- 1Department of Pediatrics, Division of Endocrinology and Diabetes, Washington University School of Medicine, Saint Louis, MO, United States
- 2Washington University School of Medicine, Saint Louis, MO, United States
- 3Department of Medicine, Division of Endocrinology, Diabetes, and Lipid Research, Washington University School of Medicine, Saint Louis, MO, United States
- 4Center for Biostatistics and Data Science, Washington University School of Medicine, Saint Louis, MO, United States
- 5Department of Psychiatry, Washington University School of Medicine, Saint Louis, MO, United States
- 6Department of Surgery, Division of Public Health Sciences, Washington University School of Medicine, Saint. Louis, MO, United States
Background: The National Academy of Medicine has formally identified transgender adults as an understudied population in critical need of health research. While national surveys, like the US Transgender survey, have characterized higher rates of depression, anxiety, suicidality and socioeconomic need in the transgender community, studies have not examined the impact of sociodemographic and clinical characteristics on mental health related outcomes.
Objective: To describe the sociodemographic and mental health characteristics of transgender adults seen at a large Midwest transgender clinic and to determine factors associated with self-reported mental health conditions.
Methods: Descriptive, retrospective, cross-sectional study of new transgender patients 18 years and older seen at a large Midwest transgender clinic between December 2019 and June 2022.
Results: A total of 482 charts were reviewed. During their initial evaluation, 11.6% (56/482) reported having a history of suicide attempt and 81.3% (392/482) reported a mental health diagnosis with the most common being depression, anxiety, attention deficit disorder, and post-traumatic stress disorder. Multivariable logistic regression results show no single factor was significantly associated with mental health diagnosis after adjusting for the effect of age and race. Patients who were new to gender affirming hormone therapy (54%, 254/468) are 2.0 (95% CI 1.4-2.9) times more likely to report having a mental health care provider than patients who were seen for continuation of therapy (46%, 214/468). Ten records with race not disclosed, 3 records with gender identity “other” and 2 records with gender identity not disclosed were excluded from analysis.
Conclusion: This study reinforces the finding that transgender adults have an increased lifetime prevalence of mental health conditions. The higher prevalence of mental health conditions in our clinic was not associated with sociodemographic factors included in the study. Furthermore, transgender patients are less likely to have seen mental healthcare providers after initiation of gender affirming hormone therapy.
Introduction
Transgender individuals experience discordance between their gender identity and their sex assigned to them at birth (1–3). Some transgender individuals experience gender dysphoria (GD), which the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) defines as “clinically significant distress or impairment in social, occupational, or other key areas of functioning.” GD affects psychosocial development and has been associated with psychiatric conditions like depression and suicidal ideation (4–6).
Despite this knowledge and having a large body of literature characterizing psychiatric diagnosis in various subsets of the U.S. cisgender population, there is a paucity of data quantifying the prevalence of psychiatric diagnosis and its burden in the adult transgender population (7).
Studies using self-reports of gender identity and its variants suggest that 0.17% to 1.3% of young adults identify as transgender (8). Even using the conservative estimate of 0.3%, the number of people living in the United States who identify as transgender is nearly 1 million (9).
The National Academy of Medicine has identified transgender adults as an understudied population in critical need of health research (10). Research in transgender adults is critical because they are particularly vulnerable to the impact of these stressors including governmental policies limiting participation in sports or access to gender affirming hormone therapy (GAHT) (11), employment discrimination leading to lack of health insurance, and refusal of health care services which would affect their socioeconomic outcomes (12–14). Socioeconomic status is associated with a number of health related outcomes (15), and it is important to understand the impact of socioeconomic status on the mental health outcomes in transgender individuals (16, 17).
Our study aims to address this knowledge gap by describing the sociodemographic and mental health characteristics of a sample of transgender adults establishing care at a Midwest tertiary medical center transgender clinic. We also describe factors associated with general mental health, including self- report of a mental health diagnosis, being prescribed psychotropic medications, and/or being seen by a licensed behavioral health professional.
Methods
This is a descriptive, retrospective, cross-sectional study. Participants included transgender patients 18 years and older seen at initial visits at the Washington University Adult Transgender Center in St. Louis, MO between December 2019 and June 2022. Patients were classified in two groups: (1) new to GAHT and (2) those continuing GAHT. The adult transgender center follows the informed consent model in which patients are placed at the center of the decision-making process (18).
While longitudinal data were collected, this analysis reports cross-sectional data at baseline. The Institutional Review Board of Washington University in St. Louis approved this research; IRB ID 202202153 in February of 2022.
Study procedures
All data were extracted from the electronic health record (Epic) into a de-identified Research Electronic Data Capture (REDCap) database. The population of interest was identified using Slicer Dicer to select patients 18 years of age and older having “transgender new” as visit type and department of endocrinology as department between December 1, 2019, and June 30, 2022. Two members of the study team extracted all data (EB, DM). Additional study team members (DM, SC) performed quality assurance on 10% of collected data by verifying collected data against medical record. A separate key linking study identifier to medical record number and protected health information was kept in a password protected file on a secure server. Data extracted from the medical record at each participant’s initial visit included:
1. Demographic data: age, race, ethnicity, sex assigned at birth, gender identity, primary and secondary health insurance, and Zip code of residency to obtain area of deprivation index.
2. Psychiatric history: Self-reported mental health diagnoses, mental health history including suicidal attempts, mental health providers defined as psychiatrist or therapist and seen over the last year, psychotropic medications prescribed, previous mental health admissions, community referrals provided in clinic.
3. Medical history: Self-reported medical diagnoses, primary care provider, referral from the pediatric center, gender-affirming treatment regimens, interest in and referrals made for gender-affirming surgery, and use of tobacco/nicotine products. The variable assessing whether an individual was referred from a pediatric transgender care provider in our health system is important because comprehensive, multidisciplinary psychosocial evaluation including mental health evaluation was required for all individuals in the pediatric center, per WPATH guidelines for adolescent transgender care. Individuals presenting for care for the first time as adults were evaluated through the informed consent model and were not required to have seen a mental health professional, also per WPATH guidelines.
Information on health insurance was collected because the health care system in the US can be defined as a mixed system of public payers (insurance plans that are funded by federal or state government for individuals with limited financial resources or high health care needs) (19), private insurance, and individual payments (self-pay). Studies have found positive and significant effects of health insurance coverage on a range of health outcomes (20–23). We further divided those with health insurance coverage between those with primary and secondary health insurance. Primary health insurance is the first to pay for medical-related expenses. Secondary health insurance covers all or part of the expenses not covered by the primary health insurance plan; for example, some private insurers offer supplementary plans to cover out-of-pocket costs like deductibles and co-pays that are not covered by the primary insurer.
