atrial flutter (AFl) between January 1, 2009 and December 31, 2017. From this population, we a priori selected patients at- risk of exposure to air and noise pollution emitted during development of an O&G site (herein referred to as exposed patients) and an unexposed population as follows.
We calculated the distance between each patient's geocoded address and the nearest O&G well site developed between 2010 and 2017 using ArcGIS Desktop 10 as described in the exposure section. We defined patients at-risk of exposure (here to in referred to as at-risk patients) as living within one mile of an O&G site based on documented noise and odor complaints, recent risk assessments, and monitoring studies indicating the potential for air and noise pollution associated with O&G well sites to impact people living within one mile (36, 48–50), as well as a robust literature supporting the use of proximity to O&G well sites as a proxy for exposure (51). Because weather, major air pollution events, and other temporal events that could exacerbate AF vary by region and AF severity may worsen over time, analysis of an location control population was necessary (47). The location control population (here to in referred to as unexposed patients) should be a population not a risk for exposure to air and noise pollution emitted from an O&G site. We selected our unexposed population from AF patients that had no O&G well sites within two miles of their home by frequency matching each at-risk patient to 13 unexposed patients by geographical region to control for regional temporal events (Supplementary Material Table S1) and year of first AF claim in the COAPCD to control for progression of AF severity. Because the spatial extent of stressors from O&G site development is not well understood and may extend beyond 1-mile, we excluded patients living 1–2 miles from an O&G site to clearly distinguish the possibility of exposure to O&G well site development stressors in at-risk patients from unexposed patients.
Exposure
We geocoded street addresses in ArcGIS Desktop 10 using Census TIGER Address Range files from 2019 to create an address locator. For patients that could not be geocoded with ArcGIS Desktop 10, we completed a second geocoding pass with the Google Geocoding API. We obtained geocoded O&G well site locations for all O&G wells developed between 2010 and 2017, the number of wells at each well site, and the dates those wells were developed (spud date, first production date) from the Colorado Oil and Gas Information System (52).
Assuming the street address in the COAPCD is also the residential address, we temporally aligned each matched control set (up to 13 patients) to the development of the O&G well site within one mile of their matched at-risk patient's street address. We defined before, during, and after development periods as follows (Figure 1). The during development period begins on the drilling date (the spud date) of the first well on the site and ends on the first production date of the last well on the site. We then added a one-month buffer to the beginning and end of the during development period to account for well site construction activities prior to drilling and higher potential activities at the beginning of production. The before and after development periods each are equal to the length of the during development period. The before period ends at the beginning of the one-month buffer period preceding the development period. The after period begins at the end of the one-month buffer following the development period.
Exclusions
We excluded patients living 1–2 miles from an O&G site (Figure 2). We next excluded 2,353 patients if the date of their first AF claim occurred later than the end of the after period because there was no evidence that the patient had AF during the follow up period. To reduce errors from unknown losses to follow up, we also excluded 5,626 patients without a claim (of any type) preceding the before period and succeeding the after period as defined in the exposure section. Our final population of 10,961 AF patients includes 1,197 at-risk and 9,764 control patients. A blinded review of claims for 1% of randomly selected at-risk and control patients confirmed 91% (90% at-risk and 94% control) patients were correctly identified as having a primary diagnosis of AF. Insufficient information was available in the remaining 9% of these patients to confirm a primary AF diagnosis.
Outcomes
We followed each patient from the beginning of their specific before period through the end of the after period (here to within referred as follow up) for incidence of an AF episode. We defined an AF episode as any claim, inpatient, outpatient, and emergency room, with a principal diagnostic code for AF or AFI (ICD-9-CM 427.3, or 427.31–2; ICD-10-CM I48.0–4, I48.9, I48.91, or I48.92), excluding AF diagnostic codes associated with an internal normalized ratio procedure (CPT4 85610, 93792, or R79.1). We considered occurrence of multiple AF diagnostic codes in one day or over consecutive days as one event. We also separately evaluated AF episodes associated with an emergency room visit (Supplementary Material Table S2). AF episodes that occurred in the buffer months were not counted.
Statistical analyses
We tested the hypothesis that there is a larger increase in incidence of AF claims during or after development of an O&G site, compared to before development, for at-risk AF patients as follows. We analyzed AF exacerbation risk with a multi-failure survival analysis by applying a Cox proportional hazard model with a robust variance estimator and clustering at the individual patient level (53, 54), using an Efron method for ties (55). We retrospectively followed each patient through their specific follow up period. We first analyzed AF exacerbation risk for only the at-risk patients (ITS) (46, 47). We then analyzed AF exacerbation risk with both the at-risk and unexposed patients (CTIS) (47), by adding an interaction term between exposure (at-risk to control referent) and period (during and after, to before referent) to our model. Parallel trend analysis indicates no difference between the exposed and unexposed populations in the before period, indicating support for the parallel assumption in CITS analysis (Supplementary Material Table S3) (56). Strong evidence of an association between proximity to development of an O&G well site and AF exacerbation is indicated if the ITS and CITS analysis yield hazard ratios (HR) of similar size (Figure 1) (47). We adjusted our model for co-variates associated with AF (biological sex, age at first AF claim in COAPCD, elevation of residence, hypertension, and diabetes) (1), and exposure (duration of well development and geographical region). We considered the direction and magnitude of individual HRs and overarching trends, based on American Statistical Association guidance (57), in both analyses.
We then stratified our population by sex, age quartiles, presence of a co-morbidity (diabetes, hypertension) and geographical region to assess whether the results between groups (e.g., male vs. female) were systematically different. Additionally, we stratified our at-risk patients into distance quartiles to assess the effect of distance from the O&G site on AF exacerbation.
We performed several sensitivity analyses. We evaluated the effect of short and long periods of well development by excluding patients with well duration periods outside the 25th—75th percentile range (75–184 days). To evaluate the impact of potential change of residence over time, we performed an analysis on patients for whom we could confirm that the street address did not change through the follow up period. Because high altitude can exacerbate AF, we performed an analysis on patients living ≤6,000 feet above sea level.
