- 1Department of Obstetrics and Gynecology, West China Second University Hospital of Sichuan University, Chengdu, Sichuan, China
- 2Key Laboratory of Birth Defects and Related Diseases of Women and Children, Ministry of Education, Sichuan University, Chengdu, Sichuan, China
- 3West China School of Medicine, Sichuan University, Chengdu, Sichuan, China
Purpose: To investigate the association of sleep quality during pregnancy on in vitro fertilization/intra-cytoplasmic sperm injection (IVF/ICSI) and natural conceiving (NC), as well as anxiety, depression, and perceived stress.
Methods: This prospective cohort study includes 500 infertile pregnant women undergoing IVF/ICSI and 678 NC women in a Sichuan birth cohort. Data on sleep, anxiety, depression, and stress was collected in the first trimester (T1), second trimester (T2), and third trimester (T3) using integrated questionnaires. Sleep quality is quantified by the Pittsburgh Sleep Quality Index (PSQI) with a cut-point of 5 indicating poor sleep. The Self-rating Anxiety Scale (SAS), the Center for Epidemiologic Study of Depression scale (CES-D), and the Perceived Stress scale (PSS) were used for assessing anxiety, depression, and perceived stress symptoms. Additionally, the matched husbands are surveyed. Multivariable logistic regression models with adjustments for influencing factors were used to estimate odds ratios (ORs) and 95% confidence intervals (CIs) for the associations of sleep quality.
Results: In the IVF/ICSI group, 61.1%, 55.5%, and 66.5% of participants in T1, T2, and T3 reported poorer sleep quality compared to the NC group, which had 43.2%, 37.4%, and 46.4% throughout the same trimesters. Additionally, the IVF/ICSI group exhibited higher levels of negative psychological factors as measured by the CES-D and PSS during T1 and T2, showing statistical significance in T1 (P = 0.008, P < 0.001) and T2 (P = 0.038, P < 0.001), except at T3 (P = 0.107, P = 0.253). In addition to psychological factors and IVF/ICSI treatment, poor sleep quality was also associated with advanced age. However, there was no significant difference in sleep quality between the husbands of the IVF/ICSI and NC groups.
Conclusion: The study reveals that women receiving IVF/ICSI treatment are at a higher risk of experiencing sleep disturbances throughout their pregnancy compared with women with natural conception. While partners typically do not report major sleep problems, they do exhibit increased anxiety levels. These findings underscore the necessity for screening and addressing sleep issues in women pregnant through assisted IVF/ICSI treatment, to promote their well-being during this critical period.
Introduction
Sleep is a vital physiological process essential for maintaining both physical and mental health, with individuals spending approximately one-third of their lifespan asleep. During pregnancy, ensuring adequate and restorative sleep is crucial not only for the mother’s well-being but also for the optimal development of the fetus. The National Sleep Foundation recommends that adults should aim for a sleep duration of seven to nine hours per night (1). A comprehensive review by Maniaci et al. highlights that conditions, like obstructive sleep apnea during pregnancy can affect maternal and fetal health, emphasizing the broader implications of sleep disturbances for pregnant women (2). These issues could negatively impact both maternal and fetal outcomes, potentially leading to complications such as preeclampsia, hypertension, gestational diabetes, cesarean deliveries, and excessive weight gain during pregnancy. However, specific guidelines for sleep duration, quality, and insomnia during pregnancy remained insufficient. Furthermore, sleep quality and disturbances are often linked to significant determinants of women’s health, particularly during critical life stages such as menstruation, pregnancy, and menopause. For instance, sleep disturbances are often associated with higher levels of depression and stress, as well as an increased risk of cardiovascular disease, hypertension, and diabetes (3). Furthermore, poor sleep quality and the prevalence of depression tend to be escalated throughout pregnancy (4). These issues could adversely affect both maternal and fetal outcomes, potentially leading to complications, including preeclampsia, hypertension, gestational diabetes, cesarean deliveries, and excessive weight gain during pregnancy (3, 5–7).
Animal studies have demonstrated that persistently disrupted light/dark cycles could significantly impair the preovulatory LH surge, leading to reduced fertility. In contrast, the reproductive effects of a single-phase shift on female mice could be minimized (8). Furthermore, sleep deprivation had been shown to diminish oocyte output, as transient activation of wake-promoting dopaminergic neurons negatively impacts reproductive performance (9). Sleep disorders were notably prevalent undergoing assisted reproductive technology (ART) treatments, and affected 57% of women undergoing in vitro fertilization/intra-cytoplasmic sperm injection(IVF/ICSI) before treatment, 43% during the stimulation phase, and 29% following embryo transfer (10). Philipsen et al. found that mean PSQI global scores before treatment were 8.1, with 91% of participants having PSQI scores > 5, indicating poor sleep quality (11). Research indicated that insufficient nocturnal sleep—specifically, less than seven hours per night with disrupted sleep patterns, is associated with reduced oocyte and embryo production. Conversely, excessively prolonged nocturnal sleep might decrease the likelihood of achieving a successful pregnancy. Additionally, the relationship between nocturnal sleep duration and ART outcomes is influenced by factors such as subjective sleep quality and maternal age (12).
Strong correlations have been established between sleep quality and both physical and mental well-being (13). The interplay between negative emotions and sleep difficulties can create a harmful cycle. Given that the high prevalence of sleep disorders among expectant mothers and their significant association with psychological symptoms, it is crucial to prioritize screening and counseling for psychological disorders in pregnant women to enhance sleep quality (4). Previous research also indicated that there are small but significant associations between stress and distress, which can further diminish the likelihood of successful pregnancies through ART (14). Moreover, the rates of anxiety and depression fluctuate depending on the stage of IVF/ICSI treatment. While many studies had examined women’s psychological health before and after IVF (15–17), few had focused on sleep quality and the psychological factors influencing sleep among IVF/ICSI patients during pregnancy. As a result, the relationship between sleep during pregnancy and positive psychological aspects remained poorly understood.
