- Department of Nephrology, People’s Hospital of Zhengzhou University, He’nan Provincial People’s Hospital, He’nan Provincial Key Laboratory of Kidney Disease and Immunology, Zhengzhou, China
Aim: Sodium-glucose cotransporter protein 2 (SGLT2) inhibitors have been shown to have renoprotective effects in clinical studies. For further validation in terms of genetic variation, drug-targeted Mendelian randomization (MR) was used to investigate the causal role of SGLT2 inhibition on eGFR effects.
Methods: Genetic variants representing SGLT2 inhibition were selected as instrumental variables. Drug target Mendelian randomization analysis was used to investigate the relationship between SGLT2 inhibitors and eGFR. The IVW method was used as the primary analysis method. As a sensitivity analysis, GWAS pooled data from another CKDGen consortium was used to validate the findings.
Results: MR results showed that hemoglobin A1c (HbA1c) levels, regulated by the SLC5A2 gene, were negatively correlated with eGFR (IVW β -0.038, 95% CI -0.061 to -0.015, P = 0.001 for multi-ancestry populations; IVW β -0.053, 95% CI -0.077 to -0.028, P = 2.45E-05 for populations of European ancestry). This suggests that a 1-SD increase in HbA1c levels, regulated by the SLC5A2 gene, is associated with decreased eGFR. Mimicking pharmacological inhibition by lowering HbA1c per 1-SD unit through SGLT2 inhibition reduces the risk of eGFR decline, demonstrating a renoprotective effect of SGLT2 inhibitors. HbA1c, regulated by the SLC5A2 gene, was negatively correlated with eGFR in both validation datasets (IVW β -0.027, 95% CI -0.046 to -0.007, P=0.007 for multi-ancestry populations, and IVW β -0.031, 95% CI -0.050 to -0.011, P=0.002 for populations of European origin).
Conclusions: The results of this study indicate that the SLC5A2 gene is causally associated with eGFR. Inhibition of SLC5A2 gene expression was linked to higher eGFR. The renoprotective mechanism of SGLT2 inhibitors was verified from the perspective of genetic variation.
1 Introduction
Chronic Kidney Disease (CKD) is a disease that seriously jeopardizes human health. In recent years, cardiorenal protection studies have made significant progress in patients with CKD, and the introduction of sodium-glucose cotransporter protein 2 (SGLT2) inhibitors in particular has provided an important new tool in the treatment of CKD (1, 2). These inhibitors target SGLT2, which is responsible for the reabsorption of glucose and sodium in the proximal tubules of the kidneys. SGLT2 inhibitors lower glucose levels and blood pressure by lowering the renal threshold for glucose excretion and by promoting negative salt and water homeostasis. They also have an effect on glomerular hemodynamics, leading to a decrease in glomerular filtration rate, which is reversible when treatment is stopped. This phenomenon is known as “glomerular feedback”. In type 2 diabetes mellitus (T2DM), SGLT2 inhibitors affect glomerular ultrafiltration by decreasing vascular resistance and inducing vasodilation. In addition, these inhibitors reduce fibrosis in the proximal tubule by decreasing energy expenditure and inhibiting the mammalian target of rapamycin (mTOR) pathway (3). Another growing area of research is the ability of SGLT2 inhibitors to induce a fasting state (4). All of these effects reduce cellular stress and inflammation in cardiac and renal tissues, which is thought to be the pathophysiologic reason for the beneficial effects of SGLT2 inhibitors on cardiac and renal function (1).
SGLT2 inhibitors, including canagliflozin, dapagliflozin, and empagliflozin, are widely approved antihyperglycemic agents that improve insulin resistance (IR) (5), and are used to reduce glycemia and cardiovascular risk in T2DM patients (6). Large clinical trials provide compelling evidence to support their beneficial effects on major adverse cardiovascular events, hospitalization for heart failure (7–11) and renal outcomes (12, 13). However, studies on genetic variants related to SGLT2 inhibitors’ renoprotective effects are limited. The SLC5A2 gene encodes SGLT2, crucial for renal glucose reabsorption. Despite promising results in clinical studies, challenges such as variable patient responses and long-term effects remain. Addressing these challenges is essential to optimize clinical application.
In the field of precision medicine, finding effective molecular targets is a key task. Traditional methods to study the mechanism of action of target proteins through pharmacology are inefficient and time-consuming. The drug target Mendelian randomization (MR) has emerged as a novel and powerful research method. Novel methods such as gene co-localization and gene variants associated with drug target mRNA expression (expression quantitative trait loci (eQTL)) can be used to create MR tool variables for drug exposure (14). The eQTL is a type of expressed quantitative trait locus, which can be classified into cis-eQTL and trans-eQTL by analyzing the relationship between the amount of gene expression and the locus. The former regulates genes that are closer together, while the latter regulates genes that are farther apart. Drug target MR utilizes genetic instrumental variables to explore the causal relationship between molecules and diseases. This approach is based on the downstream products of target proteins, using Single Nucleotide Polymorphisms (SNPs) near the coding genes of the target proteins that have significant effects on these downstream products (protein Quantitative Trait Loci (pQTL) or eQTL) as the instrumental variables. The concentration of the downstream products of the target proteins serves as the exposure, while disease serves as the endpoint. MR is then performed to verify the effect of the target proteins on the studied diseases, providing new ideas for drug development and effect prediction. This strategy can be used to investigate the biological mechanism of the effect of SGLT2 inhibition on eGFR.
Given that the genetic mechanisms of SGLT2 inhibition in CKD protection are poorly understood, we hypothesized that SGLT2 inhibitors may be causally related to eGFR. Therefore, our study was designed to assess the genetic causal effect of SGLT2 inhibition on eGFR. We performed a two-sample MR analysis using genetic variants associated with SLC5A2 gene expression and hemoglobin A1c (HbA1c) levels as instrumental variables. This helps to expand our understanding of the mechanisms of SGLT2 inhibitors in renal protection and provides evidence for this.
