- 1Department of Family and Community Medicine, Faculty of Medicine, University of Tabuk, Tabuk, Saudi Arabia
- 2Training Department, Academic Affairs and Training Administration, Ministry of Health, Tabuk, Saudi Arabia
Background: Obesity is one of the most prevalent and relevant health problems in Saudi Arabia and requires urgent attention. Family physicians are the first point of contact and one of the most important starting points for the successful treatment of being overweight or obese.
Aim: This study aimed to assess the knowledge, beliefs, and practices of primary care physicians in promoting healthy lifestyles and physical activity among obese patients.
Methods: This cross-sectional study included family physicians who were board-certified or registered in a family medicine training program and working at government family healthcare centers in Tabuk. A predesigned structured questionnaire was distributed either in a printed form or as an online survey.
Results: The study included 83 family physicians. Of these, 84.1% agreed that overweight and obese patients should be screened for dyslipidemia, and 67.5% agreed to offer advice on weight control even if the patient did not ask for it, demonstrating what family medicine physicians thought of physical inactivity (97.6%). Assessment of the obesity counseling practices of family medicine physicians revealed that approximately three-fourths (75.9%) always calculated the body mass index (BMI) of patients during obesity management, while comprehensive counseling regarding physical activity was higher (81.9%). The system for providing educational materials as part of managing overweight or obesity was found to be inadequate as 25.3% had never done so. The family medicine physicians had sufficient knowledge and positive beliefs about obesity management but also improper counseling practices. A lack of training and poor patient compliance with management plans are the main barriers to controlling obesity levels.
Introduction
Obesity is the primary cause of cardiovascular diseases (CVD), diabetes mellitus (DM), cancers, and ischemic heart disease (IHD); therefore, it is considered a major non-communicable disease in Saudi Arabia, with a high prevalence and great financial burden that is beyond the capacity of the people and government to cope with (1). Obesity is defined as abnormal or excessive fat accumulation that may impair health (2). Body mass index (BMI) is a simple index of weight and height that is commonly used to classify being overweight and obesity in adults.
Although obesity is preventable, globally, the prevalence of obesity among adults ranges from 42.4% in the United States of America to 59% in Europe, and one-third of children are obese (2).
A review of obesity prevalence in Saudi Arabia by Al-Qarni classified Saudi Arabia as having the highest prevalence in the Gulf region, with approximately one in four people being obese in 2020 (1, 3). A patient who is obese or overweight needs an effective counseling intervention, hence, family physicians are expected to provide conscious counseling in terms of individual prescriptions of optimal dietary items, calories, and physical exercise per day according to the country’s guidelines. This cross-sectional study assessed family physicians’ beliefs, knowledge, and practices in a quantitative manner. Furthermore, we explored their opinions, experiences, and beliefs regarding counseling for obesity and being overweight at primary healthcare centers (PHCs) in the Tabuk region. Due to the scarcity of data on physical activity counseling practices in PHCs in Saudi Arabia (4), we focused on the assessment of physical activity knowledge and attitudes of health providers at the PHC level; hence, we could correctly identify and address barriers to physical activity counseling.
Moreover, physical activity counseling at the PHC level is internationally recognized as a valuable and cost-effective approach to combat obesity and its associated comorbidities. According to Saudi guidelines for the management of obesity in adults in 2016, a well-organized and practical program for lifestyle intervention at the primary healthcare level is highly recommended. Likewise, the guidelines suggest individual counseling rather than providing generic educational materials and physical activity rather than no activity; thus, it encourages counseling for physical activity with diet rather than diet alone (5). In contrast, a systematic review of childhood obesity conducted by (6) classified clinic-based lifestyle interventions for obesity and revealed favorable results, suggesting family involvement and a multidisciplinary approach to be advantageous. Furthermore, student counseling is a valuable intervention option to combat obesity among school-age children in the long term (7). The study by Ghoraba et al. (8) forecasted a rising prevalence of diabetes in the coming years owing to the high prevalence of prediabetes in Saudi Arabia (23.6%); thus, the study proposed lifestyle interventions to reduce new incident cases.
This study aimed to assess the knowledge, beliefs, and practices of family physicians in promoting healthy dietary habits and physical activity among patients with obesity in Tabuk, Saudi Arabia.
Methods
Ethical considerations
This study was approved by the Ethics Committee of the University of Tabuk in Tabuk, Saudi Arabia (RB Protocol No: TU-07710221164). Informed consent was obtained from all the participants, including a consent statement from the survey. The participants were clearly informed about the nature and objectives of the study, and were also notified that their anonymized data would be used only for research purposes and that their confidentiality would be maintained.
Study design, setting, and date
This cross-sectional survey was conducted at 25 government primary healthcare centers in Tabuk City, Saudi Arabia, between May and June 2022.
