- 1School of Public Health, Wachemo University, Hossana, Ethiopia
- 2National Data Management and Analytics Center for Health, Ethiopian Public Health Institute, Addis Ababa, Ethiopia
Background: Undiagnosed hypertension is a major public health problem causing severe cardiovascular disorders that are responsible for a high proportion of morbidities and mortalities, especially among adults living in low-income countries. However, there is a paucity of information that describes its epidemiology in Ethiopia. This study aimed to assess the prevalence of undiagnosed hypertension and associated factors among adults in Durame town, southern Ethiopia.
Methods: A community-based cross-sectional study was conducted from July to September 2022. Data were collected from 526 randomly selected adults aged ≥18 years using a pre-tested questionnaire. The binary logistic regression models were used to identify factors associated with undiagnosed hypertension.
Results: The prevalence of undiagnosed hypertension among adults in Durame town, southern Ethiopia, was found to be 14.0% (95% CI: 11.2–17.1). Family history of hypertension [AOR = 6.9, 95% CI: (3.62, 13.27)], drinking too much alcohol [AOR = 5.7, 95% CI: (2.97, 10.75)], physical inactivity [AOR = 2.5, 95% CI: (1.34, 4.73)], consuming street foods regularly [AOR = 2.8, 95% CI: (1.28, 6.01)], and seeking healthcare for hypertensive symptoms without serious illness [AOR = 2.4, 95% CI: (1.28, 4.56)] were significantly associated with developing undiagnosed hypertension.
Conclusion: The study has revealed that one in seven adults had undiagnosed hypertension in the study area. Thus, interventions to prevent hypertension should target increasing awareness among people with a family history of hypertension, controlling excessive alcohol consumption, promoting physical exercise, regulating street food markets, and improving the health-seeking behavior of adults in urban settings.
Background
Hypertension is a state of systemic blood pressure defined by a systolic blood pressure of at least 140 mmHg and/or a diastolic blood pressure of at least 90 mmHg on two or more consecutive readings (1). In 2019, there were an estimated 1.28 billion adults aged 30–79 years with hypertension globally; about two-thirds of them live in low- and middle-income countries (2). Studies have revealed that the risk of developing hypertension among people living in Subsaharan Africa is increasing, possibly due to poor socioeconomic conditions, weak health infrastructure, an increasing rate of urbanization, a sedentary lifestyle, and poor nutrition (3).
There are significant gaps in hypertension diagnosis, treatment, and control strategies in Subsaharan Africa (4). A large proportion of people with hypertension remain undiagnosed for years, causing premature deaths and serious health complications such as heart failure, renal failure, stroke, and myocardial infarction. The pooled prevalence of undiagnosed hypertension was estimated to be 30%. Of those with hypertension, about 73% were unaware of their hypertensive status, 82% were not receiving treatment, and 93% did not control their blood pressure (5).
Prevention and control of hypertension continue to be a major public health challenge in Ethiopia due to a lack of transportation, a poor referral system, misconceptions about symptoms, a lack of financial and social support, and traditional healing practices (6). According to the 2016 national survey, about 77% of the participants reported that their blood pressure was never measured (7). In 2019, the hypertension treatment rate among women was only 16%, the sixth lowest rate globally (8). Moreover, the magnitude of the risk factors for hypertension, like obesity, physical inactivity, stress, unhealthy diets, tobacco use, and alcohol consumption, is increasing, especially among urban communities (9). However, there is a paucity of studies that explain the epidemiology of undiagnosed hypertension in the country. Therefore, this study was intended to assess the prevalence of undiagnosed hypertension and associated factors among adults in Durame town, southern Ethiopia. The study will provide the latest information for policymakers, planners, and programmers to design appropriate hypertension prevention and control strategies.
Methods
Study design and area
This community-based cross-sectional study was conducted in Durame town, southern Ethiopia, from July to September 2022. The town had an estimated population of 52,513 living in three kebeles (the smallest administrative unit in Ethiopia). There is one general hospital, three health centers, nine clinics, one health post, and nine drug stores (10).
Participants and data collection
All randomly selected adults aged ≥18 years who lived in the study area for at least six months without a history of hypertension and did not visit any health facility for a blood pressure check in the past year were included in the study. Adults who were unable to respond to the interview questions and/or take physical measurements were excluded from the study. Data on socio-demographic characteristics, family history of hypertension, behavioral characteristics, physical activity, dietary practices, and health-seeking behaviors were collected using a pre-tested questionnaire.