2 Methods
2.1 Study design
Figure 1 illustrates a schematic of the study design. The study was conducted in the following five steps: 1) Genetic variants representing the effects of SGLT2 inhibition were selected as instrumental variables. 2) Pooled GWAS data for T2DM was selected as a positive control. 3) The outcome factor, eGFR, was selected. 4) MR analyses were performed to estimate the causal effects of SGLT2 inhibition on eGFR.
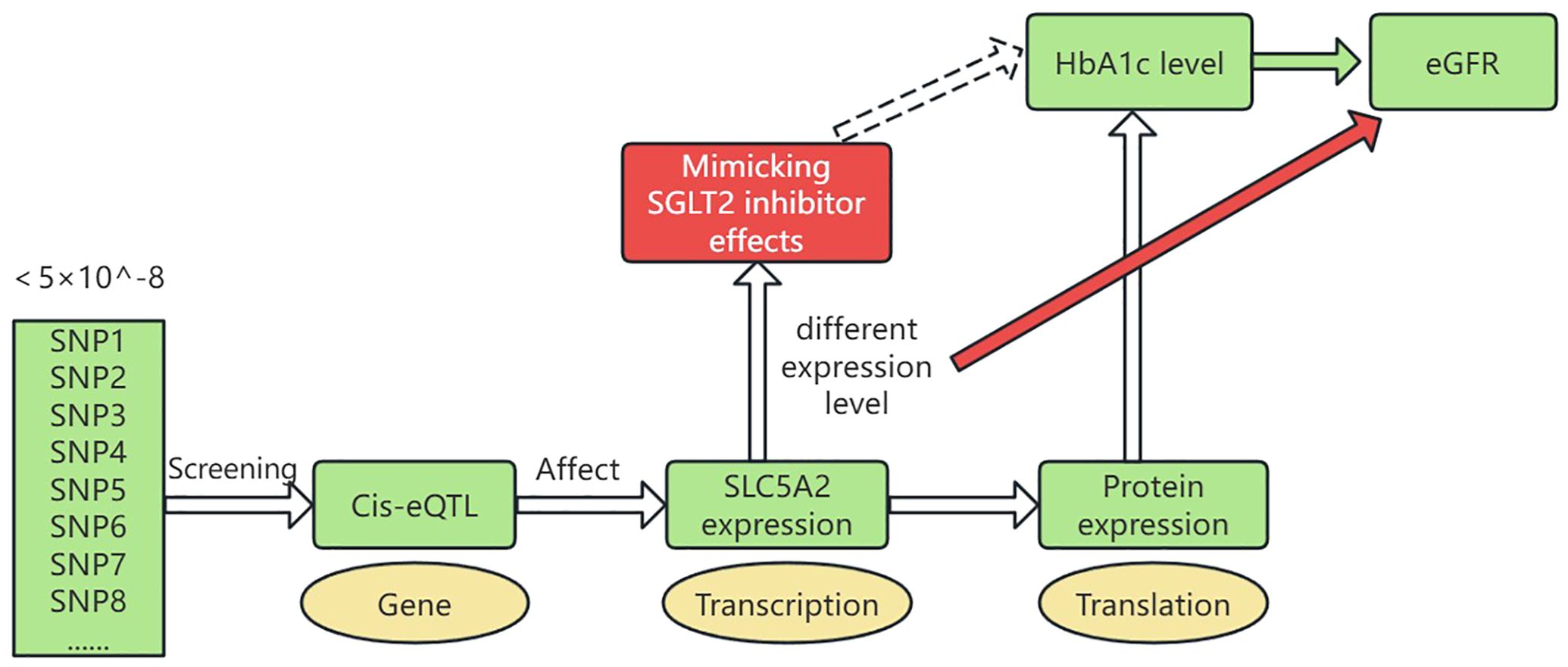
Figure 1. Drug-targeted MR study design. SGLT2, Sodium–glucose cotransporter 2; HbA1c, hemoglobin A1c; eGFR, estimated Glomerular Filtration Rate; cis-eQTL, cis-expression Quantitative Trait Locus. Genetic variants representing SLC5A2 gene expression levels were selected by screening cis-eQTLs with a genotype frequency of less than 5×10^-8. These variants influence SLC5A2 gene expression at the RNA transcription level. The expression further affects protein levels, which in turn influence HbA1c levels. Thus, different expression levels of the SLC5A2 gene can mimic the therapeutic effects of SGLT2 inhibitors (glucose-lowering effects, reduced HbA1c). We studied the impact of these varying expression levels on eGFR.
2.2 Data sources
2.2.1 Selection of genetic variants of SGLT2 inhibitors
The process of selecting genetic variants for SGLT2 inhibitors is described in detail in the study of Xu M. et al. (15). It involves four steps: First, genetic variants associated with SLC5A2 gene expression were selected by Genotype-Tissue Expression (GTEx) (16) and eQTLGen Consortium (17) data; second, the correlation of each SLC5A2 variant with HbA1c levels was assessed using UK Biobank data (18); then, the causal variants of SLC5A2 with HbA1c were verified by the co-localization method (10); and finally, six genetic variants closely associated with HbA1c and SGLT2 inhibition were screened for MR analysis by the standard clustering process and F-statistic estimation (Supplementary Table 1).