Given the small sample sizes and exploratory nature of the stratified and sensitivity analyses, no adjustments were made for multiple comparisons. All analyses were carried out using SAS 9.4 (SAS Institute, Cary, NC).
Results
Our study population included 1,197 at-risk patients and 9,764 unexposed patients l (Table 1). At-risk patients were more likely to be male, diabetic, and hypertensive than unexposed patients. At-risk patients also had a longer duration in the COAPCD. However, the highest number of total AF claims was observed in the unexposed patients.
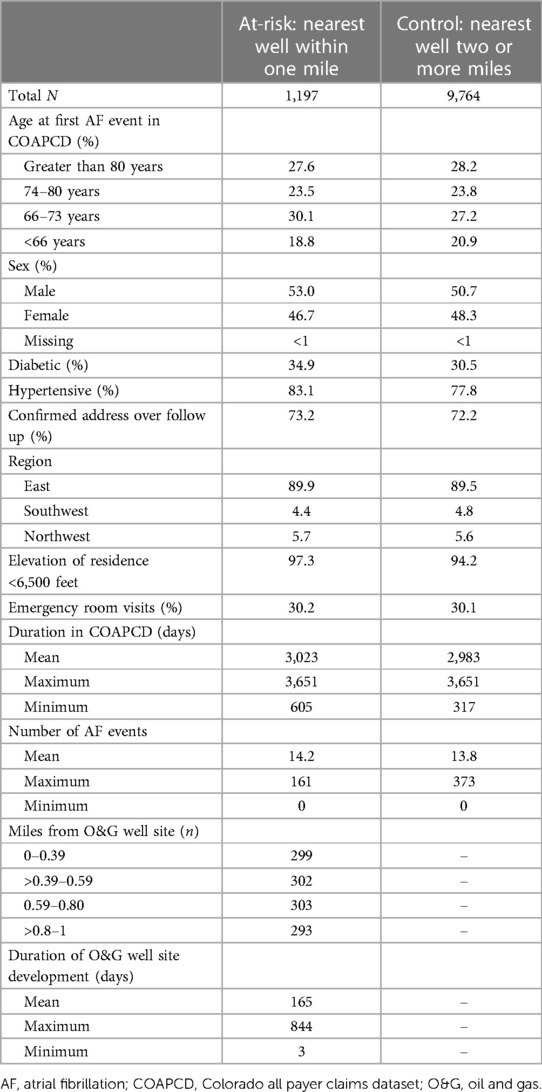
Table 1 Study population characteristics for All payer claims database patients aged 18–100 years living within one mile of an oil and gas well developed in Colorado between 2010 and 2017 or two or more miles from any Colorado oil and natural gas well site.
Table 2 presents the multi-failure survival analysis results for AF exacerbation. The analysis of the study population as a whole does not provide strong evidence of an association between AF exacerbation and proximity to O&G well site development. The ITS analysis indicates that AF exacerbation increases during (HR = 1.13, 95% CI: 0.99, 1.30) and after (HR = 1.19, 95% CI = 1.02, 1.39) well site development, compared to before well development in our total population of at-risk AF patients. With inclusion of unexposed patients in the CITS analyses this association attenuates towards the null during (HR = 1.07, 95% CI: 0.94, 1.22) and after (HR = 1.01, 95% CI: 0.88, 1.16) site development.
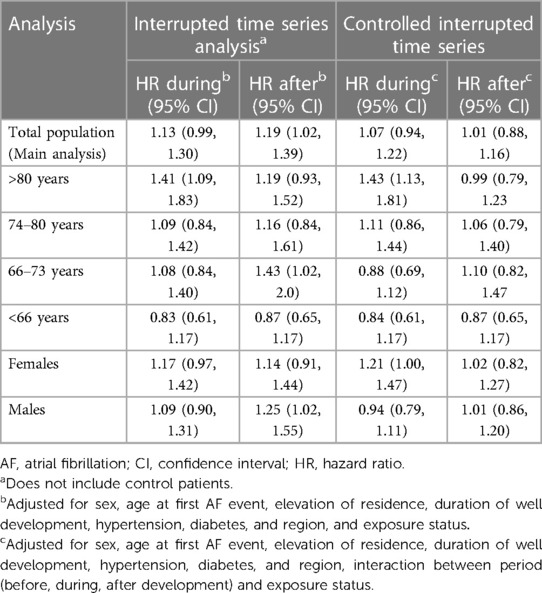
Table 2 Results from multi-failure survival analysis for AF events: hazard ratios for an AF event during and after well development periods compared to before well development.
Stratified analyses indicates that age and possibly biological sex modify the risk of an AF event during O&G well site development (Table 2). In AF patients aged >80 years, ITS and CITS results for the during well development period are similar and indicate that risk for an AF event increases during well development, but not after development. In the during O&G development period, risk of an AF event increased by 43% (HR = 1.43, 95% CI: 1.13, 1.81) in at-risk patients aged >80 years. In younger patients, results attenuated towards the null. In female AF patients, ITS and CITS results for the during well development period are similar and indicate that risk for an AF event increases during well development, but not after development. The risk for an AF event in the during O&G development period increased by 21% (HR = 1.21, 95% CI: 1.00, 1.47) in at-risk female patients. No association was observed for male patients. Stratified analysis indicated that co-morbidities and region of residence did not modify risk (Supplementary Material Table S4).
