- 1Department of Public Health, School of Public Health, College of Medicine and Health Science, Mizan-Tepi University, Mizan-Aman, Ethiopia
- 2Department of Midwifery, College of Medicine and Health Science, Mizan-Tepi University, Mizan-Aman, Ethiopia
- 3Department of Public Health, College of Medicine and Health Science, Debre Markos University, Debre Markos, Ethiopia
Background: In areas with limited resources, the lack of preparedness and limited availability of diabetes mellitus services in healthcare facilities contribute to high rates of illness and death related to diabetes mellitus. As a result, this study focused on analyzing the combined prevalence of preparedness and availability of diabetic services in countries with limited resources.
Methods: A comprehensive search was conducted across various databases, such as PubMed/MEDLINE, Web of Science, Google Scholar, and African Journal Online. The search aimed to identify primary research articles that assessed the availability and preparedness of services for individuals with type 2 diabetes mellitus specifically. The articles included in the search spanned from January 2000 to 23 February 2024. To analyze the data, a meta-analysis of proportions was performed using the random-effects model. Additionally, the researchers assessed publication bias by examining a funnel plot and conducting Egger’s test. Heterogeneity and sensitivity analyses were also conducted to evaluate the data. The findings of the study regarding the pooled prevalence of diabetes service preparedness and availability, along with their corresponding 95% confidence intervals, were presented using a forest plot.
Results: A comprehensive analysis was conducted on 16 research articles that focused on service preparedness and 11 articles that examined service availability. The sample sizes for these studies were 3,422 for service preparedness and 1,062 for service availability. The findings showed that the pooled prevalence of diabetes service preparedness was 53.0% (95% CI: 47.0-60.0). Furthermore, in this systematic synthesis, the overall pooled prevalence of service availability for diabetes mellitus was 48% (95% CI: 36.0-67.0), with the highest pooled prevalence observed in Asia, with a pooled prevalence of 58% (95% CI: 38.0-89.0).
Conclusion: Our study reveals a significant disparity in the preparedness and availability of services for diabetes mellitus, which falls below the minimum threshold set by the WHO. These findings should capture the attention of policymakers and potentially serve as a foundation for reevaluating the current approach to diabetes service preparedness and availability. To enhance the availability and preparedness of diabetes services, a tailored, multifaceted, and action-oriented approach to strengthening the health system is required.
Systematic Review Registration: https://www.crd.york.ac.uk/prospero/, identifier CRD42024554911.
Introduction
Diabetes mellitus (DM) is a highly prevalent non-communicable disease (NCD) that poses a significant risk of premature death and disability (1–3). Diabetes increases vulnerability to other NCDs by changing metabolic processes (4, 5). As a result, diabetes mellitus has become a pressing and costly public health concern, prompting global leaders to take action. The diabetes burden has increased globally from time to time. According to the International Diabetes Federation (IDF), approximately 463 million adults worldwide are affected by diabetes, with 79.4% residing in low- and middle-income countries (6–8).
Diabetes is a major contributor to severe health issues, such as renal failure, limb amputation, blindness, and cardiovascular disease. These complications not only result in physical suffering and disability but also have a profound effect on individuals’ socioeconomic status. Managing diabetes can also lead to financial difficulties and jeopardize economic well-being. Additionally, these complications can impede individuals’ capacity to work and be productive. However, adequate preparedness and access to resources can mitigate the impact of these problems (9–13).
Previous studies have revealed a significant prevalence of undiagnosed diabetes (14–17). This highlights the urgent need to prioritize the diagnosis and treatment of diabetes in order to address the detrimental impact it has on health and mortality rates (18). Regrettably, a substantial number of individuals in the surveyed countries still remain undiagnosed with diabetes. This can be attributed to various factors such as limited access to healthcare services, lack of availability, and underutilization of existing resources. These factors contribute to the higher prevalence of undiagnosed diabetes in these regions (19). Furthermore, the investigated countries showed a concerning trend where only a small percentage of diagnosed patients were receiving adequate care. This emphasizes the importance of improving the overall healthcare system’s preparedness to provide comprehensive diabetes management services (20).
Achieving universal access to NCD services requires the active engagement of all stakeholders (21). Increasing investment in prevention and accessing care is essential for the achievement of Universal health care (UHC) (22). Multi-sectorial programs were required to deliver successful services for NCD. In addition, the reduction of premature death by one-third is the targeted of sustainable development goal (23, 24). Existing evidence suggests that timely provisions of such interventions to patients are excellent economic investments in reducing future expensive treatments (21, 24).
Insufficient access to healthcare services, limited availability, and underutilization of healthcare resources are major factors that contribute to the high morbidity and mortality rates associated with diabetes mellitus. Moreover, there is a pressing need to enhance service preparedness and availability, as previous studies have highlighted significant variations in the prevalence of preparedness and availability of services for diabetes mellitus (13, 18, 25–38). However, it is important to note that previous research in this field has often relied on a single study or has been limited to local or regional samples. To obtain a more comprehensive understanding, it is crucial to conduct multi-country studies that can compare the ability of healthcare facilities to provide diabetes mellitus services across countries. By addressing these limitations and conducting multi-country studies, we can gain more reliable and comprehensive insights into the preparedness and availability of healthcare facilities to provide diabetes mellitus services in low-resource settings. Therefore, the objective of this study is to synthesize the pooled prevalence of service availability and readiness for diabetes mellitus in resource-limited countries.
Methods
Research questions
To conduct a systematic review, we aimed to determine the pooled prevalence of diabetes service availability and readiness in resource-limited countries across Africa and Asia. Our research question followed the CoCoPop format, with the condition (Co) being the health facilities or responsible individuals involved in providing diabetic services. The context (Co) focused on health facilities in resource-limited settings. The population (Pop) of interest for this systematic review and meta-analysis consisted of adults requiring screening in health facilities within these resource-limited countries. The outcome of interest was the readiness and availability of health facilities to provide diabetic services. Consequently, our research question was formulated as follows: “What is the pooled prevalence of diabetes service preparedness and availability in resource-limited settings?” This approach enabled us to identify relevant keywords and construct comprehensive search strategies for conducting a thorough literature review.
Protocol and registration
This study has been officially registered with the International Prospective Register of Systematic Reviews. The PROSPERO registration number is CRD42024554911.
Data sources and search strategy
This systematic review and meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline (39). We performed an extensive literature search using various electronic bibliographic databases such as PubMed/MEDLINE, Web of Science, Google/Google Scholar, and African Journal Online. Our main objective was to obtain accurate and reliable results so we employed a combination of keywords and a relevant thesaurus that focused on the readiness and availability of health facilities to deliver diabetic services in resource-limited countries. To identify publications discussing availability and preparedness of health facilities for diabetes mellitus, we used the following search terms: (“readiness or availability or preparedness”) AND (“diabetes mellitus” OR “DM”) AND (“Services”) AND (“Africa” or “Asia”). We included observational studies in this systematic review and meta-analysis. We independently screened titles, abstracts, and full texts of articles. In cases of disagreement regarding the inclusion of a full-text article, all authors participated in discussions to reach a consensus. To ensure transparency and adherence to a standardized approach, we developed and registered a review protocol.
Eligibility criteria
Inclusion criteria
This review followed a systematic process that involved one approach, namely CoCoPop (Condition, context, and population), to determine which studies to include. Papers that failed to meet these criteria were considered irrelevant and excluded from the review. The review only took into account papers published in English from January 2000 to February 2024, including observational studies. To assess the quality of each article, the Joanna Briggs Institute (JBI) critical appraisal tool was used, and all articles that passed the quality assessment were included in the review.
Exclusion criteria
We have excluded studies pertaining to service availability and preparedness that primarily concentrate on communications, and reviews, commentaries, letters to the editors, studies where the raw data cannot be analyzed, and protocols were excluded. In addition, studies that did not assess the overall readiness and had unclear outcomes were also excluded from this systematic review and meta-analysis.
Study data management
After conducting a comprehensive search and gathering multiple articles, we proceeded to eliminate any duplicate files. This screening process involved two stages: initially assessing the titles and abstracts, followed by conducting a full-text screening. To ensure accuracy, two independent reviewers utilized the EndNote software to evaluate the potential relevance of each article for further review. The assessment was based on a predefined set of inclusion and exclusion criteria. In cases where there were discrepancies between the reviewers’ assessments, they were resolved through discussion and by seeking input from a third reviewer. For the purpose of auditing, electronic records were maintained for both the included and excluded studies, with clear explanations provided for any exclusions made.
Quality assessment and risk of bias
To assess the risk of bias in the study, a quality assessment checklist for prevalence studies was employed. This checklist, developed by Hoy and colleagues, consists of nine items that are crucial in evaluating the quality of a study (40). These items include the target population, sampling frame, sampling method, response rate, data collection procedures, study case definition, study instruments, and parameters for the numerator and denominator. Each item contributes to a total score of 9. Based on the scores obtained, the studies were categorized as having a high-risk (0–3), moderate-risk (4–6), or low-risk (7–9) of bias. Each study underwent an independent evaluation, and the majority of them demonstrated a low risk of bias. To ensure the reliability of the results, studies with a high risk of bias were excluded from the final analysis.
Data extraction
The data extraction process utilized a Microsoft Excel template. The form underwent iterative testing and revision as necessary. Two authors, YN and DG, independently performed the extraction. In cases where there were disagreements between the data extractors, the principal author, MS Alie, facilitated discussions to resolve them. The extracted descriptive variables encompassed various aspects such as first author, country, region, study design, study period, data collection method, sample size, outcomes, response rate, and related outcomes of diabetes service availability and preparedness.
Sensitivity analyses
A thorough sensitivity analysis was conducted to assess how individual studies affected the overall estimation of prevalence. Each study was methodically removed, and the resulting impact on the estimate was carefully examined. Surprisingly, the exclusion of any single study did not have a significant effect on the pooled prevalence estimate. Furthermore, none of the studies fell outside the confidence interval’s lower and upper boundaries. These findings indicate that the collective results of the studies remained strong and consistent, reinforcing the reliability of the overall prevalence estimate.
