
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Endocrinol., 26 March 2025
Sec. Reproduction
Volume 16 - 2025 | https://doi.org/10.3389/fendo.2025.1495470
This article is part of the Research TopicLifestyle and Environmental Factors and Human FertilityView all 16 articles
Objective: To determine the relationship between physical activity (PA) patterns and infertility among women in the United States and to ascertain whether glycated hemoglobin (HbA1c) influences this association.
Design: A cross-sectional study of PA patterns and infertility was conducted. The PA classification was based on two categories: recreational PA and work-related PA. The subgroups were classified as inactive, less active, or active. We conducted data analysis via both multiple logistic regression analysis and mediation analysis.
Setting: National Health and Nutrition Examination Survey (NHANES, 2013–2018).
Participants: Women aged 18–49 years (n, 3,948).
Results: There was no statistically significant link demonstrated between infertility and work-related PA patterns. The recreational PA group may decrease the prevalence of infertility, with its occurrence being merely 0.79 times that of inactive group. (95% CI: 0.62, 1.0; p = 0.045). The consistency of this discrepancy was not preserved in Model III after the mixed effect was incorporated into the recreational PA group. The stratified research findings revealed that the association between recreational PA patterns and infertility was influenced by variables such as age, BMI, and history of diabetes. Furthermore, the mediation analysis revealed that recreational PA did not have a statistically significant direct effect on infertility (p = 0.098). HbA1c serves as a mediator in this interaction (95% CI: -0.06, -0.02).
Conclusion: Recreational PA patterns were associated with infertility among women aged 18–49 years in the United States, which was likely due to the effects of HbA1c.
Infertility is characterized as the inability to conceive following 12 months of consistent, unprotected sexual intercourse (1). This condition is a major worldwide health concern that adversely affects individual well-being and human rights. The most recent guidelines from the World Health Organization (WHO) indicate that approximately 10–15% of couples in the United States experience infertility, with the frequency of infertility increasing with age (2). Infertility is influenced by a variety of complex circumstances involving both male and female contributions. WHO guidelines identify the primary contributors to female infertility as ovulatory disorders, pelvic factors, infectious factors, immunological factors, and unexplained causes. In females, age is a paramount factor influencing fertility, as the ovarian reserve decreases with advancing age, thus resulting in a reduction in both egg quality and quantity (3). Moreover, the incidence of aneuploidy (which stems from chromosomal irregularities) is more prevalent in older women, thus increasing the likelihood of miscarriage and contributing to infertility (4). This underscores the necessity for an extensive understanding of female reproductive health, especially regarding the impact of various lifestyle factors on fertility.
PA is essential for sustaining overall health. The WHO defines PA as any bodily action that expends energy through the skeletal muscular system. Regular PA has numerous advantages, such as improved cardiovascular function, effective weight management, enhanced metabolic health, and increased mental well-being (5). These factors may indirectly affect fertility by regulating hormone balance and enhancing reproductive outcomes (6, 7).
HbA1c is an essential biomarker for evaluating long-term glucose regulation, especially in individuals with associations with diabetes. Recent studies have indicated that HbA1c may also represent overall metabolic health and can act as a marker for reproductive health (8, 9). Recent studies have also shown that an increase in HbA1c levels is significantly associated with the risk of ovarian dysfunction, which may affect ovarian health by influencing insulin resistance and the inflammatory response (10). Regular PA has been shown to lower HbA1c levels, thereby improving metabolic health and improving ovarian function (11). This effect is particularly pertinent for women, due to the fact that increased HbA1c levels have been linked to unfavorable reproductive outcomes, including heightened risks of conception challenges and hazardous pregnancy problems such as gestational diabetes mellitus, early pregnancy abortion, fetal dysplasia, etc (12). Additional data have indicated correlations among metabolic health, physical fitness, and reproductive health (13). Nevertheless, there are limited findings regarding the mediation function of HbA1c in the relationship between PA and infertility. Therefore, an understanding of the relationships among PA, HbA1c levels, and infertility may yield significant insights into prospective therapeutic options for enhancing reproductive health in aging women. This article categorized PA levels into three groups, including active, less active, and inactive groups, according to PA guidelines (14–16). A stratified study was performed to examine the associations between infertility and PA levels, as well as explore the mediating role of HbA1c in the relationship between PA and infertility, with a particular focus on female reproductive health. This analysis aims to understand how lifestyle modifications can enhance fertility outcomes and inform clinical practices for those individuals who experience infertility.
This study utilized cross-sectional survey data from the NHANES (https://wwwn.cdc.gov/nchs/nhanes/). A total of 14,948 women were included from 3 cycles of the NHANES, and 5,431 of them responded to the question on infertility. After excluding individuals aged 50 years or older who did not have exercise patterns or HbA1c indicators, the study included a total of 3,948 participants, as visually demonstrated in Figure 1. The NHANES protocols were approved by the NCHS Research Ethics Review Board, and written informed consent forms were provided by all of the participants.