In stratified analysis by distance quartile, ITS and CTIS results for the total population are similar and indicate increased risk of AF exacerbation during well site development in at-risk patients living within 0.39 miles (2,059 feet) and the increased risk does not persist after development of the well site. We observed a 35% increase in risk for AF events in at-risk patients living within 0.39 miles (2,059 feet) in the during well development period (HR = 1.35, 95% CI: 1.08, 1.69) (Figure 3, Supplementary Material Table S5). We did not observe associations at distances >0.39 miles for the total population. As in the main analysis, both age and sex modified the results. In patients aged >80 years living within 0.39 miles of an O&G development site, the risk of AF event increased by 83% during well development (HR = 1.83, 95% CI: 1.25, 2.66). Additionally, the results for patients aged >80 years indicate a trend of increasing risk of an AF event during well development as distance from the well site decreases and suggest the possibility of increased AF exacerbation risk up to 4,224 feet from the site. In female patients living within 0.39 miles of an oil and gas well development site, risk of AF event increased by 56% (95% CI: 1.13, 2.15) and 36% (95% CI: 0.89, 2.03) during and possibly after well development, respectively.
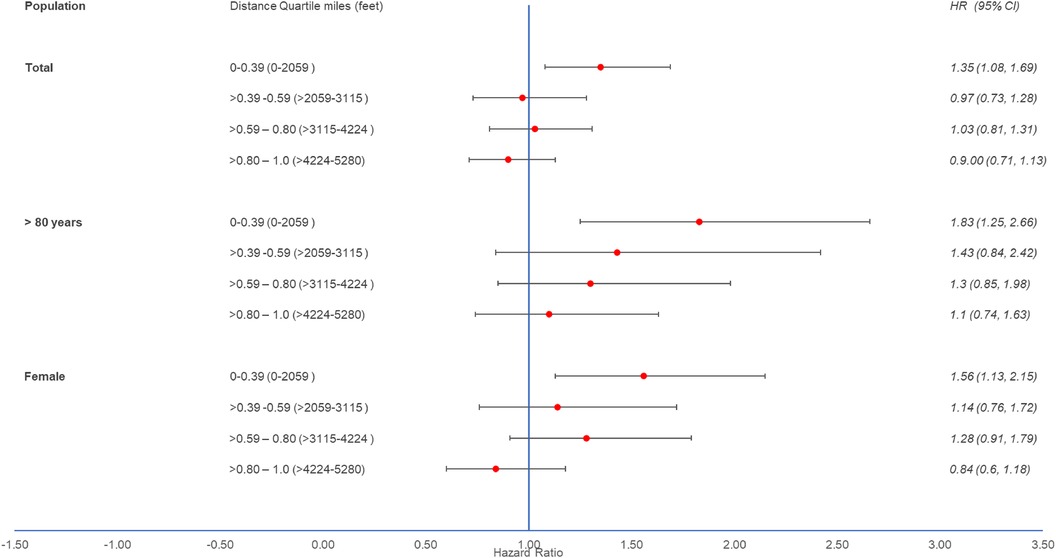
Figure 3 Hazard ratios with 95% confidence intervals from multi-failure survival analysis with control for total population, patients aged >80 years, and patients identified as female by distance quartile from oil and gas well development site: HRs of at-risk to controls for an atrial fibrillation event during O&G well site development compared to before development. HR, hazard ratio; CI, confidence interval.
Table 3 presents the multi-failure survival analysis results for AF exacerbation with an emergency room visit. The analysis of the study population as a whole does not provide strong evidence of an association between AF exacerbation with an emergency room visit and proximity to O&G well site development. The ITS analysis indicates that AF exacerbation with an emergency room visit increases during (HR = 1.57, 95% CI: 0.99, 2.47) and after (HR = 1.80, 95% CI = 1.13, 2.87) well development, compared to before well development. With inclusion of unexposed control patients in the CITS analyses this association attenuates towards the null (HR = 1.11, 95% CI: 0.79, 1.56) or after (HR = 1.24, 95% CI: 0.90, 1.70) O&G well site development.
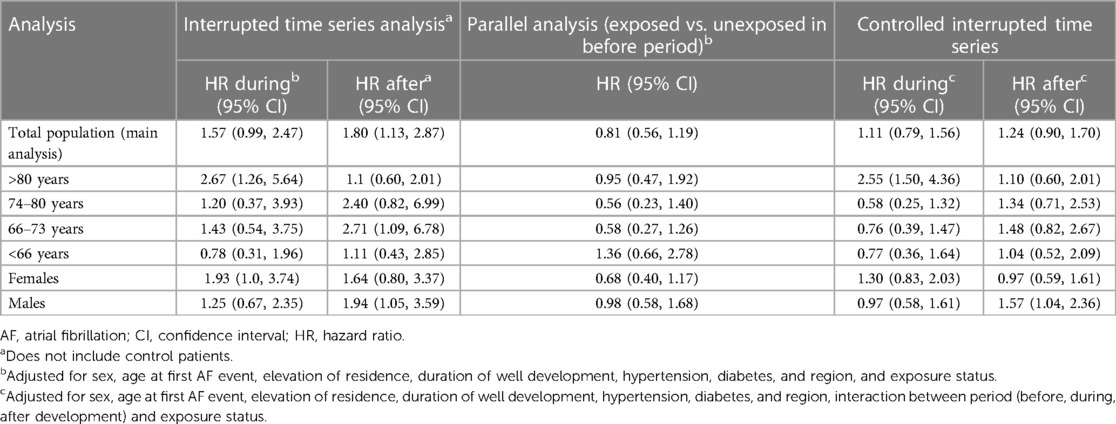
Table 3 Results from multi-failure survival analysis for AF event with an emergency room visit: hazard ratios for an AF event during and after well development periods compared to before well development.
Stratified analyses indicates that age modifies the risk of an AF event with an emergency room visits during O&G well development (Table 3). In at risk patients aged >80 years, ITS and CITS results for the during well development period are similar and indicate that risk of an AF event increases during well development. In the during well development period, risk of an AF event with an emergency room visit doubled (HR = 2.55, 95% CI: 1.50, 4.36) in at-risk patients aged >80 years. The results indicate that the risk does not persist past the well development period and show no increased risk in younger patients. Stratified analysis did not indicate biological sex, co-morbidities, or geographical region as effect modifiers (results not shown).
