- 1Department of Global Health Research, Graduate School of Medicine, Juntendo University, Tokyo, Japan
- 2Advanced Research Institute for Health Sciences, Juntendo University, Tokyo, Japan
- 3Faculty of International Liberal Arts, Juntendo University, Tokyo, Japan
- 4Central Campus, International Higher School of Medicine, Bishkek, Kyrgyzstan
Background: The high prevalence of Type 2 diabetes mellitus(T2DM) in Pakistan is a challenge to the existing healthcare system. This is the first comprehensive review of the status of glycemic control, diabetes knowledge, treatment adherence, complications and financial burden faced by the diabetic patient population of the country.
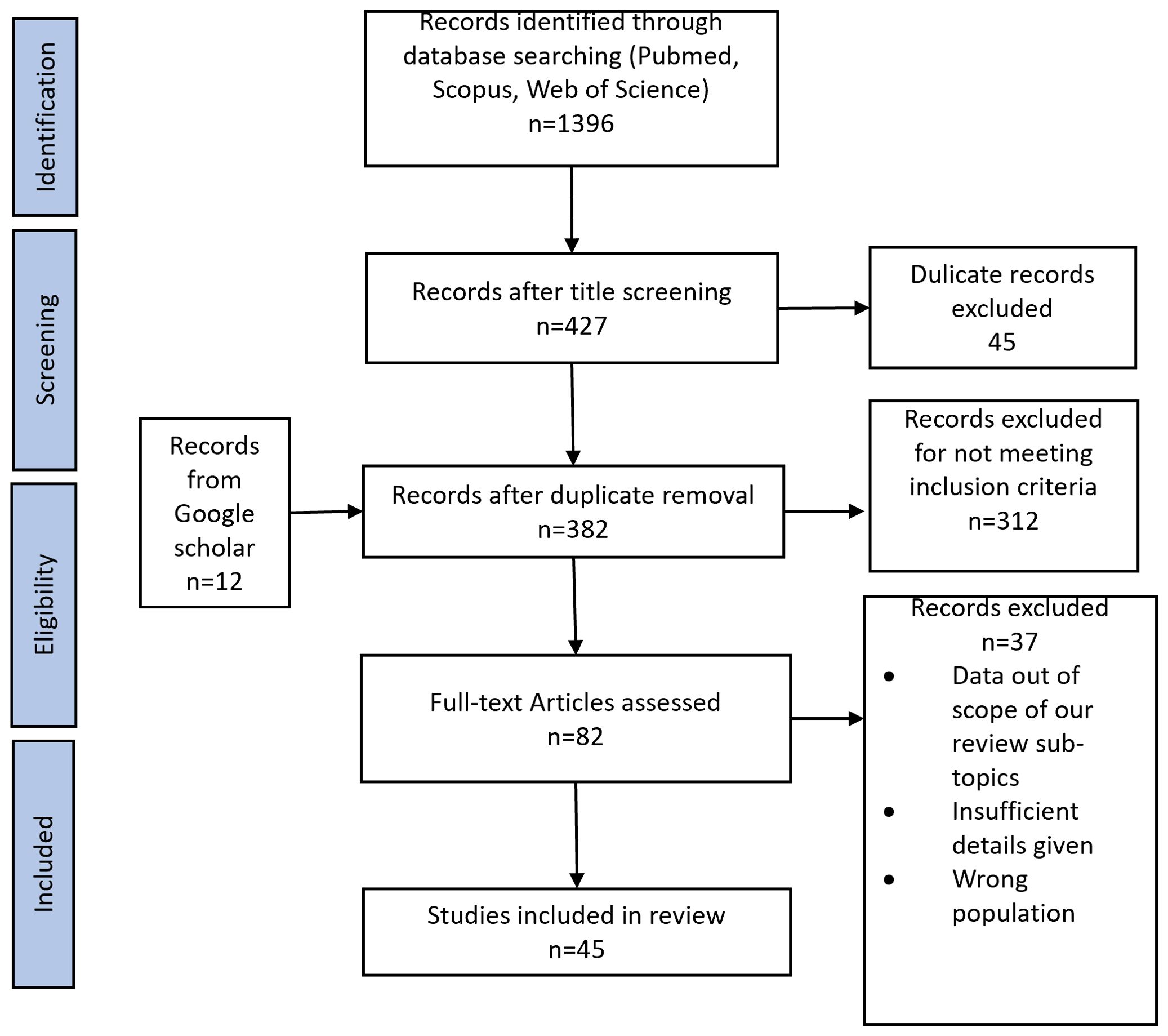
Methods: We searched PubMed, Web of Science and Scopus for studies on diabetes control, knowledge, treatment adherence, prevalence of complications and cost in Pakistan published in English from 2000 to 2024. We hand-searched Google Scholar for additional papers and included a total of 45 studies in our review.
Results: The review shows that poor glycemic control prevails among diabetic patients ranging from 44.7% to 86.4% along with half of the patients have poor diabetes knowledge (46.0% -70.0%). Treatment adherence level in diabetic patients varies widely in different studies, frequently reported complications are retinopathy (14.5%-43.0%), nephropathy (14.0%-31.0%) and neuropathy (10.8%-59.6%); and the disease poses a great deal of economic burden.
Conclusion: Most of the studies were observational. Glycemic control and knowledge among individuals with T2DM in Pakistan are inadequate, leading to a high prevalence of complications that impose significant health and economic burdens. Further longitudinal studies generating evidence of lifestyle modifications as primary and secondary prevention strategies against diabetes in the Pakistani population can form a strong foundation for awareness campaigns and policy revisions.
1 Introduction
In recent times, Type 2 diabetes (T2DM) has emerged as one of the most common non-communicable diseases in high as well as in low and middle-income countries (1). According to WHO, T2DM was the largest cause of mortality in 2019 claiming 1.5 million lives (2). As per the International Diabetes Federation (IDF) Atlas 2021, 10.5% of the adult global population (20-79 years) has diabetes. Furthermore, by 2045, 783 million adults will be diabetic (one in eight adults) as per IDF projections (3). The dynamics of this disease are changing. It is estimated that globally T2DM accounts for 12% of health expenditure in 2010 at $376 billion and is expected to reach $490 billion in 2030 (4). T2DM is one of the fastest-rising public health concern in Asian countries mainly due to lifestyle changes associated with economic transitions, globalization and urbanization (5).
Pakistan is a low-middle-income country located in South Asia. According to the second National Diabetic Survey of Pakistan NDSP (2016-2017), the weighted prevalence of diabetes was 26.3%. (28.3% in urban areas and 25.3% in rural areas), while the prevalence of pre-diabetes was 14.4% (6). Pakistan is the 5th most populous country in the world. The most recent IDF Atlas estimated that 33 million people are living with diabetes in Pakistan, which constitutes 3rd largest diabetes population globally (7). An additional 11 million adults have impaired glucose tolerance, while 8.9 million with diabetes remain undiagnosed making it a major public health concern in the country (8). The age-adjusted comparative prevalence of diabetes among the 20 to 79 years age group in Pakistan has been compared to regional countries in Figure 1 (data obtained from IDF Diabetes Atlas 10th edition 2021 (3)). The high prevalence can be attributed to the poor state of non-communicable disease risk factors in the country such as unhealthy diet, physical inactivity, increasing trends of tobacco consumption, overweight and obesity (9, 10).
