- 1AIRESS, FGSES, Mohammed VI Polytechnic University (UM6P), Ben Guerir, Morocco
- 2Department of Economics, University of Ghana, Accra, Ghana
- 3Regional Institute of Population Studies, University of Ghana, Accra, Ghana
This study investigates the impact of household cooking fuel choice on household healthcare expenditure as well as the socioeconomic and demographic factors that influence household healthcare expenditure. We employed the Tobit regression technique and data from the sixth and seventh rounds of the Ghana Living Standards Survey conducted in 2012/13 and 2016/17, respectively. The results indicate that in 2012/13, relative to households using wood as cooking fuel, households using charcoal and liquefied petroleum gas are 54.40 and 115.09 percentage points less likely to spend on healthcare services. However, the figure reduced to 28.15 and 103.25 percentage points in 2016/17 attributable possibly to a reduction in biomass energy use resulting from government liquefied petroleum gas promotion programs which helped households transition to the use of cleaner fuels. Age, education, illness reporting of the household head, total household expenditure, household size, and region of residence were found to be the determinants of household healthcare expenditure. Policy choices should focus on the use of cleaner fuel options including sustaining and extending the rural liquefied petroleum gas promotion program as well as reducing the use of dirty fuels.
1 Introduction
In many developing countries, the dependence on traditional fuels like biomass and firewood for domestic purposes is predominant as about 3 billion people depend on such fuels for cooking, heating, and lighting, and about 650 million people in Sub-Saharan Africa (SSA) will continue depending on biomass until 2040 for cooking and heating in an unsafe way (Africa Energy Outlook, 2014), while a survey of 18 African countries by the World Health Organization (WHO), 2016) shows that about 95% of households depend primarily on biomass fuels for domestic purposes. In Ghana, the Ghana Statistical Service (GSS, 2019) estimates that about 80 percent of households depend on biomass for cooking and heating.
The quest to ensure energy transition has raised concern among policymakers about the need to pay more emphasis on the impact of traditional fuel use on health and the environment (Muller and Yan, 2018), particularly among households with bad ventilation or inappropriate cookstoves (Badamassi et al., 2017). The WHO (2016) and Kamila et al. (2014) report that biomass use ranks as the most significant environmental health risk factor responsible for respiratory infections and cardiovascular diseases that have caused about 4.3 million deaths worldwide in 2012, while the Africa Energy Outlook (2014) estimates that 600,000 premature deaths occur annually in Africa from indoor air pollution. The situation is not different from what pertains to Ghana as Inkoom and Crensti (2015) report that biomass fuel use accounts for about 16,600 deaths annually.
The significant impact of dirty fuel use on health has allowed the government of Ghana to enhance its programs on the use of cleaner fuels. As such, the Rural Liquefied Petroleum Gas (LPG) Promotion Program and the Cylinder Recirculation Model were introduced (Asante et al., 2018) to increase LPG access (Asante et al., 2018), while financial motivations were provided to LPG transporters covering rural areas (Ahunu, 2015). Moreover, the government through subsidies reduced the price of LPG. Despite these policies and increased households’ income, less than a quarter of Ghanaians use LPG for cooking and heating (Karimu et al., 2016), while the impact of household cooking fuel choice on healthcare expenditure has not been assessed.
Several studies such as Alem et al. (2016), Karimu et al. (2016), Karakara and Dasmani (2019), Karakara et al. (2021), Mensah and Adu (2015), Ofori et al. (2018), and Olang et al. (2018) have focused on the determinants of household cooking fuel choice in developing countries including Ghana with some exploring these determinants in clean versus dirty energy. The problem with these studies is that they failed to consider the issue of energy choice and healthcare issues.
Others such as Karakara and Osabuohien (2020), Baumgartner et al. (2011), Khan and Lohano (2018), and Ofori et al. (2018) attempt to address this challenge by looking at the impacts of household cooking fuel choice on human health with many of them focusing on specific health conditions. For example, Ofori et al. (2018) explored the link between household dirty fuels use and blood pressure among women in southern Nigeria.
By harming people’s health, household cooking fuel choice is expected to have a profound influence on healthcare expenditures (Badamassi et al., 2017) and consequently on poverty reduction efforts that need attention. To our knowledge, very little research has been carried out on the impact of household cooking fuel choice on healthcare expenditure with most focusing on macro-analysis. However, little is known about households’ cooking fuel choice and its impact on healthcare expenditure in Ghana at the microlevel. It is against this background that this study aims at examining the impact of household cooking fuel choice on healthcare expenditure as well as the socioeconomic and demographic variables that impact healthcare expenditure.
Analyzing the impact of household cooking fuel choice on healthcare expenditure will enable the government to assess the impact of its programs on the use of cleaner fuels in households as well as design policy choices on energy and health in line with Sustainable Development Goals 3 and 7 on healthy lives and well-being for all and universal access to affordable, reliable, and modern energy services, respectively, and consequently on goal 1 on income poverty since health and energy poverty issues are significant contributors to income poverty. The study has four sections. Following this section is Section 2 which reviews the literature on the subject, while Section 3 provides the methodology, and Section 4 discusses the results. The Section 5 concludes the study.
2 Literature Review
2.1 Theoretical Review
In the literature, two main models explain households’ choice of cooking fuel: the energy ladder and fuel stacking theory. The energy ladder model postulates that as households’ income increases, they move away from more costly, more polluting, and less efficient technologies to more costly, less polluting, and more efficient technologies (Muller and Yan, 2018). The model has been used by scholars such as Hiemstra-van der Horst and Hovoka (2008) and Treiber (2012) to explain household fuel-switching patterns. The model has, however, been criticized by Hiemstra-van der Horst and Hovorka (2008) and Jebaraj and Iniyan (2006) for focusing only on income to the detriment of social and cultural factors on fuel choice, and the consumer rationality assumption of linear path movement from one fuel source to another.