Data synthesis and analysis
The data collected from various articles was processed using Microsoft Excel 2013 and then exported to R software version 4.3.2 for further analysis. Our analysis focused on examining individual studies to determine the overall prevalence, service availability, and preparedness of health facilities in delivering diabetic care services. To achieve this, we performed random-effects meta-analyses in R software, allowing us to estimate the pooled prevalence along with 95% confidence intervals (C.I.s). The results were presented using the logit transform of the individual studies, accompanied by their respective 95% confidence intervals. In this systematic review and meta-analysis, we conducted subgroup analysis, bias assessment, sensitivity analysis, and heterogeneity analysis. Given the expected variation among the studies, we employed a random-effects model and utilized I2 statistics to evaluate the level of heterogeneity. Specifically, I2 values of 25%, 50%, and 75% indicated low, medium, and high heterogeneity (41), respectively. To assess publication bias, we examined the distribution of studies in a funnel plot. Deviation from a symmetrical funnel shape can indicate the presence of publication bias. Furthermore, we performed subgroup analysis based on potential sources of heterogeneity. Additionally, we conducted a leave-one-out sensitivity analysis to assess the influence of individual studies on the overall effect, which is presented in the tables and figures.
Results
Search and eligible research reports
A total of 117 studies were browsed from PubMed/MEDLINE, Web of Science, Google/Google Scholar, African Journal Online. From a register, we found 8 articles, from websites we found three articles, and through citation searching, we found two articles. Of these studies, 84 studies were excluded due to duplication and not being in the study area. Of the remaining 46 articles, 14 articles were removed due to them being a short communication letter, protocol, or qualitative study or having unclear and unrelated outcomes. The remaining 32 articles were assessed by reviewing the full text while five articles were excluded due to outcome measurement not being related and the full text not being available to see the detailed methodology. Finally, a total of 27 studies were eligible and included in the final systematic review and meta-analysis. After careful evaluation, we found that 16 articles for diabetes service preparedness (13, 13, 28, 29, 31–34, 42–49) and 11 articles for diabetes services availability (30, 42, 45, 48, 50–56) were included in this systematic review and meta-analysis. For a visual representation of the detailed inclusion and exclusion criteria used in the study, please refer to Figure 1, displayed below as the PRISMA diagram.
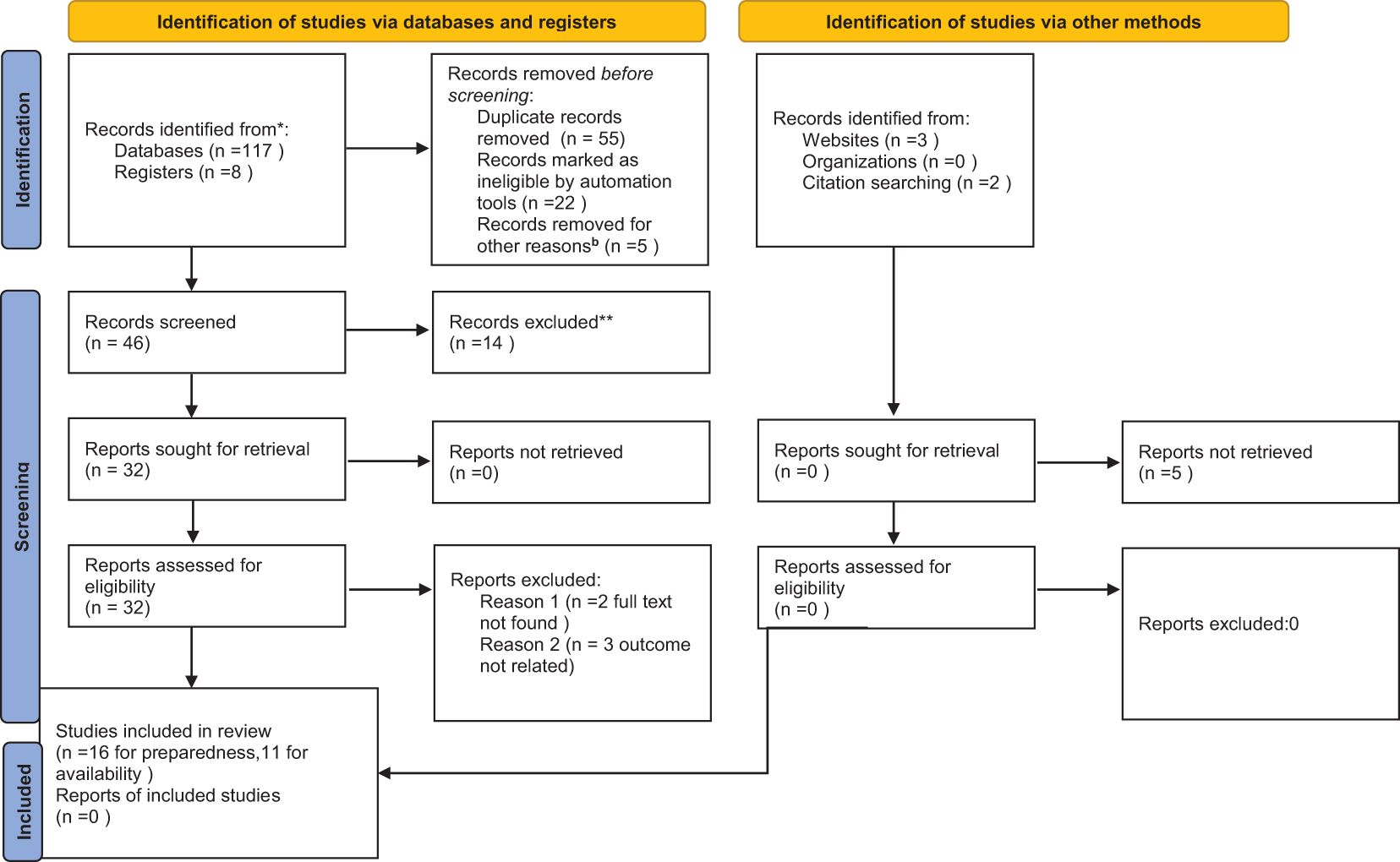
Figure 1 PRISMA 2020 flow diagram for diabetes mellitus service availability and preparedness in resource limited countries. **protocol, communication letter, not in study area and unrelated findings, other reasons=out of study area. * indicates the articles not included in this systematic review and meta-analysis.
Characteristics of the studies
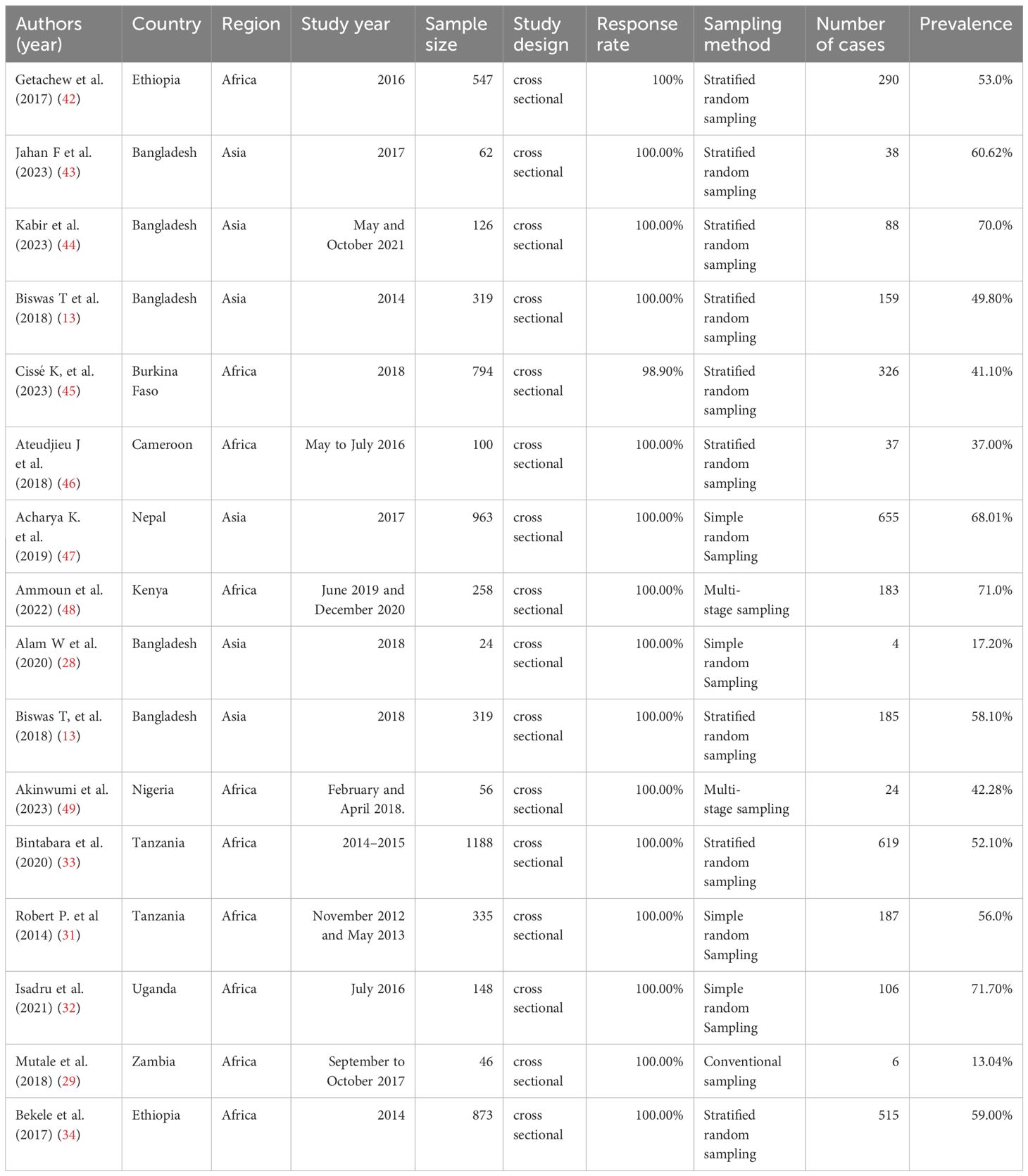
This analysis encompasses a total of 27 studies conducted in various countries. Of these, 16 studies focused on preparedness for managing diabetes, while 11 studies examined the availability of diabetes management services. Among the studies that explored diabetes service preparedness, five (31.25%) were carried out in Bangladesh, two studies were conducted in Ethiopia and Tanzania, and single studies were conducted in Zambia, Uganda, Kenya, Nepal, Cameroon, and Burkina Faso. The detailed studies on diabetes service preparedness are presented in Table 1. Regarding the aspect of diabetes service availability, two studies were conducted in Ethiopia, Vietnam, India and Kenya, and only one study conducted in Tanzania, Malawi, and Burkina Faso as shown in Table 2. The earliest survey was conducted in 2014, while the most recent one took place in 2023. In both cases cross cross-sectional studies were included. The studies that examine diabetes service preparedness are presented in Table 1 and studies examine diabetes service availability are presented in Table 2.