Sensitivity analyses excluding patients: for whom we could not confirm that the street address did not change over our follow-up period (Supplementary Material Table S6), with well development durations within the 25th to 75th percentile range (Supplementary Material Table S7); and living at an elevation less than 6,000 feet (Supplementary Material Table S8) did not inferentially change our results.
Discussion
Our results provide strong evidence (47) that older AF patients living within 0.39 miles (2,059 feet) of an O&G well site may experience increased AF exacerbation during site development with the possibility of increased AF exacerbation risk up to at least 0.8 miles (4,224) feet from the site, which does not persist past the well development period. Our results also suggest that AF patients identified as female living within 0.39 miles (2,059 feet) of an O&G site may experience increased AF exacerbation during site development, which does not appear to persist past the well development period. We did not observe increases in AF exacerbation in younger AF or male patients. Previous studies indicating that people living near O&G well sites may experience alterations in vascular function associated with AF (45), heart failure exacerbation (43), and increased hospitalization for acute MI (44), as well as exposures to noise and air pollution levels known to affect cardiovascular health (36) support these results. These important and biologically plausible findings contribute further epidemiological evidence that environmental stressors exacerbate AF.
Air and noise pollution emitted during the development of O&G well sites potentially impact all individuals residing in the vicinity of the sites (32). Exposure to noise elicits an acute stress reaction characterized by autonomic nervous system response, specifically, increased sympathetic activity (58), which plays an important role in the initiation and maintenance of AF (59). On the molecular level, beta adrenergic stimulation triggers an intracellular signaling cascade that can lead to intracellular calcium overload creating a particularly arrhythmogenic environment that promotes triggered activity. Resulting depolarizations generate spontaneous ectopy. Simultaneously, enhanced automaticity, promoted by increased circulating catecholamines, also leads to focal ectopic atrial activity. Both triggered activity and enhanced automaticity are believed to be the primary drivers for AF initiation. This stress reaction has been observed in response to road traffic noise (60); thus, it is plausible that exposure to stressful noise levels may induce AF in susceptible individuals. Additionally, alterations in autonomic tone, inflammation, oxidative stress, and changes in intracardiac filling pressures are known triggers for AF (58, 61–68) and are reported in response to PM2.5 exposure (15, 18, 69–75). Exposure to PM2.5 has been associated with increased blood pressure and acute alteration in vascular function, which may contribute to hypertension, an AF risk factor (1, 73, 76–79).
Interestingly, our results indicate that living near development of an O&G well site has a greater impact on older and female AF patients. Other studies also have observed that older adults living in close proximity to O&G well sites may bear greater health and mortality risks than younger adults (43, 80). Additionally, prior studies report that both women and the elderly are at higher risk of mortality and CV mortality when exposed to elevated PM2.5 levels (81). Our findings may be explained by age- and gender-related changes in response to physiologic stressors. Significantly higher levels of cortisol have been observed in women compared to age-matched men and older vs. younger subjects when exposed to psychological or cognitive challenges (82). It is plausible that older subjects spend more time at home, increasing the duration of exposure (83).
Our observation that AF exacerbation risk does not to persist past the well development period indicates that the increased risk is transitory in nature. A transitory increase in AF exacerbation risk could worsen AF patient acute outcomes, as evidenced by the increased risk for AF claims associated with an emergency room visit.
Our study benefited from an efficient design that accounts for unmeasured confounding, accurate definition of before, during, and after O&G well site development periods, and the availability of sequential measures of AF diagnoses and related morbidities in the COAPCD. Additionally, our temporal control design features allowed us to account for risk factors that drive AF development in an accumulating manner and time-varying variables such as season and regional air pollution events (e.g., wildfires).
Nonetheless, our study had some limitations. While our CITS design allowed us to account static environmental stressors and time varying environmental stressors a the regional level, it did not account for changing environmental stressors a the local level that may have occurred during the follow up period,, such as construction activities and development of other O&G well sites further than the closet site,. This may have biased result towards or away from the null. Assuming the street address in the COAPCD is the residential address and the possibility for change of residence in our study cohort may introduce exposure misclassification. However, our sensitivity analysis on patients for whom we could confirm the street address over the follow up period indicates that exposure misclassification from change in residential address had little effect on our results (Supplementary Material Table S6). It also is possible that some AF and co-morbidity claims were misdiagnosed. Our claim review confirmed that most (91%) patients had plausible AF diagnoses, with similar results for at-risk and control patients. Thus, this is mostly a concern for null results. Not all AF incidents may result in an COAPCD claim and not all AF patients are included in the COAPCD. Therefore, our results, may underrepresent the true incidence of AF. This too is mostly a concern for null results. It is important to appreciate that our outcome is an AF claim in the COAPCD and not new onset AF. Therefore, our results apply to the prevalence of AF. Because we did not include AF patients with addresses that could not be geocoded, our results may not be generalizable to the whole Colorado AF patient population. Because noise and air pollution measures were not available for this retrospective study, we could not elucidate specific associations between noise or air pollution and AF. Because the COAPCD includes only 65% of Colorado's population, our results may not represent the 35% of Coloradans that are uninsured or privately insured.
The prospect that proximity to O&G well site development, a significant noise and air pollution source, increases AF exacerbation risk requires attention. Health care providers should be aware of the increased risk for AF during O&G well site development for their older and female patients and provide appropriate patient education to help mitigate risk. Additionally, these findings support development of mitigation strategies and regulations to protect the health of populations living near O&G well sites. While this study advances understanding on relationships between residential proximity to development of O&G well sites and AF exacerbation, a future prospective cohort study that can follow populations for AF over the course of O&G well site development will be necessary to understand the etiological relationships between specific environmental stressors, such as noise and air pollution, and incidence and severity of AF events.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: The dataset was obtained from the Colorado All Payer Claims Dataset thru a data use agreement with the Center for Improving Value in Health Care. A data use agreement with Center for Improving Value in Health Care is required to access the data. Requests to access these datasets should be directed to Eddy Costa: ECosta@CIVHC.org.