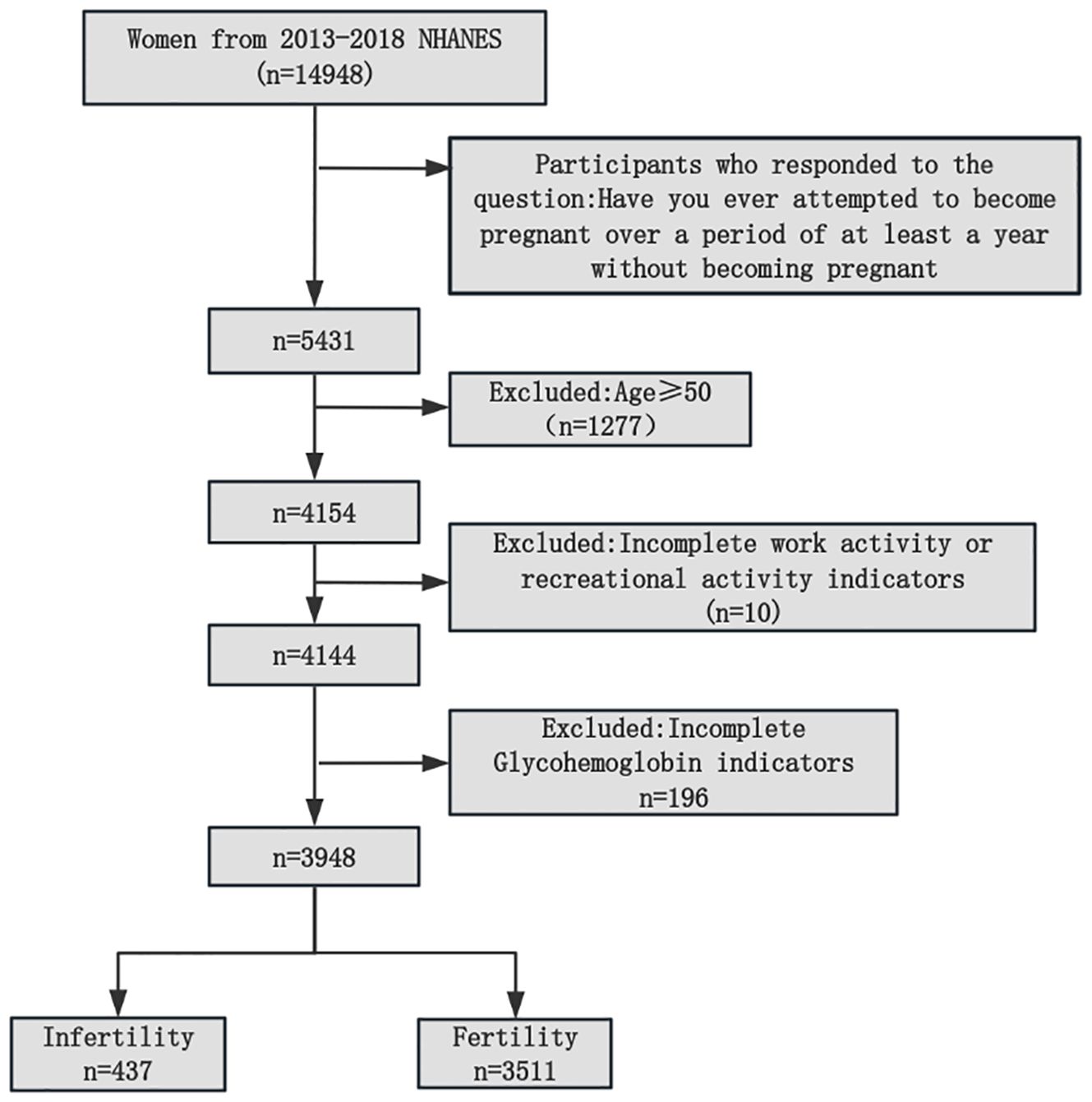
Figure 1. Flowchart of participants selection from the NHANES 2013–2018. NHANES, National Health and Nutrition Examination Survey.
The NHANES study collected data on PA via a questionnaire, in which individuals reported their own PA levels. The questions regarding PA were as follows: “Do you participate in any vigorous exercise or fitness activity on a regular basis that leads to a significant increase in your breathing or heart rate, such as running or playing basketball for at least 10 minutes?”; and “Do you often participate in any type of moderate-intensity PA, such as brisk walking, cycling, swimming, or playing volleyball, for at least 10 minutes, which causes a slight increase in your breathing and heart rate?”. This study included both work and recreational activities. According to the recommendations of WHO and national health institutions, adults aged 18–64 years need to engage in at least 150 minutes of moderate-intensity aerobic exercise (such as brisk walking or cycling) or 75 minutes of high-intensity aerobic exercise (such as running or swimming) per week to promote their health. We separately calculated the durations of both moderate- and high-intensity PA and classified PA into three categories: inactive, less active (≤ recommended amount of activity), and active (≥ recommended amount of activity) (Table 1). We reported infertility via the following question: “Have you made any attempts to conceive for a duration of at least one year without achieving pregnancy?”. We classified those individuals who responded affirmatively as infertile and those who responded negatively as fertile. We classified unanswered or refused responses as missing values. At Columbia University, Missouri, HbA1c tests were conducted. The A1c G7 HPLC Glycohemoglobin Analyzer (produced by Tosoh Medicine, Inc., 347 Oyster Pt. Blvd., Suite 201, So. San Francisco, CA 94080) was used to measure HbA1c levels.
