- 1Department of Colorectal Surgery, The First Affiliated Hospital of Wenzhou Medical University, Wenzhou, China
- 2Department of Pulmonary and Critical Care Medicine, The First Affiliated Hospital of Wenzhou Medical University, Wenzhou, China
- 3Department of Emergency, The First Affiliated Hospital of Wenzhou Medical University, Wenzhou, China
Background: Urinary incontinence (UI) is a common and troublesome global problem. The purpose was to explore the relationship between muscle quality index (MQI) and UI.
Methods: We performed a secondary analysis of the National Health and Nutrition Examination Survey (NHANES) database (2011 to 2014). Weighted logistic regression was used to analyze the relationship between MQI and UI. Subgroup analyses were further conducted to investigate the relationship. The P for trend and P for interaction were also conducted.
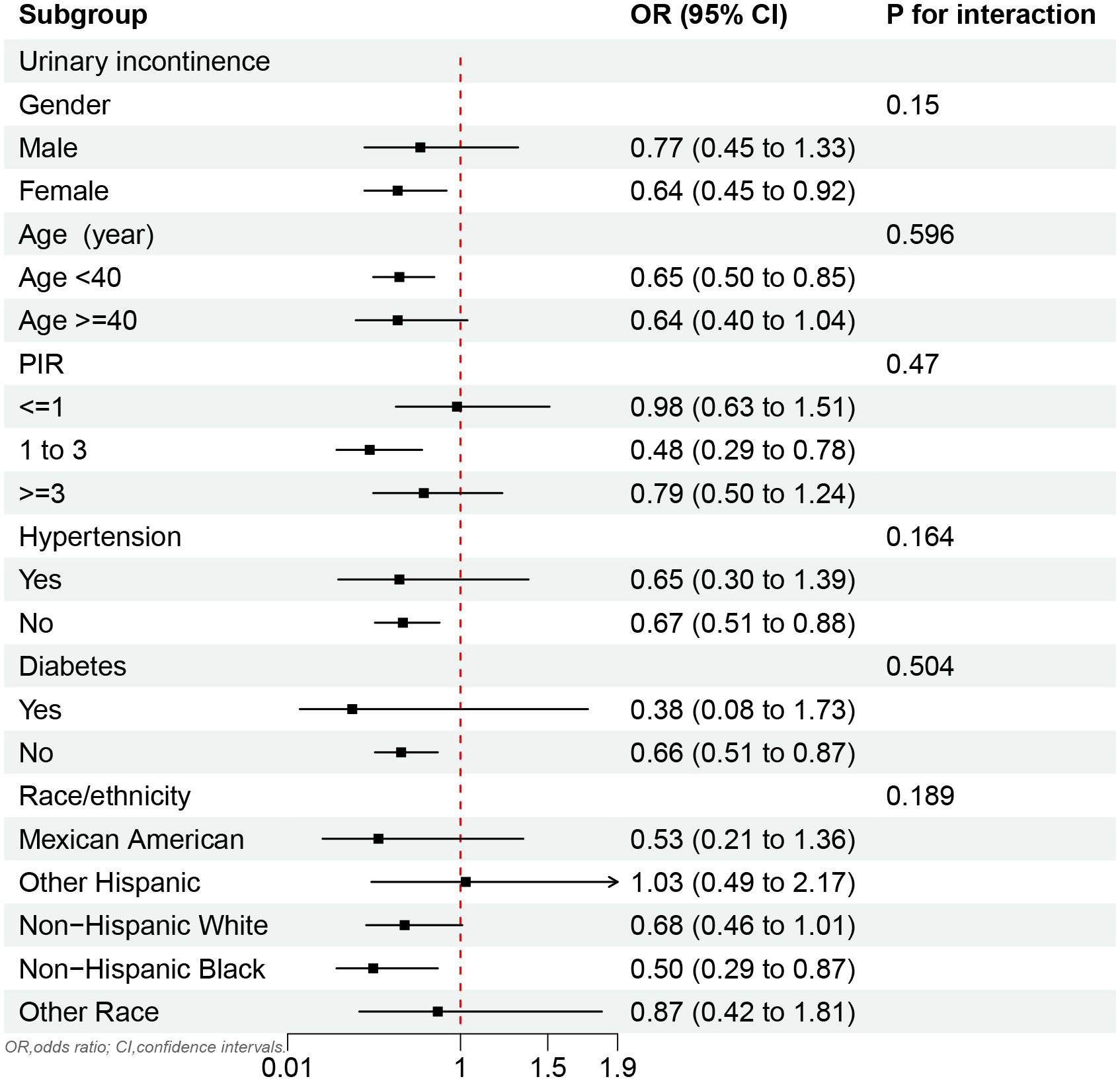
Results: A total of 2,779 participants were enrolled in the study, comprising 1,241 females and 1,538 males with a median age of 36 years. The prevalence of UI was approximately 25.45%. In adjusted model, weighted multivariate logistic regression analyses showed that MQI was significantly negatively associated with UI (OR,0.65; 95%CI,0.50 to 0.85). Furthermore, the results revealed that the highest MQI group had a 33% reduction in UI compared to the lowest MQI group and the P for trend was less than 0.05. In subgroup analysis, the MQI was negatively associated with UI in females (OR, 0.64; 95%CI, 0.45 to 0.92), under 40 years old (OR,0.65; 95%CI,0.50 to 0.85), poverty-to-income ratio of 1 to 3 (OR, 0.48; 95%CI, 0.29 to 0.78), and Non-Hispanic Black (OR, 0.50; 95%CI, 0.29 to 0.87), and in some populations without hypertension or diabetes.