Ethics statement
The studies involving humans were approved by Colorado Multi-Institutional Review Board, University of Colorado. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
LM: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. WA: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Software, Writing – original draft, Writing – review & editing. BA: Conceptualization, Formal Analysis, Funding acquisition, Validation, Writing – original draft, Writing – review & editing. CT: Conceptualization, Funding acquisition, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
Research reported in this publication was supported by the National Heart, Lung, And Blood Institute of the National Institutes of Health under Award Number R21HL145337 and the Center for Improving Value in Health Care (CIVHC). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or CIVHC.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fepid.2024.1379271/full#supplementary-material
References
1. Lip GYH, Fauchier L, Freedman SB, Van Gelder I, Natale A, Gianni C, et al. Atrial fibrillation. Nat Rev Dis Primers. (2016) 2:16016. doi: 10.1038/nrdp.2016.16
2. Williams BA, Honushefsky AM, Berger PB. Temporal trends in the incidence, prevalence, and survival of patients with atrial fibrillation from 2004 to 2016. Am J Cardiol. (2017) 120(11):1961–5. doi: 10.1016/j.amjcard.2017.08.014
3. Schnabel RB, Yin X, Gona P, Larson MG, Beiser AS, McManus DD, et al. 50 year trends in atrial fibrillation prevalence, incidence, risk factors, and mortality in the framingham heart study: a cohort study. Lancet. (2015) 386(9989):154–62. doi: 10.1016/S0140-6736(14)61774-8
4. Colilla S, Crow A, Petkun W, Singer DE, Simon T, Liu X. Estimates of current and future incidence and prevalence of atrial fibrillation in the U. S. adult population. Am J Cardiol. (2013) 112(8):1142–7. doi: 10.1016/j.amjcard.2013.05.063
5. Jackson SL, Tong X, Yin X, George MG, Ritchey MD. Emergency department, hospital inpatient, and mortality burden of atrial fibrillation in the United States, 2006 to 2014. Am J Cardiol. (2017) 120(11):1966–73. doi: 10.1016/j.amjcard.2017.08.017
6. Centers for Disease Control and Prevention. Atrial Fibrillation Fact Sheet. Available online at: https://www.cdc.gov/dhdsp/data_statistics/fact_sheets/fs_atrial_fibrillation.htm (accessed January 31, 2018).
7. Shao Q, Liu T, Korantzopoulos P, Zhang Z, Zhao J, Li G. Association between air pollution and development of atrial fibrillation: a meta-analysis of observational studies. Heart Lung. (2016) 45(6):557–62. doi: 10.1016/j.hrtlng.2016.08.001
8. Monrad M, Sajadieh A, Christensen JS, Ketzel M, Raaschou-Nielsen O, Tjønneland A, et al. Long-term exposure to traffic-related air pollution and risk of incident atrial fibrillation: a cohort study. Environ Health Perspect. (2017) 125(3):422–7. doi: 10.1289/EHP392
9. Monrad M, Sajadieh A, Christensen JS, Ketzel M, Raaschou-Nielsen O, Tjonneland A, et al. Residential exposure to traffic noise and risk of incident atrial fibrillation: a cohort study. Environ Int. (2016) 92-93:457–63. doi: 10.1016/j.envint.2016.04.039
10. Andrade J, Khairy P, Dobrev D, Stanley N. The clinical profile and pathophysiology of atrial fibrillation: relationships among clinical features, epidemiology, and mechanisms. Circ Res. (2014) 114(9):1453–8. doi: 10.1161/CIRCRESAHA.114.303211
11. Xue X, Hu J, Xiang D, Li H, Jiang Y, Fang W, et al. Hourly air pollution exposure and the onset of symptomatic arrhythmia: an individual-level case-crossover study in 322 Chinese cities. CMAJ. (2023) 195(17):E601–e611. doi: 10.1503/cmaj.220929
12. Liao D, Shaffer ML, He F, Rodriguez-Colon S, Wu R, Whitsel EA, et al. Fine particulate air pollution is associated with higher vulnerability to atrial fibrillation–the APACR study. J Toxicol Environ Health A. (2011) 74(11):693–705. doi: 10.1080/15287394.2011.556056
13. Link MS, Luttmann-Gibson H, Schwartz J, Mittleman MA, Wessler B, Gold DR, et al. Acute exposure to air pollution triggers atrial fibrillation. J Am Coll Cardiol. (2013) 62(9):816–25. doi: 10.1016/j.jacc.2013.05.043
14. Rich DQ, Mittleman MA, Link MS, Schwartz J, Luttmann-Gibson H, Catalano PJ, et al. Increased risk of paroxysmal atrial fibrillation episodes associated with acute increases in ambient air pollution. Environ Health Perspect. (2006) 114(1):120–3. doi: 10.1289/ehp.8371
15. Rich DQ, Freudenberger RS, Ohman-Strickland P, Cho Y, Kipen HM. Right heart pressure increases after acute increases in ambient particulate concentration. Environ Health Perspect. (2008) 116(9):1167–71. doi: 10.1289/ehp.11230
16. Solimini AG, Renzi M. Association between air pollution and emergency room visits for atrial fibrillation. Int J Environ Res Public Health. (2017) 14(6):661. doi: 10.3390/ijerph14060661
17. Vencloviene J, Babarskiene RM, Dobozinskas P, Dedele A, Lopatiene K, Ragaisyte N. The short-term associations of weather and air pollution with emergency ambulance calls for paroxysmal atrial fibrillation. Environ Sci Pollut Res Int. (2017) 24(17):15031–43. doi: 10.1007/s11356-017-9138-7