We conducted a thorough examination of 10 potential variables that could influence the relationship between physical activity PA and infertility. These variables included age (18–49 years), race, sex, BMI, smoking status, education, sleep, history of diabetes, poverty-to-income ratio (PIR), menstrual cycle, current pregnancy, and HbA1c. To facilitate comparative analysis, we converted continuous variables into categorical variables and divided each covariate into a reference group and additional groups for comparison. Furthermore, we designated “unknown, rejected, or undetectable” values as values that were not present or could not be determined.
The chi-square test was used to assess the statistical disparities in confounding factors between the two groups, including fertility and infertility. A logistic regression model was used to investigate the correlation between infertility and PA. The model calculated the odds ratio (OR) between infertility and various categories of work and recreational PA, and it compared the 95% confidence interval (CI) with that of women who were inactive (the reference group). The regression model was adjusted for age, race, BMI, smoking status, education, sleep, history of diabetes, poverty-to-income ratio (PIR), menstrual cycle and current pregnancy or nonpregnancy status. In Model 1, no variables were adjusted; in Model 2, racial and educational adjustments were made; and in Model III, we accounted for all of the covariates and subsequently examined them as subgroup variables in a stratified analysis. To assess the extent to which HbA1c mediates the association between PA patterns and infertility, we performed a causal mediation analysis. Initially, we employed the causal stepwise regression test to conduct linear regression and logistic regression on the dependent variable with respect to the independent variable (17). We subsequently determined the regression coefficients a, b, c, and c′ in the mediation model. The RMediation package in R software was used to calculate the 95% confidence interval of Za * Zb via the cumulative distribution approach (18). The PA pattern, infertility status, and HbA1c level were used to represent the independent variables, outcome variables, and mediating variables, respectively, in our survey. A significance threshold of P<0.05 and a Za * Zb 95% CI excluding 0 guided the determination of statistical significance.
This study included 3,948 female participants, with an average age of 33.24 ± 9.47 years; additionally, 11.07% had previously experienced infertility. Table 2 presents a thorough summary of the fundamental characteristics of the participants. Women who were over the age of 35 years, of non-Hispanic white ethnicity, and obese, in addition to having a high poverty-to-income ratio (PIR) and a history of diabetes, were more likely to experience infertility. There was no statistically significant disparity between the two groups in terms of education level, smoking status, sleep duration, or regularity of the menstrual cycle. Furthermore, individuals with infertility exhibited a notable increase in HbA1c levels compared to patients who did not have a history of infertility (2.47 ± 0.17 vs. 2.43 ± 0.2).
These findings indicated that there is no substantial association between work-related PA and infertility. However, in recreational PA, there is no substantial correlation between less active PA and infertility, whereas there is a strong association between active PA and infertility. During active PA, the likelihood of infertility is 0.79 times that during inactive PA. In Model II, after accounting for the confounding factors of race and education, the correlation remained significant (OR=0.75, 95% CI: 0.59, 0.96; p=0.02). However, in Model III, after adjusting for confounding factors in all of the covariates, the strength of this correlation was no longer statistically significant (OR = 0.82, 95% CI: 0.38, 1.78; p = 0.62), as indicated in Table 3.
A stratified analysis of the correlation between all of the covariates and infertility in three different modes of recreation-related phsical activity (PA) revealed that among women who engaged in active and less active PA, obese women (BMI ≥ 30) had a greater probability of infertility than women of normal weight; however, this difference was not observed in women without exercise. In addition, there was no statistically significant difference in the incidence of infertility between overweight women (BMI = 25–29.9) and normal-weight women among the three PA modes. More significantly, there was a significant correlation between a history of diabetes and infertility in women without exercise and in women with active PA; however, this correlation was not significant in women with less active PA, as indicated in Table 4.
Mediation analysis sought to measure the extent to which HbA1c acts as a mediator in the relationship between recreational physical PA patterns and infertility. In contrast to conventional mediation research, our study specifically examined categorical variables as both independent and dependent factors. Thus, we calculated the relative mediation effects, relative direct effects, and relative total effects and computed the mediating effect value by multiplying Za and Zb, after which we assessed the 95% confidence interval of Za * Zb via the product distribution method. The results of our study indicated that engaging in recreational active PA does not have a statistically significant direct effect on infertility (p=0.098). However, we found that HbA1c plays a mediating role in the relationship between recreational active PA and infertility, with a mediating effect of -24.9 (95% CI: -0.06, -0.02), as shown in Figure 2.