The pooled prevalence of service preparedness for DM
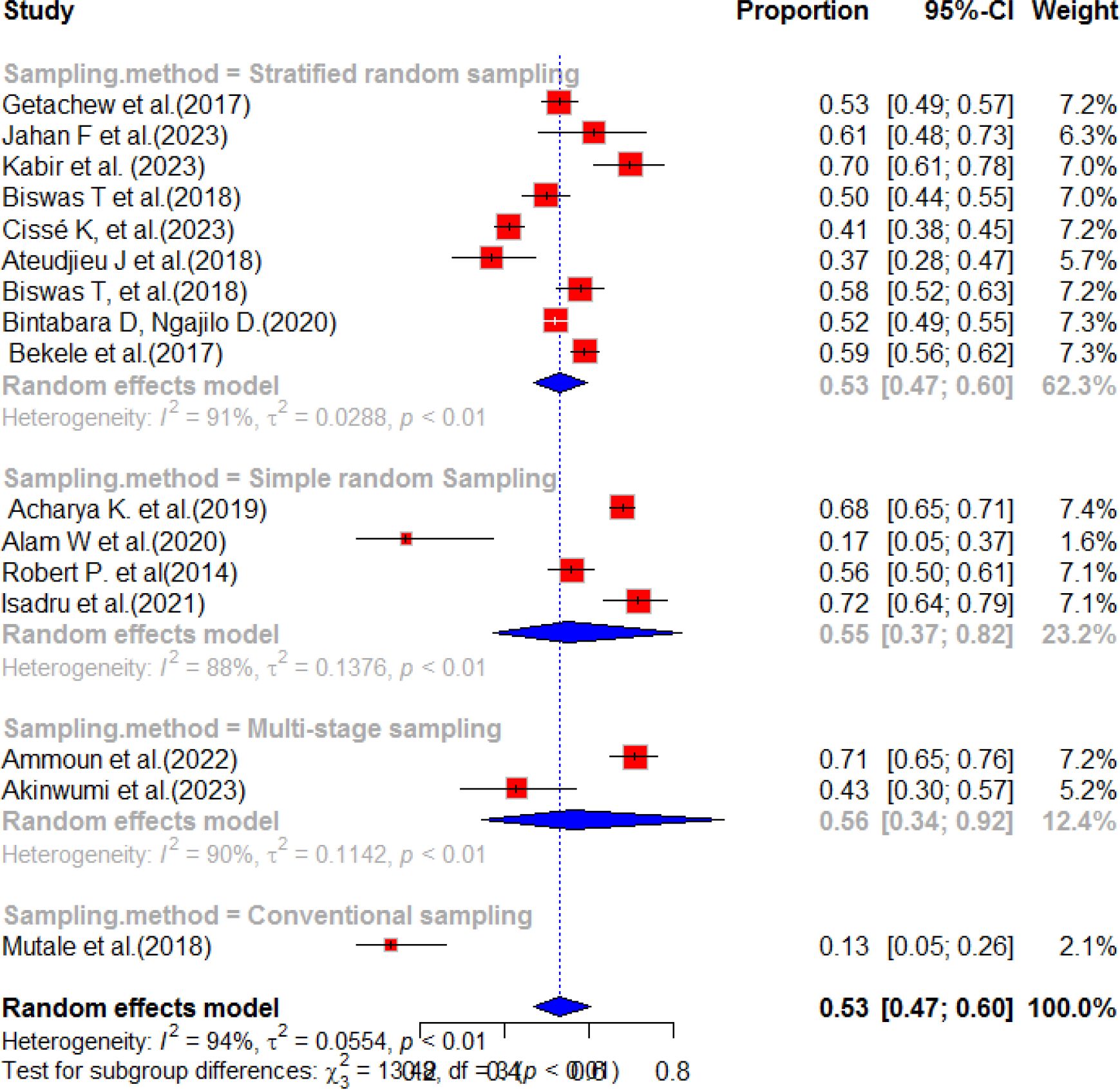
This systematic review and meta-analysis was conducted to assess the availability and preparedness of diabetes services in resource-limited countries. The study analyzed a total of 26 publications from different geographical areas, including Ethiopia, Zambia, Morocco, Bangladesh, Uganda, Kenya, Nepal, Tanzania, and Nigeria. The findings revealed that the estimated pooled prevalence of diabetes service preparedness was 53.0% (95%CI; 47.0-60.0), with a p-value of less than 0.01 and a high level of heterogeneity (I2 = 94%) (Figure 2). Figure 2 presents the pooled prevalence of diabetes mellitus service preparedness in health facilities.
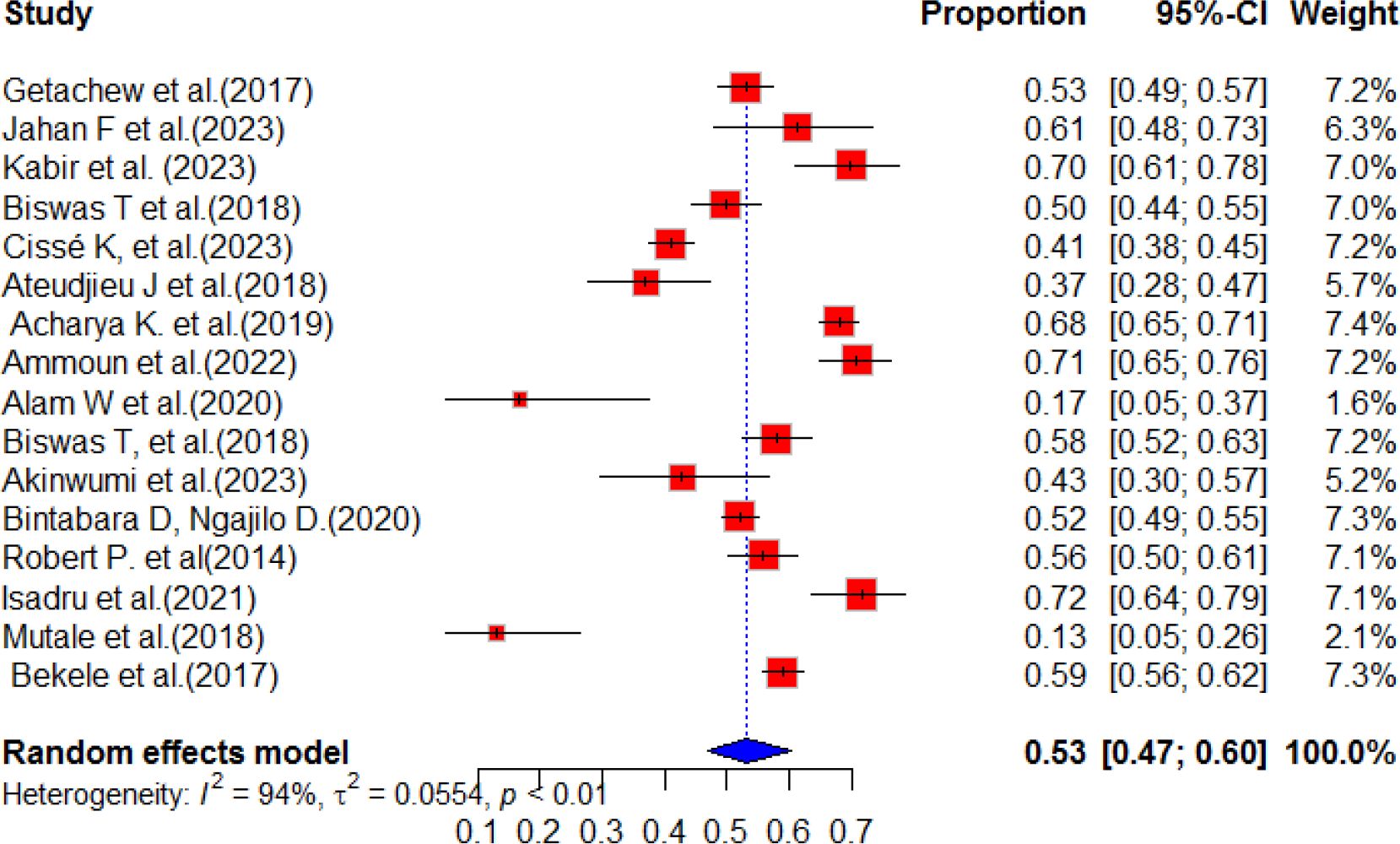
Figure 2 Random forest for DM service preparedness of health facilities in resource-limited countries.
Meta-bias in prevalence of diabetes service preparedness
The studies’s publication bias was assessed using Egger’s test and by examining the asymmetry of the funnel plot. It is important to note that funnel plots can sometimes appear highly asymmetric, even in the absence of publication bias, due to correlations between the outcome, effect size, and its standard error. In our current systematic review and meta-analysis, the results of Egger’s test indicated a p-value of 0.1119, with a bias estimate of -3.0644 (SE = 1.8063). Furthermore, the funnel plot displayed asymmetry, as illustrated in Figure 3. This finding indicates that there is no publication bias for the studies. Publication bias was also checked by using sample size and publication year in Table 3 below.