Conclusion: The study revealed that a higher MQI was associated with a lower prevalence of urinary incontinence. This study provides insights into potential preventive strategies for UI.
1 Introduction
The prevalence of urinary incontinence (UI) is quite high in the U.S. population. The prevalence of UI is increasing annually in both men and women, with a particularly sharp rise observed in men as they age (1). The UI is associated with an increased risk of mortality related to cancer and cardiovascular diseases (2). In addition, UI was positively associated with depression (3). Therefore, the prevention of UI should be emphasized among the U.S. population.
Recently, many studies have focused on the relationship between muscle and handgrip strength with human disease. For example, sarcopenia was negatively correlated with the degree of recovery of voiding function during recovery from the disease (4). Low muscle mass increases the risk of death from cardiovascular disease in diabetics (5). Similarly, low handgrip strength is associated with an increased risk of cardiovascular mortality (6). Handgrip strength has been shown to have a significant correlation with urinary incontinence in the elderly (7). Pelvic floor muscle strength is positively correlated with handgrip strength and plays an important role in female UI (8). A higher percentage of muscle-to-fat ratio may provide a protective factor against female urinary incontinence (9). Therefore, assessing the association between muscle/grip strength and UI seems promising.
An indicator that combines handgrip strength (HGS) and muscle mass is called the MQI, which is defined as handgrip strength divided by the appendicular skeletal muscle mass (ASM) (10). MQI showed a negative correlation with depression, anxiety stress, and periodontal disease (11, 12). Furthermore, mental health issues have always been a significant cause of incontinence (13) and chronic illnesses also increase the prevalence of incontinence (14). Therefore, the potential relationship between MQI and UI is worth exploring in facing the enormous challenges.
The purpose of this study was to explore the relationship between MQI and UI. We hypothesized that the MQI would be negatively associated with UI in the U.S. population. By exploring this relationship, the study hopes to make a scientific contribution to UI prevention.
2 Methods
2.1 Study population information
The NHANES is a large research program evaluating the health and nutrition of the U.S. population, including both adults and children. And it has complete demographic and medical information. Secondary analysis of these data allows for the investigation of the epidemiological characteristics of diseases, which can lead to the development of appropriate health prevention policies and the strengthening of health security measures.
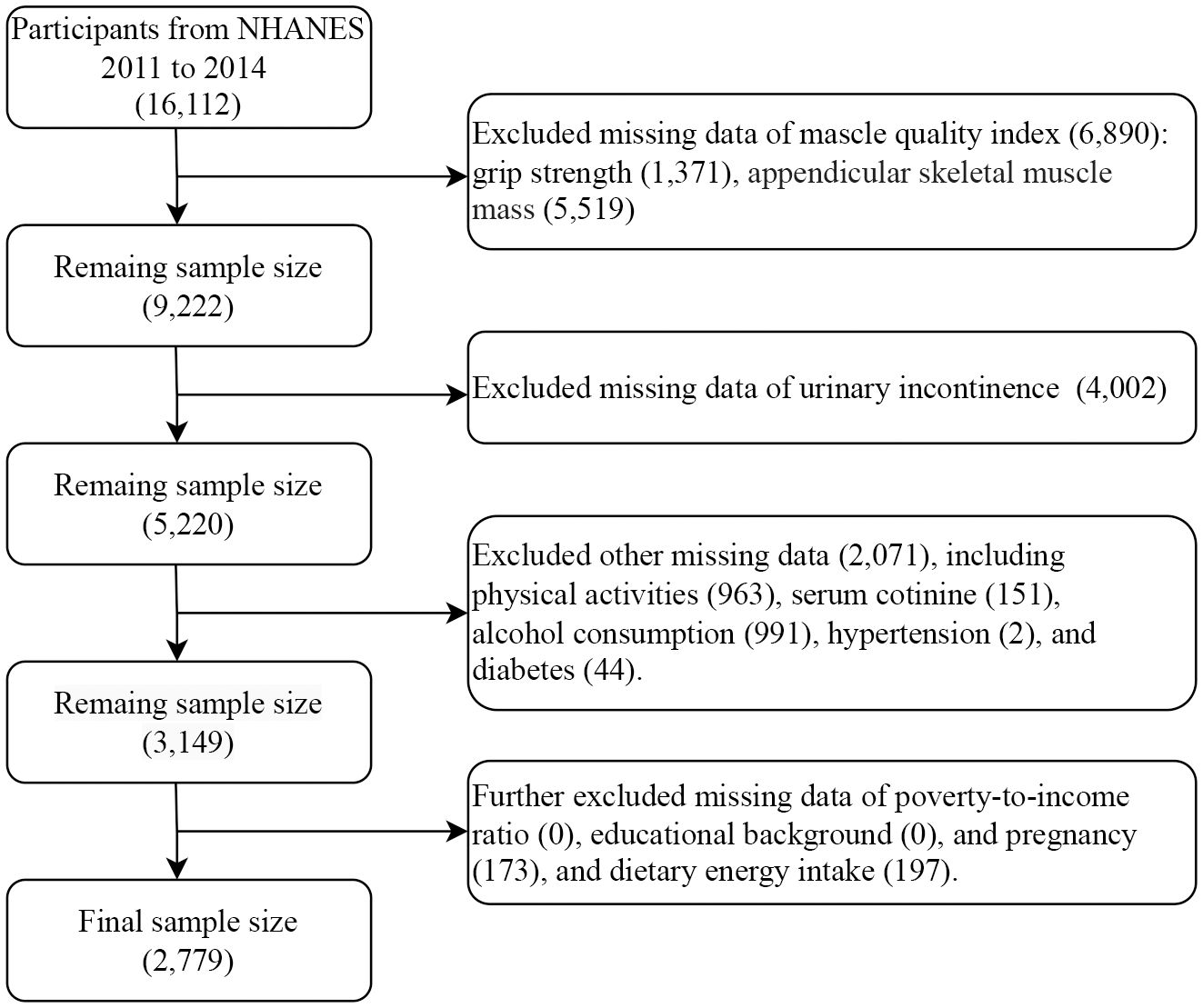
This study selected the 2011-2012 and 2013-2014 survey cycles for analysis because only these two rounds contain complete data on MQI and UI. Initially, the two survey cycles included a total of 16,112 participants. First, 6,890 participants were excluded due to missing data for calculating the MQI, including grip strength (1,371) and appendicular skeletal muscle mass (5,519). Second, participants with missing data on UI (4,002) were excluded. Subsequently, participants with missing data on other variables, including physical activity (963), serum cotinine (151), alcohol consumption (991), hypertension (2), and diabetes (44) were also excluded. Finally, participants with missing data on poverty-to-income ratio (PIR) (0), educational background (0), and pregnancy (173) or dietary energy intake data (197) were excluded from the study. Finally, the sample size analyzed by the study was 2,779 (Figure 1).