The existing body of research has largely focused on assessing sleep quality in individuals undergoing ART treatments. However, there is a notable gap in studies that investigate the impact of sleep quality among IVF/ICSI patients during pregnancy, particularly in comparison to women, who conceive naturally. In this study, we aim to gather data on sleep characteristics among women undergoing IVF/ICSI and those achieving natural conception. We hypothesize that both negative and positive psychological factors play a significant role in influencing sleep quality.
Materials and methods
Participants and study design
In this prospective cohort study, we recruited a convenience sample of 557 females who underwent ART treatment and 691 females who were natural conception and delivered at West China Second University Hospital of Sichuan University between January 2016 and July 2018. All couples included in the study were not involved in any type of prospective interventional trials. All protocols were approved by the Medical Science Ethics Board of West China Second University Hospital of Sichuan University.
Data collection
First, each participant completed a questionnaire on demographic information and at least once of questionnaire. In this prospectively longitudinal study, data was collected in the first trimester (T1, before 12 weeks of gestation), second trimester (T2, between 13-28 weeks of gestation), and third trimester (T3, after 28 weeks of gestation) using integrated questionnaires. All the subjects were fully informed of the procedures, and their written informed consent and approval were obtained. Husbands for the matched couple were questioned once during pregnancy.
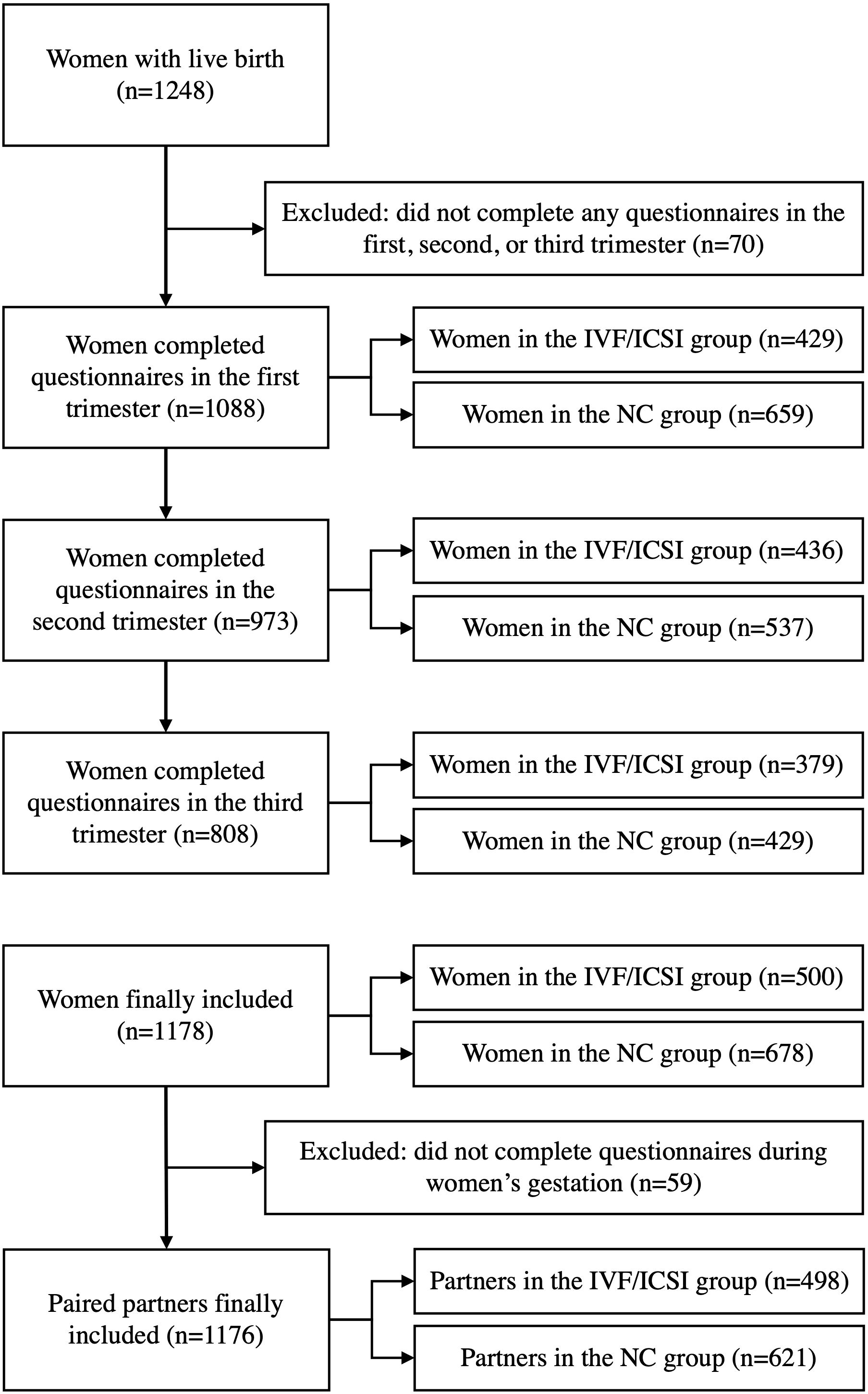
Due to incomplete questionnaire data, 57 participants from the Assisted Reproductive Technology (ART) group and 13 from the naturally conceived (NC) group were excluded from the study as they did not respond to any questionnaires. As a result, the final analysis included 500 individuals from the IVF/ICSI group and 678 from the NC group. Simultaneously, the study encompassed 498 partners of women who conceived through IVF/ICSI and 621 partners of women who conceived naturally. A detailed inclusion and exclusion flow chart was shown in Figure 1.
Pittsburgh sleep quality index
Sleep quality during pregnancy was assessed by the Pittsburgh Sleep Quality Index (PSQI), a self-reported 19-item questionnaire (18, 19). The PSQI global score, which consists of seven component scores: subjective sleep quality, subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction, was used to evaluate sleep quality. Each component score was assigned a value of 0-3 points. The PSQI global score varied from 0 to 21, with higher scores suggesting worse sleep quality. In this study, sleep quality was classified into good (score ≤ 5) and poor (score> 5) according to the global PSQI scores (19). Among the poor quality, women with scores from 6 to 10 were considered fairly good, from 11 to 15 as fairly bad, and above 15 as bad sleep.
