- 1Department of Hepatobiliary Pancreatic Splenic and Thyroid Surgery, General Hospital of Northern Theater Command, Shenyang, China
- 2Dalian Medical University, General Hospital of Northern Theater Command Training Base for Graduate, Shenyang, China
- 3Chinese Medical University, General Hospital of Northern Theater Command Training Base for Graduate, Shenyang, China
Background: There are three main surgical treatment options for secondary hyperparathyroidism (SHPT): subtotal parathyroidectomy (sPTX), total parathyroidectomy with auto-transplantation (tPTX+AT), and total parathyroidectomy (tPTX). However, a debate regarding which of these surgical methods is optimal has been ongoing. Aim of this study is to compare medical costs and final outcomes associated with the three surgical approaches for the entire treatment duration, aiming to identify the most cost-effective surgical method.
Methods: Based on previous research data from domestic and international studies, as well as data from on-site surveys, TreeAge Pro 2022 software was used to construct a Markov model for the surgical treatment of SHPT patients. The model was run using data from the 2022 registered population of end-stage renal disease dialysis patients in China (1 million) as baseline cohort. Main indicators for this analysis are total cost, quality-adjusted life years, and incremental cost-effectiveness ratio (ICER). The study period is 10 years post-surgery, with a discount rate of 5% per year. Uncertainty in the model was assessed using one-way sensitivity analysis and probabilistic sensitivity analysis (PSA).
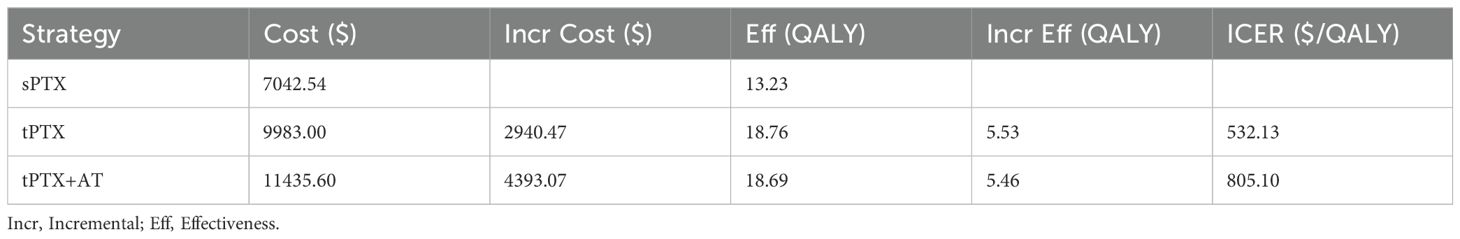
Results: The costs incurred by SHPT patients undergoing sPTX, tPTX, and tPTX+AT within 10 years post-surgery are $7042.54, $9983.00, and $11435.60, respectively, with total utilities generated being 13.23 QALYs, 18.76 QALYs, and 18.69 QALYs. Compared to sPTX, the incremental costs and incremental effects of tPTX and tPTX+AT are $2,924.71 and $4,456.66, with 5.53 QALYs and 5.46 QALYs, respectively. The ICER for tPTX and tPTX+AT groups are $532.13/QALY and $805.10/QALY, respectively, which are well below our set willingness-to-pay (WTP) threshold. Sensitivity analysis results indicate that varying any parameter within a certain range over the given time interval will not cause the ICER to exceed the WTP threshold and will not reverse the primary analysis results.
Conclusion: In the Chinese healthcare system, tPTX is considered the most cost-effective treatment for refractory hyperparathyroidism, when compared to tPTX+AT and sPTX.
1 Introduction
Secondary hyperparathyroidism (SHPT) is caused by hypocalcemia and hyperphosphatemia due to the disorder of the endocrine metabolic environment in patients with end-stage renal disease, resulting in hyperparathyroidism, parathyroid hyperplasia, and a series of clinical symptoms (1, 2). Clinically, it is characterized by a continuous rise in parathyroid hormone levels, enlargement of the parathyroid glands, and persistent bone pain, itching, insomnia, restless leg syndrome, and pathological fractures. This condition affects patient’s quality of life and can even lead to an increased risk of death (3, 4).
Currently, primary clinical treatments for SHPT include surgical and medical approaches. Medical treatment primarily involves use of calcimimetics. Researches have shown that calcimimetics, such as cinacalcet, can effectively reduce serum PTH levels and diminish the volume of parathyroid gland (5–7). However, patients with refractory SHPT, those for whom medical treatment is ineffective, or those who are intolerant to medication still require surgical intervention (8, 9). Currently, primary surgical treatments include total parathyroidectomy (tPTX), total parathyroidectomy with auto-transplantation (tPTX+AT), and subtotal parathyroidectomy (sPTX). However, a debate regarding the optimal surgical approach among these three methods remains ongoing. Several scholars have published clinical studies, systematic reviews, and meta-analyses to offer recommendations to surgeons. However, to date, there are no definitive guidelines identifying the optimal surgical method.
Our aim in this study was to determine which surgical method is most cost-effective and to offer recommendations for surgeons in selecting the appropriate treatment for SHPT.
