- 1Centre for Community Medicine, All India Institute of Medical Sciences, New Delhi, India
- 2Collaborative for Air Pollution and Health Effects Research in India (CAPHER - India), New Delhi, India
- 3Centre for Dental Education and Research, All India Institute of Medical Sciences, New Delhi, India
- 4Centre for Atmospheric Sciences, Indian Institute of Technology (IIT), Delhi, India
- 5Department of Health, Policy and Management Korea University, Seoul, South Korea
- 6Department of Pulmonary Medicine and Sleep Disorders, All India Institute of Medical Sciences, New Delhi, India
Background and aim: Several air pollution mitigation initiatives have been researched worldwide to see how efficient they are at reducing air pollution and the related health benefits. The effectiveness of these interventions for improving health outcomes is key for scaling up and increasing uptake of same by policymakers and people. We aimed to synthesize scientific evidence about the effectiveness of household-level interventions on air quality and health outcomes using a systematic approach.
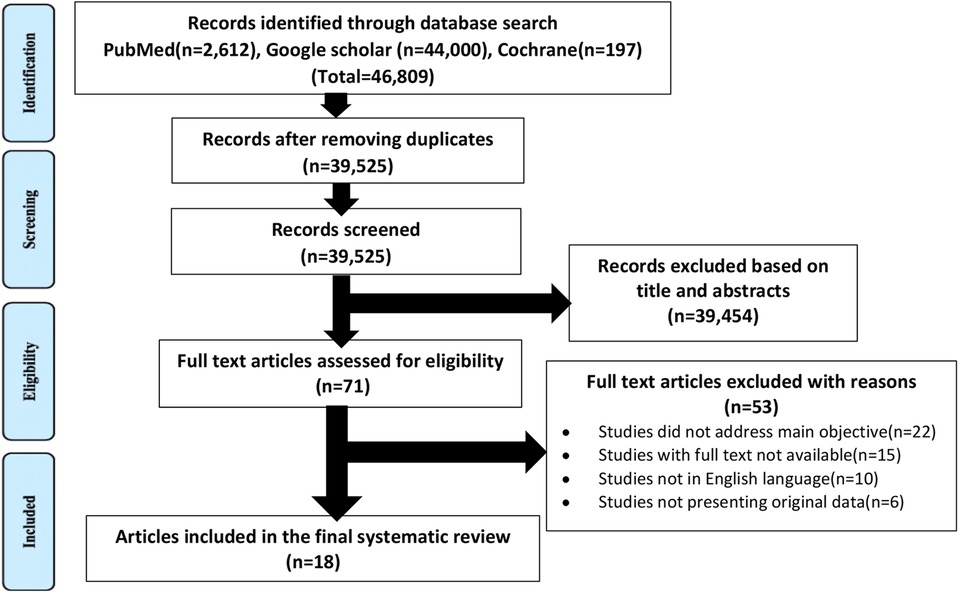
Methods: Comprehensive strategy was used to carry out a literature search in PubMed, Cochrane, and Google scholar by two independent investigators using keywords and Medical Subject Heading terms. Research articles published till the year 2021 focusing on interventions for improvement in air quality and health were selected using pre-specified eligibility criteria. All abstracts for inclusion were reviewed independently by two reviewers. In case of doubt, the articles were included for full-text review. Disagreements were resolved by discussion with the third investigator. The quality of the studies and risk of bias was assessed using the Joanna Briggs Institute critical appraisal tool and Cochrane Risk of Bias tool, version 2.0. Effect estimates were reported using odds ratio, relative risks, difference in mean, and percentage changes with 95% confidence intervals. PRISMA guidelines were used to conduct and report the systematic review. The review was registered in PROSPERO (CRD42022295393).
Results: The search resulted in the identification of 46,809 studies and 18 of them were finally included in the review using eligibility criteria. The household-level interventions were categorized mainly into air purifiers/electric heater use, cookstove use, and behavioural change interventions. These interventions resulted in a decrease in the number of daytime asthma attacks by 33%, an increase in FEV1 by 4.4%, −1.4% and 0.8% overall percent change in microvascular and lung function. PM2.5 was the most commonly reported air pollutant, its concentrations reduced in the range between 31% and 53% across the studies.