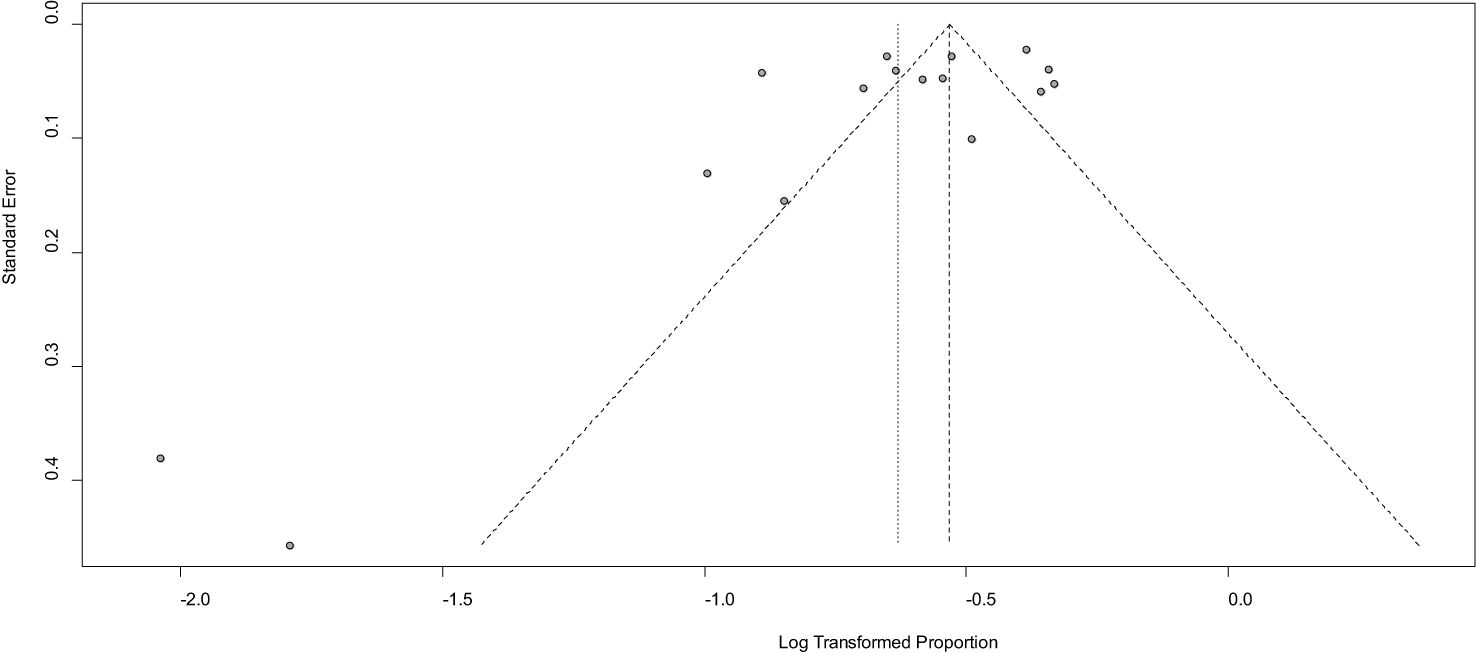
Figure 3 Funnel plot showing publication bias among the studies used to compute diabetes service preparedness in resource-limited countries, 2024.
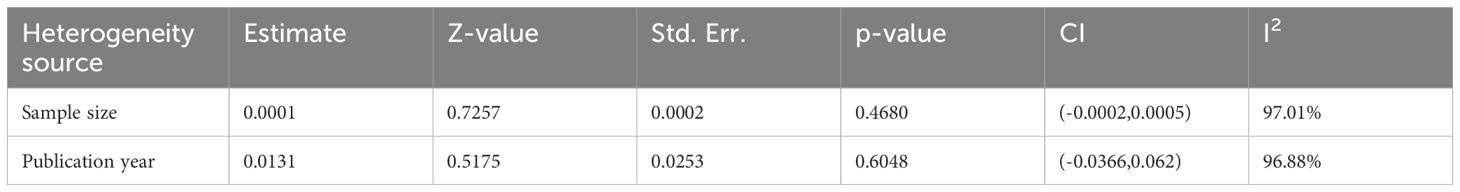
Table 3 Meta-regression analysis of factors affecting between-study heterogeneity in the prevalence of preparedness of diabetes mellitus services in health facilities.
Sensitivity analysis
The sensitivity analysis of the study was conducted. The random effects model was used to calculate a combined estimate, which showed significant variation in the evaluation of health facilities’ preparedness for DM services. To address this variation, sensitivity analysis and subgroup analysis were performed. These analyses aimed to understand the potential impact of individual studies on the overall estimate of the prevalence of DM service preparedness. Importantly, the results from the random effects model did not identify any studies that had an excessive influence on the overall estimate. To further investigate the source of heterogeneity, a meta-regression analysis was conducted, considering factors such as sample size and year of publication. However, the results showed that neither sample size nor year of publication had a significant effect on the heterogeneity observed between studies (Table 3). In addition, a sensitivity analysis for sub-group analysis by the sampling method was conducted.
Sub-group analysis of service preparedness
This study examined 10 research studies conducted in Africa and analyzed nine records from Asia to evaluate the preparedness of healthcare services for diabetes mellitus. The results revealed that the pooled prevalence of diabetes mellitus service preparedness in African countries was estimated to be 50.0% (95% CI: 42.0–60.0, I2, 94.0%) with a p-value of less than 0.01. This means that, on average, approximately 50% of the required healthcare services for NCDs were prepared in African countries. Similarly, in Asia, the pooled prevalence of diabetes service availability was found to be 59.0% (95% CI: 52.0–68.0, I2, 88.0%) with a p-value of less than 0.01 (Figure 4). This indicates that, on average, approximately 59.0% of the necessary healthcare services for NCDs were prepared in Asian countries. These findings emphasize the disparities in healthcare service preparedness for NCDs across different regions. While Asia exhibited a higher prevalence of service preparedness compared to Africa, there is still room for improvement in both regions to ensure that the essential healthcare services that individuals with NCDs need are prepared. The subgroup analysis was conducted based on sampling method of each studies. Accordingly, the highest pooled prevalence of diabetes service preparedness was observed in simple random sampling with a pooled prevalence of 55% (95% CI:37.0-82.0) and heterogeneity of 88%, p value<0.01. The second highest pooled prevalence was observed in stratified random sampling method after incorporating nine articles with a pooled result of 53% (95%CI:47-60), I2 = 91%, p value ≤ 0.01 (Figure 5).
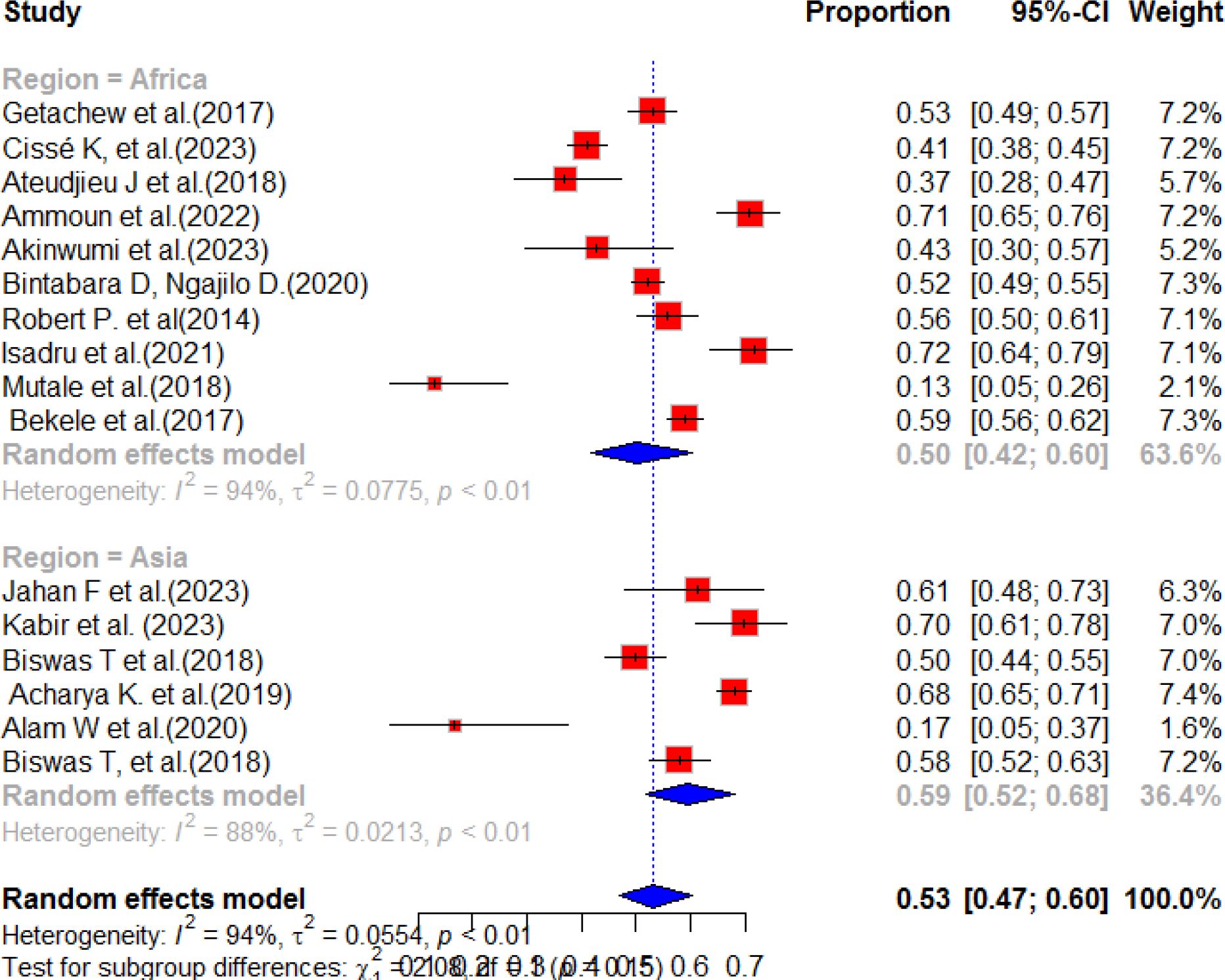
Figure 4 Sub-group analysis of the service preparedness of health facilities to deliver diabetes mellitus services in resource-limited countries.
Pooled prevalence of service availability for diabetes mellitus
According to previous literature, the availability of diabetic mellitus health services varies in resource-limited countries. A systematic synthesis of these studies revealed that the overall pooled prevalence of service availability was 48% (95%CI: 36.0, 67.0), with a high level of heterogeneity (97%) and a significant p-value of less than 0.01. The results of this systematic synthesis are presented in Figure 6.