2 Materials and methods
2.1 Model design
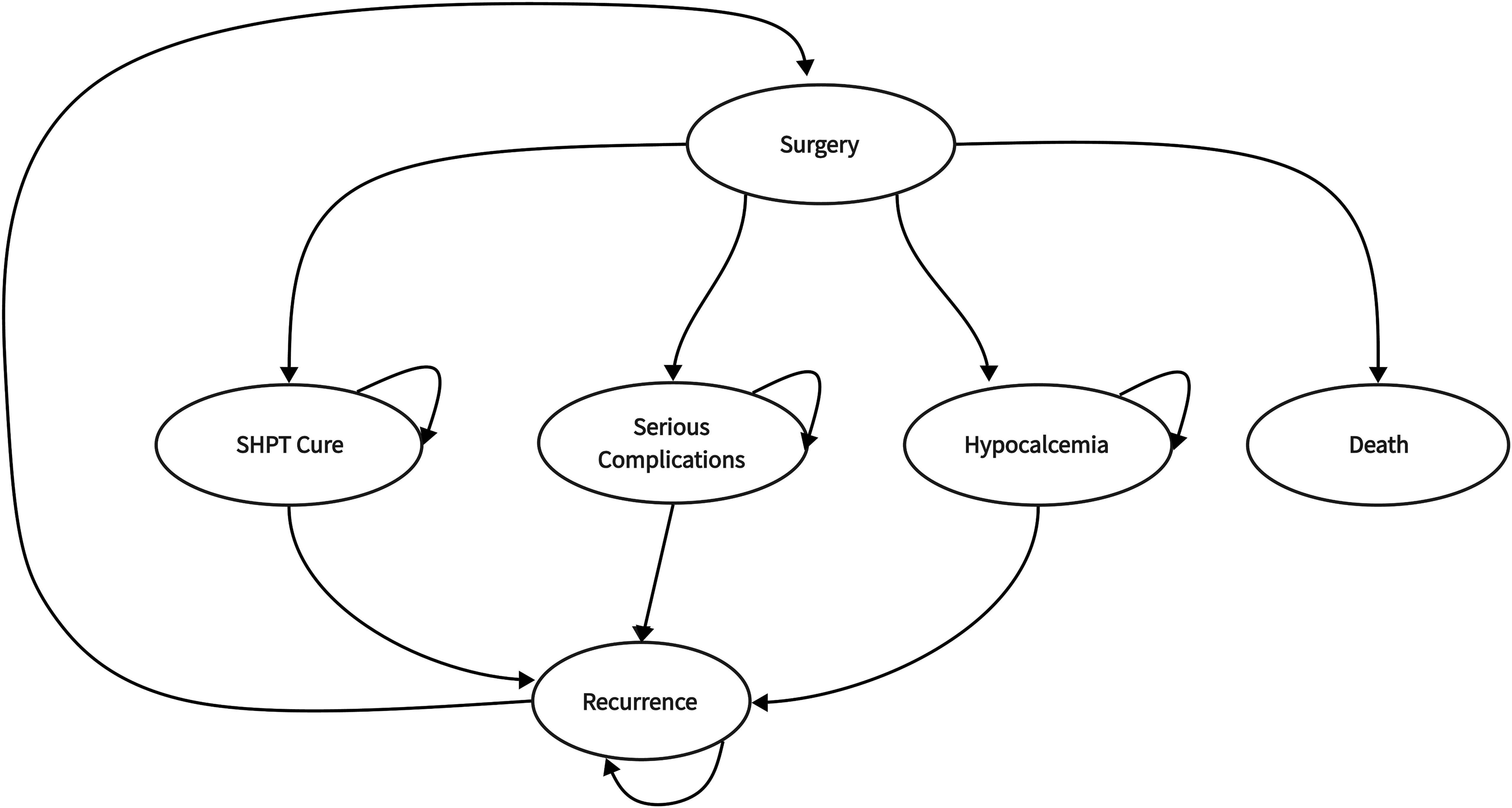
This study utilized the 2022 Chinese registry of end-stage renal disease dialysis patients (1 million) as the baseline population, assuming all these patients had SHPT and were awaiting surgical treatment. Then we used TreeAge Pro 2022 (Williamstown, MA) to develop a Markov model for the surgical treatment of SHPT from a societal perspective. The model had an annual cycle duration and terminated 10 years post-surgery. The model’s health states included post-surgical SHPT cure, surgery-induced death, post-surgical hypocalcemia, and other serious complications such as recurrent laryngeal nerve injury, bleeding, cardiovascular events, and infections.
2.2 Management strategy
In this research, the surgical strategies for SHPT included tPTX, sPTX, and tPTX+AT. In tPTX+AT, the grafts were transplanted into patient’s right forearm. After surgical treatment, patients transitioned into four predefined health states: post-surgical SHPT cure, surgery-induced death, post-surgical hypocalcemia, or other serious complications. A cohort of patients experiencing postoperative hypocalcemia received calcium supplementation therapy through administration of oral calcium carbonate tablets and calcitriol tablets. With the exception of state of death, the other three states all fall into two states of SHPT being controlled or recurrence. In tPTX+AT group, patients may experience two types of recurrence: at the right forearm graft site or in the neck. All patients with recurrence underwent reoperation, thus completing a cycle (Figure 1).