The area of deprivation index (ADI) was obtained through the neighborhood atlas organized by the University of Wisconsin using U.S. Census Bureau geographies. ADI is associated with an individual’s block group or neighborhood and measures poverty, education, housing, and employment status to provide a factor-based index used as a proxy measure of socioeconomic deprivation (24, 25). The national percentile divides ADI score into 100 equal sections, categorizing the individual block neighborhood, with those in the first percentile being the least disadvantaged and those in the hundredth percentile being the most disadvantaged.
Statistical analysis
Data are presented as median and interquartile range for continuous data that was not normally distributed, and frequency with percentage for categorical data. The association between gender identities and categorical factors were examined using Chi-square or Fisher’s exact test as appropriate. Primary outcomes of interest were defined dichotomously as 1) reporting a mental health diagnosis and 2) reporting a visit to a mental health provider over the last year. Multivariable logistic regression models were performed to assess the association between sociodemographic and clinical factors and these primary outcomes with age and race as covariates. Odds ratio (OR) values and their respective confidence interval (CI) were estimated. Ten records where race was not disclosed, 3 records where gender identity was reported as “other” with no further information and 2 records where gender identity was not disclosed were excluded from multivariable logistic regression analysis. All analyses were performed using SAS version 9.4 (SAS Institute Inc, Cary, NC). A p-value of less than or equal to 0.05 was used to determine statistical significance.
Results
A total of 482 charts were reviewed during the study period. The sample had a median age of 24 years and ranged from 18 years to 75 years of age with 46% identifying as transgender women, 38% as transgender male, and 16% as non-binary. Individuals were predominantly white, non-Hispanic (n=433, 89.8%). More than 92.7% had primary health insurance; 17.9% had Medicare or Medicaid versus 72.6% with private insurance and 9.5% of the total sample had secondary health insurance (Table 1).
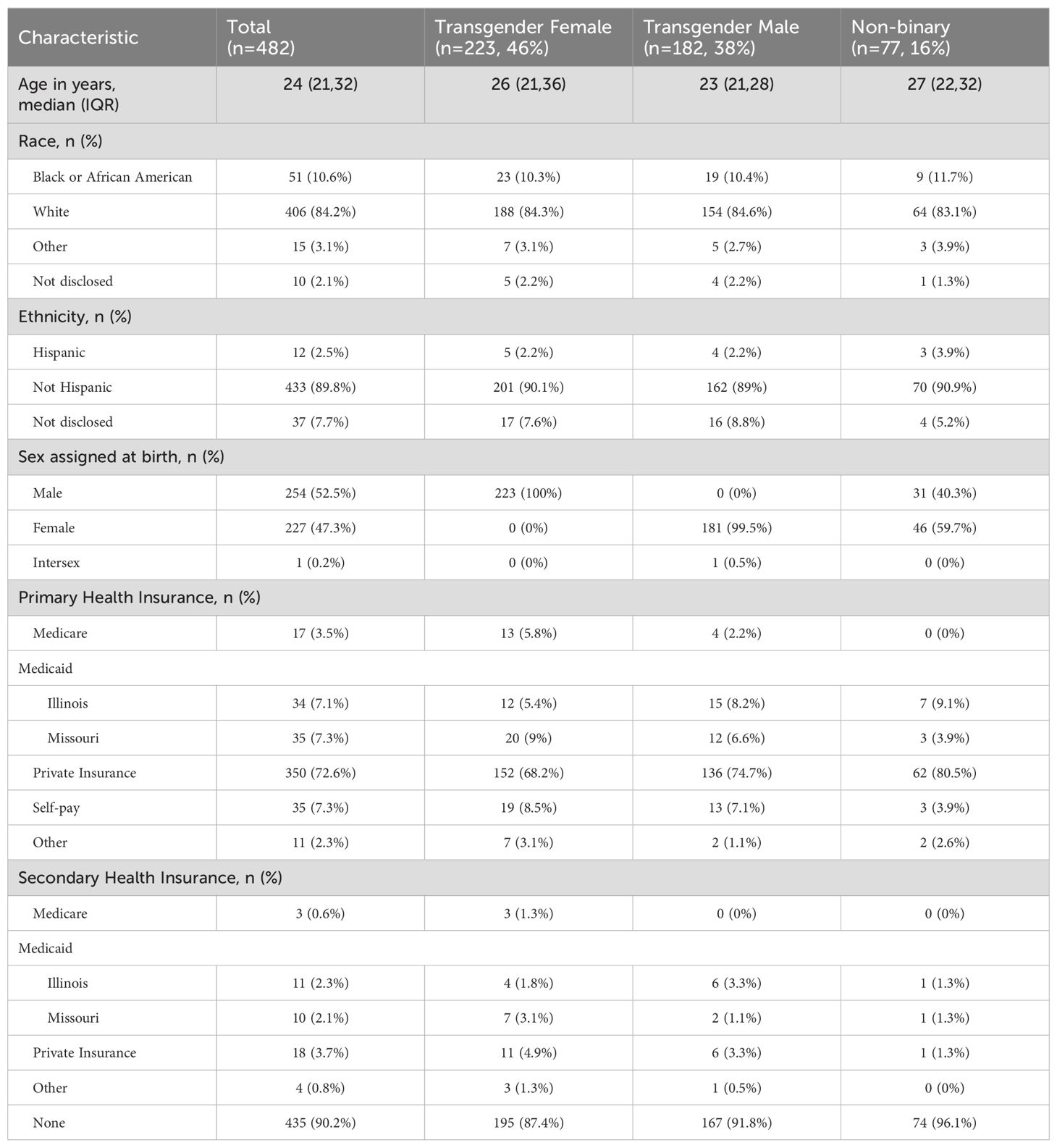
Table 1. Baseline sociodemographic characteristics of transgender patients seen at a Midwest tertiary medical center.
Area of deprivation index
This study used the national and state ADI. Out of the total sample of 482, we were able to obtain ADI on 451 transgender individuals. The sample studied had a mean national ADI percentile of the 59th percentile. Ten percent of all transgender patients were in the lower quartile of the national ADI (<25th percentile) or least disadvantaged quartile, in comparison to 30% being the top quartile (>75th percentile) or most disadvantaged quartile (Figure 1).
