
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Endocrinol. , 07 March 2025
Sec. Clinical Diabetes
Volume 16 - 2025 | https://doi.org/10.3389/fendo.2025.1471292
 Yan Jiang1*
Yan Jiang1* Jiali Yu2
Jiali Yu2Background: Research into the relationship between the ratio of high-sensitivity C-reactive protein (hs-CRP) and high-density lipoprotein cholesterol (HDL-C) concerning type 2 diabetes mellitus (T2DM) is still scarce. The hs-CRP/HDL ratio could be an important biomarker for evaluating the risk of developing diabetes. This study primarily aims to investigate the association between hs-CRP/HDL ratios and the incidence of T2DM within a defined population.
Methods: This analysis was conducted using data from 9,381 participants aged 45 and older, obtained during the 2011 wave of the China Health and Retirement Longitudinal Study (CHARLS). The study evaluated the association between the hs-CRP/HDL ratio and the risk of developing type 2 diabetes mellitus (T2DM) employing multivariate logistic regression, subgroup analyses, smooth curve fitting, and threshold effect analysis.
Results: The overall prevalence of T2DM within the study population was found to be 16.3%, with 46.1% of cases occurring in men and 53.9% in women. Participants diagnosed with T2DM demonstrated a mean hs-CRP/HDL ratio that was 1.2 times higher than that of individuals without diabetes. The adjusted odds ratio (OR) for T2DM associated with hs-CRP/HDL levels was determined to be 0.75 (95% CI: 0.64–0.87). Additionally, a significant interaction was identified between hs-CRP/HDL ratios and variables such as sex and smoking in relation to T2DM risk (P < 0.05). Further subgroup analyses examining factors like age, education, marital status, hukou status, and drinking habits did not reveal any significant interactions (all P values for interaction were >0.05).
Conclusions: The results highlight a robust association between the hs-CRP/HDL ratio and the likelihood of developing T2DM, indicating its potential as a predictive biomarker for the condition. Additional research is required to clarify the relationship between hs-CRP/HDL ratios and the incidence of T2DM.
Type 2 diabetes mellitus (T2DM), responsible for approximately 90–95% of all diabetes mellitus (DM) cases, is a major contributor to global morbidity and mortality (1, 2). Diabetes is a significant risk factor for atherosclerosis and has been linked to a higher likelihood of mortality from various cancers, infections, and cardiovascular conditions (3). The International Diabetes Federation reports that, in 2021, 10.5% of adults aged 20–79 worldwide (equivalent to 536.6 million people) were living with diabetes, a figure projected to rise to 12.2% (643 million) by 2045 (4). Given these concerning statistics, identifying modifiable risk factors for T2DM is essential to improving prevention efforts and optimizing self-management strategies.
Diabetes is often associated with abnormal lipid metabolism, which is a major contributor to the development of diabetic vascular complications. Research indicates a strong association between high low-density lipoprotein cholesterol (LDL-C) levels and a heightened risk of aortic stenosis (5). HDL-C is crucial in lowering cardiovascular risk by enabling reverse cholesterol transport and exhibiting antioxidant, anti-inflammatory, and antithrombotic effects (6). Recent research indicates an inverse relationship between elevated HDL-C levels and the onset of T2DM, especially among middle-aged and older Chinese populations (7). Research by Yang T and colleagues has also identified the triglyceride-to-HDL-C ratio as a critical risk factor for both diabetes and the onset of T2DM (8). Research indicates elevated systemic inflammatory markers in patients with both atherosclerosis and type 2 diabetes (9). This inflammatory state can lead to insulin resistance and adversely affect endothelial function (10). In addition, hs-CRP, a recognised inflammatory biomarker, has been associated with diabetic nephropathy in several studies, highlighting its importance in the prediction and diagnosis of diabetes-related complications (11, 12).
HDL-C and hs-CRP are important and cost-effective biomarkers that are widely used to assess the risk of cardiovascular disease through their ratio (13). Despite well-documented significance in cardiovascular health, research on the hs-CRP/HDL-C ratio’s link to T2DM is limited. This study performed a cross-sectional analysis to explore the significance of the hs-CRP/HDL-C ratio in relation to T2DM. The aim is to improve the understanding of how this biomarker may influence diabetes risk and to support the development of clinical strategies aimed at early detection and intervention.
