- 1Department of Obstetrics and Gynecology, The Second Clinical Medical College, Jinan University, Shenzhen, China
- 2Center for Reproductive Medicine, Department of Obstetrics and Gynecology, Peking University, Beijing, China
- 3Department of Obstetrics and Gynecology, Shenzhen People’s Hospital (the Second Clinical Medical College of Jinan University and the First Affiliated Hospital of Southern University of Science and Technology), Shenzhen, China
Introduction: Endometriosis is delineated as a benign yet steroid-dependent disorder characterized by the ectopic presence of endometrial glandular and stromal cells outside the uterine cavity, affecting estimated 10%–15% of women of reproductive age, 20%–50% of all women with infertility and costing a great economic burden per-patient. Endometriosis exerts pervasive influence on multiple facets of female reproductive physiology. Given its characterization as a chronic inflammatory disorder, escalated levels of pro-inflammatory cytokines were unequivocally recognized as well-established characteristics of endometriosis, which might attribute to mechanisms like retrograde menstruation, progesterone receptor resistance, and immune dysregulation. Therapeutic utilization of non-steroidal anti-inflammatory drugs (NSAIDs) like aspirin, analgesic agent for reducing pain, inflammation, and fever, could be holding promise in augmenting reproductive outcomes of endometriosis women. Therefore, the objective of this comprehensive review is to elucidate the intricate interplay between endometriosis and aspirin, both within the context of infertility and beyond. We meticulously explore potential pharmacological agents targeting endometriosis, which may concurrently optimize the efficacy of reproductive interventions, while also delving into the underlying mechanistic pathways linking endometriosis with inflammatory processes.
Methods: We conducted a comprehensive search in the data available in PubMed and the Web of Science using the terms ‘endometriosis’ and ‘aspirin’. Then analyzed the identified articles based on established inclusion and exclusion criteria independently by three reviewers.
Results: The survey of the chosen terms revealed 72 articles, only 10 of which were considered for review.
Discussion: Based on the research available currently, it is not substantial enough to address the conclusion that aspirin shall be an effective therapeutic choice for endometriosis, further studies are needed to elucidate the efficacy, safety profile, and optimal dosing regimens of aspirin in the context of endometriosis treatment.
Introduction
Endometriosis is widely recognized as a profound clinical challenge for women of reproductive age, profoundly compromising reproductive function across its entirety. Characterized by the aberrant presence of endometrial tissue beyond the confines of the uterine cavity, this condition afflicts approximately 10%-15% of reproductive-aged women and is identified in up to 50% of women facing infertility issues (1, 2). The typical clinical presentations of endometriosis include infertility, persistent pelvic pain, and escalating dysmenorrhea (3). The American Society for Reproductive Medicine initially formulated and subsequently revised its diagnostic criteria in 1997, categorizing endometriosis into three distinct subtypes: ovarian endometriomas (OMA), deep infiltration endometriosis (DIE), and superficial peritoneal lesions (SUP). Notably, the ectopic proliferation of endometrial tissue within the ovaries, either unilaterally or bilaterally, culminating in the formation of cystic masses referred to as OMA, predominantly impairs women’s reproductive capabilities by disrupting oocyte formation and maturation (4).
The etiological underpinnings of endometriosis remain elusive, although several theoretical frameworks have been posited to elucidate its pathogenesis (5). Foremost among these is the retrograde menstruation theory originally postulated by Sampson, which currently stands as the prevailing hypothesis in the field. The Sampson’s theory states that viable endometrial tissue refluxes into the peritoneal cavity through the fallopian tubes and subsequently implants into the peritoneal tissue and/or pelvic organs (6). Unfortunately, this theory fails to explain the fact that 80% to 90% of women had experienced retrograde menstruation but only 10% to 15% of women had endometriosis. Complementary theories include the epithelial–mesenchymal transition, hormonal dysregulation, immune system aberrations, and genetic predispositions are therefore posited as potential contributory factors to the onset and progression of endometriosis (7–10). Furthermore, an expanding body of literature underscores the increasingly recognized role of inflammation as a central contributor to the pathogenesis and persistence of endometriosis (11).