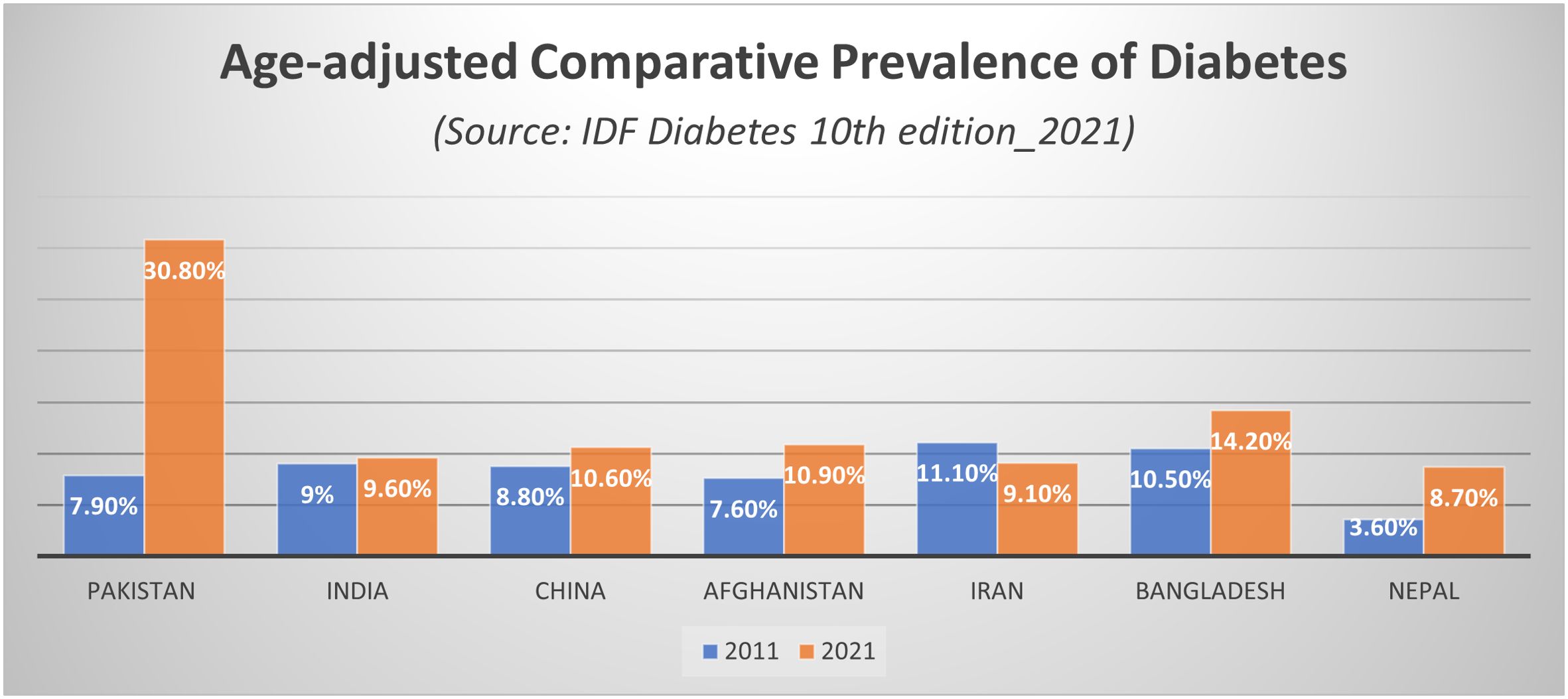
Figure 1. Age-adjusted comparative prevalence of diabetes. Source: IDF Diabetes Atlas 10th edition 2021.
An important aspect of diabetes in resource-limited settings like Pakistan is its economic impact. High expenses can quickly drain household and national resources thereby deterring poverty reduction initiatives. The real burden of this disease is due to chronic complications which lead to increased morbidity and mortality. Thus, in addition to the primary prevention strategies, secondary prevention of diabetic complications in individuals who have already developed the disease is equally essential in reducing the health and economic burden of T2DM. A cornerstone for improving diabetes outcomes and proper management is patient education about the disease (11). Lower mortality and positive health outcomes in people living with T2DM have also been found to be associated with good treatment adherence (12–14). On the other hand, poor glycemic control is linearly correlated with microvascular complications of diabetes (15–17). With the current prevalence statistics, every fourth adult in Pakistan is diabetic. We, therefore, consider it important to examine the situation of people living with this disease. Our objective is to collate data on the status of glycemic control among diabetic patients, diabetic knowledge, compliance to treatment, the prevalence of complications and cost; with the aim to help tailor secondary prevention strategies according to the needs of the diabetic population of the country.
2 Methods
2.1 Study design
The goal of a scoping review is to map the literature on a broad research theme and to identify the gaps. It is a preferred study design when there are uncertainties and/or deficiencies in the volume of literature. We conducted this scoping review based on the York methodology outlined by Arksey and O’Malley (18) with the aim to capture all literature regardless of study design and quality. As suggested by the framework, we followed the five stages: (1) identifying the research question (2) identifying relevant studies (3) selecting appropriate studies (4) data charting and (5) collating summarizing and reporting results (Supplementary File 1). The conduct of this review was consistent with the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA-ScR) Extension for Scoping Reviews (19).
2.2 Eligibility criteria
Inclusion criteria were: (1) articles published from 2000 to 2024 (2) articles published in the English language (3) articles that addressed one of the five main areas of this review (prevalence of uncontrolled diabetes, complications, cost, medication adherence and awareness) and (4) articles for which full text was obtained for this review.
Exclusion criteria were: (1) studies that do not fulfill the above criteria (2) review papers reporting the results of other studies (3) studies conducted among the Pakistani diaspora residing abroad.
2.3 Search strategy
We used relevant search terms with appropriate Boolean operators and filters to comprehensively search studies published in the English language between 2000 to 2024 on different databases (PubMed, Web of Science, Scopus and Google Scholar). (Supplementary File 2). Necessary adjustments were made in the search term depending on the database used.
2.4 Selection of studies
The search identified a total of 1396 studies from the abovementioned databases. Initially, the titles of the identified studies were screened independently for relevance. Titles deemed relevant by any evaluator were retained for abstract screening. Subsequently, the evaluators examined the abstracts of retained studies to identify those deemed worthy of full article screening. Discussions were performed in case of any disagreement until an agreement was reached regarding article inclusion. Lastly, full text was examined for final inclusion. Two reviewers (HT and IA) extracted the data and an impartial third reviewer provided advice regarding article selection. Step-wise article selection process is shown in the PRISMA flow chart in Figure 2.
2.5 Data items and charting process
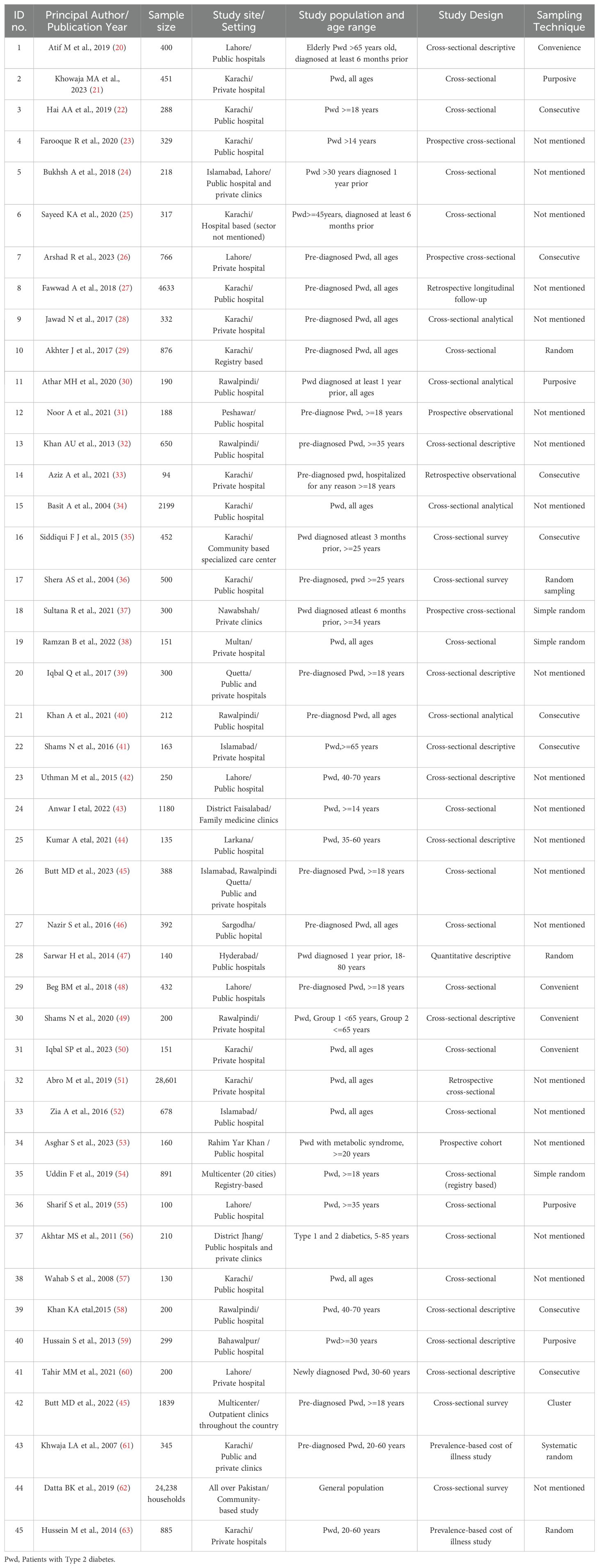
For all studies reviewed, data were extracted and charted regarding sample size, study population, study setting and instrument/criteria used for results. The extracted data from all sources was transferred to Endnote by three reviewers (HT, HK and SS). Collated data was rechecked by the third reviewer (IA) and matched with original sources. A separate excel sheet was generated for data about each theme from where the relevant data was summarized and charted in main manuscript. A full list of articles according to sub-themes is given in Supplementary File 3. Other than charting, we conducted a narrative descriptive synthesis of determinants and factors associated with the results from each theme. Assessment of risk bias and appraisal of quality of included sources was not done. The characteristics of the included studies are given in Table 1.