Self-rating anxiety scale
Anxiety was measured with the Zung’s Self-Rating Anxiety Scale (SAS) (20). The scale includes 20 items that cover 4 groups of manifestations: cognitive, autonomic, motor, and central nervous system symptoms. Each item is scored on a Likert-type scale of 1-4 (1 = none or a little of the time, 2 = some of the time, 3= good part of the time, 4 = most or all of the time). Anxiety standard scores ≥ 50 were considered to be at risk for clinical anxiety. Among the anxiety group, women with scores from 50 to 60 were considered as mild anxiety, from 60 to 70 as middle anxiety, and above 70 as severe anxiety (21).
Center for epidemiologic study of depression scale
Depression was assessed using the Center for Epidemiologic Study of Depression Scale (CES-D). The CES-D consists of 20 items which are rated using a 4-point ordered response set to indicate how frequently symptoms were experienced during the previous week (0 = rarely or none of the time, 1= some or a little of the time, 2 = occasionally or a moderate amount of the time, 3 = most or all of the time). Total score of CES-D was generated by summing their item responses and ranging from 0 to 60 (higher scores indicating more depressive symptoms). Participants with CES-D scores ≥16 were considered at risk for clinical depression (22).
Perceived stress scale
Perceived stress was assessed with the Perceived Stress Scale (PSS-10) (23), which consists of 10 items purported to measure the degree of nonspecific appraised stress in the past month on a 5-point Likert scale (0 = never, 1 = almost never, 2= sometimes, 3 = fairly often, 4 = very often). The total PSS score ranged from 0 to 40, The stress level increases depending on the increase in score.
Statistical analysis
SPSS 25.0 (IBM, Armonk, NY, USA) was used to analyze the study data. Baseline characteristics were summarized as mean (standard deviation, SD) for continuous variables, and frequencies (percentages) for categorical variables. Differences in these characteristics between the three nighttime sleep duration groups were compared by analysis of variance (for continuous variables) and Chi-square tests (for categorical variables). Nominal variables were tested either with the Chi-square test or Fisher’s exact test. Odds ratios (ORs) and their 95% confidence intervals (CIs) were estimated through multivariable logistic regression models to evaluate the influencing factors of the sleep quality of participants. The P-value of < 0.05 was considered statistically significant.
Results
Baseline characteristics and obstetric characteristics
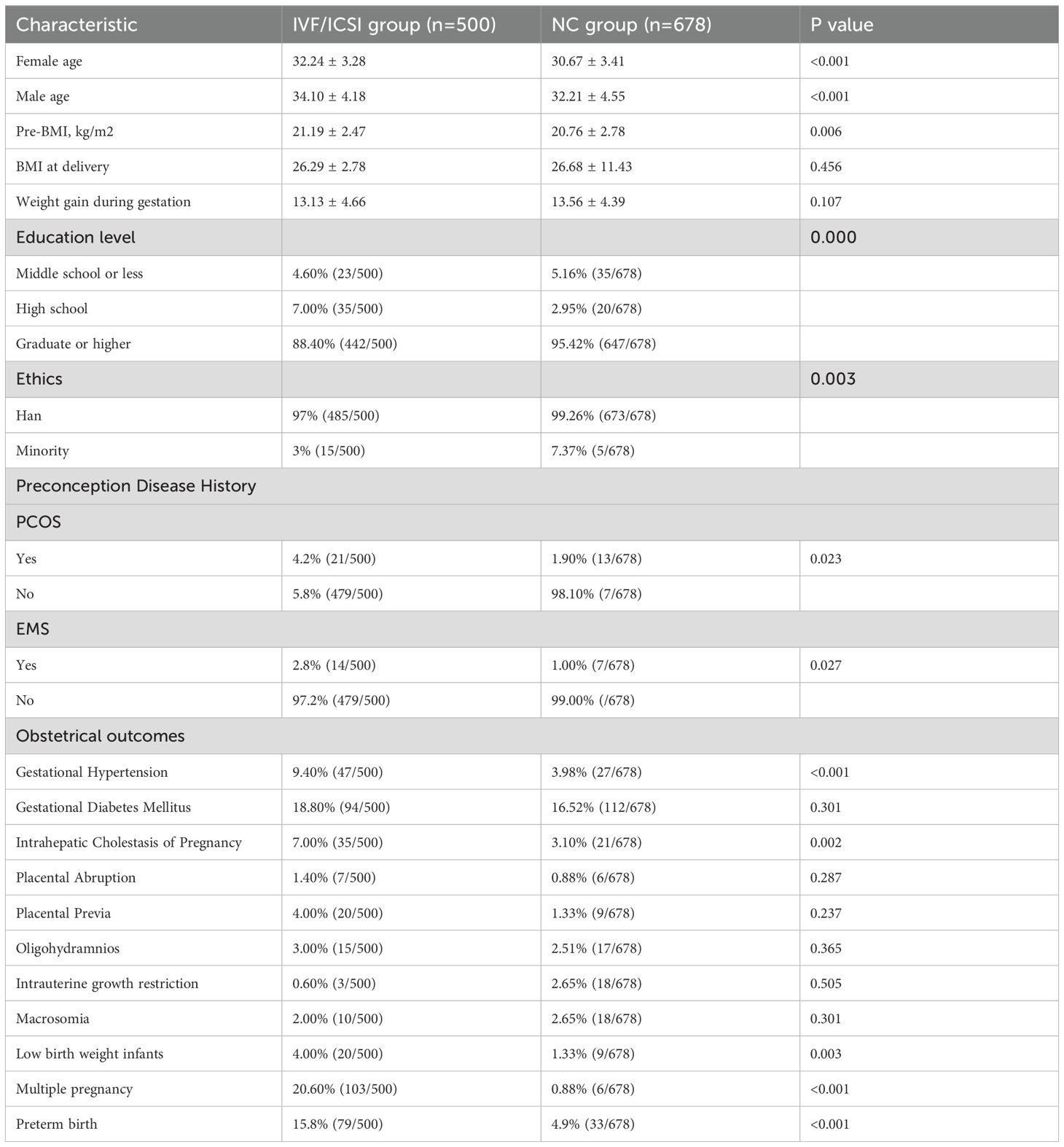
A total of 1,178 cases of women were included in the final analysis of this study, with 500 participants in the IVF/ICSI group, with 429, 436, and 379 women in T1, T2 and T3 of pregnancy. The average( ± SD) age and pre-BMI were 32.24 ± 3.28 and 21.19 ± 2.47. Most participants were of Han ethnicity (97%). In the NC group, 678 women were included, with 659, 537, and 429 women in T1, T2 and T3 of pregnancy. The average( ± SD) age and pre-BMI were 30.67 ± 3.41 and 20.76 ± 2.78. Most participants were of Han ethnicity (99.26%). The basic characteristics of the patients are presented in Table 1. The rate of twin pregnancies varied significantly between the groups, with 20.6% of the IVF/ICSI-treated women and 0.88% of the NC women having twins. Furthermore, we observed that the incidence of preterm birth was 15.8% in the IVF/ICSI group compared to 4.9% in the naturally conceiving group. Meanwhile, the prevalence of intrahepatic cholestasis of pregnancy, gestational hypertension, and hypothyroidism was notably higher among women undergoing IVF/ICSI compared to those in the NC group. Additionally, the occurrence of low-birth-weight infants was significantly higher among the IVF/ICSI group than in those conceived naturally (Table 1).