The CHARLS is an ongoing nationally representative longitudinal survey targeting adults aged 45 years and above. It aims to investigate aging in China and support interdisciplinary research by providing high-quality household microdata. The baseline survey for CHARLS was conducted during 2011–2012, encompassing 450 communities and villages across 150 districts in 28 provinces throughout the country, with subsequent follow-up surveys conducted every 2 to 3 years. Blood samples for the CHARLS dataset were collected during both the baseline and follow-up phases in 2011 and 2015, respectively. The National Development Institute of Peking University (IRB00001052-11015) approved the research project of CHARLS, and all participants signed an informed consent form before participating in the study. This cross-sectional study followed the ‘Strengthening the Reporting of Observational Studies in Epidemiology’ (STROBE) guidelines. All methods were conducted in accordance with relevant regulations and guidelines (14). For this analysis, data were drawn from the 2011 baseline survey, which included an initial cohort of 17,707 participants. Participants were excluded if they were under 45 years of age, missing data on high-sensitivity C-reactive protein (hs-CRP), high-density lipoprotein cholesterol (HDL-C), covariates and lacking documentation of diabetes or hyperglycemia. Finally, we included 9,381 participants in this study. The exclusion process is shown in Figure 1.
The concentrations of high-sensitivity C-reactive protein (hs-CRP) and high-density lipoprotein cholesterol (HDL-C) were measured in refrigerated blood samples using standard enzyme colorimetric assays at the Youanmen Center for Clinical Laboratory, Capital Medical University. The hs-CRP/HDL-C ratio was derived by dividing the hs-CRP concentration (expressed in mg/L) by the HDL-C level (expressed in mg/dL).
In this study, type 2 diabetes mellitus (T2DM) was defined based on criteria established by the American Diabetes Association in 2005. Specifically, T2DM was diagnosed if participants had a fasting blood glucose level of 126 mg/dL (7 mmol/L) or higher, a random blood glucose level of 200 mg/dL (11.1 mmol/L) or greater, an HbA1c level of 6.5% or above, or if they self-reported a diagnosis of diabetes or hyperglycemia in response to the question, “Have you ever been diagnosed with diabetes or hyperglycemia?”.
Socio-demographic information included age, sex, education level (divided into ‘primary school or less’ and ‘secondary school or higher’), hukou status (categorized as ‘agricultural’ or ‘non-agricultural’), and marital status (designated as ‘married’ or ‘unmarried’).
Health-related behaviors were assessed through various parameters, including smoking status (categorized as “never” versus “former or current smoker”), drinking patterns (classified as “never,” “former,” or “current drinker”), and duration of sleep. This health-related information was gathered using self-reported questionnaires facilitated by trained interviewers. For anthropometric data, systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured as the average of three readings obtained with an Omron HEM-7200 sphygmomanometer, ensuring precision in the evaluation of these vital signs.
Continuous variables were presented as means with standard deviations (SD) for normally distributed data and as medians with interquartile ranges (IQR) for skewed distributions. Categorical variables were reported as frequencies and percentages. One-way ANOVA, Kruskal–Wallis H test, or chi-square test was employed to compare the differences of variables among different quartiles the hs-CRP/HDL-C ratio. Logistic regression analyses, incorporating both unadjusted and adjusted models, were employed to examine the relationship between the hs-CRP/HDL ratio and the risk of T2DM development. The adjusted models incorporated various covariates such as age, sex, education level, marital status, hukou status, lifestyle factors like smoking and drinking, body mass index (BMI), SBP, DBP, lipid profile measures including total cholesterol (TC), triglycerides (TG), and low-density lipoprotein cholesterol (LDL-C). Penalized splines were employed for smooth curve fitting to evaluate the association between the hs-CRP/HDL-C ratio and T2DM. Sensitivity analyses were conducted to verify the robustness of the findings, and the trend significance was assessed by categorizing the hs-CRP/HDL-C ratio. Subgroup analyses were performed by stratifying relevant covariates to explore potential effect modification. Data analysis utilized R version 4.2.1 (The R Foundation, Vienna, Austria) and Free Statistics software version 1.9.2 (Beijing Free Clinical Medical Technology Co., Ltd, Beijing, China). p < 0.05 indicated statistical significance.