Contradicting the energy ladder model, the fuel stacking theory argues that households adopt a multiple fuel use approach in which modern fuels are added to traditional fuels and not completely removed as households’ income increases (Martins, 2005; Treiber, 2012). In addition toincome, the theory perceived factors such as fuel accessibility and availability, household cooking practices, and health impact as the main drivers influencing households’ fuel-switching decisions previously neglected by the energy ladder model (Hosier and Dowd 1987). Multiple fuel use is practiced by many households in developing countries by climbing up and down the energy ladder instead of the traditional linear fuel switching (Leach, 1992; Martins, 2005).
Models on the impact of households’ cooking fuel choice on health and consequently healthcare expenditure have centered on the environmental health pathway developed by Smith and Pillarisetti (2017). The concept posits that indoor air pollution starts with sources of pollution, moves to environmental levels, then to human exposures and doses within the body, and finally to health impacts. It provides a better understanding of pollution risks associated with using household cooking fuel, especially biomass fuels.
2.2 Empirical Review
Empirically, what determines household healthcare expenditure in the developing world has been well researched with many diverse results. Using the 2010 household income and expenditure survey and the ordinary least square (OLS) technique, Molla et al. (2017) investigated the determinants of out-of-pocket healthcare expenditure in Bangladesh. The authors concluded that urban households spend more on healthcare than rural dwellers and those factors such as income, ill-health, and household size were the main predictors of healthcare expenditure. Similar research carried out in China by You and Kobayashi (2011) using the 2004 China Health and Nutrition Survey data and the Heckman selection model examined the determinants of out-of-pocket health expenditure. They concluded that age, educations, and income of households were positive predictors of household health expenditure while urban households compared to rural spend more on health.
Malik and Syed (2012) explored factors influencing healthcare expenditure in Pakistan using the 2004/5 Pakistan Standard of Living Measurement Survey dataset and the OLS and established that non-food household expenditure and household characteristics were significant determinants of household healthcare expenditure. In general, factors such as the presence of illness, income, health insurance, and residence location, among others are prominently highlighted in many studies related to determinants of healthcare expenditure (Akanda et al., 2011; Molla et al., 2017).
Many studies have also examined the impact of household cooking fuel choices on health and the environment in the developing world. A recent study by Khan and Lohano (2018) found that children in households using modern fuels are less likely to have symptoms of respiratory infection than those in households using traditional fuels using the 2012/2013 Pakistan Demographic and Health Survey and the logistic model. A similar study by Acharya et al. (2015) found that the use of solid fuel in kitchens is a risk factor for acute respiratory tract infection among under-five children in Nepal using the 2011 Nepal Demographic and Health Survey.
Investigating the impact of residential fuel combustion on health expenditures in 44 Sub-Saharan African countries, Badamassi et al. (2017) employed the general method of moments (GMM) technique. Their results showed that residential fuel combustion was significantly correlated with higher health expenditures. The authors proposed health policies that boost households’ access and use of modern fuels and improved cookstoves use in SSA. Capuno et al. (2018) in their study revealed that the use of clean fuel can lower the incidence of severe coughing in young children by 2.4 percentage points in the Philippines using the propensity score matching method and the 2013 National Demographic and Health Survey.
Using baseline data from a randomized controlled trial of an improved household energy initiative and the logit model in Rwanda, Das et al. (2018) concluded that children are more likely to experience symptoms of respiratory infection, illness with cough, and difficulty in breathing from indoor pollution, while evidence from Khan et al. (2017) in Bangladesh revealed that indoor use of solid fuel increases the risk of acute respiratory infection, pregnancy complication, cesarean delivery, and low birth weight. Baumgartner et al. (2011) established that exposure to indoor biomass combustion is associated with an increase in blood pressure among rural Chinese women using a mixed-effects log-linear regression model. In a related study, Ofori et al. (2018) examined the link between household biomass fuel use and blood pressure among women in southern Nigeria using survey data from 389 women and established a significant link between household biomass fuel use and high blood pressure.
The work of Duflo et al. (2008) in India observed a significant association between the use of traditional fuels/stoves and respiratory illness and recommended an increase in ventilation and subsidizing cleaner fuel technologies, while Boy et al. (2002) examined the relationship between exposure to smoke during pregnancy and birth weight in Guatemala and established a positive relation. Other studies have also established specific health effects of biomass use including pneumonia in children (Bautista et al., 2009; Kurmi et al., 2010), tuberculosis (Lin et al., 2007), and age-related cataracts (Zodpey and Ughade, 1999). In gist, the literature points to the negative impact of household cooking fuel on health outcomes and by implication on household healthcare. However, very little research has been carried out on the dynamics of fuel choices and the impact on healthcare expenditure, justifying the need for this study.