Sleep quality, anxiety, depression, and perceived stress in different trimesters in pregnant women
In T1, 429 women from the IVF/ICSI group, and 659 women from the NC group completed the questionnaire. The median global PSQI scores were 7 for the IVF/ICSI group and 5 for the NC group (P< 0.001). During T2, 436 women in the IVF/ICSI group participated in the survey, with537 women in the NC group. The median PSQI scores for this trimester were 6 points for the IVF/ICSI group and 5 points for the NC group (p < 0.001). In T3, 379 women from the IVF/ICSI group answered the questionnaire, compared to 429 women from the NC group. The PSQI scores were presented as a median of 7 points in the IVF/ICSI group and 5 points in the NC group (p < 0.001). Overall, when compared to the NC group during pregnancy, women undergoing ART exhibited significantly poorer sleep quality.
Pregnant women undergoing IVF/ICSI showed similar median scores on SAS throughout their pregnancy compared to those who conceived naturally (Table 2). Specifically, the scores were 39.79 for the IVF/ICSI group versus 39.91 for the NC group in T1 (P = 0.827), 38.52 versus 38.77 points in T2 (P = 0.874), and 40.01 versus 40.07 points in T3 (P = 0.689).

Table 2. Sleep quality, anxiety, depression, and stress in different trimesters between the IVF/ICSI and NC group.
In contrast, the median scores for CES-D and PSS in the IVF/ICSI group were significantly lower than those in the NC group during T1 and T2. Specifically, the CES-D scores were 13.74 for the IVF/ICSI group compared to 15.11 for the NC group in T1 (P = 0.008) and 11.88 versus 13.1 in T2 (P = 0.038). For the PSS, the scores were 12.28 for the IVF/ICSI group versus 14.02 in T1 (P < 0.0001) and 11.51 compared to 12.56 in T2 (P < 0.001). However, in T3, the median scores of CES-D and PSS for both groups were similar across groups: CES-D was 12.63 versus 13.77 (P = 0.107) and PSS was 11.93 versus 12.29 (P = 0.253) (Table 2).
The relationship between sleep quality and trimesters
In the IVF/ICSI group, 38.90% (167 out of 429) of women reported experiencing good sleep quality during T1, which declined to 33.5% (127 out of 379) in T3. Both of these figures were lower than the 44.5% (194 out of 436) who reported good sleep quality in T2. Similarly, in the NC group, the second trimester also showed the highest proportion of reported good sleep quality. Throughout their pregnancies, only a small number of women in the NC group reported poor sleep quality. In contrast, 17.7% (67 out of 379) of women in the IVF/ICSI group reported poor sleep quality in the third trimester, a significant increase from the 9.1% (39 out of 429) reported in T1 and 8.5% (37 out of 436) in T2. Overall, the second trimester was associated with the highest T1quality of sleep for both groups throughout the entire pregnancy (Figure 2).
