
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Epidemiol., 11 January 2023
Sec. Cardiovascular Epidemiology
Volume 2 - 2022 | https://doi.org/10.3389/fepid.2022.1044111
This article is part of the Research TopicWomen In Cardiovascular EpidemiologyView all 4 articles
Background: Sleep is important for maintaining the metabolic processes in the body, and hence, disruption in sleep leads to metabolic derangement and accelerated atherosclerosis. The effect of sleep duration on subclinical atherosclerosis has been examined in several studies; however, data regarding sleep quality is lacking. The study aimed to assess the association between sleep quality and carotid intima-media thickness among healthy young doctors.
Materials and Methods: This was an observational cross-sectional study among 110 healthy young resident doctors. Anthropometric data were recorded and morning fasting venous blood samples were collected to assess fasting blood sugar, lipid profile and glycosylated haemoglobin (HbA1c). Pittsburgh Sleep Quality Index and Berlin questionnaire assessed subjective sleep quality and risk for obstructive sleep apnea, respectively. Carotid ultrasonography was done to detect the intima-media thickness.
Results: Average age of the participants was 26.45 (±1.43) years, and 51.8% were male. Self-reported poor sleep quality was found in 54.5%. Carotid intima-media thickness (CIMT) was increased among 44.5% of participants. In the multivariate analysis, only poor sleep quality appeared to be associated with higher CIMT (P < 0.001, OR = 7.4; 95% CI = 2.70–20.32). When different components of sleep quality was analyzed through multivariate logistic regression, subjective sleep onset latency (>30 min), sleep efficiency (<85%) and sleep disturbance was found to be associated with the increased CIMT.
Conclusion: Poor sleep quality, especially prolonged sleep onset latency, poor sleep efficiency, and sleep disturbance are associated with increased carotid intima-media thickness among healthy young adults.
Medical residents spend long hours in patient care as well as study, resulting in sleep deprivation (1). A decent amount of literature has discussed sleep deprivation among medical residents and its adverse consequences on social, health and occupational aspects (1). Sleep deprivation has been found to impair cognition, prolong reaction time, enhance errors, sleepiness, irritability, reduce empathy, motor vehicle accidents, and increase the use of hypnotics and alcohol (1). Optimal sleep duration is important as both long (>9 h/day) as well as short (<7 h/day) have been found to increase the risk for cardiovascular disorders, including systemic hypertension, diabetes mellitus, metabolic syndrome and mortality from cardiovascular disorders (2). Both long and short sleep duration has been found to increase the carotid intima-media thickness (CIMT), however recent literature gives a contrasting evidence showing no association between sleep duration and CIMT (3–6).
Sleep duration and sleep quality represent two different aspects of sleep-related health (7). Optimal duration of sleep for an individual has been conceptualized as one which provides a feeling of “rested” upon awakening and allow one to perform well during the day with a considerable inter-individual variation (8). Considering this, it may be possible that reported short or long sleep duration in previous studies was physiological, at least for a few participants (3–5). Hence, assessing sleep duration without considering sleep quality may introduce bias in the studies correlating CIMT with sleep duration (3–5, 7).
While sleep duration is determined by an interplay of genetic, environmental and health-related factors, including the use of exogenous chemicals, viz., addictive substances and medications, sleep quality is a broader concept (8). Determinants of sleep quality among young adults include physical activity, quality of social interactions, stimulants intake, stress, sleep-wake patterns, sleep onset latency, wake after sleep onset, number of awakenings and total sleep time (9, 10). Sleep quality is also affected by sleep disorders like obstructive sleep apnea, insomnia and restless legs syndrome (11–13). Hence, sleep quality provides a comprehensive assessment of sleep and daytime functions compared to sleep duration. Sleep quality is a subjective phenomenon, and literature suggests that actigraphy and polysomnography data has a poor correlation with subjectively reported sleep quality (10, 14).
Carotid intima media thickness (CIMT) is a reliable marker of early atherosclerosis and hence a predictor for atherosclerotic cardiovascular disease (15, 16). The evidence till date have been derived from middle to old age population with comorbidities (5, 15, 17–19) except a few study which is done among young adult (20, 21). Increasing age has been a consistent independent risk factor for increased CIMT (18, 21, 22).
Literature regarding the assessment of sleep quality among medical residents is limited (23–26). Available studies show that 45% to 90% of medical residents report poor sleep quality. Poor sleep quality has been associated with fatigue, memory lapses, perceived stress, heartburn, irritable bowel syndrome and depression among medical residents (23–25). Considering the inclusive nature of “sleep quality”, it is possible that sleep quality might influence the CIMT among medical residents, as has been observed among middle-aged women (27). However, such data is not available. We hypothesized that poor sleep quality is associated with greater CIMT in medical residents, an otherwise healthy young population, similar to what has been reported among middle-aged women even after excluding potential confounders.