Conclusion: Our review provided consistent evidence for the effectiveness of household-level interventions thus associated with improvements in cardiovascular and respiratory symptoms.
Systematic Review Registration: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=295393, identifier, CRD42022295393
1 Introduction
Air pollution is considered a significant public health challenge globally. Air pollution is a major and growing risk factor for ill health in India, contributing significantly to the country's burden of disease (1). The United Nations Sustainable Development Goals (SDGs) target 3.9.1 focus on for reduction of the burden of deaths and illnesses from air pollution. Of the total 480·7 million DALYs in India in 2017, about 38·7 million were attributable to air pollution alone (2). A study published by the World Bank in 2016 revealed that air pollution cost India approximately 8% of its GDP or $560 billion in 2013, because of lost productivity due to premature mortality and morbidity (1). Although levels have reduced in high-income countries over the past two decades, they have risen sharply over that same period in India and other low- and middle-income countries (3). According to new estimates by WHO, about 3.2 million deaths are attributed to household air pollution exposure from using unclean fuels and technologies for cooking. Daily exposure to very high levels of household air pollution puts household members, particularly women and children, at greater risk of chronic diseases (4). To improve air quality, a broad range of interventions both at the population level and individual level have been implemented. These include national and sub-national (provincial/county/federal or state level) regulations as well as local actions and may involve either single or multiple governmental sectors (5). Research generally shows that the prolusion of multiple interventions over long periods is associated with improved air quality and health (6). However, documenting impact of each intervention with qualitative assessment of studies on air quality and health outcomes is essential for scaling up measures in public health practice. Hence, we had carried out this systematic synthesis of available evidence along with quality assessment of each study.
2 Methods
2.1 Protocol and registration
The review was conducted and reported in accordance with Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines (7). It has been registered on PROSPERO, an international prospective register of systematic reviews (ID: CRD42022295393).
2.2 Research question
Are household-level interventions effective in reducing the impact of air pollution on health outcomes?
2.3 Search strategy
A comprehensive strategy was used to carry out a literature search in Pub Med, Cochrane, and Google scholar databases. The search terms were “household interventions”, “air purifiers”, “exposure assessment”, “air pollution”, “effectiveness”, “cookstove use”, “residential interventions”, “behavioural interventions”, “impact” were combined using Boolean operators “OR” and “AND”. Two investigators (HRS, HN) independently screened the titles and abstracts of the studies to identify all potentially eligible studies. In cases of doubt, the articles were included for full-text review. Search for sources of grey literature like conference proceedings, theses and dissertations, reports, guideline and policy documents, newspaper blogs were also conducted. In addition to searching electronic databases, a hand search of the bibliographies of all relevant articles was also done. Any disagreement between the reviewers was resolved by consensus or by consultation with a third investigator (AK). Criteria used to identify eligible studies for this systematic review were –
2.3.1 Inclusion criteria
Full text published studies till March 2021 in the English language, Studies conveying information on household-level interventions to tackle air pollution, and studies assessing the impact of household-level intervention with quantitative estimations were included.
2.3.2 Exclusion criteria
Scoping reviews without quantitative data, policy reviews, case series, case reports, editorials, and letters were excluded from the review.
The PICOS approach was used for the extraction of data from the selected studies.
Participants: Eligible population can be any group of individuals exposed to an intervention of interest; Intervention: Household-level interventions, residential interventions, behavioral interventions; Controls/comparators: To provide a comprehensive review of the evidence on subject, we did not restrict interventions studies by type of comparator used; Outcome: Concentrations of PM2.5, PM10, nitrogen dioxide, carbon monoxide, sulphur dioxide, ozone, black carbon, black smoke, soot, elemental carbon, ultrafine particles, all-cause mortality, cause-specific mortality, premature mortality, respiratory effects, cardiovascular effects, neurological effects; Studies: All cross-sectional, Randomized controlled trial, quasi-experimental or non-randomized experimental studies.
In the case of each eligible study, a data extraction form in a Microsoft Excel spreadsheet was used to extract data. Extracted data included information on the study title, authors, year of publication, study location, intervention, type of intervention, exposure level assessment, source of exposure data, outcome parameters, source of health outcome, and effect estimate.