2.3 Data sources
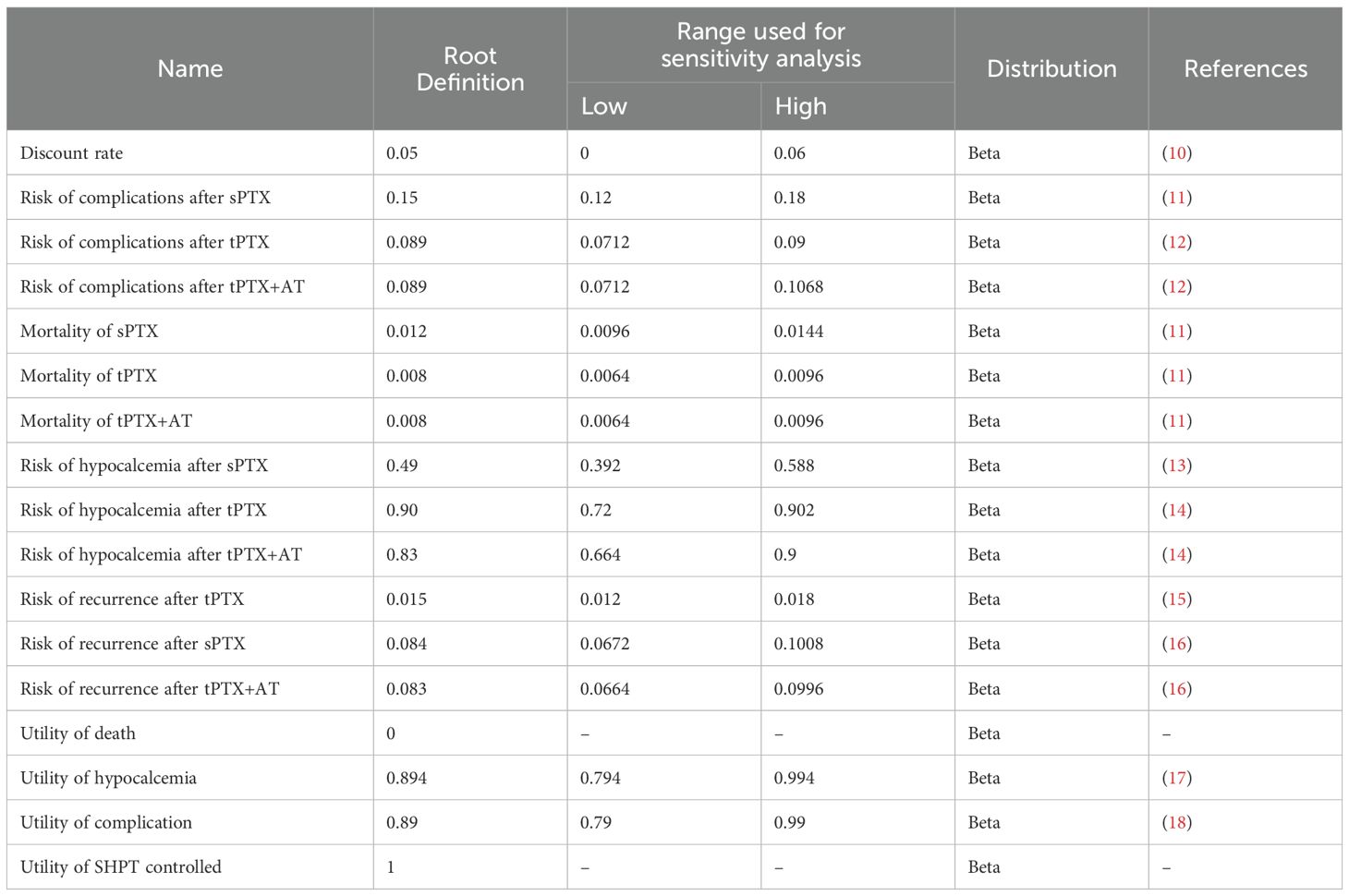
Main parameter values of the Markov model for cost-effectiveness of surgical treatment in patients with SHPT are presented in Table 1. Our study’s data inclusion criteria: original research or meta-analyses published in domestic and international journals from 2015 to 2023, focusing on parathyroidectomy alone without transcervical thymectomy. The surgery must have involved the complete removal of four parathyroid glands, with no definitive ectopic parathyroid glands identified in preoperative examinations or intraoperative exploration. Exclusion criteria: presence of ectopic parathyroid glands, failure to completely remove all four parathyroid glands during surgery, and data indicating residual parathyroid glands identified after tPTX+AT or tPTX procedures.
2.3.1 Epidemiology
In the model, epidemiological parameters used, including rates of post-surgical hypocalcemia, rates of other serious complications, mortality rates, recurrence rates, and rates of post-surgical SHPT cure, were all obtained from previously published literature, both domestic and international.
Since the previously published domestic and international literature did not directly provide mortality rates for the three types of surgery, we assumed that the 30-day postoperative mortality rates represent surgery-related mortality rates. Previous studies have shown that there is no significant difference in surgery time between tPTX and tPTX+AT (14). Therefore, we assumed that the mortality rates and the rates of other serious complications for these two surgical methods are same.