2.2.2 Study outcome
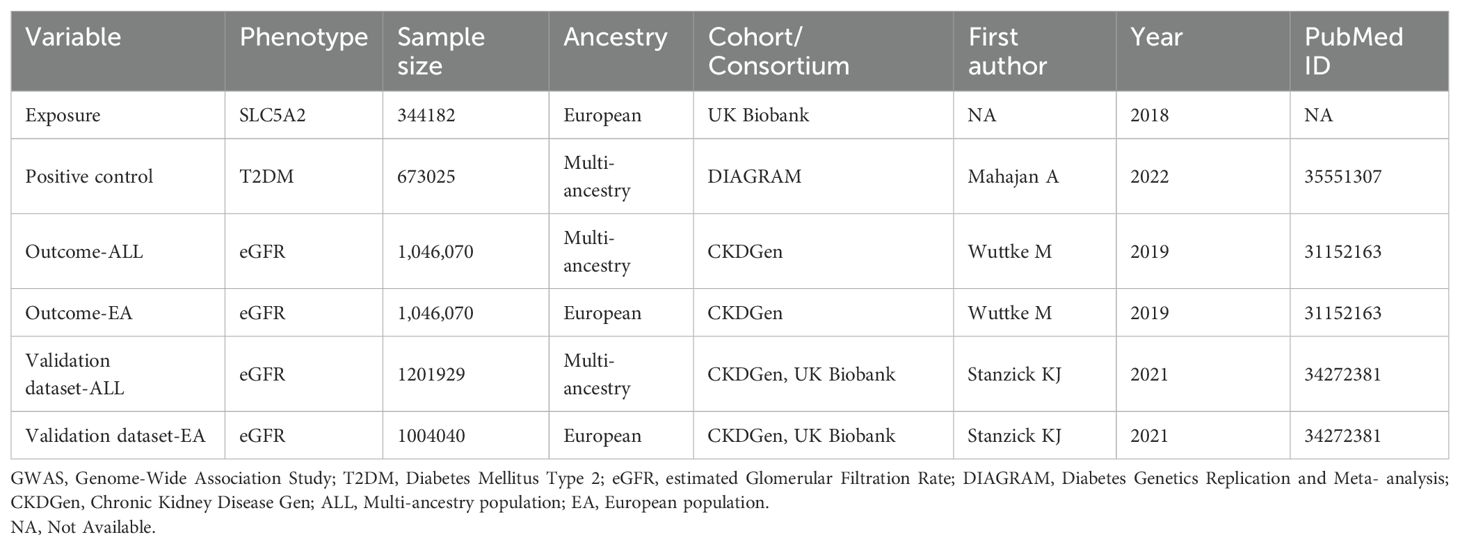
The GWAS data used in this study included the year of publication, sample size, SNP counts, and population information, as detailed in Table 1. The outcome GWAS data in this study were extracted from specialized disease databases. GWAS data for T2DM were obtained from the Diabetes Genetics Replication and Meta-analysis (DIAGRAM) consortium, and GWAS data for eGFR were obtained from the CKDGen consortium.
2.2.2.1 Positive control data
Positive control MR analysis justifies the genetic tool of a drug by demonstrating the expected effect on an outcome that has an established causal relationship with the target drug (19). SGLT2 inhibitors are used as a glucose-lowering drug with the intended indication of T2DM. Therefore, T2DM GWAS pooled data was selected as a positive control. The T2DM data in this study was obtained from one of the largest diabetes case-control studies published in 2022 in the DIAGRAM consortium. This study was conducted by Mahajan et al. The GWAS meta-analysis included 22 GWAS studies involving 180,834 patients with T2DM and 492,191 controls, as well as five lineage groups (51.1% of European ancestry) (20).
2.2.2.2 Study outcome data
Genetic associations for eGFR were obtained from a meta-analysis of publicly available CKDGen studies (21). All participants were of European ancestry, with a mean age of 54 years. All genetic correlations were adjusted for sex, age, study center, genetic rationale, components, correlations, and other study-specific characteristics (22). To confirm the robustness of the results of this study, we performed MR analysis using eGFR meta-analysis GWAS data from a diverse ancestry cohort (n ≥ 61 studies) and from a European ancestry cohort (n ≥ 42 studies). Detailed information is provided in Table 1.
2.2.2.3 Validation of outcome data
In addition, as a sensitivity analysis, the results of this study were validated using GWAS pooled data from another CKDGen meta-analysis using eGFR GWAS data from Stanzick et al, which is publicly accessible on the official website of CKDGen (23). Also, this data has been integrated into the GWAS Catalog database (GCST90103633, GCST90103634) (Table 1).
The GWAS summary statistics used in this study can be found in the IEU OpenGWAS project (https://gwas.mrcieu.ac.uk/), the GTEx portal (https://www.gtexportal.org/), the eQTLGen consortium (https://eqtlgen.org/), the DIAGRAM consortium (https://diagram-consortium.org/), CKDGen (https://ckdgen.imbi.uni-freiburg.de/), UKB Research (https://www.nealelab.is/uk-biobank, ukb-d-30750_irnt), and the GWAS Catalog (https://www.ebi.ac.uk/gwas/downloads/summary-statistics, GCST008058, GCST008064, GCST90103633, GCST90103634).
2.3 Statistical analysis
In the first place, genetic variant screening for SGLT2 inhibitors applied a generalized inverse variance weighting (IVW) method to consider the correlation of six predictors. MR effects were estimated by the LD matrix and IVW and MR-Egger methods to improve the efficiency and stability of the analysis (24). Subsequently, in MR analysis, the IVW method was used as the primary method to explore the effect of SGLT2 inhibition on the positive control T2DM and the study outcome eGFR (19). Various methods (including MR-Egger, weighted median, simple, and weighted models) were applied to test the reliability and stability of the results. The Strengthening the Reporting of Observational Studies in Epidemiology-Mendelian Randomization (STROBE-MR) guidelines were applied to guide the design of this study and the writing of the results (19). All statistical analyses were performed using the “Two-sample MR” (version 0.5.6) and “MR” (version 0.5.1) packages in the R software (version 4.3.2) environment. To more accurately interpret causality, we set the level of statistical significance to the Bonferroni-corrected level, that is, P < 0.0083. All MR analyses were performed using the Mendelian randomization R package and the TwoSampleMR R package (github.com/MRCIEU/TwoSampleMR). We plotted the results as forest plots using code from the ggplot 2 package in R.
As a sensitivity analysis, we applied an independent validation with a separate dataset. The validation data came from GWAS pooled data from another CKDGen meta-analysis, details of which are shown in Table 1.
To control for heterogeneity, we applied the MR multivalent residuals and outliers (MR-PRESSO) method. To test potential MR hypotheses, such as assessing the effect of directional pleiotropy, we applied the generalized MR-Egger regression method. Both tests of pleiotropy using the MR-Egger intercept term and tests of heterogeneity among predictors (Cochran Q statistic for IVW and global test for MR-PRESSO) were used to quantify the level of pleiotropy in the MR analysis. Compared to the MR-Egger, the MR-PRESSO method has higher accuracy for identifying levels of multivalence and outliers (25). The stability of outliers and results was also tested using the leave-one-out sensitivity analysis method, funnel plots, and scatter plots.