2.4 Quality and bias assessment
Quality assessment was performed independently by two investigators (HRS, HN) for each included study using the Joanna Briggs Institute (JBI) critical appraisal tool for quasi-experimental studies (8) and validated Cochrane Risk of Bias Tool, version 2.0 for randomized control trials (9). Any type of disagreement was resolved by consulting a third independent investigator (AK). With these evaluation tool, the methodological quality of the included studies was evaluated, and the extent to which a study has addressed the possibility of bias in its design, conduct and analysis was determined.
2.5 Data synthesis
A narrative synthesis was undertaken for each study. Data collected were tabulated reporting study characteristics, intervention, exposure measurements, and outcome details.
2.6 Effect estimates
Estimates of relative risks or odds ratios, and difference in mean percentage changes presented with 95% confidence intervals were extracted from papers (where available) to compare outcomes in the intervention and control groups.
3 Results
3.1 Study description
A total of 46,809 records were obtained from the databases using a search strategy. After removing duplicates and screening titles and abstracts, 71 studies remained for the full-text review. Of these, 18 studies met the eligibility criteria and were finally included in our review. The PRISMA flow diagram for the study selection process can be seen in Figure 1.
3.2 Characteristics of included studies
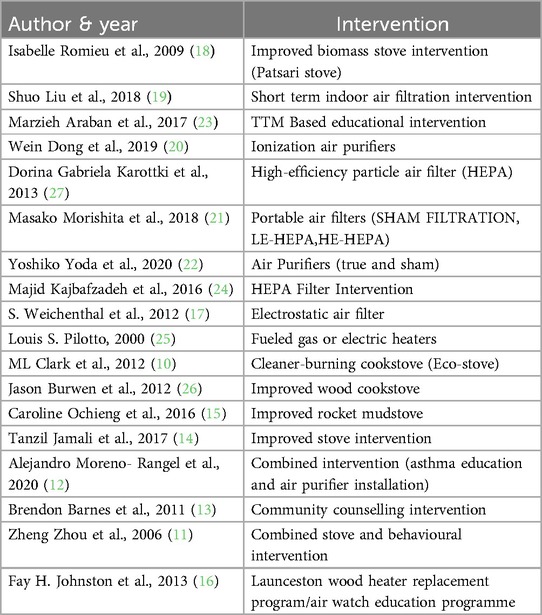
Studies included in this review were published between 2001 and 2021. Out of 18 included studies, seven studies were non-randomized experimental (10–16), and the remaining eleven studies were randomized control trials (17–27). The geographical location of the studies was diverse. Three of studies were conducted in China (11, 19, 20), two of them were conducted in United States (12, 21), Australia (16, 25) and Canada (17, 24) while rest of them were conducted in Mexico (18), Denmark (27) Iran (23), Ghana (26), Kenya (15), Nicaragua (10), Pakistan (14), Japan (22) and South Africa (13) respectively. This review comprises both studies that measure health only and studies that measure air quality, either alone or in combination with health outcomes. Exposure to air pollutants like particulate matter 2.5, particulate matter 10, ozone, black carbon, Sulphur dioxide, carbon monoxide, and respirable particles have been measured in about 16 studies. Similarly, health effects in terms of all-cause mortality, cardiovascular mortality, respiratory mortality, childhood asthma, general well-being, respiratory symptoms, non respiratory symptoms, cardiovascular and pulmonary effects, air pollution exposure behaviour have been assessed in the majority of studies.
3.3 Outcomes
Among 18 finally included studies, 13 of the studies focused on both health and air quality outcomes while three of them and two studies focused on air quality outcomes and health outcomes alone respectively.
3.3.1 Air quality outcome
Regarding the air quality outcomes of the review, the effects of 11 interventions were assessed in relation to PM2.5 (10, 12, 14, 17–22, 24, 27), four interventions in relation to PM10 (13, 16, 17, 20), six interventions in relation to carbon monoxide (10, 11, 13–15, 26), two interventions in relation to ozone (20, 22), three interventions with respect to black carbon (19, 20, 27),one intervention each in relation to nitrogen oxide (25), sulphur dioxide (11), respirable particle (11), negative air ions (20) and particle number concentrations (27) respectively.