2.2 Exposure definition
MQI (Kg/Kg) was defined as an exposure factor in this study. The MQI was obtained by dividing the hand-grip strength (HGS) by appendicular skeletal muscle mass (ASM). HGS was measured by a grip strength test using a handgrip dynamometer. Participants were asked to go through the test three times with each hand. HGS was the sum of the largest reading from each hand. Muscle mass is obtained by dual-energy X-ray absorptiometry. ASM was the sum of the muscle mass of the four limbs (excluding bone mineral content).
2.3 Outcome definition
The outcome of this study was UI. According to a previous study, urinary incontinence was defined as any one of an affirmative answer to the following three questions. 1) “During the past 12 months, have you leaked or lost control of even a small amount of urine with an activity like coughing, lifting or exercise?”. 2) “During the past 12 months, have you leaked or lost control of even a small amount of urine with an urge or pressure to urinate and you couldn’t get to the toilet fast enough?”. 3) “During the past 12 months, have you leaked or lost control of even a small amount of urine without an activity like coughing, lifting, or exercise, or an urge to urinate?”.
2.4 Variable selections
This study included as many covariates as possible in interviews and physical examinations of the population that could influence the MQI and UI. First, demographic factors included gender, age, race/ethnicity, educational background, and PIR. In addition, several lifestyle factors were also included as covariates in the analysis, including smoking status (serum cotinine), alcohol consumption, and physical activity. These lifestyle factors have been demonstrated to be closely associated with urinary symptoms (15–17). Physical activity was measured as metabolic equivalent score * frequency of each body activity per week * duration of each body activity (18). Two chronic diseases (hypertension, diabetes), which were associated with UI, were also included as covariates (19, 20). Finally, given the significant role of diet in the study, total dietary energy intake was included as a covariate to account for its potential influence (21).
2.5 Statistical analysis
Categorical variables in this study are expressed as weighted percentages. Continuous variables were tested for normal distribution and all continuous variables were non-normally distributed, the results are expressed as median (IQR). We categorized the MQI into quartiles, the lowest MQI quartiles, the lower MQI quartiles, the higher MQI quartiles, and the highest MQI quartiles. The Kruskal-Wallis test was used for non-normally continuous variables while the Rao-Scott test was used for categorical variables to compare the MQI quartile. Additionally, the corresponding effect sizes were calculated. For continuous variables, Cohen’s d was calculated, and for categorical variables, Cramer’s V was computed. Weighted univariate and multivariate logistic regression models were used to investigate the potential relationship between MQI and UI. Odds ratio (OR) and 95% confidence intervals (CI) were obtained. The model 1 was a crude model with any covariates, the model 2 was adjusted for gender and age, and the model 3 was adjusted for all covariates above. Furthermore, P for rends was also estimated. In addition, subgroup analyses were also performed as well as the calculation of P for interaction. All analyses were performed in R (4.2.2) and a P value less than 0.05 was deemed statistically significant.
