
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Environ. Sci., 13 July 2023
Sec. Toxicology, Pollution and the Environment
Volume 11 - 2023 | https://doi.org/10.3389/fenvs.2023.1149314
This article is part of the Research TopicRecent Research Advances on Heavy Metals, Microplastics, Persistent Organic Pollutants, and Solid Waste in Aquatic and Terrestrial EcosystemsView all 11 articles
The plight of humanity in refugee camps is an age-old issue, as is the ever-increasing issue of waste management, especially medical waste. Though situations have improved in recent times for refugee camps, the same cannot be concurred about medical waste management, as it increases in amount every day. This is the first study on the refugee camp, which was conducted to assess the status of medical waste management and to quantify and characterize medical wastes disposed of in the Rohingya refugee camp at Cox’s Bazar, Bangladesh. A cross-sectional, qualitative, and quantitative study was done. A total of 499 households, 30 solid waste collectors, 30 HCF workers, and 21 solid waste management (SWM) plant workers were interviewed by KoBo Toolbox. Monthly medical waste collection data from February to June 2022 was also collected. Data collection, processing, and statistical analysis were done using Origin Pro and SPSS software. It was found that the camps did not follow any specific guidelines for medical waste management except for a few segregations in healthcare facilities (HCF). Though 88% of the respondents were aware of the hazardous nature of medical waste, most of them disposed of these wastes in open places (49%) and drains (44%), and 70% did not segregate it from regular waste at the household level. Moreover, 73% of solid waste management workers found medical waste daily in communal bins. The HCF did not keep any records on the production of medical waste. Different types of medical waste were found in communal bins; glass bottles containing medicines were common among them. Data from the material recovery facility (MRF) of this camp showed that the highest amount of medical waste found in the communal bins was in April (65 kg) during the seasonal change from spring to summer and the lowest in February (12.7 kg). Moreover, HCF’s existing medical waste management practices were analyzed with SWOT and DPSIR framework. Based on all the findings, a comprehensive on-site and off-site management plan for medical waste is also proposed here. That will help the concerned prepare a camp medical waste management guideline.
“Nothing on Earth is more international than disease,” said Paul Russel. Health and disease have no political or geographical boundaries (WHO, 1980). Health care facility has been established worldwide to save us from different diseases (Alam, 2019; Barua and Hossain, 2021; Khalid et al., 2021). This facility creates a special kind of waste that is called medical waste (MW). Environmental protection and public health are seriously threatened by medical waste. Due to its rise in volume, medical waste management (MWM) difficulties that exist worldwide have been made worse in the COVID-19 pandemic (Barua and Hossain, 2021; Khalid et al., 2021). The World Health Organization (WHO) defines medical waste as “Waste that is produced in the diagnosis, treatment, or immunization of individuals or animals in research related there, or in the manufacturing or testing of biologicals” (Windfeld and Brooks, 2015). WHO predicts that hazardous compounds that may be infectious, poisonous, or radioactive comprise about 20% of these medical wastes (Birchard, 2002). Medical waste contributes to the second-largest volume of hazardous waste in the nation, according to Asian Development Bank’s hazardous waste inventory from 2008 (Hasnat and Sinha, 2010). MWM is one of the many intricate and demanding problems that humankind is currently experiencing as the world’s population grows and the need for medical services rises (Windfeld and Brooks, 2015). When medical waste is not managed and is therefore disposed of inappropriately, there is a significant danger of infection or injury for medical staff as well as risk for the general public due to the release of microorganisms from medical institutions and hazardous properties of medical waste into the environment (Mohee, 2005; Chauhan and Singh, 2016; Mitiku et al., 2022; Wassie et al., 2022). So MWM is an important event for all countries. Most industrialized countries have laws governing medical waste, but there is typically minimal guidance on campsite medical waste management (Mbongwe et al., 2008; Prem Ananth et al., 2010). As a result, medical waste in different campsites is not adequately managed, and various pathogens and infectious agents can frequently spread (Kwikiriza et al., 2019).
Bangladesh is a small developing country. The population of Bangladesh is higher than its area. This large number of people in Bangladesh requires many healthcare facilities to get proper health treatment. This establishment also produces a large number of medical waste. In Bangladesh, medical waste generation is estimated to be roughly 0.5 kg/patient/day under typical circumstances (Hassan et al., 2008; Biswas et al., 2011). In opposition to this, during the COVID-19 pandemic, waste production increased to 3.4 kg/patient/day, around 6.8 times more than usual (ADB, 2020). Medical waste management was a predicament in Bangladesh even before the pandemic ensued (Barua and Hossain, 2021). After the pandemic, the condition becomes more worst. In 2004, the first environmental assessment and action plan for the country’s sector addressing MWM in the areas of health, nutrition, and population was made public. It was later upgraded in 2011 (Barua and Hossain, 2021). Bangladesh published its first MWM rules in 2008. Later, from 2009 onwards, some Non-Government Organizations (NGOs) came forward for MWM. However, Bangladesh has yet to demonstrate proper implementation of the MWM system’s rules. Failure to implement adequate MWM might endanger the country’s ecology and biodiversity (Hassan et al., 2008; Barua and Hossain, 2021).
On the 25th of August in 2017, a previously unprecedented surge of Rohingya refugees from Myanmar’s Rakhine State began arriving in Cox’s Bazar of Bangladesh. They are predominantly Forcibly Displaced Myanmar Nationals (FDMNs) from Myanmar who have fled to Bangladesh. In the Cox’s Bazar area, as of October 2019, there were an estimated 911,566 Rohingya refugees, 905,754 of whom were housed in 34 refugee camps (Security and Management, 2019). This created a humanitarian disaster and necessitated considerable cooperation among several stakeholders to face this. (Alam, 2019; Lewis, 2019; MacLean, 2019; Jeffries et al., 2021). This demographic group also has significant and diverse physical and mental health requirements, including issues with sexual and reproductive health, infectious diseases, chronic illnesses, physical impairments, injuries, and emergencies (Kwikiriza et al., 2019; Al-Khatib et al., 2020; Andrew et al., 2021; Jeffries et al., 2021). To give them medical support, non-governmental organizations such as the United Nations High Commission for Refugees (UNHCR), International Organization for Migration (IOM), Bangladesh Rural Advancement Committee (BRAC), Gonoshasthaya Kendra (GK), and United Nations International Children Emergency Fund (UNICEF) establish health camp facilities. These procedures create massive medical waste containing infectious and pathogenic contaminants. Exposure to hazardous medical wastes can cause infections, infertility, genital deformities, hormonally triggered cancers, mutagenicity, dermatitis, asthma, and neurological disorders in human beings (New WHO Handbook on Healthcare Waste Management, 2013). Typhoid, cholera, hepatitis, AIDS, and other viral infections can be transmitted through sharps contaminated with blood (Oli et al., 2016; Kenny and Priyadarshini, 2021). Considering the issue, managing medical waste is necessary for the Rohingya camp (Chauhan and Singh, 2016). However, there is very little specific and detailed literature on medical waste management in humanitarian campsites (De Montclos and Kagwanja, 2000; Oka, 2014; Ekezie et al., 2019; Karsu et al., 2019; Zarei, 2022). As a result, medical waste poses considerable health and environmental risks to camp people and the surrounding locality. This study has been conducted to eradicate this issue and ensure more efficient medical waste management in campsites. It will also critique existing management facilities and show possible mitigation alternatives. That will help the concerned prepare a camp medical waste management guideline and ensure SDG 3.
The specific objective of this study is (1) to characterize medical waste generated with regular solid waste in the context of the refugee camp, (2) to find out the efficiency of existing medical waste management with SWOT analysis and DPSIR framework, (3) to recommend an alternative for more efficient medical waste management in the humanitarian context.
The study area is mainly conducted in the Rohingya camps. The refugee camp is situated in the southeast part of Bangladesh, in Cox’s Bazar city of the Chattogram division. The massive influx of refugees into Bangladesh from violence in the neighbouring country Myanmar now stands at 33 crowded camps in Cox’s Bazar district (Figure 1). The main source of quantitative data in this study was from the FDMNs, solid waste management personnel from Camp-15 (Ukhia). This camp houses refugees from the Rakhine state of the neighbouring country Myanmar. The camp and the respondents in the questionnaire survey were selected through a random sampling method, more specifically, the purposive random sampling method, which was done to ensure the most effective data collection in the study to paint out the complete scenario.