Table 1 outlines the baseline demographic and clinical characteristics of the study population, which included 9,381 participants. The median age of the entire cohort was 71 years (interquartile range [IQR]: 65-78). Notably, individuals diagnosed with type 2 diabetes mellitus (T2DM) were significantly older, with a median age of 73 years (IQR: 67-80), compared to 71 years (IQR: 64-78) for those without diabetes (p < 0.001). While the overall sex distribution was similar, with 46.1% of participants being male, significant differences were observed in clinical parameters. T2DM patients had higher mean systolic blood pressure (135.1 mmHg) compared to Non-T2DM individuals (129.5 mmHg, p < 0.001), as well as higher diastolic blood pressure (77.3 mmHg vs. 75.4 mmHg, p < 0.001).
Furthermore, individuals with T2DM presented a higher median body mass index (BMI) of 24.3 compared to 22.9 in the Non-T2DM group (p < 0.001), along with significantly elevated glucose levels (161.4 mg/dL vs. 100.1 mg/dL, p < 0.001). Lipid profile analysis indicated that T2DM patients had notably higher total cholesterol levels (199.6 mg/dL vs. 192.0 mg/dL, p < 0.001) and triglycerides (185.1 mg/dL vs. 121.0 mg/dL, p < 0.001), while exhibiting lower high-density lipoprotein cholesterol (HDL-C) levels (46.4 mg/dL vs. 52.1 mg/dL, p < 0.001). Additionally, levels of hs-CRP were significantly greater in the T2DM cohort (1.4 mg/L) compared to Non-T2DM individuals (1.0 mg/L, p < 0.001). The hs-CRP/HDL-C ratio was also markedly higher in the T2DM group at 3.2, in contrast to 2.0 for the Non-T2DM group (p < 0.001).
Table 2 presents the relationship between the hs-CRP/HDL-C ratio and the likelihood of developing type 2 diabetes mellitus (T2DM), including the analysis of different quartiles of this ratio. There was a clear trend indicating that the risk of T2DM increased progressively across the quartiles of the hs-CRP/HDL-C ratio (p for trend <0.001). Specifically, when comparing the first quartile (Q1) to the second quartile (Q2), the latter exhibited the highest risk for T2DM, with an odds ratio (OR) of 0.75 (95% CI: 0.64–0.87) after controlling for confounding factors such as age, sex, body mass index (BMI), smoking status, and alcohol intake (Table 3).