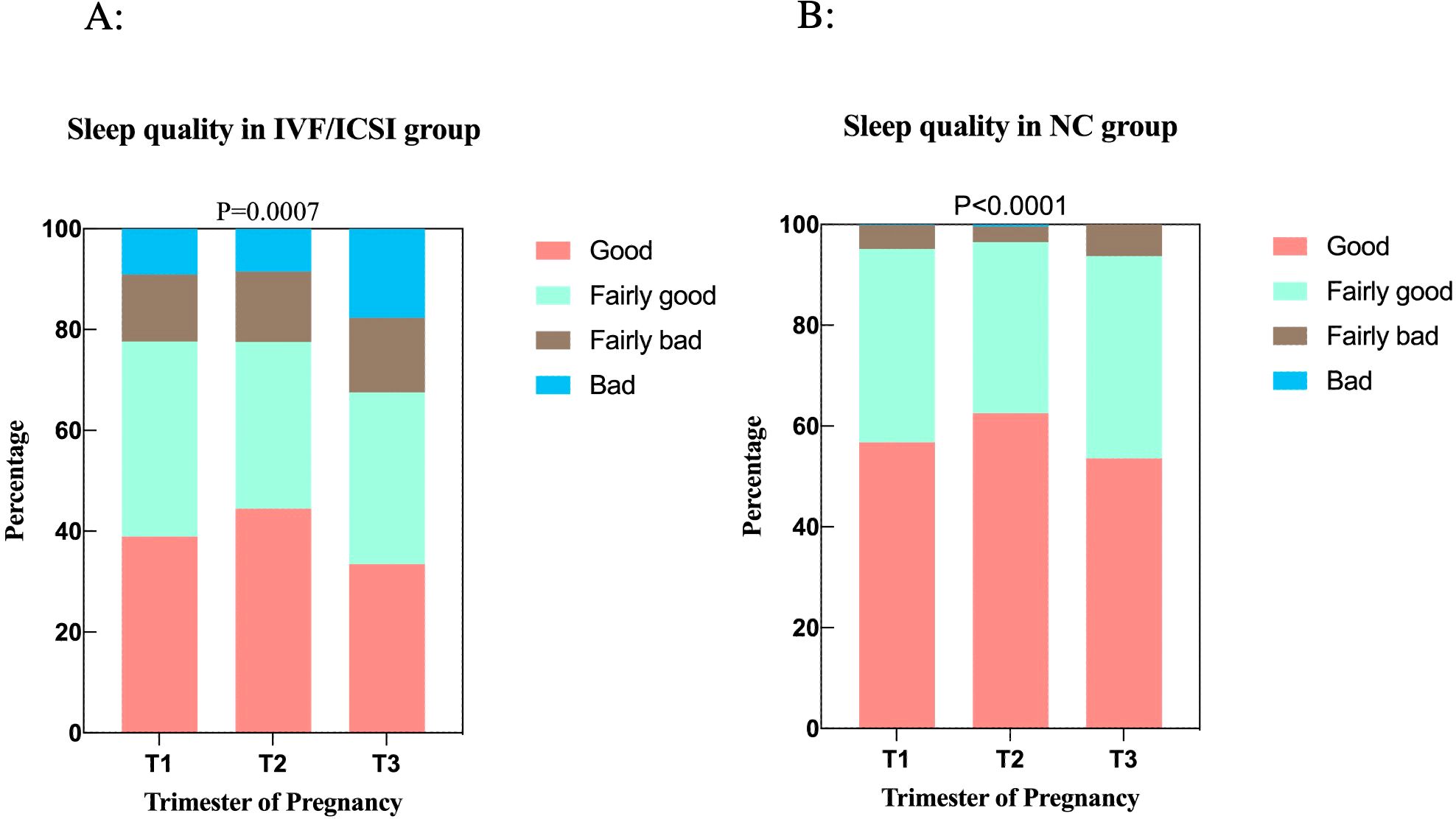
Figure 2. The relationship between sleep quality and trimesters. (A) Sleep quality in the IVF/ICSI group among three trimesters. (B) Sleep quality in the NC group among three trimesters.
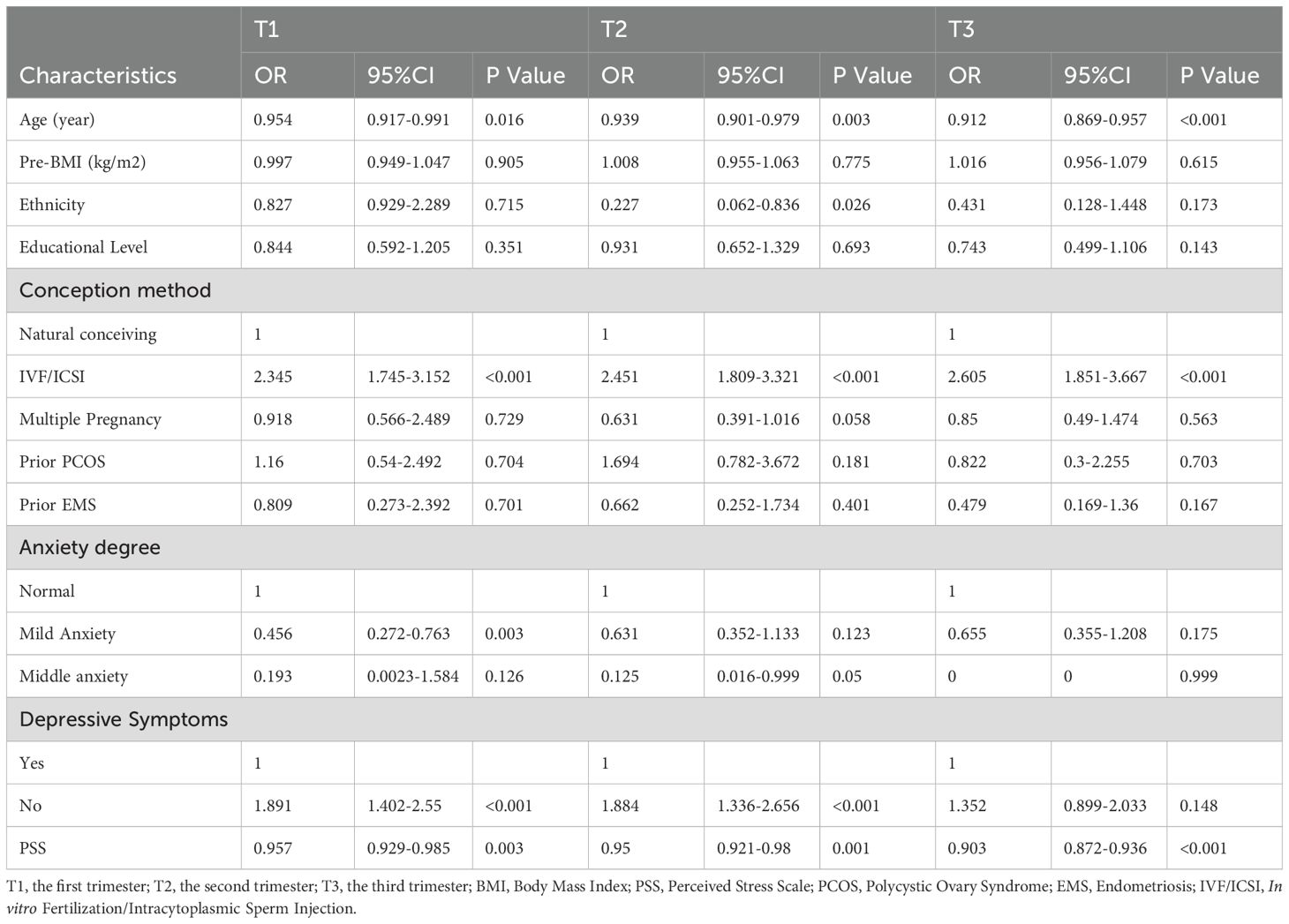
We further studied the relationship between demographics and fertility characteristics, psychological characteristics, and sleep quality. A logistic stepwise regression model was constructed for sleep quality based on female age, pre-BMI, ethnicity, educational level, conception methods (IVF/ICSI or NC group), number of pregnancies, prior diseases (polycystic ovary syndrome and endometriosis), anxiety degree, depressive symptoms, and PPS. We found that female age, conception methods, anxiety degree, depressive symptoms, and PPS affect the sleep quality of pregnant women during the whole gestation (Table 3).
