- 1Department of Endocrinology, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania
- 2First Endocrinology Department, “C. I. Parhon” National Institute of Endocrinology, Bucharest, Romania
- 3Department of Endocrinology, Aalborg University Hospital, Aalborg, Denmark
- 4Steno Diabetes Center North Jutland, Aalborg, Denmark
Editorial on the Research Topic
Cancer risk in patients with acromegaly – is extensive screening needed?
Acromegaly is a rare endocrine disorder characterized by excessive growth hormone (GH) and insulin-like growth factor I (IGF-I) production. Its symptoms include enlarged extremities and organs; complications are cardiovascular, respiratory, metabolic, musculoskeletal, neurological, benign and malign tumors (1–3). However, the extent to which acromegaly increases cancer risk and mortality remains controversial, as does the need for extensive screening. The most recent consensus statement did not establish whether colonoscopy should be performed in all patients at diagnosis, regardless of age (4). The previous guideline of Endocrine Society recommended a baseline screening colonoscopy, with follow-up every five years if polyps are present or IGF-1 levels are elevated (5). For other cancers associated with acromegaly, including thyroid cancer, screening should be performed according to guidelines for the general population (4, 6).
While GH may play a role in malignancy progression (enhancing promitogenic and anti-apoptotic properties), it does not seem to induce malignancy (7). Complications of acromegaly, such as increased intestinal size or diabetes are other risk factors for malignancy (8). However, the risk of malignancies in acromegaly remains controversial. Epidemiological studies show diverging results. Up to 2016, a modestly increased cancer risk was reported, especially for colon and thyroid neoplasms (9–12). Several studies have since then reported an increased cancer risk (10–16), while others have not (17) – see Table 1. A recent meta-analysis revealed an increased risk of thyroid, colorectal, brain, gastric, urinary, hematological, pancreatic, small intestine, and connective tissue cancer (18). From an epidemiological perspective, conflicting data could be explained by study limitations such as the low number of patients, surveillance bias, the lack of adjustment of confounding variables, the heterogeneity of control groups (general population/other pituitary adenomas), and inaccuracies in comparison older and more recent studies due to time-depended changes in life expectancy, modifications in cancer.
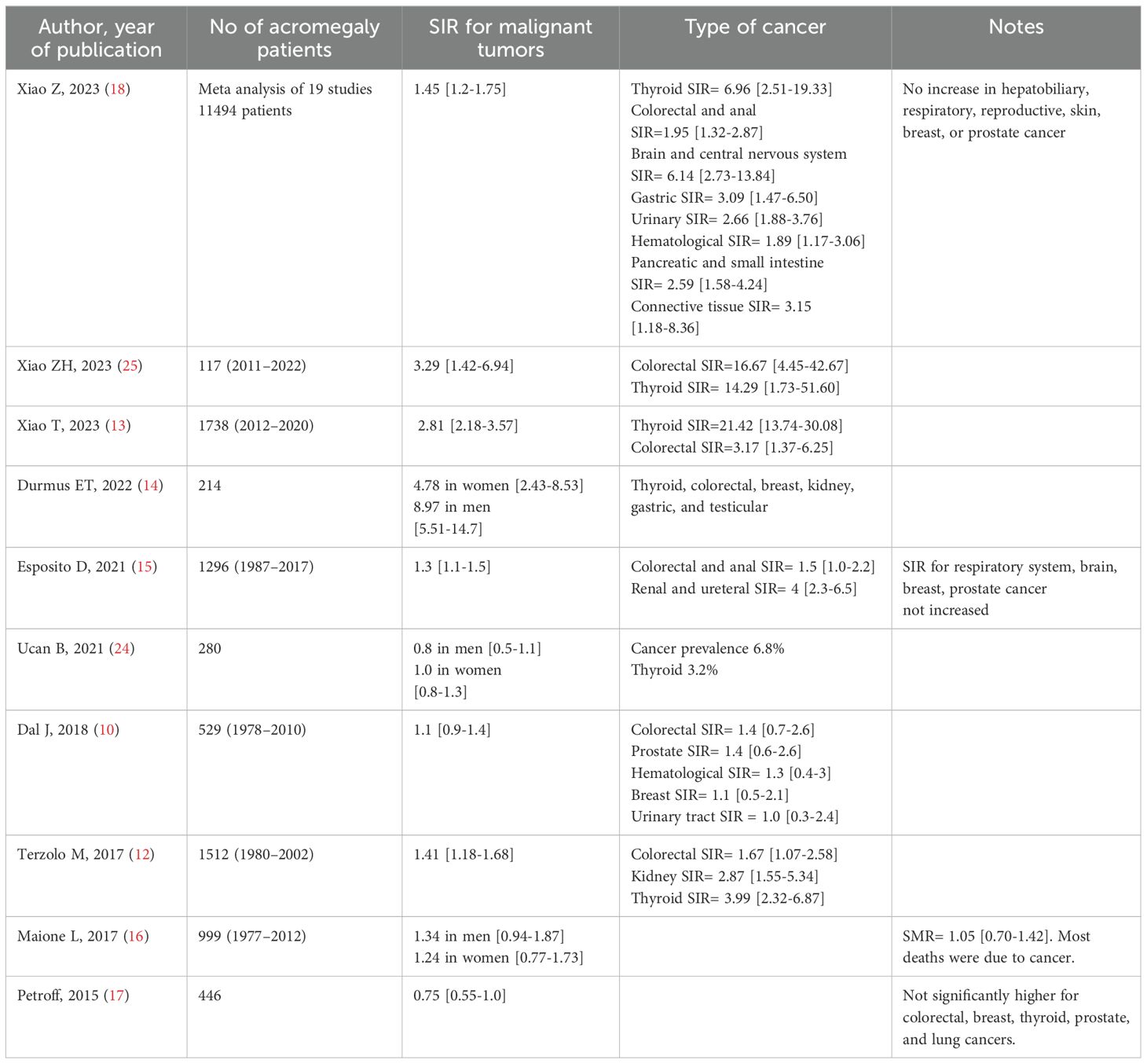
Table 1. Incidence of cancer in acromegaly patients in selected studies published in the last 10 years.
The current Frontiers in Endocrinology Research Topic presents real-life data from several large cohorts of acromegaly patients. Advances in acromegaly treatment have led to a greater potential to achieve disease control by decreasing the GH and IGF-I burden and improving follow-up care which may reduce cancer risk (19). Furthermore, the overall increased awareness of acromegaly, with decreasing diagnostic delay, and increasing incidence rate of patients with a milder phenotype of acromegaly, possibly also affect the cancer risk (20–22).