After completing the interview, the data collectors measured the participants' weight and height. The weight was measured by using a portable digital weight scale and recorded to the nearest 0.1 kg. The height was measured by using a portable Stadiometer and recorded to the nearest 0.1 cm. The participants were instructed to stand on the footplate with their backs to the Stadiometer, their legs straight, their arms at their sides, and their shoulders relaxed, and touch the Stadiometer at their heels, buttocks, upper back, and head. Then, the headpiece was lowered until it touched the crown of the head firmly, compressing the hair.
Blood pressure was measured using a standard mercury sphygmomanometer with a cuff size that covers two-thirds of the upper arm. No exercise, smoking, coffee, or tea were allowed 30 min before the measurement. The participants were instructed to sit on the chair with their legs uncrossed, feet on the floor, back supported, arm supported on the desk to keep the upper arm at the same level as the heart, and an empty bladder guaranteed. The upper arm was uncovered two inches above the elbow crease. A cuff is placed on the brachial artery in the upper arm. Three blood pressure measurements were taken 10 min apart in a sitting position. Finally, the average of the three readings was taken to determine the blood pressure status of the respondents.
Data quality control
The questionnaire was translated into Amharic, the official language, and back to English to maintain consistency in meaning. The interview questionnaire was pilot tested on 26 adults living in Teza Agara that had characteristics nearly similar to Durame town in order to identify the interview questions and physical measurements that needed adjustments. The data collectors and supervisors received intensive training for two days on how to obtain ethical consent, conduct interviews, measure weight, height, and blood pressure, and keep records. The collected data were checked for consistency and completeness on a daily basis.
Sample size calculation
Epi Info version 7 was used to determine the minimum sample size of 526 by taking the 28.8% expected proportion of undiagnosed hypertension (9), 5% margin of error, 95% confidence level, 1.5 design effects, and 10% non-response rate.
Sampling procedure
Multistage sampling was used to recruit the study participants. In the first stage, four ketenes (villages in the kebeles) were selected from a pool of 10 ketenes by using the lottery method. The town administrative office provided the list of households in each selected ketene, which was used as a sampling frame. At the second stage, a total of 526 samples were proportionally allocated to each selected ketene (i.e., 100 for Arada ketene, 144 for Teza ketene, 139 for Arada Girige ketene, and 143 for Abonsa ketene). At the last stage, the households with the eighth interval in the sampling frame of each ketene were selected for the data collection. If more than one eligible adult was present in the selected household, one household member was selected randomly using the lottery method.
Data management and statistical analyses
The data were entered into EpiData version 4.6 and analyzed on SPSS version 26. Frequency and percentage were used to present categorical data, whereas mean and standard deviation were used to present continuous data. All independent variables were fitted separately into a bivariate logistic regression model to estimate the degree of association with undiagnosed hypertension among adults. Then, variables with a p-value < 0.25 were exported to a multivariable logistic regression model to control confounders. The model's fitness was checked by the Hosmer-Lemeshow goodness-of-fit test. A multicollinearity test was also done by examining the standard error (SE) for the b coefficient. A SE > 2 indicates the presence of multicollinearity among independent variables. In this case, SE was less than 2 for all variables. The statistical significance was declared by using an odds ratio (OR) with a 95% confidence interval (CI).
Operational definitions
Undiagnosed hypertension: refers to a systolic blood pressure of ≥140 mmHg or a diastolic blood pressure of ≥90 mmHg and/or both (1), without a prior history of hypertension, and having not visited any health facility for a blood pressure check in the past year. The average of three sphygmomanometer readings taken 10 min apart in a sitting position was used to determine the blood pressure status.
Prehypertension: refers to a systolic blood pressure of 120–139 mmHg or a diastolic pressure of 80–89 mmHg and/or both (1).
Normal blood pressure: refers to a systolic blood pressure between 90 and 120 mmHg and a diastolic blood pressure between 60 and 80 mmHg (1).
Body mass index: refers to a quotient of weight divided by height squared (kg/m2).
Drank too much alcohol: refers to adults who drank over 330 ml of beer (5% alcohol), 330 to 750 ml of wine (20%–25% alcohol), or 200–250 ml of local alcohol, like tella (8%–15% alcohol), tej (10%–13% alcohol), or arake (40%–45% alcohol), per week (1).
Family history of hypertension: refers to a history of hypertension in the father, mother, or both as reported by the respondent.
Low consumption of fruits and/or vegetables: refers to adults who ate fruits and/or vegetables less than five times per day. One serving is equivalent to one apple, orange, or banana, or three tablespoons of cooked vegetables (1).
Physical inactivity: refers to adults who undertake less than 150 min of moderate-intensity physical activity per week, less than 75 min of vigorous-intensity physical activity per week, or a combination of both (11).