For a more rigorous interpretation of causality, we also used the Bonferroni correction based on the number of SNPs analyzed in the final MR. We used the significance level after performing the Bonferroni correction, which was set at 0.0083 (0.05 divided by 6 SNPs), to control for the rate of false discovery of multiple comparisons. In each independent SNP analysis, we compared the P value to 0.0083 to determine whether statistical significance existed.
3 Results
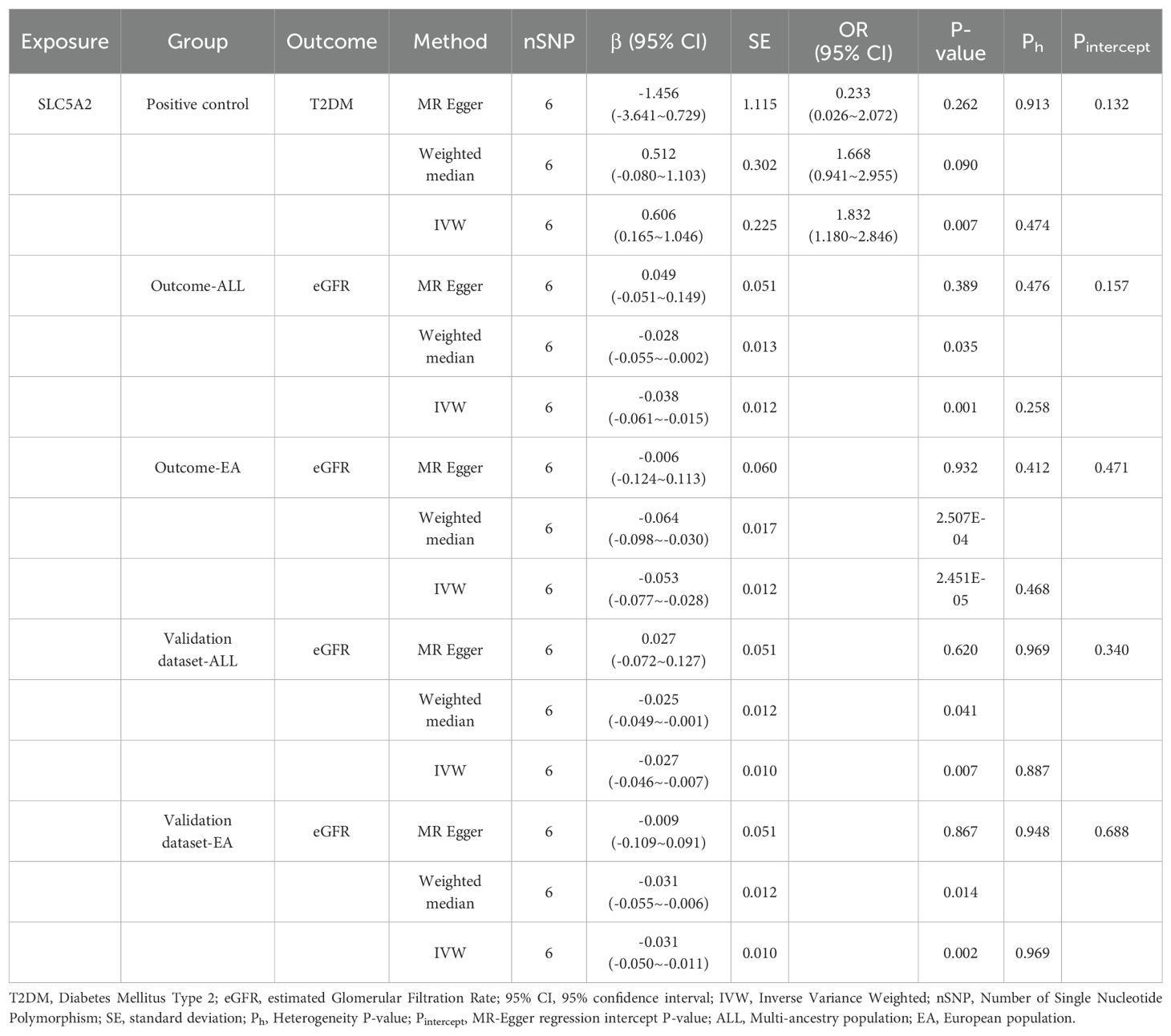
3.1 Effect of positive control-SLC5A2 on T2DM
To conduct a positive control, T2DM GWAS data were selected as outcome data and analyzed using MR with SLC5A2. As shown in Table 2, the MR results indicated that a 1-SD increase in HbA1c regulated by SLC5A2 was associated with an 83% increase in the risk of T2DM (IVW OR 1.83, 95% CI: 1.180-2.846, p = 0.007). This result effectively mimics the pharmacological inhibition mechanism of SGLT2 inhibitors, demonstrating that SGLT2 inhibition reduces the risk of T2DM. SGLT2 inhibitors, as glucose-lowering drugs, have an established causal relationship with T2DM, and the results of the positive control analysis were consistent with the expected outcomes. This suggests that SGLT2 inhibition decreases the risk of T2DM and demonstrates that the target gene, SLC5A2, can serve as a genetic tool for the drug target of SGLT2 inhibitors.
3.2 Effect of SLC5A2 on eGFR
The IVW method showed evidence to support a causal association between SLC5A2 and eGFR (Table 2, Figures 2, 3). As shown in Table 2, the MR results indicated that the SLC5A2 gene, was negatively correlated with eGFR (IVW β -0.038, 95% CI -0.061 to -0.015, P = 0.001 for multi-ancestry populations; IVW β -0.053, 95% CI -0.077 to -0.028, P = 2.45E-05 for populations of European ancestry). This suggests that each 1-SD increase in HbA1c predicted by the SLC5A2 gene is associated with a decrease in eGFR.