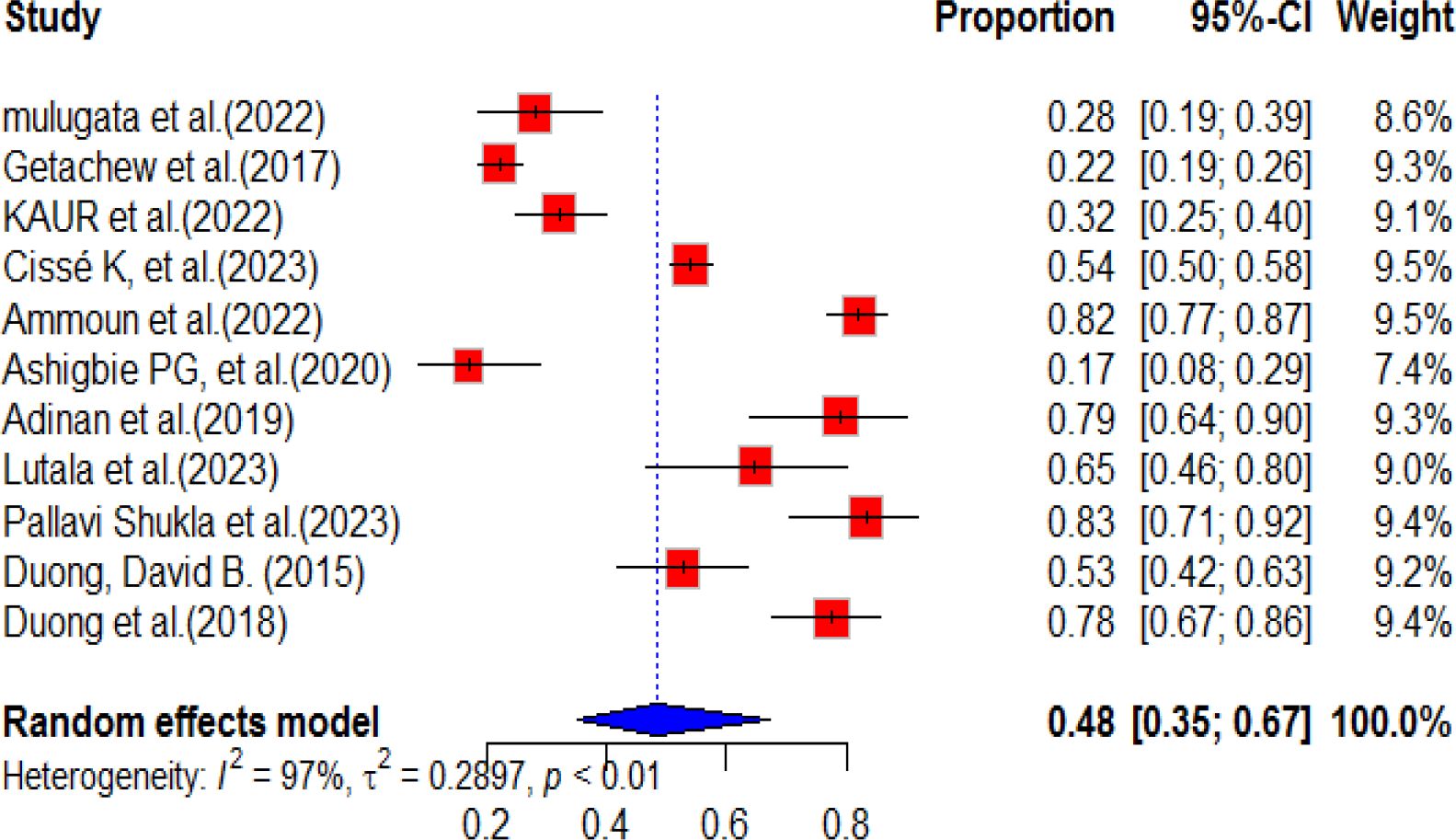
Figure 6 Forest plot of the availability of DM service in health facilities in resource-limited countries.
Sub-group analysis of diabetes service availability
According to a systematic review and meta-analysis, sub-group analyses were conducted for each region included in the individual studies. The highest prevalence of diabetes service availability was observed in Asia, with a pooled prevalence of 58% (95% CI: 38.0-89.0). However, there was a high level of heterogeneity (I2 = 95%, p-value<0.01) in this region. In contrast, the pooled prevalence of diabetes mellitus service availability in Africa was relatively low, at 43% (95% CI: 27.0-69.0), with a high level of heterogeneity (98%, p-value<0.01). The overall pooled prevalence of diabetes mellitus service availability in resource-limited countries was found to be 48% (95% CI: 35.0-67.0) (Figure 7). A subgroup analysis was conducted based on the sampling method and, based on the finding, five studies were included for multi-stage sampling with a pooled prevalence of 50.0% (95%CI: 27.0-93.0) and heterogeneity of 93%, p value<0.01 (Figure 8).
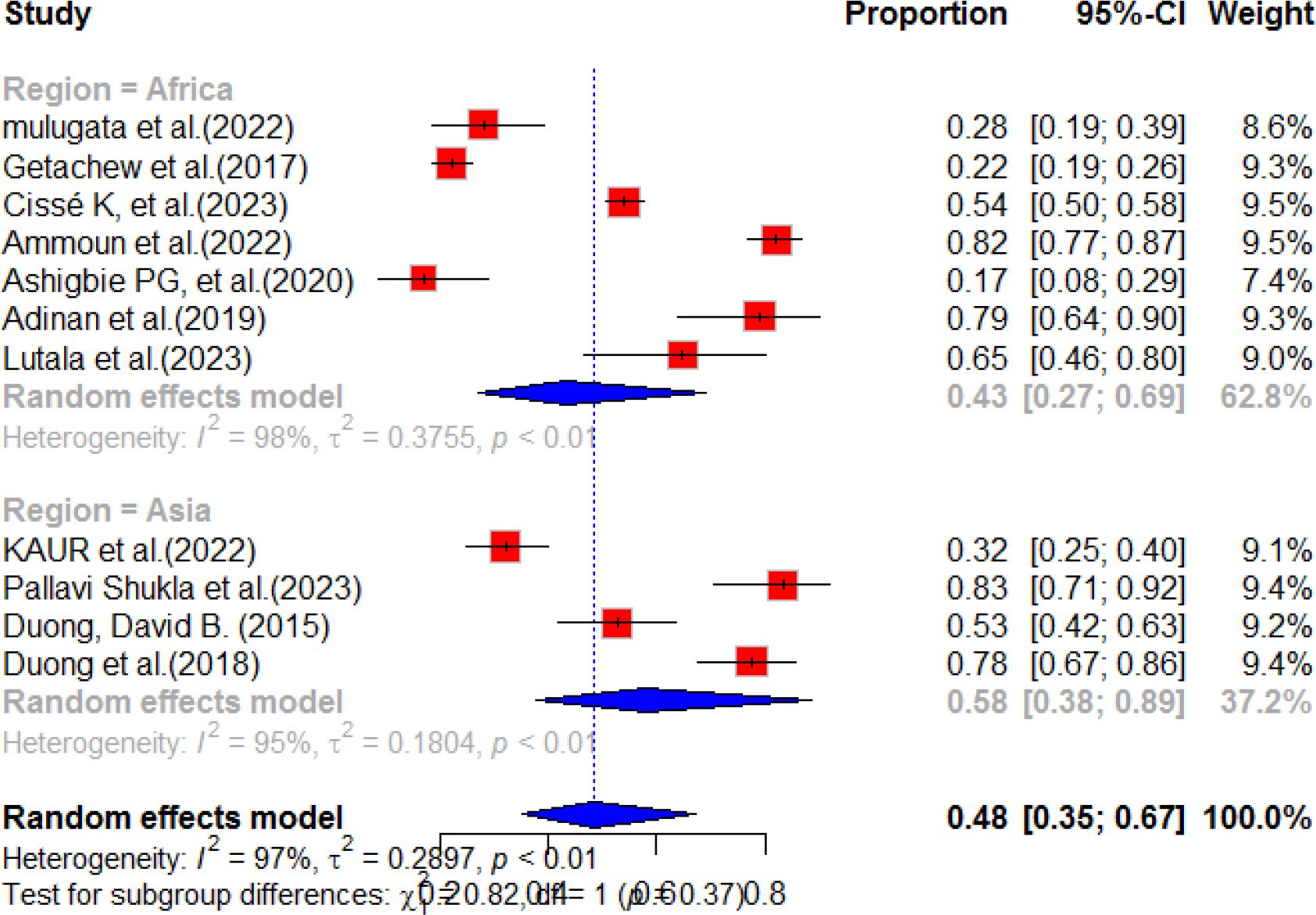
Figure 7 Sub-group analysis forest plot of the availability of diabetes services in health facilities in resource-limited countries.