When assessed as a continuous variable, the hs-CRP/HDL-C ratio remained significantly associated with T2DM, yielding an OR of 0.49 (95% CI: 0.38–0.63). Figure 2 illustrates the association between the hs-CRP/HDL-C ratio and T2DM risk. Additionally, restricted cubic spline regression analysis revealed a linear correlation between the hs-CRP/HDL-C ratio and the likelihood of T2DM (p for linear <0.001). This consistent pattern reinforces the potential of the hs-CRP/HDL-C ratio as an important marker in assessing diabetes risk.
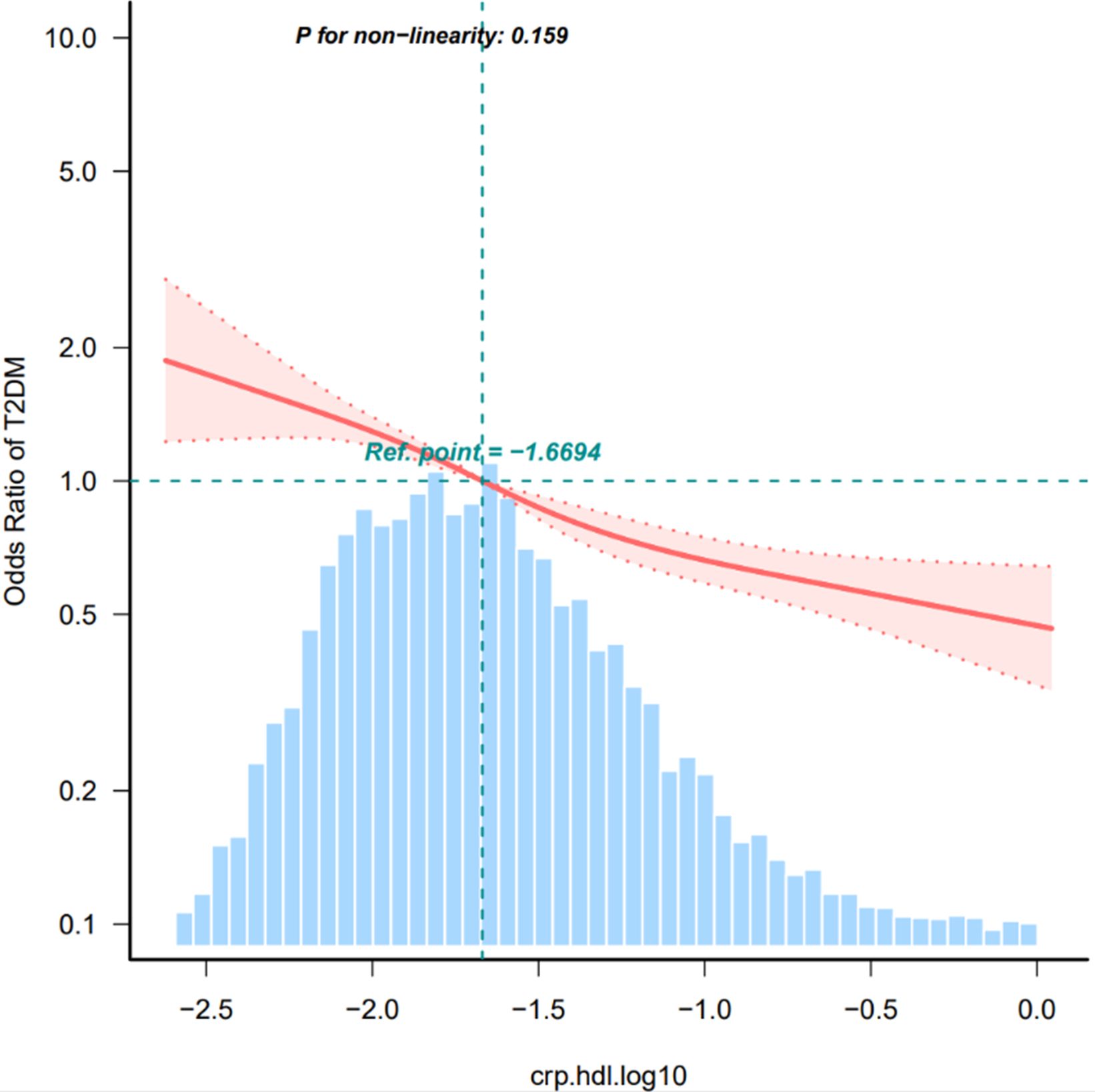
Figure 2. Restricted cubic spline of the association between hs-CRP/HDL and the risk of T2DM. The model was adjusted for age, sex, smoking status, drinking status, BMI. The plot shows a linear relationship between hs-CRP/HDL and the risk of T2DM. T2DM, diabetes mellitus; BMI, body mass index, HDL-C, high-density lipoprotein cholesterol; hs-CRP, Hypersensitive C-reactive protein. Only 99% of the data is shown.
To assess whether the hs-CRP/HDL-C ratio influences the risk of developing type 2 diabetes mellitus (T2DM) differently across various subgroups, participants were categorized based on their individual characteristics. The findings indicated that the impact of the hs-CRP/HDL-C ratio on T2DM risk remained consistent throughout these subgroups. Notably, a significant interaction was observed between the hs-CRP/HDL-C ratio and factors such as sex and smoking status (p for interaction <0.05).
In males, an increase of one interquartile range (IQR) in the hs-CRP/HDL-C ratio was linked to a 99.5% increase in the likelihood of developing T2DM, resulting in an odds ratio (OR) of 0.65 (95% CI: 0.49–0.78). However, it is important to consider that these results may lack clinical significance due to the multiple comparisons conducted and the similar patterns observed in the associations (Figure 3).