3 Materials and Methods
3.1 Theoretical Framework
Following Parker and Wong (1997), we assume that households derive utility (
i = 1, 2, 3,…..,n,where
Substituting Eq. 2 into (1) gives (3) that shows household health utility function:
We assume that households face monetary constraints to produce health for consumption. Following Parker and Wong (1997), we assume that healthcare service utilization is a demand derived from the demand for health. Therefore, healthcare demand could be formulated through an aggregate utility function for all members of the household. The maximization problem for the household is therefore expressed as:
where
Eq. 5 is then augmented with a vector of household main cooking and social and demographic variables
3.2 Empirical Models and Descriptive Statistics
The Tobit model deals with censored regression, and therefore households with zero healthcare expenditure are censored and used for the analysis. The functional form for the Tobit model is given as:
where
The conditional expectation of the dependent variable given the independent variables is presented in Eq. 8:
Eq. 8 can be written in a linear form as Eq. 9:
where
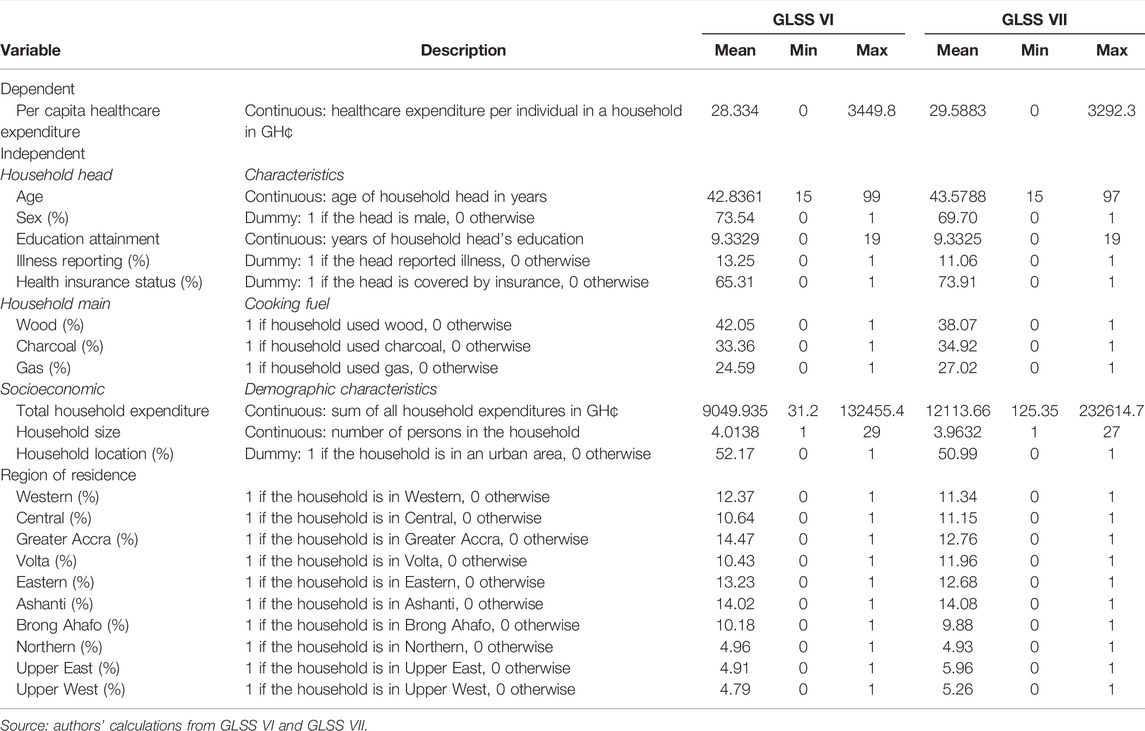
The difference between the maximum and minimum values of the variables helps to determine the spread. The bigger the gap of a variable, the larger the standard deviation of the said variable.
3.3 Data Sources
The study uses two nationwide cross-sectional survey data—the Ghana Living Standards Survey VI and VII (GLSS VI and VII) conducted by the GSS in 2012/13 and 2016/2017, respectively. Out of the 16,000 and 14,000 households surveyed in 2016/17 and 2012/13, about 10,797 and 8,769 households representing 67.5 and 64.6 percent provided information on the three main cooking fuels, respectively. The analysis is therefore made using these households. The data contain detailed information on households’ demographic and socioeconomic characteristics as well as other key variables like migration, employment, remittances, housing, fuel use, and household expenditure, among others.
3.4 Estimation Technique
Two main estimation techniques have been used to study the determinants of healthcare expenditure: Tobit estimation techniques used by Mugisha et al. (2002) and the OLS used by Molla et al. (2017) and Malik and Syed (2012). In this study, we use the Tobit regression model and the OLS model for robustness check. The reason is that the OLS is usually used for data with less zero observations (Yeboah, 2018). However, in the GLSS data, there is some zero healthcare expenditure. Ignoring such zeros biases the results and destroys the linearity assumption making the use of OLS not the best (Jelani and Tan, 2012). The Tobit regression model, however, addresses such issues and the problem of heteroscedasticity. We also employed the logarithmic transformation of the household healthcare expenditure to reduce heteroscedasticity. This generated a problem for using the log of zero observations which does not exist, as some households had zero healthcare expenditure. To address this problem, a value of one is assigned in place of zero household healthcare expenditures so that after log transformation they could remain in the dataset following You and Kobayashi (2011). For household head’s years of education, one is added to each observation so that after log transformation zero years of education observations could remain in the dataset.
Price is considered a vital variable for estimating expenditure functions. However, Deaton (1987) and Deaton et al. (1989) argue that the price variable is mostly considered unobservable in most empirical studies on expenditure functions. The available data lacked price information and quantities of health services purchased and therefore considered unobserved. Parker and Wong (1997) argue that in such a case, one can approximate the variation in prices using health insurance coverage of households and regional locations. We, therefore, include health insurance coverage and region of residence of households in our model to serve as an indicator of regional variation in prices to reflect the realities in Ghana. Sawdust, animal waste, kerosene, electricity, and other fuels were not included in the analysis because they were used by only 1.5 and 1.6% of households in 2012/13 and 2016/17 for cooking, respectively. We use the maximum likelihood estimation and STATA 15.0 econometric software for the estimations.