3 Results
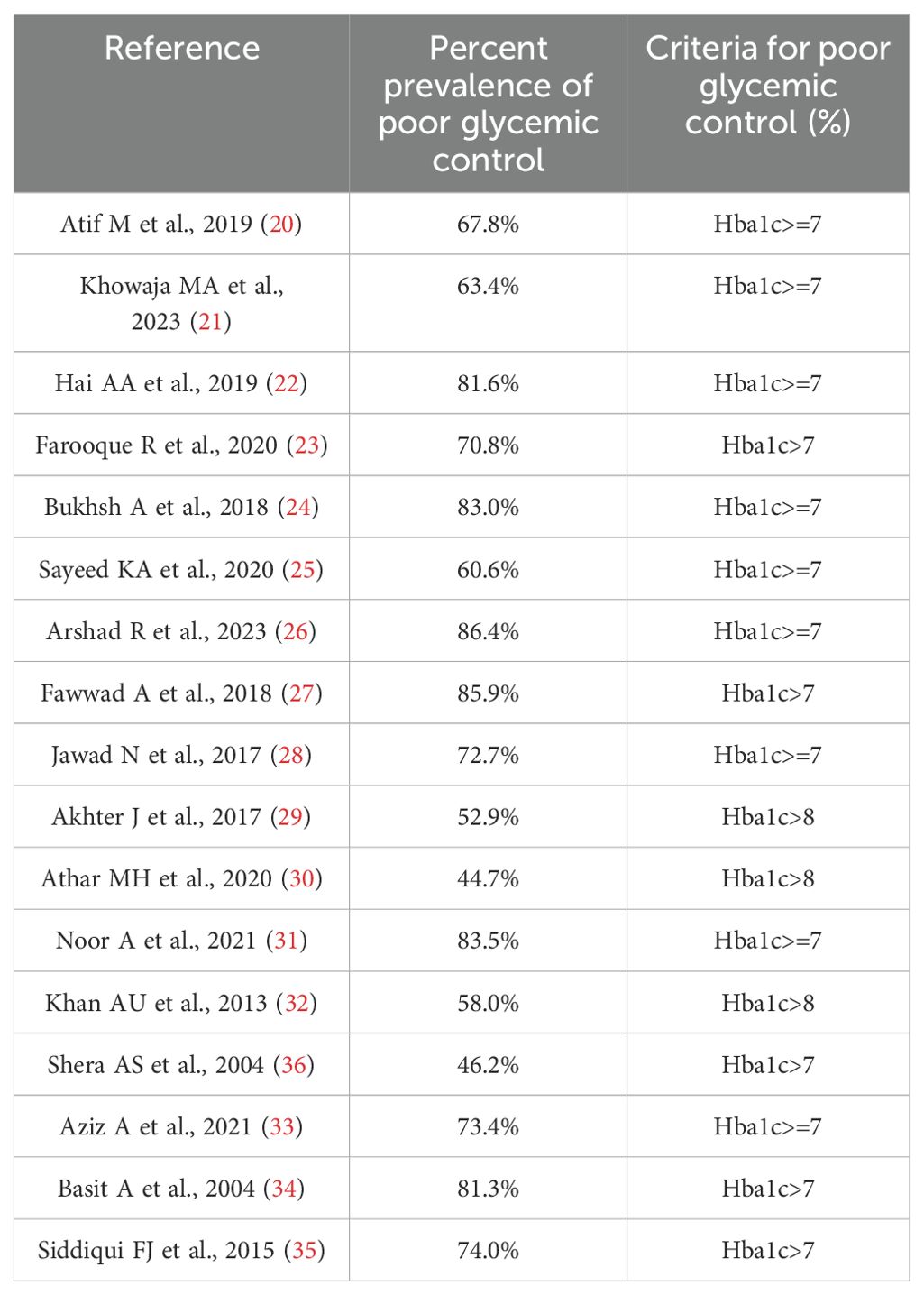
3.1 Uncontrolled diabetes and poor glycemic control
Among different cross-sectional studies conducted in the country, poor glycemic control ranged from 44.7% to 86.4% (cutoff value of Hba1c varied a little among studies) as shown in Table 2. Factors associated with poor glycemic control mentioned by Saeed et al., (64) are compromised self-care, poor adherence to medication, lack of social support and low literacy level (25). Arshad R et al., (26) documented in their study that only 9% of female diabetic patients had normal BMI, which explained a higher prevalence of poor glycemic control in women as compared to men in that study (26). The compliance of checking Hba1c was also found to be inadequate (58.5%) in diabetic patients by Aziz et al., (33). Anwer et al. (65) in his study on 1180 diabetic patients from urban and rural areas of the Faisalabad district documented that 40% of diabetic patients never had their Hba1c checked (43).
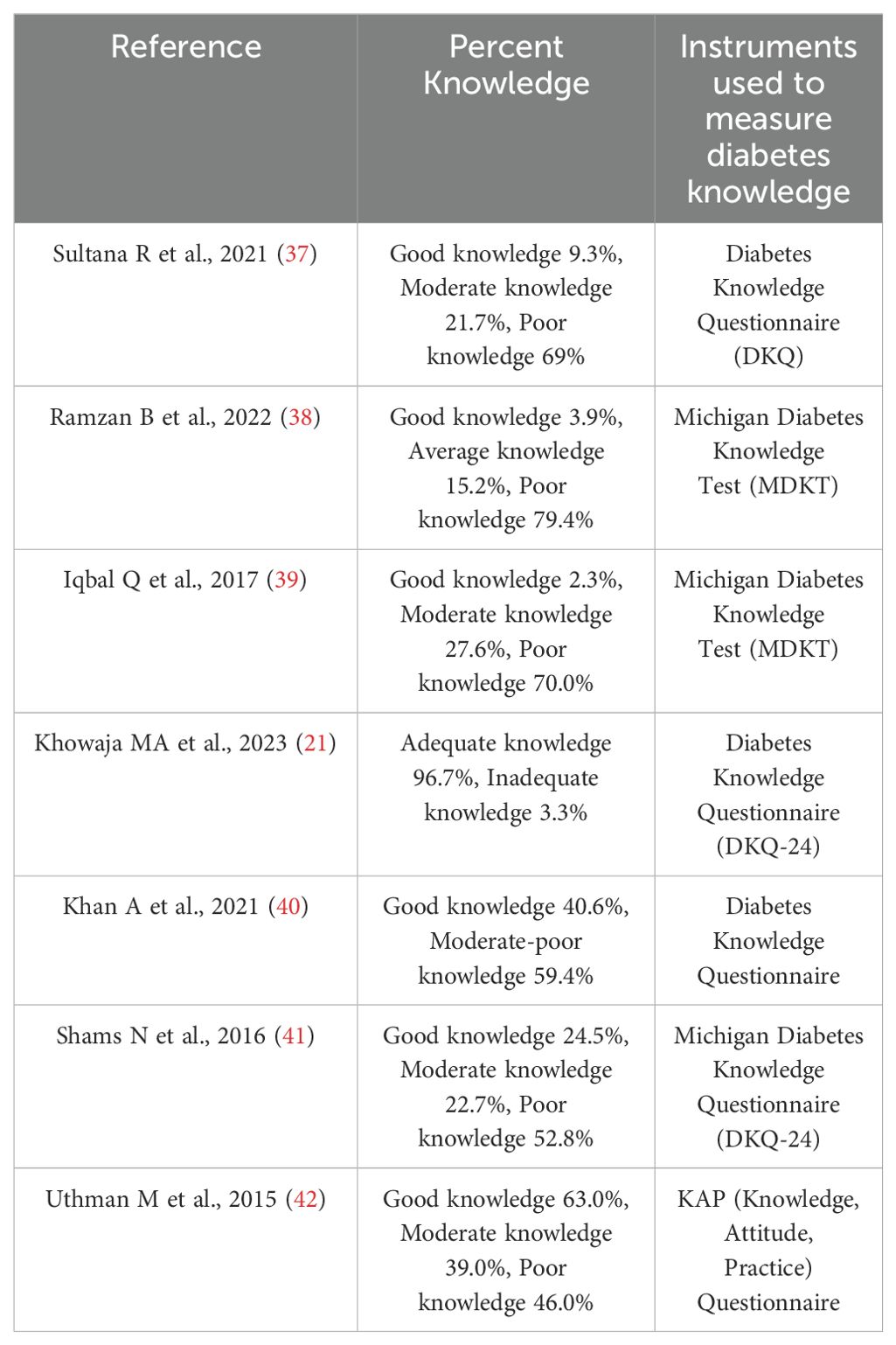
3.2 Diabetes awareness
The knowledge and awareness about the disease in the diabetic population is generally poor as shown in Table 3. Anwar I et al., 2022, a survey conducted in rural and urban areas of Faisalabad district on 1180 diabetic patients found better knowledge of diabetic complications in women compared to men (43). Shams et al. (66) has documented illiteracy, poverty, poor glycemic control, poor dietary control and use of alternate modes of therapy as factors associated with poor diabetes knowledge in elderly diabetics (41). Uthman M et al., (42) found in their KAP (Knowledge, Attitude, Practice) study that good diabetes knowledge exists in 63.0% of respondents, however good practice towards diabetes was found in 7.0% only (42). Kumar A et al., (44) found inadequate knowledge of the symptoms and self-management of hypoglycemia in 42.5% of T2DM (44).