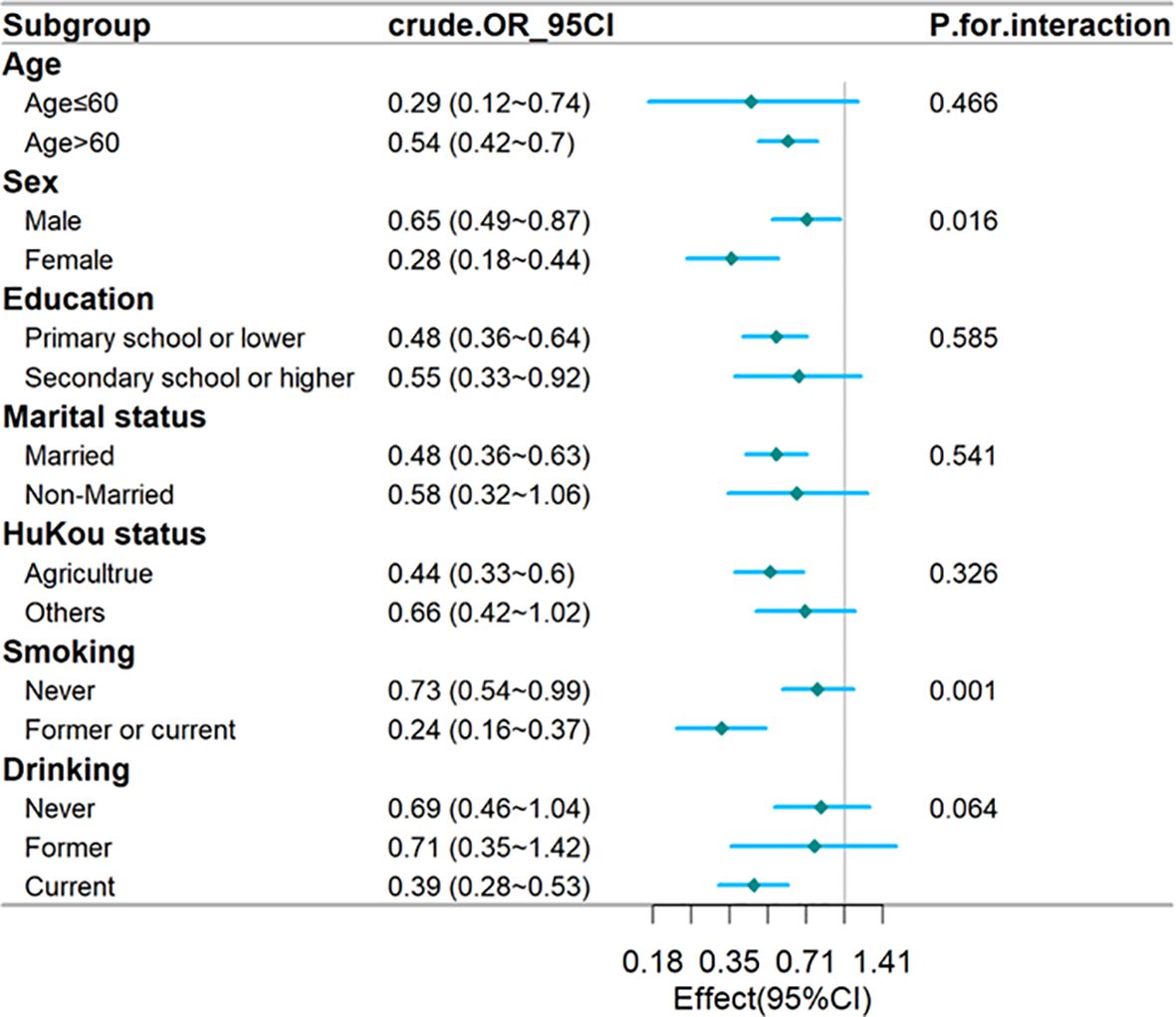
Figure 3. Forest plot of stratified analysis of the association of hs-CRP/HDL-C ratio with the risk of T2DM. The plot shows that there were significant interactions between hs-CRP/HDL-C ratio and sex. OR, odds ratio; CI, confidence intervals; T2DM, type 2 diabetes mellitus; hs-CRP, Hypersensitive C-reactive protein; HDL-C, high-density lipoprotein cholesterol.
In a cross-sectional study involving 9,381 participants, both baseline and follow-up data revealed a significant link between the development of T2DM and the hs-CRP to HDL-C ratio. Subgroup analyses based on age, education, marital status, hukou status, and drinking habits indicated no significant interactions. A significant interaction was identified between the hs-CRP/HDL-C ratio and variables like sex and smoking status (p < 0.05). The hs-CRP/HDL-C ratio appears to be a significant biomarker for predicting T2DM risk.
To control for potential confounders, we established three logical regression models to analyze the association between hs-CRP/HDL-C ratio and T2DM. In fully adjusted model 3, the effect value is 0.59 (0.46~0.76). Simultaneously, we divided hs-CRP/HDL-C ratio into three groups and conducted sensitivity analysis on results, which showed that the results were stable and reliable (Table 2). Additionally, we validated the results in age, education, marital status, hukou status, and drinking habits and found that they were stable in all subgroups without interaction. A significant interaction was identified between the hs-CRP/HDL-C ratio and variables like sex and smoking status (p < 0.05) (Figure 3). The fitting curve (Figure 2) between hs-CRP/HDL-C ratio and T2DM was drawn after adjustment according to model 2, in order to better present this result and observe the linear relationship between hs-CRP/HDL-C ratio and T2DM. This is also consistent with our validation of trend lines.