Sample size and sampling technique
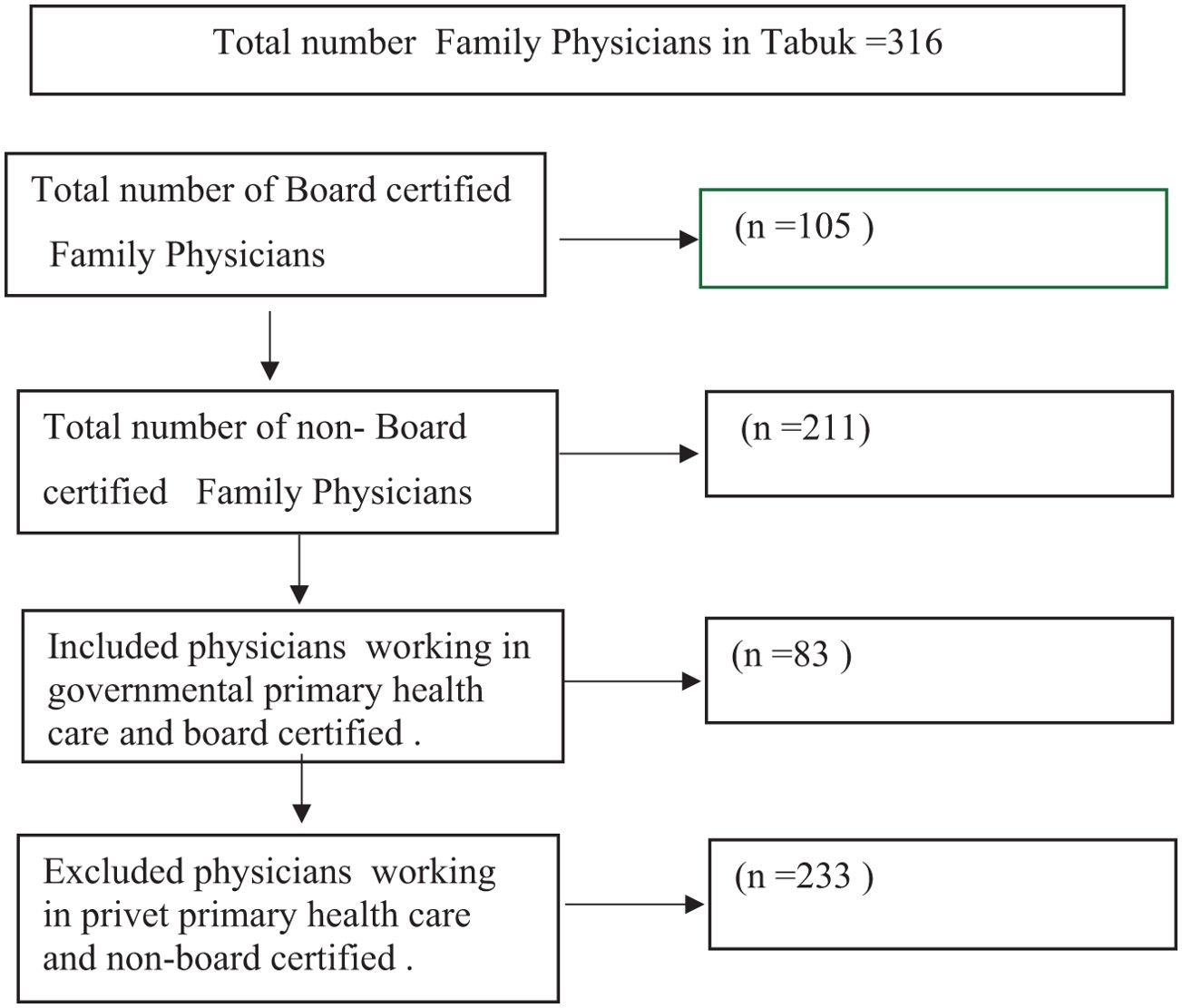
The sample size was calculated using the following formula: n=Z2 P Q/d2, where Z = 95% confidence (1.96) and P = number of family physicians and residents in Tabuk City, with a 5% confidence interval. The sample size was calculated to be 83 participants (Figure 1).
The unit of analysis was the family medicine physician, and the sampling followed the rule of dual-frame sampling for a standalone facility survey approach (WHO, 2003). Therefore, the sampling of the healthcare centers followed a simple random sampling technique. An updated list of healthcare facilities was used to create a list frame sample for facilities and an area frame sample was used to balance coverage through the allocation of healthcare facilities, using an updated map from the Ministry of Health. All 25 government primary healthcare centers in Tabuk City were included in the study.
Eligibility criteria
Family physicians who were board-certified or registered in the family medicine training program and working at government family healthcare centers in Tabuk were included in the study. Family physicians who were not board-certified or registered in the family medicine training program and those working at private family healthcare centers were excluded.
Data collection tool
A pre-designed structured questionnaire was used to collect data. The questionnaire was validated using two previously published research articles, with some minor modifications (9–11). The questionnaire consisted of 37 items. Part 1 consisted of seven statements regarding personal data, including age, gender, nationality, experience, average number of patients per day, and final qualifications. Part 2 contained nine statements that tested knowledge of the health risks of obesity, diagnosis, and lifestyle (diet and exercise). Responses to the statements were categorized as “Yes” for affirmative answers, “No” for non-affirmative answers, and “Not sure” at the GP’s discretion. Part 3 used a 10-point scale to measure responses, with an attitude rating on a five-point Likert scale (strongly agree, agree, neither, disagree, and strongly disagree) and consisted of statements. Item agreement scores were calculated using a scale [minimum of one (completely disagree) to a maximum of five (completely agree)]. Agreement was scored as 4 or 5 (agree and strongly agree), disagreement was scored as 1 or 2 (disagree and strongly disagree), and neutrality was scored as 3. Part 4 consisted of 10 statements to measure responses related to barriers to the adequate management of overweight and obesity with answers of “Agree”, “Neither”, or “Disagree.” Part 5 consisted of nine statements that measured responses to (always, often, or never) assessing practice. We also asked about possible causes of obesity using a list of 10 possible causes of obesity.
Procedure
The questionnaires were distributed in either a printed or an online form. The participants were met at their workplace by the co-authors, and all family physicians, including residents, registrars, and consultants, were invited to participate after a general explanation of the study’s aim.
Statistical analysis
The collected data were recorded, verified, and tabulated using the Statistical Package for Social Sciences (IBM SPSS Statistics), version 22.0 for Windows (IBM Corp., Armonk, N.Y., USA). Descriptive statistics (frequencies and percentages) were calculated. Inferential statistics were calculated using the chi-square test for the associations between age groups, gender, qualifications, and the practices of the respondents. Differences were considered statistically significant at P < 0.05.