3.3 Diabetes treatment adherence
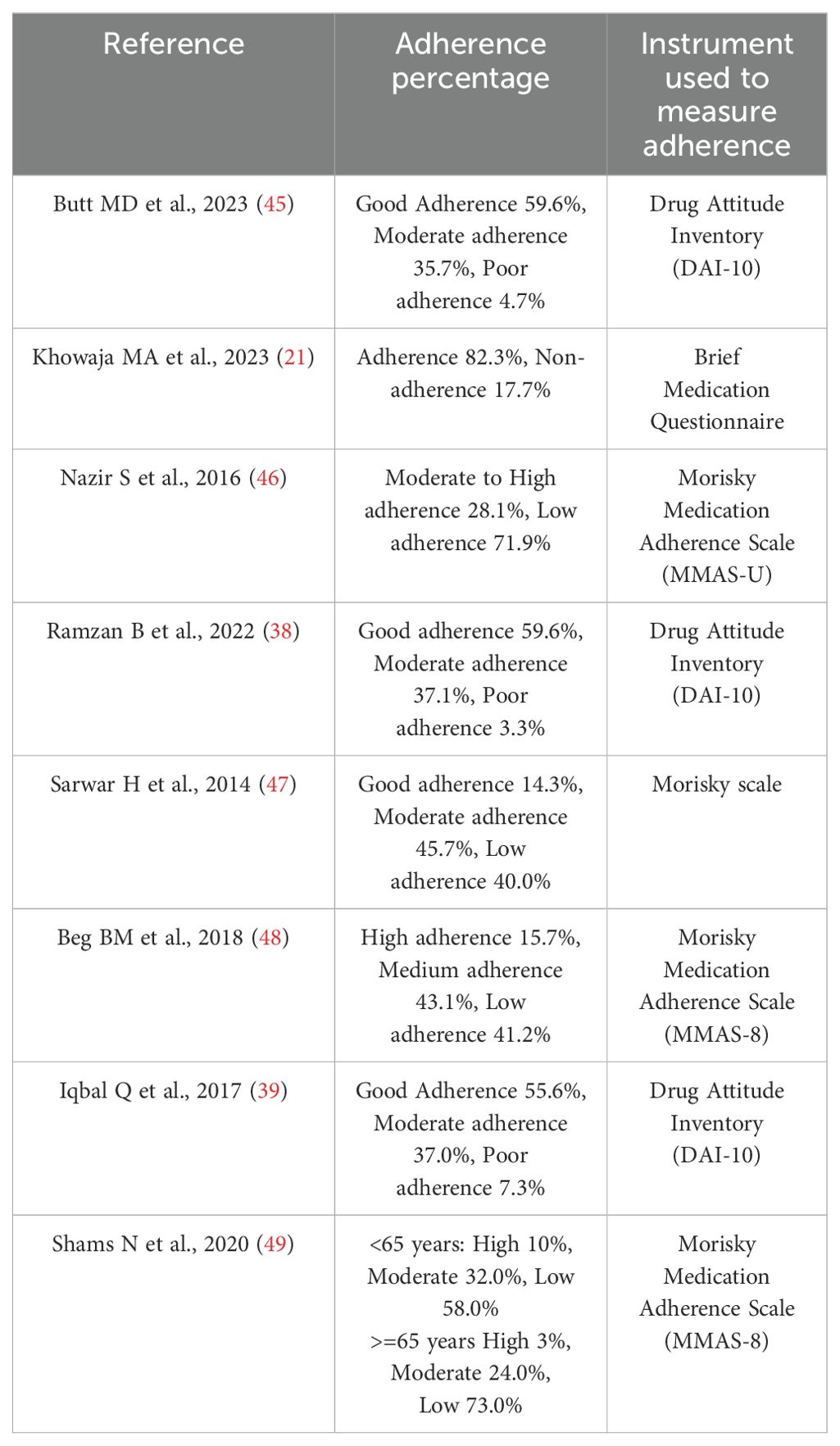
Standard treatments for controlling glucose levels include oral hypoglycemics and insulin. In Pakistan, Metformin has the highest (51.3%) prescription rate followed by insulin/analogues (34.6%) (45). Butt MD et al., (45) documented in their recent multicenter cross-sectional study that the majority (26%) of patients with T2DM received triple therapy while 34.7% received monotherapy (45). Adherence to treatment according to our selected papers varies according to the study site as shown in Table 4.
A survey conducted in Karachi by Iqbal SP et al., (39) documented that patients cited side effects of medicines as the most common factor related to non-compliance followed by forgetfulness, complex regime and financial constraints (50). Polypharmacy, combined anti-diabetic regimes, visual morbidity and physical dependence were the factors associated with poor adherence in geriatric diabetic patients according to Shams N et al., (49). Beg BM et al., (48) found in their study conducted in Lahore that the majority of patients who were non-adherent had low literacy levels (48).