The study was a cross-sectional descriptive study conducted among apparently healthy resident doctors in a teaching hospital. The study was conducted after getting approval from the Institutional Ethics committee (Letter number-****/IEC/20/857). Based on the previous literature, the sample size was calculated using the prevalence of sleep disturbance (7%) among resident doctors of a teaching institute (28). Considering 95% confidence interval and 5% absolute precision, the estimated sample size was 100. 10% of participants were added to address non-response.
The study was planned in a teaching hospital to recruit healthy young participants. The postgraduate residents from all the departments of same year accounting to 121, were listed. It helped minimising heterogeneity among study participants in terms of duty hours, shift duty, and level of stress. All the residents were below 30 years.. After the “line listing” of all resident doctors meeting the age criteria, participant selection was made using a “simple random sampling” method [sequence generated by open access computer-based software programme (QuickCalcs http://www.graphpad.com/quickcalcs/)].
Eligible study participants were approached and explained about the rationale of the study. Written informed consent was obtained from those agreeing to participate. However, those with a known history of diabetes, hypertension, coronary artery disease and cerebrovascular disease were excluded. A family history of cardiovascular disease was also obtained from the participants, and those having a positive family history were considered to have an increased risk of atherosclerosis.
Demographic details included age, gender and marital status. Participants were individually assessed for their anthropometric measurements. Weight (Kg), height(cm), waist circumference and waist-hip ratio were measured as per standard guidelines (29). Body mass index (BMI) was calculated, and groups were made as per guidelines for the Asian population (30). Blood pressure measurement was done using an aneroid sphygmomanometer following the auscultatory method for each participant. The measurement was taken twice, and the average was recorded. Participants having systolic blood pressure(SBP) ≥ 140 mmHg or diastolic blood pressure(DBP) ≥ 90 mmHg on two occasions a few days apart were considered to have hypertension (31).
Subjective sleep quality was assessed using Pittsburgh Sleep Quality Index (PSQI) (32). It differentiates “poor” from “good” sleep quality based on a global score which is calculated using seven components- subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medications, and daytime dysfunction over the last month. Global PSQI score ≤5 indicates good sleep quality, while a score of >5 shows poor sleep quality. Using a cut-off score of 5, PSQI has a sensitivity of 89.6% and specificity of 86.5%, respectively, to differentiate between good and poor sleep quality (32).
OSA risk was assessed using the Berlin questionnaire(BQ) as the sleep laboratory was closed during the Corona virus disease-19 (COVID-19) pandemic (33). It consists of 3 categories which ultimately classifies the participants into low risk or high risk of sleep apnea. BQ has 86% sensitivity and 77% specificity to differentiate between how and high risk of OSA. Its positive predictive value is 0.89 (33). A meta-analysis has shown that it is a good screening tool for OSA (34).
Metabolic syndrome was diagnosed based on the National Cholesterol Education Program and Adult Treatment Panel III (NCEP-ATP III) criteria (35). Questions were asked about the present status of smoking, and participants were classified into two categories-smoker and non-smoker). Similarly, based on usual dietary habits, participants were categorized into vegetarian and non-vegetarian.
Carotid intima-media thickness (CIMT) was assessed by high-resolution B-mode ultrasonography (SonoSite machine- M-Turbo; Fujifilm SonoSite Inc., USA) with a broadband width linear array transducer (6–13 MHz probe) following standard guidelines (36). The radiologist performing CIMT measurement was kept blinded to participants' sleep and other health-related data to remove the bias. Measurements were taken in the supine position with the head of the participant resting comfortably, the neck slightly hyper-extended and rotated opposite the probe. A wedge pillow at an angle of 45° was used to ensure lateral rotation. On longitudinal 2D ultrasound images of the carotid artery, the near and far walls were displayed as two echogenic lines (the adventitia and intima), separated by the hypoechoic media. The distance between the first bright line of the far wall (lumen-intima interface) and the second bright line (media-adventitia interface) was defined as the CIMT. This study measured right and left side IMT distal 10 mm of the common carotid artery in the far wall. Six values of CIMT (three on each side) were obtained, and the average of these measurements was taken for final analysis. Carotid IMT >0.7 mm was considered as increased, and ≤0.7 mm was taken as normal (37).
Lipid profile was measured after eight hours of fasting (Beckman coulter AU680 machine; Beckman Coulter, Inc., USA and EMBEE diagnostic reagent kit; Embee Diagnostics, India).