2.3.2 Cost
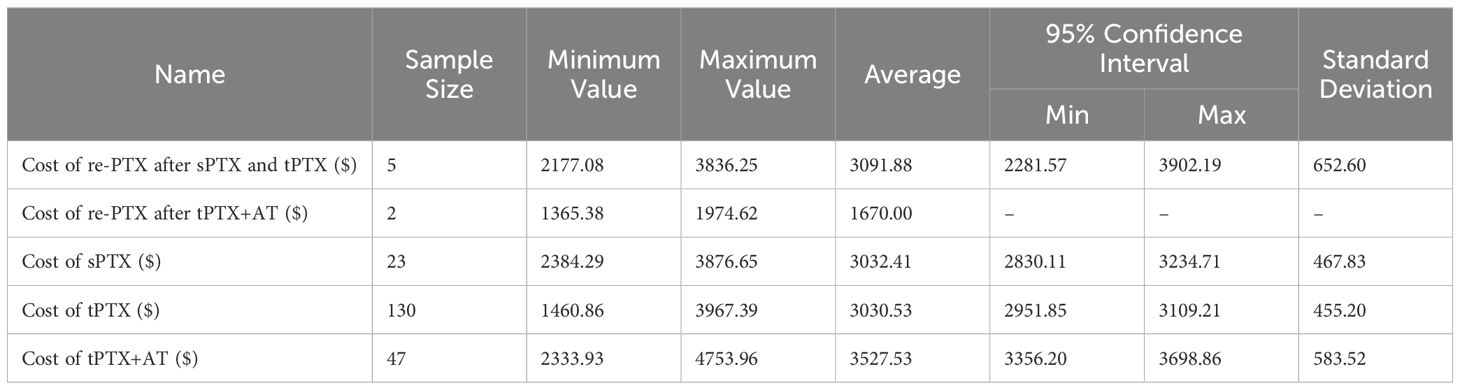
The costs included in this study primarily consist of direct medical costs, which encompass medication fees, examination fees, laboratory fees, surgical operation and material costs, nursing fees, and hospitalization costs. These were obtained from on-site surveys conducted in representative tertiary hospitals in China. The total of 207 cases of SHPT surgeries performed at this hospital, including 130 cases of tPTX, 23 cases of tPTX+AT, 47 cases of sPTX, 5 cases of SHPT recurrence surgeries, and 2 cases of the right forearm graft removal surgeries. As several datasets followed a normal distribution, the mean was used to construct the model (Table 2). We also used 5% discount rate to eliminate the effects of inflation.
2.3.3 Utility
Using quality-adjusted life years (QALYs) to assess health outcomes, ranging from 0 to 1. Post-surgical SHPT cure equals 1, death equals 0, the utility values of post-surgical hypocalcemia and other serious complications were obtained from published literature both domestically and internationally.
2.4 Base-case analysis
Incremental Cost-Effectiveness Ratio (ICER) is employed to evaluate SHPT surgical strategies. ICER refers to the cost required per additional QALY. ICER is computed using TreeAge Pro 2022 software with formula: ICER = (Cost of Strategy 2 - Cost of Strategy 1)/(QALY of Strategy 2 - QALY of Strategy 1). QALY values are determined by multiplying the survival time in a specific health state by the health utility of that state. The willingness to pay (WTP) threshold is set at $12,700 USD, based on China’s per capita Gross Domestic Product (GDP) in 2023.
2.5 Sensitivity analysis
We conducted one-way sensitivity analysis to assess the stability of the Markov model. By varying a single parameter within its range while keeping other parameters constant, we calculated changes in ICER to generate tornado diagrams. Probability sensitivity analysis was employed to evaluate cost-effectiveness under the WTP threshold, assigning specific distributions to model parameters. Monte Carlo simulations were conducted with 1,000 iterations and recalculations on a cohort of 1,000 patients to further elucidate the optimal treatment strategy under conditions of uncertainty.
3 Results
3.1 Base-case results
The number of dialysis patients registered in China in 2022 was used as a parameter in the cost-effectiveness analysis of three surgical approaches for secondary hyperparathyroidism (SHPT) within the Markov model. The costs incurred by SHPT patients undergoing sPTX, tPTX, and tPTX+AT over a 10-year period after surgery were $7042.53, $9983.00, and $11435.60 respectively, with total utilities generated of 13.23 QALY, 18.76 QALY, and 18.69 QALY. Compared with sPTX, the abbreviation costs and the incremental effects of tPTX and tPTX+AT were $2940.47, $4393.07 and 5.53 QALY, 5.46 QALY respectively. The ICERs for the tPTX and tPTX+AT groups are $532.13/QALY and $805.10/QALY, respectively, both of which are below the Willingness-To-Pay (WTP) threshold of $12,700 (Table 3).
3.2 Sensitivity analysis
The tornado diagram from one-way sensitivity analysis shows that, when comparing tPTX with sPTX, the top three parameters that significantly influence ICER value are post-sPTX hypocalcemia rate, post-sPTX recurrence rate, and cost of tPTX. Moreover, the smaller values of the first two variables, the larger the ICER value becomes, whereas opposite trend is observed for the latter variable (Figure 2A). When comparing tPTX+AT with sPTX, the top three parameters that significantly influence ICER value are post-sPTX hypocalcemia rate, post-sPTX recurrence rate, and post-tPTX+AT hypocalcemia rate. Moreover, the smaller values of the first two variables, the larger ICER value becomes, whereas opposite trend is observed for the latter variable (Figure 2B). Notably, varying any parameter within a specified range over given time period does not lead to an ICER exceeding the WTP threshold nor does it reverse primary analysis results, demonstrating the robustness of the model.