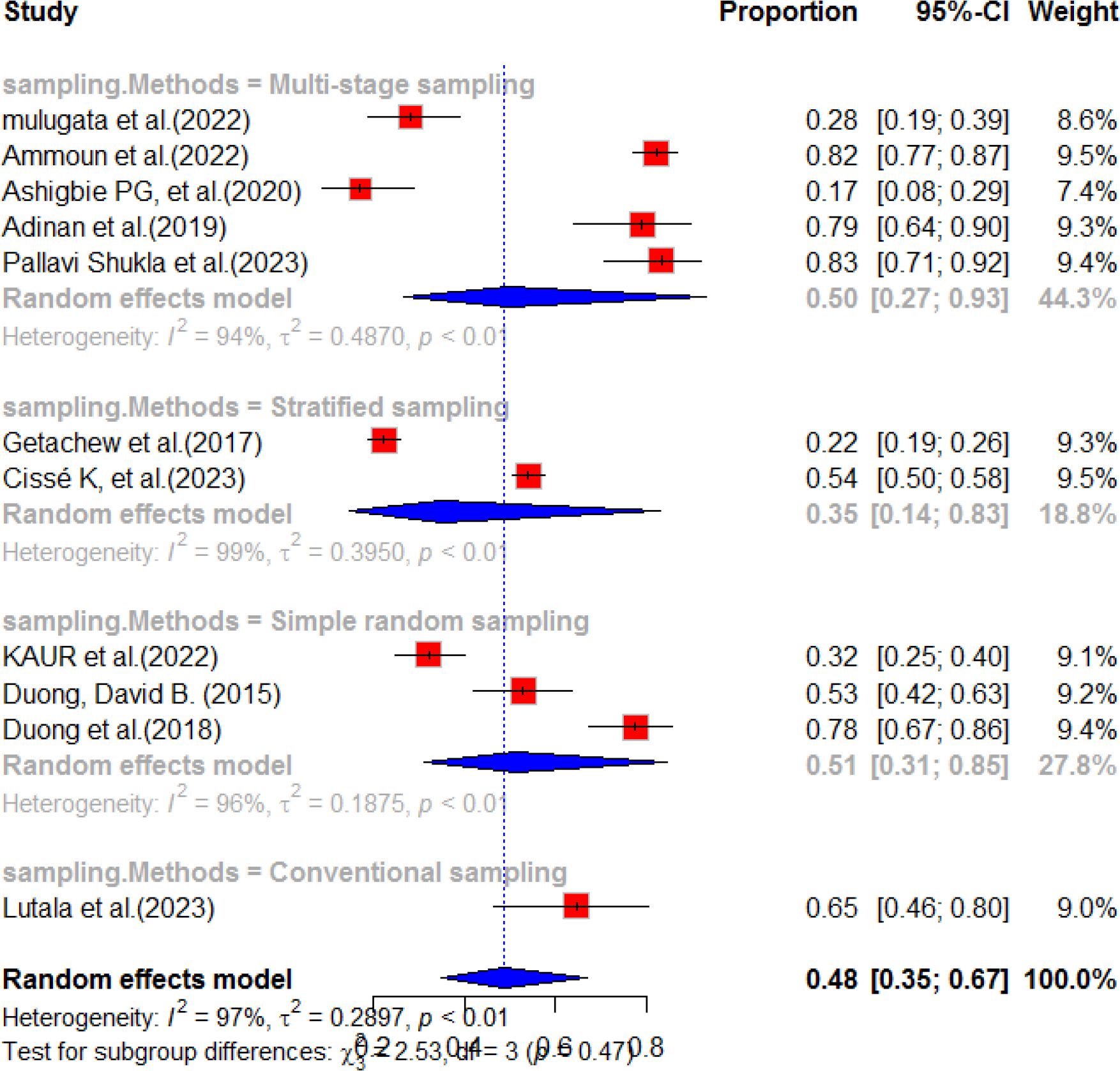
Figure 8 Subgroup analysis by the sampling method of diabetes service availability in resource limited-countries, 2024.
Meta-bias in prevalence of diabetes service availability
The publication bias of the studies was checked by using the Egger’s test and funnel plot asymmetry. The Egger’s test of the studies indicated that there is no publication bias. The quantitative heterogeneity of the studies was tau2 = 0.6444[0.3386; 1.7139]; tau = 0.8027 [0.5819; 1.309] and I2 = 98.1% [97.6%; 98.5%]; H=7.19[6.40; 8.09]. The graphic presentation of this publication bias is presented in funnel plot. The funnel plot of this systematic review indicate there is no visible publication bias (Figure 9). The Egger’s test was statistically non-significant with a p-value of 0.1221, with a bias estimate of -5.4489 (SE = 3.1925). Since the Egger’s test was not significant, trim and fill analysis was not necessary to conduct.
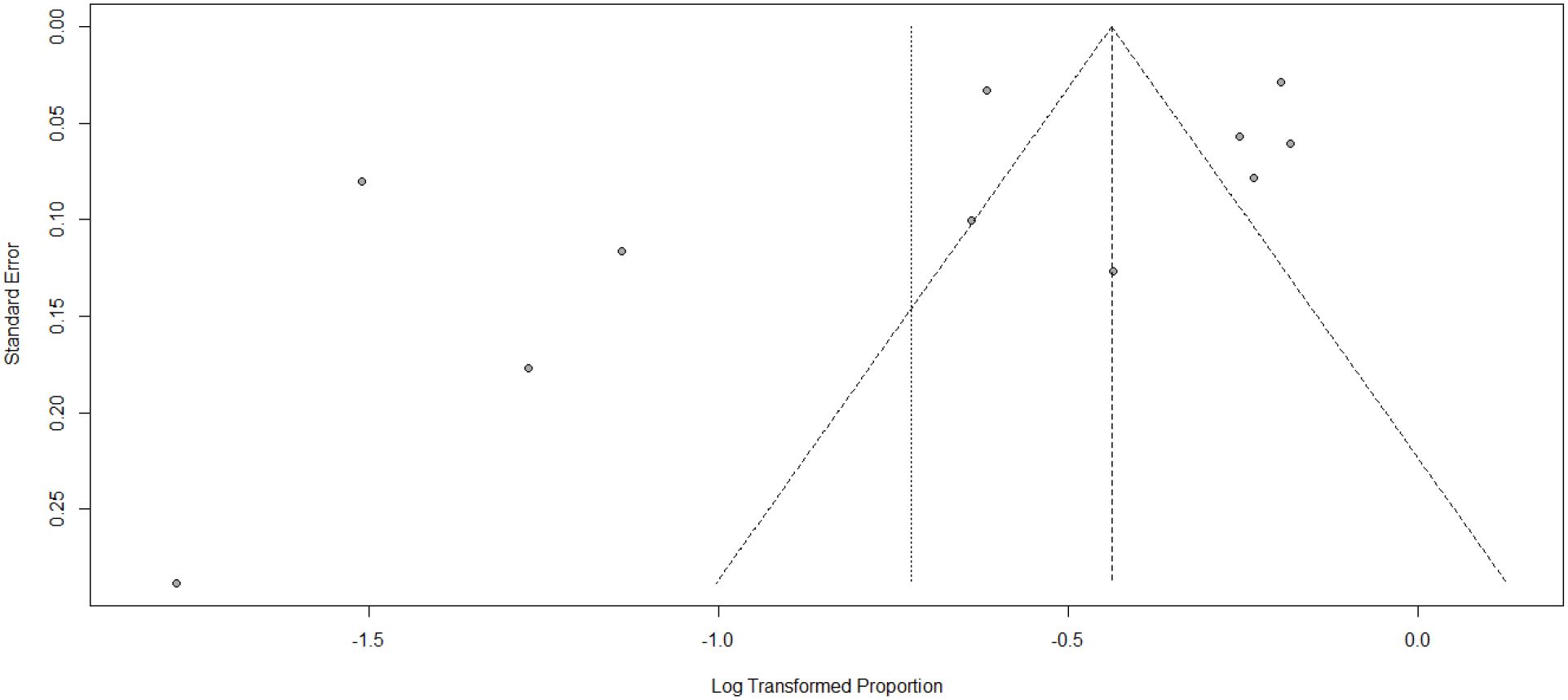
Figure 9 Funnel plot showing publication bias among studies used to compute diabetes service availability in resource-limited countries, 2024.
Sensitivity analysis
Sensitivity analysis of the studies was conducted and the result is presented in Figure 9. The random effects model was used to calculate a combined estimate, which showed significant variation in the evaluation of the availability of health facilities’ DM services. To address this variation, sensitivity analysis and subgroup analysis were performed. The sensitivity analysis of the study showed all had equal contribution except two studies. These analyses aimed to understand the potential impact of individual studies on the overall estimate of the prevalence of DM service availability. Importantly, the results from the random effects model did not identify any studies that had an excessive influence on the overall estimate. In addition, a sensitivity analysis was also conducted based on subgroup analysis by the sampling method. Nearly all the studies contributed to the pooled result for diabetes service availability. To further investigate the source of heterogeneity, a meta-regression analysis was conducted, considering factors such as sample size and year of publication. However, the results showed that neither sample size nor year of publication had a significant effect on the heterogeneity observed between studies (Table 4).
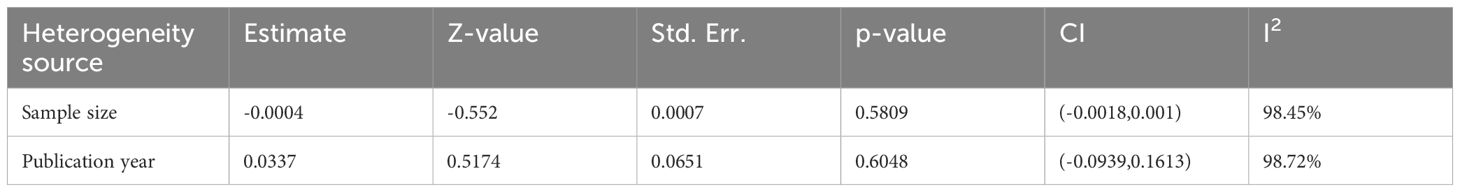
Table 4 Meta-regression analysis of factors affecting between-study heterogeneity in the prevalence of availability of diabetes mellitus services in health facilities.
Risk of bias evaluation
The Newcastle-Ottawa Scale (NOS) was used to evaluate the quality and potential bias of the studies. This assessment system considers three key parameters: selection, comparability, and outcome. A maximum of 9 points can be assigned, with one author conducting the assessment and another author independently reviewing it to ensure accuracy. The total score determines the level of bias risk, which is categorized as high (less than 5 points), moderate (between 6 and 7 points), or low (between 8 and 9 points) (57) (Supplementary Table 1).
Discussion
This study aimed to assess diabetes service preparedness and availability in resource-limited countries. The meta-analysis revealed that the pooled estimated diabetes service preparedness in healthcare facilities was 53.0%, which is higher than previous studies conducted in Nigeria (58), Burkina Faso (59), and Bangladesh (28). The disparity may be attributed to policies and program variation across the countries regarding diabetes service preparedness in healthcare systems. Other possible explanations for this finding could be variation in health system readiness and some health system only consider the provider perspective. Moreover, the pooled evidence from our study provides stronger support compared to the individual studies conducted in a single area. This highlights the importance of conducting multi-country and multidimensional studies when designing programs and shaping policies for non-communicable disease control. It is evident that in resource-limited countries there are numerous undiagnosed cases of diabetes mellitus, which may be attributed to inadequately prepared health facilities.
The findings of this systematic review on diabetes service preparedness are lower than those of a study conducted in Uganda (32). This difference suggests that health systems can vary significantly between countries. The World Health Organization has also highlighted the variation in health system preparedness across different nations (60). Insufficient preparedness of healthcare facilities to deliver diabetes management services has been identified as a concern (29–35, 38). The possible explanation for this could be that the approaches and the methodologies of health systems may vary from country to country. These findings highlight the need to enhance the readiness of health facilities in low-resource countries to effectively address the escalating diabetes epidemic. The measurement of health system preparedness is universally accepted and recognized worldwide. This indicates that a country’s preparedness is influenced by factors such as political commitment, economic growth, and structural elements. Consequently, addressing the preparedness of diabetes mellitus services requires a multidimensional approach and involvement from multiple sectors.