To do random sampling in this case, the sample size was calculated as follows (Krejcie and Morgan, 1970)
Where N = Population Size; p = Population proportion; Z = Critical value of the normal distribution at the required confidence level; e = Margin of error. N is the sample size which is calculated and determined as 378 (=n) based on the following parameters. N is the population size, 21050; z value is 1.96 at 95% confidence level, e is the confidence interval or margin of error expressed as decimal (0.05), and population proportion, p is 0.5.
This study interviewed 499 households, 30 solid waste collectors, 30 HCF workers from 7 HCF, and 21 solid waste management (SWM) plant workers. Sample selection was made using random sampling. In addition to this, 15 KIIs (Key Informant Interviews), 5 IDI (In-Depth Interviews), and 10 FGDs (Focus Group Discussion) were conducted for collecting qualitative data from relevant stakeholders such as the Government of Bangladesh (GoB), WHO, NGOs, and International Non-governmental Organization (INGOs), hospital workers, doctors, nurses, local people, UNO, chairman, government workers.
The participants faced the questionnaire (qualitative and quantitative) physically and faced to face. An introductory briefing was given to them where the objectives of the study as well as ethical issues, were described. Then, informed verbal consent was taken from the participants before surveying. Field visits and household surveys were also conducted. Kobo Toolbox software (https://www.kobotoolbox.org/) was used in the continuous collection of data and as safe storage for the database. Interviews are done with the help of it. All of the questions were asked in Bengali and the answers were translated into English when the paper was written.
Key informative interviews (KII), In-depth interviews (IDI), and semi-structured interviews are done to explore the experiences of targeted participants and the meanings they attribute to them. Researchers encouraged the participants to talk about issues or tropics they want from them by asking open-ended questions, in one-to-one interviews (Tong et al., 2007). All of the selected people were interviewed by the definite questionaries prepared by the authors, and the answers were collected for further data analysis.
FGD is a helpful tool for finding specific scientific data from a community. It is often conducted with 4–10 people. However, the moderator has the option to moderate the talking or responding issue. In this part, the selected people answered the moderator’s questions by interacting with each other (Tong et al., 2007). Two to five people from our team were present when this FGD was conducted. One was assigned to give them key point to talk and moderate the conversation. All of their conversations were recorded with their proper consent to ensure accuracy.
In addition, data from the MRF was also collected from their log book from February to June 2022.
The questionnaire was designed to facilitate the assessment of the current pattern of medical waste management in the Rohingya camp, which adds to the challenges of SWM in Rohingya camps at Cox’s Bazar. The information collected by this questionnaire attempted to accumulate information addressing the generation of different medical wastes amount and sources from other locations at the community level. All of the surveys started with demographic questions such as name, age, and sex, followed by questions about household-level practices to manage solid and medical waste. The interviewer asked about the respondents’ knowledge of medical waste status as a hazard if they purchased medical items and the availability of medical items. If yes, where and what do they do after using the medical articles, and is any medical waste collection point available in their community? The solid waste management workers survey questionnaire included questions on their view of the impact of solid waste disposal on polluting the environment, the status of waste (existence of waste communal bin nearby, regular waste collection, waste left in communal bins, drains, roads/open space), where, by whom, the process of, at what time of the day, and how often household waste are disposed. The types of waste generated, segregation of waste into organic and inorganic, knowledge about waste processing, satisfaction with the collection level, and if any knowledge or message was provided to them were also among the questions asked.
Survey questions to waste collectors included how often they collected daily waste in the week, methods used to collect day-to-day waste, where they were collected from if they found medical waste during regular waste collection, and what they did with it.
Survey questions to SWM plant workers/volunteers/stuff contained, plant location, coverage block of solid waste management plant, population coverage from this plant, if any medical waste came to the plant from community level, how they are processed, and finally, how they are managed. In the case of HCF workers, questionaries contain the amounts of medical waste generated in HCF, what is the type of waste they generate, do they segregate them, how they manage their waste, do they satisfied with the existing waste management procedures, and what can be done to improve it.
For IDI, FGD the moderating conversation points were as follows: do they have knowledge about medical waste, is medical waste properly managed here, what is the procedure to manage them, is there any regulatory body for monitoring medical waste, are they satisfied with the management, and what should be done for the betterment of medical waste management.
Microsoft Excel was also used in the processing and analysis of the data. The collected data is analyzed with descriptive statistics in narrative form and through percentage analysis. Pearson Correlation Coefficient values were calculated, and a correlation matrix was produced for some datasets as required. Origin Pro-2022 was also used for creating graphs and statistical analysis. SWOT and DPSIR were performed based on the qualitative and quantitative data. The details are provided in the following subsection (SWOT analysis and DPSIR analysis).
Based on the KII, IDI, and FGD from the relevant stakeholders, SWOT analyses are performed. SWOT means strength, weakness, opportunity, and threat analysis of a definite organization, system, or guidelines (Büyüközkan and Ilıcak, 2019; Shammi et al., 2022). Among them, strengths and weaknesses are internal factors, and opportunities and threats are external factors. For the strength, weakness, opportunity, and threat part, the strengths, weaknesses, opportunities, and threats of existing waste management procedures are identified. This is done based on the KII, IDI, FGD, and literature surveys.
A causal relationship is established for portraying societal and environmental interactions using the Driver-Pressure-State-Impact-Response (DPSIR) framework. It is a tactical and logical instrument for identifying, evaluating, and summarizing environmental issues at various spatial and temporal scales (Tscherning et al., 2012; Skondras and Karavitis, 2015; Vardopoulos et al., 2021). This analysis was also performed based on KII, IDI, and FGD information and a literature review. It is often used to link different parameters or factors with each other in qualitative data representation.
For reviewing the literature, first of all the available literature, reports of different NGOs and governments in medical and solid waste management were collected. Then they were analyzed, and information related to our research question was segregated for use and compared with our analyzed data.
All of the participants are first informed about the research objectives, and they were interviewed only if they agreed to participate. No interview was taken without their consent. In a continuous interviewing process, if anyone wished to terminate, they were able to do so.
The respondents belonged to Refugee Camp 15 (Blocks A, C, D, E, F, G, H). There were 279 (55.9%) male respondents and 220 (44.1%) female respondents. Their age varied from 19 to 60 years, with a mean age of 35. The current mechanism of waste disposal in this community location was documented since the medical waste was disposed of mixed with household waste. The respondents were asked questions to find their knowledge of the relationship between waste disposal and the environment. The refugees of the camp responded that unplanned dumping might have a serious effect on the environment and opined some causes or a combination of causes for this happening.
Most of the respondents (about 91% respondents) have an idea about the fact that inadequately disposed of solid waste can pollute the environment; 88% of respondents also concluded that medical waste could also pose threats to nature (Table 1). Moreover, most people opined that the disruption of nature was due to the absence of any communal bins nearby and the consequent existence of the waste being left in open drains. Many people also thought it was due to waste not being collected regularly and them being left on roadsides or open places. Many of them said that they came to know of this knowledge of disruption of the environment by waste through various WASH agencies and NGOs that helped build their awareness on the matter. However, at the community level, no system is yet established for medical waste management.
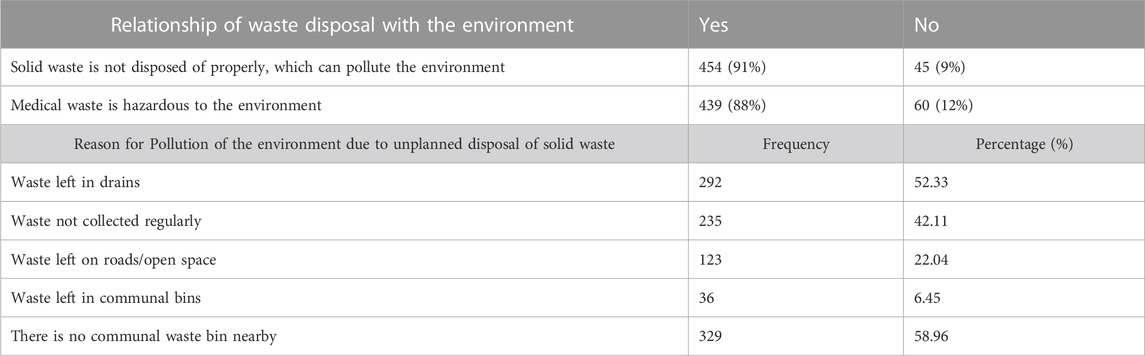
TABLE 1. Opinion of the household survey respondents on the relationship of waste disposal with the environment and the reason for pollution of the environment due to unplanned disposal of solid waste.