Data from the Danish nationwide AcroDEN cohort (739 patients treated since 1990) demonstrate improved diagnostics, with a continual increase in the likelihood of being diagnosed and treated for conditions such as diabetes, heart disease, sleep apnea, joint disease, and osteoporosis (Rosendal et al.). Also, an increased proportion of patients achieving hormonal disease control was reported (69% to 88%). The risk of being diagnosed with cancer did in contrast not significantly change, with an overall cancer risk of 1.1 (10) and a mortality rate of 1.3, mainly attributed to cardiovascular mortality (9, 10).
Rolla et al. assessed acromegaly’s complications at a referral center in Poland. In a series of 179 patients (1976–2018), 40% were cured by surgery, and 31% were pharmacologically controlled. During 496 hospitalizations, 43 colonoscopies were performed, and 21 colonic polyps were discovered (11.7% of cases). Despite the frequent use of thyroid ultrasound (198/496 hospitalizations) and a high proportion of goiter (52%), only two cases of thyroid cancer were diagnosed (24). A similar low risk of thyroid cancer in acromegaly was reported from the AcroDEN cohort (10).
The effect of modern treatment was further reported by Galoiu S et al. from a referral center in Romania, including 399 acromegaly (2001–2022). The surgical cure rate was 31% and the pharmacologically controlled was 22%. The standardized mortality rate (SMR) was 1.18, and decreased (from SMR=1.25) to a level comparable to the reference population (SMR=1.09) in patients diagnosed after 2008. Males had a lower mortality ratio (SMR=0.99), compared to females with acromegaly (SMR=1.63) (Găloiu et al.). Several studies have reported a similar trend, with decreasing mortality and a shift in the causes of death resembling those of the reference population (21). In the AcroDEN cohort, the mortality was slightly increased (SIR=1.3), whereas cancer-specific mortality was not (10).
The incidence of benign tumors is increased in acromegaly (SIR=2.4) (15). Guo et al. conducted a systematic review of 24 studies on the prevalence of meningiomas in patients with acromegaly or those exposed to exogenous GH therapy. Meningiomas occurred either synchronous or metachronous with acromegaly; no significant correlation was found between GH/IGF-1 levels and meningioma size; some patients with acromegaly and meningiomas were treated with radiotherapy, which is known to increase the risk of developing a second brain tumor (23) In four cases of acromegaly with meningiomas, without previous radiotherapy, there was a family history of pituitary adenomas and cancers. The authors suggest that hereditary cancer syndromes might play a role in the co-occurrence of acromegaly and meningiomas (Guo et al.). Whereas skin cancer risk is not increased in acromegaly (18), skin lesions were more frequently observed in acromegaly compared to patients with non-functioning pituitary adenomas. There was an improvement of these skin lesions three months after surgery in younger patients and patients who presented with the highest GH levels (Guo et al.).