PM2.5 was the most commonly reported air pollutant. Its concentrations significantly decreased in the range between 31% and 53% (10, 12, 17–22, 24, 27) across studies. The PM10, black carbon and carbon monoxide concentrations reduced between 28% and 85% (13, 16, 17, 20), 35.3%–50% (19, 20, 27) and 69%–72% (10, 11, 13–15, 26) respectively suggesting improvement in air quality after implementation of interventions such as air purifier installation, improved cookstove use and health education.
Source of exposure data
The source of exposure data in 11 studies were air quality monitors (10–13, 15, 17, 19–21, 25), while the remaining seven studies (14, 16, 18, 22–24, 27) has not given any clear information about it.
3.3.2 Health outcome
With regard to health outcomes of the review, the effects of two interventions were assessed relation to air pollution exposure reduction (13, 23), one intervention in relation to all cause mortality, cardiovascular and respiratory mortality (16), two interventions in relation to asthma prevalence (12, 25) and remaining were assessed in relation to respiratory effects (10, 14, 17, 18, 20, 22, 25, 27), cardiovascular effects (10, 14, 17, 19–21, 24, 27), microvascular function (24, 27), endothelial function (17, 24) and self-reported symptoms (26).
In most of the studies, household-level interventions such as the use of newer stoves and air filters contributed to a decrease in the number of daytime asthma attacks by 33% (25) and pediatric asthma related quality of life by 6.08 points (12), an increase in FEV1 by 4.4% (20), −1.4% and 0.8% overall percent change in microvascular and lung function (17, 25, 27), 14.7% decrease in FeNO (20), reduction in annual all-cause mortality by 11.4% (16), cardiovascular mortality by 17.9% (16), respiratory mortality by 22.8% (16). Only two studies observed no statistically significant effects on pulmonary function (22), microvascular and lung function, or the biomarkers of systemic inflammation (24) among study subjects.
Source of health outcome data
In this review, primary and secondary data collection procedures were implemented to gather health outcome data. In a study, by Fay H. Johnston et al., mortality data was obtained from Australian Bureau of Statistics whereas hospital admissions data for respiratory infections were provided by the Tasmania Department of Health and Human Services (16). In another study,primary data was collected using The International Union Against Tuberculosis and Lung Disease questionnaire for respiratory symptoms (14) whereas S. Weichenthal et al. used questionnaires to collect demographic information,baseline health and home characteristic data (17). In addition to this,multiple survey tools (12, 26), and telephonic interviews (23) were employed to collect the health data. For remaining studies, biochemical, pulmonary and hematological tests such as microvascular function, endothelial function, ECG monitoring,peak exploratory flow rate, FEV1,biomarker assay etc were performed using various blood pressure devices (14, 17, 19, 21) and spirometers (14, 17, 18, 22, 25, 27) either by trained investigators (20, 25) or manually (10).
3.4 Household-level interventions
18 finally included studies in the review focused on household-based interventions aimed at reducing indoor air pollution. These interventions are not a viable long-term alternative to emissions reductions. But some of them may have value—particularly in high pollution settings, for vulnerable individuals, and/or when emissions cannot be managed at the source. They have been further categorized into the following (Refer Table 1).
3.4.1 Air purifiers/electric heater use
Seven studies evaluated the impact of air purifiers or filters (portable air filters) (21) ionization air purifiers (20), HEPA filters (24, 27), true air purifiers (22), electrostatic air filters (17) and Beijing indoor air purifier (19) on various health effects. In two studies, unflued gas heaters (25) and wood heaters (16) were replaced by electric heaters.
3.4.2 Cookstove use
In about five studies effectiveness of different cookstove interventions such as improved biomass stove (18) Ecostove (10), rocket mudstove (15), improved wood cookstove (26), and improved stove (14) were studied respectively.
3.4.3 Behavioural change interventions
Remaining studies focused on behavioural interventions either alone or in combination with other intervention like Transtheoretical model based educational intervention (23), community education campaigns (13), combined stove and health education intervention (11), and combined asthma education and air purifier installation intervention (12).