Sleep quality, anxiety, depression, and perceived stress in paired partners
In the study, 498 matched partners from the IVF/ICSI group and 621 partners from the NC group were included. The male partners in the IVF/ICSI group exhibited slightly higher SAS scores compared to those in the NC group (P<0.001), indicating a potential increase in anxiety levels. However, there was no significant differences in sleep quality, depression levels, or stress perception of the male partners in the IVF/ICSI and NC groups (Table 4).
Discussion
In this prospective cohort study, our findings reveal that women in the IVF/ICSI group consistently report significantly poorer sleep quality throughout all three trimesters compared to naturally conceiving women. To our knowledge, this study is the first to provide a comprehensive assessment of sleep quality, anxiety, depression, and perceived stress across different stages of pregnancy in both IVF/ICSI and naturally conceiving individuals. In the stratified analysis, we discovered that the association of sleep quality during the gestation during gestation was specifically influenced by maternal age, conception methods, anxiety status, depressive symptoms, and perceived stress. To the best of our knowledge, this is the first prospective study to evaluate sleep quality differences between the IVF/ICSI and NC groups during pregnancy.
The study revealed that a troubling trend in sleep quality among women undergoing IVF/ICSI during pregnancy. Only 38.93% reported good sleep quality in T1, decreasing to 33.51% in T3, though there was a slight improvement to 44.5% in T2. These findings are significant, as they aligned with previous research showing that pregnancy often leads to sleep disturbances, especially for those with infertility histories. Multivariate logistic regression analysis showed that age, conception methods, depression, anxiety, and perceived stress significantly impacted sleep quality. Although age was found to be significantly associated with reduced sleep quality, the group of women receiving IVF/ICSI treatment is significantly older than the natural conception group, which obviously impacts the finding of the difference between the two groups. Previous studies also have shown that sleep quality in pregnant women declines with increasing age (24). Furthermore, a meta-analysis of quantitative sleep parameters has demonstrated that sleep quality naturally diminishes as individuals age (25). Pregnant women aged 30 and older are more likely to experience stress and depressive symptoms during pregnancy, which may also elevate the risk of postpartum depression in this age group (26).
Sleep disorders are prevalent during pregnancy. Previous studies demonstrated that pregnant women experience variable levels of sleep quality deficits across all trimesters (24). PSQI scores exhibited an upward trend as pregnancy progressed, with the sleep quality of pregnant women being particularly susceptible to disruptions in the late stages of pregnancy (4). Contributing factors include emotional stress from the IVF process, physical discomfort as pregnancy progresses, and hormonal changes affecting sleep (27). Notably, the observed sleep decline in the NC group suggests that sleep issues during pregnancy are influenced by physiological and psychological demands rather than just conception methods. This study is consistent with previous findings, which suggest that around 46% of pregnant people experience sleep difficulties, with a notable drop in sleep quality occurring during the third trimester (28). This highlights the need for further investigation into sleep patterns among pregnant women, taking into account their medical histories and current health. During pregnancy, the significance of sleep for maintaining physical health was highlighted linking compromised sleep quality to negative pregnancy outcomes. The decline in sleep quality may impact maternal and fetal health, increasing risks of gestational complications, postpartum depression, and impaired maternal-fetal attachment. Studies have identified associations between sleep-disordered breathing and conditions such as gestational diabetes and hypertension (3, 29, 30). Additionally, insomnia and obstructive sleep apnea have been correlated with the increased risk of preterm birth (29).
Anxiety, depression, and stress associated with infertility treatment are essential issues. Our results reveal that while both groups exhibited similar median anxiety scores as measured by the SAS, pregnant women in the IVF/ICSI group reported significantly lower median scores on both the CES-D and PSS during T1 and T2. The retained comparability of anxiety scores across both groups throughout the pregnancy, with no statistically significant differences, suggested that the process of conception-whether through IVF/ICSI or natural means- does not lead to significant differing levels of anxiety in pregnant women. This could imply that the act of pregnancy itself, along with the accompanying physiological and emotional changes, may predispose all pregnant individuals to experience a standard level of anxiety regardless of their conception method. Significant differences in CES-D and PSS scores during the first two trimesters indicate that the IVF/ICSI group experiences lower depressive symptoms and perceived stress early in pregnancy. This may stem from a sense of accomplishment and relief from overcoming infertility. However, in the third trimester, CES-D and PSS scores equalize between groups, likely due to increased discomfortness and anxiety about childbirth affecting all pregnant women. This aligned with literature indicating that the third trimester often brings heightened physical discomfort and concerns about maternal health, impacting mental health. These findings underscored the need for individualized care approaches, suggesting that early emotional support and psychological interventions for the IVF/ICSI group could enhance their positive mental state. A study involving 842 patients undergoing IVF treatment showed that 39.4% of patients felt anxious, and 28.5% had depressive symptoms (31). Even though it is not entirely clear to what extent mental disorders affect fertility and to what extent infertility affects mental health (32), targeted interventions addressing psychological factors are crucial as pregnancies progress and challenges intensify.