In summary, acromegaly is associated with an increased risk of certain types of cancers, although the specific evidence remains controversial. Early diagnosis and advances in the treatment of acromegaly improved disease control and decreased mortality rates. Current data do not justify extensive cancer screening beyond standard guidelines, although clinical attention is crucial, especially in elderly patients (13, 24), in patients with a longer disease duration (14, 25), and in acromegaly patients with diabetes mellitus (25) Large studies with long follow-up are needed to further understand the impact of GH excess on cancer risk and to refine screening protocols.
Author contributions
RAT: Writing – original draft, Writing – review & editing. JD: Writing – original draft, Writing – review & editing.
Conflict of interest
JD received an unrestricted research grant from Pfizer and Ipsen.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Slagboom TNA, van Bunderen CC, De Vries R, Bisschop PH, Drent ML. Prevalence of clinical signs, symptoms and comorbidities at diagnosis of acromegaly: a systematic review in accordance with PRISMA guidelines. Pituitary. (2023) 26:319–22. doi: 10.1007/s11102-023-01322-7
2. Gadelha MR, Kasuki L, Lim DST, Fleseriu M. Systemic complications of acromegaly and the impact of the current treatment landscape: An update. Endocrine Rev. (2019) 40:268–332. doi: 10.1210/er.2018-00115
3. Fleseriu M, Langlois F, Lim DST, Varlamov EV, Melmed S. Acromegaly: pathogenesis, diagnosis, and management. Lancet Diabetes Endocrinol. (2022) 10:804–26. doi: 10.1016/S2213-8587(22)00244-3
4. Giustina A, Biermasz N, Casanueva FF, Fleseriu M, Mortini P, Strasburger C, et al. Consensus on criteria for acromegaly diagnosis and remission. Pituitary. (2024) 27:7–22. doi: 10.1007/s11102-023-01360-1
5. Giustina A, Barkan A, Beckers A, Biermasz N, Biller BMK, Boguszewski C, et al. A consensus on the diagnosis and treatment of acromegaly comorbidities: An update. J Clin Endocrinol Metab. (2020) 105:dgz096. doi: 10.1210/clinem/dgz096
6. Lai NB, Garg D, Heaney AP, Bergsneider M, Leung AM. No benefit of dedicated thyroid nodule screening in patients with acromegaly. Endocrine Pract. (2020) 26:16–21. doi: 10.4158/EP-2019-0254
7. Pekic S, Stojanovic M, Popovic V. Pituitary tumors and the risk of other Malignancies: is the relationship coincidental or causal? Endocrine Oncol. (2022) 2:R1–13. doi: 10.1530/EO-21-0033
8. Lega IC, Lipscombe LL. Review: diabetes, obesity, and cancer-pathophysiology and clinical implications. Endocrine Rev. (2020) 41:bnz014. doi: 10.1210/endrev/bnz014
9. Dal J, Feldt-Rasmussen U, Andersen M, Kristensen LØ, Laurberg P, Pedersen L, et al. Acromegaly incidence, prevalence, complications and long-term prognosis: a nationwide cohort study. Eur J Endocrinol. (2016) 175:181–90. doi: 10.1530/EJE-16-0117
10. Dal J, Leisner MZ, Hermansen K, Farkas DK, Bengtsen M, Kistorp C, et al. Cancer incidence in patients with acromegaly: A cohort study and meta-analysis of the literature. J Clin Endocrinol Metab. (2018) 103:2182–8. doi: 10.1210/jc.2017-02457
11. Wolinski K, Stangierski A, Dyrda K, Nowicka K, Pelka M, Iqbal A, et al. Risk of Malignant neoplasms in acromegaly: a case–control study. J Endocrinol Invest. (2017) 40:319–22. doi: 10.1007/s40618-016-0565-y
12. Terzolo M, Reimondo G, Berchialla P, Ferrante E, Malchiodi E, De Marinis L, et al. Acromegaly is associated with increased cancer risk: A survey in Italy. Endocrine-Related Cancer. (2017) 24:495–504. doi: 10.1530/ERC-16-0553