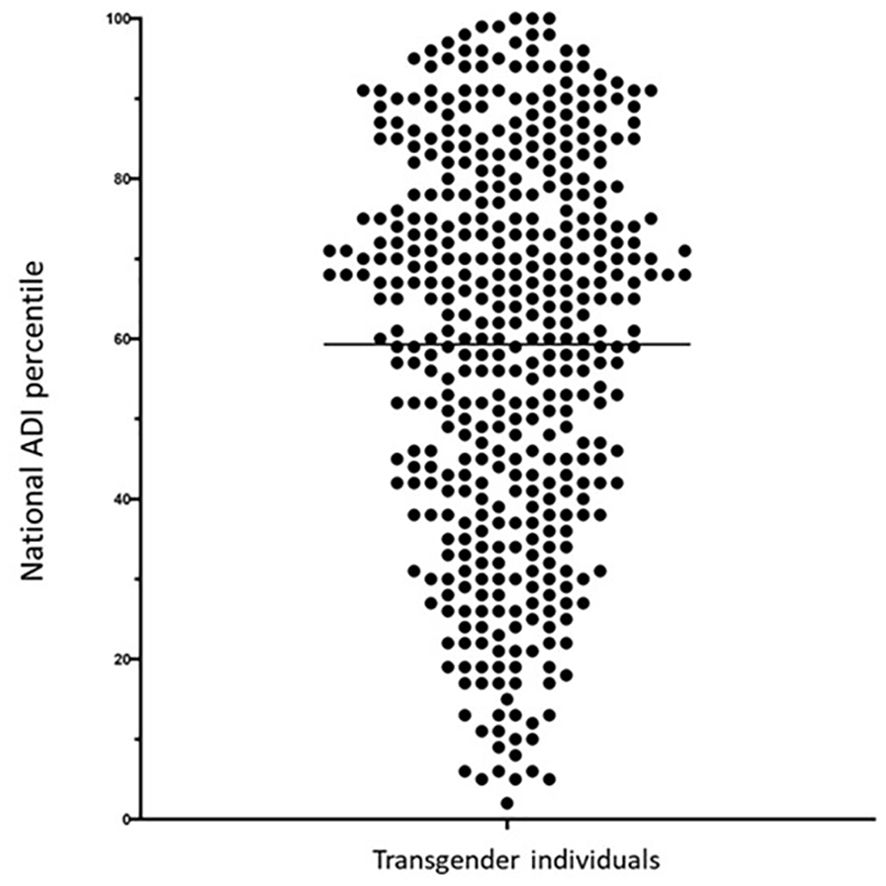
Figure 1. National area of deprivation index percentile of transgender patients seen at an academic center in the Midwest between December 2019 and June 2022. Each circle represents a transgender patient at a national ADI percentile and solid line represent the mean of the sample. The population increases as the national percentile increases to the most disadvantage percentiles.
The state ADI is presented in deciles. A decile groups the ADI score into 10 equal sections, following the same interpretation as the national ADI score percentile. In our sample, we obtained a mean state ADI decile of 5 with approximately 16% of patients in the 1st state ADI decile and about 6% in the 10th state ADI decile (Figure 2).
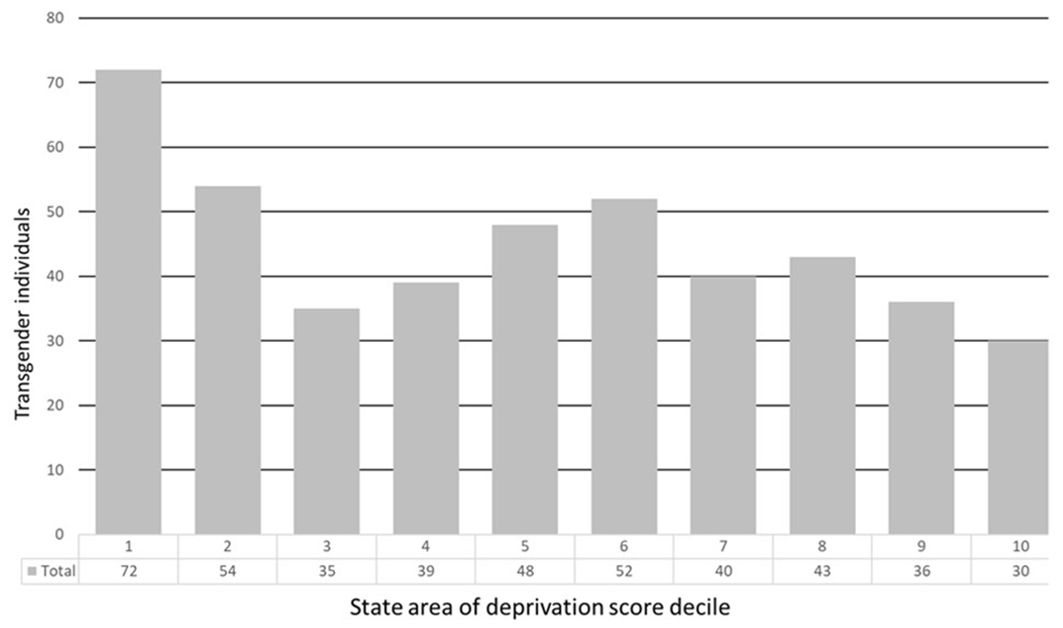
Figure 2. State area of deprivation index decile of transgender patients seen at an academic center in the Midwest between December 2019 and June 2022.
Clinical characteristics
Even though more than 90% of patients had primary insurance, less than half of them had a psychiatrist or therapist and about two thirds reported having a primary care physician, indicating the multidimensional complexity in accessing health care that is not solely dependent in health insurance coverage. Also, 11.6% reported having a history of suicide attempt during their initial evaluation (Table 2).