3.5 Quality assessment in included studies
The JBI appraisal checklist (8) covers nine sets of criteria through which bias was assessed for quasi-experimental studies. Each item/criterion is assessed by scoring (yes = 1, no = 0 and unclear or not applicable = 0). Overall risk of bias for the included studies was then categorized into “high”, “moderate” and “low” according to the total score obtained of each (high risk of bias: 0–3, moderate risk of bias: 4–6, low risk of bias: 7–9) The risks of bias in the randomized controlled trials were assessed using the validated Cochrane RoB-2.0 tool (9). The tool includes seven domains relevant to the major sources of bias. All the studies reported a randomization process however, neither specifically reported their method of random sequence generation. Only three studies (20, 23, 24) reported allocation concealment. About seven (17, 20, 22–25, 27) studies described blinding of participants, personnel, and outcome assessors. Nine studies (17–20, 22–27) reported results on the outcomes described in their method sections; thus, the risk of selective reporting bias of outcomes appears to be low.
4 Discussion
Present review identified the available evidence regarding intervention targeted towards improving the indoor air quality on various health outcomes. Emissions, exposure rates and consequently health effects are influenced by the type of intervention. Thus, contributing to the heterogeneity between the studies. Consistent results were observed for the effect of decreased pollutant levels and the positive impact on health throughout different intervention studies. An improvement in microvascular function, lung function, brachial blood pressure, pulse wave velocity, FEV1,endothelial function and biomarkers of systemic inflammation associated with decrease in indoor air pollutants was observed in seven studies following use of high-efficiency particulate air (HEPA), ionization and electrostatic air purifiers. This supports the results of systematic reviews by Dalia Walzar et al. (28), Xi Xia et al. (29) and Ellen McDonald et al. (30) which suggests that even a small decrease in the distribution of blood pressure in a population may significantly reduce cardiovascular morbidity and mortality. Household interventional studies in low- and middle-income countries have involved “clean” cookstoves with improved combustion efficiency or ventilation and household air filters with improvement in the respiratory symptoms, and decrease in clinic visits, school absenteeism, hospitalizations, premature births, all -cause mortality, cardiovascular illness were observed. Review also reported decrease in mortality. These findings are consistent with the studies by Deborah Onakomaiya et al. (31), Megha Thakur et al. (32), Fatmi and Coggon (33), Emma Thomas et al. (34). Susann Henschel et al. (35) and Dean E. Schraufnagel et al. (36) also that source reduction strategies for improving air quality showed impact on improvement in health outcomes. Two of the studies by Brendons Barnes et al. (23) and Marzieh Araban et al. (13) provide tentative evidence that a health behaviour change intervention (focusing on health education models) has the potential to reduce indoor air pollution, especially in vulnerable groups. The review findings also suggest that current stand-alone household interventions generate little health benefits. Multi-faceted interventions could offer an opportunity to reduce exposure to household air pollution that could have a marked public health impact, especially in low and middle-income countries.
5 Strengths and limitations
To the best of our knowledge, this review is the first of its kind to assess the impact of household-level interventions on air quality and health outcomes. The strength of our study lies in its comprehensive search of multiple databases, including regional bibliographic databases, and its inclusion of multiple air pollutants and health outcomes. Three reviewers independently assessed the articles based on a priori eligibility criteria. We reported the findings according to recommendations by the Preferred reporting items for Systematic review and meta-analysis statement. The review question was clearly defined. All these aspects ensure that the results reported here are valid and relevant.
There are, however, several limitations that need to be acknowledged. Firstly only, articles published till March 2021 were included, thus most current studies are not included in this review. Secondly, there was a substantial amount of heterogeneity amongst the studies attributed to their methods, assessment techniques and variety of health outcomes. Thirdly, quality of studies reported satisfactory level. Hence, same should be considered while interpreting the results. Cost-benefit or cost-effectiveness analysis of interventions are necessary to get better understanding of effectiveness of the interventions, which was out of scope for this study. Fourth, we could not be able to employ meta-analysis approach due to high level of heterogeneity.
6 Implications for policy and research
Current review suggested that well designed and monitored interventions has impact on improving indoor air quality. Hence this review has policy and research implications in the form of sustained investment on continued household level interventions Such as provision of clean cooking fuel to the vulnerable households. Air purifiers use for improvement of air quality needs further investigation and guarded recommendations. Importance of awareness generation and behaviour change communication has been substantially highlighted further by this review. Hence, needs sustained investment at population level. However, costing studies for effectiveness of the variety of household level interventions are needed. As indoor air quality also impacts ambient air quality levels, sustain efforts for implementing interventions are needed to achieve WHO recommendation targets (37) with respect to major air pollutants (PM10, PM2.5) for respective countries.