3.4 Prevalence of diabetic complications
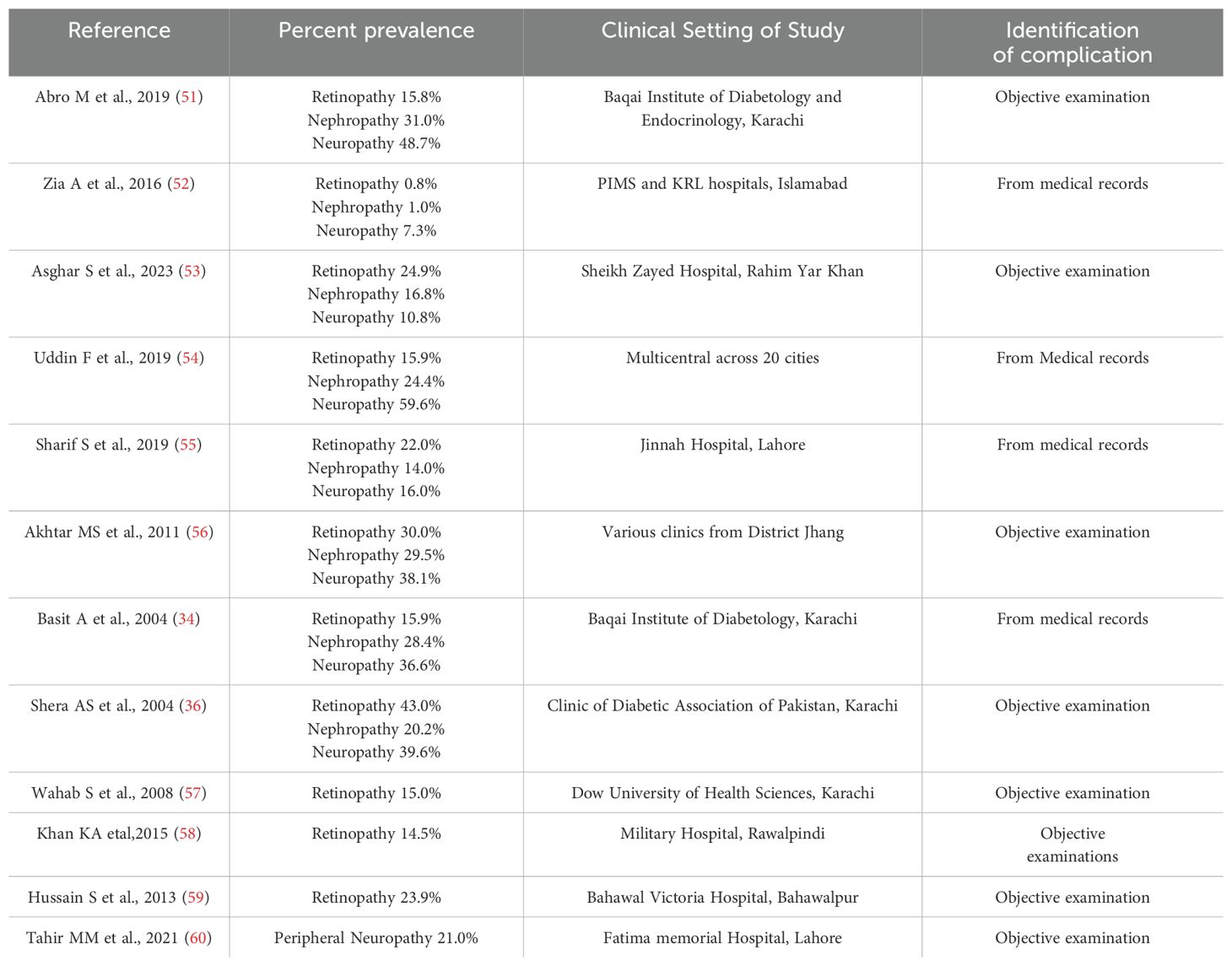
Micro and macrovascular complications of diabetes increase the disease burden on patients as well as the health system. A study conducted by Zia A et al., (52), in the capital, documented the percent prevalence of diabetic macrovascular complications as ischemic heart disease 28.2%, stroke 8.5%, peripheral vascular disease 5.4% (52). Uddin et al. (67) in their national, multicenter observational study conducted across 20 cities in Pakistan documented micro and macrovascular complication prevalence to be 68.6% and 9.0% respectively with commonly observed macrovascular complications being angina (5.2%), myocardial infarction (3.3%), peripheral arterial disease (2.2%) and stroke (2.0%) (54). Basit et al., in 2004 documented hypertension as the most common macrovascular complication in Karachi (50.4%) followed by coronary artery disease (15.1%) (34). The prevalence of microvascular complications is given in Table 5.
3.5 Cost and financial burden
A recent multicenter study conducted by Butt MD et al., (68) documented the total annual cost of diabetes in Pakistan to be $740 per person, out of which direct cost was $646.7, while indirect cost was $93.65 (68). Although at the lower end of the general global trend (direct cost: $242 to $11,917, indirect cost: $45 to $16,914 (1)), this is a substantially large expenditure relative to the average income in Pakistan. Hussain M et al., (63) in his survey in Karachi sampling 885 diabetic patients documented that the largest cost is accounted for by medication followed by physician consultation, with none of the participants indicating any coverage by insurance or employer (63). Diabetes management accounts for 62.0% of the per capita income in Pakistan (with a per capita income of $1193.73 as per World Bank data, (69)) (68). A recent nationally representative survey in Pakistan found that catastrophic health expenditure is 6.7 percentage points higher for households consuming blood pressure and diabetes medication (62). A prevalence-based cost of illness study conducted in Karachi by Khawaja LA et al., 2007 documented that 18.0% of total family income is spent on diabetes care (61). Based on the prevalence of T2DM in Pakistan, as reported by International Diabetes Foundation, Butt MD et al., (68) computed the total burden of diabetes management to be $24.42 billion which constitutes 1.6% of Pakistan’s GDP (World Bank data, 2021) (68).
4 Discussion
The rising diabetes burden is a major concern in Pakistan. We found in our review that the majority of the diabetic population in Pakistan has poor glycemic control. Many studies pointed out a relatively higher prevalence of poor glycemic control among people belonging to low socioeconomic classes and with lower education levels; which is consistent with overall health inequity prevailing in the country. People belonging to lower socioeconomic classes tend to adhere less to medication and lifestyle modifications eventually leading to further deterioration of glycemic control (70). With the exception of one study (Arshad et al., (26)), glycemic control did not differ significantly between men and women. However, previous reviews on the Pakistani population have documented a higher prevalence of obesity in Pakistani women as compared to men (71, 72), which can be one of the contributing factors towards poor control of diabetes. Women in Pakistani culture are deprived of outdoor leisure exercise facilities especially in rural areas (26). Other contributing factors such as differences in lifestyle factors and genetic predispositions should be explored in future studies. Our findings are consistent with other studies which found poor diabetes control in most low-middle-income countries (73, 74). Additionally, we found poor compliance of diabetes patients with Hba1c testing.
The poor control of diabetes can be explained by other findings of this study such as poor awareness and unsatisfactory medication adherence among patients with diabetes. We included studies that used validated instruments to measure medication adherence and diabetes knowledge. The studies assessing diabetes knowledge had consistent results of poor diabetes knowledge in the majority of patients except the study conducted by Khowaja et al., (21). It was a hospital-based study conducted in the endocrinology clinics of Aga Khan Hospital, Karachi (21). The inconsistency may be due to the fact that this hospital has patient education program in place whereby brochures with frequently asked questions about diabetes and other diseases are provided to the patients and caregivers (75). Also, a hospital-based study conducted in specialized clinics may give better results in terms of disease awareness since better-aware patients are more likely to visit these specialized clinics. It is important to impart relevant disease knowledge to diabetic patients to improve awareness in order to achieve long term glycemic control and prevent complications. Evidence-based and culturally tailored free of cost education programmes should be developed and made available to people living with diabetes especially those with poor access to health facilities.
Studies assessing medication adherence showed substantial variance in results with particularly lower adherence in geriatric patients with diabetes. Inadequate medication adherence is found in the literature to be a major challenge, especially in developing countries (76, 77). However, we found that very few studies (48–50) explored the determinants of poor adherence in the Pakistani population. The main determinants that we found in our review are fear of side effects, illiteracy, complex medication regimens and high cost of medicines. Current scheme of universal health coverage in Pakistan does not cover outpatient consultation or medicine cost. Thus, high cost of medicines coupled with low awareness hinders medication adherence. Patient education about doses and side-effects of medicines and improving doctor-patient relationship can also be beneficial. Further studies in this area can help guide the researchers and decision-makers in selecting appropriate interventions and tailoring them to target the specific determinants of poor medication adherence in the country.
One of the well-known outcomes of poor diabetes control is microvascular complications such as retinopathy, neuropathy and nephropathy. The current review found a high prevalence of these complications in Pakistan. Excluding statistics from one study (Zia A et al., (52)), the prevalence of diabetic retinopathy was 14.5%-43.0%, nephropathy 14.0%-31.0% and neuropathy 10.8%-59.6%. The study by Zia A. et al., (52) gives very small percent prevalence of microvascular complications as compared to the rest of the studies. The author attributes this inconsistency to differences in socioeconomic and lifestyle factors since the study was conducted in two tertiary-care hospitals in the capital city of Islamabad (52). Diabetes-related complications contribute to high financial burdens and low quality of life. Awareness regarding complications in diabetes patients was found to be better in 41-65 years age group and women (43). Comparable figures of microvascular complication prevalence in regional countries are found in the literature (78–80). Precise understanding of the rural-urban variations and trends in diabetes-related complications remains a gap in Pakistan for which we recommend further studies in this domain.
Overall, the current financial burden associated with this disease in the country is very high. Our review shows that high medicine price is a significant contributor to the management cost of diabetes in Pakistan. A systematic review found diabetes medicine price as the biggest burden of the cost of this disease in the neighbouring country of India as well (81). Ensuring access and affordability of diabetes medication is, therefore, crucial to achieve better disease control in developing countries. Devising new healthcare policies and introducing new generic medicines should also be considered.