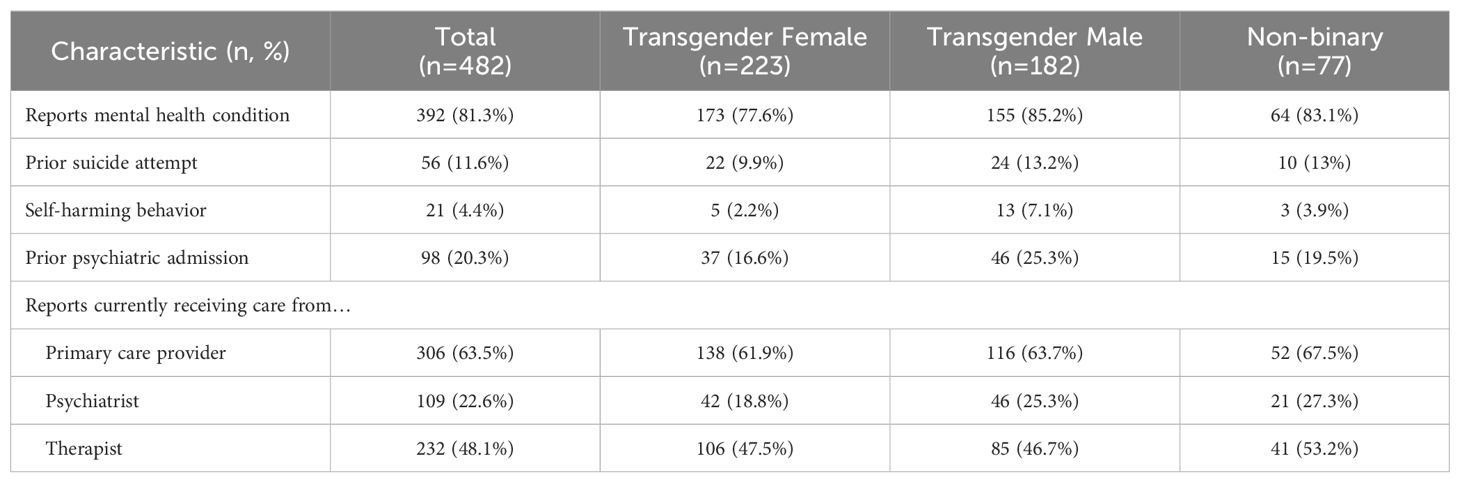
Table 2. Baseline self-reported mental health history of transgender patients seen at a Midwest tertiary medical center.
Eighty percent of the patients reported a mental health diagnosis with the most common diagnoses being depression (n=320, 66.4%), any anxiety disorder (n= 278, 57.7%), and attention deficient hyperactivity disorder ADHD (n= 83, 17.2%) (Table 3). Use of psychotropic medications serves as another measure of prevalence of mental health conditions. At their initial patient visit, 48.5% reported a psychotropic medication (Table 4). The most common groups of psychotropic medications reported were selective serotonin reuptake inhibitor (SSRI), anxiolytics, and ADHD medications. Among the category other psychotropic medications, the most reported were bupropion (n=22, 4%) and trazadone (n=10, 2%).
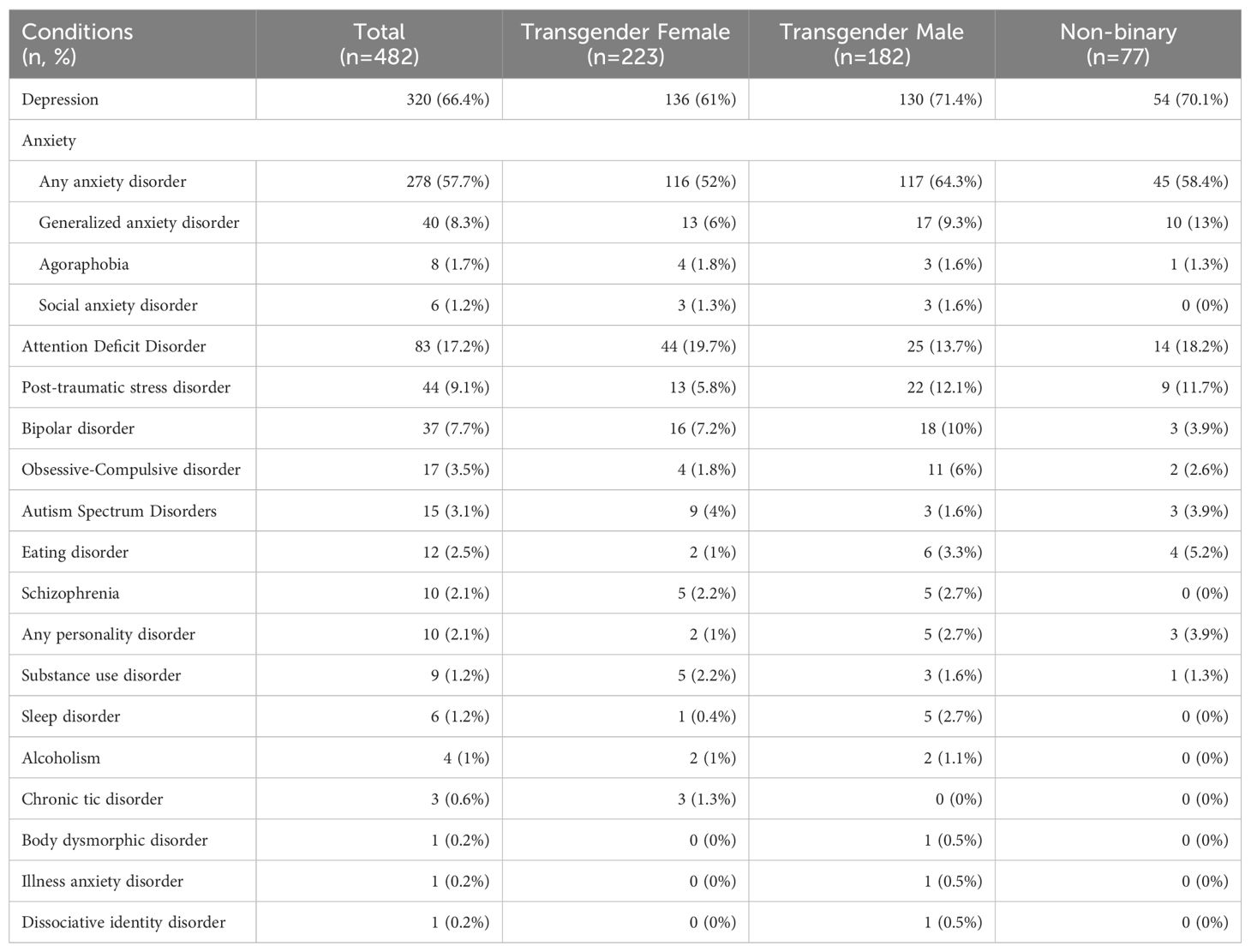
Table 3. Baseline self-reported mental health conditions of transgender patients seen at a Midwest tertiary medical center.