3 Results
3.1 Characteristics of the participants
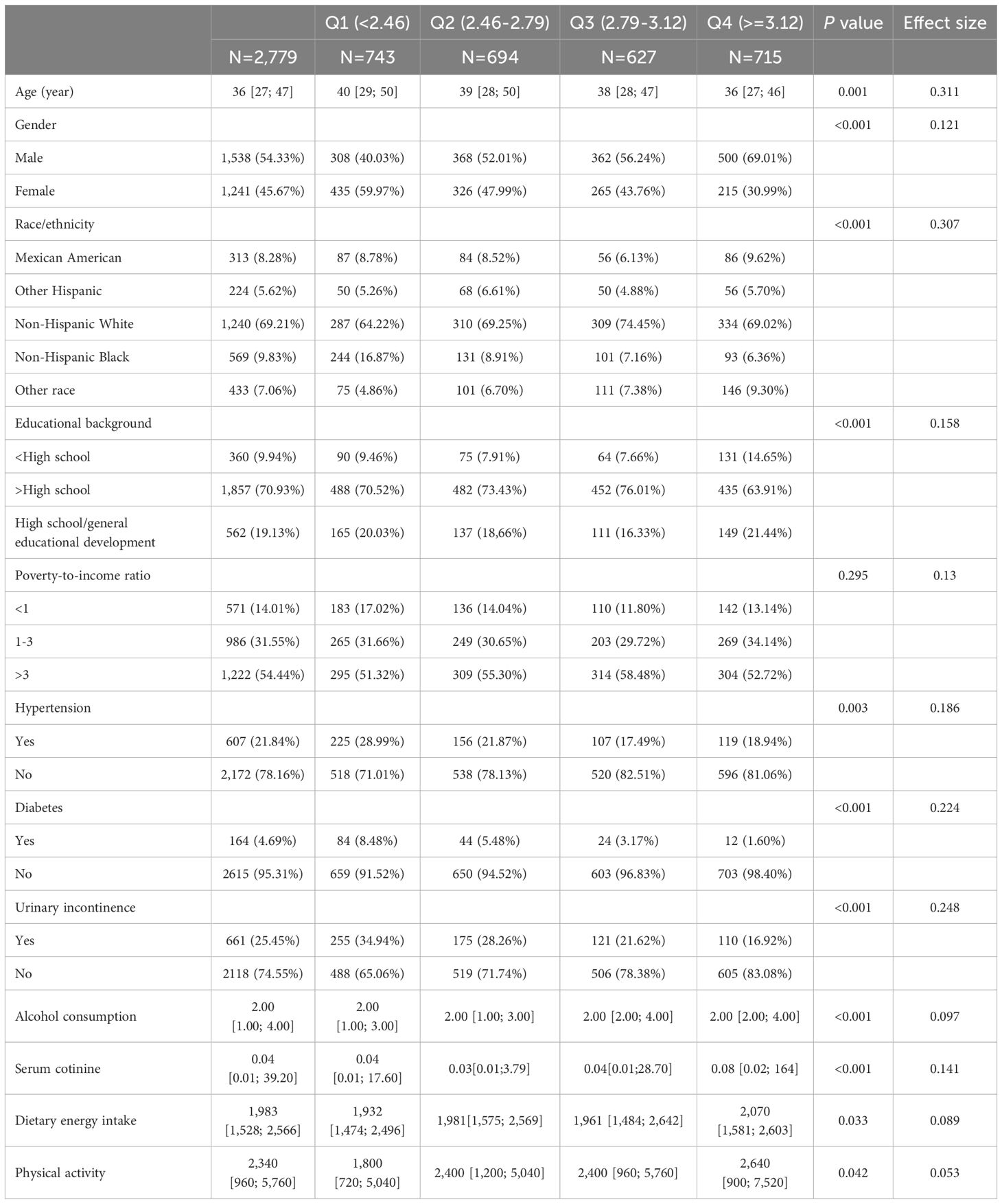
A total of 2,779 participants consisting of 1,538 males and 1,241 females were included in the final analyses (Table 1). The majority of the race/ethnicity was Non-Hispanic White and owned the educational level above high school. The prevalence of UI in the population was 25.45% and had a decreased trend from Q1 to Q4, as well as the prevalence of hypertension and diabetes (P value was less than 0.05). In addition, compared to the Q1 group, the Q4 group exhibited higher dietary energy intake, greater alcohol consumption, higher cotinine levels, and more physical activity.
3.2 Baseline characteristics of urinary incontinence
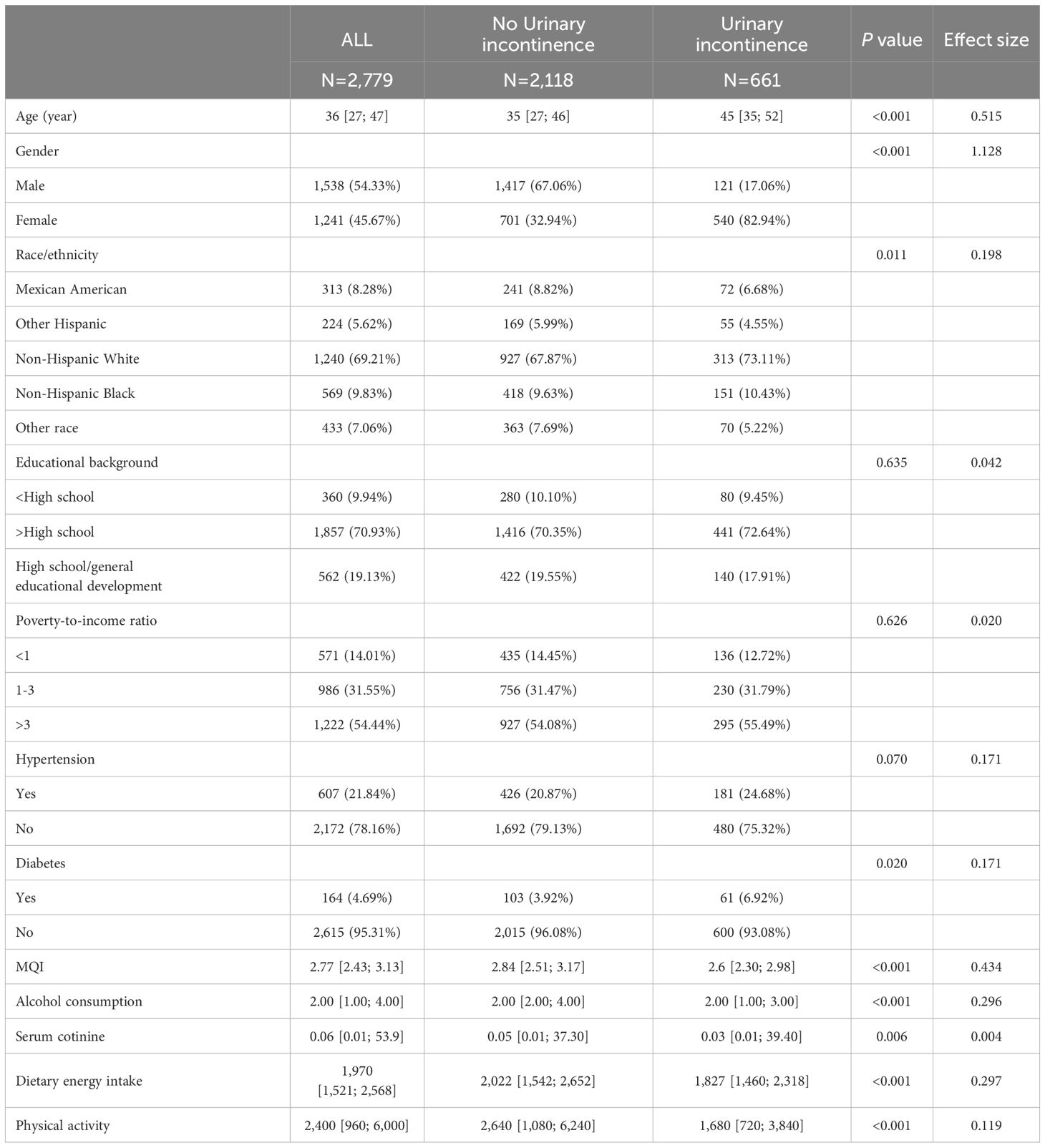
Compared to no urinary incontinence participants, the urinary incontinence population was older, had a large proportion of Non-Hispanic White females, and was more likely to have hypertension and diabetes, less physical activity and MQI levels, and low dietary energy intake (P < 0.05). There were also differences in serum cotinine level and alcohol consumption (Table 2).