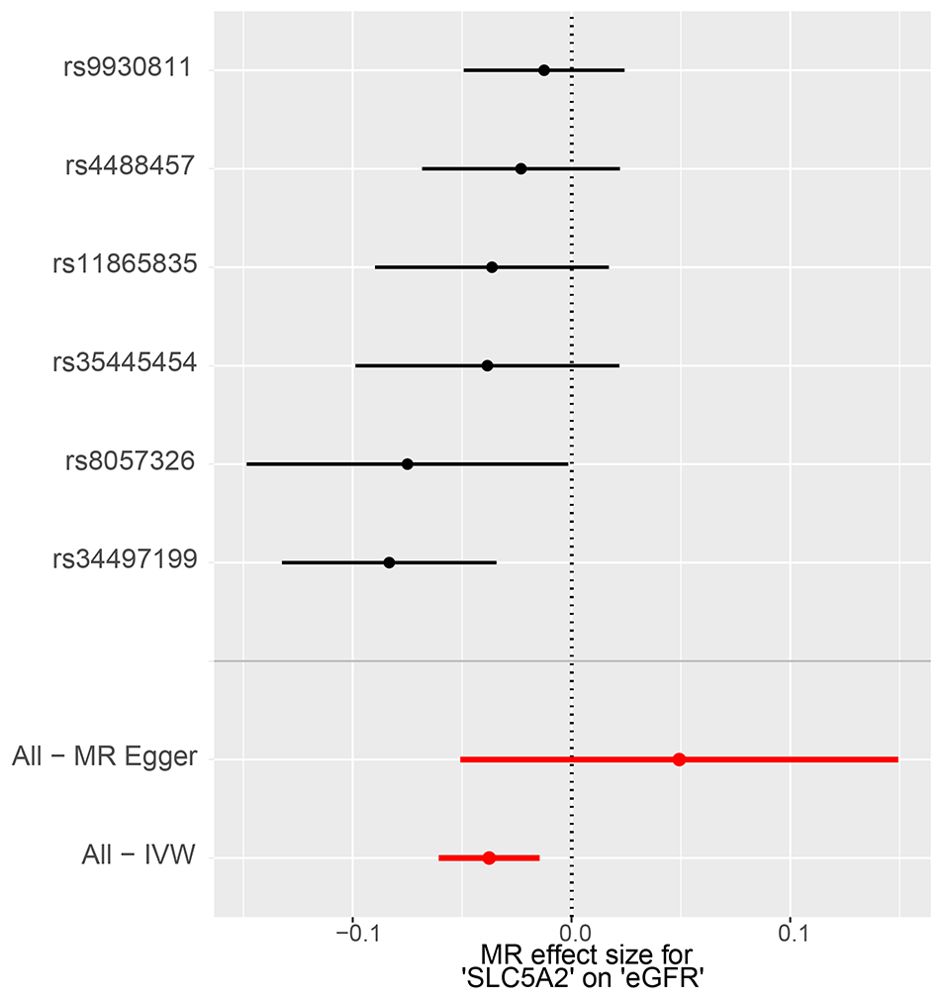
Figure 2. MR forest plot of the effect of SLC5A2 on eGFR in multi-ancestry populations. eGFR, estimated Glomerular Filtration Rate; IVW, Inverse Variance Weighted; MR, Mendelian randomization.
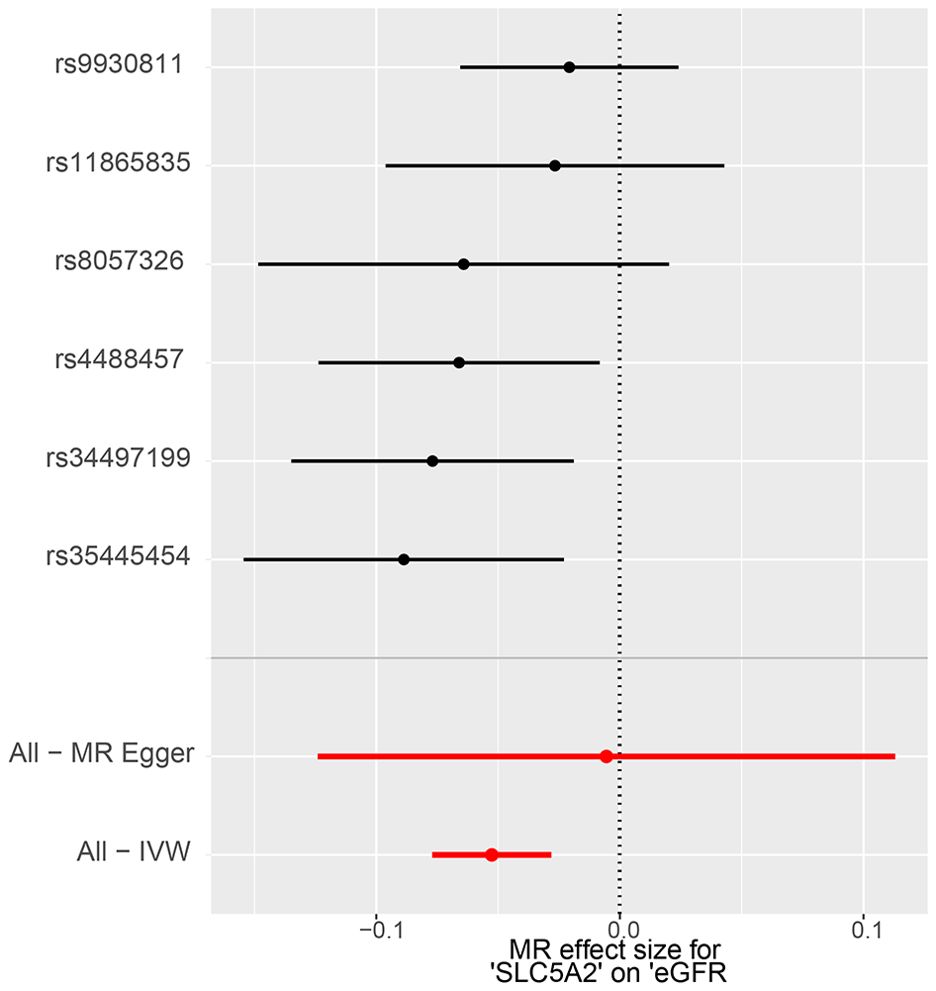
Figure 3. MR forest plot of the effect of SLC5A2 on eGFR in European populations. eGFR, estimated Glomerular Filtration Rate; IVW, Inverse Variance Weighted; MR, Mendelian randomization.