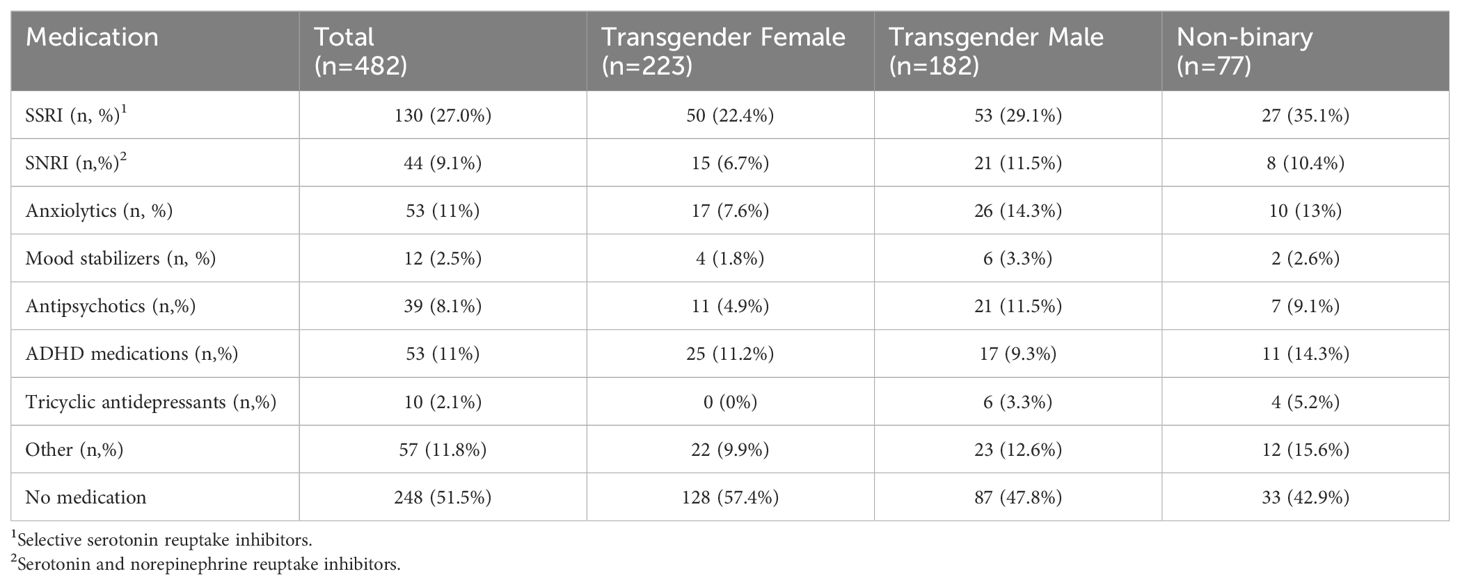
Table 4. Baseline psychotropic medications reported by transgender patients seen at a Midwest tertiary medical center.
After their initial evaluation, the GAHT regimen most commonly prescribed to transgender females was sublingual 17-beta estradiol co-prescribed with spironolactone as an androgen blocker. The GAHT regimen most commonly prescribed to transgender males was intramuscular or subcutaneous testosterone (Table 5).

Table 5. Gender affirming hormone therapy prescribed to transgender patients seen at a Midwest tertiary medical center during their initial visit.
Effect of medical and sociodemographic factors on self-reported mental health diagnosis
A multivariable logistic regression model was constructed to assess associations between self-reported mental health diagnosis and medical and sociodemographic factors including gender identity, primary health insurance, initiation or continuation of GAHT, referral from the Pediatric Center, and the Area of Deprivation Index corresponding to the individual’s zip code or residence at a state and national level. The covariates that were included in the model were age and race. Logistic regression results (Table 6) show none of the factors was significantly associated with self-reported mental health diagnosis during the initial visit.
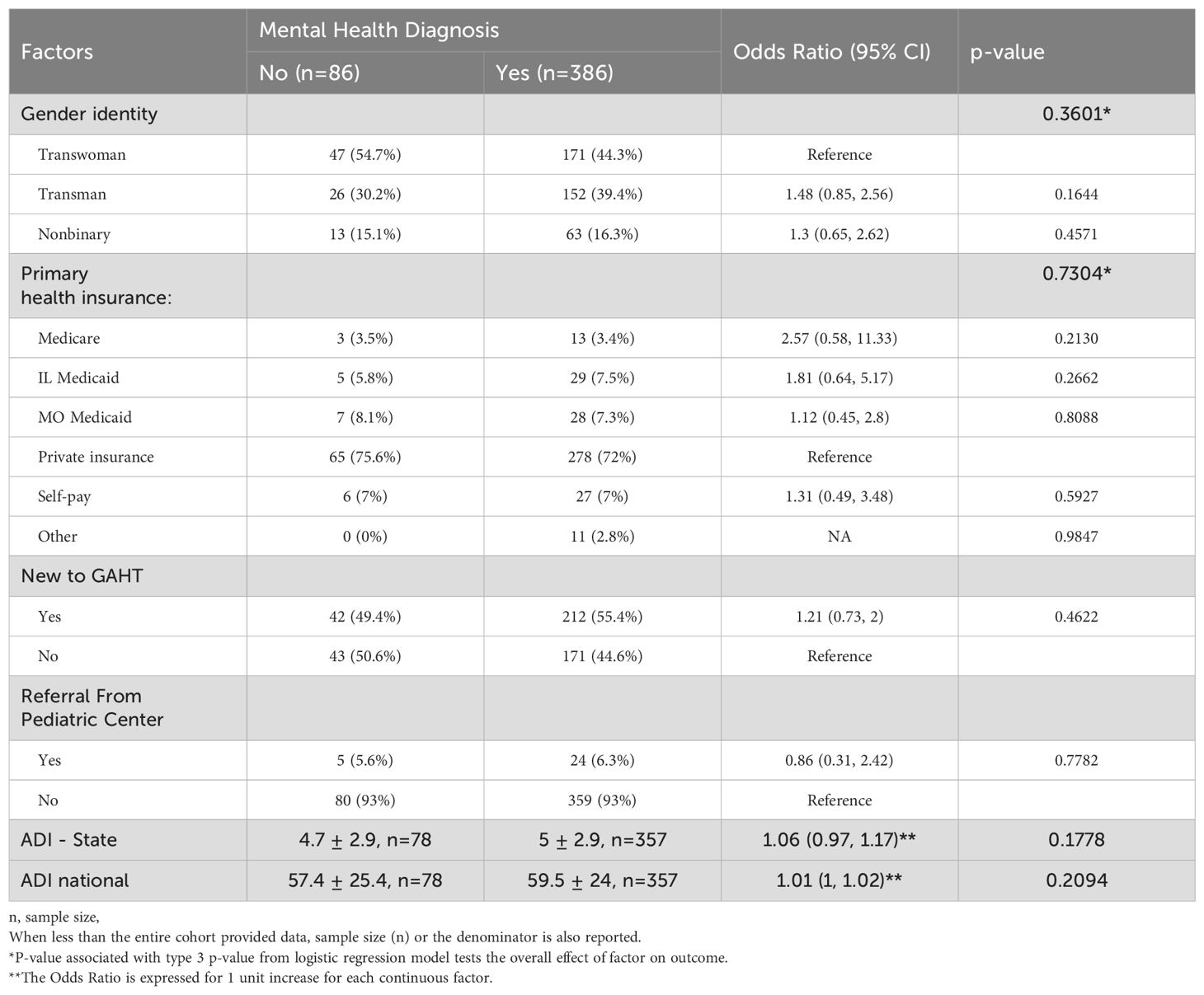
Table 6. Effect of factors on mental health diagnosis after adjusting for the effect of age and race in transgender patients seen at a Midwest tertiary medical center.