Fasting blood sugar (FBS) was measured for each participant after 8 h of fasting by the hexokinase method. (Beckman coulter AU480 machine Beckman Coulter, Inc., USA and EMBEE diagnostic reagent kit; Embee Diagnostics, India).
Glycated haemoglobin (HbA1c) was assessed for each participant using the high-performance liquid chromatography method (G8 90SL model, Tosoh Bioscience, Inc., USA).
The data was analyzed using Statistical Package for Social Sciences (SPSS) version 23.0 (IBM Corp. Released 2015. IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY). The Shapiro-Wilk test was applied to check the normality of data. Descriptive statistics were calculated. Statistical significance of qualitative variables was calculated using the Chi-Square test. Quantitative variables having normal distribution were compared using an independent sample t-test. Variables having statistical significance in univariate analysis were considered for multivariate logistic regression analysis to develop a model for increased CIMT.
A total of 110 participants were enrolled, and the response rate was 100%. The average age was 26.45 (±1.43) years with approximately equal gender distribution (51.8% male). 57.3% had normal BMI, 36.4% were obese grade 1, and 6.3% were obese grade II according to Asian-Pacific cut off points (30). There was no racial and ethnicity difference among the participants. None of the participants had family history of coronary and cerebrovascular disease. None of the participants reported sleeping pill usage. Carotid IMT was increased (>0.7 mm) among 44.5% of participants. Comparison of clinico-demographic factors between participants with normal and increased CIMT is depicted in Table 1. Poor sleep each of the components of the PSQI questionnaire was associated with increased CIMT (Figure 1).
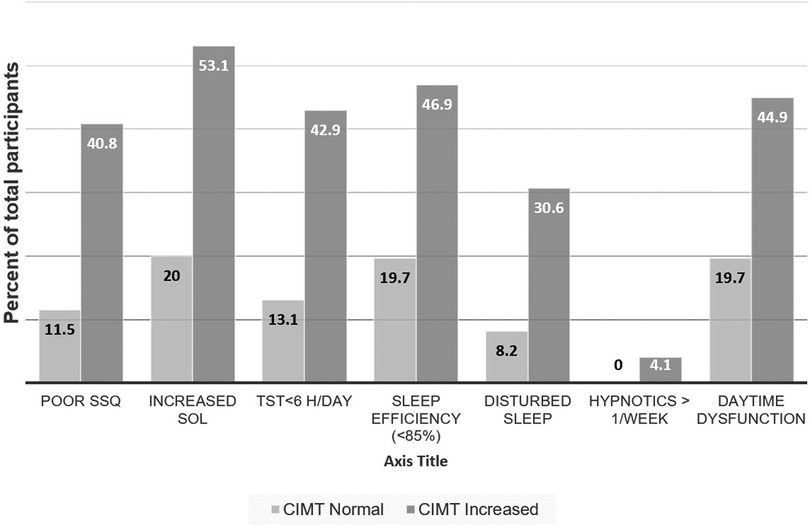
Figure 1. Proportions of subjects having dysfunction on various components of Sleep Quality. SSQ-subjective sleep quality, SOL-sleep onset latency, TST-total sleep time.
Multivariate logistic regression included poor sleep quality (as measured by global PSQI score) as well as other known risk factors for subclinical atherosclerosis. This model was overall significant [χ2 (9) = 43.57; P < 0.001], classified 75.4% cases correctly and showed 43.8% variation in the dependent variable (increased CIMT). Only poor sleep quality was associated with higher CIMT (P < 0.001, OR = 7.4; 95% CI = 2.70–20.32) (Table 2).
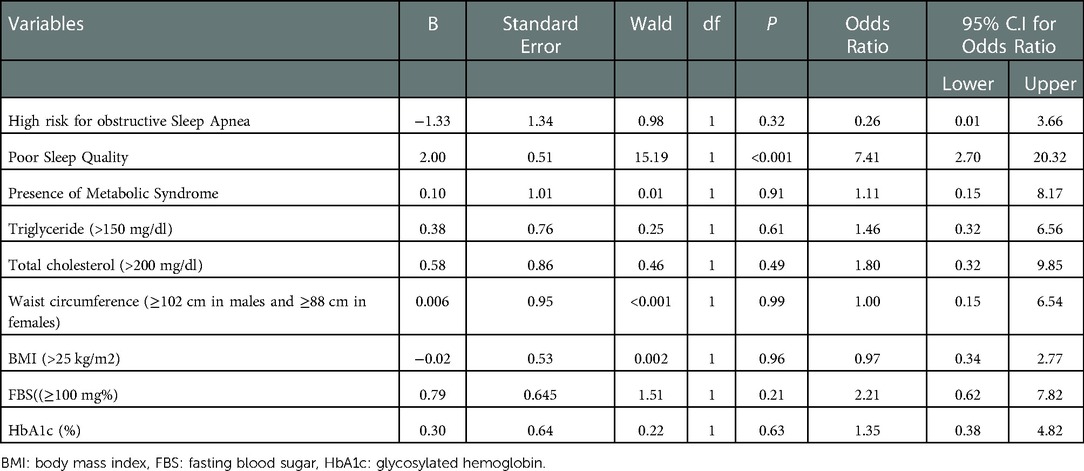
Table 2. Multivariate logistic regression model showing risk factors for increased carotid intima media thickness.