Several studies explored the associations between various biomarkers and the risk of T2DM in middle-aged and elderly populations. Hs-CRP was found to be positively associated with T2DM risk (15). The hs-CRP/HDL-C ratio emerged as a significant predictor of cardiovascular disease risk (13). Several lipid parameters, including non-HDL-C, TG, TC/HDL-C, and TG/HDL-C, demonstrated superior performance in predicting T2DM incidence (16, 17). Time-dependent TG/HDL-C ratios were positively associated with T2DM risk in elderly Chinese populations (18). Additionally, hs-CRP levels were linked to metabolic syndrome and low HDL-C levels (19). These findings highlight the importance of considering inflammatory and lipid markers in assessing T2DM risk and potential interventions for middle-aged and elderly individuals.
Some studies may partially explain the underlying mechanisms. Throughout T2DM progression, plasma triglycerides and LDL-C typically rise, while HDL-C levels tend to decline (20). HDL-C exhibits cardioprotective effects, including antioxidant, antithrombotic, and anti-inflammatory properties. It plays a crucial role in reverse cholesterol transport, modulates immune processes, and inhibits endothelial dysfunction (21, 22). HDL-C dysfunction, including structural changes and metabolic abnormalities, is linked to the pathogenesis and prognosis of T2DM, beyond mere alterations in HDL-C levels (23). However, low HDL-C levels may affect glucose homeostasis by reducing insulin secretion, insulin sensitivity and direct glucose uptake by muscle via adenosine monophosphate(AMP)-activated protein kinase (24). In addition, HDL-C has also been shown to potentially regulate glucose homeostasis through mechanisms such as insulin secretion, direct glucose uptake by muscle and increased insulin sensitivity (25). This impacts insulin secretion and blood glucose regulation, potentially leading to diabetes. HDL-C plays a role in cholesterol transport and reduced HDL-C levels can compromise cell membrane stability, impacting insulin receptor structure and function, which in turn influences insulin secretion and sensitivity (26–28). These findings support the idea that raising HDL-C levels could be a viable therapeutic approach to reduce the risk of developing T2DM (29). Hs-CRP, a well-established marker of inflammation, has been recognized as a risk factor for T2DM in cohort studies, particularly when elevated (15). In addition, people in the pre-diabetic stage with moderate to high levels of hs-CRP have an increased risk of developing diabetes compared to those with lower levels (30).
Most research into the prediction of T2DM risk has focused on individual lipid or inflammatory markers. In contrast, this study examines the interaction between lipid metabolism and inflammation, focusing specifically on composite inflammatory lipid markers found in peripheral blood. Such an integrated approach could be of significant benefit to clinicians, particularly primary care providers, by facilitating early intervention in patients at risk of diabetes, ultimately helping to reduce disease progression and improve patient outcomes. Therefore, we speculate that lowering hs-CRP/HDL ratio may be a good way to regulate the health status of T2DM patients. However, more prospective studies are needed to determine whether this study is applicable to a wider population.
Nonetheless, this research is subject to certain limitations. Firstly, it relies on secondary data, which can be affected by measurement inaccuracies, variations in case definitions and differences in study design. The inclusion of participants with baseline hypertension and hyperlipidaemia, along with their use of antihypertensive and lipid-lowering medications, may impact the accuracy of hs-CRP and HDL-C measurements. This study focused on middle-aged and elderly individuals in China, indicating the necessity for future research to validate findings in a more diverse population. Finally, the cross-sectional design limits the ability to establish a temporal relationship between hs-CRP and HDL-C levels.