Conversion to mimic pharmacological inhibition, that is, lowering genetically predicted HbA1c per 1-SD unit by SGLT2 inhibition, reduces the risk of eGFR decline, which means that SGLT2 inhibitors are demonstrated to have a nephroprotective effect. All of the above P-values were less than 0.083 (Bonferroni-corrected significance level), suggesting statistical significance and robust results.
3.3 Validation and sensitivity analysis
First, as a sensitivity analysis, this study was validated using GWAS pooled data from another CKDGen meta-analysis, which yielded consistent findings across both multi-ancestry and European populations (Table 2, Supplementary Figures 1, 2). The validation data indicated a negative correlation between HbA1c predicted by the gene SLC5A2 and eGFR. Specifically, for multi-ancestry populations, IVW β was -0.027 (95% CI -0.046 to -0.007, P=0.007), and for populations of European ancestry, IVW β was -0.031 (95% CI -0.050 to -0.011, P=0.002). These results are consistent with the primary study outcomes.
Secondly, as shown in Table 2, MR analyses applying the weighted median method in the positive control, primary outcome, and validation outcome groups yielded consistent findings.
Third, the IVW heterogeneity test using the Cochran Q test in each group separately showed that neither the Q statistic nor the P value was significant (P > 0.05), implying that there was no evidence of heterogeneity in the effect of SGLT2 inhibition on eGFR. The test of pleiotropy using the MR-Egger intercept term showed that the P-value for the intercept was greater than 0.05, which implies that horizontal pleiotropy was not shown (Table 2).
Fourth, as shown in Supplementary Figures 3-6, the leave-one-out analysis in the primary outcome data and validation data for both multi-ancestry and European populations indicated that the effect sizes remained on the same side of the reference line 0, demonstrating robust results. This analysis confirms the negative correlation between the SLC5A2 gene and eGFR.
Overall, the results of the MR analysis in this study were robust.
4 Discussion
In this study, we performed MR analysis of drug targets and determined the genetic causal effect of SGLT2 inhibitors on eGFR. This finding provides genetic validation of the mechanism of action of SGLT2 inhibitors in improving renal function and delaying CKD progression.
Several large clinical observational or randomized controlled studies have found that canagliflozin, dapagliflozin, and empagliflozin produce a sustained improvement in kidney disease prognosis, including slowing eGFR decline, reducing albuminuria, and lowering the risk of renal failure (1, 13, 26, 27). This improvement is not only seen in T2DM patients, but patients without diabetes can also benefit. Based on extensive evidence of SGLT2 inhibitors in patients with CKD, KDIGO updated its clinical practice guideline in 2022 to recommend SGLT2 inhibitors as preferred therapeutic agents for managing T2DM combined with CKD (2). SGLT2 inhibitors are crucial for managing T2DM combined with atherosclerotic cardiovascular disease (ASCVD). They are the first-line therapeutic agents for patients with T2DM combined with ASCVD, cardiovascular risk factors, heart failure (HF), and CKD. Additionally, SGLT2 inhibitors are recommended for treating patients with HF or CKD who do not have comorbid diabetes (28).
It is worth noting that the currently completed randomized controlled trials of various SGLT2 inhibitors have different requirements for minimum eGFR levels in the enrollment criteria. Moreover, there are differences in the design of clinical studies for different SGLT2 inhibitors, and the respective protocols may be heterogeneous, so the findings of clinical studies corresponding to one drug may not be directly generalizable to other drugs of the same class. Randomized controlled trials are generally costly and lengthy. In contrast, a new research approach in recent years, drug-targeted MR, has significant advantages. MR is a method that utilizes genetic variants closely associated with exposure as a potentially unconfounded tool to infer a causal relationship between exposure and outcome. New approaches, such as genetic co-localization and genetic variation (eQTL) associated with drug target mRNA expression, can be used to create MR instrumental variables for use in drug targets (14), which has become a new research hotspot.
Previous MR studies have further explored the benefits of SGLT2 inhibitors. Xu M et al. (15) investigated the role of SGLT2 inhibition in reducing coronary artery disease (CAD) and T2DM. They found that SGLT2 inhibition lowered the risk of both conditions, with choline metabolites partly mediating these effects. Another study focused on HF and identified that SGLT2 inhibition reduced HF risk through anti-inflammatory mechanisms, specifically via the CXCL10 biomarker (29). These studies support our findings and highlight the broader therapeutic potential of SGLT2 inhibitors in managing complex diseases like CKD, T2DM, CAD, and HF.
To the best of our knowledge, few relevant MR studies have explored the genetic causal effect of SGLT2 inhibition on the effects of eGFR. A recently published study by Wang Z et al. investigated the role of circulating metabolites in the renoprotective effects of SGLT2 inhibition, specifically identifying small high-density lipoprotein (HDL) particles as mediators in this process (30). However, our study differs in that it focuses on the direct genetic causal effect of SGLT2 inhibition on eGFR using MR analysis without considering metabolic intermediates. Our MR analysis revealed that genetically predicted SGLT2 inhibition resulted in a reduced risk of eGFR decline. This result supports the association between IR and renal function found in previous observational studies, using genetic data to provide further causal evidence. The EMPA-KIDNEY trial (27), the most extensive international multicenter, randomized, double-blind, placebo-controlled clinical trial in CKD to date, confirmed that empagliflozin treatment significantly reduced the risk of the primary endpoint event, which includes kidney disease progression and cardiovascular death, compared to placebo. An updated subgroup analysis of the EMPA-KIDNEY study confirmed that Engeletin significantly slows the progression of chronic kidney function in a broad population of CKD patients regardless of CKD etiology, diabetes status, eGFR and urinary ACR levels (31, 32). Our findings provide timely and robust evidence for the role of SGLT2 inhibition in reducing CKD risk.