In the case of waste disposal practices of the respondents, it was found that disposal methods of their household wastes varied from person to person, as shown in Supplementary Table S1. Most people dump waste in an open place near households (48.92%) and into the drains (43.91%). Some people say that the waste collector collects their waste from their door; some also throw it in the communal bin. At the same time, a portion of the population dumps it by the side of the road (22.58%). The community’s current practices of medical waste disposal systems were also found through the gender roles of household waste disposal. The HH’s waste disposal activity was carried out majorly by women at 414 (74%), while men disposed of HH’s waste 85 (15%) times. Most people were found to dispose of their waste on an everyday basis (70.79%), majorly in the morning and the evening. People used polythene (57.17%) and household bins (32.08%) to contain and throw waste outside. When asked about the type of waste produced in their household, they listed organic and inorganic materials, including vegetable waste, fish waste, polythene bags, papers, packets, clothes, leaves, etc. Almost 70% of the participants did not segregate their waste into organic and inorganic categories. Some people demonstrated that their waste materials were taken to their camp’s solid waste management plant, some by CARE (Cooperative for Assistance and Relief Everywhere) and some by BDRC (Bangladesh Development Research Center). However, 32.62% of people had no idea about the processing of their disposed waste or where they were being taken. However, most people seemed satisfied with their locality’s waste collection practices. Yet more than 70% of participants claimed they were made aware of waste disposal or the importance of segregation by different organizations.
The status of medical waste generation, disposal practices, and the respondents’ knowledge level are demonstrated in Table 2. 83.87% of respondents said that they purchased medical items for their families. The medical item type they bought included syrup bottles, tablets, capsules, and syringes for injections. They bought vitamins, paracetamols, metero, omeprazole, diarrhea medicine, cough, fever, and gastric medicines such as the domperidone family of medicines. They purchased these medicines from markets (they named five such markets), hospitals (3 hospitals), pharmacies, and other small shops around their locality. This gives the idea of the availability of many places to buy medicines from the locality. 86.74% said medical items were relatively available. On the other hand, 81.9% of respondents said that there were no medical waste collection points in their community. As a result, they mostly threw the medical items in communal bins after using them (23.48%), kept them in their household (39.78%), or threw them in an open place after using them (15.05%). Some people threw them in the drains. The rest of the respondents disposed of them in latrine rings, on the ground, or buried into the ground and given to waste collectors. From our observations and the respondents’ statements, it was pretty clear that the camp has no establishments or infrastructure for hazardous medical waste.
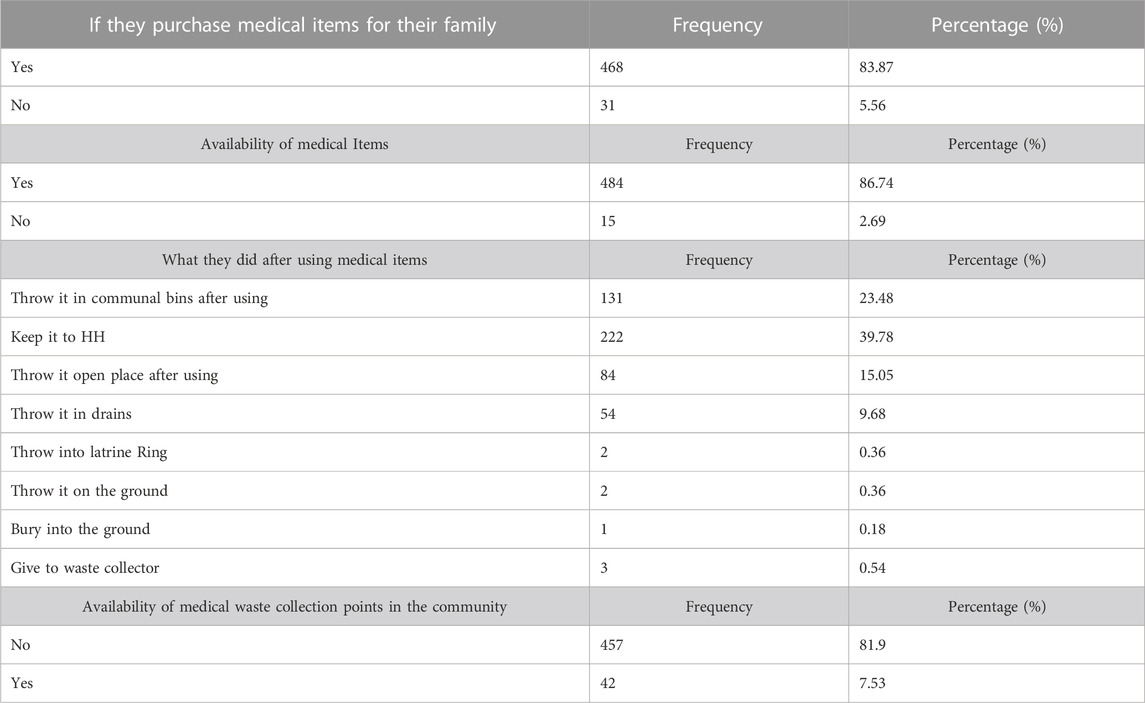
TABLE 2. Status of medical waste generation and disposal practices as well as the knowledge level of the respondents.
Solid waste collection is mainly done by the WASH actors in the camps. They are mostly government employees employed to collect waste. Camp local waste collectors collect waste from the community level, and by transportation, this waste is sent to MRF for further processing (Supplementary Table S2). Key findings from the respondents showed that predominantly 100% of waste collectors were male. The waste collection was done 5 days a week. As shown in Supplementary Table S2, solid waste vans and wheelbarrows are used for daily waste collection in camps. Wastes are mainly collected from household levels, roads, drains, shared spaces, and communal bins. This matches with the responses from the form of the household respondents where they expressed that they threw waste at these exact places. After the collection of waste, all waste was transferred to the solid waste management plant. They found medical waste mixed with general waste regularly. The current practice is to store medical waste in plants, and finally, the medical waste is dumped or open burned in most themes.
The HCF is one of the major sources of medical waste generation. A total (of n = 7) healthcare facilities were surveyed. They included BDRCS (Bangladesh Red Crescent Society), Save the Children, BRAC, GK, IOM, and others. To identify the current practices at the camp level HCF survey was conducted. Different types of hazardous waste can be generated in all clinical institutions, including hospitals, health centers, dispensaries, and special clinics. The average waste generation rate for HCF was 2 kg per day. Types of waste generated in the healthcare facility as per our survey, were general waste, infectious waste, sharp objects, recyclables waste, chemicals (liquid and solid) waste, pharmaceutical waste, and anatomical waste. In terms of safe handling of medical waste, 57% of HCF said their safety levels were satisfactory, whereas 43% of HCF said it was insufficient. In this study, all the facilities used plastic bins for disposal and containing waste.
Medical waste has not received much attention in camps, and this study shows that it is disposed of together with domestic waste by the community. Figure 2 shows that 71% of HCF have their medical waste management system, 15% of HCF are transferred to a third party, and 14% dump their waste, which is threatening the environment. This is a clear indicator that through HCF, hazardous medical waste can be released in the camps as a wellbeing threat to public health. The authorities claimed they have some medical waste treatment facilities, but they cannot properly manage medical waste. They are suffering from a lack of equipment, training, and monitoring systems. 86% of the facilities did not recycle or put to recycle any of their wastes. All of this indicates less concern about the environment among the individuals in the refugee camp.