4 Results and Discussions
In this section, we discuss the results. We begin by investigating the correlation between the independent variables using the variance inflation factor (VIF) to test for multicollinearity. The results from the VIF test (Supplementary Appendix S1) indicate that the VIF values for all the variables are less than ten, suggesting that the model is free from multicollinearity (Islam et al., 2017). The Breusch–Pagan/Cook–Weisberg heteroskedasticity test and Ramsey Regression Equation Specification Error Test (RESET) post estimation test were undertaken for the OLS model (Supplementary Appendix S3, S4). The Ramsey RESET result indicates our model is well fitted and does not suffer from omitted variables at a 5% significant level. We also use the robust standard error approach to obtain unbiased standard errors of the coefficients. For the Tobit model, following Jelani and Tan (2012), we reduce heteroscedasticity by taking log-transformation of the dependent variable.
4.1 Household Cooking Fuel Choice on Health Expenditure
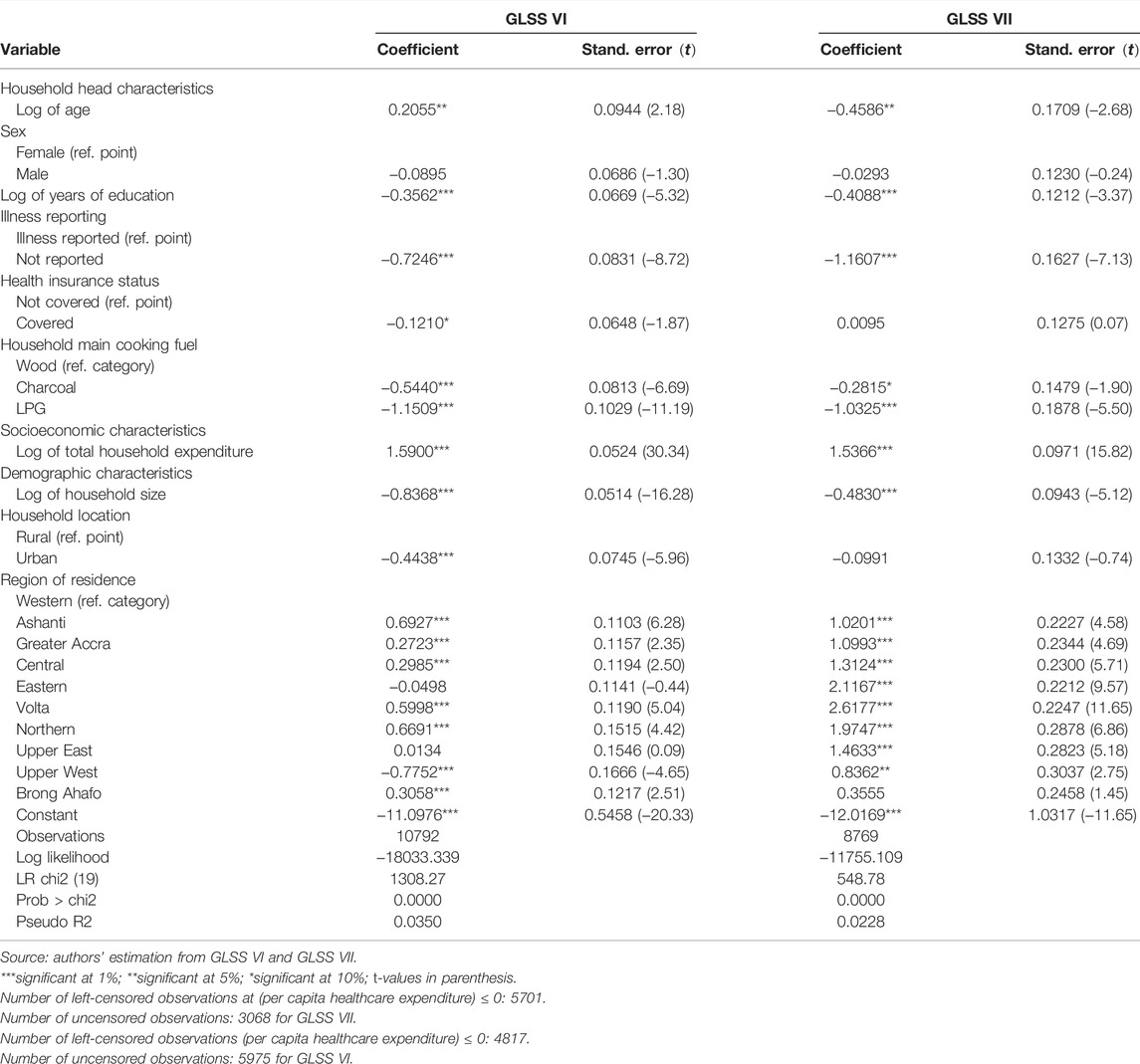
Results of the Tobit estimation are presented in Table 2. In 2012/13, relative to households using wood as cooking fuel, households using charcoal and LPG are 54.40 and 115.09 percentage points less likely to spend on healthcare services, respectively, at a 1 percent significant level. However, in 2016/17, relative to households using wood as their main cooking fuel, those using charcoal and LPG are 28.15 and 103.25 percentage points less likely to spend on healthcare services at 10 and 1 percent significant levels, respectively. The reason could be that emissions from the combustion of various cooking fuels have varying effects on the health of users (Singh et al., 2016). Whiles modern fuels like LPG generate less harmful emissions, traditional fuels such as wood and charcoal generate more harmful emissions. (Badamassi et al., 2017). Hence, households using LPG and charcoal are less exposed to harmful emissions than those using wood. In Ghana, many households depend on wood as their main cooking fuel, especially in rural areas (Mensah and Adu, 2015). However, the use of wood as cooking fuel has been found to have adverse effects on human health (WHO, 2016; Badamassi et al., 2017) and hence driving up healthcare expenditure as the results indicate.