Street foods: refers to foods and beverages that were prepared and sold by vendors in streets and public places for consumption.
Results
Socio-demographic characteristics
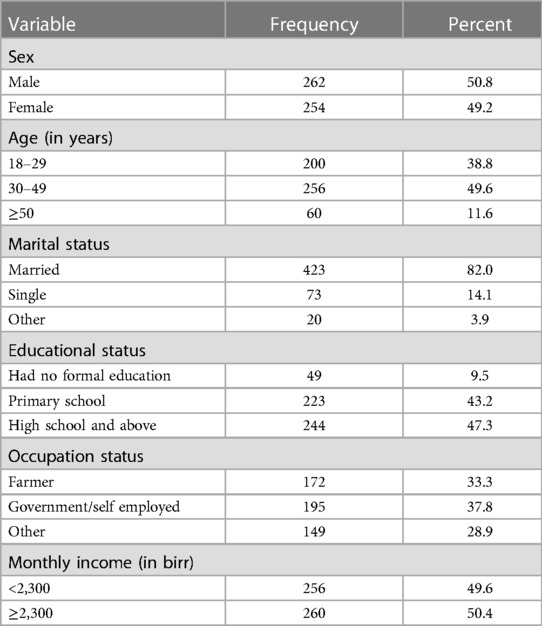
A total of 516 adults participated in the study, making the response rate 98.1%. Of whom, 50.8% were males. The mean age with a standard deviation was 34 ± 11. Nearly half, 49.6%, of the participants belonged to the age group of 30–49 years. The majority, 82.0%, of the participants were married. About 47.3% of the participants had a high school or higher certificate. Regarding occupation, the proportion of government/self-employed and farmers was 37.8% and 33.3%, respectively. About half, 49.6%, of the participants earned a monthly income of less than 2,300 birr (Table 1).
Behavioural characteristics
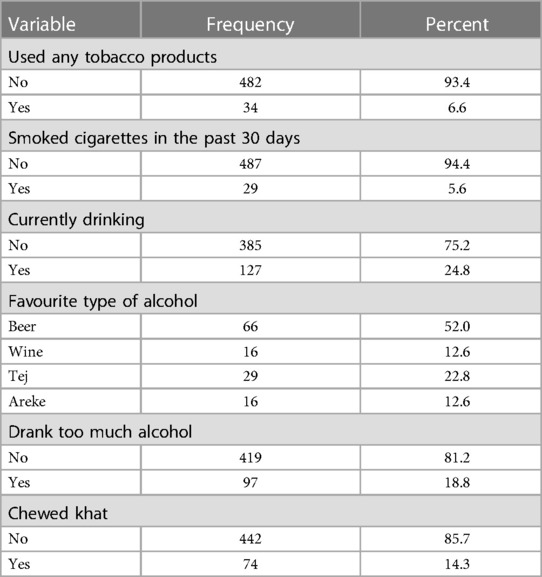
The majority, 93.4%, of the participants did not use any tobacco products. A nearly similar proportion, 94.4%, of them did not smoke cigarettes in the past 30 days. About three-fourths of the participants did not drink alcohol during the data collection. Beer was a favourite type of alcoholic drink for nearly half, 52.0%, of the participants. The majority, 81.2%, of the participants did not drink too much alcohol. The proportion of those who did not chew khat was 85.7% (Table 2).
Participants' knowledge about hypertension
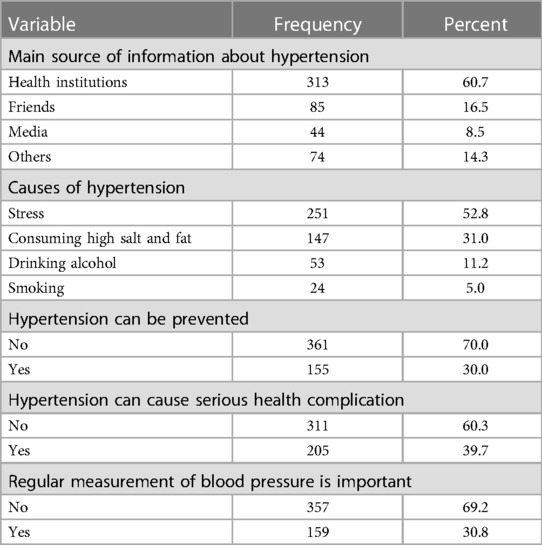
All adults who participated in this study heard about hypertension. The main source of information about hypertension was health institutions, which accounted for 60.7%. The major cause of hypertension was reported to be stress (52.8%), followed by high salt and fat consumption (30%). More than two-thirds, or 70%, of the participants reported that hypertension could not be prevented. The majority, 60.3%, of the participants did not report that hypertension could cause serious health complications. Less than one-third, or 30.8%, of the participants reported that regular measurement of blood pressure was important to prevent hypertension (Table 3).