According to our systematic review and meta-analysis result, the level of health facility preparedness for diabetes mellitus in Africa was found to be 50% (95% CI; 42.0, 60.0). However, in Asia, the pooled prevalence of diabetic service preparedness was higher, at 59% (95% CI: 52.0, 68.0). In comparison, Africa had a lower prevalence of service preparedness for diabetes mellitus. This could be due to Africa being focused on the management of acute infections (61). The study also suggested that the preparedness of diabetic services in different countries and regions is closely linked to their economic growth and health system priority. Therefore, it is crucial for resource-limited countries to focus on service mitigation and integration to address the preparedness problem and reduce the burden of undiagnosed diabetes mellitus in their communities.
Service availability in healthcare is crucial for identifying and managing chronic illnesses in a community. Unfortunately, in 2013, an estimated 174.8 million people worldwide (62) were undiagnosed with diabetes due to various reasons. This systematic review and meta-analysis revealed that the availability of diabetes mellitus services in resource-limited countries was only 48%. This is lower than the World Health Organization’s recommendation that at least 80% (36) of health facilities should have essential medication available. The finding is lower than studies conducted in Kenya (48), Tanzania (30), India (54), and Vietnam (56). The slow pace at which these countries are addressing the growing burden of diabetes is concerning. Inadequate availability of essential anti-diabetic medication has also been reported in other low-resource settings in different countries (29–35, 38). Additionally, while diabetes management guidelines were more likely to be present in health facilities, trained workers were less common. This is alarming because even if protocols are available, they may not be followed if employees are not properly trained. This implies that mitigation health sector transformation with multi-sectorial collaboration is essential to improve the availability of diabetes mellitus services in resource limited countries. In addition, appropriate and mitigated implementation of universal health coverage with strict follow up could improve the availability of the services. Furthermore, working in a balanced way, with both supply-side and demand-side perspectives and the effective implementation of the WHO health system framework, could be improve the availability of diabetes mellitus services in resource-limited setting.
The sub-group analysis indicated that Asia had a higher service availability compared with Africa. While the implementation of universal health coverage (63) has been incorporated all over the world, resource variation and limitation may contribute to the variation of diabetes mellitus service availability. This implies that effective implementation and monitoring of universal health coverage could improve the availability of diabetes services in resource-limited countries.
Conclusion
The findings of this systematic review and meta-analysis fall below the targets set by the World Health Organization (36). The overall pooled prevalence of service availability and service preparedness were lower than the sustainable development goal of health for all and the WHO’s availability of services (24, 36). The findings highlight the urgent need for interventions and improvements in healthcare services in resource-limited countries. Governments should prioritize the implementation of universal healthcare and primary healthcare to enhance service availability. Investing in health facilities and integrating services for non-communicable and infectious diseases can improve healthcare capacity and preparedness. A tailored and action-oriented approach to health system strengthening is crucial for improving the preparedness and availability of diabetes mellitus services.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
MA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. DG: Conceptualization, Formal analysis, Methodology, Project administration, Supervision, Visualization, Writing – original draft, Writing – review & editing. AA: Funding acquisition, Investigation, Methodology, Software, Visualization, Writing – original draft, Writing – review & editing. YN: Data curation, Formal analysis, Methodology, Software, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2024.1427175/full#supplementary-material
Abbreviations
DM, diabetes mellitus; NCD, No communicable disease; UHC, Universal Health Coverage (UHC); PICOS=participant, intervention, Comparison, Outcome, Study design; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; WHO, World Health Organization.
References
1. World Health Organization. Noncommunicable diseases: progress monitor 2022. Geneva, Switzerland: World Health Organization (2022). Available at: https://apps.who.int/iris/bitstream/handle/10665/353048/9789240047761-eng.pdf.
2. Smith L, Shin JI, Hwang SY, Tizaoui K, Dragioti E, Jacob L, et al. Global Burden of Disease study at the World Health Organization: research methods for the most comprehensive global study of disease and underlying health policies. Life Cycle. (2022) 2:e8. doi: 10.54724/lc.2022.e8
3. Budreviciute A, Damiati S, Sabir DK, Kodzius R. Management and prevention strategies for non-communicable diseases (NCDs) and their risk factors. Front Public Health. (2020) 8:574111. doi: 10.3389/fpubh.2020.574111
4. Collaborators GRF. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet (London England). (2016) 388:1659. doi: 10.1016/S0140-6736(16)31679-8
5. Wamai RG, Kengne AP, Levitt N. Non-communicable diseases surveillance: overview of magnitude and determinants in Kenya from STEPwise approach survey of 2015. BMC Public Health. (2018) 18:1–8. doi: 10.1186/s12889-018-6051-z
6. Roth G, Global Burden of Disease Collaborative Network. Global burden of disease study 2017 (GBD 2017) results. Seattle, United States: institute for health metrics and evaluation (IHME), 2018. Lancet. (2018) 392:1736–88. doi: 10.1016/S0140-6736(18)32203-7
7. WHO CO. Responding to community spread of COVID-19 reference WHO/COVID-19/community_Transmission/20201. Geneva, Switzerland: World health organization (2020).
8. Afroz A, Zhang W, Loh AJW, Lee DXJ, Billah B. Macro-and micro-vascular complications and their determinants among people with type 2 diabetes in Bangladesh. Diabetes Metab Syndrome: Clin Res Rev. (2019) 13:2939–46. doi: 10.1016/j.dsx.2019.07.046
9. Goyal R, Singhal M, Jialal I. Type 2 diabetes. In: StatPearls. StatPearls Publishing, Treasure Island (FL (2023).
10. Organization WH. Building resilience: a key pillar of health 2020 and the sustainable development goals: examples from the WHO small countries initiative. Budapest, Norway: Iris International repository (2017).
11. Latif ZA, Ashrafuzzaman S, Amin MF, Gadekar AV, Sobhan MJ, Haider T. A cross-sectional Study to evaluate diabetes management, control and complications in patients with type 2 diabetes in Bangladesh. BIRDEM Med J. (2017) 7:17–27. doi: 10.3329/birdem.v7i1.31268
12. Stringer JS, Chisembele-Taylor A, Chibwesha CJ, Chi HF, Ayles H, Manda H, et al. Protocol-driven primary care and community linkages to improve population health in rural Zambia: the Better Health Outcomes through Mentoring and Assessment (BHOMA) project. BMC Health Serv Res. (2013) 13:1–10. doi: 10.1186/1472-6963-13-S2-S7
13. Biswas T, Haider MM, Gupta RD, Uddin J. Assessing the readiness of health facilities for diabetes and cardiovascular services in Bangladesh: a cross-sectional survey. BMJ Open. (2018) 8:e022817. doi: 10.1136/bmjopen-2018-022817
14. Dessie G, Mulugeta H, Amare D, Negesse A, Wagnew F, Getaneh T, et al. A systematic analysis on prevalence and sub-regional distribution of undiagnosed diabetes mellitus among adults in African countries. J Diabetes Metab Disord. (2020) 19:1931–41. doi: 10.1007/s40200-020-00635-9
15. Bantie GM, Wondaye AA, Arike EB, Melaku MT, Ejigu ST, Lule A, et al. Prevalence of undiagnosed diabetes mellitus and associated factors among adult residents of Bahir Dar city, northwest Ethiopia: a community-based cross-sectional study. BMJ Open. (2019) 9(10):e030158. doi: 10.1136/bmjopen-2019-030158
16. Damtie S, Workineh L, Berhan A, Tiruneh T, Legese B, Getie B, et al. The magnitude of undiagnosed diabetes mellitus, prediabetes, and associated factors among adults living in Debre Tabor town, northcentral Ethiopia: A community-based cross-sectional study. Heliyon. (2023) 9(7):e17729. doi: 10.1016/j.heliyon.2023.e17729
17. Ogurtsova K, Guariguata L, Barengo NC, Ruiz PL-D, Sacre JW, Karuranga S, et al. IDF diabetes Atlas: Global estimates of undiagnosed diabetes in adults for 2021. Diabetes Res Clin practice. (2022) 183:109118. doi: 10.1016/j.diabres.2021.109118
18. Rahman M, Nakamura K, Kizuki M. Socioeconomic differences in the prevalence, awareness, and control of diabetes in Bangladesh. J Diabetes its Complications. (2015) 29:788–93. doi: 10.1016/j.jdiacomp.2015.04.011
19. Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas. Diabetes Res Clin practice. (2019) 157:107843. doi: 10.1016/j.diabres.2019.107843
20. O'Neill K, Takane M, Sheffel A, Abou-Zahr C, Boerma T. Monitoring service delivery for universal health coverage: the Service Availability and Readiness Assessment. Bull World Health organization. (2013) 91:923–31. doi: 10.2471/BLT.12.116798
21. WHO G. Global status report on noncommunicable diseases 2010. Geneva, Switzerland: WHO Library Cataloguing-in-Publication Data (2011).
22. Ssengooba F, Kiwanuka S, Rutebemberwa E, Ekirapa-Kiracho E. Universal health coverage in Uganda: looking back and forward to speed up the progress. Kampala Uganda: Makerere University (2017).
23. WHA71 R. 1. Thirteenth general programme of work 2019– 2023. Seventy-first World Health Assembly Vol. 25. Geneva: World Health Organization (2018).
25. Federation ID. IDF diabetes atlas. 8th edition. Brussels, Belgium: International diabetes federation (2017) p. 905–11.