The differences in the marginal effects of households using LPG and charcoal are 12.65 and 26.25 percentage points, respectively, less likely to spend on healthcare over the 5 years using wood as the reference point. This suggests the impact has marginally reduced over the 5 years for households using LPG and charcoal. This could be attributed to the enhanced programs on the use of cleaner fuels such as the Rural LPG Promotion Program and the Cylinder Recirculation Model and crudely suggests that these government policies are having a positive impact.
4.2 Household Head Characteristics
With regards to household head characteristics, almost all the variables were statistically significant except the sex of the household head in both 2012/13 and 2016/17. In 2012/13, a percentage increase in the age of the household head results in a 0.21 percent increase in per capita household healthcare expenditure. This is consistent with the life cycle hypothesis that older household heads can afford more healthcare than the younger ones who face financial constraints and consistent with the study of Van Minh et al. (2013) and You and Kobayashi (2011). However, in 2016/17, a percentage increase in the age of the household head reduces per capita household healthcare expenditure by 0.46 percent and supports the work of Rous and Hotchkiss (2003). An explanation for such a change in the sign of the age of household heads over the 5 years could be the increase in the National Health Insurance Scheme (NHIS) enrollment from 65.31 percent in 2012/13 to 73.60 percent in 2016/17 (Aryeetey et al., 2016) with higher enrollment for older people due to the premium exemption policy under the scheme for the aged that has significantly helped them (Duku et al., 2015).
In 2012/13 and 2016/17, a percentage increase in households’ head years of education resulted in a 0.36 and 0.41 percentage decrease in per capita household healthcare expenditure, respectively, suggesting that household heads with higher education are less likely to spend on healthcare in both years. An explanation could be that household heads with higher education are more aware of the negative effects of health which pushes them to focus on preventive than curative than those with low education. The results support the study of Rous and Hotchkiss (2003) but contradict that of Malik and Syed (2012).
In 2012/13, relative to households headed by persons with reported illness, those without reported illness are 72.46 percentage points less likely to spend on healthcare services. However, in 2016/17, those without reported illness are 116.07 percentage points less likely to spend on healthcare than those with reported illness. This is consistent with studies by Brown et al. (2014) and Molla et al. (2017). The difference in the coefficients could be associated with the success of NHIS in improving the health status of households in Ghana over the 5 years (Aryeetey et al., 2016).
Household heads covered by health insurance has a negative and significant (at 10 percent) effect on per capita household healthcare expenditure. Specifically, in 2012/13, relative to household heads not covered by health insurance, those covered by health insurance are 12.10 percentage points less likely to spend on healthcare services. This finding confirms the financial protection role of health insurance coverage and is in line with Van Minh et al. (2013) but contradicts the results by You and Kobayashi (2011). However, in 2016/17, household heads covered by health insurance had a positive influence on per capita healthcare expenditure but was not statistically significant. The reason for the variation in the results between 2012/13 and 2016/17 may be attributed to the few challenges confronting the NHIS during the period that made many households resort to the cash and carry system (Alhassan et al., 2016).
4.3 Socioeconomic and Demographic Characteristics
Expectedly, in 2012/13 and 2016/17, a percentage increase in household expenditure resulted in households being 1.59 and 1.54 percentage points, respectively, more likely to spend on healthcare suggesting that healthcare is a normal good. This result is in line with studies by Brown et al. (2014), Molla et al. (2017), Parker and Wong (1997), and You and Kobayashi (2011). The changes in the coefficients from 1.59 percent in 2012/13 to 1.54 percent in 2016/17 could be attributed to the National Health Insurance Scheme (NHIS) covering part of the health cost of households (Aryeetey et al., 2016).
In 2012/13 and 2016/1, a percentage increase in household size resulted in the household being 0.84 and 0.48 percentage points less likely to spend on healthcare services, respectively, suggesting that larger households are generally associated with poorer households that do not have enough income to afford healthcare service (Brown et al., 2014) and hence less per capita household healthcare expenditure. This result confirms the study of Brown et al. (2014) and Van Minh et al. (2013) but contradicts that of Molla et al. (2017) and Rous and Hotchkiss (2003).
With regards to location, in 2012/13, urban households were 44.38 percentage points less likely to spend on healthcare than their rural counterparts. This is in line with studies by Van Minh et al. (2013) but contradicts that of Malik and Syed (2012) and Molla et al. (2017). Urban households may use more LPG as cooking fuel than their rural counterparts who may use charcoal or wood (Mensah and Adu, 2015) and therefore get sick and spend more. However, in 2016/17, a negative influence of urban households on per capita household healthcare expenditure was observed though not statistically significant.
In 2012/13, relative to households in the Western region, households in Ashanti, Greater Accra, Central, Volta, Northern and Brong Ahafo regions are 69.27, 27.23, 29.85, 59.98, 66.91, and 30.58 percentage points, respectively, more likely to spend on healthcare services. Households in the Eastern and Upper West regions are, however, 4.89 and 77.52 percentage points less likely to spend on healthcare services than those in the Western region. More need to be carried out to explain the less likelihood of households in the Eastern region spending more on healthcare than those in the Western region. However, the Upper West region could be attributed to the low level of income as the region is one of the poorest regions in Ghana (GSS, 2019). However, in 2016/17, relative to households in the Western region, those in Ashanti, Greater Accra, Central, Eastern, Volta, Northern, and Upper East and Upper West regions are 102.01, 109.93, 131.24, 211.67, 261.77, 197.47, 146.33, and 83.62 percentage points, respectively, more likely to spend on healthcare services. The increase in the magnitude of the coefficient in 2017/18 compared to 2012/13 in many of the regions suggests that households in those regions pay more than those in the Western region over the 5-year period and could be attributed to additional payments in the form of consultation and medicines by many households over the 5-year period (Okoroh et al., 2018).
Results of the OLS estimation presented in Supplementary Appendix S2 are quite similar to those of the Tobit estimations confirming the robustness of our estimation, though the magnitudes of the effects are a little higher for the Tobit than the OLS.