Prevalence of undiagnosed hypertension
The mean systolic blood pressure with a standard deviation was 113 ± 23 mmHg, and the mean diastolic blood pressure with a standard deviation was 76 ± 10 mmHg. The distribution of blood pressure was observed to be higher than these among participants in the age group of 30–49 years, attended primary school and below, had a family history of hypertension, physically inactive, drank too much alcohol, drank tej, areke, wine and beer, chewed khat, and consumed street foods regularly (Table 4). The prevalence of undiagnosed hypertension was 14% (95% CI: 11.2–17.1%), whereas the prevalence of prehypertension was 10.1% (95% CI: 7.8–12.8%).
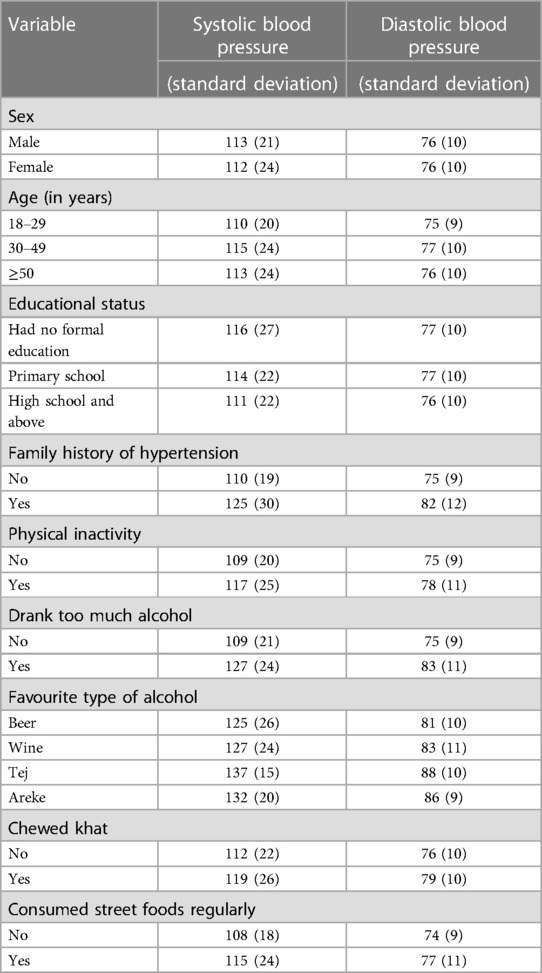
Table 4. Distribution of systolic and diastolic blood pressure of adults in Durame town, southern Ethiopia, 2022.
Factors associated with undiagnosed hypertension
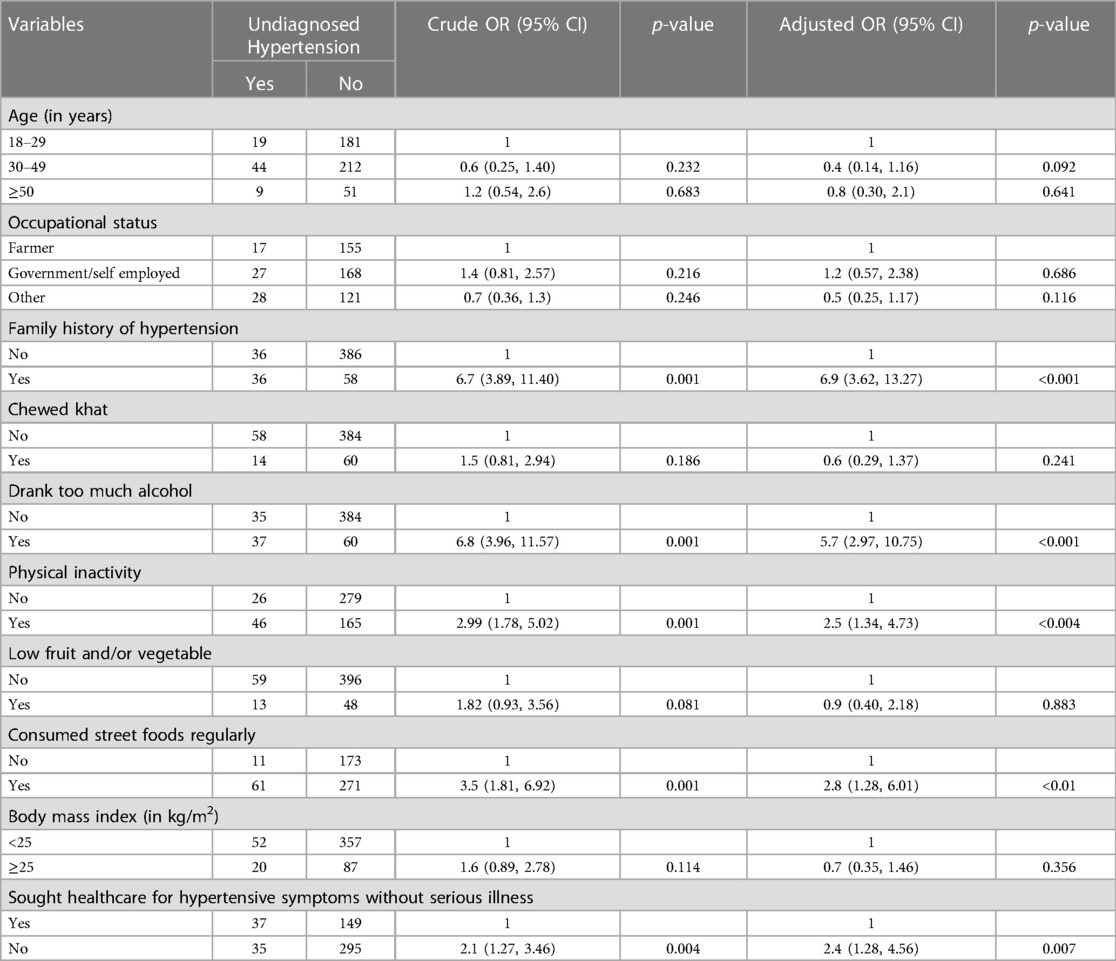
Age, occupation status, family history of hypertension, drinking too much alcohol, chewing khat, physical inactivity, low consumption of fruits and/or vegetables, body mass index, consuming street foods, and healthcare for hypertensive symptoms without serious illness showed association with undiagnosed hypertension in the bivariate analysis at p-value < 0.25. Family history of hypertension [Adjust OR (AOR) = 6.9, 95% CI: (3.62, 13.27)], drinking too much alcohol [AOR = 5.7, 95% CI: (2.97, 10.75)], physical inactivity [AOR = 2.5, 95% CI: (1.34, 4.73)], consuming street foods regularly [AOR = 2.8, 95% CI: (1.28, 6.01)], and seeking healthcare for hypertensive symptoms without serious illness [AOR = 2.4, 95% CI: (1.28, 4.56)] remained significant in the multivariable logistic regression model (Table 5).
Discussion