When the effect of different components of sleep quality on CIMT was analyzed through multivariate logistic regression, the model was overall significant [χ2 (7) = 39.70; P < 0.001], it classified 75.2% cases correctly and showed 40.8% variation in the dependent variable (increased CIMT). Subjective sleep onset latency, sleep efficiency and sleep disturbance was associated with higher odds for increased CIMT (Table 3).
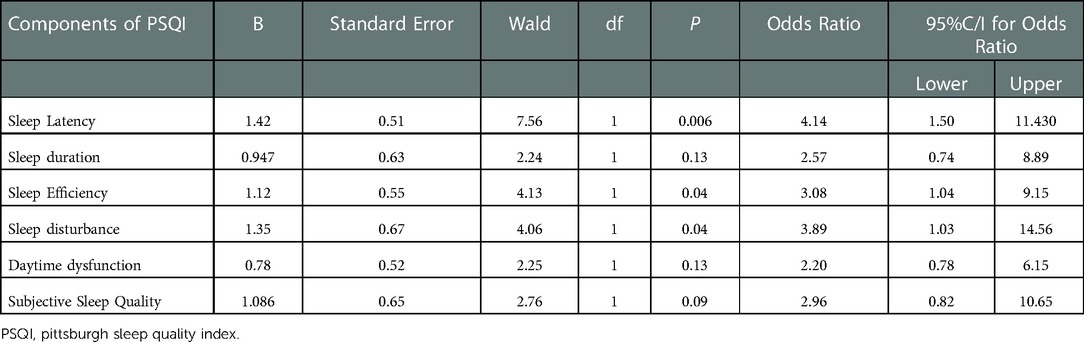
Table 3. Multivariate logistic regression model of sleep components of PSQI for increased carotid intima media thickness.
The present study involving 110 young, apparently healthy adult post-graduate medical residents showed that 54.5% of the participants reported their sleep quality as poor, and 44.5% had increased CIMT. Multivariate analysis depicted that after controlling for all confounders, only subjective poor sleep quality was associated with increased odds for increased CIMT (Table 2), especially sleep onset latency > 30 min, sleep efficiency <85% and sleep disturbance (Table 3).
This study showed that nearly half of the randomly selected resident doctors reported poor sleep quality across various specialities. Approximately similar results have been reported in earlier studies with higher rates among residents of clinical departments (24, 38, 39). Poor sleep quality among medical residents has been found to increase the risk of depressive symptoms, poor concentration, fatigue and daytime sleepiness (24, 39). Similarly, sleep deprivation, one of the components of sleep quality, has been found to induce stress and sympathetic activation, in turn increasing the risk for cardiovascular disorders (40). Moreover, poor sleep quality also produces oxidative stress, which enhances the risk for arterial injury and thus, can contribute to atherosclerosis, as was observed in this study (17, 41).
Previous studies have attempted to find an association between atherosclerosis and poor sleep quality among middle-aged patients having type 2 diabetes (42), middle-aged women (27), and middle age community-dwelling population (17). Present study expands to the previous study's findings by showing that poor sleep quality is associated with subclinical atherosclerosis among otherwise healthy young populations.
The present study has shown that factors that are traditionally considered as increasing the risk for atherosclerosis (dyslipidaemia, body mass index, smoking, fasting blood sugar, waist circumference) are less likely to play a dominant role in subclinical atherosclerosis at least in the presence of poor sleep quality (Table 2). Results of the present investigation are supported by a previous study by Domínguez et al. (43) who reported that short sleep duration (<6 h/day) and sleep fragmentation which are components of sleep quality (Figure 1) were associated with subclinical atherosclerosis even after controlling for other confounding variables e.g., age, gender, BMI, smoking, alcohol, physical activity, depression, perceived stress, blood pressure, risk for OSA, fasting glucose, total cholesterol and daily calorie intake. This research was furthered by Vallat et al. (44), who have shown that sleep fragmentation was associated with coronary artery calcification; however, this effect was mediated through increased neutrophil counts even after controlling for the age, gender, BMI, smoking status, blood pressure, use of antihypertensive medications, insomnia and obstructive sleep apnea. Cayres et al. (42) has also shown that truncal fat did not mediate the association between poor sleep quality and CIMT or femoral IMT (FIMT), supporting the results of the present study, where adiposity was measured using surrogate but validated markers of adiposity (body mass index, waist-hip ratio and waist circumference). Interestingly, a direct association between femoral IMT and poor sleep quality, but not with CIMT, has been reported in the past (42). It is possible that atherosclerosis starts in the femoral artery and then progresses to the carotid artery, perhaps due to greater sheer and tear in the femoral artery (42). Thus, previous studies also support the fact that perhaps, sleep quality is an important factor in the development of subclinical atherosclerosis. However, femoral IMT was not assessed in the present study and should be investigated in future.