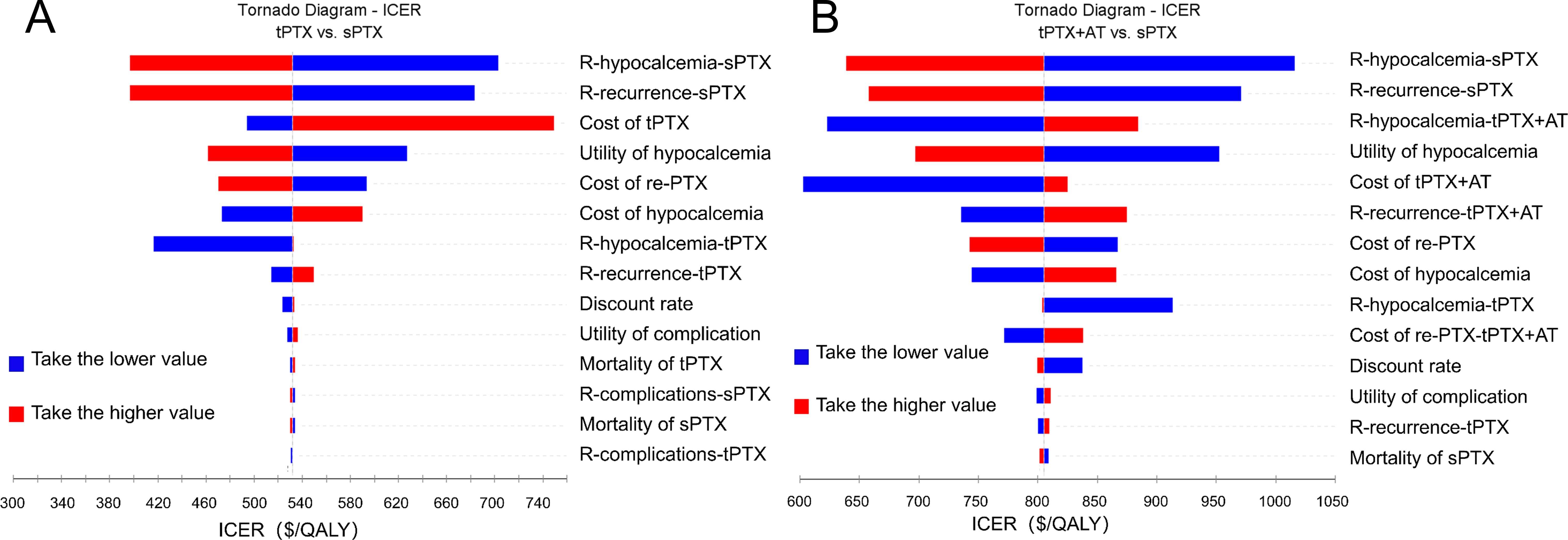
Figure 2. One-way sensitivity analysis. (A) Tornado diagram of tPTX vs sPTX; (B) Tornado diagram of tPTX+AT vs sPTX. R, Risk.
The results of probability sensitivity analysis indicate that, at the specified WTP threshold, tPTX and tPTX+AT have a 100% probability of cost-effectiveness compared with sPTX (Figures 3A, B). When compared with tPTX+AT, tPTX has a 95.70% probability of being cost-effective (Figure 3C). The cost-effectiveness acceptability curve shows that tPTX remains superior to the other two strategies, with the curve flattening as willingness to pay increases. At a specified willingness to pay of $12,700 USD, tPTX maintains cost-effectiveness in 95.7% of iterations, while tPTX+AT and sPTX maintain cost-effectiveness in 4.3% and 0% of iterations respectively (Figure 3D).
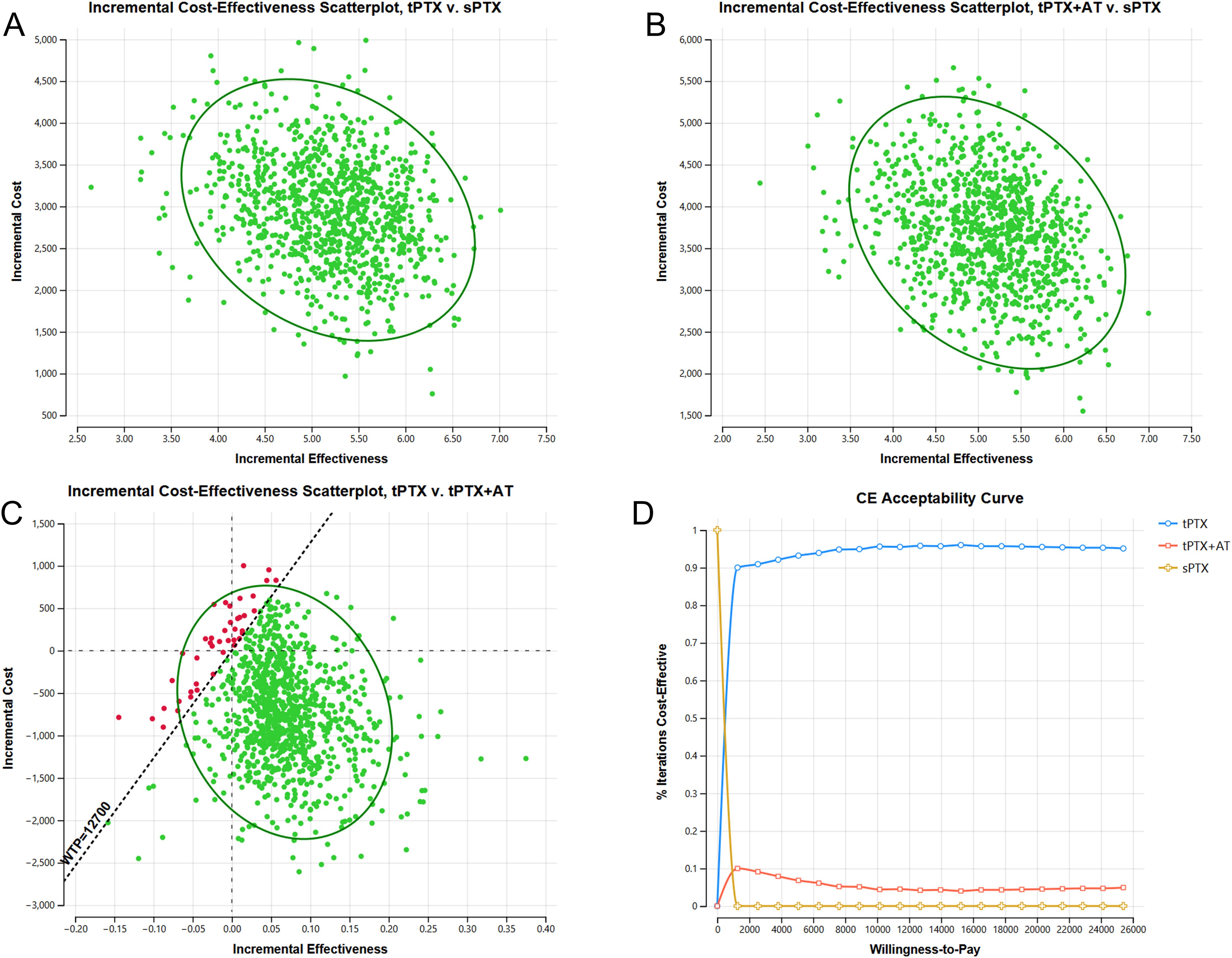
Figure 3. The results of probability sensitivity analysis. (A) Incremental cost-effectiveness scatterplot of tPTX vs sPTX; (B) Incremental cost-effectiveness scatterplot of tPTX+AT vs sPTX; (C) Incremental cost-effectiveness scatterplot of tPTX vs tPTX+AT; (D) Cost-effectiveness acceptability curve.