A significant finding and drawback of the existing healthcare management of medical waste are being found regularly in the communal bin (Figure 3). Among 21 SWM workers, 73% of waste collectors said that while collecting waste, they found medical waste regularly during the collection of solid waste. Whereas 27% of respondents said that they did not find medical waste on a daily basis. Figure 3B shows the average medical waste found in a communal bin, and Figure 3A shows the waste in a segregated way.
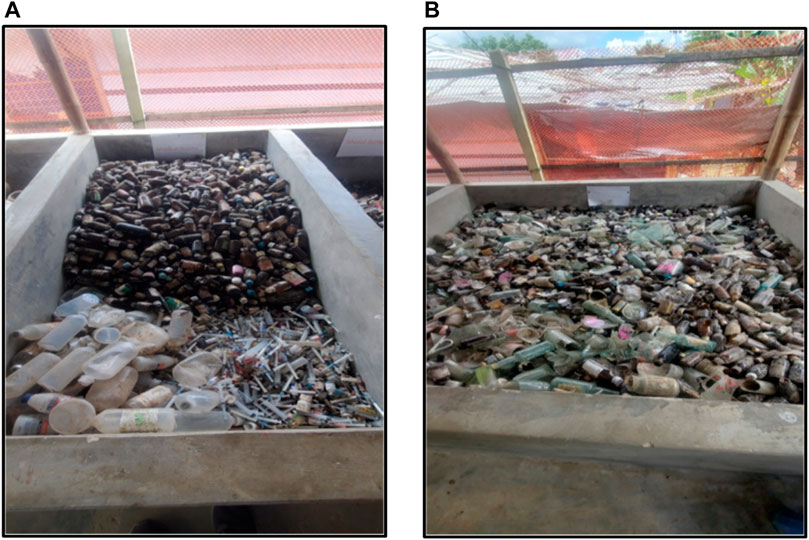
FIGURE 3. Current practice of storage of medical waste in MRF (Material Recovery Facility) In (A) (Medical waste in a segregated way), (B) (Medical waste is mixed with other Solid waste).
After collecting waste from the communal places, waste collectors transport waste to SWM plants. Finally, medical waste is dumped or buried in the soil, posing a threat or creating a hazard to the environment.
In Camp-15 Block-E, an MRF survey and regular data collection were conducted to identify the amount of medical waste coming to MRFs from camps. These MRF facilities mainly collect solid waste, followed by segregation, storing, and recycling of solid waste. Data on waste coming to the plant was collected every day for 5 months to know the amount of medical waste coming from camps. Figure 4 shows the monthly amount of medical waste generated in the camp’s communal places. The trend of generation of medical waste shows less in February (12.7 kg) and March (22.7 kg) at the end of the winter season in Bangladesh. After the winter season, the generation of waste increases. At the beginning of the summer season, medical waste generation is highest in April (65 kg) and then in May, which then somewhat maintains the high rate up to the rainy season in June.

FIGURE 4. Medical waste generation in Rohingya camp. Here, (A) Monthly MW generation (B) Average waste types generation.
During data collection, emphasis was put on the pattern of medical waste which is coming to MRF. This was done to understand the category of medical waste generated. Total data of 5 months were collected from MRF. Supplementary Figure S1 shows the breakdown of different categories of medical waste throughout the 5 months and an overall depiction. In February of 2022, medical waste was comprised of 64% bottles, 8% Plastic syrup bottles, 24% syringes and 4% saline bags. In March, there were 94% of bottles, 4% of Plastic syrup bottles, 2% of syringes and 0% saline bags generated in communal places. In April, the month of highest generated waste, 67% bottles, 26% Plastic syrup bottles, 5% syringes and 2% saline bags were collected. A somewhat similar trend was followed in May and June as well. A positive linear correlation exists between wastes generated every month (Supplementary Table S3). This shows a consistent trend of waste generation from month to month. An opposite trend is observed between different categories of waste, with only the exception of the use of glass bottles of medicines and syringes which have a positive linear correlation between them. Thus, the use of glass bottles of medicines has changed consistently with the use of syringes. The others had a negative linear correlation, as they did not increase or decrease usage with their counterparts. Overall, 94% of the medical waste was found to be general waste, including the daily use of medicines and non-infectious particles. Also, 5% sharp waste was found in the study, which is a threat to the community and also the environment because; it can cause injuries to humans and animals.
During this study, the waste type of camp-15 was observed. The percentage and amount of medical waste found in the communal bin were measured. Monthly data collection from the camp’s MRF showed that a total of 48,518 kg of solid waste was generated, containing 221 kg of medical waste in 5 months. The average medical waste in the communal bin is 44.2 kg/month. Moreover, the percentage shows that a total of 0.5% of medical waste is generated in camps while segregating from solid waste.
HCF inside the camp generally generates general wastes (such as packaging materials, food wastes, papers, etc.), sharps (such as syringes and needles, slides, cover slips, etc.), pharmaceutical waste (such as vials, expired vaccines, medicines, etc.), and infectious waste (PPE including used gloves and masks, band-aids, gauges, blood, placenta, etc.). These medical wastes were first segregated into different color-coded bins. Based on the field observation, only one of them had proper on-site treatment facilities (Autoclaving/Ash pit/Deep burial pit), they mostly handover to a third party (WASH collectors and sharps to the nearby Ukhiya Upazila health complex) without any disinfection processes (Figure 5). But they are suffering from a lack of infrastructure facilities, space, and electricity. In some cases, they also do open burning or open dumping of medical waste. Moreover, there was no liquid waste management facility in any HCF. According to them, liquid waste generation is very low in health camps. For this reason they don’t treat it, and instead dump it in the drainage system. There were no specific guidelines or SOPs (standard operating procedures) for camp medical waste management in the Rohingya camp. Moreover, they needed to correctly maintain occupational health safety protocols for medical waste management workers, and there is no training facility for medical waste management workers and authorities. A logbook and monitoring system to preserve the amount of medical waste generation and treatment are also unavailable.
SWOT analysis is the most helpful tool to assess the efficiency of the existing facility or process. It also helps us to find out the weakness, opportunities, and threats. All of these characteristics make it more feasible in strategic management (Büyüközkan & Ilıcak, 2019; Shammi et al., 2022). Figure 6 represents the SWOT of the existing medical waste management scenario in the Rohingya camp.
The main strength of this MWM in the campsite is that authorities are willing to implement proper MWM procedures. Every HCF in the campsite contains a color-coded segregation waste bin. Moreover, international organizations are involved in funding and managing refugee campsites.
Proper guidelines and SOPs for campsite MWM are the main weakness of existing campsite MWM. Because there are no specific guidelines and SOPs for medical waste management available now, for that reason, campsite medical waste is not managed correctly. It also suffers from the lack of monitoring systems, infrastructure, training systems, power supplies, and water supplies issues. The humanitarian crisis and shortage of area are other weaknesses in proper MWM.
Tremendous opportunities are available for better campsite MWM. One of the most significant opportunities is to create SOPs and specific guidelines for medical waste management in the campsite. Implementing new infrastructure facilities (Autoclaving, Deep burial pit, Ash pit, and Placenta pit) is another opportunity to make it more efficient. Furthermore, a robust monitoring system and training program on MWM can be implemented.
One of the most hazardous and concerning threats to the existing management of medical waste management MWM is untreated medical waste which has been found in the communal bins. It will spread the infectious disease among the contacted people. It will create a serious health threat to the entire community. Moreover, open waste burning helps spread disease and causes air pollution.
The DPSIR model is the most often used method for establishing the connection between ecological causes and any problem’s impacts (Vardopoulos et al., 2021). The DPSIR framework has some limitations, such as its inability to indicate non-linear links, account for natural drivers of environmental changes, and clearly define fresh indicators of progress or trends unless investigated at frequent intervals (Skondras and Karavitis, 2015). A total of 499 household surveys, 30 solid waste collectors, and 21 SWM plant workers KII, FGD, IDI, newspaper reports, research organizations report, and existing literature on MWM are the critical elements of the DPSIR framework. The summary of qualitative findings of the responses is shown using a DPSIR framework. The driving forces-pressure-state-impact-response (DPSIR) framework (Figure 7) was developed based on the stakeholder analysis and presented here to visualize the actual scenario of medical waste management in the Rohingya camp.