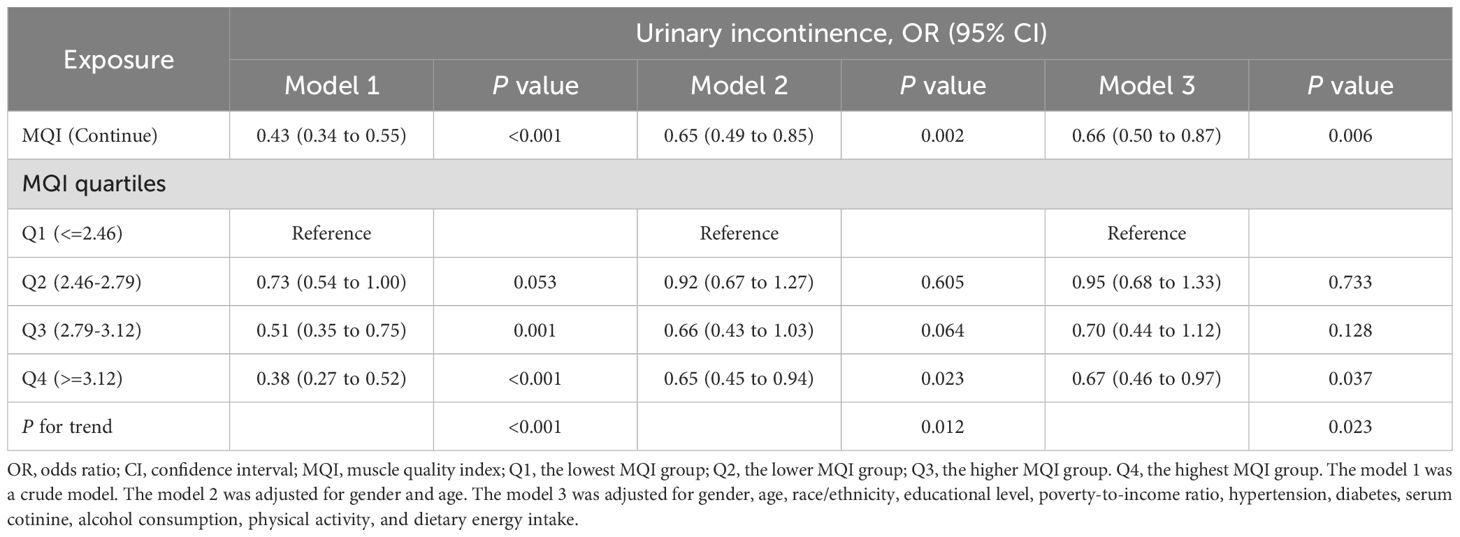
3.3 Relationship between muscle quality index and urinary incontinence
Table 3 demonstrated that MQI was significantly negatively correlated with UI. The OR (95%CI) in model 1 was 0.43 (0.34 to 0.55), in model 2 it was 0.65 (0.49 to 0.85), and in adjusted model 3 it was 0.67 (0.51 to 0.87). Furthermore, the OR (95%CI) were 0.94 (0.68 to 1.31), 0.71 (0.45 to 1.12), and 0.66 (0.46 to 0.94) from Q1 to Q4 in model 3, which revealed that the highest MQI group had a 34% reduction in UI compared to the lowest MQI group.
3.4 Subgroup analysis
In subgroup analysis, the MQI was negatively associated with UI in females (OR, 0.64; 95%CI, 0.45 to 0.92), those under 40 years old (OR, 0.65; 95%CI, 0.50 to 0.85), those with PIR of 1 to 3 (OR, 0.48; 95%CI, 0.29 to 0.78), and Non-Hispanic Black (OR, 0.50; 95%CI, 0.29 to 0.87). In addition, a negative correlation was also found in some populations without chronic diseases (hypertension and diabetes) (Figure 2).
4 Discussion
4.1 Main results
The results found that MQI showed a significant negative relationship with UI. Not only in the crude Model 1 and Model 2, but also in the fully adjusted Model 3, the negative association between MQI and UI remained consistent and robust. The UI might be decreased by 34% with each unit increased in MQI. Moreover, this negative association persisted in females, PIR (1 to 3), those aged under 40 years, those without diabetes or hypertension, and Non-Hispanic Black. Low levels of MQI might function as a risk indicator for the UI population.