Multiple studies have established the correlation between total sleep time and atherosclerosis risk factors (3–5). These studies have found a U shape association between total sleep time and increased CIMT (3–5). Though the meta-analysis has found an increased risk for diabetes mellitus, hypertension, coronary artery disease and obesity with total sleep time <6 h, short sleep was not associated with dyslipidaemia and depression (45). Another meta-analysis suggested that sleep duration <5 h/day was associated with metabolic syndrome, which is a risk factor for atherosclerosis (46). Similarly, an association between sleep disturbance, long sleep duration (>8 h/day) and increased systemic inflammation (increased C-reactive protein and IL-6) was reported in another meta-analysis but not with the short sleep duration (47). Present study also showed that sleep duration was not associated with increased CIMT while sleep disturbance, sleep onset latency and sleep efficiency were associated with CIMT.
However, several questions remain to be answered, e.g., Is there a causal relationship?; Are the results of the present study applicable to subjects having traditional risk factors for atherosclerosis, e.g., elderly, those with diabetes, those having metabolic syndrome or established cardiovascular disorders and heavy smokers?; does the relative contribution of various risk factors, including sleep quality and disturbance differ with regards to atherosclerosis?; is increased CIMT reversible with the improvement in sleep quality or sleep duration? Finding answers to these questions in well-designed prospective studies in the future can have a large impact on the health of resident doctors and that of the general population as components of sleep quality are modifiable factors.
Like any other scientific study, this study also suffered some methodological shortcomings. First, the data were cross-sectional, and hence only association could be established. Second, physical activity, perceived stress and the effect of irregular sleep-wake cycles were not measured. Since the participants were medical residents, it was assumed that they did not have a sedentary lifestyle. Third, smoking and dietary habits were measured as dichotomous variables, which may have a dose effect on atherosclerosis. Fourth, the effect of alcohol intake could not be assessed as participants were hesitant to respond. However, since all the participants were engaged in active work, chances of having alcohol dependence were negligible. Fifth, assessment of the interaction between sleep quality, sleep deprivation and shift work on CIMT after controlling for the confounding variables is a new area that should be addressed in future studies. Lastly, since the participants were medical doctors with adequate knowledge of risk factors for atherosclerosis, it was possible that they were trying to keep their lifestyle as healthy as possible, and hence, results “cannot be generalized”.
Strengths of the study included the inclusion of a younger sample without any other comorbidities, unlike previous studies (3–5, 17, 27). Secondly, optimal measures were taken to reduce bias, e.g., participants were selected using simple random sampling, most of the measures were self-reported, investigators indulged in anthropometric, and CIMT assessment was blinded to the status of sleep quality. Third, contrary to earlier studies, the present study assessed not only sleep duration as one of the components of sleep quality but also the qualitative assessment of “restful” “sleep”.
Poor Sleep quality is significantly associated with increased carotid intima-media thickness. Focusing on Sleep quality, being a modifiable risk factor, may prevent or reverse accelerated atherosclerosis; however, it remains to be answered in future studies.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by All india institute of medical science, Rishikesh, IEC/20/857. The patients/participants provided their written informed consent to participate in this study.
PS: has designed the study, collected the data, searched the literature, and drafted the manuscript. MP and RG: conceptualized the study, searched the literature, analyzed results, and drafted the manuscript. LS and PS: critically reviewed the manuscript. All authors contributed to the article and approved the submitted version.
I would like to express my thanks to the head of the department for giving me this opportunity and I extend my gratitude to Dr Rajat Ranka and Dr Aishwarya M for continuous support during this project.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fepid.2022.1044111/full#supplementary-material.