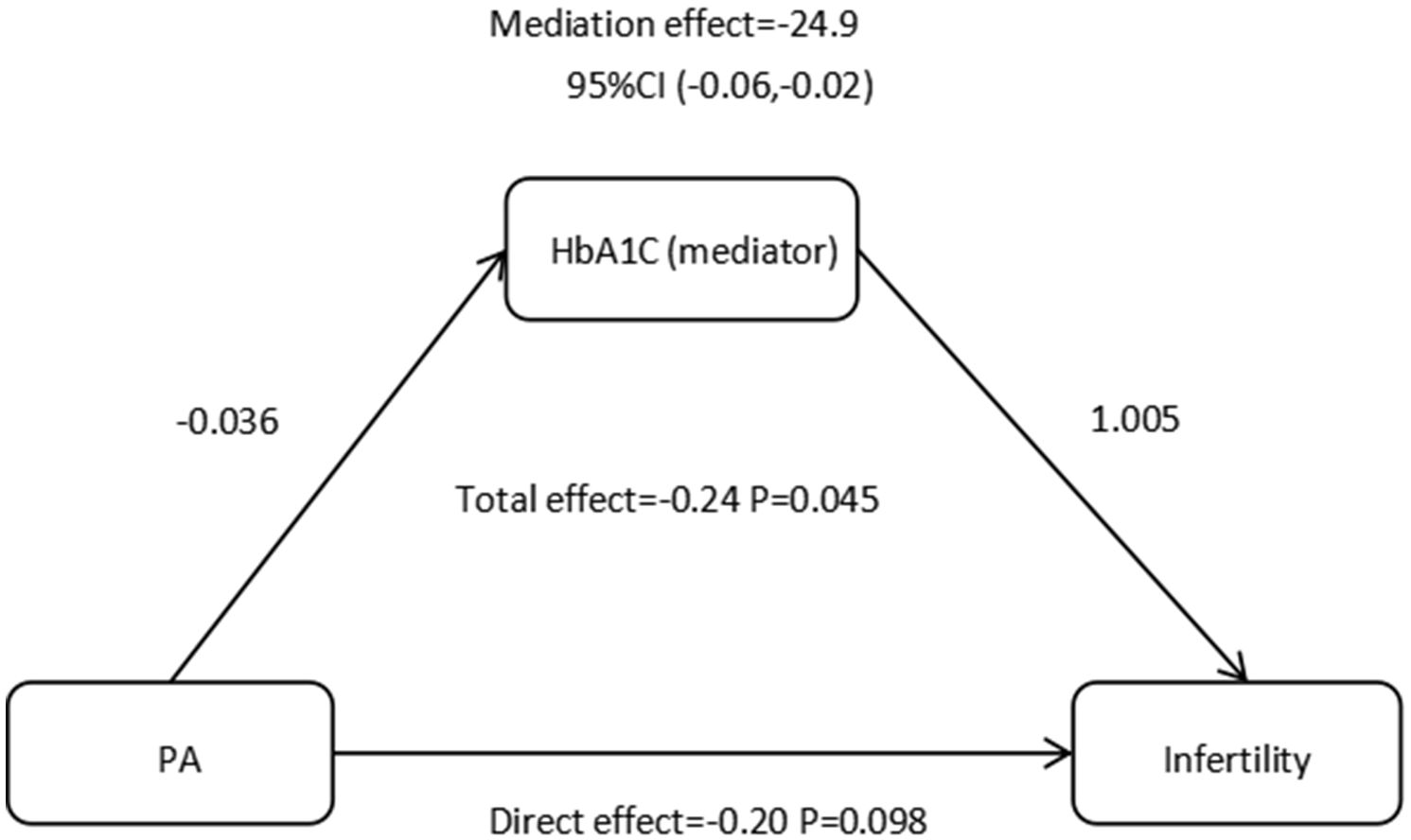
Figure 2. Effect of the HbA1C (mediators) on the relationship between PA (exposure) and infertility (outcome). HbA1C, glycosylated hemoglobinl; PA, physical activity.
As society progresses and educational levels improve, an increasing number of individuals over the age of 35 express their desire to become pregnant, and infertility is particularly common among older women. While aging is the primary cause of declining fertility, the development of assisted reproductive technology in recent years has provided the possibility of reproduction for older infertile women. As a result, physiological and individual factors play an important role for women of advanced reproductive age. Our study extended the age range of the research subjects to females aged 18 to 49, potentially increasing the universality and application of the research findings, allowing them to span a broader range of female populations and providing more thorough data support for clinical treatment. This study primarily investigated the role of HbA1c in modulating the link between PA and infertility. We performed a cross-sectional study utilizing a questionnaire survey to examine the interrelations among PA, HbA1c, and infertility within a population that willingly participated in the survey in the United States throughout the same period of time. The incidence of infertility is lower with active PA, as recommended by WHO, than with inactive PA. However, this tendency was solely evident in recreation-related PA, with no differences in infertility rates being associated with work-related PA. Moreover, HbA1c is negatively correlated with PA and positively correlated with infertility, and it may mediate the link between PA and infertility. The impact of obesity and a history of diabetes on infertility is primarily mediated by PA.