This study aimed to assess the prevalence of undiagnosed hypertension and associated factors among adults in Durame town, southern Ethiopia, in 2022. The study has revealed that the prevalence of undiagnosed hypertension was 14.0% (95% CI: 11.2–17.1%). Moreover, family history of hypertension, drinking too much alcohol, physical inactivity, consuming street foods regularly, and seeking healthcare for hypertensive symptoms without serious illness were found to be significantly associated with undiagnosed hypertension.
The prevalence of undiagnosed hypertension observed in this study was consistent with other studies conducted in Addis Ababa city, 13.25%; Hawasa city, 12.3%; Dano district, 14.6%; and Debre-Markos town, 12.7% (12–15). The possible explanation for the observed similarity might be that the study participants in all the studies were adults over the age of 18 years. People in similar age groups might share similar lifestyles, health-seeking behavior, and socio-economic contexts. However, the observed prevalence was lower than reports from Gunchire district, 18.8%; Bahir-Dar city, 24.8%; Wolaita-Sodo town, 28.8%; Sudan, 38.2%; and Lebanon, 42.69% (9, 16–19). The disparity might be due to the fact that different standards were used to define the cut-off point for hypertension. The previous studies used the World Health Organization pre-hypertension stage to define the hypertension cut-off point; however, this cut-off point was proposed to define hypertension among individuals with comorbidities (20). The socio-demographic and ethnic differences among the populations could also determine the risk of developing hypertension. Furthermore, the prevalence of undiagnosed hypertension identified in this study was higher than that reported from Gilgal-Gibe field research site (7.5%), India (10.1%), the USA (6.5%), and Iran (4.8%) (21–24). The Gilgel-Gibe study was conducted in rural settings and might have a protective effect against developing hypertension (25). Socio-economic, access to healthcare facilities, and lifestyle differences could explain the observed variation.