Results
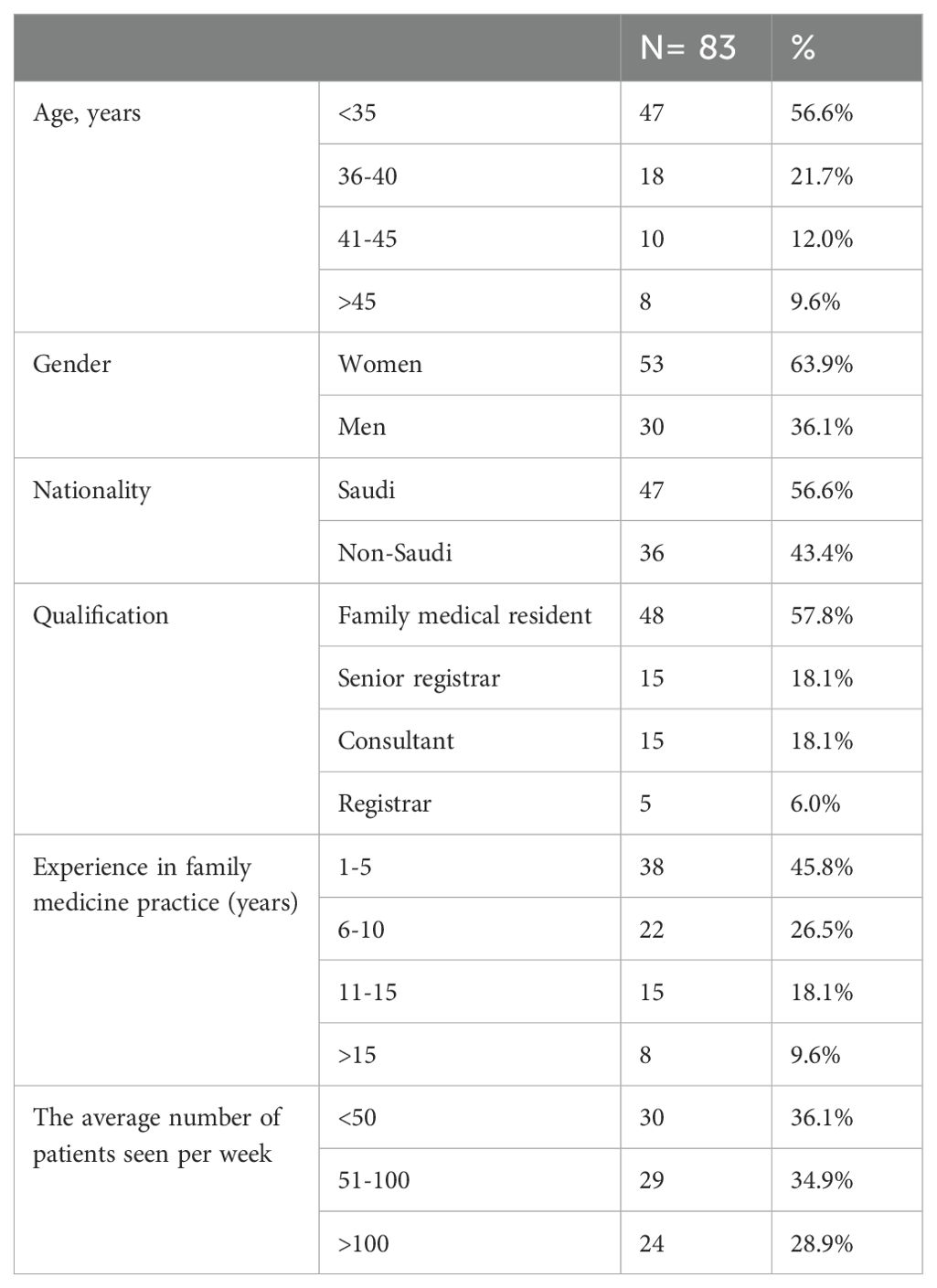
This study included 83 family medical physicians. Women constituted 63.9% of the total population. The most common age group was <35 years (56.6%). Saudi physicians accounted for 56.6% of the sample, whereas non-Saudi physicians accounted for 43.4%. Most participants were residents (57.8%), senior registrars (18.1%), consultants (18.1%), or registrars (6.0%). Most had clinical experience of 1-5 or 6-10 years (45.8% and 26.5%, respectively), followed by 11-15 years (18.1%). Finally, 30 (36.1%) and 29 (34.9%) physicians observed fewer than 50 and 50-100 patients per week, respectively (Table 1).
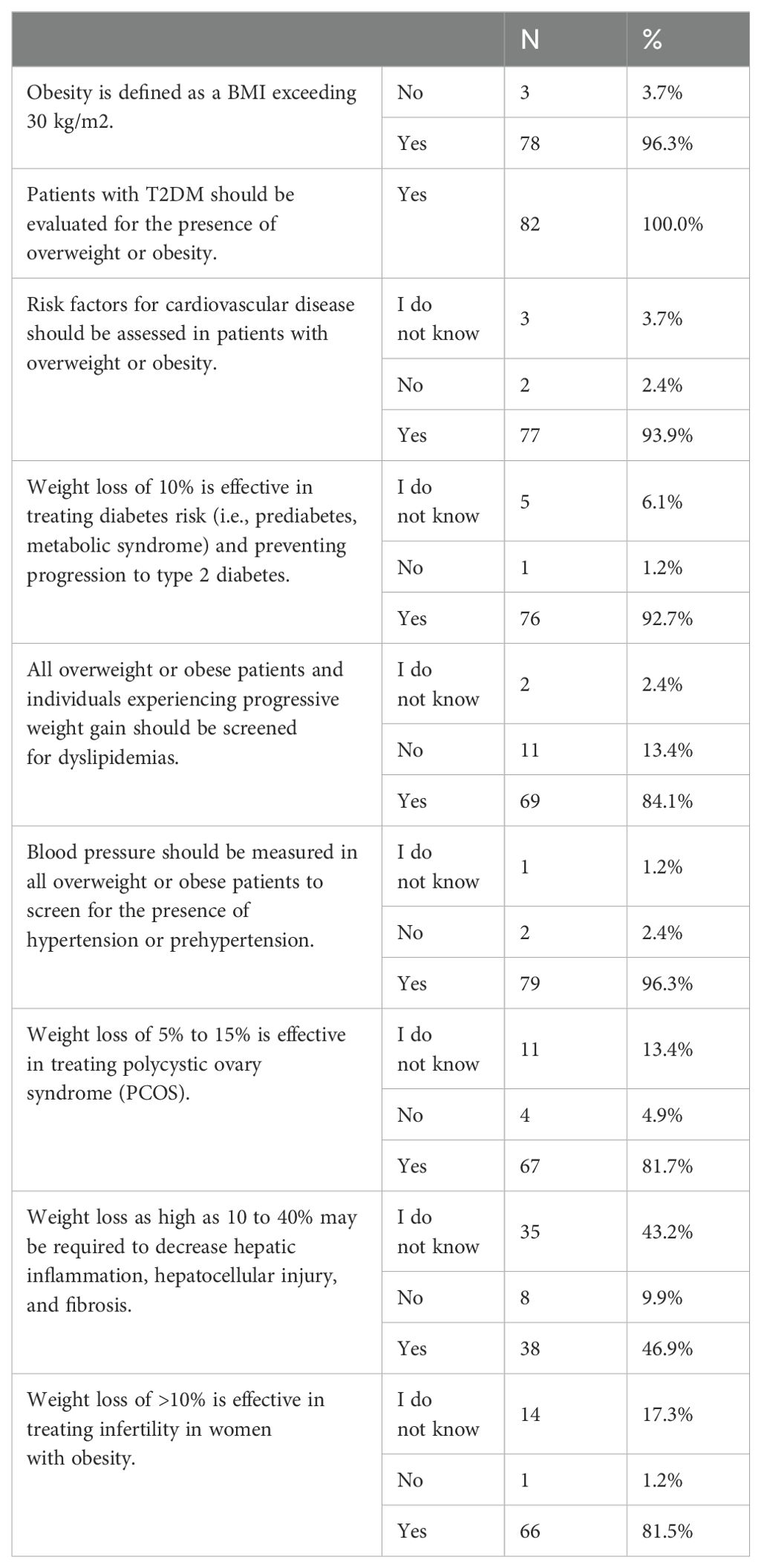
Table 2 shows the knowledge of family medicine physicians regarding being overweight or obese and the necessity of weight loss. The majority (96.3%) knew that obesity was defined as a BMI > 30 kg/m2, and all (100%) physicians knew that patients with type 2 diabetes should be evaluated for being overweight or obese. Furthermore, 92.7% realized that 10% weight loss was effective in preventing the progression of prediabetes to type 2 diabetes, whereas 81.7% understood that 5%–15% weight loss was effective in treating polycystic ovary syndrome. There was insufficient knowledge about the value of weight loss in decreasing hepatic inflammation, hepatocellular injury, and fibrosis by 10–40%; 46.9% knew this, while 43.2% did not. In addition, 17.3% of the participants did not know that >10% weight loss was effective in treating infertility in women with obesity. Additionally, 77 respondents (93.9%) knew that counseling overweight or obese clients should include investigating risk factors for cardiovascular disease, while 3.7% did not know. Most of the participants (96.3%) recognized the benefit of measuring blood pressure in all overweight or obese patients by screening for the presence of hypertension or prehypertension, whereas 84.1% agreed that overweight and obese clients should be screened for dyslipidemia.