18. Buteau S, Goldberg MS. A structured review of panel studies used to investigate associations between ambient air pollution and heart rate variability. Environ Res. (2016) 148:207–47. doi: 10.1016/j.envres.2016.03.013
19. Thacher JD, Poulsen AH, Hvidtfeldt UA, Raaschou-Nielsen O, Ketzel M, Jensen SS, et al. Long-term exposure to transportation noise and risk for atrial fibrillation: a danish nationwide cohort study. Environ Res. (2022) 207:112167. doi: 10.1016/j.envres.2021.112167
20. Dahlquist M, Frykman V, Stafoggia M, Qvarnström E, Wellenius GA, Ljungman PLS. Short-term ambient air pollution exposure and risk of atrial fibrillation in patients with intracardiac devices. Environ Epidemiol. (2022) 6(4):e215. doi: 10.1097/EE9.0000000000000215
21. Dahlquist M, Frykman V, Kemp-Gudmunsdottir K, Svennberg E, Wellenius GA, Ljungman PLS. Short-term associations between ambient air pollution and acute atrial fibrillation episodes. Environ Int. (2020) 141:105765. doi: 10.1016/j.envint.2020.105765
22. Sadlonova M, Senges J, Nagel J, Celano C, Klasen-Max C, Borggrefe M, et al. Symptom severity and health-related quality of life in patients with atrial fibrillation: findings from the observational ARENA study. J Clin Med. (2022) 11(4):1140. doi: 10.3390/jcm11041140
23. Münzel T, Gori T, Babisch W, Basner M. Cardiovascular effects of environmental noise exposure. Eur Heart J. (2014) 35(13):829–36. doi: 10.1093/eurheartj/ehu030
24. Jarup L, Babisch W, Houthuijs D, Pershagen G, Katsouyanni K, Cadum E, et al. Hypertension and exposure to noise near airports: the HYENA study. Environ Health Perspect. (2008) 116(3):329–33. doi: 10.1289/ehp.10775
25. Pirrera S, De Valck E, Cluydts R. Nocturnal road traffic noise: a review on its assessment and consequences on sleep and health. Environ Int. (2010) 36(5):492–8. doi: 10.1016/j.envint.2010.03.007
26. Carrington MJ, Trinder J. Blood pressure and heart rate during continuous experimental sleep fragmentation in healthy adults. Sleep. (2008) 31(12):1701–12. doi: 10.1093/sleep/31.12.1701
27. Wang Q, Xi B, Liu M, Zhang Y, Fu M. Short sleep duration is associated with hypertension risk among adults: a systematic review and meta-analysis. Hypertens Res. (2012) 35:1012. doi: 10.1038/hr.2012.91
28. Sabanayagam C, Shankar A. Sleep duration and cardiovascular disease: results from the national health interview survey. Sleep. (2010) 33(8):1037–42. doi: 10.1093/sleep/33.8.1037
30. Czolowski ED, Santoro RL, Srebotnjak T, Shonkoff SB. Toward consistent methodology to quantify populations in proximity to oil and gas development: a national spatial analysis and review. Environ Health Perspect. (2017) 125(8):086004. doi: 10.1289/EHP1535
31. McKenzie LM, Allshouse WB, Burke T, Blair BD, Adgate JL. Population size, growth, and environmental justice near oil and gas wells in Colorado. Environ Sci Technol. (2016) 50(21):11471–80. doi: 10.1021/acs.est.6b04391
32. Adgate JL, Goldstein BD, McKenzie LM. Potential public health hazards, exposures and health effects from unconventional natural gas development. Environ Sci Technol. (2014) 48(15):8307–20. doi: 10.1021/es404621d
33. King GE. Hydraulic Fracturing 101: What Every Representative, Environmentalist, Regulator, Reporter, Investor, University Researcher, Neighbor and Engineer Should Know About Estimating Frac Risk and Improving Frac Performance in Unconventional Gas and Oil Wells. Woodlands, TX: Semantics Scholar (2012).
34. Hecobian A, Clements AL, Shonkwiler KB, Zhou Y, MacDonald LP, Hilliard N, et al. Air toxics and other volatile organic compound emissions from unconventional oil and gas development. Environ Sci Technol Lett. (2019) 6(12):720–6. doi: 10.1021/acs.estlett.9b00591
35. Radtke C, Autenrieth DA, Lipsey T, Brazile WJ. Noise characterization of oil and gas operations. J Occup Environ Hyg. (2017) 14(8):659–67. doi: 10.1080/15459624.2017.1316386
36. Allshouse WB, McKenzie LM, Barton K, Brindley S, Adgate JL. Community noise and air pollution exposure during the development of a multi-well oil and gas pad. Environ Sci Technol. (2019) 53(12):7126–85. doi: 10.1021/acs.est.9b00052
37. Witter RZ, McKenzie L, Stinson KE, Scott K, Newman LS, Adgate J. The use of health impact assessment for a community undergoing natural gas development. Am J Public Health. (2013) 103(6):1002–10. doi: 10.2105/AJPH.2012.301017
38. McKenzie LM, Guo R, Witter RZ, Satvitz DA, Newman LS, Adgate JL. Birth outcomes and maternal residential proximity to natural gas development in rural Colorado. Environ Health Perspect. (2014) 122:412–7. doi: 10.1289/ehp.1306722
39. McKenzie LM, Allshouse W, Daniels S. Congenital heart defects and intensity of oil and gas well site activities in early pregnancy. Environ Int. (2019) 132:104949. doi: 10.1016/j.envint.2019.104949
40. Janitz AE, Dao HD, Campbell JE, Stoner JA, Peck JD. Association between benzene and congenital anomalies in Oklahoma, 1997–2009. Occup Environ Med. (2018) 75(11):822–9. doi: 10.1136/oemed-2018-105054