5 Conclusion and Recommendations
In this study, we assess the impact of the choice of household cooking fuels on household healthcare expenditure using data from the GLSS VI and VII and the Tobit estimation technique. The results indicate that in 2012/13, relative to households using wood as cooking fuel, households using charcoal and LPG are 54.40 and 115.09 percentage points less likely to spend on healthcare services. However, the figure reduced to 28.15 and 103.25 percentage points, in 2016/17, attributable to a modest reduction in biomass energy use possibly as a result of LPG promotion activities put in place by the government which helped households’ transition to the use of improved fuels. Age, education, illness reporting of the household head, total household expenditure, household size, and region of residence were found to be the determinants of household healthcare expenditure. Policy choices should focus on the use of cleaner fuel options including strengthening the National LPG Promotion program, Rural LPG Promotion program, increase in subsidies of LPG, and extending the LPG Cylinder Recirculation Model to rural areas as well as addressing the issues on LPG supply constraints. Enhancing incomes through poverty reduction activities and increasing education will also be imperative as they impact healthcare expenditure positively. Furthermore, studies could focus on capturing information on multiple fuel use, associating diseases with specific cooking fuels, and the price of healthcare services as well as focusing on using direct health outcomes such as illness reporting.
Data Availability Statement
Publicly available datasets were analyzed in this study. These data can be found at: https://open.africa/dataset/ghana-living-standards-survey-glss-7-2017.
Ethics Statement
Ethical review and approval were not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
DT, DA, and BD contributed to the conceptualization of the study. DT developed the methodology and supervised the study. DA undertook the literature review, and BD performed the analysis. All the authors contributed to writing different sections of the manuscript, proofread the manuscript, and approved the submission of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fenvs.2022.861204/full#supplementary-material
References
Abdul-Wakeel Karakara, A., and Dasmani, I. (2019). An Econometric Analysis of Domestic Fuel Consumption in Ghana: Implications for Poverty Reduction. Cogent Soc. Sci. 5, 1697499. doi:10.1080/23311886.2019.1697499
Acharya, P., Mishra, S. R., and Berg-Beckhoff, G. (2015). Solid Fuel in Kitchen and Acute Respiratory Tract Infection Among under Five Children: Evidence from Nepal Demographic and Health Survey 2011. J. Community Health 40 (3), 515–521. doi:10.1007/s10900-014-9965-0
Ahunu, L. (2015). LPG Promotion Program. Available online: https://acep.africa/file/2019/11/THELPGPROMOTIONPROGRAMME1.pdf (accessed on February 18, 2021).
Akanda, M., Salam, A., and Minowa, M. (2011). Household Demand for Health Care and Health Care Expenditure by Controlling Endogeneity Bias in Bangladesh. Dhaka Univ. J. Sci. 59 (1), 137–146.
Alem, Y., Beyene, A. D., Köhlin, G., and Mekonnen, A. (2016). Modeling Household Cooking Fuel Choice: A Panel Multinomial Logit Approach. Energy Econ. 59, 129–137. doi:10.1016/j.eneco.2016.06.025
Alhassan, R. K., Nketiah-Amponsah, E., and Arhinful, D. K. (2016). A Review of the National Health Insurance Scheme in Ghana: what Are the Sustainability Threats and Prospects? PloS One 11 (11), e0165151. doi:10.1371/journal.pone.0165151
Aryeetey, G. C., Westeneng, J., Spaan, E., Jehu-Appiah, C., Agyepong, I. A., and Baltussen, R. (2016). Can Health Insurance Protect against Out-Of-Pocket and Catastrophic Expenditures and Also Support Poverty Reduction? Evidence from Ghana's National Health Insurance Scheme. Int. J. Equity Health 15 (1), 116. doi:10.1186/s12939-016-0401-1
Asante, K. P., Afari-Asiedu, S., Abdulai, M. A., Dalaba, M. A., Carri’on, I. A., Dickinson, K L., et al. (2018). Ghana’s Rural Liquefied Petroleum Gas Program Scale Up: A Case Study. Energy. Sustain. Dev. 46, 94–102. doi:10.1016/j.esd.2018.06.010
Badamassi, A., Xu, D., and Leyla, B. (2017). The Impact of Residential Combustion Emissions on Health Expenditures: Empirical Evidence from Sub-saharan Africa. Atmosphere 8 (9), 157. doi:10.3390/atmos8090157
Baumgartner, J., Schauer, J. J., Ezzati, M., Lu, L., Cheng, C., Patz, J. A., et al. (2011). Indoor Air Pollution and Blood Pressure in Adult Women Living in Rural China. Environ. Health Perspect. 119 (10), 1390–1395. doi:10.1289/ehp.1003371
Bautista, L. E., Correa, A., Baumgartner, J., Breysse, P., and Matanoski, G. M. (2009). Indoor Charcoal Smoke and Acute Respiratory Infections in Young Children in the Dominican Republic. Am. J. Epidemiol. 169 (5), 572–580. doi:10.1093/aje/kwn372
Boy, E., Bruce, N., and Delgado, H. (2002). Birth Weight and Exposure to Kitchen Wood Smoke during Pregnancy in Rural Guatemala. Environ. Health Perspect. 110 (1), 109–114. doi:10.1289/ehp.02110109
Brown, S., Hole, A. R., and Kilic, D. (2014). Out-of-pocket Health Care Expenditure in Turkey: Analysis of the 2003-2008 Household Budget Surveys. Econ. Model. 41, 211–218. doi:10.1016/j.econmod.2014.05.012
Capuno, J. J., Tan, C. A. R., and Javier, X. (2018). Cooking and Coughing: Estimating the Effects of Clean Fuel for Cooking on the Respiratory Health of Children in the Philippines. Glob. Public Health 13 (1), 20–34. doi:10.1080/17441692.2016.1202297
Das, I., Pedit, J., Handa, S., and Jagger, P. (2018). Household Air Pollution (HAP), Microenvironment and Child Health: Strategies for Mitigating HAP Exposure in Urban Rwanda. Environ. Res. Lett. 13 (4), 45011. doi:10.1088/1748-9326/aab047
Deaton, A. (1987). Estimation of Own-And Cross-Price Elasticities from Household Survey Data. J. Econ. 36 (1–2), 7–30. doi:10.1016/0304-4076(87)90041-8
Deaton, A. S., Ruiz-Castillo, J., and Thomas, D. (1989). The Influence of Household Composition on Household Expenditure Patterns: Theory and Spanish Evidence. J. Political Econ. 97 (1), 179–200. doi:10.1086/261597
Duflo, E., Greenstone, M., and Hanna, R. (2008). Indoor Air Pollution, Health and Economic Well-Being. Surv. Perspect. Integrating Environ. Soc. 1 (1), 1–9. doi:10.5194/sapiens-1-1-2008
Duku, S. K. O., van Dullemen, C. E., and Fenenga, C. (2015). Does Health Insurance Premium Exemption Policy for Older People Increase Access to Health Care? Evidence from Ghana. J. Aging & Soc. Policy 27 (4), 331–347. doi:10.1080/08959420.2015.1056650
GSS (2019). Ghana Living Standards Survey Round 7 (GLSS 7): Main Report. Ghana: Ghana Statistical Services Accra.