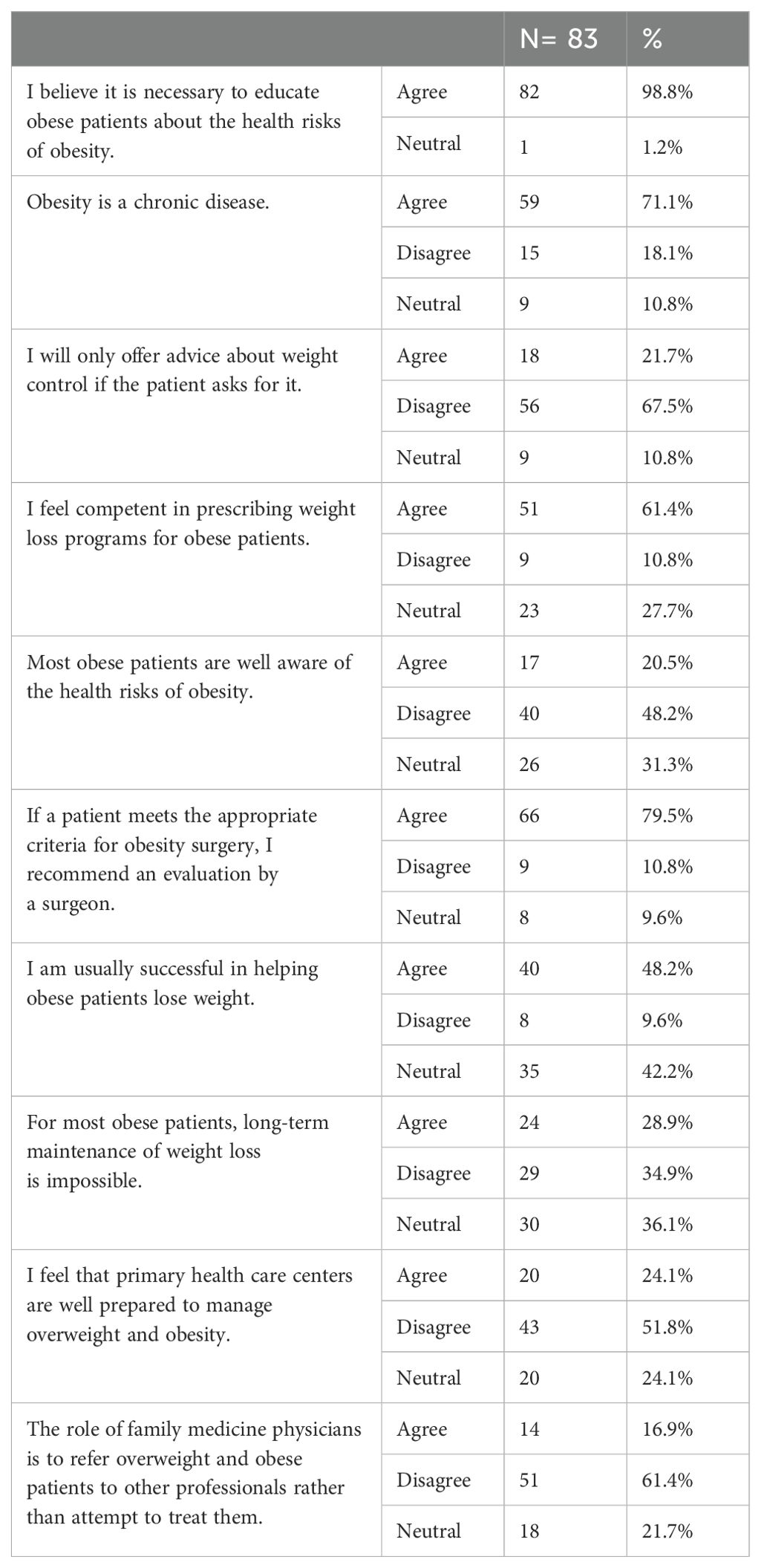
The beliefs of the family medicine physicians regarding the management of obesity and being overweight are presented in Table 3. In total, 59 (71.1%) physicians agreed with the chronic nature of obesity, whereas a high percentage (98.8%) agreed with the necessity of health education for obese patients regarding the health risks of obesity. However, only 67.5% agreed to offer advice on weight control even if the patient did not ask for it. Among the study participants, 61.4% felt competent in prescribing weight loss programs for obese patients, less than half (48.2%) agreed that they were usually successful in helping obese patients lose weight, 42.2% were neutral, and 79.5% agreed to recommend an evaluation by a surgeon if a patient met the appropriate criteria for obesity surgery. However, 38.6% thought that the role of family medicine physicians was to refer overweight or obese patients to other professionals rather than to attempt to treat them, and 51.8% felt that primary healthcare centers were not well prepared to manage overweight or obese patients. Furthermore, 64.1% believed that the long-term maintenance of weight loss was impossible in most obese patients.
The data displayed in Table 4 demonstrates that family medicine physicians believed that physical inactivity (97.6%), endocrine disorders (84.3%), genetic factors (81.9%), overeating (80.7%), and a high-fat diet (75.9%) were the most frequent risk factors for obesity in Saudi Arabia. Moreover, a lack of training (72.3%) and poor patient adherence to the management plan (71.1%) were considered crucial barriers to obesity management in Saudi Arabia.