Environmental safeguard policy, international organizations, national and international guidelines, and international fundings are the main driving force of medical waste management in the Rohingya camps. They had the capability to improve or degrade pressure (congested area, over population, regulatory restriction) and states (unemployment policy, lack of MWM facility, lack of training, guidelines, and monitoring facility). In combination, these could be used to control the impact of the mismanagement of medical waste in the Rohingya camp. The adverse effects of MW mismanagement include communal waste, community transmission, environmental degradation, and human health risk.
This negative impact has also pressurized the community to respond in order to solve these issues. The response includes creating medical waste management guidelines and ensuring treatment facilities for campsite MWM, establishing SOPs, training an inspection team, ensuring record maintenance for MWM, and building up awareness among the stakeholders. All of this response will also modifies the state, pressure, and impact.
For the creation of an MWM procedure for the campsite, top-down and bottom-up management procedures should establish (Figure 8). Top-down and bottom-up approaches can be implemented to ensure sustainable MWM in Rohingya camps. In the top-down segment, a set of well-regulated stratified national bodies will exist, including the national advisory body, policy, stakeholders, technical body, capacity building, source of finance, and medical waste management system (MWMS). These bodies will be responsible for developing a campsite medical waste management policy and SOPs which are further directed towards forming an MWMS with the help of the technical committee. After that, sufficient stakeholder engagement will be done, followed by capacity building in terms of separations, collections, and final treatment, and the potential financial policy will also be settled by this top-down segment authority.
On the other hand, the bottom-up segment will be responsible for implementing the developed systems through capacity building of stakeholders, creating skilled manpower by ensuring training and education, awareness development, creating social enterprises, monitoring and evaluation, and performance review and evaluation of the system. This comprehensive approach (top-down and bottom-up) could ensure sustainable medical waste management in the Rohingya camp in Bangladesh.
In 2008, Bangladesh’s government established the country’s first laws governing the handling of biomedical waste. That is entitled “Bangladesh Medical Waste (Management and Processing) Rules 2008”(Bio-Medical Waste Management (Amendment) Rules (BMD), 2008) and governed by the Environment Conservation Rules, 1997 (ECR′97), the Bangladesh Environmental Conservation Act (1995) (Amended in 2010). According to medical waste management and processing rules 2008, waste should be segregated at the generation source in definite color-coded bins. Then this waste should be treated according to its category. Waste treatment methods are fixed for each type. There were also guidelines and standards fixed for treatment methods and safe disposal. A strong penalty is also mentioned for violation of these rules are also enacted. Above all the strengths, it also suffers from various weaknesses. Due to interministerial disagreements and rivalry among the authorities, the rules were not well implemented. Even after 13 years, the national advisory council was never established because of the rivalry between the authorities. The 2008 regulations did not specify the roles and responsibilities of government entities such as the Department of Environment (DoE), which is part of the Ministry of Environment, Forest, and Climate Change, the Directorate General of Health Services (DGHS), which is part of the Ministry of Health and Family Welfare, and the Dhaka North and South City Corporations (DNCC/DSCC), which are in charge of managing municipal solid waste and medical waste, respectively. A major weakness is that there is no strong monitoring team to ensure this management. The standard and treatment method should also improve with modern technology. There should be a provision for reporting system in every healthcare facility. Record of waste generation and treatment must be kept in a log book.
Medical waste is any by-product of medical institutes, hospitals, health camps, pharmacies, pathologies, or other related organizations and establishments. In Rohingya camps, 88% of people are familiar with the hazardous effects of the mismanagement of waste. The knowledge rate about waste management is comparatively more satisfied than in other studies (Alomari et al., 2021). This is probably due to the benefit of different NGOs working in campsites.
A total of 91% of respondents said solid waste in Rohingya camps must be managed properly. They are found in roads, open places, and drains. This scenario is similar to the study of Nigeria (Orhorhoro and Oghoghorie, 2019) and the United States (Abdel-Shafy and Mansour, 2018). That indicates the mismanagement of solid waste worldwide and in the Rohingya camps.
Medical items are available to purchase from outside the healthcare camp. They can easily buy medical items from outside. But medical items sold and purchased in campsites are forbidden (De Montclos and Kagwanja, 2000; Werker, 2007). This medical item by-product medical waste needs to be properly handled. They generally mixed it with household waste or dumped it on roadsides or other open places. It converts general waste to infectious or hazardous waste (Jang et al., 2006; Oroei et al., 2014). This presents health risks to the surrounding community, waste management workers, and the environment.
Healthcare facilities generate medical waste of around 2 kg daily. The medical waste generation rate in healthcare camps is lower than in different hospitals (Cheng et al., 2009; Taghipour and Mosaferi, 2009). The medical waste is properly segregated in different color-coded plastic bins. Among different types of medical waste, liquid waste generation is very low in Rohingya camp healthcare centers. According to them, 71% have their own waste management facilities, 14% took help from a third party, and the rest open-dumped this waste. Generally, Wash and upazila health complex are the third party in Rohingya camp medical waste management.
Medical waste, such as sharp waste, may carry germs of diseases such as hepatitis B and AIDS (Henry et al., 1990; Almuneef and Memish, 2003)). This waste also increase the risk of exposure range from gastro-enteric, respiratory, Ocular infection, Anthrax, Meningitis, Acquired immunodeficiency syndrome (AIDS), Viral hepatitis A, B &C, Avian influenza, Haemorrhagic fevers, Septicaemia, Bacteraemia, and skin problems to more lethal diseases such as HIV/AIDS and Hepatitis (Rao, 2008; Babanyara and Ibrahim, 2013; New WHO Handbook on Healthcare Waste Management, 2013). Around 5.2 million people (including 4 million children) die annually from waste-related diseases globally (Akter, 2000). Despite this progress, in 2010, unsafe injections were still responsible for as many as 33 800 new HIV infections, 1.7 million hepatitis B infections, and 315 000 hepatitis C infections (Pépin et al., 2014). Furthermore, medical waste contains potentially hazardous microorganisms that might infect hospital patients, healthcare employees, and the general public. Additional potential infectious concerns include the transmission of drug-resistant microorganisms from healthcare facilities into the environment. It may also threaten doctors, patients, workers of HCF, workers of solid waste management workers, waste collectors, transporters, and visitors. Al-Khatib, (2013a) also mentioned the health risk of waste workers in his study. In another study, Jagger, (1999) reported that workers in support services linked to low-level health facilities (LLHFs) such as laundries, waste handling, and transportation service are often at risk.
In general, sharp waste management is a significant problem due to its ever-growing and endless generation. Though sharp waste constitutes a small fraction of solid medical waste, its potential environmental and health hazards could be deleterious if improperly handled. Syringes and needles are of particular concern because they constitute an essential part of the sharp waste and often are contaminated with patient body fluids.
The major concern of medical waste management in Rohingya camps is medical waste found in communal bins. This waste is mostly glass bottles, plastic bottles, syringes, and saline bags. Data from the MRF shows that 0.05% of the waste they collected is medical waste. This data also cleared that medical waste generation increased in the winter season. A study in Southern Gana also found medical waste in their daily communal bin. The probability of founding this waste was 89% (Udofia et al., 2017). Brazil (Da Silva et al., 2005) and Korea (Jang et al., 2006) also faced similar patterns of a problem in managing their waste. If medical waste is mixed with general waste in this process, it increases the volume of infectious waste, as it can contaminate general waste. For that reason, if this mixing process continues in Rohingya camps, it will create a considerable health risk for the camp community, the surrounding local community, SWM workers, and the environment (Al-Khatib, 2013b). It will also create a crucial burden for sustainably managing waste.
Another major concern is that the health camps of in the Rohingya camps also suffer from a lack of infrastructure facilities and water facilities, power shortage, area shortage, and inadequate training and proper monitoring systems. This causes a serious hamper in the medical waste management sector. Moreover, none of the health camps treated their liquid waste. According to them, the generation of this type of waste inside the health camp is very low. In addition, there is no provision for maintaining log books for medical waste generation and treatment entry. It creates a loop in proper medical waste management procedures. There is also no standard operating procedures (SOPs) or specific guideline maintaining rules for the health camps. That makes mismanagement in medical waste management. A lack of strong monitoring or regulating body and improper training makes it worst.