Hiemstra-Van der Horst, G., and Hovorka, A. J. (2008). Reassessing the “Energy Ladder”: Household Energy Use in Maun, Botswana. Energy Policy 36 (9), 3333–3344. doi:10.1016/j.enpol.2008.05.006
Hosier, R. H., and Dowd, J. (1987). Household Fuel Choice in Zimbabwe. Resour. Energy 9 (4), 347–361. doi:10.1016/0165-0572(87)90003-x
Inkoom, D. K. B., and Crentsil, A. O. (2015). “Estimation of Indoor Air Pollution and Health Impacts Due to Biomass Burning in Rural Northern Ghana,” in Case Studies for Developing Globally Responsible Engineers, GDEE (eds.) (Barcelona: Global Dimension in Engineering Education).
Africa Energy Outlook (2014). “A Focus on Energy Prospects in Sub-Saharan Africa,“ in World Energy Outlook Special Report (Paris: International Energy Agency (IEA)).
Islam, R., Ghani, A. B. A., Mahyudin, E., and Manickam, N. (2017). Determinants of Factors that Affecting Inflation in Malaysia. Int. J. Econ. Financial Issues 7 (2), 355–364.
Jebaraj, S., and Iniyan, S. (2006). A Review of Energy Models. Renew. Sustain. Energy Rev. 10 (4), 281–311. doi:10.1016/j.rser.2004.09.004
Jelani, J., and Tan, A. K. G. (2012). Determinants of Participation and Expenditure Patterns of Private Tuition Received by Primary School Students in Penang, Malaysia: An Exploratory Study. Asia Pac. J. Educ. 32 (1), 35–51. doi:10.1080/02188791.2012.655238
Kamila, S., Kappen, J., Rysankova, D., Hyseni, B., and Putti, R. V. (2014). Clean and Improved Cooking in Sub-saharan Africa. Washington, DC, USA: World Bank.
Karakara, A. A., Osabuohien, E. S., and Asongu, S. (2021). Domestic Energy Consumption in Ghana: Deprivation versus Likelihood of Access. Meq 32, 804–821. doi:10.1108/meq-11-2020-0247
Karakara, A. A., and Osabuohien, E. S. (2020). Clean versus Dirty Energy: Empirical Evidence from Fuel Adoption and Usage by Households in Ghana. Afr. J. Sci. Technol. Innovation Dev. 13 (7), 785–795. doi:10.1080/20421338.2020.1816266
Karimu, A. (2015). Cooking Fuel Preferences Among Ghanaian Households: an Empirical Analysis. Energy Sustain. Dev. 27, 10–17. doi:10.1016/j.esd.2015.04.003
Karimu, A., Mensah, J. T., and Adu, G. (2016). Who Adopts LPG as the Main Cooking Fuel and Why? Empirical Evidence on Ghana Based on National Survey. World Dev. 85, 43–57. doi:10.1016/j.worlddev.2016.05.004
Khan, M. N., B. Nurs, C. Z., Mofizul Islam, M., Islam, M. R., and Rahman, M. M. (2017). Household Air Pollution from Cooking and Risk of Adverse Health and Birth Outcomes in Bangladesh: a Nationwide Population-Based Study. Environ. Health 16 (1), 57. doi:10.1186/s12940-017-0272-y
Khan, M. S. B., and Lohano, H. D. (2018). Household Air Pollution from Cooking Fuel and Respiratory Health Risks for Children in Pakistan. Environ. Sci. Pollut. Res. 25 (25), 24778–24786. doi:10.1007/s11356-018-2513-1
Kurmi, O. P., Semple, S., Simkhada, P., Smith, W. C. S., and Ayres, J. G. (2010). COPD and Chronic Bronchitis Risk of Indoor Air Pollution from Solid Fuel: a Systematic Review and Meta-Analysis. Thorax 65 (3), 221–228. doi:10.1136/thx.2009.124644
Leach, G. (1992). The Energy Transition. Energy Policy 20 (2), 116–123. doi:10.1016/0301-4215(92)90105-b
Lin, H.-H., Ezzati, M., and Murray, M. (2007). Tobacco Smoke, Indoor Air Pollution and Tuberculosis: a Systematic Review and Meta-Analysis. PLoS Med. 4 (1), e20. doi:10.1371/journal.pmed.0040020
Martins, J. (2005). The Impact of the Use of Energy Sources on the Quality of Life of Poor Communities. Soc. Indic. Res. 72 (3), 373–402. doi:10.1007/s11205-004-5583-z
Mensah, J. T., and Adu, G. (2015). An Empirical Analysis of Household Energy Choice in Ghana. Renew. Sustain. Energy Rev. 51, 1402–1411. doi:10.1016/j.rser.2015.07.050
Molla, A. A., Chi, C., and Mondaca, A. L. N. (2017). Predictors of High Out-Of-Pocket Healthcare Expenditure: an Analysis Using Bangladesh Household Income and Expenditure Survey, 2010. BMC Health Serv. Res. 17 (1), 94. doi:10.1186/s12913-017-2047-0