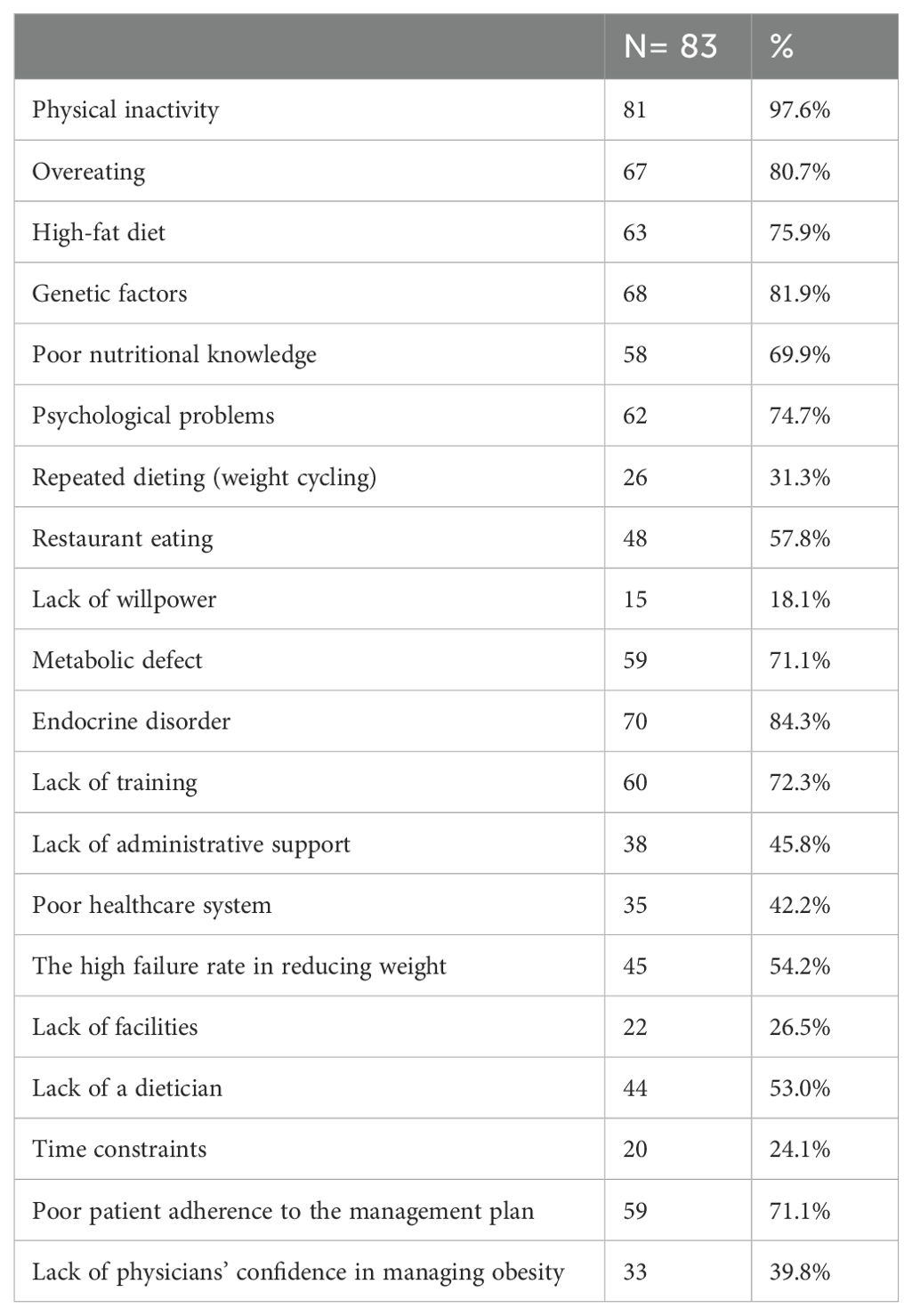
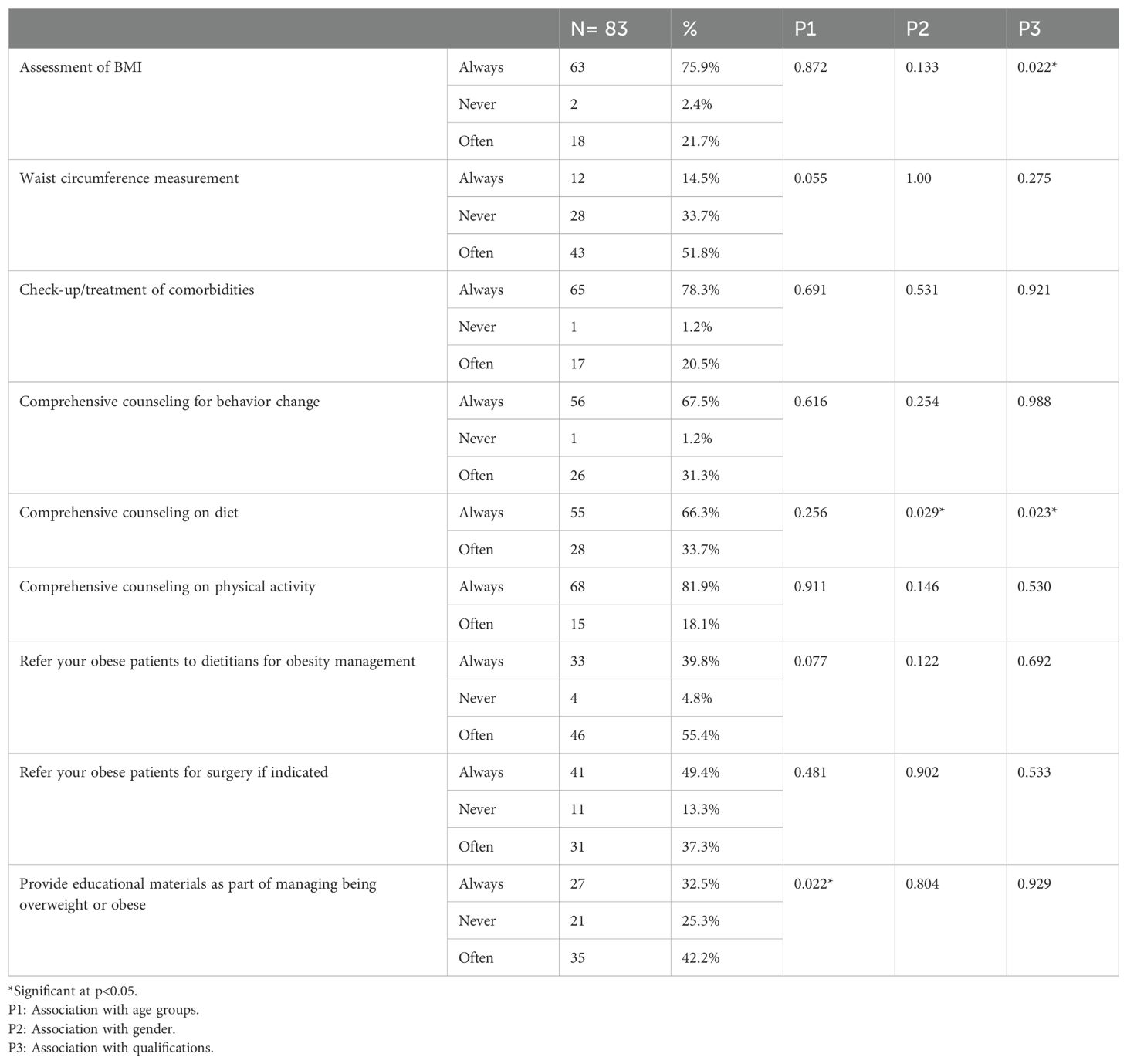
Table 4. Attitudes of family medicine physicians toward risk factors of obesity and barriers to obesity management in Saudi Arabia.