Effect of medical and sociodemographic factors on having a mental health care provider
A multivariable logistic regression model was constructed to assess associations between having a mental health care provider with medical and sociodemographic factors including gender identity, primary health insurance, initiation, or continuation of GAHT, referral from the Pediatric Center, and the Area of Deprivation Index corresponding to the individual’s zip code of residence at a state and national level. The covariates that were included in the model were age and race. Logistic regression results (Table 7) show patients who were new to GAHT were more likely to report having a mental health care provider in the adjusted model (aOR 2.0, 95% CI 1.4-2.9).
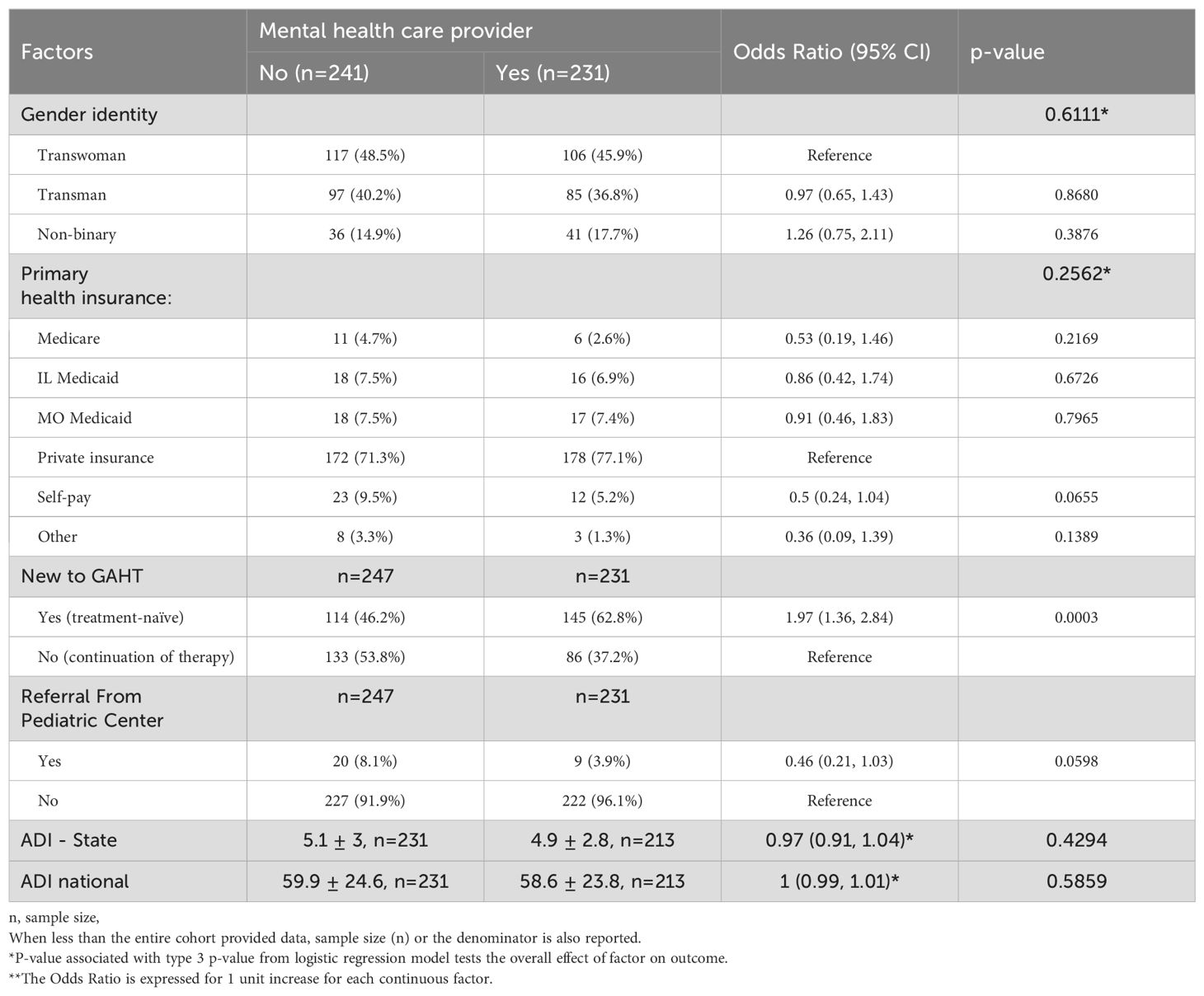
Table 7. Effect of factors on having a mental health care provider in transgender patients seen at a Midwest tertiary medical center.
Discussion
Research in transgender adults has been recognized as an understudied area, hence, the importance of this study characterizing sociodemographic factors and mental health diagnosis in transgender adults seen at a Midwest academic center. It also provides a unique perspective on the impact of sociodemographic factors in history of mental health diagnosis and access to a mental health provider. Among the sociodemographic factors, we included the state and national area of deprivation index to provide a consistent and standardized measure that might be difficult to capture in clinical settings (24).
Our study found transgender individuals seen in our clinic have a 81% life-time prevalence of mental health conditions with depression and anxiety being the most common, with a life-time self-reported prevalence of 66.4% and 57.7% respectively. Our results are similar to those described in a US cross-sectional study of 25,233 transgender inpatient encounters (10), which showed that 76.7% of all transgender inpatient encounters had at least one mental health disorder diagnosis, and these hospital encounters were more than 3 times as likely to have a mood disorder diagnosis than cisgender inpatient encounters. These results extend observations from the multicenter European Network for the Investigation of Gender Incongruence study showing that 70% of transgender participants have a life-time prevalence of affective and anxiety disorder (26, 27). For contrast, the lifetime prevalence of depression and anxiety in US adults is 47.6% and 31.1%, respectively (28).
Furthermore, there were no differences in the life-time prevalence of any mental health condition between gender identities nor a relationship between sociodemographic factors and reported history of mental health diagnosis. Prior studies have shown transgender individuals have higher rates of mental health conditions compared to their cisgender peers (29, 30). These findings have been explained by the minority stress model, which refers to the psychosocial stressors that transgender individuals experience on account of their (gender) minority status (31, 32). After adjusting for socio-economic factors, our study findings support the conclusions of prior research that this difference in mental health diagnosis prevalence between transgender and cisgender individuals is, in part, due to gender dysphoria, minority stress and its implications as a proximal stressor (32, 33). Socioeconomic factors were not associated with the prevalence of mental health diagnosis in our sample, while socioeconomic status has been implicated as an important moderator of stress and psychological health outcomes in other populations (34–36) Transgender individuals experience employment and education discrimination in our society which impact socioeconomic status, potentially confounding the relationship between mental health and socioeconomic status in this population.