4 Discussion
Secondary hyperparathyroidism (SHPT) is a common condition among end-stage renal disease patients, resulting from metabolic disturbances. These patients often face substantial financial burdens due to the necessity of long-term or lifelong dialysis treatment or kidney transplantation. For patients with refractory SHPT, surgical treatment is the preferred option, making a selection of the most cost-effective surgical approach crucial. This study used basic data from existing clinical research to conduct an inaugural cost-effectiveness analysis of three surgical procedures for treating SHPT.
Our research findings suggest that, within the context of the Chinese healthcare system, total parathyroidectomy (tPTX) is a more cost-effective surgical treatment for patients with secondary hyperparathyroidism (SHPT) compared to the other two surgical approaches. This outcome is attributable to the relatively high risk of hypocalcemia associated with tPTX, which is offset by its lower recurrence rate, thereby reducing the likelihood of reoperation, lowering overall treatment costs, and yielding better health outcomes. These findings have significant implications for allocation of medical resources and decision-making in the management of patients with end-stage renal disease complicated by SHPT in China.
The sensitivity analysis results highlight that the post-sPTX hypocalcemia rate, post-sPTX recurrence rate, post-tPTX+AT hypocalcemia rate, and the cost of tPTX are four parameters most significantly affecting the incremental cost-effectiveness ratio (ICER). Thus, reducing postoperative hypocalcemia rates and treatment costs is crucial for enhancing cost-effectiveness. In conclusion, improving surgical techniques and perioperative management to lower the risk of postoperative hypocalcemia, or reforming the medical insurance system to reduce costs, can achieve better cost-effectiveness.
A meta-analysis incorporating 10 studies with a total of 1283 patients compared the postoperative efficacy of tPTX and tPTX+AT. The findings revealed that, in comparison to tPTX+AT, tPTX group exhibited significantly lower rates of recurrence, recurrence or persistent secondary hyperparathyroidism (SHPT), reoperation due to recurrence or persistent SHPT, and had shorter operation times. Nevertheless, tPTX group had a higher risk of hypoparathyroidism compared with tPTX+AT group, while no significant differences were observed in other aspects. Consequently, the authors suggested that tPTX might be more advantageous in treating SHPT compared to tPTX+AT (12). Additionally, a retrospective randomized controlled study of 46 patients compared the long-term and short-term outcomes of subtotal parathyroidectomy (sPTX) with tPTX+AT. The study indicated that tPTX+AT, relative to sPTX, enhances the long-term control of elevated parathyroid hormone levels and helps in preventing disease recurrence, albeit with a higher risk of long-term hypocalcemia (19). From above two studies, we can conclude that among the three surgical methods, tPTX has more advantages in surgical treatment of SHPT, which is consistent with our analysis from a cost-effectiveness perspective.
However, some researchers have presented different viewpoints. A network meta-analysis, which included 26 studies involving a total of 5063 patients, compared the three surgical methods regarding their rates of postoperative hypocalcemia (or hypoparathyroidism), recurrence, and reoperation. This study ultimately recommended tPTX+AT as the most effective and safest surgical treatment for SHPT, with the fewest adverse reactions (20), which is inconsistent with our results. This discrepancy may be due to the fact that the aforementioned studies did not account for the relationship between costs and postoperative outcomes. They overlooked the higher costs associated with reoperations due to the higher recurrence rate of tPTX+AT, which led to different conclusions compared to our study.
Although several randomized controlled studies have demonstrated that both sPTX and tPTX+AT are effective in treating SHPT, some scholars argue that CKD can stimulate the residual parathyroid glands, potentially leading to persistent or recurrent SHPT in patients. Therefore, to prevent persistence or recurrence, tPTX is considered the preferred surgical method for SHPT patients (21).