The assessment of obesity counseling practices by family medicine physicians revealed that approximately three-fourths (75.9%) always calculated BMI during obesity management while measuring waist circumference was always performed by 14.5% and often performed by 51.8%. Check-up/treatment of comorbidities was always considered by 78.3% of physicians and was often performed by 20.5%. Comprehensive counseling practices for behavioral change were always provided by 67.5% and were often provided by 31.3%. Comprehensive counseling on diet was either always (66.3%) or often (33.7%) provided, although comprehensive counseling on physical activity was more common (81.9%). The system for providing educational materials as part of managing overweight or obesity was found to be inadequate as 25.3% had never done so. In obesity management, improper practices, such as a high percentage of referrals to dieticians (95.2%) and non-referral of obese patients for surgery when indicated (13.3%), were recorded (Table 5).
Inferential statistics revealed that the assessment of BMI was significantly higher among residents than among registrars and consultants (p=0.022). The practice of comprehensive counseling on diet was significantly higher among residents (p=0.023) and among women (p=0.029). Moreover, providing educational materials as part of managing being overweight or obese was significantly higher among physicians aged less than 35 years than among the older age groups (p=0.022) (Table 5).
Discussion
Obesity is a major public health concern worldwide. Family medicine physicians are the first point of contact for patients and should have sufficient knowledge, attitudes, and beliefs about obesity control (12, 13). This study aimed to assess the practices, knowledge, and beliefs of family physicians regarding the promotion of healthy dietary habits and physical activity among obese or overweight patients in Saudi Arabia.
Our main findings demonstrate that the physicians had positive beliefs regarding obesity management. However, a lack of physician training and poor patient adherence to the management plan were the common barriers to obesity management. Insufficient counseling practices by the family medicine physicians were also noted. Young physicians provided inadequate educational materials for managing obesity.
Female Saudi residents aged less than 35 years with clinical experience of 1-5 or 6-10 years usually examined less than 50 and 50-100 patients per week, respectively. Comparable findings were reported by Alsaati and Almasaodi (14), who evaluated the knowledge, attitudes, and skills of family residents in Makkah regarding obesity. Sebiany (10) included 130 participants, with a mean age of 41 years and an average work experience of 12 years. Young physicians are suitable subjects for training and educational efforts that are intended to improve obesity management (15).
Most of the physicians had sufficient knowledge of the definition of obesity and subsequent obesity-related morbidities, including type 2 diabetes mellitus, cardiovascular diseases, dyslipidemia, polycystic ovary disease, and infertility. However, there was insufficient knowledge regarding the value of weight loss in reducing hepatic inflammation, hepatocellular injury, and fibrosis. Family medicine residents in Makkah were found to have sufficient knowledge of obesity management and the associated comorbidities (14). This could be attributed to the fact that the resident physicians had more recent degrees, updated their knowledge regularly, and had sufficient experience. Furthermore, sufficient knowledge about weight loss may be required to decrease hepatic diseases and could be improved by increasing physicians’ awareness and training regarding the benefits of obesity management (16).
In our study, most of the family medicine physicians believed that obesity is a chronic disease. Furthermore, most physicians had positive beliefs about obesity. They agreed to the necessity of health education for obese patients about the health risks of obesity through the offering of advice about weight control even if the patient does not ask for it, and prescribing weight loss programs. Primary care physicians are the primary point of contact for patients and should identify an obesity case, initiate treatment with lifestyle modifications and obesity drugs, and refer the patient for bariatric surgery when indicated (17). In the present study, the obesity knowledge of the physicians was fair. However, there is still room for improvement, in particular, regarding knowledge of the role of weight loss in the prevention of metabolic-associated fatty liver disease and polycystic ovary syndrome, and in dyslipidemia screening. In addition, nearly one-third of the family physicians did not view obesity as a chronic disease, 32.5% advised weight control only when asked by the patients, and 38.5% felt incompetent in prescribing weight loss programs to obese patients. Counseling regarding obesity treatment, the inclusion of lifestyle interventions and other effective obesity drugs such as glucagon-like receptor-1 agonists, and referring patients for bariatric surgery are vital and should be enforced by including them in the medical curriculum and through continuous education. Primary care physicians need to adhere to the guidelines for obesity management using a multidisciplinary approach. Importantly, Asian people are at higher risk of the development cardiovascular disease at a lower body mass index compared to the Western population (18, 19).
Several Saudi studies have reported similar findings to ours (14, 20, 21). In Norway (22), most general practitioners said that it was their responsibility to manage adults with obesity, and felt secure doing so. However, a Swedish study (23) showed a paradoxical attitude toward obesity among physicians. Although Swedish physicians were able to help obese individuals, most agreed that it was the patient’s obligation to lose weight. Another Swedish study (24) stated that physicians felt frustrated when trying to help obese individuals and referred them to undergo bariatric surgery. These discrepancies in physicians’ beliefs and attitudes can be attributed to the differences in populations and cultures.
In this study, the family medicine physicians believed that physical inactivity, endocrine disorders, genetic factors, overeating, and a high-fat diet are the most frequent risk factors for obesity. These factors can alter the ability of the hypothalamus to regulate one’s appetite, leading to increased hunger or delayed satiety (25). Similarly, Sebiany (10) and Khalifa et al. (26) reported that Saudi physicians are aware of the risk factors for obesity. The main constraints on obesity management in our study were related to the healthcare system and patient factors. In addition, a lack of training and poor patient compliance with management plans were the most common barriers reported in several studies (13, 19, 20, 25). Patient non-compliance could be explained by cultural, social, or psychological factors. Swedish primary care physicians stated that a lack of time and resources during doctor-patient consultations was the biggest barrier to discussing weight loss management with their patients (23). Meanwhile, an American study (27) revealed that the biggest obstacles to treating obesity were a lack of physician confidence and a lack of patient drive. These different barriers may be related to the different populations studied.