A growing body of literature shows positive benefits of GAHT on mental health, with the most consistent effects being decreases in depressive symptoms, psychological distress, and potentially reduced general anxiety (37, 38), which could explain why patients who are seen for consultation for initiating GAHT are almost two times more likely to have seen their mental health provider over the last year than those seen for continuation of therapy, and the reason why patients referred for continuation of therapy may be less likely to need ongoing mental health support. In our study population, approximately one in every 8 transgender adults reported a prior suicide attempt during their initial appointment, which is approximately 5 times higher than the lifetime prevalence of suicidal attempts in the general population based on previously-reported data in a US cross-national sample (39).
This study has several important strengths including the large sample size and the description of binary and non-binary gender identities with subsequent analysis for potential differences between the groups. Also, the collection of data included zip codes, allowing the ADI to be utilized as a standardized method for incorporating socioeconomic data (that would be otherwise difficult to obtain from medical records) into our analysis. The study also has some limitations. First, this was a retrospective chart review. Data collection was limited to information that was included in the electronic health record for clinical rather than research purposes. Hence, it is possible that information about visits to mental health care providers and mental health diagnoses were incompletely captured. Information on mental diagnoses was self-reported in many cases and could be partial or limited to the recall of patients during appointments. ADI data capture population level socioeconomic status characteristics and are used as a proxy for individual-level social determinants of health. We recognize that population-level data have limits in this regard and may incompletely represent individual circumstances and needs. Additionally, as a cross-sectional analysis, we can only establish relationships of association and not causal effect between the factors and outcomes studied.
Conclusions
In summary, this study provides insight on the psychosocial characteristics of transgender adults during their initial appointment at a Midwest transgender center. It demonstrates that transgender adults continuing GAHT are less likely to have seen a mental health provider in the prior year than they were before initiating GAHT. We show a lack of relationship between sociodemographic factors and the prevalence of mental health conditions in our study population.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by The Washington University in St. Louis Institutional Review Board. Human Research Protection Office. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
SC: Conceptualization, Data curation, Formal Analysis, Investigation, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. DM: Data curation, Writing – review & editing. EB: Data curation, Writing – review & editing. KW: Writing – review & editing. JW: Formal Analysis, Writing – review & editing. GN: Methodology, Supervision, Writing – review & editing. TB: Supervision, Writing – review & editing. CH: Conceptualization, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work is supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, grant number K23HD096204.
Conflict of interest
CH is a consultant for Teladoc Health.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Unger CA. Hormone therapy for transgender patients. Transl Androl Urol. (2016) 5:877–84. doi: 10.21037/tau
2. Winter S, Diamond M, Green J, Karasic D, Reed T, Whittle S, et al. Transgender people: health at the margins of society. Lancet. (2016) 388:390–400. doi: 10.1016/S0140-6736(16)00683-8
3. Boucher FJO, Chinnah TI. Gender dysphoria: A review investigating the relationship between genetic influences and brain development. Adolesc Health Med Ther. (2020) 11:89–99. doi: 10.2147/AHMT.S259168
4. Kaltiala-Heino R, Bergman H, Työläjärvi M, Frisén L. Gender dysphoria in adolescence: current perspectives. Adolesc Health Med Ther. (2018) 9:31–41. doi: 10.2147/AHMT
5. Kyriakou A, Nicolaides NC, Skordis N. Current approach to the clinical care of adolescents with gender dysphoria. Acta BioMed. (2020) 91:165–75.
6. Cooper K, Russell A, Mandy W, Butler C. The phenomenology of gender dysphoria in adults: A systematic review and meta-synthesis. Clin Psychol Rev. (2020) 80:101875. doi: 10.1016/j.cpr.2020.101875
7. Bockting WO, Miner MH, Swinburne Romine RE, Hamilton A, Coleman Stigma E.. Stigma, mental health, and resilience in an online sample of the US transgender population. Am J Public Health. (2013) 103:943–51. doi: 10.2105/AJPH.2013.301241
8. Connolly MD, Zervos MJ, Barone CJ, Johnson CC, Joseph CL. The mental health of transgender youth: advances in understanding. J Adolesc Health. (2016) 59:489–95. doi: 10.1016/j.jadohealth.2016.06.012
9. Meerwijk EL, Sevelius JM. Transgender population size in the United States: a meta-regression of population-based probability samples. Am J Public Health. (2017) 107:216. doi: 10.2105/AJPH.2016.303578a
10. Hanna B, Desai R, Parekh T, Guirguis E, Kumar G, Sachdeva R. Psychiatric disorders in the U.S. transgender population. Ann Epidemiol. (2019) 39:1–7.e1. doi: 10.1016/j.annepidem.2019.09.009
11. Barbee H, Deal C, Gonzales G. Anti-transgender legislation-A public health concern for transgender youth. JAMA Pediatr. (2022) 176:125–6. doi: 10.1001/jamapediatrics.2021.4483
12. Fredriksen-Goldsen KI, Cook-Daniels L, Kim H-J, Erosheva EA, Emlet CA, Hoy-Ellis CP, et al. Physical and mental health of transgender older adults: an at-risk and underserved population. Gerontologist. (2014) 54(3):488–500. doi: 10.1093/geront/gnt021
13. Hughto JMW, Gunn HA, Rood BA, Pantalone DW. Social and medical gender affirmation experiences are inversely associated with mental health problems in a U.S. Non-probability sample of transgender adults. Arch Sexual Behav. (2020) 49:2635–47. doi: 10.1007/s10508-020-01655-5
14. Reisner SL, Poteat T, Keatley J, Cabral M, Mothopeng T, Dunham E, et al. Global health burden and needs of transgender populations: a review. Lancet. (2016) 388:412–36. doi: 10.1016/S0140-6736(16)00684-X
15. Kivimäki M, Batty GD, Pentti J, Shipley MJ, Sipilä PN, Nyberg ST, et al. Association between socioeconomic status and the development of mental and physical health conditions in adulthood: a multi-cohort study. Lancet Public Health. (2020) 5:e140–9. doi: 10.1016/S2468-2667(19)30248-8
16. Shangani S, Gamarel KE, Ogunbajo A, Cai J, Operario D. Intersectional minority stress disparities among sexual minority adults in the USA: the role of race/ethnicity and socioeconomic status. Cult Health Sex. (2020) 22:398–412. doi: 10.1080/13691058.2019.1604994
17. Baum A, Garofalo JP, Yali AM. Socioeconomic status and chronic stress: does stress account for SES effects on health? Ann New York Acad Sci. (1999) 896:131–44.