BMI, body mass index; BQ, berlin questionnaire; CIMT, carotid intima-media thickness; COVID-19, Corona virus disease-19; DBP, diastolic blood pressure; FBS, fasting blood sugar; FIMT, femoral IMT; HbA1c, glycosylated haemoglobin; IEC, institutional ethics committee; NCEP-ATP III, national cholesterol education program and adult treatment panel III; OSA, obstructive sleep apnea; PSQI, pittsburgh sleep quality index; SBP, systolic blood pressure; SPSS, statistical package for social sciences.
1. Mansukhani MP, Kolla BP, Surani S, Varon J, Ramar K. Sleep deprivation in resident physicians, work hour limitations, and related outcomes: a systematic review of the literature. Postgrad Med. (2012) 124(4):241–9. doi: 10.3810/PGM.2012.07.2583
2. Krittanawong C, Tunhasiriwet A, Wang Z, Zhang H, Farrell AM, Chirapongsathorn S, et al. Association between short and long sleep durations and cardiovascular outcomes: a systematic review and meta-analysis. Eur Hear Journal Acute Cardiovasc Care. (2019) 8(8):762–70. doi: 10.1177/2048872617741733
3. Blasco-Colmenares E, Moreno-Franco B, Latre ML, Mur-Vispe E, Pocovi M, Jarauta E, et al. Sleep duration and subclinical atherosclerosis: the aragon Workers’ health study. Atherosclerosis. (2018) 274:35–40. doi: 10.1016/J.ATHEROSCLEROSIS.2018.05.003
4. Ma CC, Burchfiel CM, Charles LE, Dorn JM, Andrew ME, Gu JK, et al. Associations of objectively measured and self-reported sleep duration with carotid artery intima media thickness among police officers. Am J Ind Med. (2013) 56(11):1341–51. doi: 10.1002/AJIM.22236
5. Sands MR, Lauderdale DS, Liu K, Knutson KL, Matthews KA, Eaton CB, et al. Short sleep duration is associated with carotid intima-media thickness among men in the coronary artery risk development in young adults (CARDIA) study. Stroke. (2012) 43(11):2858–64. doi: 10.1161/STROKEAHA.112.660332
6. Souza SP, Santos RB, Santos IS, Parise BK, Giatti S, Aielo AN, et al. Obstructive sleep apnea, sleep duration, and associated mediators with carotid intima-Media thickness: the ELSA-brasil study. Arterioscler Thromb Vasc Biol. (2021) 41(4):1549–57. doi: 10.1161/ATVBAHA.120.315644
7. Bin YS. Is sleep quality more important than sleep duration for public health? Sleep. (2016) 39(9):1629–30. doi: 10.5665/SLEEP.6078
8. Chaput J-P, Dutil C, Sampasa-Kanyinga H. Sleeping hours: what is the ideal number and how does age impact this? Nat Sci Sleep. (2018) 10(421). doi: 10.2147/NSS.S163071
9. Wang F, Bíró É. Determinants of sleep quality in college students: a literature review. EXPLORE. (2021) 17(2):170–7. doi: 10.1016/J.EXPLORE.2020.11.003
10. Goelema MS, Regis M, Haakma R, van den Heuvel ER, Markopoulos P, Overeem S. Determinants of perceived sleep quality in Normal sleepers. Behav Sleep Med. (2019) 17(4):388–97. doi: 10.1080/15402002.2017.1376205
11. Harvey AG, Stinson K, Whitaker KL, Moskovitz D, Virk H. The subjective meaning of sleep quality: a comparison of individuals with and without insomnia. Sleep. (2008) 31(3):383. doi: 10.1093/SLEEP/31.3.383
12. Dunietz GL, Lisabeth LD, Shedden K, Shamim-Uzzaman QA, Bullough AS, Chames MC, et al. Restless legs syndrome and sleep-wake disturbances in pregnancy. J Clin Sleep Med. (2017) 13(7):863–70. doi: 10.5664/JCSM.6654
13. Bajaj JS, Thacker LR, Leszczyszyn D, Taylor SA, Heuman DM, Raman S, et al. Effects of obstructive sleep apnea on sleep quality, cognition, and driving performance in patients with cirrhosis. Clin Gastroenterol Hepatol. (2014) 13(2):390–397.e1. doi: 10.1016/J.CGH.2014.08.028
14. W A, L YT, K G, A J, Å T. Relationships between questionnaire ratings of sleep quality and polysomnography in healthy adults. Behav Sleep Med. (2016) 14(2):185–99. doi: 10.1080/15402002.2014.974181
15. Wijeratne T, Menon R, Sales C, Karimi L, Crewther S. Carotid artery stenosis and inflammatory biomarkers: the role of inflammation-induced immunological responses affecting the vascular systems. Ann Transl Med. (2020) 8(19):1276. doi: 10.21037/atm-20-4388
16. Yang CW, Guo YC, Li CI, Liu CS, Lin CH, Liu CH, et al. Subclinical atherosclerosis markers of carotid intima-media thickness, carotid plaques, carotid stenosis, and mortality in community-dwelling adults. Int J Environ Res Public Health. (2020) 17(13):1–14. doi: 10.3390/ijerph17134745
17. Del Brutto OH, Mera RM, Zambrano M, Simon LV, Matcha GV, Castillo PR. Sleep quality correlates with the carotid intima-media thickness in stroke-free community-dwelling adults living in rural Ecuador. The atahualpa project. Sleep Med. (2019) 55:22–5. doi: 10.1016/j.sleep.2018.11.017
18. Original Research: Carotid Intima-Media Thickness and Its Associations with Type 2 Diabetes Mellitus in South Africans.