Assessment of BMI was significantly associated with qualification level. Registrants and consultants may be involved in other tasks, such as research or education of medical students, and may be up-to-date on recent guidelines. Residents may have insufficient time to check recent guidelines (28). A BMI assessment is recommended for the diagnosis and evaluation of obesity (29). Improper practices were reported regarding waist circumference measurement and non-referral of obese patients to dietitians or surgery when indicated. In Makkah, most physicians did not diagnose a patient as being overweight or obese based on waist circumference (14). Our study supported the previous findings because only a minority of the primary care physician measured the waist circumference of their patients, putting them at high risk of cardiovascular disease and mortality (30). The lower rate of waist circumference measurement is in line with a previous study. Waist circumference is a simple measurement that predicts cardiovascular disease and diabetes mellitus development and the inclusion of it in routine obesity management is encouraged (31).
Moreover, comprehensive counseling on diet was significantly higher among female physicians and was correlated with qualification level. Similarly, Foster et al. (32) reported that women had suitable attitudes and practices toward obesity management compared to men. Ferrante et al. (33) found no gender differences in physicians’ attitudes toward obesity management. In our study, young physicians provided inadequate educational materials for managing being overweight or obese. The finding that 25.3% of the physicians had never provided educational materials as part of obesity management is concerning as educational material is a promising intervention in obesity prevention (34). Plausible explanations could be a lack of available materials, insufficient training, or time constraints. Thus, training courses and providing educational materials are highly recommended. Furthermore, this could be explained by a lack of training and knowledge regarding recent guidelines. In contrast to our findings, Carrasco et al. (23) reported that young Swedish physicians had more recent training and were more knowledgeable about guidelines.
Our findings suggest that young family medicine physicians should receive training and education on obesity-related concerns to address obesity more successfully. Moreover, family medicine residents act as a bridge between different services for managing obesity and helping physicians analyze patients’ weight and health in relation to their weight status (35). Creating interdisciplinary teams for managing obesity and connecting family medicine residents to a wider array of other healthcare experts and programs would be helpful in obesity management.
Limitations
The subjectivity of the self-administered questionnaire and the possibility that family medicine physicians discussed the findings among themselves represent the limitations of the current study. The sample is limited to family physicians in Tabuk, which may not reflect practices in other regions of the country. Variations in healthcare access, resources, and patient demographics across different regions could significantly impact the generalizability of the findings. Furthermore, larger, multicenter studies combining surveys with interviews or observational data are required. Improving the infrastructure within which family physicians operate and more comprehensive obesity management programs and patient follow-up systems are highly recommended.
Conclusion
The family medicine physicians in Tabuk City have adequate knowledge about obesity and positive attitudes toward obesity management. However, their counseling practices were poor. The main obstacles to controlling obesity are a lack of training and poor patient adherence to the management plan. Training courses and the inclusion of obesity management in medical training is highly recommended.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics statement
This study was approved by the Ethics Committee of the University of Tabuk in Tabuk, Saudi Arabia. RB Protocol No: UT-163-51-2022. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
AA: Project administration, Supervision, Writing – original draft. MAla: Data curation, Investigation, Validation, Writing – review & editing. MAlm: Data curation, Formal analysis, Investigation, Methodology, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The authors extend their appreciation to the Deanship of Scientific Research at the University of Tabuk for funding this study under research number (S-1440-0289).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Habbab RM, Bhutta ZA. Prevalence and social determinants of overweight and obesity in adolescents in Saudi Arabia (2020): A systematic review. Clin Obes. 10:e12400. doi: 10.1111/cob.12400
2. Boutari C, Mantzoros CS. A 2022 update on the epidemiology of obesity and a call to action: as its twin COVID-19 pandemic appears to be receding, the obesity and dysmetabolism pandemic continues to rage on. Metabolism. (2022) 133:155217. doi: 10.1016/j.metabol.2022.155217
3. Al-Omar HA, Alshehri A, Abanumay A, Alabdulkarim H, Alrumaih A, Eldin MS, et al. The impact of obesity in Saudi Arabia: healthcare resource use and costs associated with obesity-related complications. Adv Ther. (2023) 40:1430–43. doi: 10.1007/s12325-023-02426-z
4. Alahmed Z, Lobelo F. Physical activity promotion in Saudi Arabia: A critical role for clinicians and the health care system (2018). J Epidemiol Glob Health. 7 Suppl 1:S7–S15. doi: 10.1016/j.jegh.2017.10.005
5. Afif WFB. A systematic review of the impact of lifestyle intervention on childhood obesity. EC Paediatrics. (2017) 3:447–56.
6. Alfadda AA, Al-Dhwayan MM, Alharbi AA, Al Khudhair BK, Al Nozha OM, Al-Qahtani NM, et al. The Saudi clinical practice guideline for the management of overweight and obesity in adults. Saudi Med J. (2016) 37:1151. doi: 10.15537/smj.2016.10.14353
7. Alotaibi T. Combating Overweight and Obesity among School Children and Adolescents through Student Counselling in Saudi Arabia. Eur J Multidiscip Stud. (2017) 6:252–60. doi: 10.26417/ejms.v6i1.p252-260
8. Ghoraba MA, Shiddo OA, Almuslmani M, Jallad I, Khan A, Maranan G, et al. Prevalence of prediabetes in family and community medicine department, security forces hospital, Riyadh, Saudi Arabia. Int J Med Sci Public Health. (2016) 5:777–84. doi: 10.5455/ijmsph.2016.11122015277
9. Epling JW, Morley CP, Ploutz-Snyder R. Family physician attitudes in managing obesity: a cross-sectional survey study. BMC Res Notes. (2011) 4:473. doi: 10.1186/1756-0500-4-473