To the best of our knowledge, this review is the first to collate articles related to the above-mentioned themes in the diabetic patient population of Pakistan. We used robust methods in screening, extracting and reviewing the data. A timely review of the literature and diverse inclusion criteria are additional strengths of this study. The interpretation of the findings of this review has to be done in light of certain limitations. First, there was limited evidence to provide valid estimates at regional and national levels and according to patient characteristics such as gender, age etc. Second, most of the included studies are cross-sectional surveys. So, it is not possible to identify cause and effect. Third, since the study was intended to be a scoping review and not systematic, we did not do quality assessment or risk of bias for included studies. However, we included only those studies which used validated instruments to measure outcomes.
The government has taken many steps to control the burden of diabetes. Important ones include the recent opening of the Diabetes Registry of Pakistan (DROP) (82); the National Association of Diabetes Educators of Pakistan (NADEP), established in 2010 (83); and the Diabetes Prevention Program (DPP) by the Diabetes Association of Pakistan (84). To increase awareness, massive education campaign is needed. We recommend the use of digital platforms which is a cost-effective population-based approach. In Pakistan, the health system in rural and urban slum communities is successfully strengthened by Lady health workers at household and community levels. However, currently, they have a focused scope of maternal, child and reproductive health (85). We recommend widening their scope to include diabetes prevention and control. This will help produce an equitable improvement of diabetes control in the country. Therefore, training of lady health workers and primary health care professionals about the diagnosis and monitoring of diabetes along with diabetes prevention through lifestyle behaviors modification would be a timely investment to reduce the growing burden of diabetes. Collaborative approaches with health organizations in local and national communities will enhance the effect and reach of already existing initiatives. Ongoing evaluation of current interventions and programs is also critical. Meanwhile, it is important to secure universal access to diagnosis, treatment and monitoring of diabetes mellitus to the public.
5 Conclusion
The findings of this review highlight the dismal status of diabetes control and inadequate level of diabetes knowledge in Pakistan. The prevalence of diabetic complications is high and the disease poses a significant financial burden on diabetic patients as well as the health system. A well-organized education campaign is needed to raise awareness in this regard. We have included our recommendations for the advancement of diabetes research and prevention strategies in Pakistan. We hope that current strategies and future directions can successfully cater to the rising diabetes menace in the country.
Author contributions
HT: Investigation, Formal analysis, Data curation, Writing – original draft, Methodology, Conceptualization. IA: Investigation, Formal analysis, Supervision, Writing – review & editing, Writing – original draft, Methodology, Conceptualization. HK: Writing – review & editing, Visualization, Investigation. YS: Writing – review & editing, Methodology. MO: Writing – review & editing, Methodology. MA: Writing – review & editing, Methodology. SS: Writing – review & editing, Investigation. MY: Writing – review & editing, Supervision, Funding acquisition.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to thank the authors and participants of all the included studies.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2024.1441591/full#supplementary-material
References
1. Seuring T, Archangelidi O, Suhrcke M. The economic costs of type 2 diabetes: A global systematic review. Pharmacoeconomics. (2015) 33:811–31. doi: 10.1007/s40273-015-0268-9
2. Diabetes_WHO (2023). Available online at: https://www.who.int/news-room/fact-sheets/detail/diabetes. (accessed March 18, 2024)
3. International diabetes federation (2024). Available online at: https://diabetesatlas.org/. (accessed April 22, 2024)
4. Zhang P, Zhang X, Brown J, Vistisen D, Sicree R, Shaw J. Global healthcare expenditure on diabetes for 2010 and 2030. Diabetes Res Clin Pract. (2010) 87:293–301. doi: 10.1016/j.diabres.2010.01.026
5. Hills AP, Arena R, Khunti K, Yajnik CS, Jayawardena R, Henry CJ. Epidemiology and determinants of type 2 diabetes in south Asia. Lancet Diabetes Endocrinol. (2018) 6:966–78. doi: 10.1016/s2213-8587(18)30204-3
6. Abdul B, Asher F, Qureshi H, Shera AS. Prevalence of diabetes, pre-diabetes and associated risk factors: second National Diabetes Survey of Pakistan (NDSP), 2016–2017. BMJ Open. (2018) 8:e020961. doi: 10.1136/bmjopen-2017-020961
7. Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. (2022) 183:109119. doi: 10.1016/j.diabres.2021.109119
8. Bhutta ZA, Haq ZU, Basit A. Diabetes in Pakistan: addressing the crisis. Lancet. (2022) 10:309–10. doi: 10.1016/S2213-8587(22)00102-4
9. Rafique I, Saqib MAN, Munir MA, Qureshi H, Rizwanullah KSA, Khan SA, et al. Prevalence of risk factors for noncommunicable diseases in adults: key findings from the Pakistan STEPS survey. East Mediterr Health J. (2018) 24:33–41. doi: 10.26719/2018.24.1.33
10. Hall JN, Moore S, Harper SB, Lynch JW. Global variability in fruit and vegetable consumption. Am J Prev Med. (2009) 36:402–409.e5. doi: 10.1016/j.amepre.2009.01.029
11. Funnell MM, Brown TL, Childs BP, Haas LB, Hosey GM, Jensen B, et al. National standards for diabetes self-management education. Diabetes Care. (2007) 30:1630–7. doi: 10.2337/dc07-9923
12. Krapek K, King K, Warren SS, George KG, Caputo DA, Mihelich K, et al. Medication adherence and associated hemoglobin A1c in type 2 diabetes. Ann Pharmacother. (2004) 38:1357–62. doi: 10.1345/aph.1D612
13. Rhee MK, Slocum W, Ziemer DC, Culler SD, Cook CB, El-Kebbi IM. Patient adherence improves glycemic control. Diabetes Educ. (2005) 31:240–50. doi: 10.1177/0145721705274927
14. Simpson SH, Eurich DT, Majumdar SR, Padwal RS, Tsuyuki RT, Varney J, et al. A meta-analysis of the association between adherence to drug therapy and mortality. Bmj. (2006) 333:15. doi: 10.1136/bmj.38875.675486.55
15. Stolar M. Glycemic control and complications in type 2 diabetes mellitus. Am J Med. (2010) 123:S3–S11. doi: 10.1016/j.amjmed.2009.12.004
16. Gaster B, Hirsch IB. The effects of improved glycemic control on complications in type 2 diabetes. Arch Internal Med. (1998) 158:134–40. doi: 10.1001/archinte.158.2.134
17. Monami M, Candido R, Pintaudi B, Targher G, Mannucci E. Improvement of glycemic control in type 2 diabetes: A systematic review and meta-analysis of randomized controlled trials. Nutrition Metab Cardiovasc Dis. (2021) 31:2539–46. doi: 10.1016/j.numecd.2021.05.010
18. Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implementation Sci. (2010) 5:1–9. doi: 10.1186/1748-5908-5-69
19. Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Internal Med. (2018) 169:467–73. doi: 10.7326/M18-0850
20. Atif M, Saleem Q, Asghar S, Malik I, Ahmad N. Extent and predictors of poor glycaemic control among elderly Pakistani patients with type 2 diabetes mellitus: A multi-centre cross-sectional study. Medicina. (2019) 55:21. doi: 10.3390/medicina55010021
21. Khowaja MA, Rozi S, Sawani S, Ahmed A. Factors associated with Diabetes Empowerment among patients with type 2 diabetes, at OPD setting, Karachi, Pakistan. Sci Rep. (2023) 13:7165. doi: 10.1038/s41598-023-34385-4
22. Hai AA, Iftikhar S, Latif S, Herekar F, Patel MJ. Diabetes self-care activities and their relation with glycemic control in patients presenting to The Indus Hospital, Karachi. Cureus. (2019) 11:2377–385. doi: 10.7759/cureus.6297
23. Farooque R, Herekar F, Iftikhar S, Patel MJ. The frequency of poor sleep quality in patients with diabetes mellitus and its association with glycemic control. Cureus. (2020) 12. doi: 10.7759/cureus.11608
24. Bukhsh A, Khan TM, Nawaz MS, Ahmed HS, Chan KG, Lee LH, et al. Association of diabetes-related self-care activities with glycemic control of patients with type 2 diabetes in Pakistan. Patient preference adherence. (2018) 12:2377–85. doi: 10.2147/PPA.S177314
25. Sayeed KA, Qayyum A, Jamshed F, Gill U, Usama SM, Asghar K. Impact of diabetes-related self-management on glycemic control in type II diabetes mellitus. Cureus. (2020) 12. doi: 10.7759/cureus.7845
26. Arshad R, Iqbal S, Sarwar U, Amir M, Waqar S, Naqvi ASA H. Effect of obesity, socioeconomic status and gender on glycemic control in diabetic patients. Rawal Med J. (2023) 48:651–1.