19. Rizza S, Longo S, Piciucchi G, Romanello D, Mavilio M, Montagna M, et al. Carotid intimal medial thickness in rotating night shift is related to IL1β/IL6 axis. Nutr Metab Cardiovasc Dis. (2020) 30(10):1826–32. doi: 10.1016/J.NUMECD.2020.05.028
20. Cayres SU, Vanderlei LCM, MacHado-Rodrigues AM, Werneck AO, Barbosa MF, Fernandes RA. Adiposity and physical activity do not mediate the longitudinal association between sleep quality and arterial thickness among adolescents. J Clin Sleep Med. (2019) 15(2):215–21. doi: 10.5664/JCSM.7620
21. Kasliwal RR, Bansal M, Desai N, Kotak B, Raza A, Vasnawala H, et al. A study to derive distribution of carotid intima media thickness and to determine its COrrelation with cardiovascular risk factors in asymptomatic nationwidE Indian population (SCORE-India). Indian Heart J. (2016) 68(6):821–7. doi: 10.1016/J.IHJ.2016.04.009
22. Song F, Zou J, Song Z, Xu H, Qian Y, Zhu H, et al. Association of adipocytokines with carotid intima Media thickness and arterial stiffness in obstructive sleep apnea patients. Front Endocrinol. (2020) 11:177. doi: 10.3389/FENDO.2020.00177
23. Chang Q, Xia Y, Bai S, Zhang X, Liu Y, Yao D, et al. Association between Pittsburgh sleep quality Index and depressive symptoms in Chinese resident physicians. Front Psychiatry. (2021) 0:879. doi: 10.3389/FPSYT.2021.564815
24. Jaradat R, Lahlouh A, Mustafa M. Sleep quality and health related problems of shift work among resident physicians: a cross-sectional study. Sleep Med. (2020) 66:201–6. doi: 10.1016/J.SLEEP.2019.11.1258
25. Ajgaonkar JR, Bidikar MP. Sleep assessment and perceived stress amongst medical postgraduate residents. Int J Med Biomed Stud. (2019) 3(6):28–32. doi: 10.32553/ijmbs.v3i6.287
26. Purim KSM, Guimarães ATB, Titski ACK, Leite N. Sleep deprivation and drowsiness of medical residents and medical students. Rev Col Bras Cir. (2016) 43(6):438–44. doi: 10.1590/0100-69912016006005
27. Thurston RC, Chang Y, von Känel R, Barinas-Mitchell E, Jennings JR, Hall MH, et al. Sleep characteristics and carotid atherosclerosis among midlife women. Sleep. (2017) 40(2). doi: 10.1093/SLEEP/ZSW052
28. D HSS, Singh A C. Sleep pattern, sleep problems and comorbidities among resident doctors at a tertiary care institution in India: a cross sectional study. Int J Community Med Public Heal. (2017) 4(12):4477. doi: 10.18203/2394-6040.ijcmph20175165
29. World Health Organisation (WHO). WHO | Waist Circumference and Waist–Hip Ratio. Report of a WHO Expert Consultation. Geneva, 8–11 December 2008. (2008); (December):8–11. http://www.who.int
30. Lim JU, Lee JH, Kim JS, Hwang YI, Kim TH, Lim SY, et al. Comparison of world health organization and Asia-pacific body mass index classifications in COPD patients. Int J Chron Obstruct Pulmon Dis. (2017) 12:2465. doi: 10.2147/COPD.S141295
31. Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 International society of hypertension global hypertension practice guidelines. Hypertension. (2020) 75(6):1334–57. doi: 10.1161/HYPERTENSIONAHA.120.15026
32. Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28(2):193–213. doi: 10.1016/0165-1781(89)90047-4
33. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Available at: https://reference.medscape.com/medline/abstract/10507956 (Accessed November 15, 2021).