7 Conclusion
Our review provided consistent evidence for the effectiveness of household-level interventions such as use of cook stoves, use of air filters and education driven initiatives for improving air quality and cardiovascular and respiratory health outcomes. Thus, highlighted the importance of sustained efforts in customizing and implementing these interventions at community level.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
HRS: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. HN: Data curation, Formal analysis, Writing – original draft, Writing – review & editing. SD: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AK: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. PS: Conceptualization, Investigation, Methodology, Project administration, Software, Visualization, Writing – original draft, Writing – review & editing. KM: Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. Funding for this project was provided by the Office of Principal Scientific Advisor, Government of India.
Acknowledgments
We thank all the staff who contributed their time to our research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The handling editor SC declared a past co-authorship with the author SD.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. P. H. F. of India and C. for E. Health, Air pollution and health in India: A review of the current evidence and opportunities for the future (2017). Available online at: http://archive.nyu.edu/handle/2451/42304 (accessed March 28, 2022).
2. Balakrishnan K, Dey S, Gupta T, Dhaliwal RS, Brauer M, Cohen AJ, et al. The impact of air pollution on deaths, disease burden, and life expectancy across the states of India: the global burden of disease study 2017. Lancet Planet Health. (2019) 3(1):e26–39. doi: 10.1016/S2542-5196(18)30261-4
3. Boogaard H, Walker K, Cohen AJ. Air pollution: the emergence of a major global health risk factor. Int. Health. (2019) 11(6):417–21. doi: 10.1093/inthealth/ihz078
4. Downloads | Tracking SDG 7. Available online at: https://trackingsdg7.esmap.org/downloads (accessed September 15, 2022).
5. Pandey A, Brauer M, Cropper ML, Balakrishnan K, Mathur P, Dey S, et al. Health and economic impact of air pollution in the states of India: the global burden of disease study 2019. Lancet Planet Health. (2021) 5(1):e25–38. doi: 10.1016/S2542-5196(20)30298-9
6. Burns J, Boogaard H, Polus S, Pfadenhauer LM, Rohwer AC, van Erp AM, et al. Interventions to reduce ambient air pollution and their effects on health: an abridged cochrane systematic review. Environ Int. (2020) 135:105400. doi: 10.1016/j.envint.2019.105400
7. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
8. Appendix 3.3: JBI Critical appraisal Checklist for Quasi-Experimental Studies (non-randomized experimental studies) - JBI Manual for Evidence Synthesis - JBI Global Wiki Available online at: https://jbi-global-wiki.refined.site/space/MANUAL/3290005878/Appendix+3.3%3A+JBI+Critical+appraisal+Checklist+for+Quasi-Experimental+Studies+(non-randomized+experimental+studies (accessed March 28, 2022).
9. RoB 2: A revised Cochrane risk-of-bias tool for randomized trials | Cochrane Bias. Available online at: https://methods.cochrane.org/bias/resources/rob-2-revised-cochrane-risk-bias-tool-randomized-trials (accessed March 28, 2022).