The potential mechanisms linking SLC5A2 inhibition and eGFR may involve reduced expression of SLC5A2, inhibition of SGLT2 receptors, leading to decreased reabsorption of glucose and sodium in renal tubules, which results in osmotic diuresis and lower blood pressure (1). Additionally, these inhibitors may exert anti-inflammatory effects, alleviate renal oxidative stress, and modulate metabolic pathways, collectively supporting renal function (3, 4).
However, there are some limitations to this study. First, this study could only predict the effect of drugs on eGFR by interfering with the encoded proteins (targeting effect). We cannot rule out the possibility that drugs alter eGFR risk through other proteins (off-target effects). Second, our MR analyses estimated SGLT2 inhibition based on targeted reductions in genetically predicted HbA1c levels rather than direct effects of SGLT2 inhibitors. This is based on the assumption that the effect of SGLT2 inhibitors on HbA1c levels is proportional to their overall effect, which may be inconsistent with the actual mechanism of SGLT2 inhibitors. In addition, the drug formulation, dosage, and mode of administration of SGLT2 inhibitors can influence their effects on eGFR. These factors should be taken into account when interpreting our findings. Third, genetic variation reflects the effect of lifelong exposure to a biomarker on outcome and therefore cannot be used to directly estimate the expected impact of short-term pharmacologic changes in that biomarker (33). This means that the effect sizes in our study may not be comparable to those reported in trials or observational studies. Fourth, although the MR-Egger method is dependent on the orientations of SNPs and can influence the outcome of the analysis, our study conducted a pleiotropy test using the MR-Egger intercept term, which showed no evidence of horizontal pleiotropy (P > 0.05). Finally, our analyses were conducted mainly in European populations. Therefore, this limits the generalizability of our findings to other ethnicities. The potential for confounding factors in observational data must also be considered, as they might affect the accuracy and applicability of the results.
Future studies should explore the genetic causal effect of SGLT2 inhibition on eGFR in diverse populations to enhance the generalizability of the findings. Additionally, future research should aim to integrate genetic evidence with experimental and clinical studies to provide a comprehensive understanding of how SGLT2 inhibitors can be leveraged to protect against CKD progression.
5 Conclusions
Our results show that SLC5A2 is negatively correlated with eGFR, identifying a causal role of SGLT2 inhibition with eGFR. By modeling the drug-targeted effects of SGLT2 inhibitors, it was thus concluded that inhibition of SLC5A2 gene expression was causally associated with higher eGFR. The renoprotective effect of SGLT2 inhibitors was validated from the perspective of genetic variation, and also provided MR evidence for SGLT2 inhibitors as first-line therapeutic agents for CKD patients.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary material.
Ethics statement
This research has been conducted using the publicly available data. No original data were collected for the MR study. Ethical approval for each of the studies included in the investigation can be found in the original publications (including informed consent from each participant). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
GL: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The author would like to express his gratitude to all colleagues in the department. I sincerely acknowledge Dr. Wentao Ni (People’s Hospital of Peking University) for his guidance and assistance with the Mendelian randomization analysis method.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2024.1418575/full#supplementary-material
References
1. Maxson R, Starr J, Sewell J, Lyas C. SGLT2 inhibitors to slow chronic kidney disease progression: A review. Clin Ther. (2024) 46:e23–8. doi: 10.1016/j.clinthera.2023.10.014
2. Kidney Disease: Improving Global Outcomes (KDIGO) Diabetes Work Group. KDIGO 2022 clinical practice guideline for diabetes management in chronic kidney disease. Kidney Int. (2022) 102:S1–S127. doi: 10.1016/j.kint.2022.06.008
3. Scurt FG, Ganz MJ, Herzog C, Bose K, Mertens PR, Chatzikyrkou C. Association of metabolic syndrome and chronic kidney disease. Obes Rev. (2024) 25:e13649. doi: 10.1111/obr.13649
4. Packer M. Critical reanalysis of the mechanisms underlying the cardiorenal benefits of SGLT2 inhibitors and reaffirmation of the nutrient deprivation signaling/autophagy hypothesis. Circulation. (2022) 146:1383–405. doi: 10.1161/CIRCULATIONAHA.122.061732
5. Kullmann S, Hummel J, Wagner R, Dannecker C, Vosseler A, Fritsche L, et al. Empagliflozin improves insulin sensitivity of the hypothalamus in humans with prediabetes: A randomized, double-blind, placebo-controlled, phase 2 trial. Diabetes Care. (2022) 45:398–406. doi: 10.2337/dc21-1136
6. Heerspink HJL, Perkins BA, Fitchett DH, Husain M, Cherney DZI. Sodium glucose cotransporter 2 inhibitors in the treatment of diabetes mellitus: cardiovascular and kidney effects, potential mechanisms, and clinical applications. Circulation. (2016) 134:752–72. doi: 10.1161/CIRCULATIONAHA.116.021887
7. Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. (2015) 373:2117–28. doi: 10.1056/NEJMoa1504720
8. Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. (2017) 377:644–57. doi: 10.1056/NEJMoa1611925
9. Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. (2019) 380:347–57. doi: 10.1056/NEJMoa1812389
10. Cannon CP, Pratley R, Dagogo-Jack S, Mancuso J, Huyck S, Masiukiewicz U, et al. Cardiovascular outcomes with ertugliflozin in type 2 diabetes. N Engl J Med. (2020) 383:1425–35. doi: 10.1056/NEJMoa2004967
11. McMurray JJV, Solomon SD, Inzucchi SE, Køber L, Kosiborod MN, Martinez FA, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. (2019) 381:1995–2008. doi: 10.1056/NEJMoa1911303
12. Wanner C, Inzucchi SE, Lachin JM, Fitchett D, von Eynatten M, Mattheus M, et al. Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med. (2016) 375:323–34. doi: 10.1056/NEJMoa1515920
13. Perkovic V, Jardine MJ, Neal B, Bompoint S, Heerspink HJL, Charytan DM, et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med. (2019) 380:2295–306. doi: 10.1056/NEJMoa1811744
14. Walker VM, Kehoe PG, Martin RM, Davies NM. Repurposing antihypertensive drugs for the prevention of Alzheimer’s disease: a Mendelian randomization study. Int J Epidemiol. (2020) 49:1132–40. doi: 10.1093/ije/dyz155
15. Xu M, Zheng J, Hou T, Lin H, Wang T, Wang S, et al. SGLT2 inhibition, choline metabolites, and cardiometabolic diseases: A mediation mendelian randomization study. Diabetes Care. (2022) 45:2718–28. doi: 10.2337/dc22-0323
16. GTEx Consortium. The GTEx Consortium atlas of genetic regulatory effects across human tissues. Science. (2020) 369:1318–30. doi: 10.1126/science.aaz1776
17. Võsa U, Claringbould A, Westra H-J, Bonder MJ, Deelen P, Zeng B, et al. Large-scale cis- and trans-eQTL analyses identify thousands of genetic loci and polygenic scores that regulate blood gene expression. Nat Genet. (2021) 53:1300–10. doi: 10.1038/s41588-021-00913-z
18. Elsworth B, Lyon M, Alexander T, Liu Y, Matthews P, Hallett J, et al. The MRC IEU OpenGWAS data infrastructure. Genetics. (2020). doi: 10.1101/2020.08.10.244293. preprint.