Overall medical waste management in a humanitarian context is challenging, as basic human needs are not adequately available. But the current situation of the Rohingya camp is comparatively well organized than Palestine (Al-Khatib, 2007; Al-Khatib, 2008). But adequate steps must be taken for proper waste management in Rohingya camps.
Medical waste management guideline for Rohingya camp is created based on the field experience of health camp from KII, FGD, IDI, and the available literature. Medical waste from the health camp can be treated in two ways. One is being treated at an on-site waste management facility, and another is being handed over to a third party after disinfecting. HCF should record the amount of medical waste generation and treated waste amount. They must submit a report every month to the corresponding authorities. All of the processes must be regulated by a proper monitoring system and strong penalties must be fixed in case of violating guidelines.
At first, camp medical waste must be segregated in color-coded bins like Figure 9. Infectious waste must be disinfected using an autoclave or chemical disinfection. If there is no lack of electricity issues, then they can use an autoclave. Otherwise, they will use a chemical disinfection process. Then, after disinfecting, sharp and pharmaceutical waste should be transferred to a deep burial pit, ash pit, or placenta pit. After this process, the end product can be disposed to a landfill site, or the material recovery site for reused and recycling. General waste can be transferred to a communal bin and handover to a third party (Figure 9). If liquid waste is produced in HCF then it will go through a chemical disinfection process. All medical waste management workers must wear proper PPE (personal protective equipment) to protect them from the hazardous effects of medical waste. The authority for medical waste management must adequately follow the occupational health and safety rules, as this profession has many occupational health risks (Al-Khatib, 2013a). Moreover, if it is needed to store medical waste in the on-site treatment plant or HCF, it must be stored by properly maintaining medical waste storage guidelines (WHO, 2005a; Al-Khatib, 2013b). In addition, medical waste management workers and authorities at HCF, On-site, and off-site treatment plants must be adequately trained. They should know the importance of medical waste management and its mismanagement effect. All of the processes must be monitored by a strong regulatory body. If any non-conformity occurs, then there must be rules and regulations for penalty. Moreover, all of the treatment quality standards must satisfy the Medical waste management rules 2008 and WHO guidelines.
Off-site management can be done in a definite place, where HCF waste will be collected from every camp HCF facility and treated separately (Figure 10). This place can be the nearest Upazila healthcare establishment. As it already managed the HCF waste. But proper infrastructure, training, and logistic support must be ensured for the HCF workers of the Upazila complex. At first infectious waste must be disinfected by autoclaving or microwaving, or a chemical disinfection process depending on the availability of electricity. Then it can be further treated in a deep burial pit or ash pit or placenta pit or sharp pit. Pharmaceutical waste (expired medicine, saline, discarded vials) can be chemically disinfected and further treated by a deep burial pit, ash pit, or sharp pit. Sharp waste (needles, broken vials) must be decontaminated by autoclaving or shredding. Then it can be further treated by deep burial pit or ash pit or sharp pit or incineration. General waste can be reused, recycled, or handed over to a third party. In the case of liquid waste, it goes through a chemical disinfection process. Moreover, occupational health safety protocols for waste management workers must also be implemented appropriately (Al-Khatib, 2013a). If waste needs to keep stored for off-site treatment, then it should also follow the guideline of medical waste storage (WHO, 2005b; Al-Khatib, 2013b).
There were several medical waste guidelines for the safe handling and disposal of medical waste worldwide (WHO, 1999; UNEP, 2001; WHO, 2005a; UNEP, 2006; UNDP, 2010; DoE, 2012; Medical Waste US EPA, 2022; New WHO Handbook on Healthcare Waste Management, 2013). All of the rules and guidelines go through different amendments and improvements several times. Treatment methods for medical waste depend on the characteristics, quantification, capacity, financial capability, space, infrastructure, operation procedure, and skills to handle medical waste. The available technologies for MWM are thermal process, chemical process, radiation technology, biological process, and mechanical process. In Asian regions, the technology mostly used for medical waste treatment is the autoclave, incineration, chemical disinfection, microwaving, deep burial pit, ash pit, placenta pit, hydrolysis, encapsulation, and pyrolysis (Bio-Medical Waste Management (Amendment) Rules (BMD); Manekar et al., 2022; Medical Waste Management Rules in Pakistan, 2005; The Medical Waste Management Rules, 2008; Ye et al., 2022; Yong et al., 2009).
Waste treatment methods may also pose a threat to humankind. In the incineration process, flue gas is created. This flue gas has a destructive impact on the human body. This effect is also worst when the incineration process is poorly managed. If poorly managed, it also produces volatile metals, polycyclic aromatic hydrocarbons, particulates, dioxins, and furans (Fritsky et al., 2001; Lee et al., 2002; Segura-Muñoz et al., 2004; Al-Khatib, 2013a). This causes damage to our lungs, kidneys, immune system, and neurological system. Some of them are also carcinogenic, it also capable of creating cancer. Ash from incineration, placenta pits, and deep burial pits also poses a health threat to humankind. When sharp waste is handled, it also threatens to cut our bodies. Autoclaving procedures, chemical disinfection, and microwaving must be done carefully, because if temperature and other parameters are not properly maintained, it will create serious health threats for the physical properties of waste. Post-treatment water should also be properly maintained because it contains hazardous organic and inorganic compounds. Deep burial pits, ash pits, placenta pits, and landfill should also contain the threat of creating odour, smoke, and leachate. For that reason, following proper guidelines according to surrounding circumstances is essential when treating this waste.
The disposal of medical waste is a growing environmental problem in the Rohingya refugee camps, owing to the absence of proper management facilities, knowledge, and establishments. In these camps, the management of solid waste has gained attention, but the management of medical waste has received little attention. But medical waste is capable of imposing potential environmental hazards and public health risks on camp people and surroundings. The study has attempted to quantify different medical wastes generated in community places in the study area camp-15. Both non-infectious and infectious wastes were found to be generated in these places. Our field data show that community people do not segregate their generated wastes, and they dispose of their domestic waste at the same site as regular solid waste. Data analysis shows no specific handling process or collection system in camps for MWM. With the complete picture in view, the authors suggest a holistic management system for medical waste in the humanitarian context for the safeguarding of the environment and public health.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the participants was not required to participate in this study in accordance with the national legislation and the institutional requirements.
MH: conceptualization, data acquisition, analysis, manuscript preparation FC: data acquisition, analysis, manuscript preparation AH: data acquisition, field survey, analysis RA: analysis, manuscript preparation MR: conceptualization, data acquisition, analysis, manuscript preparation, supervision. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fenvs.2023.1149314/full#supplementary-material
Abdel-Shafy, H. I., and Mansour, M. S. M. (2018). Solid waste issue: Sources, composition, disposal, recycling, and valorization. Egypt. J. Petroleum 27 (4), 1275–1290. doi:10.1016/J.EJPE.2018.07.003
ADB (2020). Managing infectious medical waste during the COVID-19 pandemic. Mandaluyong, Philippines: Asian Development Bank.
Akter, N. (2000). Medical waste management: A review. Available at:https://www.researchgate.net/publication/228409823_Medical_waste_management_a_review (Accessed February, 2000).
Al-Khatib, I. A. (2008). Management of solid medical waste in the private medical sector in the Occupied Palestinian Territory: Problems and remedial measures. East. Mediterr. Health J. WHO 14 (5), 1164–1172.
Al-Khatib, I. A. (2013a). Impact of medical waste handling on the occupational safety for cleaners in the hospitals of the city of Jenin, Palestine. Dirasat J. Eng. Sci. 39 (1), 1–11.
Al-Khatib, I. A., Khalaf, A. S., Al-Sari, M. I., and Anayah, F. (2020). Medical waste management at three hospitals in Jenin district, Palestine. Environ. Monit. Assess. 192 (1), 10–15. doi:10.1007/s10661-019-7992-0
Al-Khatib, I. A. (2007). Medical waste management in healthcare centers in the Occupied Palestinian Territory. World Health Organ. East. Mediterr. Health J. 13 (3), 694–705.
Al-Khatib, I. A. (2013b). Problems of management of medical solid waste at primary health care centres in the Palestinian Territory and their remedial measures. East. Mediterr. Health J. 19 (3), S152–S158.