27. Fawwad A, Mustafa N, Zafar AB, Khalid M. Incidence of microvascular complications of type 2 diabetes: A 12 year longitudinal study from Karachi-Pakistan. Pak J Med Sci. (2018) 34:1058–63. doi: 10.12669/pjms.345.15224
28. Jawad N, Naveed S, Ali Z, Jafri S, Ahmad SM, Baloch Qutrio ZA. anthropometry and diabetic control in Pakistan. Indo Am J Of Pharm Sci. (2017) 4:3722–8. doi: 10.5281/zenodo.1036563
29. Akhter J, Ahmed A, Mawani M, Lakhani L, Kalsekar A, Tabassum S, et al. Patterns, control and complications of diabetes from a hospital based registry established in a low income country. BMC Endocrine Disord. (2017) 17:30. doi: 10.1186/s12902-017-0179-1
30. Athar MH, Nisar S, Zubair U, Bin Mumtaz H. Impact of general education status on glycemic control in patients of diabetes mellitus. Pakistan Armed Forces Med J. (2020) 70:S26–30. https://pafmj.org/PAFMJ/article/view/3788.
31. Noor A, Rahman MU, Faraz N, Samin KA, Ullah H, Ali A. Relationship of homocysteine with gender, blood pressure, body mass index, hemoglobin A1c, and the duration of diabetes mellitus type 2. Cureus. (2021) 13:e19211. doi: 10.7759/cureus.19211
32. Khan AU, Khan MZA, Nadeem M, Bangash RY, Fakhr A. Status of glycemic control in patients of type 2 diabetes mellitus. Pakistan Armed Forces Med J. (2013) 63:275–8. https://pafmj.org/PAFMJ/article/view/2272.
33. Aziz A, Ali SA. Compliance of checking HbA1c in a tertiary care hospital of Pakistan. Pakistan J Med Sci. (2021) 37:142. doi: 10.12669/pjms.37.1.2814
34. Basit A, Hydrie MZI, Hakeem R, Ahmedani MY, Masood Q. Frequency of chronic complications of type 2 diabetes. J Coll Physicians Surg Pak. (2004) 14:79–83.
35. Siddiqui FJ, Avan BI, Mahmud S, Nanan DJ, Jabbar A, Assam PN. Uncontrolled diabetes mellitus: prevalence and risk factors among people with type 2 diabetes mellitus in an Urban District of Karachi, Pakistan. Diabetes Res Clin Pract. (2015) 107:148–56. doi: 10.1016/j.diabres.2014.09.025
36. Shera AS, Jawad F, Maqsood A, Jamal S, Azfar M, Ahmed U. Prevalence of chronic complications and associated factors in type 2 diabetes. J Pak Med Assoc. (2004) 54:54–9.
37. Sultana R, Mughal UUR, Ghoto MA, Muhammad S, Abbas J, Laghari SH. Awareness and Lifestyle Practices among Type-II Diabetics Pertaining to the Disease Attended at Outpatient Clinics of Nawabshah, Shaheed Benazirabad. J Pharm Res Int. (2021) 33:67–75. doi: 10.9734/jpri/2021/v33i29A31565
38. Ramzan B, Hassali A, Hashmi F, Saleem F, Gardezi S, Hussain I, et al. Impact of diabetes-related knowledge and medication adherence on quality of life among type 2 diabetes patients in a tertiary health facility in Multan, Pakistan. Trop J Pharm Res. (2022) 21:871–7. doi: 10.4314/tjpr.v21i4.26
39. Iqbal Q, ul Haq N, Bashir S, Bashaar M. Profile and predictors of health related quality of life among type II diabetes mellitus patients in Quetta city, Pakistan. Health Qual Life Outcomes. (2017) 15:142. doi: 10.1186/s12955-017-0717-6
40. Khan A, Farooq A, Arshad AR, Rashid S. Awareness regarding diabetes and its management amongst patients visiting tertiary care hospitals and its impact on glycemic control. Pakistan Armed Forces Med J. (2021) 71:1815–19. https://pafmj.org/PAFMJ/article/view/2998.
41. Shams N, Amjad S, Seetlani NK, Ahmed W. Diabetes knowledge in elderly type 2 diabetes mellitus patients and association with glycemic control. J Liaquat Univ Med Health Sci. (2016) 15:71–7. doi: 10.22442/jlumhs.161520468
42. Uthman M, Ullah Z, Shah NU. Knowledge, attitude and practice (KAP) survey of type 2 diabetes mellitus. Age (years). (2015) 9:351–5.
43. Anwer I, Shahzad M, Ijaz N, Gill SI, Shahzad A, Usman M. Awareness and understanding of diabetes complications among patients of diabetes mellitus. Age (years). (2022) 14:266. doi: 10.53350/pjmhs2216192
44. Kumar A, Shaikh ZA, Prithian SL, Shaikh BA, Ansari IA, Hyder I. Knowledge of Hypoglycemic Symptoms and their Self-Management among patients with Type II Diabetes Mellitus. Pakistan J Health Med Sci. (2021) 15:2961–2. doi: 10.53350/pjmhs2115112961
45. Butt MD, Ong SC, Rafiq A, Malik T, Sajjad A, Batool N, et al. An observational multi-center study on type 2 diabetes treatment prescribing pattern and patient adherence to treatment. Sci Rep. (2023) 13:23037. doi: 10.1038/s41598-023-50517-2
46. Nazir SUR, Hassali MA, Saleem F, Bashir S, Aljadhey H. Disease related knowledge, medication adherence and glycaemic control among patients with type 2 diabetes mellitus in Pakistan. Primary Care Diabetes. (2016) 10:136–41. doi: 10.1016/j.pcd.2015.09.004
47. Sarwar H, Dayo A, Ghoto MA, Ishaq H, Baloch N, Memmon N, et al. Adherence with prescribed medications among diabetes mellitus II patients. Int J Pharm Sci Rev Res. (2014) 24:246–52.
48. Beg BM, Khan H, Hasan D, Izhar Z, Amin U, Areej S. Evaluation of medication adherence among diabetics: a cross-sectional study in Lahore, Punjab, Pakistan. Independent J Allied Health Sci. (2018) 1:27–32.
49. Shams N, Amjad S, Seetlani NK, Niaz F, Farhat S, Bashir F. Geriatric Type 2 diabetes; the risk factors and associations for medication non-adherence. Prof Med J. (2020) 27:260–7. doi: 10.29309/TPMJ/2020.27.02.3300
50. Iqbal SP, Farid R, Arshad A. Noncompliance to treatment and its associated factors among patients with diabetes mellitus in karachi. J Shalamar Med Dental College-JSHMDC. (2023) 4:104–10. doi: 10.53685/jshmdc.v4i2.189
51. Abro M, Zafar AB, Fawwad A, Mustafa N, Tahir B, Riaz M, et al. Prevalence of diabetic micro vascular complications at a tertiary care unit of Karachi, Pakistan. Int J Diabetes Developing Countries. (2019) 39:325–30. doi: 10.1007/s13410-018-0683-5
52. Zia A, Bhatti A, Jalil F, Wang X, John P, Kiani AK, et al. Prevalence of type 2 diabetes–associated complications in Pakistan. Int J Diabetes Developing Countries. (2016) 36:179–88. doi: 10.1007/s13410-015-0380-6
53. Asghar S, Shahid S, Fatima M, Bukhari SMH, Siddiqui SN. Metabolic syndrome in type 2 diabetes mellitus patients: prevalence, risk factors, and associated microvascular complications. Cureus. (2023) 15. doi: 10.77592/cureus.39076
54. Uddin F, Ali B, Junaid N. Prevalence of diabetic complications in newly diagnosed type 2 diabetes patients in Pakistan: findings from national registry. J Ayub Med Coll Abbottabad. (2019) 30:652–8.