This study has revealed that there is a significant association between family history of hypertension and undiagnosed hypertension. The odds of developing hypertension among adults who had a family history of hypertension were seven times higher among those who had not. This was consistent with reports from other locations in Ethiopia, like Hawassa city, Dano district, and Debre-Markos town (12, 13, 15, 26). This could be explained by the fact that family members might share similar risk factors and inherit genetic traits for developing hypertension. Thus, community-based interventions to reduce the burden of hypertension should include creating awareness among people with a family history of hypertension.
This study has revealed that the odds of developing hypertension among those adults who drank too much alcohol were nearly six times higher compared to those who did not. This was in agreement with studies from Ethiopia and Japan (16, 27–30). Hence, disseminating health information on the harmful effects of excessive alcohol consumption, restricting alcohol advertisements, and decreasing the availability and accessibility of alcohol through increasing alcohol taxation and regulating alcohol sales can be recommended.
Insufficient physical activity is one of the major modifiable risk factors for hypertension. In this study, the odds of developing hypertension among adults who did not engage in sufficient physical activity were about three times higher than those who did. Previous studies from Bahir-Dar city, Gunchire district, and Hosanna town supported this evidence (9, 19, 31). Physical activity is not at a moderate level in urban areas of Ethiopia because of increasing urbanization, and people usually use taxes and motor cycles to move from place to place (7, 32). This suggests that urban public health programs should target promoting physical exercise among community members to reduce the risk of developing hypertension.
This study has indicated that the odds of developing hypertension among adults who consumed street foods regularly were about three times higher compared to those who did not. This was consistent with reports from Tanzania and Italy (33, 34). This could be due to the fact that street foods usually have a high quantity of carbohydrate, saturated fat, and sodium; thus, consuming these foods might contribute to the development of undiagnosed hypertension (35). This indicated that there is a need to regulate street food markets in urban settings.
The odds of developing hypertension among adults who did not seek healthcare for hypertensive symptoms without serious illness were about two times higher than those who did. This was consistent with studies from Dano and Gunchire districts, Ethiopia (9, 13). Many people living in resource-limited countries practice prolonged self-treatment as the first step in the health-seeking process. Therefore, strengthening the health extension program can improve the health-seeking behaviour of people living in resource-limited settings.
This study has limitations. Establishing a cause-and-effect relationship between the independent variables and hypertension was difficult because of the cross-sectional nature of the study. The other limitation was that the study measured blood pressure three times in one visit, which differed from the clinical practice guidelines recommendation of two visits (1, 36). Moreover, the blood pressure measurement was limited to only behavioural and physical measurements of the participants and did not include biochemical measurements.
Conclusion
The study has revealed that one in seven adults had undiagnosed hypertension in the study area. Thus, interventions to prevent hypertension should target increasing awareness of people with family histories of hypertension, controlling excessive alcohol consumption, promoting physical exercise, regulating street food markets, and improving the health-seeking behavior of adults in urban settings.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by The study was approved by the Institutional Review Board of Wachemo University via the School of Graduate Studies (Ref No: 840/14). Informed consent was obtained from the study participants. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Authors contributions
AS, ST, LA, and MS conceived, designed, and conducted the study. ST, LA, and MS supervised and provided mentorship. AS, ST, LA, and MS involved in the analysis and interpretation of the findings. ST wrote the manuscript. All authors contributed to the article and approved the submitted version.
Acknowledgments
The authors wish to thank the Durame town health office for logistic and administrative support and the data collectors for their support in making this study possible. They also extend their deepest gratitude to the study participants.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Federal Ministry of Health. Guidelines on clinical and programmatic management of major non-communicable diseases. Addis Ababa, Ethiopia: Federal Ministry of Health (2016).
2. Jaffar S, Ramaiya K, Karekezi C, Sewankambo N, Jaffar S, Ramaiya K, et al. Controlling diabetes and hypertension in sub-saharan Africa: lessons from HIV programs. Lancet. (2021) 398(10306):1111–3. doi: 10.1016/S0140-6736(21)01731-1
3. Guwatudde D, Nankya-Mutyoba J, Kalyesubula R, Laurence C, Adebamowo C, Ajayi I, et al. The burden of hypertension in sub-saharan Africa: a four-country cross-sectional study. BMC Public Health. (2015) 15:1211. doi: 10.1186/s12889-015-2546-z
4. Chow CK, Teo KK, Rangarajan S, Islam S, Gupta R, Avezum A, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. (2013) 310(9):959–68. doi: 10.1001/jama.2013.184182
5. Ataklte F, Erqou S, Kaptoge S, Taye B, Echouffo-Tcheugui JB, Kengne AP. Burden of undiagnosed hypertension in sub-saharan Africa: a systematic review and meta-analysis. Hypertension. (2015) 65(2):291–8. doi: 10.1161/HYPERTENSIONAHA.114.04394
6. Federal Ministry of Health. National strategic plan for the prevention and control of major non-communicable diseases: Strategy on prevention and control of cardiovascular diseases, diabetes mellitus, chronic kidney diseases and chronic respiratory diseases. Addis Ababa, Ethiopian: Federal Ministry of Health (2020).