4.2 Comparison and interpretations
In recent years, there has been an increased focus on the impact of muscle mass on urinary tract symptoms as well as overall health. Urethral function declines by approximately 15% per 10 years. The effects of aging on the function of the urethra are obvious (22). Most importantly, aging is accompanied by loss of muscle mass and function (23). There are differences in skeletal muscle aging between females and males, with age having a more profound effect on skeletal muscle in women (24). The UI was more common in females. The impact of changes in muscle characteristics on the body has been demonstrated in certain contexts. In older men, thigh muscle strength and urinary symptoms were negatively correlated (25). Neuroelectric stimulation affecting muscle size and strength was shown to reverse the onset of hospitalized disability (26). In the future, modulation of limb muscle size and strength to regulate MQI level appears to be a viable approach to preventing UI.
The findings also suggested that MQI shows a negative correlation with UI in non-diabetic and hypertensive patients. Diabetes is associated with accelerated skeletal muscle damage (27). An overactive bladder accompanied by sympathetic excitation is evident in hypertension patients (28). Few studies have investigated the role of MQI in diabetic and hypertension patients. People with diabetes and hypertensive tend to be concerned about other, more common complications. This would be a new direction for future research. However, muscle abnormalities may have been manifested in pre-diabetes (29). Interestingly, the relationship between MQI and UI exhibits gender differences, with this association being particularly significant in females. Anatomical and hormonal differences, as well as the impact of childbirth and menopause on pelvic floor function, contribute to the increased risk of UI in females. For example, differences in sex hormones between men and women may also contribute to this phenomenon. Low estrogen levels in females have been associated with an increased risk of UI (30). Furthermore, low testosterone levels in females are also considered a risk factor for UI (31). Additionally, postmenopausal females are more susceptible to developing UI (32). Lower-income individuals often face barriers to accessing healthcare, including limited availability of preventive services and treatments for UI. Consistent with our findings, in contexts of relatively lower economic status, food insecurity is associated with a higher prevalence of sarcopenia, which in turn increases the risk of UI (33). Furthermore, higher levels of chronic stress and occupational hazards may exacerbate the relationship between UI and MQI. Among non-Hispanic Black individuals, the proportion of shift work was higher. Shift work was positively associated with urinary incontinence in women but showed no significant association in males (34). Females under financial stress reported twice as many lower urinary tract symptoms (including UI) as women without financial stress (35). Notably, participants were more likely to discuss incontinence when severe incontinence was present. Female with diabetes, the largest group of incontinence sufferers, were also reluctant to discuss diabetes. People with diabetes tended to be concerned about other, more common complications. Those with lower household incomes were less likely to discuss incontinence with the interviewer (36). However, UI appears to be prevalent among low-income older adults in other countries (37). Therefore, although we have not reached valid conclusions in the low- and high-income groups. However, attention to them cannot be reduced.
4.3 Strengths and limitations
First, the population included in this study was a weighted, nationally representative population. Second, the sample size of this study was large enough that the results were meaningful in the population. In addition, this study included covariates that could influence exposure factors and outcomes as much as possible, making the results more reliable.
However, the limitations were also evident. First, the outcomes were based on participants’ subjective responses, which could lead to misinformation. Second, the most significant drawback was that this study was a cross-sectional study, which did not allow for the determination of causality, but only correlation analysis. While the study provided valuable insights into MQI and UI, it was cross-sectional design limits the ability to infer causality. Longitudinal studies were necessary to determine the temporal relationship between UI and MQI. Furthermore, randomized controlled trials were essential to evaluate the effectiveness of specific interventions targeting MQI. This would help infer causality between UI and MQI and provide a robust foundation for clinical decision-making. Finally, multicenter studies involving diverse populations could enhance the generalizability and stability of the findings.
It remains unknown whether systemic muscle-strengthening training can reverse existing UI, as muscle loss and UI may interact due to various factors, including aging, gender differences, and chronic diseases. Clinically, targeted interventions to prevent muscle loss may help reduce the prevalence of UI, particularly in high-risk populations. However, it is important to note that once UI and significant muscle loss have occurred, some interventions may be insufficient to alleviate UI symptoms. Additionally, the impact of early muscle-strengthening interventions on UI prevention is an essential area of investigation.