34. Senaratna CV, Perret JL, Matheson MC, Lodge CJ, Lowe AJ, Cassim R, et al. Validity of the Berlin questionnaire in detecting obstructive sleep apnea: a systematic review and meta-analysis. Sleep Med Rev. (2017) 36:116–24. doi: 10.1016/J.SMRV.2017.04.001
35. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults T HE THIRD REPORT OF THE EX-pert Panel on Detection, Evalu-ation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III, or ATP III) constitutes the National. Accessed November 15, 2021. www.nhlbi.nih.gov
36. Stein JH, Korcarz CE, Hurst RT, Lonn E, Kendall CB, Mohler ER, et al. Use of carotid ultrasound to identify subclinical vascular disease and evaluate cardiovascular disease risk: a consensus statement from the American society of echocardiography carotid intima-Media thickness task force endorsed by the society for vascular medicine. J Am Soc Echocardiogr. (2008) 21(2):93–111. doi: 10.1016/j.echo.2007.11.011
37. Kasliwal R, Bansal M, Desai D, Sharma M. Carotid intima-media thickness: current evidence, practices, and Indian experience. Indian J Endocrinol Metab. (2014) 18(1):13–22. doi: 10.4103/2230-8210.126522
38. Murthy V, Nayak A. Assessment of sleep quality in post-graduate residents in a tertiary hospital and teaching institute. Ind Psychiatry J. (2014) 23(1):23. doi: 10.4103/0972-6748.144952
39. Zebrowski JP, Pulliam SJ, Denninger JW, Berkowitz LR. So tired: predictive utility of baseline sleep screening in a longitudinal observational survey cohort of first-year residents. J Gen Intern Med. (2018) 33(6):825–30. doi: 10.1007/S11606-018-4348-3/FIGURES/1
40. Morales J, Yáñez A, Fernández-González L, Montesinos-Magraner L, Marco-Ahulló A, Solana-Tramunt M, et al. Stress and autonomic response to sleep deprivation in medical residents: a comparative cross-sectional study. PLoS One. (2019) 14(4). doi: 10.1371/JOURNAL.PONE.0214858
41. Van Cauter E, Tasali E. Endocrine physiology in relation to sleep and sleep disturbances. In: Principles and practice of sleep medicine. Elsevier (2017) p. 202–19
42. Osonoi Y, Mita T, Osonoi T, Saito M, Tamasawa A, Nakayama S, et al. Poor sleep quality is associated with increased arterial stiffness in Japanese patients with type 2 diabetes mellitus. BMC Endocr Disord. (2015) 15(1). doi: 10.1186/S12902-015-0026-1
43. Domínguez F, Fuster V, Fernández-Alvira JM, Fernández-Friera L, López-Melgar B, Blanco-Rojo R, et al. Association of sleep duration and quality with subclinical atherosclerosis. J Am Coll Cardiol. (2019) 73(2):134–44. doi: 10.1016/j.jacc.2018.10.060
44. Vallatid R, Shahid VD, Redlineid S, Attia P, Walkerid MP. Broken sleep predicts hardened blood vessels. PLoS biology. (2020) 18(6):e3000726. doi: 10.1371/journal.pbio.3000726
45. Itani O, Jike M, Watanabe N, Kaneita Y. Short sleep duration and health outcomes: a systematic review, meta-analysis, and meta-regression. Sleep Med. (2017) 32:246–56. doi: 10.1016/J.SLEEP.2016.08.006
46. Iftikhar IH, Donley MA, Mindel J, Pleister A, Soriano S, Magalang UJ. Sleep duration and metabolic syndrome. An updated dose-risk metaanalysis. Ann Am Thorac Soc. (2015) 12(9):1364–72. doi: 10.1513/ANNALSATS.201504-190OC
Keywords: physician health, subclinical atherosclerosis, sleep hygiene, sleep medicine, cardiovascular medicine
Citation: Sethi PP, Pathania M, Gupta R, Sharma P and Saini LK (2023) Poor quality sleep is associated with greater carotid intima media thickness among otherwise healthy resident doctors. Front. Epidemiol. 2:1044111. doi: 10.3389/fepid.2022.1044111
Received: 16 September 2022; Accepted: 13 December 2022;
Published: 11 January 2023.
Edited by:
Theophilus I. Emeto, James Cook University, AustraliaReviewed by:
Biju Soman, Sree Chitra Tirunal Institute for Medical Sciences and Technology (SCTIMST), India© 2023 Sethi, Pathania, Gupta, Sharma and Saini. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Monika Pathania YW5zaHVwYXRoYW5pYTI3QGdtYWlsLmNvbQ==
Specialty Section: This article was submitted to Cardiovascular Epidemiology, a section of the journal Frontiers in Epidemiology
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.