Alam, J. (2019). The current Rohingya crisis in Myanmar in historical perspective. J. Muslim Minority Aff. 39 (1), 1–25. doi:10.1080/13602004.2019.1575560
Almuneef, M., and Memish, Z. A. (2003). Effective medical waste management: It can be done. Am. J. Infect. Control 31 (3), 188–192. doi:10.1067/mic.2003.43
Alomari, A. H., Aga, O., El Sahmarany, L., Hegazi, M., and Almulla, L. (2021). Public perception towards medical waste generated in the environment during the COVID-19 pandemic in Eastern Province, Saudi Arabia. Heliyon 7 (11), e08363. doi:10.1016/J.HELIYON.2021.E08363
Andrew, T., Luca, V., Angeliki;, N., Luca;, P. K. G., and Daniele, D. V. (2021). Inform report 2021. Luxembourg: Publications Office of the European Union.
Babanyara, Y. Y., and Ibrahim, D. (2013). Poor medical waste management (MWM) practices and its risks to human health and the environment: A literature review energy efficiency evaluation for residential buildings view project environmental pollution view project. Int. J. Environ. Ecol. Geol. Min. Eng. 7, 512–519.
Barua, U., and Hossain, D. (2021). A review of the medical waste management system at Covid-19 situation in Bangladesh. J. Material Cycles Waste Manag. 23 (6), 2087–2100. doi:10.1007/s10163-021-01291-8
Bio-Medical Waste Management (Amendment) Rules (BMD) (2008). The Medical Waste Management Rules, 2008 - Chancery Law Chronicles. http://www.clcbd.org/document/133.html#google_vignette (Retrieved from: July 4, 2023).
Birchard, K. (2002). Out of sight, out of mind.the medical waste problem. Lancet 359 (9300), 56. doi:10.1016/S0140-6736(02)07256-2
Biswas, A., Amanullah, A., and Santra, S. (2011). Medical waste management in the tertiary hospitals of Bangladesh: An empirical enquiry. ASA Univ. Rev. 5 (2), 10.
Büyüközkan, G., and Ilıcak, Ö. (2019). Integrated SWOT analysis with multiple preference relations: Selection of strategic factors for social media. Kybernetes 48 (3), 451–470. doi:10.1108/k-12-2017-0512
Chauhan, A., and Singh, A. (2016). Healthcare waste management: A state-of-the-art literature review. Int.J. Environ. Waste Manag. 18 (2), 120–144. doi:10.1504/ijewm.2016.080400
Cheng, Y. W., Sung, F. C., Yang, Y., Lo, Y. H., Chung, Y. T., and Li, K. C. (2009). Medical waste production at hospitals and associated factors. Waste Manag. 29 (1), 440–444. doi:10.1016/J.WASMAN.2008.01.014
Da Silva, C. E., Hoppe, A. E., Ravanello, M. M., and Mello, N. (2005). Medical wastes management in the south of Brazil. Waste Manag. 25 (6), 600–605. doi:10.1016/J.WASMAN.2004.03.002
De Montclos, M. A. P., and Kagwanja, P. M. (2000). Refugee camps or cities? The socio-economic dynamics of the dada and kakuma camps in northern Kenya. J. Refug. Stud. 13 (2), 205–222. doi:10.1093/JRS/13.2.205
DoE (United States Department of Energy) (2012). Thermal treatment technologies [fact sheet]. Argonne, IL: Argonne National Laboratory.
Ekezie, W., Timmons, S., Myles, P., Siebert, P., Bains, M., and Pritchard, C. (2019). An audit of healthcare provision in internally displaced population camps in Nigeria. J. Public Health (Oxford, Engl. 41 (3), 583–592. doi:10.1093/PUBMED/FDY141
Fritsky, K., Kumm, J., and Wilken, M. (2001). Combined PCDD/F destruction and particulate control in a baghouse: Experience with a catalytic filter system at a medical waste incineration plant. J. Air Waste Manag. Assoc. 51, 1642–1649. doi:10.1080/10473289.2001.10464391
Hasnat, A., and Sinha, M. (2010). Technical assistance consultant ’ s report managing hazardous wastes. Mandaluyong, Philippines: Asian Development Bank.
Hassan, M. M., Ahmed, S. A., Rahman, K. A., and Biswas, T. K. (2008). Pattern of medical waste management: Existing scenario in Dhaka City, Bangladesh. BMC Public Health 8, 36–10. doi:10.1186/1471-2458-8-36
Henry, K., Campbell, S., Jackson, B., Balfour, H., Rhame, F., Sannerud, K., et al. (1990). Long-term follow-up of health care workers with work-site exposure to human immunodeficiency virus. JAMA 263 (13), 1765–1766. doi:10.1001/jama.1990.03440130045016
Jagger, J. (1996). Reducing occupational exposure to bloodborne pathogens: Where do we stand a decade later? Infect. Control Hosp. Epidemiol. 17 (9), 573–575. doi:10.2307/30141942
Jang, Y. C., Lee, C., Yoon, O. S., and Kim, H. (2006). Medical waste management in Korea. J. Environ. Manag. 80 (2), 107–115. doi:10.1016/J.JENVMAN.2005.08.018
Jeffries, R., Abdi, H., Ali, M., Bhuiyan, A. T. M. R. H., Shazly, M. E., Harlass, S., et al. (2021). The health response to the Rohingya refugee crisis post August 2017: Reflections from two years of health sector coordination in Cox’s Bazar, Bangladesh. PLoS ONE 16, e0253013–e0253015. doi:10.1371/journal.pone.0253013
Karsu, O., Kara, B. Y., and Selvi, B. (2019). The refugee camp management: A general framework and a unifying decision-making model. J. Humanit. Logist. Supply Chain Manag. 9 (2), 131–150. doi:10.1108/jhlscm-01-2018-0007
Kenny, C., and Priyadarshini, A. (2021). Review of current healthcare waste management methods and their effect on global health. Healthc. Switz. 9 (3), 284. doi:10.3390/healthcare9030284
Khalid, S., Haq, N., Sabiha, Z. U. A., Latif, A., Khan, M. A., Iqbal, J., et al. (2021). Current practices of waste management in teaching hospitals and presence of incinerators in densely populated areas. BMC Public Health 21 (1), 1340–1410. doi:10.1186/s12889-021-11389-1
Krejcie, R. V., and Morgan, D. (1970). Determining sample size for research activities. NEA Res. Bull. 30, 607–610. doi:10.1177/001316447003000308
Kwikiriza, S., Stewart, A. G., Mutahunga, B., Dobson, A. E., and Wilkinson, E. (2019). A whole systems approach to hospital waste management in rural Uganda. Front. Public Health 7, 136. doi:10.3389/fpubh.2019.00136
Lee, W-J., Liow, M. C., Tsai, P. J., and Hsieh, L. T. (2002). Emission of polycyclic aromatic hydrocarbons from medical waste incinerators. Atmos. Environ. 36, 781–790. doi:10.1016/s1352-2310(01)00533-7
Lewis, D. (2019). Humanitarianism, civil society and the Rohingya refugee crisis in Bangladesh. Third World Q. 40 (10), 1884–1902. doi:10.1080/01436597.2019.1652897
MacLean, K. (2019). The Rohingya crisis and the practices of erasure. J. Genocide Res. 21 (1), 83–95. doi:10.1080/14623528.2018.1506628
Manekar, S. S., Bakal, R. L., Jawarkar, R. D., and Charde, M. S. (2022). Challenges and measures during management of mounting biomedical waste in COVID-19 pandemic: An Indian approach. Bull. Natl. Res. Centre 46 (1), 159–9. doi:10.1186/S42269-022-00847-4
Mbongwe, B., Mmereki, B. T., and Magashula, A. (2008). Healthcare waste management: Current practices in selected healthcare facilities, Botswana. Waste Manag. 28 (1), 226–233. doi:10.1016/j.wasman.2006.12.019
Medical Waste US EPA (2022). EPA issues hazardous medical waste disposal guide - Recycling Today. (n.d.). https://www.recyclingtoday.com/news/epa-medical-waste-hazardous-guide-disposal/ (Retrieved from: July 4, 2023).