18. Chiang T, Bachmann GA. The informed consent model is adequate for gender-affirming treatment: issues related with mental health assessment in the United States. J Sexual Med. (2023) 20:584–7. doi: 10.1093/jsxmed/qdad019
19. Institute of Medicine Committee on the Consequences of, U. Health insurance is a family matter. Washington (DC: National Academies Press (US (2002). Copyright 2002 by the National Academy of Sciences. All rights reserved.
20. Institute of Medicine Committee on the Consequences of, U. Care without coverage: too little, too late. Washington (DC: National Academies Press (US (2002). Copyright 2002 by the National Academy of Sciences. All rights reserved.
21. De Lew N, Greenberg G, Kinchen K. A layman's guide to the U.S. health care system. Health Care Financ Rev. (1992) 14:151–69.
22. McWilliams JM. Health consequences of uninsurance among adults in the United States: recent evidence and implications. Milbank Q (2009) 87(2):443–94. doi: 10.1111/j.1468-0009.2009.00564.x
23. McMaughan DJ, Oloruntoba O, Smith ML. Socioeconomic status and access to healthcare: interrelated drivers for healthy aging. Front Public Health. (2020) 8:231. doi: 10.3389/fpubh.2020.00231
24. Knighton AJ, Savitz L, Belnap T, Stephenson B, VanDerslice J. Introduction of an area deprivation index measuring patient socioeconomic status in an integrated health system: implications for population health. EGEMS (Wash DC). (2016) 4:1238. doi: 10.13063/2327-9214.1238
25. Kind AJH, Buckingham WR. Making neighborhood-disadvantage metrics accessible — The neighborhood atlas. New Engl J Med. (2018) 378:2456–8. doi: 10.1056/NEJMp1802313
26. Heylens G, Elaut E, Kreukels BP, Paap MC, Cerwenka S, Richter-Appelt H, et al. Psychiatric characteristics in transsexual individuals: multicenter study in four European countries. Br J Psychiatry. (2014) 204:151–6. doi: 10.1192/bjp.bp.112.121954
27. Mueller SC, De Cuypere G, T'Sjoen G. Transgender research in the 21st century: A selective critical review from a neurocognitive perspective. Am J Psychiatry. (2017) 174:1155–62. doi: 10.1176/appi.ajp.2017.17060626
28. Lee B, Wang Y, Carlson SA, Greenlund KJ, Lu H, Liu Y, et al. National, state-level, and county-level prevalence estimates of adults aged ≥18 years self-reporting a lifetime diagnosis of depression - United States, 2020. MMWR Morb Mortal Wkly Rep. (2023) 72:644–50. doi: 10.15585/mmwr.mm7224a1
29. Wanta JW, Niforatos JD, Durbak E, Viguera A, Altinay M. Mental health diagnoses among transgender patients in the clinical setting: an all-payer electronic health record study. Transgend Health. (2019) 4:313–5. doi: 10.1089/trgh.2019.0029
30. Pinna F, Paribello P, Somaini G, Corona A, Ventriglio A, Corrias C, et al. Mental health in transgender individuals: a systematic review. Int Rev Psychiatry. (2022) 34:292–359. doi: 10.1080/09540261.2022.2093629
31. Gamarel KE, Reisner SL, Laurenceau JP, Nemoto T, Operario D. Gender minority stress, mental health, and relationship quality: a dyadic investigation of transgender women and their cisgender male partners. J Fam Psychol. (2014) 28:437–47. doi: 10.1037/a0037171
32. Hunter J, Butler C, Cooper K. Gender minority stress in trans and gender diverse adolescents and young people. Clin Child Psychol Psychiatry. (2021) 26:1182–95. doi: 10.1177/13591045211033187
33. Lindley L, Galupo MP. Gender dysphoria and minority stress: Support for inclusion of gender dysphoria as a proximal stressor. Psychol Sexual Orientation Gender Diversity. (2020) 7:265. doi: 10.1037/sgd0000439
34. Yu Y, Williams DR. Socioeconomic status and mental health . In: Handbook of the sociology of mental health. Washington, DC, USA: Springer (1999). p. 151–66.
35. Businelle MS, Mills BA, Chartier KG, Kendzor DE, Reingle JM, Shuval K. Do stressful events account for the link between socioeconomic status and mental health? J Public Health. (2013) 36:205–12.
36. Weinberg D, Stevens GWJM, Duinhof EL, Finkenauer C. Adolescent socioeconomic status and mental health inequalities in the Netherlands, 2001–2017. Int J Environ Res Public Health. (2019) 16:3605. doi: 10.3390/ijerph16193605
37. Nguyen HB, Chavez AM, Lipner E, Hantsoo L, Kornfield SL, Davies RD, et al. Gender-affirming hormone use in transgender individuals: impact on behavioral health and cognition. Curr Psychiatry Rep. (2018) 20:110. doi: 10.1007/s11920-018-0973-0
38. Doyle DM, Lewis TOG, Barreto M. A systematic review of psychosocial functioning changes after gender-affirming hormone therapy among transgender people. Nat Hum Behav. (2023) 7:1320–31. doi: 10.1038/s41562-023-01605-w
Keywords: transgender, socioeconomical impact, mental health, gender affirming health care, retrospective study
Citation: Cortez S, Moog D, Baranski E, Williams K, Wang J, Nicol G, Baranski T and Herrick CJ (2024) Assessment of sociodemographic and psychiatric characteristics of transgender adults seen at a Midwest tertiary medical center. Front. Endocrinol. 15:1445679. doi: 10.3389/fendo.2024.1445679
Received: 07 June 2024; Accepted: 13 August 2024;
Published: 04 September 2024.
Edited by:
Rosa Fernández, University of A Coruña CICA-INIBIC Strategic Group, SpainReviewed by:
Arcangelo Barbonetti, University of L’Aquila, ItalyLuuk Kalverdijk, University Medical Center Groningen, Netherlands
Copyright © 2024 Cortez, Moog, Baranski, Williams, Wang, Nicol, Baranski and Herrick. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Samuel Cortez, c2NvcnRlekB3dXN0bC5lZHU=
†These authors have contributed equally to this work and share senior authorship
 Samuel Cortez
Samuel Cortez Dominic Moog2
Dominic Moog2 Ginger Nicol
Ginger Nicol Thomas Baranski
Thomas Baranski