55. Sharif S, Raza MT, Mushtaq S, Afreen B, Hashmi BA, Ali MH, et al. Frequency of depression in patients with type 2 diabetes mellitus and its relationship with glycemic control and diabetic microvascular complications. Cureus. (2019) 11. doi: 10.77592/cureus.5145
56. Akhtar MS, Rafique S, Akhtar MS, Irfan HM. Prevalence of diabetic complications in an urban district of Jhang (Punjab) Pakistan. Can J App Sci. (2011) 1:43–9. doi: 10.21065/19257430.43.1
57. Wahab S, Mahmood N, Shaikh Z, Kazmi WH. Frequency of retinopathy in newly diagnosed type 2 diabetes patients. JPMA. J Pakistan Med Assoc. (2008) 58:557–61.
58. Khan KA, Kamran SM, Qureshi MN, Jamal Y. Frequency of retinopathy in newly diagnosed patients of type 2 diabetes mellitus (DM): retinopathy in type 2 DM. Pakistan Armed Forces Med J. (2015) 65:63–7. https://pafmj.org/PAFMJ/article/view/671.
59. Hussain S, Qamar MR, Iqbal MA, Ahmad A, Ullah E. Risk factors of retinopathy in type 2 diabetes mellitus at a tertiary care hospital, Bahawalpur Pakistan. Pak J Med Sci. (2013) 29:536–9. doi: 10.12669/pjms.292.3066
60. TAHIR MM, Chachar AZK, Haider M, Shamim A, Asif M, Ali S. Frequency of peripheral neuropathy in newly diagnosed type 2 diabetes presenting in a tertiary care hospital of lahore. Pakistan Journal of Medical and Health Sciences (2021) 15(7):1676–79. doi: 10.53350/pjmhs211571676
61. Khowaja LA, Khuwaja AK, Cosgrove P. Cost of diabetes care in out-patient clinics of Karachi, Pakistan. BMC Health Serv Res. (2007) 7:189. doi: 10.1186/1472-6963-7-189
62. Datta BK, Muhammad Jami H, Asma S. Assessing the relationship between out-of-pocket spending on blood pressure and diabetes medication and household catastrophic health expenditure: evidence from Pakistan. Int J Equity Health. (2019) 18. doi: 10.1186/s12939-018-0906-x
63. Hussain M, Naqvi SBS, Khan MA, Rizvi M, Alam S, Abbas A, et al. Direct cost of treatment of diabetes mellitus type 2 in Pakistan. Int J Pharm Pharm Sci. (2014) 6:261–4.
64. Khalid AS, Azwa Q, Fatima J, Usman G, Syed MU, Kanza A, et al. Impact of diabetes-related self-management on glycemic control in type II diabetes mellitus. Cereus. (2020) 4. doi: 10.7759/cureus.7845
65. Anwer I, Shahzad M, Ijaz N, Iqbal Gill SI, Shahzad A, Usman M, et al. Awareness and understanding of diabetes complications among patients of diabetes Mellitus. Pak J Med Health Sci. (2021) 14:92–5. doi: 10.53350/pjmhs2216192
66. Nadia S, Sadia A, Kumar SN, Furquana N, Shahzia F, Farhat B. Geriatric Type 2 diabetes; the risk factors and associations for medication non-adherence. Professional Med J. (2020) 27:260–7. doi: 10.29309/TPMJ/2020.27.02.3300
67. Fareed U, Beena A, Nabeea J. Prevalence of diabetic complications in newly diagnosed type 2 diabetes patients in Pakistan: findings from national registry. J Ayub Med Coll Abbottabad. (2018) 30:652-8.
68. Butt MD, Ong SC, Wahab MU, Rasool MF, Saleem F, Hashmi A, et al. Cost of illness analysis of type 2 diabetes mellitus: the findings from a lower-middle income country. Int J Environ Res Public Health. (2022) 19:12611. doi: 10.3390/ijerph191912611
69. World Bank data. Diabetes-WHO, IDF atlas, Pakistan Diabetes Prevention Program (PakDPP), Agha Khan University (2021).
70. Rahman M, Nakamura K, Hasan SM M, Seino K, Mostofa G. Mediators of the association between low socioeconomic status and poor glycemic control among type 2 diabetics in Bangladesh. Sci Rep. (2020) 10:6690. doi: 10.1038/s41598-020-63253-8
71. Tanzil S, Jamali T. Obesity, an emerging epidemic in Pakistan-a review of evidence. J Ayub Med Coll Abbottabad. (2016) 28:597–600.
72. Mehboob B, Safdar NF, Zaheer S. Socio-economic, environmental and demographic determinants of rise in obesity among Pakistani women: a systematic review. J Pak Med Assoc. (2016) 66:1165–72.
73. Aschner P, Galstyan G, Yavuz DG, Litwak L, Gonzalez-Galvez G, Goldberg-Eliaschewitz F, et al. Glycemic control and prevention of diabetic complications in low-and middle-income countries: an expert opinion. Diabetes Ther. (2021) 12:1491–501. doi: 10.1007/s13300-021-00997-0
74. Borgharkar SS, Das SS. Real-world evidence of glycemic control among patients with type 2 diabetes mellitus in India: the TIGHT study. BMJ Open Diabetes Res Care. (2019) 7:e000654. doi: 10.1136/bmjdrc-2019-000654
75. Aga Khan University Hospital. Patient education material. In: The Aga Khan University Hospital offers a wide range of information and education materials for patients on various diseases and conditions. These are designed to help patients better manage and understand their disease (2024) (Karachi, Pakistan: Agha Khan University Hospital.). Available at: https://hospitals.aku.edu/Pakistan/patients-families/Pages/Patient%20Educational%20Material.aspx.
76. Sharma T, Kalra J, Dhasmana D, Basera H. Poor adherence to treatment: A major challenge in diabetes. Age (Yrs). (2014) 15:26–9.
77. Medi RK, Mateti UV, Kanduri KR, Konda SS. Medication adherence and determinants of non-adherence among south Indian diabetes patients. J Soc Health Diabetes. (2015) 3:048–51. doi: 10.4103/2321-0656.140892
78. Afroz A, Alam K, Hossain MN, Biswas A, Ali L, Magliano DJ, et al. Burden of macro- and micro-vascular complications of type 2 diabetes in Bangladesh. Diabetes Metab Syndrome: Clin Res Rev. (2019) 13:1615–22. doi: 10.1016/j.dsx.2019.03.001
79. Unnikrishnan R, Anjana RM, Mohan V. Diabetes mellitus and its complications in India. Nat Rev Endocrinol. (2016) 12:357–70. doi: 10.1038/nrendo.2016.53
80. Mishra S, Pant B, Subedi P. The prevalence of diabetic retinopathy among known diabetic population in Nepal. Kathmandu Univ Med J. (2016) 14:134–9.
81. Oberoi S, Kansra P. Economic menace of diabetes in India: a systematic review. Int J Diabetes developing countries. (2020) 40:464–75. doi: 10.1007/s13410-020-00838-z
82. Basit A, Fawwad A, Baqa K. Diabetes registry of Pakistan. Pak J Med Sci. (2020) 36:578–80. doi: 10.12669/pjms.36.3.1877
83. National association of diabetes educators of Pakistan (2024). Available online at: https://www.nadep.org.pk/About.html. (accessed February 2, 2024)
84. Pakistan diabetes prevention (2024). Available online at: https://pakdpp.org.pk/prevention/. (accessed February 2, 2024)
Keywords: T2DM, glycemic control, awareness, medication adherence, complications, cost, Pakistan
Citation: Taimur H, Ahmad I, Khan H, Shirayama Y, Okamoto M, Aung MN, Shabbir S and Yuasa M (2024) A scoping review of type 2 diabetes mellitus in Pakistan investigating the status of glycemic control, awareness, treatment adherence, complications and cost. Front. Endocrinol. 15:1441591. doi: 10.3389/fendo.2024.1441591
Received: 04 June 2024; Accepted: 21 October 2024;
Published: 22 November 2024.
Edited by:
Tadese Melaku Abegaz, The Ohio State University, United StatesReviewed by:
Sueziani Binte Zainudin, Sengkang General Hospital, SingaporeSridhar R. Gumpeny, Endocrine and Diabetes Centre, India
Copyright © 2024 Taimur, Ahmad, Khan, Shirayama, Okamoto, Aung, Shabbir and Yuasa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ishtiaq Ahmad, YWhtYWRAanVudGVuZG8uYWMuanA=; ZHJpc2h0aWFxbWluaGFzQGdtYWlsLmNvbQ==
 Hira Taimur1
Hira Taimur1 Ishtiaq Ahmad
Ishtiaq Ahmad Hamza Khan
Hamza Khan Myo Nyein Aung
Myo Nyein Aung