Although our study, like the aforementioned studies, found that tPTX is the optimal surgical method, other literature suggests that after kidney transplantation, stability of the internal environment reduces the stimulation of the parathyroid glands, thereby lowering the risk of SHPT. Consequently, it is recommended that patients awaiting kidney transplantation undergo tPTX+AT or sPTX to prevent hypoparathyroidism (19, 22). The KIDIGO guidelines even explicitly state that tPTX is contraindicated for patients waiting for kidney transplantation (23). Therefore, we recommend tPTX+AT for SHPT patients who are awaiting kidney transplantation.
The model designed in this study has the following limitations. First, the primary limitation of this study is that, apart from cost data, all other data in the model were derived from previously published literature rather than a purpose-built cohort study., which may lead to bias in the study results. Secondly, patients with ectopic parathyroid glands were not included in this study. which may require more extensive surgical removal. This exclusion could affect our results by influencing the costs and postoperative complications. In addition, the tPTX and tPTX+AT data included in this study were limited to cases where transcervical thymectomy was not performed during surgery. The inclusion or exclusion of thymectomy may influence the choice of the optimal surgical approach by affecting postoperative outcomes and overall costs. Finally, while the direct medical cost data were obtained from real-world on-site surveys, most of the other parameter values in the model were derived from original studies conducted internationally. Consequently, the findings of this study may have limited applicability on a global scale and are more specifically tailored to the Chinese healthcare context. Therefore, we designed one-way sensitivity analysis and probabilistic sensitivity analysis during our research to minimize the impact of these limitations. Despite these limitations, we believe that our study can provide valuable recommendations for the surgical treatment of SHPT.
5 Conclusion
According to our research, in Chinese healthcare system, tPTX as the first-line treatment for end-stage renal disease secondary to refractory hyperparathyroidism is considered to have the highest cost-effectiveness compared to tPTX+AT and sPTX. This conclusion is based on a comprehensive analysis of the existing data on the costs and health outcomes associated with the three different treatment strategies. However, for patients awaiting kidney transplantation, we recommend tPTX+AT. Additionally, reducing the incidence of postoperative hypocalcemia during surgical treatment is crucial for enhancing cost-effectiveness.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
QS: Conceptualization, Data curation, Methodology, Software, Writing – original draft, Formal analysis, Writing – review & editing. YZ: Conceptualization, Supervision, Writing – review & editing. GC: Data curation, Supervision, Writing – review & editing. BN: Conceptualization, Data curation, Supervision, Writing – review & editing. YF: Data curation, Formal analysis, Writing – original draft. NZ: Data curation, Formal analysis, Writing – review & editing. WX: Data curation, Formal analysis, Writing – review & editing. WZ: Conceptualization, Funding acquisition, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by Medical and Industrial Cross Joint Project of Liaoning Province (NO.2022-YGJC-11).
Acknowledgments
The authors thank WZ for his support of this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Shindo M, Lee JA, Lubitz CC, McCoy KL, Orloff LA, Tufano RP, et al. The changing landscape of primary, secondary, and tertiary hyperparathyroidism: highlights from the american college of surgeons panel, "What's new for the surgeon caring for patients with hyperparathyroidism. J Am Coll Surg. (2016) 222:1240–50. doi: 10.1016/j.jamcollsurg.2016.02.024
2. Kim SM, Long J, Montez-Rath ME, Leonard MB, Norton JA, Chertow GM. Rates and outcomes of parathyroidectomy for secondary hyperparathyroidism in the United States. Clin J Am Soc Nephrol. (2016) 11:1260–7. doi: 10.2215/CJN.10370915
3. Leifheit-Nestler M, Große Siemer R, Flasbart K, Richter B, Kirchhoff F, Ziegler WH, et al. Induction of cardiac FGF23/FGFR4 expression is associated with left ventricular hypertrophy in patients with chronic kidney disease. Nephrol Dial Transplant. (2016) 31:1088–99. doi: 10.1093/ndt/gfv421
4. Liu ZH, Yu XQ, Yang JW, Jiang AL, Liu BC, Xing CY, et al. Prevalence and risk factors for vascular calcification in Chinese patients receiving dialysis: baseline results from a prospective cohort study. Curr Med Res Opin. (2018) 34:1491–500. doi: 10.1080/03007995.2018.1467886
5. Komaba H, Nakanishi S, Fujimori A, Tanaka M, Shin J, Shibuya K, et al. Cinacalcet effectively reduces parathyroid hormone secretion and gland volume regardless of pretreatment gland size in patients with secondary hyperparathyroidism. Clin J Am Soc Nephrol. (2010) 5:2305–14. doi: 10.2215/CJN.02110310
6. Tatsumi R, Komaba H, Kanai G, Miyakogawa T, Sawada K, Kakuta T, et al. Cinacalcet induces apoptosis in parathyroid cells in patients with secondary hyperparathyroidism: histological and cytological analyses. Nephron Clin Pract. (2013) 124:224–31. doi: 10.1159/000357951