41. Tang IW, Langlois PH, Vieira VM. Birth defects and unconventional natural gas developments in Texas, 1999–2011. Environ Res. (2021) 194:110511. doi: 10.1016/j.envres.2020.110511
42. Willis MD, Carozza SE, Hystad P. Congenital anomalies associated with oil and gas development and resource extraction: a population-based retrospective cohort study in Texas. J Expo Sci Environ Epidemiol. (2023) 33(1):84–93. doi: 10.1038/s41370-022-00505-x
43. McAlexander TP, Bandeen-Roche K, Buckley JP, Pollak J, Michos ED, McEvoy JW, et al. Unconventional natural gas development and hospitalization for heart failure in Pennsylvania. J Am Coll Cardiol. (2020) 76(24):2862–74. doi: 10.1016/j.jacc.2020.10.023
44. Denham A, Willis MD, Croft DP, Liu L, Hill EL. Acute myocardial infarction associated with unconventional natural gas development: a natural experiment. Environ Res. (2021) 195:110872. doi: 10.1016/j.envres.2021.110872
45. McKenzie LM, Crooks J, Peel JL, Blair BD, Brindley S, Allshouse WB, et al. Relationships between indicators of cardiovascular disease and intensity of oil and natural gas activity in northeastern Colorado. Environ Res. (2019) 170:56–64. doi: 10.1016/j.envres.2018.12.004
46. Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. (2017) 46(1):348–55. doi: 10.1093/ije/dyw098
47. Lopez Bernal J, Cummins S, Gasparrini A. The use of controls in interrupted time series studies of public health interventions. Int J Epidemiol. (2018) 47(6):2082–93. doi: 10.1093/ije/dyy135
48. McKenzie LM, Blair B, Hughes J, Allshouse WB, Blake NJ, Helmig D, et al. Ambient nonmethane hydrocarbon levels along Colorado’s northern front range: acute and chronic health risks. Environ Sci Technol. (2018) 52(8):4514–25. doi: 10.1021/acs.est.7b05983
49. Holder C, Hader J, Avanasi R, Hong T, Carr E, Mendez B, et al. Evaluating potential human health risks from modeled inhalation exposures to volatile organic compounds emitted from oil and gas operations. J Air Waste Manage Assoc. (2019) 69:1503–24. doi: 10.1080/10962247.2019.1680459
50. Weisner ML, Allshouse WB, Erjavac BW, Valdez AP, Vahling JL, McKenzie LM. Health symptoms and proximity to active multi-well unconventional oil and gas development sites in the city and county of broomfield, Colorado. Int J Environ Res Public Health. (2023) 20(3):2634. doi: 10.3390/ijerph20032634
51. Deziel NC, Brokovich E, Grotto I, Clark CJ, Barnett-Itzhaki Z, Broday D, et al. Unconventional oil and gas development and health outcomes: a scoping review of the epidemiological research. Environ Res. (2020) 182:109124. doi: 10.1016/j.envres.2020.109124
52. Commission COaGC. Colorado Oil and Gas Information System. Available online at: https://cogcc.state.co.us/cogis/ (accessed June 30, 2014).
53. Wei LJ, Lin DY, Weissfeld L. Regression analysis of multivariate incomplete failure time data by modeling marginal distributions. J Am Stat Assoc. (1989) 84(408):1065–73. doi: 10.1080/01621459.1989.10478873
54. Allison PD. Survival Analysis Using SAS: A Practical Guide Second Edition. 2nd ed. Cary, NC USA: SAS Institute Inc. (2010).
55. Lin W, Zhu T, Xue T, Peng W, Brunekreef B, Gehring U, et al. Association between changes in exposure to air pollution and biomarkers of oxidative stress in children before and during the Beijing olympics. Am J Epidemiol. (2015) 181(8):575–83. doi: 10.1093/aje/kwu327
56. Nianogo RA, Benmarhnia T, O'Neill S. A comparison of quasi-experimental methods with data before and after an intervention: an introduction for epidemiologists and a simulation study. Int J Epidemiol. (2023) 52(5):1522–33. doi: 10.1093/ije/dyad032
57. Wasserstein RL, Lazar NA. The ASA statement on p-values: context, process, and purpose. Am Stat. (2016) 70(2):129–33. doi: 10.1080/00031305.2016.1154108
58. Ulrich-Lai YM, Herman JP. Neural regulation of endocrine and autonomic stress responses. Nat Rev Neurosci. (2009) 10(6):397–409. doi: 10.1038/nrn2647
59. Chen P-S, Chen LS, Fishbein MC, Lin S-F, Nattel S. Role of the autonomic nervous system in atrial fibrillation. Pathophysiol Ther. (2014) 114(9):1500–15. doi: 10.1161/CIRCRESAHA.114.303772
60. Babisch W. The noise/stress concept, risk assessment and research needs. Noise and Health. (2003) 5(18):1–11.12631430
61. Aviles RJ, Martin DO, Apperson-Hansen C, Houghtaling PL, Rautaharju P, Kronmal RA, et al. Inflammation as a risk factor for atrial fibrillation. Circulation. (2003) 108(24):3006–10. doi: 10.1161/01.CIR.0000103131.70301.4F
62. Hu Y-F, Chen Y-J, Lin Y-J, Chen S-A. Inflammation and the pathogenesis of atrial fibrillation. Nat Rev Cardiol. (2015) 12:230. doi: 10.1038/nrcardio.2015.2
63. Otto CM. Heartbeat: inflammatory biomarkers in atrial fibrillation. Heart. (2016) 102(7):485–6. doi: 10.1136/heartjnl-2016-309537
64. Gutierrez A, Van Wagoner DR. Oxidant and inflammatory mechanisms and targeted therapy in AF: an update. J Cardiovasc Pharmacol. (2015) 66(6):523–9. doi: 10.1097/FJC.0000000000000313
65. Li J, Solus J, Chen Q, Rho YH, Milne G, Stein CM, et al. The role of inflammation and oxidative stress in atrial fibrillation. Heart Rhythm. (2010) 7(4):438–44. doi: 10.1016/j.hrthm.2009.12.009