Medical waste management rules in pakistan (2023). Medical waste management rules in Pakistan - google Search. Available at: https://www.google.com/search?q=medical+waste+management+rules+in+pakistan (Accessed April 16, 2023).
Mitiku, G., Admasie, A., Birara, A., and Yalew, W. (2022). Biomedical waste management practices and associated factors among health care workers in the era of the Covid-19 pandemic at metropolitan city private hospitals, Amhara region, Ethiopia, 2020. PLOS ONE 17 (4), e0266037. doi:10.1371/JOURNAL.PONE.0266037
Mohee, R. (2005). Medical wastes characterisation in healthcare institutions in Mauritius. Waste Manag. 25 (6), 575–581. doi:10.1016/j.wasman.2004.10.003
New WHO Handbook on Healthcare Waste Management (2013). New WHO Handbook on healthcare waste management | health care without harm. Available at: https://noharm-global.org/articles/news/global/new-who-handbook-healthcare-waste-management (Accessed April 16, 2023).
Oka, R. C. (2014). Coping with the refugee wait: The role of consumption, normalcy, and dignity in refugee lives at kakuma refugee camp, Kenya. Am. Anthropol. 116 (1), 23–37. doi:10.1111/AMAN.12076
Oli, A. N., Ekejindu, C. C., Adje, D. U., Ezeobi, I., Ejiofor, O. S., Ibeh, C. C., et al. (2016). Healthcare waste management in selected government and private hospitals in Southeast Nigeria. Asian Pac. J. Trop. Biomed. 6 (1), 84–89. doi:10.1016/j.apjtb.2015.09.019
Orhorhoro, E. K., and Oghoghorie, O. (2019). Review on solid waste generation and management in sub-saharan africa: A case study of Nigeria. J. Appl. Sci. Environ. Manag. 23 (9), 1729–1737. doi:10.4314/jasem.v23i9.19
Oroei, M., Momeni, M., Palenik, C. J., Danaei, M., and Askarian, M. (2014). A qualitative study of the causes of improper segregation of infectious waste at Nemazee Hospital, Shiraz, Iran. J. Infect. Public Health 7 (3), 192–198. doi:10.1016/J.JIPH.2014.01.005
Pépin, J., Chakra, C. N. A., Pépin, E., Nault, V., and Valiquette, L. (2014). Evolution of the global burden of viral infections from unsafe medical injections, 2000-2010. PLoS ONE 9 (6), 1–8. doi:10.1371/journal.pone.0099677
Prem Ananth, A., Prashanthini, V., and Visvanathan, C. (2010). Healthcare waste management in Asia. Waste Manag. 30 (1), 154–161. doi:10.1016/j.wasman.2009.07.018
Rao, P. H. (2008). Report: Hospital waste management-awareness and practices: A study of three states in India. Waste Manag. Res. J. Int. Solid Wastes Public Clean. Assoc. ISWA 26 (3), 297–303. doi:10.1177/0734242X08088693
Segura-Muñoz, S. I., Takayanagui, A. M. M., Trevilato, T. M. B., Santos, C. B., and Hering, S. E. (2004). Trace metal distribution in surface soil in the area of a municipal solid waste landfill and a medical waste incinerator. Bull. Environ. Contam. Toxicol. 72, 157–164. doi:10.1007/s00128-003-0254-3
Shammi, M., Rahman, M. M., Ali, M. L., Khan, A. S. M., Siddique, M. A. B., Ashadudzaman, M., et al. (2022). Application of short and rapid strategic environmental assessment (SEA) for biomedical waste management in Bangladesh. Case Stud. Chem. Environ. Eng. 5, 100177. doi:10.1016/j.cscee.2021.100177
Skondras, N. A., and Karavitis, C. A. (2015). Evaluation and comparison of DPSIR framework and the combined swot–dpsir analysis (csda) approach: Towards embracing. Glob. NEST J. 17 (1), 198–209.
Taghipour, H., and Mosaferi, M. (2009). Characterization of medical waste from hospitals in Tabriz, Iran. Sci. Total Environ. 407 (5), 1527–1535. doi:10.1016/J.SCITOTENV.2008.11.032
The Medical Waste Management Rules (2008). The medical waste management rules, 2008 - chancery law chronicles. Available at: http://www.clcbd.org/document/133.html#google_vignette (Accessed April 16, 2023).
Tong, A., Sainsbury, P., and Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 19 (6), 349–357. doi:10.1093/INTQHC/MZM042
Tscherning, K., Helming, K., Krippner, B., Siebe, S., and y Paloma, S. G. (2012). Does research applying the DPSIR framework support decision making? Land use policy 29 (1), 102–110. doi:10.1016/j.landusepol.2011.05.009
Udofia, E. A., Gulis, G., and Fobil, J. (2017). Solid medical waste: A cross sectional study of household disposal practices and reported harm in southern Ghana. BMC Public Health 17 (1), 464. doi:10.1186/s12889-017-4366-9
UNDP (United Nations Development Programme) (2010). Guidance on the clean-up, temporary or intermediate storage, and transport of mercury waste from healthcare facilities. Geneva: United Nations Development Programme Global Environment Facility Project on Healthcare Waste and Secretariat of the Basel Convention.
UNEP (2006). Guidelines on best available techniques and provisional guidance on best environmental practices relevant to Article 5 and Annex C of the Stockholm Convention on Persistent Organic Pollutants. Geneva: Secretariat of the Stockholm Convention.
UNEP (United Nations Environment Programme) (2001). Thailand dioxin sampling and analysis program – report. Geneva: United Nations Envronment Programme Chemicals.
Vardopoulos, I., Konstantopoulos, I., Zorpas, A. A., Limousy, L., Bennici, S., Inglezakis, V. J., et al. (2021). Sustainable metropolitan areas perspectives through assessment of the existing waste management strategies. Environ. Sci. Pollut. Res. 28 (19), 24305–24320. doi:10.1007/s11356-020-07930-1
Wassie, B., Gintamo, B., Mekuria, Z. N., and Gizaw, Z. (2022). Healthcare waste management practices and associated factors in private clinics in addis ababa, Ethiopia. Environ. Health Insights 16, 117863022110733–10. doi:10.1177/11786302211073383
WHO (1980). Glossary on solid waste, Copenhagen. Copenhagen, Denmark: World Health Organization Regional Office for Europe.
WHO (2005a). “Safe management of bio-medical sharps waste in India: A report on alternative treatment and nonburn disposal practices. Geneva: World Health Organization.
WHO (World Health Organization) (1999). Guidelines for the safe disposal of unwanted pharmaceuticals in and after emergencies. Geneva: World Health Organization.
WHO (World Health Organization) (2005b). Management of solid health-care waste at primary health-care centres: A decision-making guide. Geneva: World Health Organization.
Windfeld, E. S., and Brooks, M. S. L. (2015). Medical waste management - a review. J. Environ. Manag. 163, 98–108. doi:10.1016/j.jenvman.2015.08.013
Ye, J., Song, Y., Liu, Y., and Zhong, Y. (2022). Assessment of medical waste generation, associated environmental impact, and management issues after the outbreak of COVID-19: A case study of the hubei province in China. PLOS ONE 17 (1), e0259207. doi:10.1371/JOURNAL.PONE.0259207
Yong, Z., Gang, X., Guanxing, W., Tao, Z., and Dawei, J. (2009). Medical waste management in China: A case study of nanjing. Waste Manag. 29 (4), 1376–1382. doi:10.1016/J.WASMAN.2008.10.023
Keywords: health care facility, medical waste management, SWOT, DPSIR, WHO, health risk
Citation: Haque MR, Chowdhury FN, Hossain A, Akter R and Rahman MM (2023) An emerging concern of medical waste management in Rohingya refugee camps at Cox’s Bazar, Bangladesh: existing practice and alternatives. Front. Environ. Sci. 11:1149314. doi: 10.3389/fenvs.2023.1149314
Received: 21 January 2023; Accepted: 16 June 2023;
Published: 13 July 2023.
Edited by:
Zhenming Zhang, Guizhou University, ChinaReviewed by:
Issam A. Al-Khatib, Birzeit University, PalestineCopyright © 2023 Haque, Chowdhury, Hossain, Akter and Rahman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Md. Mostafizur Rahman, cmFobWFubW1AanVuaXYuZWR1
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.