The findings from this cross-sectional study indicate a positive association between the hs-CRP/HDL ratio and the risk of developing type 2 diabetes mellitus (T2DM) within the CHARLS cohort. Nonetheless, additional research is needed to validate and confirm these results in different populations and settings.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
The studies involving humans were approved by the Peking University BiomedicalEthics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. The human samples used in this study were acquired from primarily isolated as part of your previous study for which ethical approval was obtained. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
YJ: Writing – original draft. JY: Writing – original draft.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
We would like to express our sincere gratitude to Dr. Jie Liu from the Department of Vascular and Endovascular Surgery at the Chinese PLA General Hospital & Physician-Scientist Center of China for his invaluable contributions, including statistical support, guidance on study design, and insightful comments on the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Holman N, Wild SH, Khunti K, Knighton P, O’Keefe J, Bakhai C, et al. Incidence and characteristics of remission of type 2 diabetes in england: A cohort study using the national diabetes audit. Diabetes Care. (2022) 45:1151–61. doi: 10.2337/dc21-2136
2. Chen L, Islam RM, Wang J, Hird TR, Pavkov ME, Gregg EW, et al. A systematic review of trends in all-cause mortality among people with diabetes. Diabetologia. (2020) 63:1718–35. doi: 10.1007/s00125-020-05199-0
3. Rao Kondapally Seshasai S, Kaptoge S, Thompson A, Di Angelantonio E, Gao P, Sarwar N, et al. Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med. (2011) 364:829–41. doi: 10.1056/NEJMoa1008862
4. Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. (2022) 183:109119. doi: 10.1016/j.diabres.2021.109119
5. Nazarzadeh M, Pinho-Gomes A-C, Bidel Z, Dehghan A, Canoy D, Hassaine A, et al. Plasma lipids and risk of aortic valve stenosis: a Mendelian randomization study. Eur Heart J. (2020) 41:3913–20. doi: 10.1093/eurheartj/ehaa070
6. Jung E, Kong SY, Ro YS, Ryu HH, Shin SD. Serum cholesterol levels and risk of cardiovascular death: A systematic review and a dose-response meta-analysis of prospective cohort studies. Int J Environ Res Public Health. (2022) 19:8272. doi: 10.3390/ijerph19148272
7. Cao X, Tang Z, Zhang J, Li H, Singh M, Sun F, et al. Association between high-density lipoprotein cholesterol and type 2 diabetes mellitus among Chinese: the Beijing longitudinal study of aging. Lipids Health Dis. (2021) 20:71. doi: 10.1186/s12944-021-01499-5
8. Yang T, Liu Y, Li L, Zheng Y, Wang Y, Su J, et al. Correlation between the triglyceride-to-high-density lipoprotein cholesterol ratio and other unconventional lipid parameters with the risk of prediabetes and Type 2 diabetes in patients with coronary heart disease: a RCSCD-TCM study in China. Cardiovasc Diabetol. (2022) 21:93. doi: 10.1186/s12933-022-01531-7
9. Ménégaut L, Laubriet A, Crespy V, Leleu D, Pilot T, Van Dongen K, et al. Inflammation and oxidative stress markers in type 2 diabetes patients with Advanced Carotid atherosclerosis. Cardiovasc Diabetol. (2023) 22:248. doi: 10.1186/s12933-023-01979-1
10. Aldhahi W, Hamdy O. Adipokines, inflammation, and the endothelium in diabetes. Curr Diabetes Rep. (2003) 3:293–8. doi: 10.1007/s11892-003-0020-2
11. Lin C-C, Li C-I, Liu C-S, Liao L-N, Yang C-W, Lin C-H, et al. Association of high-sensitivity C-reactive protein and diabetic nephropathy in patients with type 2 diabetes: a Mendelian randomization study. BMJ Open Diabetes Res Care. (2023) 11:e003197. doi: 10.1136/bmjdrc-2022-003197
12. Association between high-sensitivity C-reactive protein and diabetic kidney disease in patients with type 2 diabetes mellitus - pubMed . Available online at (Accessed November 28, 2024).