10. Sebiany AM. Primary care physicians' knowledge and perceived barriers in the management of overweight and obesity. J Family Community Med. (2013) 20:147–52. doi: 10.4103/2230-8229.121972
11. Schwenke M, Luppa M, Pabst A, Welzel FD, Löbner M, Luck-Sikorski C, et al. Attitudes and treatment practice of general practitioners towards patients with obesity in primary care. BMC Fam Pract. (2020) 21:169. doi: 10.1186/s12875-020-01239-1
12. Bardia A, Holtan SG, Slezak JM, Thompson WG. Diagnosis of obesity by primary care physicians and impact on obesity management. Mayo Clinic Proc. (2007) 82:927–32. doi: 10.4065/82.8.927
13. Sharaf SE, Al-shalabi BT, Althani GF, Bazuhair HM, FaIraq BJ, Ali FA, et al. Obesity self-management: knowledge, attitude, practice, and pharmaceutical use among healthy obese individuals in Saudi Arabia. Int J Family Community Med. (2021) 5:110–21. doi: 10.15406/ijfcm.2021.05.00232
14. Alsaati O, Almasaodi K. Knowledge, Attitude and Practices about Obesity Management among Saudi Board of Family Medicine Residents in Makkah Al-Mukarramah: A Cross-sectional Study. Am J Med Sci Med. (2020) 8:134–43. doi: 10.12691/ajmsm-8-3-6
15. Sanchez-Ramirez DC, Long H, Mowat S, Hein C. Obesity education for front-line healthcare providers. BMC Med Educ. (2018) 18:278. doi: 10.1186/s12909-018-1380-2
16. Dicker D, Kornboim B, Bachrach R, Shehadeh N, Potesman-Yona S, Segal-Lieberman G. ACTION-IO as a platform to understand differences in perceptions, attitudes, and behaviors of people with obesity and physicians across countries - the Israeli experience. Israel J Health Policy Res. (2020) 9:56. doi: 10.1186/s13584-020-00404-2
17. Guglielmi V, Capoccia D, Russo B, Lubrano C, Mariani S, Poggiogalle E, et al. Knowledge, experiences, and perceptions relating to obesity management among primary care physicians in the Lazio Region, Italy. Front Endocrinol (Lausanne). (2023) 14:1249233. doi: 10.3389/fendo.2023.1249233
18. Bischoff SC, Boirie Y, Cederholm T, Chourdakis M, Cuerda C, Delzenne NM, et al. Towards a multidisciplinary approach to understand and manage obesity and related diseases. Clin Nutr. (2017) 36:917–38. doi: 10.1016/j.clnu.2016.11.007
19. Ogawa W, Hirota Y, Miyazaki S, Nakamura T, Ogawa Y, Shimomura I, et al. Definition, criteria, and core concepts of guidelines for the management of obesity disease in Japan. Endocr J. (2024) 71:223–31. doi: 10.1507/endocrj.EJ23-0593
20. Al-Khaldi Y, Melha WA, Al-Shahrani A, Al-Saleem S, Hamam M. Knowledge, attitude and practice of primary health care physicians in Aseer region regarding obesity. Saudi J Obes. (2014) 2:54. doi: 10.4103/2347-2618.147343
21. Alshammari Al-Shammari YfYF. Attitudes and practices of primary care physicians in the management of overweight and obesity in eastern Saudi Arabia. Int J Health Sci. (2014) 8:151–8. doi: 10.12816/0006081
22. Martins C, Norsett-Carr A. Obesity knowledge among final-year medical students in Norway. Obes facts. (2017) 10:545–58. doi: 10.1159/000481351
23. Carrasco D, Thulesius H, Jakobsson U, Memarian E. Primary care physicians’ knowledge and attitudes about obesity, adherence to treatment guidelines and association with confidence to treat obesity: a Swedish survey study. BMC primary Care. (2022) 23:208. doi: 10.1186/s12875-022-01811-x
24. Memarian E, Carrasco D, Thulesius H, Calling S. Primary care physicians’ knowledge, attitudes and concerns about bariatric surgery and the association with referral patterns: a Swedish survey study. BMC endocrine Disord. (2021) 21:62. doi: 10.1186/s12902-021-00723-8
25. Lin X, Li H. Obesity: epidemiology, pathophysiology, and therapeutics. Front Endocrinol. (2021) 12:706978. doi: 10.3389/fendo.2021.706978
26. Khalifa A, Alanazi M, Alotaibi A, Aldaham A, Dahham A, Qabaja AR, et al. Obesity and associating factors: a cross-sectional study in Riyadh, Saudi Arabia. Int J Diabetes Developing Countries. (2020) 4:417–22. doi: 10.24911/IJMDC.51-1576386160
27. Harris IM, McNeilly H, Benamer H, Ward DJ, Sitch AJ, Parry J. Factors affecting consultant attitudes to undertaking undergraduate medical student teaching in the UK: a systematic review. BMJ Open. (2021) 11:e042653. doi: 10.1136/bmjopen-2020-042653
28. Salinas GD, Glauser TA, Williamson JC, Rao G, Abdolrasulnia M. Primary care physician attitudes and practice patterns in the management of obese adults: results from a national survey. Postgraduate Med. (2011) 123:214–9. doi: 10.3810/pgm.2011.09.2477
29. Semlitsch T, Stigler FL, Jeitler K, Horvath K, Siebenhofer A. Management of overweight and obesity in primary care-A systematic overview of international evidence-based guidelines. Obes Rev. (2019) 20:1218–30. doi: 10.1111/obr.12889
30. Liu S, Yu J, Wang L, Zhang X, Wang F, Zhu Y. Weight-adjusted waist index as a practical predictor for diabetes, cardiovascular disease, and non-accidental mortality risk. Nutr Metab Cardiovasc Dis. (2024) 34:2498–510. doi: 10.1016/j.numecd.2024.06.012
31. Ross R, Neeland IJ, Yamashita S, Shai I, Seidell J, Magni P, et al. Waist circumference as a vital sign in clinical practice: a Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat Rev Endocrinol. (2020) 16:177–89. doi: 10.1038/s41574-019-0310-7
32. Foster GD, Wadden TA, Makris AP, Davidson D, Sanderson RS, Allison DB, et al. Primary care physicians’ attitudes about obesity and its treatment. Obes Res. (2003) 11:1168–77. doi: 10.1038/oby.2003.161
33. Ferrante J, Piasecki A, Ohman-Strickland P, Crabtree B. Family physicians’ Practices and attitudes regarding care of extremely obese patients. Obes (Silver Spring Md). (2009) 17:1710–6. doi: 10.1038/oby.2009.62
34. Thomas K, Löf M, Lundgren M, Fagerström M, Hesketh KD, Brown V, et al. MINISTOP 3.0: Implementation of a mHealth obesity prevention program within Swedish child healthcare - study protocol for a cluster randomized controlled trial. BMC Public Health. (2024) 24:2594. doi: 10.1186/s12889-024-20137-0
Keywords: obesity, knowledge, beliefs, practice, family physicians
Citation: Alatawi AM, Alanazi MA and Almohammadi MA (2024) Family physicians’ knowledge, beliefs, and practices in promoting healthy lifestyles and weight management for obese patients in Tabuk, Saudi Arabia. Front. Endocrinol. 15:1456086. doi: 10.3389/fendo.2024.1456086
Received: 28 June 2024; Accepted: 29 October 2024;
Published: 22 November 2024.
Edited by:
Alexandre Gabarra Oliveira, São Paulo State University, BrazilReviewed by:
Maria João Lima, Instituto Politecnico de Viseu, PortugalAureliusz Kosendiak, University of Lower Silesia, Poland
Copyright © 2024 Alatawi, Alanazi and Almohammadi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Amirah M. Alatawi, QW0uYWxhdGF3aUB1dC5lZHUuc2E=
†ORCID: Amirah M. Alatawi, orcid.org/0000-0003-4638-9990
Mansuor A. Alanazi, orcid.org/0000-0002-7256-6033
 Amirah M. Alatawi
Amirah M. Alatawi Mansuor A. Alanazi1†
Mansuor A. Alanazi1†