The analysis of partners of pregnant women in the IVF/ICSI and NC groups revealed important insights into the emotional landscape surrounding ART and natural conception. With 498 partners from the IVF/ICSI group and 621 from the NC group, the study robustly compared mental health indicators, particularly anxiety levels measured by SAS scores. Partners in the IVF/ICSI group showed slightly higher anxiety scores, suggesting that the stress of infertility treatments affects their mental well-being. The emotional toll of IVF/ICSI, marked by uncertainty and financial strain, likely contributed to this heightened anxiety, aligning with literature on the psychological burden faced by couples undergoing fertility treatments. Interestingly, despite the increased anxiety, no significant differences in sleep quality, depression, or perceived stress were found between the two groups. This might suggest that while anxiety is a concern for IVF/ICSI partners, it does not lead to poorer sleep or higher depression levels compared to NC partners. The lack of sleep quality differences may reflect a broader trend where partners face similar sleep challenges during pregnancy, regardless of the conception method. These findings highlighted the need to consider partners’ mental health, especially for those undergoing IVF/ICSI. Future research should explore factors contributing to partner anxiety and potential interventions.
One limitation of this study is the absence of data on participants’ prior history of sleep, depression, and anxiety. This information could have provided a more comprehensive understanding of the psychological factors influencing sleep quality during pregnancy, particularly in women undergoing IVF/ICSI treatment. The lack of this data may limit our ability to fully assess the impact of pre-existing mental health conditions on the observed outcomes. Another notable limitation of this study is the reliance on self-reported questionnaires to assess sleep quality among participants. While these instruments provide valuable insights, they are subjective and may be influenced by various biases, including recall bias and social desirability bias. Previous research mainly focused on specific aspects of psychological distress without considering the interplay of multiple influencing factors. A more reliable insights into this association was highlighted. For sleep issues during pregnancy, there are pharmacological options, but there’s a lack of human data on their safety during pregnancy and lactation, raising concerns about potential birth defects and neonatal withdrawal (33). Future studies should utilize longitudinal designs to track mental health changes throughout pregnancy and identify key factors. This knowledge is vital for healthcare providers to establish support systems that help pregnant women maintain their psychological well-being during this critical period.
Conclusions
Achieving a pregnancy and establishing a family life holds significant value for individuals undergoing IVF/ICSI as it greatly influences their overall life happiness. Consequently, even slight increases in the likelihood of achieving a pregnancy may warrant the implementation of various measures aimed at achieving success. Our study indicates that a notable concern regarding sleep quality during pregnancy among women in both IVF/ICSI and NC groups, calling for immediate attention from health professionals to address this crucial aspect of maternal health. Moreover, our current understanding of the potential impact of sleep, perceived stress, and distress on the progression from early pregnancy stage to live births remains incomplete. While IVF/ICSI partners exhibit higher anxiety, the absence of significant differences in other mental health aspects underscores the importance of understanding psychological dynamics and addressing the mental health needs of both partners to foster a supportive pregnancy environment.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Medical Science Ethics Board of West China Second University Hospital of Sichuan University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
YX: Formal Analysis, Investigation, Writing – original draft, Data curation, Methodology, Conceptualization. RP: Data curation, Investigation, Writing – review & editing. LX: Investigation, Formal Analysis, Validation, Writing – review & editing. SL: Funding acquisition, Supervision, Writing – review & editing. XL: Funding acquisition, Methodology, Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by a grant from National Key R&D Program of China (No.2016YFC100206).
Acknowledgments
We would like to thank our colleagues at the Reproductive Medicine Center for their direct and indirect contributions to the project. We appreciate Dr. Tianji Liao for her assistance in the statistical analysis. We would like to acknowledge Dr. Jeannie Z.Y. Tan from Heriot-Watt University for language editing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Smiley A, King D, Bidulescu A. The association between sleep duration and metabolic syndrome: the NHANES 2013/2014. Nutrients. (2019) 11:2582. doi: 10.3390/nu11112582
2. Maniaci A, Via LL, Pecorino B, Chiofalo B, Scibilia G, Lavalle S, et al. Obstructive sleep Apnea in pregnancy: a comprehensive review of maternal and fetal implications. Neurol Int. (2024) 16:522. doi: 10.3390/neurolint16030039
3. Lai Y, Wang C, Ouyang J, Wu L, Wang Y, Wu P, et al. Association between nighttime sleep duration, midday napping, and sleep quality during early pregnancy and risk of gestational diabetes mellitus: a prospective cohort study in China. Sleep Med. (2024) 119:164–71. doi: 10.1016/j.sleep.2024.04.003
4. Bahani M, Zhang Y, Guo Y, Haretebieke S, Wu D, Zhang L. Influencing factors of sleep quality in pregnant: a structural equation model approach. BMC Psychol. (2024) 12:171. doi: 10.1186/s40359-024-01657-1
5. O’Brien LM, Bullough AS, Owusu JT, Tremblay KA, Brincat CA, Chames MC, et al. Pregnancy-onset habitual snoring, gestational hypertension, and preeclampsia: prospective cohort study. Am J Obstet Gynecol. (2012) 207:487.e1–9. doi: 10.1016/j.ajog.2012.08.034