26. Organization WH. Service availability and readiness assessment (SARA). Geneva, Switzerland: WHO (2019).
27. Ghimire U, Shrestha N, Adhikari B, Mehata S, Pokharel Y, Mishra SR. Health system’s readiness to provide cardiovascular, diabetes and chronic respiratory disease related services in Nepal: analysis using 2015 health facility survey. BMC Public Health. (2020) 20:1–15. doi: 10.1186/s12889-020-09279-z
28. Alam W, Nujhat S, Parajuli A, Banyira L, Mohsen WAM, Sutradhar I, et al. Readiness of primary health-care facilities for the management of non-communicable diseases in rural Bangladesh: a mixed methods study. Lancet Global Health. (2020) 8:S17. doi: 10.1016/S2214-109X(20)30158-3
29. Mutale W, Bosomprah S, Shankalala P, Mweemba O, Chilengi R, Kapambwe S, et al. Assessing capacity and readiness to manage NCDs in primary care setting: Gaps and opportunities based on adapted WHO PEN tool in Zambia. PloS One. (2018) 13:e0200994. doi: 10.1371/journal.pone.0200994
30. Adinan J, Manongi R, Temu GA, Kapologwe N, Marandu A, Wajanga B, et al. Preparedness of health facilities in managing hypertension & diabetes mellitus in Kilimanjaro, Tanzania: a cross sectional study. BMC Health Serv Res. (2019) 19:1–9. doi: 10.1186/s12913-019-4316-6
31. Peck R, Mghamba J, Vanobberghen F, Kavishe B, Rugarabamu V, Smeeth L, et al. Preparedness of Tanzanian health facilities for outpatient primary care of hypertension and diabetes: a cross-sectional survey. Lancet Global Health. (2014) 2:e285–e92. doi: 10.1016/S2214-109X(14)70033-6
32. Isadru VR, Nanyonga RC, Alege JB. Health facilities’ readiness to manage hypertension and diabetes cases at primary health facilities in bidibidi refugee settlement, Yumbe District, Uganda. J Trop Med. (2021) 2021:1415794. doi: 10.1155/2021/1415794
33. Bintabara D, Shayo FK. Disparities in availability of services and prediction of the readiness of primary healthcare to manage diabetes in Tanzania. Primary Care Diabetes. (2021) 15:365–71. doi: 10.1016/j.pcd.2020.11.007
34. Bekele A, Getachew T, Amenu K, Defar A, Teklie H, Gelibo T, et al. Service availability and readiness for diabetes care at health facilities in Ethiopia. Ethiopian J Health Dev. (2017) 31:110–8.
35. Tolu G, Tafese F, Nemera G, Teferi E, Wondafrash B, Fekadu S. Readiness of primary health care facilities in Jimma zone to provide diabetic services for diabetic clients, Jimma zone, southwest Ethiopia, March 2013. (2016).
36. Rawal LB, Kanda K, Biswas T, Tanim MI, Poudel P, Renzaho AM, et al. Non-communicable disease (NCD) corners in public sector health facilities in Bangladesh: a qualitative study assessing challenges and opportunities for improving NCD services at the primary healthcare level. BMJ Open. (2019) 9:e029562. doi: 10.1136/bmjopen-2019-029562
37. Islam MR, Laskar SP, Macer D. A study on service availability and readiness assessment of non-communicable diseases using the who tool for Gazipur district in Bangladesh. Bangladesh J Bioethics. (2016) 7:1–13. doi: 10.3329/bioethics.v7i2.30785
38. Bintabara D, Ngajilo D. Readiness of health facilities for the outpatient management of non-communicable diseases in a low-resource setting: an example from a facility-based cross-sectional survey in Tanzania. BMJ Open. (2020) 10:e040908. doi: 10.1136/bmjopen-2020-040908
39. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J surgery. (2021) 88:105906. doi: 10.1016/j.ijsu.2021.105906
40. Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. (2012) 65:934–9. doi: 10.1016/j.jclinepi.2011.11.014
41. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58. doi: 10.1002/sim.1186
42. Getachew T, Bekele A, Amenu K, Defar A, Teklie H, Taye G, et al. Service availability and readiness for major non-communicable diseases at health facilities in Ethiopia. Ethiopian J Health Dev. (2017) 31:384–90.
43. Jahan F, Ahmed A, Mohsin FM, Rahman S, Sayeed A, Nahar L, et al. Changes in the readiness of healthcare systems to provide diabetes-and cardiovascular disease-related services: A comparison of indices using data from the 2014 and 2017 Bangladesh Health Facility Surveys. F1000Research. (2023) 12:898. doi: 10.12688/f1000research
44. Kabir A, Karim MN, Billah B. The capacity of primary healthcare facilities in Bangladesh to prevent and control non-communicable diseases. BMC Primary Care. (2023) 24:60. doi: 10.1186/s12875-023-02016-6
45. Cissé K, Samadoulougou S, Kaboré J, Somda P, Zongo A, Traoré S, et al. Healthcare system’s preparedness to provide cardiovascular and diabetes-specific care in the context of geopolitical crises in Burkina Faso: a trend analysis from 2012 to 2018. BMJ Open. (2023) 13:e065912. doi: 10.1136/bmjopen-2022-065912
46. Ateudjieu J, Awolu MM, Martin YN, Joel BE, Thomas A, Watcho P, et al. Assessing the availability and readiness of diabetes healthcare service in the west region of Cameroon. Int J Adv Res Publications. (2018) 2:79–84. doi: 10.3399/bjgp16X683509
47. Yusuf SS, Acharya K, Ahmed R, Ahmed A. Understanding general health service readiness and its correlates in the health facilities of Bangladesh: evidence from the Bangladesh Health Facility Survey 2017. J Public Health. (2021), 1–12. doi: 10.1007/s10389-021-01522-0
48. Ammoun R, Wami WM, Otieno P, Schultsz C, Kyobutungi C, Asiki G. Readiness of health facilities to deliver non-communicable diseases services in Kenya: a national cross-sectional survey. BMC Health Serv Res. (2022) 22:985. doi: 10.1186/s12913-022-08364-w
49. Akinwumi AF, Esimai OA, Arije O, Ojo TO, Esan OT. Preparedness of primary health care facilities on implementation of essential non-communicable disease interventions in Osun state South-West Nigeria: a rural–urban comparative study. BMC Health Serv Res. (2023) 23:154. doi: 10.1186/s12913-023-09138-8
50. Mulugeta TK, Kassa DH. Readiness of the primary health care units and associated factors for the management of hypertension and type II diabetes mellitus in Sidama, Ethiopia. PeerJ. (2022) 10:e13797. doi: 10.7717/peerj.13797
51. Kaur P, Borah P, Gaigaware P, Mohapatra P, Das NK, Uike PV, et al. Preparedness of primary & secondary care health facilities for the management of non-communicable diseases in tribal population across 12 districts in India. Indian J Med Res. (2022) 156:260–8. doi: 10.4103/ijmr.ijmr_3248_21
52. Ashigbie PG, Rockers PC, Laing RO, Cabral HJ, Onyango MA, Buleti JPL, et al. Availability and prices of medicines for non-communicable diseases at health facilities and retail drug outlets in Kenya: a cross-sectional survey in eight counties. BMJ Open. (2020) 10:e035132. doi: 10.1136/bmjopen-2019-035132
53. Lutala P, Nyasulu P, Muula AS. Perceived readiness for diabetes and cardiovascular care delivery in Mangochi, Malawi: multicentre study from healthcare providers’ perspectives. BMC Primary Care. (2023) 24:85. doi: 10.1186/s12875-023-02033-5
54. Shukla P, Priya H, Meena JK, Singh S, Bairwa M, Saini A. Readiness and motivation of ASHAs towards their participation in non-communicable disease control programmein north India: A cross sectional study. Asian Pacific J Cancer Prevention: APJCP. (2023) 24:3235. doi: 10.31557/APJCP.2023.24.9.3235
55. Duong DB. Understanding the service availability for non-communicable disease prevention and control at Public Primary Care Centers in Northern Vietnam. Harvard Library (2015) 10–22.
56. Duong DB, Van Minh H, Ngo LH, Ellner AL. Readiness, availability and utilization of rural Vietnamese health facilities for community based primary Care of non-communicable Diseases: a CrossSectional survey of 3 provinces in northern Vietnam. Int J Health Policy management. (2019) 8:150. doi: 10.15171/ijhpm.2018.104
57. Luchini C, Veronese N, Nottegar A, Shin JI, Gentile G, Granziol U, et al. Assessing the quality of studies in meta-research: Review/guidelines on the most important quality assessment tools. Pharm statistics. (2021) 20:185–95. doi: 10.1002/pst.2068
58. Akinwumi AF, Esimai OA, Arije O, Ojo TO, Esan OT. Preparedness of primary health care facilities on implementation of essential non-communicable disease interventions in Osun State South-West Nigeria: a rural–urban comparative study. BMC Health Serv Res. (2023) 23:1–12. doi: 10.1186/s12913-023-09138-8
59. Cissé K, Kirakoya F. Health facilities readiness to provide primary cardiometabolic healthcare in Burkina Faso, 2012-2018. Eur J Public Health. (2022) 32:ckac129. 651. doi: 10.1093/eurpub/ckac129.651
60. Organization WH. Service availability and readiness assessment (SARA). Geneva, Switzerland: World Health Organization (2015).
61. Beaglehole R, Epping-Jordan J, Patel V, Chopra M, Ebrahim S, Kidd M, et al. Improving the prevention and management of chronic disease in low-income and middle-income countries: a priority for primary health care. Lancet. (2008) 372:940–49. doi: 10.1016/S0140-6736(08)61404-X
62. Beagley J, Guariguata L, Weil C, Motala AA. Global estimates of undiagnosed diabetes in adults. Diabetes Res Clin practice. (2014) 103:150–60. doi: 10.1016/j.diabres.2013.11.001
63. World health organization. Universal health coverage 2020 (2024). Available online at: https://www.google.com/url?sa=t&source=web&rct=j&opi=89978449.
Keywords: availability, preparedness, diabetes mellitus, DM, low and middle countries
Citation: Alie MS, Girma D, Adugna A and Negesse Y (2024) Diabetes mellitus service preparedness and availability: a systematic review and meta-analysis. Front. Endocrinol. 15:1427175. doi: 10.3389/fendo.2024.1427175
Received: 03 May 2024; Accepted: 28 June 2024;
Published: 19 July 2024.
Edited by:
Hamid Reza Baradaran, Iran University of Medical Sciences, IranReviewed by:
Seyyed Amir Yasin Ahmadi, Iran University of Medical Sciences, IranModupi Peter Mphekgwana, University of Limpopo, South Africa
Copyright © 2024 Alie, Girma, Adugna and Negesse. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Melsew Setegn Alie, bWVsc2V3c2V0ZWduMjAxMEBnbWFpbC5jb20=
 Melsew Setegn Alie
Melsew Setegn Alie Desalegn Girma2
Desalegn Girma2 Yilkal Negesse
Yilkal Negesse