7. Fukagawa M, Fukuma S, Onishi Y, Yamaguchi T, Hasegawa T, Akizawa T, et al. Prescription patterns and mineral metabolism abnormalities in the cinacalcet era: results from the MBD-5D study. Clin J Am Soc Nephrol. (2012) 7:1473–80. doi: 10.2215/CJN.13081211
8. Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Update Work Group. KDIGO 2017 clinical practice guideline update for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease-mineral and bone disorder (CKD-MBD). Kidney Int Suppl (2011). (2017) 7:1–59. doi: 10.1016/j.kisu.2017.04.001
9. Tominaga Y, Matsuoka S, Uno N. Surgical and medical treatment of secondary hyperparathyroidism in patients on continuous dialysis. World J Surg. (2009) 33:2335–42. doi: 10.1007/s00268-009-9943-3
10. Yue X, Li Y, Wu J, Guo JJ. Current development and practice of pharmacoeconomic evaluation guidelines for universal health coverage in China. Value Health Reg Issues. (2021) 24:1–5. doi: 10.1016/j.vhri.2020.07.580
11. Anderson K Jr, Ruel E, Adam MA, Thomas S, Youngwirth L, Stang MT, et al. Subtotal vs. total parathyroidectomy with autotransplantation for patients with renal hyperparathyroidism have similar outcomes. Am J Surg. (2017) 214:914–9. doi: 10.1016/j.amjsurg.2017.07.018
12. Liu ME, Qiu NC, Zha SL, Du ZP, Wang YF, Wang Q, et al. To assess the effects of parathyroidectomy (TPTX versus TPTX+AT) for Secondary Hyperparathyroidism in chronic renal failure: A Systematic Review and Meta-Analysis. Int J Surg. (2017) 44:353–62. doi: 10.1016/j.ijsu.2017.06.029
13. Yuan Q, Liao Y, Zhou R, Liu J, Tang J, Wu G. Subtotal parathyroidectomy versus total parathyroidectomy with autotransplantation for secondary hyperparathyroidism: an updated systematic review and meta-analysis. Langenbecks Arch Surg. (2019) 404:669–79. doi: 10.1007/s00423-019-01809-7
14. Schlosser K, Bartsch DK, Diener MK, Seiler CM, Bruckner T, Nies C, et al. Total parathyroidectomy with routine thymectomy and autotransplantation versus total parathyroidectomy alone for secondary hyperparathyroidism: results of a nonconfirmatory multicenter prospective randomized controlled pilot trial. Ann Surg. (2016) 264:745–53. doi: 10.1097/SLA.0000000000001875
15. Li C, Lv L, Wang H, Wang X, Yu B, Xu Y, et al. Total parathyroidectomy versus total parathyroidectomy with autotransplantation for secondary hyperparathyroidism: systematic review and meta-analysis. Ren Fail. (2017) 39:678–87. doi: 10.1080/0886022X.2017.1363779
16. Chen J, Jia X, Kong X, Wang Z, Cui M, Xu D. Total parathyroidectomy with autotransplantation versus subtotal parathyroidectomy for renal hyperparathyroidism: A systematic review and meta-analysis. Nephrol (Carlton). (2017) 22:388–96. doi: 10.1111/nep.2017.22.issue-5
17. Bhattacharyya N, Fried MP. Assessment of the morbidity and complications of total thyroidectomy. Arch Otolaryngol Head Neck Surg. (2002) 128:389–92. doi: 10.1001/archotol.128.4.389
18. Rocke DJ, Goldstein DP, de Almeida JR. A cost-utility analysis of recurrent laryngeal nerve monitoring in the setting of total thyroidectomy. JAMA Otolaryngol Head Neck Surg. (2016) 142:1199–205. doi: 10.1001/jamaoto.2016.2860
19. Zmijewski PV, Staloff JA, Wozniak MJ, Mazzaglia PJ. Subtotal parathyroidectomy vs total parathyroidectomy with autotransplantation for secondary hyperparathyroidism in dialysis patients: short- and long-term outcomes. J Am Coll Surg. (2019) 228:831–8. doi: 10.1016/j.jamcollsurg.2019.01.019
20. Hou J, Shan H, Zhang Y, Deng X, Guo B, Kang J, et al. Network meta-analysis of surgical treatment for secondary hyperparathyroidism. Am J Otolaryngol. (2020) 41:102370. doi: 10.1016/j.amjoto.2019.102370
21. Tominaga Y, Katayama A, Sato T, Matsuoka S, Goto N, Haba T, et al. Re-operation is frequently required when parathyroid glands remain after initial parathyroidectomy for advanced secondary hyperparathyroidism in uraemic patients. Nephrol Dial Transplant. (2003) 18(Suppl 3):iii65–70. doi: 10.1093/ndt/gfg1017
22. Nichol PF, Starling JR, Mack E, Klovning JJ, Becker BN, Chen H. Long-term follow-up of patients with tertiary hyperparathyroidism treated by resection of a single or double adenoma. Ann Surg. (2002) 235:673–8. doi: 10.1097/00000658-200205000-00009
Keywords: secondary hyperparathyroidism, parathyroidectomy, cost-effectiveness analysis, Markov model, surgical approaches
Citation: Sa Q, Zhou Y, Cheng G, Nan B, Feng Y, Zhang N, Xie W and Zhang W (2025) Cost-effectiveness analysis of three surgical approaches for parathyroidectomy in secondary hyperparathyroidism patients. Front. Endocrinol. 15:1495818. doi: 10.3389/fendo.2024.1495818
Received: 13 September 2024; Accepted: 31 December 2024;
Published: 27 January 2025.
Edited by:
Claudio Casella, University of Brescia, ItalyReviewed by:
Takahisa Hiramitsu, Japanese Red Cross Nagoya Daini Hospital, JapanLaura Musso, University of Genoa, Italy
Copyright © 2025 Sa, Zhou, Cheng, Nan, Feng, Zhang, Xie and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wei Zhang, emhhbmdfd2VpXzE5ODBAMTYzLmNvbQ==
†These authors have contributed equally to this work
 Qila Sa
Qila Sa Yinghui Zhou
Yinghui Zhou Guangming Cheng1
Guangming Cheng1 Boyuan Nan
Boyuan Nan Wei Zhang
Wei Zhang