5 Conclusion
In conclusion, the negative correlation between MQI and UI in this study suggests that UI seems to be prevented by changing the level of MQI. In daily life, people at risk of UI should be more muscular strength exercise thus reducing the incidence of UI. However, more prospective studies are necessary. It also provides a new perspective for the prevention of UI worldwide. However, more effective indicators related to UI should be continuously explored. By addressing these questions, future research can provide clearer guidance on the role of muscle strengthening in both the prevention and management of UI.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by The National Centre for Health Statistics (NCHS) Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
YH: Investigation, Writing – original draft, Formal Analysis. HX: Formal Analysis, Investigation, Writing – original draft. SX: Writing – original draft. CC: Writing – original draft, Formal Analysis, Methodology, Supervision. XL: Methodology, Supervision, Writing – original draft, Writing – review and editing, Conceptualization, Investigation.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We are grateful to the staff and participants in the NHANES initiative.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Li J, Xie R, Tian H, Wang D, Mo M, Yang J, et al. Association between triglyceride glucose body mass index and urinary Incontinence: A cross-sectional study from the national health and nutrition examination survey (Nhanes) 2001 to 2018. Lipids Health Dis. (2024) 23:304. doi: 10.1186/s12944-024-02306-7
2. Kim SJ, Park SG, Pak S, Lee YG, Cho ST. Association between urgency urinary incontinence and cause-specific mortality: A population-based analysis. World J Urol. (2024) 43:22. doi: 10.1007/s00345-024-05347-w
3. Filipas DK, Labban M, Beatrici E, Stone BV, Qian ZJ, Zaplatnikova A, et al. Association of urinary incontinence and depression: findings from the national health and nutrition examination survey. Urology. (2023) 181:11–7. doi: 10.1016/j.urology.2023.08.008
4. Kido Y, Yoshimura Y, Wakabayashi H, Momosaki R, Nagano F, Bise T, et al. Sarcopenia is associated with incontinence and recovery of independence in urination and defecation in post-acute rehabilitation patients. Nutrition. (2021) 91-92:111397. doi: 10.1016/j.nut.2021.111397
5. Kim D, Lee J, Park R, Oh CM, Moon S. Association of low muscle mass and obesity with increased all-cause and cardiovascular disease mortality in us adults. J Cachexia Sarcopenia Muscle. (2024) 15:240–54. doi: 10.1002/jcsm.13397
6. Xiong L, Zeng Z, Wang S, Liao T, Wang X, Wang X, et al. The association of handgrip strength with all-cause and cardiovascular mortality: results from the national health and nutrition examination survey database prospective cohort study with propensity score matching. Front Nutr. (2023) 10:1183973. doi: 10.3389/fnut.2023.1183973
7. Corral-Pérez J, Ávila-Cabeza-de-Vaca L, Valero-Cantero I, González-Mariscal A, Ponce-González JG, Vázquez-Sánchez M, et al. Predictors of urinary and faecal incontinence in pre-frail and frail older adults: A cross-sectional study of the fragsalud project. J Gerontol A Biol Sci Med Sci. (2024) 79:glae072. doi: 10.1093/gerona/glae072
8. Bag Soytas R, Soytas M, Danacioglu YO, Citgez S, Yavuzer H, Can G, et al. Relationship between the types of urinary incontinence, handgrip strength, and pelvic floor muscle strength in adult women. Neurourol Urodyn. (2021) 40:1532–8. doi: 10.1002/nau.24699
9. Hong D, Zhang H, Yu Y, Qian H, Yu X, Xiong L. Total muscle-to-fat ratio influences urinary incontinence in United States adult women: A population-based study. Front Endocrinol (Lausanne). (2024) 15:1309082. doi: 10.3389/fendo.2024.1309082
10. Lopes LCC, Vaz-Gonçalves L, Schincaglia RM, Gonzalez MC, Prado CM, de Oliveira EP, et al. Sex and population-specific cutoff values of muscle quality index: results from nhanes 2011-2014. Clin Nutr. (2022) 41:1328–34. doi: 10.1016/j.clnu.2022.04.026
11. Barahona-Fuentes G, Huerta Ojeda ÁChecktae, Romero GL, Delgado-Floody P, Jerez-Mayorga D, Yeomans-Cabrera MM, et al. Muscle quality index is inversely associated with psychosocial variables among Chilean adolescents. BMC Public Health. (2023) 23:2104. doi: 10.1186/s12889-023-16978-w
12. Song J, Wu Y, Ma H, Zhang J. Association between muscle quality index and periodontal disease among american adults aged ≥ 30 years: A cross-sectional study and mediation analysis. BMC Oral Health. (2023) 23:918. doi: 10.1186/s12903-023-03520-y
13. Zhang X, Ma L, Li J, Zhang W, Xie Y, Wang Y. Mental health and lower urinary tract symptoms: results from the nhanes and mendelian randomization study. J Psychosom Res. (2024) 178:111599. doi: 10.1016/j.jpsychores.2024.111599
14. Valerio PM, Zordão CC, Gonçalves VE, Hasegawa MSR, Jorge CH, Moisés ECD, et al. Urinary incontinence in the third trimester of pregnancy of type 1 diabetic women. Reprod Sci. (2024) 31:1558–64. doi: 10.1007/s43032-024-01488-w
15. Michel KF, Rangnekar AN, Slinger M, Gan ZS, Smith AL. Association of smoking status and pack year history with urinary urgency symptoms. Neurourol Urodyn. (2024) 43:1842–9. doi: 10.1002/nau.25587
16. Zhang D, Sánchez-Polán M, Silva-Jose C, Díaz-Blanco Á, Brik M, Arias AM, et al. Prenatal exercise decreases urinary incontinence in late pregnancy and 3 months postpartum: A randomized controlled trial. Med Sci Sports Exerc. (2025) 57:555–62. doi: 10.1249/mss.0000000000003597