By distinguishing our study from previous studies, we specifically offer a novel perspective by categorizing PA patterns in accordance with World Health Organization(WHO) guidelines. This choice was based on the clear notion that neither high-intensity nor moderate PA encompasses the duration of the activity. Research has indicated that moderate PA enhances pregnancy rates in women with reproductive problems and that consistent moderate PA supports reproductive health maintenance (19–21). HaKimi et al. analyzed an extensive amount of literature and proposed that exceeding 60 minutes of strenuous exercise on a daily basis increases the chance of anovulation; however, 30–60 minutes of moderate-intensity exercise may mitigate ovulatory infertility. Therefore, following the WHO guidelines, we classify exercise into inactive, less active, and active exercise types while considering both exercise intensity and duration (22).
Our research indicated that the relationship between different types of physical PA and infertility is inconsistent. recreation-related PA is strongly associated with reduced infertility rates, which is consistent with the findings of previous studies that highlighted its importance for improving reproductive health in women of childbearing age (23). We propose that this effect is due to the advantageous benefits of consistent recreational activity, as recommended by WHO. This may mitigate the adverse effects of an energy deficit on fertility by increasing the body’s metabolic rate, regulating endocrine function and strengthening immunity (24). However, such nonlinear associations have not been recognized between work-related PA and infertility. Research on the relationship between work-related PA and infertility has produced inconsistent findings. Some evidence indicated that increased levels of work-related PA are associated with a greater risk of infertility (25). However, other studies suggested that insufficient work-related PA may adversely affect fertility (26). Furthermore, our research revealed no substantial correlation between work-related PA and infertility. We have analyzed potential explanations and shown that PA predominantly affects female reproductive health via metabolic control, whereas work activities denote obligations that individuals must fulfill during working hours, which often entails extended and low-intensity static tasks. Unlike leisure activities, which are predominantly subjective, work-related PA may not aid in metabolic regulation. A study of Taiwanese workers also revealed no significant relationship between work-related PA and metabolic markers (27, 28). This may also be linked to endocrine regulation. Research has indicated that PA augments the body’s biosynthetic response by increasing the levels of growth hormone and insulin-like growth factor, thus promoting reproductive health (29). The research by Schjeldrup Skarpsno (30) suggested a correlation between professional activity and insomnia, which clearly affects endocrine function.
Previous studies have reported that abnormal HbA1c is related to pregnancy problems. High HbA1c can increase the risk of gestational diabetes mellitus (31), and may also increase the risk of early abortion and premature birth (32, 33). Most importantly, our research suggests that HbA1c may play a role in the connection between recreation-related PA and infertility. Our data indicate that PA can downregulate HbA1c and has a negative correlation with infertility, which is consistent with the findings of previous studies (34, 35). HbA1c serves as a diagnostic tool for monitoring diabetes. Numerous studies have investigated the effects of a physically active lifestyle on individuals who are diagnosed with diabetes (36, 37). A previous study revealed that children diagnosed with type 1 diabetes who had lower levels of PA had poorer blood glucose control than did children who participated in more consistent PA. The level of HbA1c was significantly elevated in the less physically active group compared with the more physically active group (38). An analysis of a population sample of women aged 18–45 years in the United States revealed a notably positive association between HbA1c levels and infertility (39). However, this study investigated the role of HbA1c in influencing the association between PA patterns and infertility. We identified the mediating regulatory function of HbA1c. The findings of this study demonstrated that recreation-related PA does not have a statistically significant direct effect on infertility, as evidenced by a coefficient of -0.20. These findings suggest that the influence of exercise on infertility is consistently moderated by additional factors. The statistical analysis demonstrated that the mediating effect of HbA1c was significant, as evidenced by a coefficient of -24.9. These findings provide some evidence for the potential role of HbA1c in the modulation of PA on infertility, but more research is required to establish a definitive conclusion.
Finally, we unexpectedly found that the influence of obesity and a history of diabetes on infertility is mainly regulated by PA. The impact of obesity on the incidence of infertility mainly occurs in the active and less active population, thus indicating that weight loss in women who exercise is beneficial for their reproductive health, whereas weight loss alone does not promote female reproductive health in women who do not exercise. This may indicate that simply losing weight is not related to promoting reproductive health. A large amount of clinical data has confirmed that weight loss can improve reproductive function, and weight loss has become a basic component of infertility treatment for obese individuals (40). However, previous research has shown that increasing weight loss in obese or overweight women before IVF treatment does not improve reproductive outcomes (41). Our research results also confirmed this finding. In addition, among the less active population, a history of diabetes does not affect the incidence of infertility, which indicates that less activity may be beneficial to women with a history of diabetes.