6. Pauley AM, Moore GA, Mama SK, Molenaar P, Symons Downs D. Associations between prenatal sleep and psychological health: a systematic review. J Clin Sleep Med JCSM Off Publ Am Acad Sleep Med. (2020) 16:619–30. doi: 10.5664/jcsm.8248
7. Gay CL, Richoux SE, Beebe KR, Lee KA. Sleep disruption and duration in late pregnancy is associated with excess gestational weight gain among overweight and obese women. Birth Berkeley Calif. (2017) 44:173–80. doi: 10.1111/birt.12277
8. Bahougne T, Kretz M, Angelopoulou E, Jeandidier N, Simonneaux V. Impact of circadian disruption on female mice reproductive function. Endocrinology. (2020) 161:bqaa028. doi: 10.1210/endocr/bqaa028
9. Potdar S, Daniel DK, Thomas FA, Lall S, Sheeba V. Sleep deprivation negatively impacts reproductive output in Drosophila melanogaster. J Exp Biol. (2018) 221:jeb174771. doi: 10.1242/jeb.174771
10. Goldstein CA, Lanham MS, Smith YR, O’Brien LM. Sleep in women undergoing in vitro fertilization: a pilot study. Sleep Med. (2017) 32:105–13. doi: 10.1016/j.sleep.2016.12.007
11. Philipsen MT, Knudsen UB, Zachariae R, Ingerslev HJ, Hvidt JEM, Frederiksen Y. Sleep, psychological distress, and clinical pregnancy outcome in women and their partners undergoing in vitro or intracytoplasmic sperm injection fertility treatment. Sleep Health. (2022) 8:242–8. doi: 10.1016/j.sleh.2021.10.011
12. Yao Q-Y, Yuan X-Q, Liu C, Du Y-Y, Yao Y-C, Wu L-J, et al. Associations of sleep characteristics with outcomes of IVF/ICSI treatment: a prospective cohort study. Hum Reprod. (2022) 37:1297–310. doi: 10.1093/humrep/deac040
13. Lund HG, Reider BD, Whiting AB, Prichard JR. Sleep patterns and predictors of disturbed sleep in a large population of college students. J Adolesc Health Off Publ Soc Adolesc Med. (2010) 46:124–32. doi: 10.1016/j.jadohealth.2009.06.016
14. Matthiesen SMS, Frederiksen Y, Ingerslev HJ, Zachariae R. Stress, distress and outcome of assisted reproductive technology (ART): a meta-analysis. Hum Reprod Oxf Engl. (2011) 26:2763–76. doi: 10.1093/humrep/der246
15. Kirca N, Ongen M. Perceived stress and sleep quality before oocyte pick-up, embryo transfer, and pregnancy test in women receiving in vitro fertilization treatment. Sleep Breath Schlaf Atm. (2021) 25:1977–85. doi: 10.1007/s11325-021-02328-w
16. Huang L-H, Kuo C-P, Lu Y-C, Lee M-S, Lee S-H. Association of emotional distress and quality of sleep among women receiving in-vitro fertilization treatment. Taiwan J Obstet Gynecol. (2019) 58:168–72. doi: 10.1016/j.tjog.2018.11.031
17. Liu Y-F, Fu Z, Chen S-W, He X-P, Fan L-Y. The analysis of anxiety and depression in different stages of in vitro fertilization-embryo transfer in couples in China. Neuropsychiatr Dis Treat. (2021) 17:649–57. doi: 10.2147/NDT.S287198
18. Mollayeva T, Thurairajah P, Burton K, Mollayeva S, Shapiro CM, Colantonio A. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: A systematic review and meta-analysis. Sleep Med Rev. (2016) 25:52–73. doi: 10.1016/j.smrv.2015.01.009
19. Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4
20. Zung WW. A rating instrument for anxiety disorders. Psychosomatics. (1971) 12:371–9. doi: 10.1016/S0033-3182(71)71479-0
21. Zung WW, Magruder-Habib K, Velez R, Alling W. The comorbidity of anxiety and depression in general medical patients: a longitudinal study. J Clin Psychiatry. (1990) 51 Suppl:77–80.
22. Roberts RE, Vernon SW. The Center for Epidemiologic Studies Depression Scale: its use in a community sample. Am J Psychiatry. (1983) 140:41–6. doi: 10.1176/ajp.140.1.41
23. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. (1983) 24:385–96. doi: 10.2307/2136404
24. Sedov ID, Cameron EE, Madigan S, Tomfohr-Madsen LM. Sleep quality during pregnancy: A meta-analysis. Sleep Med Rev. (2018) 38:168–76. doi: 10.1016/j.smrv.2017.06.005
25. Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. (2004) 27:1255–73. doi: 10.1093/sleep/27.7.1255
26. Gao M, Hu J, Yang L, Ding N, Wei X, Li L, et al. Association of sleep quality during pregnancy with stress and depression: a prospective birth cohort study in China. BMC Pregnancy Childbirth. (2019) 19:444. doi: 10.1186/s12884-019-2583-1
27. Andersen ML, Hachul H, Ishikura IA, Tufik S. Sleep in women: a narrative review of hormonal influences, sex differences and health implications. Front Sleep. (2023) 2:1271827. doi: 10.3389/frsle.2023.1271827
28. Pengo MF, Won CH, Bourjeily G. Sleep in women across the life span. Chest. (2018) 154:196–206. doi: 10.1016/j.chest.2018.04.005
29. Facco FL, Parker CB, Reddy UM, Silver RM, Koch MA, Louis JM, et al. Association between sleep-disordered breathing and hypertensive disorders of pregnancy and gestational diabetes mellitus. Obstet Gynecol. (2017) 129:31–41. doi: 10.1097/AOG.0000000000001805
30. Wilson DL, Walker SP, Fung AM, Pell G, O'Donoghue FJ, Barnes M, et al. Sleep-disordered breathing in hypertensive disorders of pregnancy: a BMI-matched study. J Sleep Res. (2018) 27:e12656. doi: 10.1111/jsr.12656
31. Xu H, Ouyang N, Li R, Tuo P, Mai M, Wang W. The effects of anxiety and depression on in vitro fertilisation outcomes of infertile Chinese women. Psychol Health Med. (2017) 22:37–43. doi: 10.1080/13548506.2016.1218031
32. Szkodziak F, Krzyżanowski J, Szkodziak P. Psychological aspects of infertility. A systematic review. J Int Med Res. (2020) 48:300060520932403. doi: 10.1177/0300060520932403
Keywords: sleep quality, anxiety, depression, perceived stress, assisted reproductive technology, natural conceiving, pregnancy
Citation: Xie Y, Peng R, Xiao L, Li S and Li X (2025) Sleep quality during pregnancy following assisted reproductive technology and natural conceiving: a prospective birth cohort study. Front. Endocrinol. 15:1497722. doi: 10.3389/fendo.2024.1497722
Received: 17 September 2024; Accepted: 31 December 2024;
Published: 22 January 2025.
Edited by:
Claus Yding Andersen, University of Copenhagen, DenmarkReviewed by:
Basilio Pecorino, Kore University of Enna, ItalyEvangelia Elenis, Uppsala University Hospital, Sweden
Copyright © 2025 Xie, Peng, Xiao, Li and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaohong Li, Nzg1MzY1NjEwQHFxLmNvbQ==
 Yidong Xie
Yidong Xie Ruoti Peng3
Ruoti Peng3 Li Xiao
Li Xiao Shangwei Li
Shangwei Li