13. Xiao T, Jiao R, Yang S, Wang Y, Bai X, Zhou J, et al. Incidence and risk factors of cancers in acromegaly: a Chinese single-center retrospective study. Endocrine. (2023) 82:368–78. doi: 10.1007/s12020-023-03447-y
14. Durmuş ET, Atmaca A, Çolak R, Durmuş B. Cancer prevalence and cancer screening in patients with acromegaly: a single center experience. Endocrine. (2022) 77:363–71. doi: 10.1007/s12020-022-03082-z
15. Esposito D, Ragnarsson O, Johannsson G, Olsson DS. Incidence of benign and Malignant tumors in patients with acromegaly is increased: A nationwide population-based study. J Clin Endocrinol Metab. (2021) 106:3487–96. doi: 10.1210/clinem/dgab560
16. Maione L, Brue T, Beckers A, Delemer B, Petrossians P, Borson-Chazot F, et al. Changes in the management and comorbidities of acromegaly over three decades: The French acromegaly registry. Eur J Endocrinol. (2017) 176:645–55. doi: 10.1530/EJE-16-1064
17. Petroff D, Tönjes A, Grussendorf M, Droste M, Dimopoulou C, Stalla G, et al. The incidence of cancer among acromegaly patients: Results from the German acromegaly registry. J Clin Endocrinol Metab. (2015) 100:3894–902. doi: 10.1210/jc.2015-2372
18. Xiao Z, Xiao P, Wang Y, Fang C, Li Y. Risk of cancer in acromegaly patients: An updated meta-analysis and systematic review. PloS One. (2023) 18:e0285335. doi: 10.1371/journal.pone.0285335
19. Arlien-Søborg MC, Dal J, Heck A, Stochholm K, Husted E, Feltoft CL, et al. Acromegaly management in the Nordic countries: A Delphi consensus survey. Clin Endocrinol (Oxf). (2024) 101:263–73. doi: 10.1111/cen.15095
20. Aagaard C, Christophersen AS, Finnerup S, Rosendal C, Gulisano HA, Ettrup KS, et al. The prevalence of acromegaly is higher than previously reported: Changes over a three-decade period. Clin Endocrinol (Oxf). (2022) 97:773–82. doi: 10.1111/cen.14828
21. Rosendal C, Arlien-Søborg MC, Nielsen EH, Andersen MS, Feltoft CL, Kistorp C, et al. The changing landscape of acromegaly – an epidemiological perspective. Rev Endocr Metab Disord. (2024) 25:691–705. doi: 10.1007/s11154-024-09875-z
22. Petrossians P, Daly AF, Natchev E, Maione L, Blijdorp K, Sahnoun-Fathallah M, et al. Acromegaly at diagnosis in 3173 patients from the Liège Acromegaly Survey (LAS) Database. Endocr Relat Cancer. (2017) 24:505–18. doi: 10.1530/ERC-17-0253
23. Hamblin R, Vardon A, Akpalu J, Tampourlou M, Spiliotis I, Sbardella E, et al. Risk of second brain tumour after radiotherapy for pituitary adenoma or craniopharyngioma: a retrospective, multicentre, cohort study of 3679 patients with long-term imaging surveillance. Lancet Diabetes Endocrinol. (2022) 10:581–8. doi: 10.1016/S2213-8587(22)00160-7
24. Ucan B, Kizilgul M, Karci AC, Duger H, Erkam Sencar M, Imga NN, et al. The prevalence of cancer and its relation to disease activity in patients with acromegaly: two centers’ Experience. Endocrine Pract. (2021) 27:51–5. doi: 10.4158/EP-2020-0398
Keywords: acromegaly, cancer, incidence, prevalence, screening, thyroid, colorectal
Citation: Trifănescu RA and Dal J (2024) Editorial: Cancer risk in patients with acromegaly – is extensive screening needed? Front. Endocrinol. 15:1503633. doi: 10.3389/fendo.2024.1503633
Received: 29 September 2024; Accepted: 11 October 2024;
Published: 28 October 2024.
Edited and Reviewed by:
Claire Perks, University of Bristol, United KingdomCopyright © 2024 Trifănescu and Dal. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Raluca Alexandra Trifănescu, cmFsdWNhLnRyaWZhbmVzY3VAdW1mY2Qucm8=; Jakob Dal, amFrb2IuZGFsQHJuLmRr
†ORCID: Jakob Dal, orcid.org/0000-0002-0610-7867
 Raluca Alexandra Trifănescu
Raluca Alexandra Trifănescu Jakob Dal
Jakob Dal