Our research provides further evidence for the negative correlation between PA and infertility; moreover, based on previous reports, we found no significant correlation between work-related PA and infertility incidence. These findings suggest that recreation-related PA has greater significance in promoting reproductive health. In addition, mediation analysis revealed potential reasons for the association between PA and infertility. Based on these data, it will be possible to provide patients with more accurate and evidence-based advice to determine the optimal frequency and intensity of exercise, thus increasing their chances of pregnancy. Finally, the findings of hierarchical analysis also suggest that, in our clinical research, the body mass index of individuals who exercise is more worthy of attention, and less active PA is more recommended for women with a history of diabetes.
However, this study has several significant drawbacks. The cross-sectional approach that was used in our study did not allow us to establish a cause-effect association between PA and infertility. To confirm this relationship, additional prospective cohort studies or randomized controlled trials are needed. Furthermore, the identification of diseases depends on self-reported responses from participants, which could lead to the introduction of recall bias and misclassification. Nevertheless, prior research has demonstrated that data obtained from the NHANES are reliable for evaluating the prevalence of infertility in the entire population (42, 43). Finally, future research might look into the reasons and treatment methods of infertility in women of different ages, as well as how to provide more individualized fertility support to women of all ages.
In conclusion, the findings of this study revealed that confounding factors had a significant influence on the correlation between the two variables. Although stratified analysis has been conducted, further inquiries are needed to explore the relationships between confounding factors and infertility. Although mediation analysis is essential, it is worth noting that the results obtained within the cross-sectional framework are still correlated and do not prove causal relationships.
Our results revealed that HbA1c may play a potencial mediation role in the association between PA and infertility, thus revealing a potential mechanism underlying the association between PA and infertility, which offers valuable insights for establishing healthy PA guidelines for women. However, due to the fact that this study was a cross-sectional study, more prospective cohort studies are needed in the future to explore causality.
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author/s.
The studies involving humans were approved by NCHS Ethics Review Board (ERB). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
PC: Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Validation, Writing – original draft. LZ: Software, Writing – review & editing. YM: Project administration, Writing – review & editing. SZ: Formal analysis, Methodology, Supervision, Writing – review & editing. GH: Funding acquisition, Resources, Supervision, Writing – review & editing.
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the National Natural Science Foundation of China (grant number: 8226060384, 2022). Research sponsor Dr. Guanyou Huang participated in the design and paper review of the study.
This work was conducted with support from the reproductive medicine center, the Department of Obstetrics and Gynecology, and the affiliated hospital of Guizhou Medical University.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2025.1495470/full#supplementary-material
1. Carson SA, Kallen AN. Diagnosis and management of infertility: A review. JAMA. (2021) 326:65–76. doi: 10.1001/jama.2021.4788
2. Zegers-Hochschild F, Adamson GD, Dyer S, Racowsky C, de Mouzon J, Sokol R, et al. The international glossary on infertility and fertility care, 2017. Hum Reprod. (2017) 32:1786–801. doi: 10.1093/humrep/dex234
3. Park SU, Walsh L, Berkowitz KM. Mechanisms of ovarian aging. Reproduction. (2021) 162:R19–r33. doi: 10.1530/REP-21-0022
4. Vitagliano A, Paffoni A, Viganò P. Does maternal age affect assisted reproduction technology success rates after euploid embryo transfer? A systematic review and meta-analysis. Fertil Steril. (2023) 120:251–65. doi: 10.1016/j.fertnstert.2023.02.036
5. Pedersen BK, Saltin B. Exercise as medicine - evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand J Med Sci Sports. (2015) 25 Suppl 3:1–72. doi: 10.1111/sms.12581
6. Collee J, Mawet M, Tebache L, Nisolle M, Brichant G. Polycystic ovarian syndrome and infertility: overview and insights of the putative treatments. Gynecol Endocrinol. (2021) 37:869–74. doi: 10.1080/09513590.2021.1958310
7. Xie F, You Y, Guan C, Gu Y, Yao F, Xu J. Association between physical activity and infertility: a comprehensive systematic review and meta-analysis. J Transl Med. (2022) 20:237. doi: 10.1186/s12967-022-03426-3
8. Hernaez A, Lee Y, Page CM, Skara KH, Haberg SE, Magnus P, et al. Impaired glucose tolerance and cardiovascular risk factors in relation to infertility: a Mendelian randomization analysis in the Norwegian Mother, Father, and Child Cohort Study. Hum Reprod. (2024) 39:436–41. doi: 10.1093/humrep/dead234
9. Liao CC, Lee CI, Liao KR, Li JM. Association between serum glycated hemoglobin levels and female infertility: A cross-sectional survey and genetic approach. Int J Mol Sci. (2024) 25:9668. doi: 10.3390/ijms25179668
10. Kadiroğulları P, Demir E, Bahat PY, Kıyak H, Seckin KD. Evaluation of relationship between HbA1c levels and ovarian reserve in patients with type 1 diabetes mellitus. Gynecol Endocrinol. (2020) 36:426–30. doi: 10.1080/09513590.2019.1708893
11. Yun I, Joo HJ, Park YS, Park EC. Association between physical exercise and glycated hemoglobin levels in Korean patients diagnosed with diabetes. Int J Environ Res Public Health. (2022) 19:3280. doi: 10.3390/ijerph19063280
12. Nair R, Meadows E, Sheer R, Lipkovich I, Poon JL, Zhao Z, et al. Activation, physical activity, and outcomes among individuals with T2D. Am J Manag Care. (2022) 28:374–80. doi: 10.37765/ajmc
13. Cowan S, Lim S, Alycia C, Pirotta S, Thomson R, Gibson-Helm M, et al. Lifestyle management in polycystic ovary syndrome - beyond diet and physical activity. BMC Endocr Disord. (2023) 23:14. doi: 10.1186/s12902-022-01208-y
14. WHO Guidelines Approved by the Guidelines Review Committee. Global Recommendations on Physical Activity for Health. Geneva: World Health Organization Copyright © World Health Organization (2010).
15. Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. (2020) 54:1451–62. doi: 10.1136/bjsports-2020-102955
16. Pratt M. What’s new in the 2020 world health organization guidelines on physical activity and sedentary behavior? J Sport Health Sci. (2021) 10:288–9. doi: 10.1016/j.jshs.2021.02.004
17. Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. (1986) 51:1173–82. doi: 10.1037/0022-3514.51.6.1173
18. Mackinnon DP, Cox MC. Commentary on “Mediation analysis and categorical variables: the final frontier” by dawn iacobucci. J Consum Psychol. (2012) 22:600–2. doi: 10.1016/j.jcps.2012.03.009
19. Starowicz J, Pratt K, McMorris C, Brunton L. Mental health benefits of physical activity in youth with cerebral palsy: A scoping review. Phys Occup Ther Pediatr. (2022) 42:434–50. doi: 10.1080/01942638.2022.2060058
20. Premusz V, Makai A, Perjes B, Mate O, Hock M, Acs P, et al. Multicausal analysis on psychosocial and lifestyle factors among patients undergoing assisted reproductive therapy - with special regard to self-reported and objective measures of pre-treatment habitual physical activity. BMC Public Health. (2021) 21:1480. doi: 10.1186/s12889-020-09522-7
21. Rebar AL, Stanton R, Geard D, Short C, Duncan MJ, Vandelanotte C. A meta-meta-analysis of the effect of physical activity on depression and anxiety in non-clinical adult populations. Health Psychol Rev. (2015) 9:366–78. doi: 10.1080/17437199.2015.1022901
22. Hakimi O, Cameron LC. Effect of exercise on ovulation: A systematic review. Sports Med. (2017) 47:1555–67. doi: 10.1007/s40279-016-0669-8
23. Zhang H, Hua L, Liu D, Su X, Chen J, Chen J. Effects of physical activity on infertility in reproductive females. Reprod Biol Endocrinol. (2024) 22:62. doi: 10.1186/s12958-024-01234-6
24. Bartlett DB, Willis LH, Slentz CA, Hoselton A, Kelly L, Huebner JL, et al. Ten weeks of high-intensity interval walk training is associated with reduced disease activity and improved innate immune function in older adults with rheumatoid arthritis: a pilot study. Arthritis Res Ther. (2018) 20:127. doi: 10.1186/s13075-018-1624-x
25. Gudmundsdottir SL, Flanders WD, Augestad LB. Physical activity and fertility in women: the North-Trøndelag Health Study. Hum Reprod. (2009) 24:3196–204. doi: 10.1093/humrep/dep337
26. Dhair A, Abed Y. The association of types, intensities and frequencies of physical activity with primary infertility among females in Gaza Strip, Palestine: A case-control study. PLoS One. (2020) 15:e0241043. doi: 10.1371/journal.pone.0241043
27. Huang JH, Li RH, Huang SL, Sia HK, Lee SS, Wang WH, et al. Relationships between different types of physical activity and metabolic syndrome among Taiwanese workers. Sci Rep. (2017) 7:13735. doi: 10.1038/s41598-017-13872-5
28. Feig EH, Levy DE, McCurley JL, Rimm EB, Anderson EM, Gelsomin ED, et al. Association of work-related and leisure-time physical activity with workplace food purchases, dietary quality, and health of hospital employees. BMC Public Health. (2019) 19:1583. doi: 10.1186/s12889-019-7944-1
29. Butt MS, Saleem J, Zakar R, Aiman S, Khan MZ, Fischer F. Benefits of physical activity on reproductive health functions among polycystic ovarian syndrome women: a systematic review. BMC Public Health. (2023) 23:882. doi: 10.1186/s12889-023-15730-8
30. Skarpsno ES, Nilsen TIL, Sand T, Hagen K, Mork PJ. Work-related mental fatigue, physical activity and risk of insomnia symptoms: longitudinal data from the norwegian HUNT study. Behav Sleep Med. (2020) 18:488–99. doi: 10.1080/15402002.2019.1614927
31. Zhang J, Zhou F, Xu T, Xu J, Li Y, Lin L, et al. The diagnostic value of glycosylated hemoglobin for gestational diabetes mellitus in Asian populations: A systematic review and meta-analysis. J Obstet Gynaecol Res. (2022) 48:902–11. doi: 10.1111/jog.15170