13. Gao Y, Wang M, Wang R, Jiang J, Hu Y, Wang W, et al. The predictive value of the hs-CRP/HDL-C ratio, an inflammation-lipid composite marker, for cardiovascular disease in middle-aged and elderly people: evidence from a large national cohort study. Lipids Health Dis. (2024) 23:66. doi: 10.1186/s12944-024-02055-7
14. Noah N. The STROBE initiative: STrengthening the Reporting of OBservational studies in Epidemiology (STROBE). Epidemiol Infect. (2008) 136:865. doi: 10.1017/S0950268808000733
15. Yang X, Tao S, Peng J, Zhao J, Li S, Wu N, et al. High-sensitivity C-reactive protein and risk of type 2 diabetes: A nationwide cohort study and updated meta-analysis. Diabetes Metab Res Rev. (2021) 37:e3446. doi: 10.1002/dmrr.3446
16. Peng J, Zhao F, Yang X, Pan X, Xin J, Wu M, et al. Association between dyslipidemia and risk of type 2 diabetes mellitus in middle-aged and older Chinese adults: a secondary analysis of a nationwide cohort. BMJ Open. (2021) 11:e042821. doi: 10.1136/bmjopen-2020-042821
17. Song Q, Liu X, Wang A, Wang Y, Zhou Y, Zhou W, et al. Associations between non-traditional lipid measures and risk for type 2 diabetes mellitus in a Chinese community population: a cross-sectional study. Lipids Health Dis. (2016) 15:70. doi: 10.1186/s12944-016-0239-y
18. Zheng D, Li H, Ai F, Sun F, Singh M, Cao X, et al. Association between the triglyceride to high-density lipoprotein cholesterol ratio and the risk of type 2 diabetes mellitus among Chinese elderly: the Beijing Longitudinal Study of Aging. BMJ Open Diabetes Res Care. (2020) 8:e000811. doi: 10.1136/bmjdrc-2019-000811
19. Fu S, Ping P, Luo L, Ye P. Deep analyses of the associations of a series of biomarkers with insulin resistance, metabolic syndrome, and diabetes risk in nondiabetic middle-aged and elderly individuals: results from a Chinese community-based study. Clin Interv Aging. (2016) 11:1531–8. doi: 10.2147/CIA.S109583
20. Farbstein D, Levy AP. HDL dysfunction in diabetes: causes and possible treatments. Expert Rev Cardiovasc Ther. (2012) 10:353–61. doi: 10.1586/erc.11.182
21. Martagon AJ, Zubirán R, González-Arellanes R, Praget-Bracamontes S, Rivera-Alcántara JA, Aguilar-Salinas CA. HDL abnormalities in type 2 diabetes: Clinical implications. Atherosclerosis. (2024) 394:117213. doi: 10.1016/j.atherosclerosis.2023.117213
22. HDL cholesterol and protective factors in atherosclerosis - PubMed . Available online at (Accessed January 1, 2025).
23. Xepapadaki E, Nikdima I, Sagiadinou EC, Zvintzou E, Kypreos KE. HDL and type 2 diabetes: the chicken or the egg? Diabetologia. (2021) 64:1917–26. doi: 10.1007/s00125-021-05509-0
24. Kraegen EW, Cooney GJ, Turner N. Muscle insulin resistance: a case of fat overconsumption, not mitochondrial dysfunction. Proc Natl Acad Sci U.S.A. (2008) 105:7627–8. doi: 10.1073/pnas.0803901105
25. Drew BG, Rye K-A, Duffy SJ, Barter P, Kingwell BA. The emerging role of HDL in glucose metabolism. Nat Rev Endocrinol. (2012) 8:237–45. doi: 10.1038/nrendo.2011.235
26. Ma W, Lin M, Ding H, Lin G, Zhang Z. [amp]]beta;-COP as a component of transport vesicles for HDL apolipoprotein-mediated cholesterol exocytosis. PloS One. (2016) 11:e0151767. doi: 10.1371/journal.pone.0151767
27. Bardini G, Dicembrini I, Rotella CM, Giannini S. Correlation between HDL cholesterol levels and beta-cell function in subjects with various degree of glucose tolerance. Acta Diabetol. (2013) 50:277–81. doi: 10.1007/s00592-011-0339-0
28. Wang X, Huang C, Liu Y, Han Y, Hu H. Association of estimated glomerular filtration rate and incident pre-diabetes: A secondary 5-year longitudinal cohort study in Chinese people. Front Endocrinol (Lausanne). (2022) 13:965545. doi: 10.3389/fendo.2022.965545
29. Fazio S, Linton MF. Killing two birds with one stone, maybe: CETP inhibition increases both high-density lipoprotein levels and insulin secretion. Circ Res. (2013) 113:94–6. doi: 10.1161/CIRCRESAHA.113.301832
Keywords: type 2 diabetes mellitus, Hs-CRP, HDL, inflammatory markers, CHARLS
Citation: Jiang Y and Yu J (2025) Association between hs-CRP/HDL with type 2 diabetes mellitus in middle-aged and elderly people: a cross-sectional study from CHARLS. Front. Endocrinol. 16:1471292. doi: 10.3389/fendo.2025.1471292
Received: 27 July 2024; Accepted: 04 February 2025;
Published: 07 March 2025.
Edited by:
Sui Kiat Chang, Universiti Tunku Abdul Rahman, MalaysiaReviewed by:
Ai Kah Ng, University of Malaya, MalaysiaCopyright © 2025 Jiang and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yan Jiang, amlhbmd5YW5AbnR1LmVkdS5jbg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.