Mugisha, F., Kouyate, B., Gbangou, A., and Sauerborn, R. (2002). Examining Out-Of-Pocket Expenditure on Health Care in Nouna, Burkina Faso: Implications for Health Policy. Trop. Med. Int. Health 7 (2), 187–196. doi:10.1046/j.1365-3156.2002.00835.x
Muhammad Malik, A., and Azam Syed, S. (2012). Socio-economic Determinants of Household Out-Of-Pocket Payments on Healthcare in Pakistan. Int. J. Equity Health 11 (1), 51. doi:10.1186/1475-9276-11-51
Muller, C., and Yan, H. (2018). Household Fuel Use in Developing Countries: Review of Theory and Evidence. Energy Econ. 70, 429–439. doi:10.1016/j.eneco.2018.01.024
Ofori, S. N., Fobil, J. N., and Odia, O. J. (2018). Household Biomass Fuel Use, Blood Pressure and Carotid Intima Media Thickness; a Cross Sectional Study of Rural Dwelling Women in Southern Nigeria. Environ. Pollut. 242, 390–397. doi:10.1016/j.envpol.2018.06.102
Okoroh, J., Essoun, S., Seddoh, A., Harris, H., Weissman, J. S., Dsane-Selby, L., et al. (2018). Evaluating the Impact of the National Health Insurance Scheme of Ghana on Out of Pocket Expenditures: a Systematic Review. BMC Health Serv. Res. 18 (1), 426. doi:10.1186/s12913-018-3249-9
Olang, T. A., Esteban, M., and Gasparatos, A. (2018). Lighting and Cooking Fuel Choices of Households in Kisumu City, Kenya: A Multidimensional Energy Poverty Perspective. Energy Sustain. Dev. 42, 1–13. doi:10.1016/j.esd.2017.09.006
Parker, S. W., and Wong, R. (1997). Household Income and Health Care Expenditures in Mexico. Health Policy 40 (3), 237–255. doi:10.1016/s0168-8510(97)00011-0
Rous, J. J., and Hotchkiss, D. R. (2003). Estimation of the Determinants of Household Health Care Expenditures in Nepal with Controls for Endogenous Illness and Provider Choice. Health Econ. 12 (6), 431–451. doi:10.1002/hec.727
Singh, A., Khan, A. H., Gupta, S., Verma, A. K., Chauhan, D. S., and Zaidi, J. (2016). Indoor Air Quality Monitoring of Biomass Fuel Vis-À-Vis Smoke Emission in Rural Poor Communities and Their Health Risks in Bundelkhand Region. Central India.
Smith, K. R., and Pillarisetti, A. (2017). Household Air Pollution from Solid Cookfuels and its Effects on Health. Inj. Prev. Environ. Health, 133–152. doi:10.1596/978-1-4648-0522-6_ch7
Treiber, M. U. (2012). Fuel and Stove Diversification in the Light of Energy Transition and Technology Adoption Theory. Ås: Norwegian University of Life Sciences.
Van Minh, H., Kim Phuong, N. T., Saksena, P., James, C. D., and Xu, K. (2013). Financial Burden of Household Out-Of Pocket Health Expenditure in Viet Nam: Findings from the National Living Standard Survey 2002-2010. Soc. Sci. Med. 96, 258–263. doi:10.1016/j.socscimed.2012.11.028
World Health Organization (2016). Burning Opportunity: Clean Household Energy for Health, Sustainable Development, and Wellbeing of Women and Children. Geneva: WHO Press.
Yeboah, P. A. (2018). Child Fostering and Education Expenditure in Ghana. Accra: University of Ghana.
You, X., and Kobayashi, Y. (2011). Determinants of Out-Of-Pocket Health Expenditure in China. Appl. Health Econ. Health Policy 9 (1), 39–49. doi:10.2165/11530730-000000000-00000
Keywords: health expenditure, cooking, fuel choice, dynamic, Ghana
Citation: Azorliade DA, Twerefou DK and Dovie DBK (2022) The Impact of Household Cooking Fuel Choice on Healthcare Expenditure in Ghana. Front. Environ. Sci. 10:861204. doi: 10.3389/fenvs.2022.861204
Received: 24 January 2022; Accepted: 22 April 2022;
Published: 27 May 2022.
Edited by:
Claude Njomgang, University of Yaoundé II, CameroonReviewed by:
Alhassan Karakara, University of Cape Coast, GhanaKeith Dana Thomsen, Lawrence Livermore National Laboratory (DOE), United States
Copyright © 2022 Azorliade, Twerefou and Dovie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Daniel Kwabena Twerefou, ZGt0d2VyZWZvdUB1Zy5lZHUuZ2g=
 Dictus Atsu Azorliade
Dictus Atsu Azorliade Daniel Kwabena Twerefou
Daniel Kwabena Twerefou Delali Benjamin K. Dovie
Delali Benjamin K. Dovie