7. Ethiopian Public Health Institute. Ethiopia STEPS report on risk factors for chronic non-communicable diseases and prevalence of selected NCDs. Addis Ababa, Ethiopian: Ethiopian Public Health Institute (2016).
9. Demamu H, Abinet A, Hilina G, Nega Y. Undiagnosed hypertension and its associated factors among adult people living in southern Ethiopia: evidence from gunchire woreda of gurage zone. J Hypertens Manag. (2021) 7(1):1–8. doi: 10.23937/2474-3690/1510063
10. Kembata-Tembaro Zone Health Office. Kedida-Gamela district tuberculosis report. Durame, Kembata-Tembaro Zone: Kembata-Tembaro Zone Health Office (2020).
11. Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World health organization 2020 guidelines on physical activity and sedentary behavior. Br J Sports Med. (2020) 54:1451–62. doi: 10.1136/bjsports-2020-102955
12. Wachamo D, Geleta D, Woldesemayat EM. Undiagnosed hypertension and associated factors among adults in hawela tula sub-city, Hawassa, Southern Ethiopia: a community-based cross-sectional study. Risk Manag Healthc Policy. (2020) 13:2169–77. doi: 10.2147/RMHP.S276955
13. Regea F, Birhanu A, Shibiru A. Distribution of risks and prevalence of unscreened hypertension among adults living in rural of dano district, west shewa, oromia, Ethiopia, 2020: a community-based cross-sectional study. Clin Epidemiol Glob Health. (2022) 13:100908. doi: 10.1016/j.cegh.2021.100908
14. Getachew F, Dirar A, Solomon D. Prevalence of undiagnosed hypertension and associated factors among residents in gulele Sub-City, Addis Ababa, Ethiopia. J Community Med Health Educ. (2018) 8(1):590. doi: 10.4172/2161-0711.1000590
15. Essa E, Shitie D, Yirsaw MT, Wale MZ. Undiagnosed hypertension and associated factors among adults in dabre-markos town, northwest Ethiopia: a community-based cross-sectional study. SAGE Open Med. (2022) 10:20503121221094223. doi: 10.1177/20503121221094223
16. Ayalew TL, Wale BG, Zewudie BT. Burden of undiagnosed hypertension and associated factors among adult population in Wolaita-Sodo town, Wolaita zone, Southern Ethiopia. BMC Cardiovasc Disorders. (2022) 22:293. doi: 10.1186/s12872-022-02733-3
17. Kanj H, Khalil A, Kossaify A. Predictors of undiagnosed and uncontrolled hypertension in the local community of byblos, Lebanon. Health Serv Insights. (2018) 11:1178632918791576. doi: 10.1177/1178632918791576
18. Bushara SO, Noor SK, Elmadhoun WM, Sulaiman AA, Ahmed MH. Undiagnosed hypertension in a rural community in Sudan and association with some features of the metabolic syndrome: how serious is the situation? Ren Fail. (2015) 37(6):1022–6. doi: 10.3109/0886022X.2015.1052951
19. Dejenie M, Kerie S, Reba K. Undiagnosed hypertension and associated factors among bank workers in bahir-dar city, northwest Ethiopia, 2020: a cross-sectional study. PLoS One. (2021) 16(5):e0252298. doi: 10.1371/journal.pone.0252298
20. World Health Organization. Guideline for the pharmacological treatment of hypertension in adults. Geneva, Switzerland: World Health Organization (2021).