66. Van Wagoner DR. Oxidative stress and inflammation in atrial fibrillation: role in pathogenesis and potential as a therapeutic target. J Cardiovasc Pharmacol. (2008) 52(4):306–13. doi: 10.1097/FJC.0b013e31817f9398
67. Samman Tahhan A, Sandesara PB, Hayek SS, Alkhoder A, Chivukula K, Hammadah M, et al. Association between oxidative stress and atrial fibrillation. Heart Rhythm. (2017) 14(12):1849–55. doi: 10.1016/j.hrthm.2017.07.028
68. Lam CSP, Rienstra M, Tay WT, Liu LCY, Hummel YM, van der Meer P, et al. Atrial fibrillation in heart failure with preserved ejection fraction: association with exercise capacity, left ventricular filling pressures, natriuretic peptides, and left atrial volume. JACC Heart Fail. (2017) 5(2):92–8. doi: 10.1016/j.jchf.2016.10.005
69. Fiordelisi A, Piscitelli P, Trimarco B, Coscioni E, Iaccarino G, Sorriento D. The mechanisms of air pollution and particulate matter in cardiovascular diseases. Heart Fail Rev. (2017) 22(3):337–47. doi: 10.1007/s10741-017-9606-7
70. Cole-Hunter T, Weichenthal S, Kubesch N, Foraster M, Carrasco-Turigas G, Bouso L, et al. Impact of traffic-related air pollution on acute changes in cardiac autonomic modulation during rest and physical activity: a cross-over study. J Expo Sci Environ Epidemiol. (2015) 26:133. doi: 10.1038/jes.2015.66
71. Peters A, Fröhlich M, Döring A, Immervoll T, Wichmann HE, Hutchinson WL, et al. Particulate air pollution is associated with an acute phase response in men. Results from the MONICA–Augsburg study. Eur Heart J. (2001) 22(14):1198–204. doi: 10.1053/euhj.2000.2483
72. Kelly FJ, Fussell JC. Role of oxidative stress in cardiovascular disease outcomes following exposure to ambient air pollution. Free Radic Biol Med. (2017) 110:345–67. doi: 10.1016/j.freeradbiomed.2017.06.019
73. Brook RD, Brook JR, Urch B, Vincent R, Rajagopalan S, Silverman F. Inhalation of fine particulate air pollution and ozone causes acute arterial vasoconstriction in healthy adults. Circulation. (2002) 105(13):1534–6. doi: 10.1161/01.CIR.0000013838.94747.64
74. Møller P, Christophersen DV, Jacobsen NR, Skovmand A, Gouveia ACD, Andersen MHG, et al. Atherosclerosis and vasomotor dysfunction in arteries of animals after exposure to combustion-derived particulate matter or nanomaterials. Crit Rev Toxicol. (2016) 46(5):437–76. doi: 10.3109/10408444.2016.1149451
75. Cascio WE. Proposed pathophysiologic framework to explain some excess cardiovascular death associated with ambient air particle pollution: insights for public health translation. Biochim Biophys Acta. (2016) 1860(12):2869–79. doi: 10.1016/j.bbagen.2016.07.016
76. Brook RD, Rajagopalan S. Particulate matter, air pollution, and blood pressure. J Am Soc Hypertens. (2009) 3(5):332–50. doi: 10.1016/j.jash.2009.08.005
77. Dales R, Liu L, Szyszkowicz M, Dalipaj M, Willey J, Kulka R, et al. Particulate air pollution and vascular reactivity: the bus stop study. Int Arch Occup Environ Health. (2007) 81(2):159–64. doi: 10.1007/s00420-007-0199-7
78. Rundell KW, Hoffman JR, Caviston R, Bulbulian R, Hollenbach AM. Inhalation of ultrafine and fine particulate matter disrupts systemic vascular function. Inhal Toxicol. (2007) 19(2):133–40. doi: 10.1080/08958370601051727
79. Nurnberger J, Keflioglu-Scheiber A, Opazo Saez AM, Wenzel RR, Philipp T, Schafers RF. Augmentation index is associated with cardiovascular risk. J Hypertens. (2002) 20(12):2407–14. doi: 10.1097/00004872-200212000-00020
80. Li L, Dominici F, Blomberg AJ, Bargagli-Stoffi FJ, Schwartz JD, Coull BA, et al. Exposure to unconventional oil and gas development and all-cause mortality in medicare beneficiaries. Nat Energy. (2022) 7(2):177–85. doi: 10.1038/s41560-021-00970-y
81. Franklin M, Zeka A, Schwartz J. Association between PM2.5 and all-cause and specific-cause mortality in 27 US communities. J Expo Sci Environ Epidemiol. (2007) 17(3):279–87. doi: 10.1038/sj.jes.7500530
82. Seeman TE, Singer B, Wilkinson CW, McEwen B. Gender differences in age-related changes in HPA axis reactivity. Psychoneuroendocrinology. (2001) 26(3):225–40. doi: 10.1016/S0306-4530(00)00043-3
Keywords: atrial fibrillation, oil and natural gas development, cohort study, environmental epidemiology, hydraulic fracturing, air pollution, noise pollution
Citation: McKenzie LM, Allshouse WB, Abrahams B and Tompkins C (2024) Oil and gas development exposure and atrial fibrillation exacerbation: a retrospective study of atrial fibrillation exacerbation using Colorado's all payer claims dataset. Front. Epidemiol. 4:1379271. doi: 10.3389/fepid.2024.1379271
Received: 30 January 2024; Accepted: 3 June 2024;
Published: 19 June 2024.
Edited by:
Alexandra Schneider, Helmholtz Association of German Research Centres (HZ), GermanyReviewed by:
Matteo Renzi, Local Health Authority Rome 1, ItalyMassimo Stafoggia, Regional Health Service of Lazio, Italy
© 2024 McKenzie, Allshouse, Abrahams and Tompkins. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lisa M. McKenzie, lisa.mckenzie@cuanschutz.edu
 Lisa M. McKenzie
Lisa M. McKenzie William B. Allshouse1
William B. Allshouse1 Christine Tompkins
Christine Tompkins