10. Clark ML, Bachand AM, Heiderscheidt JM, Yoder SA, Luna B, Volckens J, et al. Impact of a cleaner-burning cookstove intervention on blood pressure in Nicaraguan women. Indoor Air. (2013) 23(2):105–14. doi: 10.1111/ina.12003
11. Zhou Z, Jin Y, Liu F, Cheng Y, Liu J, Kang J, et al. Community effectiveness of stove and health education interventions for reducing exposure to indoor air pollution from solid fuels in four Chinese provinces. Environ Res Lett. (2006) 1(1):014010. doi: 10.1088/1748-9326/1/1/014010
12. Moreno-Rangel A, Baek J, Roh T, Xu X, Carrillo G. Assessing impact of household intervention on indoor air quality and health of children with asthma in the US-Mexico border: a pilot study. J Environ Public Health. (2020) 2020:e6042146. doi: 10.1155/2020/6042146
13. Barnes B, Mathee A, Thomas E. The impact of health behaviour change intervention on indoor air pollution indicators in the rural north west province, South Africa. J Energy South Afr. (2011) 22:35–44. doi: 10.17159/2413-3051/2011/v22i3a3220
14. Jamali T, Fatmi Z, Shahid A, Khoso A, Kadir MM, Sathiakumar N. Evaluation of short-term health effects among rural women and reduction in household air pollution due to improved cooking stoves: quasi experimental study. Air Qual Atmosphere Health. (2017) 10(7):809–19. doi: 10.1007/s11869-017-0481-0
15. Ochieng C, Vardoulakis S, Tonne C. Household air pollution following replacement of traditional open fire with an improved rocket type cookstove. Sci Total Environ. (2017) 580:440–7. doi: 10.1016/j.scitotenv.2016.10.233
16. Johnston FH, Hanigan IC, Henderson SB, Morgan GG. Evaluation of interventions to reduce air pollution from biomass smoke on mortality in Launceston, Australia: retrospective analysis of daily mortality, 1994–2007. Br Med J. (2013) 346:e8446. doi: 10.1136/bmj.e8446
17. Weichenthal S, Mallach G, Kulka R, Black A, Wheeler A, You H, et al. A randomized double-blind crossover study of indoor air filtration and acute changes in cardiorespiratory health in a First Nations community. Indoor Air. (2013) 23(3):175–84. doi: 10.1111/ina.12019
18. Romieu I, Riojas-Rodríguez H, Marrón-Mares AT, Schilmann A, Perez-Padilla R, Masera O. Improved biomass stove intervention in rural Mexico: impact on the respiratory health of women. Am J Respir Crit Care Med. (2009) 180(7):649–56. doi: 10.1164/rccm.200810-1556OC
19. Liu S, Chen J, Zhao Q, Song X, Shao D, Meliefste K, et al. Cardiovascular benefits of short-term indoor air filtration intervention in elderly living in Beijing: an extended analysis of BIAPSY study. Environ Res. (2018) 167:632–8. doi: 10.1016/j.envres.2018.08.026
20. Dong W, Liu S, Chu M, Zhao B, Yang D, Chen C, et al. Different cardiorespiratory effects of indoor air pollution intervention with ionization air purifier: findings from a randomized, double-blind crossover study among school children in Beijing. Environ Pollut. (2019) 254(Pt B):113054. doi: 10.1016/j.envpol.2019.113054
21. Morishita M, Adar SD, D'Souza J, Ziemba RA, Bard RL, Spino C, et al. Effect of portable air filtration systems on personal exposure to fine particulate matter and blood pressure among residents in a low-income senior facility: a randomized clinical trial. JAMA Intern Med. (2018) 178(10):1350–7. doi: 10.1001/jamainternmed.2018.3308
22. Yoda Y, Tamura K, Adachi S, Otani N, Nakayama SF, Shima M. Effects of the use of air purifier on indoor environment and respiratory system among healthy adults. Int J Environ Res Public Health. (2020) 17(10):3687. doi: 10.3390/ijerph17103687
23. Araban M, Tavafian SS, Zarandi SM, Hidarnia AR, Burri A, Montazeri A. A behavioral strategy to minimize air pollution exposure in pregnant women: a randomized controlled trial. Environ Health Prev Med. (2017) 22:26. doi: 10.1186/s12199-017-0633-8
24. Kajbafzadeh M, Brauer M, Karlen B, Carlsten C, van Eeden S, Allen RW. The impacts of traffic-related and woodsmoke particulate matter on measures of cardiovascular health: a HEPA filter intervention study. Occup Environ Med. (2015) 72(6):394–400. doi: 10.1136/oemed-2014-102696
25. Pilotto LS, Nitschke M, Smith BJ, Pisaniello D, Ruffin RE, McElroy HJ, et al. Randomized controlled trial of unflued gas heater replacement on respiratory health of asthmatic schoolchildren. Int J Epidemiol. (2004) 33(1):208–14. doi: 10.1093/ije/dyh018
26. A Rapid Assessment Randomized-Controlled Trial Of Improved Cookstoves In Rural Ghana, 3IE. Available online at: https://developmentevidence.3ieimpact.org/search-result-details/impact-evaluation-repository/a-rapid-assessment-randomized-controlled-trial-of-improved-cookstoves-in-rural-ghana/7004 (accessed March 28, 2022).