21. Undavalli VK, Madala P, Narni H. Prevalence of undiagnosed hypertension: a public health challenge. Int J Community Med Public Health. (2018) 5(4):1366–70. doi: 10.18203/2394-6040.ijcmph20180974
22. Birlew T, Alemseged F. Risk factors for hypertension among adults. An analysis of survey data on chronic non-communicable disease at gilgel-gibe field research center, southwest Ethiopia. Sci J Publ Health 2015; 3(2):281–90. doi: 10.11648/j.sjph.20150302.29
23. Park S, Gillespie C, Baumgardner J, Yang Q, Valderrama AL, Fang J, et al., Modeled state-level estimates of hypertension prevalence and undiagnosed hypertension among US adults during 2013-2015. J Clin Hypertens. (2018) 20(10):1395–410. doi: 10.1111/jch.13388
24. Dolatabadi AA, Motamedi M, Hatamabadi H, Alimohammadi H. Prevalence of undiagnosed hypertension in the emergency department. Trauma Mon. (2014) 19(1):e7328. doi: 10.5812/traumamon.7328
25. Kibret KT, Mesfin YM. Prevalence of hypertension in Ethiopia: a systematic meta-analysis. Public Health Rev. (2015) 36:14. doi: 10.1186/s40985-015-0014-z
26. Paulose T, Nkosi ZZ, Endriyas M. Prevalence of hypertension and its associated factors in Hawassa city administration, southern Ethiopia: a community-based cross-sectional study. PLoS One. (2022) 17(3):e0264679. doi: 10.1371/journal.pone.0264679
27. Dereje N, Earsido A, Temam L, Abebe A. Uncovering the high burden of hypertension and its predictors among adult population in Hosanna town, southern Ethiopia: a community-based cross-sectional study. BMJ open. (2020) 10:e035823. doi: 10.1136/bmjopen-2019-035823
28. Zewudie BT, Tenaw SG, Solomon M, Mesfin Y, Abebe H, Mekonnen Z, et al. The magnitude of undiagnosed hypertension and associated factors among HIV-positive patients attending antiretrovarial therapy clinics of butajira general hospital, Gurage zone, southern Ethiopia. SAGE Open Med. (2022) 10:20503121221094454. doi: 10.1177/20503121221094454
29. Nawata K, Matsumoto A, Kajihara R, Kimura M. Evaluadtion of the distribution and factors affecting blood pressure using medical check-up data in Japan. Health. (2017) 9:124–37. doi: 10.4236/health.2017.91009
30. Nawata K. An analysis of blood pressure situations in Japan using the large-scale medical check-up dataset. Health. (2021) 13:736–56. doi: 10.4236/health.2021.137057
31. Asfaw LS, Ayanto SY, Gurmamo FL. Hypertension and its associated factors in Hossana town, southern Ethiopia. BMC Res Notes. (2018) 11:306. doi: 10.1186/s13104-018-3435-1
32. Tekalegn Y, Solomon D, Sahiledengle B, Beressa G, Desta F, Tolcha F, et al. Level of physical activity and its associated factors among adults in southeast Ethiopia: a community-based cross-sectional study. BMJ Open. (2022) 12(11):e063333. doi: 10.1136/bmjopen-2022-063333
33. Kagaruki GB, Mahande MJ, Kimaro GD, Ngadaya ES, Mayige TM, Selemani M, et al.. Prevalence and correlates of cardio-metabolic risk factors among regular street food consumers in Dar es Salaam, Tanzania. Diabetes Metab Syndr Obes. (2021) 14:1011–24. doi: 10.2147/DMSO.S287999
34. Buscemi S, Barile A, Maniaci V, Batsis JA, Mattina A, Verga S. Characterization of street food consumption in Palermo: possible effects on health. Nutr. (2011) 10:119. doi: 10.1186/1475-2891-10-119
35. Nonato IL, Minussi LOA, Pascoal GB, De-Souza DA. Nutritional issues concerning street foods. J Clin Nutr Diet. (2016) 2:1–7. doi: 10.4172/2472-1921.100014
Keywords: alcohol consumption, family history of hypertension, health-seeking behavior, hypertension, physical activity, street foods, undiagnosed hypertension
Citation: Suliman A, Tadesse S, Abute L and Selamu M (2023) Prevalence of undiagnosed hypertension and associated factors among adults in Durame town, Southern Ethiopia: a cross-sectional study. Front. Epidemiol. 3:1205857. doi: 10.3389/fepid.2023.1205857
Received: 14 April 2023; Accepted: 16 November 2023;
Published: 27 November 2023.
Edited by:
Tobias Kurth, Charité University Medicine Berlin, GermanyReviewed by:
Suhaily Mohd Hairon, Universiti Sains Malaysia Health Campus, MalaysiaKazumitsu Nawata, Hitotsubashi University, Japan
Enver Envi Roshi, University of Medicine, Albania
© 2023 Suliman, Tadesse, Abute and Selamu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sebsibe Tadesse c2JzYnRhZGVzc2U5MEBnbWFpbC5jb20=
 Abebe Suliman1
Abebe Suliman1 Sebsibe Tadesse
Sebsibe Tadesse