17. Zhang Y, Qin W. Relationship between alcohol use and overactive bladder disease: A cross-sectional study of the nhanes 2005-2016. Front Public Health. (2024) 12:1418117. doi: 10.3389/fpubh.2024.1418117
18. Tian X, Xue B, Wang B, Lei R, Shan X, Niu J, et al. Physical activity reduces the role of blood cadmium on depression: A cross-sectional analysis with nhanes data. Environ pollut. (2022) 304:119211. doi: 10.1016/j.envpol.2022.119211
19. Hamshari S, Sholi S, Jamous MA, Taha A, Aghbar A, Alwafa RA, et al. An evaluation of lower urinary tract symptoms among patients with hypertension: A cross-sectional study. J Family Med Prim Care. (2024) 13:3195–202. doi: 10.4103/jfmpc.jfmpc_231_24
20. Silveira THR, Silva FH, Hill WG, Antunes E, de Oliveira MG. Targeting nadph oxidase as an approach for diabetic bladder dysfunction. Antioxidants (Basel). (2024) 13:1155. doi: 10.3390/antiox13101155
21. Maserejian NN, Giovannucci EL, McVary KT, McGrother C, McKinlay JB. Dietary macronutrient and energy intake and urinary incontinence in women. Am J Epidemiol. (2010) 171:1116–25. doi: 10.1093/aje/kwq065
22. Afyouni AS, Wu YX, Balis UGJ, DeLancey J, Sadeghi Z. An overview of the effect of aging on the female urethra. Urol Clin North Am. (2024) 51:239–51. doi: 10.1016/j.ucl.2024.02.001
23. Wang M, Wu X, Jiao Y, Yin W, Zhang L. Life-long aerobic exercise is a nonpharmacological approach for inducing autophagy and delaying muscle atrophy in the aging population. Aging Dis. (2024) 0318. doi: 10.14336/ad.2024.0318
24. Moreira-Pais A, Vitorino R, Sousa-Mendes C, Neuparth MJ, Nuccio A, Luparello C, et al. Mitochondrial remodeling underlying age-induced skeletal muscle wasting: let’s talk about sex. Free Radic Biol Med. (2024) 218:68–81. doi: 10.1016/j.freeradbiomed.2024.04.005
25. Langston ME, Cawthon PM, Lu K, Scherzer R, Newman JC, Covinsky K, et al. Associations of lower extremity muscle strength, area, and specific force with lower urinary tract symptoms in older men: the baltimore longitudinal study of aging. J Gerontol A Biol Sci Med Sci. (2024) 79:glae008. doi: 10.1093/gerona/glae008
26. Alqurashi HB, Robinson K, O’Connor D, Piasecki M, Gordon AL, Masud T, et al. The effects of neuromuscular electrical stimulation on hospitalised adults: systematic review and meta-analysis of randomised controlled trials. Age Ageing. (2023) 52:afad236. doi: 10.1093/ageing/afad236
27. Lisco G, Disoteo OE, De Tullio A, De Geronimo V, Giagulli VA, Monzani F, et al. Sarcopenia and diabetes: A detrimental liaison of advancing age. Nutrients. (2023) 16:63. doi: 10.3390/nu16010063
28. Akbar A, Liu K, Michos ED, Bancks MP, Brubaker L, Markossian T, et al. Association of overactive bladder with hypertension and blood pressure control: the multi-ethnic study of atherosclerosis (Mesa). Am J Hypertens. (2022) 35:22–30. doi: 10.1093/ajh/hpaa186
29. Karlsson J, Rønneberg R. Muscle metabolism and quality (Mqi) in prediabetic sedentary man. Mol Cell Biochem. (1998) 178:69–75. doi: 10.1023/a:1006815406524
30. Li W, Wang Z, Li X, Luo R, Huang J, Liu B, et al. Associations between serum estrogen levels and urinary incontinence in women: A cross-sectional analysis of nhanes 2013 to 2016. Urology. (2024) 188:63–9. doi: 10.1016/j.urology.2024.04.029
31. Li W, Huang J, Chen J, Zhang C, Luo R, Liu B, et al. Associations between serum testosterone levels and overactive bladder in women: A cross-sectional research of nhanes 2011 to 2016. Int Urol Nephrol. (2024) 56:2521–9. doi: 10.1007/s11255-024-03996-9
32. Huang X, Hu W, Li L. Association between triglyceride-glucose index and its correlation indexes and stress urinary incontinence in postmenopausal women: evidence from nhanes 2005-2018. Lipids Health Dis. (2024) 23:419. doi: 10.1186/s12944-024-02414-4
33. Xiao Y, Yin S, Bai Y, Wang J, Cui J, Yang Y, et al. A positive association between food insecurity and the prevalence of overactive bladder in U.S. Adults. Front Nutr. (2023) 10:1329687. doi: 10.3389/fnut.2023.1329687
34. Diao J, Xie L, Wu B, Chen L, Jing H. Bladder health in U.S. Shift workers: A cross-sectional study (Nhanes). Urol J. (2024). doi: 10.22037/uj.v21i.8265
35. Brady SS, Arguedas A, Huling JD, Hellemann G, Lewis CE, Fok CS, et al. Financial strain across 25 years and women’s bladder health: A life course perspective. Am J Obstet Gynecol. (2024) 230:77.e1–.e12. doi: 10.1016/j.ajog.2023.09.096
36. Duralde ER, Walter LC, Van Den Eeden SK, Nakagawa S, Subak LL, Brown JS, et al. Bridging the gap: determinants of undiagnosed or untreated urinary incontinence in women. Am J Obstet Gynecol. (2016) 214:266.e1–.e9. doi: 10.1016/j.ajog.2015.08.072
Keywords: muscle quality index, urinary incontinence, NHANES, cohort study, epidemiology
Citation: Hu Y, Xu H, Xie S, Chen C and Lei X (2025) Relationship between muscle quality index and urinary incontinence among U.S. population: evidence from NHANES 2011 to 2014. Front. Endocrinol. 16:1533617. doi: 10.3389/fendo.2025.1533617
Received: 24 November 2024; Accepted: 13 March 2025;
Published: 08 April 2025.
Edited by:
Dustin J Oranchuk, University of Colorado, United StatesReviewed by:
Mark Manago, University of Colorado, United StatesHüsniye Dinç Kaya, Istanbul University-Cerrahpasa, Türkiye
Copyright © 2025 Hu, Xu, Xie, Chen and Lei. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chengshui Chen, Y2hlbmNoZW5nc2h1aUB3bXUuZWR1LmNu; Xiong Lei, bGVpeGlvbmdAd211LmVkdS5jbg==
†These authors have contributed equally to this work
 Yiwang Hu1†
Yiwang Hu1† Hanyan Xu
Hanyan Xu Shuying Xie
Shuying Xie Chengshui Chen
Chengshui Chen Xiong Lei
Xiong Lei