27. Karottki DG, Spilak M, Frederiksen M, Gunnarsen L, Brauner EV, Kolarik B, et al. An indoor air filtration study in homes of elderly: cardiovascular and respiratory effects of exposure to particulate matter. Environ Health Glob Access Sci Source. (2013) 12:116. doi: 10.1186/1476-069X-12-116
28. Walzer D, Gordon T, Thorpe L, Thurston G, Xia Y, Zhong H, et al. The effects of home particulate air filtration on blood pressure: a systematic review. Hypertens. (2020) 76(1):44–50. doi: 10.1161/HYPERTENSIONAHA.119.14456
29. Xia X, Chan KH, Lam KBH, Qiu H, Li Z, Yim SHL, et al. Effectiveness of indoor air purification intervention in improving cardiovascular health: a systematic review and meta-analysis of randomized controlled trials. Sci Total Environ. (2021) 789:147882. doi: 10.1016/j.scitotenv.2021.147882
30. McDonald E, Cook D, Newman T, Griffith L, Cox G, Guyatt G. Effect of air filtration systems on asthma: a systematic review of randomized trials. Chest. (2002) 122(5):1535–42. doi: 10.1378/chest.122.5.1535
31. Onakomaiya D, Gyamfi J, Iwelunmor J, Opeyemi J, Oluwasanmi M, Obiezu-Umeh C, et al. Implementation of clean cookstove interventions and its effects on blood pressure in low-income and middle-income countries: systematic review. BMJ Open. (2019) 9(5):e026517. doi: 10.1136/bmjopen-2018-026517
32. Thakur M, Nuyts PAW, Boudewijns EA, Flores Kim J, Faber T, Babu GR, et al. Impact of improved cookstoves on women’s and child health in low and middle income countries: a systematic review and meta-analysis. Thorax. (2018) 73(11):1026–40. doi: 10.1136/thoraxjnl-2017-210952
33. Fatmi Z, Coggon D. Coronary heart disease and household air pollution from use of solid fuel: a systematic review. Br Med Bull. (2016) 118(1):91–109. doi: 10.1093/bmb/ldw015
34. Thomas E, Wickramasinghe K, Mendis S, Roberts N, Foster C. Improved stove interventions to reduce household air pollution in low and middle income countries: a descriptive systematic review. BMC Public Health. (2015) 15(1):650. doi: 10.1186/s12889-015-2024-7
35. Henschel S, Atkinson R, Zeka A, Le Tertre A, Analitis A, Katsouyanni K, et al. Air pollution interventions and their impact on public health. Int J Public Health. (2012) 57(5):757–68. doi: 10.1007/s00038-012-0369-6
36. Schraufnagel DE, Balmes JR, Cowl CT, De Matteis S, Jung SH, Mortimer K, et al. Air pollution and noncommunicable diseases: a review by the forum of international respiratory societies’ environmental committee, part 1: the damaging effects of air pollution. Chest. (2019) 155(2):409–16. doi: 10.1016/j.chest.2018.10.042
37. Hoffmann B, Boogaard H, de Nazelle A, Andersen ZJ, Abramson M, Brauer M, et al. WHO air quality guidelines 2021–aiming for healthier air for all: a joint statement by medical, public health, scientific societies and patient representative organisations. Int J Public Health. (2021) 66:1604465. doi: 10.3389/ijph.2021.1604465
Keywords: air pollution, household, interventions, air quality, health impact
Citation: Salve HR, Nawaz H, Dey S, Krishnan A, Sharma P and Madan K (2024) Effectiveness of household-level interventions for reducing the impact of air pollution on health outcomes – a systematic review. Front. Environ. Health 3:1410966. doi: 10.3389/fenvh.2024.1410966
Received: 2 April 2024; Accepted: 9 September 2024;
Published: 25 October 2024.
Edited by:
Sourangsu Chowdhury, Centre for International Climate and Environmental Research (CICERO), NorwayReviewed by:
Tunde Ogbemi Etchie, Federal University Lokoja, NigeriaBinaya K. C., Kathmandu University, Nepal
Copyright: © 2024 Salve, Nawaz, Dey, Krishnan, Sharma and Madan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Harshal Ramesh Salve, aGFyc2hhbHNhbHZlQHltYWlsLmNvbQ==
 Harshal Ramesh Salve
Harshal Ramesh Salve Huma Nawaz3
Huma Nawaz3 Sagnik Dey
Sagnik Dey Anand Krishnan
Anand Krishnan Karan Madan
Karan Madan