19. Burgess S, Davey Smith G, Davies NM, Dudbridge F, Gill D, Glymour MM, et al. Guidelines for performing Mendelian randomization investigations: update for summer 2023. Wellcome Open Res. (2019) 4:186. doi: 10.12688/wellcomeopenres.15555.3
20. Mahajan A, Spracklen CN, Zhang W, Ng MCY, Petty LE, Kitajima H, et al. Multi-ancestry genetic study of type 2 diabetes highlights the power of diverse populations for discovery and translation. Nat Genet. (2022) 54:560–72. doi: 10.1038/s41588-022-01058-3
21. Köttgen A, Pattaro C. The CKDGen Consortium: ten years of insights into the genetic basis of kidney function. Kidney Int. (2020) 97:236–42. doi: 10.1016/j.kint.2019.10.027
22. Wuttke M, Li Y, Li M, Sieber KB, Feitosa MF, Gorski M, et al. A catalog of genetic loci associated with kidney function from analyses of a million individuals. Nat Genet. (2019) 51:957–72. doi: 10.1038/s41588-019-0407-x
23. Stanzick KJ, Li Y, Schlosser P, Gorski M, Wuttke M, Thomas LF, et al. Discovery and prioritization of variants and genes for kidney function in >1. 2 million individuals. Nat Commun. (2021) 12:4350. doi: 10.1038/s41467-021-24491-0
24. Burgess S, Zuber V, Valdes-Marquez E, Sun BB, Hopewell JC. Mendelian randomization with fine-mapped genetic data: Choosing from large numbers of correlated instrumental variables. Genet Epidemiol. (2017) 41:714–25. doi: 10.1002/gepi.22077
25. Verbanck M, Chen C-Y, Neale B, Do R. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat Genet. (2018) 50:693–8. doi: 10.1038/s41588-018-0099-7
26. Heerspink HJL, Stefánsson BV, Correa-Rotter R, Chertow GM, Greene T, Hou F-F, et al. Dapagliflozin in patients with chronic kidney disease. N Engl J Med. (2020) 383:1436–46. doi: 10.1056/NEJMoa2024816
27. The EMPA-KIDNEY Collaborative Group, Herrington WG, Staplin N, Wanner C, Green JB, Hauske SJ, et al. Empagliflozin in patients with chronic kidney disease. N Engl J Med. (2023) 388:117–27. doi: 10.1056/NEJMoa2204233
28. Chen TK, Hoenig MP, Nitsch D, Grams ME. Advances in the management of chronic kidney disease. BMJ. (2023) 383:e074216. doi: 10.1136/bmj-2022-074216
29. Guo W, Zhao L, Huang W, Chen J, Zhong T, Yan S, et al. Sodium-glucose cotransporter 2 inhibitors, inflammation, and heart failure: a two-sample Mendelian randomization study. Cardiovasc Diabetol. (2024) 23:118. doi: 10.1186/s12933-024-02210-5
30. Wang Z, Wei J, Zhao W, Shi R, Zhu Y, Li X, et al. SGLT2 inhibition, high-density lipoprotein, and kidney function: a mendelian randomization study. Lipids Health Dis. (2024) 23:84. doi: 10.1186/s12944-024-02072-6
31. EMPA-KIDNEY Collaborative Group. Impact of primary kidney disease on the effects of empagliflozin in patients with chronic kidney disease: secondary analyses of the EMPA-KIDNEY trial. Lancet Diabetes Endocrinol. (2024) 12:51–60. doi: 10.1016/S2213-8587(23)00322-4
32. EMPA-KIDNEY Collaborative Group. Effects of empagliflozin on progression of chronic kidney disease: a prespecified secondary analysis from the empa-kidney trial. Lancet Diabetes Endocrinol. (2024) 12:39–50. doi: 10.1016/S2213-8587(23)00321-2
Keywords: sodium-glucose cotransporter protein 2 (SGLT2) inhibition, SLC5A2, eGFR, drug target Mendelian randomization, insulin resistance
Citation: Liu G (2024) Assessment of the effect of the SLC5A2 gene on eGFR: a Mendelian randomization study of drug targets for the nephroprotective effect of sodium-glucose cotransporter protein 2 inhibition. Front. Endocrinol. 15:1418575. doi: 10.3389/fendo.2024.1418575
Received: 16 April 2024; Accepted: 14 August 2024;
Published: 29 August 2024.
Edited by:
Divya Bhatia, NewYork-Presbyterian, United StatesReviewed by:
Jasna Klen, University Medical Centre Ljubljana, SloveniaNing Jie, Shenzhen Longhua District Central Hospital, China
Copyright © 2024 Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gailing Liu, bGl1Z2FpbGluZzdAMTI2LmNvbQ==
 Gailing Liu
Gailing Liu