32. Chen X, Zhang Y, Chen H, Dou Y, Wang Y, He W, et al. Association between serum glycated hemoglobin levels at early gestation and the risk of subsequent pregnancy loss in pregnant women without diabetes mellitus: prospective cohort study. JMIR Public Health Surveill. (2023) 9:e46986. doi: 10.2196/46986
33. Chen H, Tan Q, Lai S, Mai H, Wang D. Association between glycated hemoglobin and the risk of neonatal respiratory distress syndrome in preterm premature rupture of membranes pregnancies. Sci Rep. (2024) 14:27122. doi: 10.1038/s41598-024-78679-7
34. Jansson AK, Chan LX, Lubans DR, Duncan MJ, Plotnikoff RC. Effect of resistance training on HbA1c in adults with type 2 diabetes mellitus and the moderating effect of changes in muscular strength: a systematic review and meta-analysis. BMJ Open Diabetes Res Care. (2022) 10:e002595. doi: 10.1136/bmjdrc-2021-002595
35. Mussawar M, Balsom AA, Totosy de Zepetnek JO, Gordon JL. The effect of physical activity on fertility: a mini-review. F S Rep. (2023) 4:150–8. doi: 10.1016/j.xfre.2023.04.005
36. Aljawarneh YM, Wardell DW, Wood GL, Rozmus CL. A systematic review of physical activity and exercise on physiological and biochemical outcomes in children and adolescents with type 1 diabetes. J Nurs Scholarsh. (2019) 51:337–45. doi: 10.1111/jnu.2019.51.issue-3
37. Elmesmari R, Reilly JJ, Martin A, Paton JY. Accelerometer measured levels of moderate-to-vigorous intensity physical activity and sedentary time in children and adolescents with chronic disease: A systematic review and meta-analysis. PLoS One. (2017) 12:e0179429. doi: 10.1371/journal.pone.0179429
38. Beraki A, Magnuson A, Sarnblad S, Aman J, Samuelsson U. Increase in physical activity is associated with lower HbA1c levels in children and adolescents with type 1 diabetes: results from a cross-sectional study based on the Swedish pediatric diabetes quality registry (SWEDIABKIDS). Diabetes Res Clin Pract. (2014) 105:119–25. doi: 10.1016/j.diabres.2014.01.029
39. Yu L, Li X, Xi K, Wu R. Elevated hbA1c level has a linear association with infertility in women. Clin Lab. (2024) 70. doi: 10.7754/Clin.Lab.2023.230725
40. Dağ Z, Dilbaz B. Impact of obesity on infertility in women. J Turk Ger Gynecol Assoc. (2015) 16:111–7. doi: 10.5152/jtgga.2015.15232
41. Jeong HG, Cho S, Ryu KJ, Kim T, Park H. Effect of weight loss before in vitro fertilization in women with obesity or overweight and infertility: a systematic review and meta-analysis. Sci Rep. (2024) 14:6153. doi: 10.1038/s41598-024-56818-4
42. Ji X, Ye Y, Wang L, Liu S, Dong X. Association between nutrient intake and female infertility: a study based on NHANES database. J Obstet Gynaecol. (2023) 43:2285025. doi: 10.1080/01443615.2023.2285025
Keywords: physical activity (PA), activity patterns, infertility, glycated hemoglobin (HbA1c), mediation
Citation: Chen P, Zhu L, Mou Y, Zhao S and Huang G (2025) The association between glycated hemoglobin, physical activity and infertility: a multiple logistic regression and mediation analysis based on the NHANES database. Front. Endocrinol. 16:1495470. doi: 10.3389/fendo.2025.1495470
Received: 12 September 2024; Accepted: 10 March 2025;
Published: 26 March 2025.
Edited by:
María Laura Ribeiro, CONICET Centro de Estudios Farmacológicos y Botánicos (CEFYBO), ArgentinaReviewed by:
Muniyappan Madesh, Yangzhou University, ChinaCopyright © 2025 Chen, Zhu, Mou, Zhao and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shuyun Zhao, emhhb3NodXl1bnNjaUAxMjYuY29t; Guanyou Huang, Z3VhbnlvdWh1YW5nQGhvdG1haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.