Treatment of endometriosis is aimed at suppressing lesion growth, alleviating pain, and ideally addressing the systemic effects of the disease. Surgical and pharmacological interventions are now two prevailing therapeutic strategies employed in the management of endometriosis. Surgical interventions, such as lesion ablation or excision, can offer temporary relief from symptoms, they shall also entail potential risks, notably the compromise of ovarian reserve, particularly due to thermal and electric injuries during ovarian cystectomy in cases with OMAs. For the majority of endometriosis patients, pharmacological treatments like progestogens or combined oral contraceptive pills (COCs) are commonly recommended (12). However, their effectiveness can sometimes be hindered by the inherent progesterone resistance observed in endometriotic lesions (13, 14). In addressing this therapeutic challenge, the use of gonadotropin-releasing hormone (GnRH) analogues, including both GnRH agonists and GnRH antagonists, has been advocated. Every medal has its reverse, the subsequent hypoestrogenic states can lead to discomforts such as vasomotor symptoms and decreased bone mineral density. Consequently, the use of “add-back therapy” of estrogen becomes necessary, which in essence exacerbates severity of endometriosis. In terms of relieving endometriosis-related pain, the concurrent use of analgesic agents, specifically NSAIDs, in conjunction with COCs or progestogens is supported by European Society of Human Reproduction and Embryology and the Royal College of Obstetricians and Gynecologists, and is recommended as the cornerstone pharmacotherapeutic approach for addressing indeterminate endometriosis-related pain.
Aspirin, as one of the three classic drugs in the history of medicine, chemically known as acetylsalicylic acid, possesses the capability to inhibit cyclooxygenase enzymes (COX-1 and COX-2), which are responsible for the conversion of arachidonic acid to prostaglandins, thereby reducing pain, inflammation, and fever. With an annual global consumption approximating 40,000 tons, aspirin represents a time-honored and frequently prescribed analgesic agent employed for pain management and inflammation attenuation (15). The use of aspirin for pain relief traces its roots back to ancient civilizations, with Chinese healers and Egyptians utilizing natural sources of salicylates for analgesic purposes. However, it wasn’t until the early 20th century, around 1900, that water-soluble aspirin tablets were first made available, marking a significant milestone in the discovery and development of this widely used medication (16). Since its inception, aspirin has evolved to become one of the most commonly prescribed analgesic and anti-inflammatory agents worldwide. Its versatile applications extend across various medical specialties, permeating virtually every department of medicine (17). From cardiology to oncology, and from rheumatology to gynecology, aspirin’s multifaceted pharmacological properties have established its indispensable role in contemporary medical practice.
Immunohistochemical investigations demonstrated that cyclooxygenase is expressed in various reproductive tissues, including the endometrial epithelium and fallopian tube secretory epithelial cells, although not in ciliated epithelial cells, cervical epithelium, and myometrial cells (18). As a pivotal enzyme regulating prostaglandin synthesis, COX-2 enhances invasiveness and promotes angiogenesis. Meanwhile, in ectopic endometrium of individuals with endometriosis, COX-2 expression is markedly upregulated, therefore facilitating the adhesion and invasiveness of endometrial cells (19–21).
The objective of this systematic review is to rigorously evaluate the current scientific literature regarding the potential association between aspirin and endometriosis, with an emphasis on inflammatory mechanisms. This includes an in-depth and critical analysis of both in vivo and in vitro experimental studies, and a comprehensive examination of clinical trial findings. The overarching objective is to elucidate potential therapeutic interventions that may hold promise for future clinical applications in the field of obstetrics and gynecology for the management of endometriosis.
Methods
We searched the data available in PubMed and the Web of Science. The terms investigated include ‘endometriosis’ and ‘aspirin’. Three reviewers analyzed the data in an independent manner and only studies having at least one of the following characteristics were considered: observational or experimental, analytical or descriptive studies of the association between aspirin and endometriosis. Review and opinion studies were excluded as well as non-English manuscripts.
Results
The survey of the chosen terms revealed 72 articles, only 10 of which were considered for review by satisfying the established inclusion criteria and fully analyzed.
In a seminal study by Nasiri N et al., a significant positive correlation was established between the expression levels of nuclear factor-κB (NF-κB) and the proliferative and adhesive capabilities of eutopic endometrial stromal cells. The NF-κB signaling pathway serves as a critical nexus within inflammatory cascades, dysregulation or aberrant activation of which has been implicated in the pathophysiology of a wide spectrum of inflammatory and autoimmune conditions, including endometriosis. Intriguingly, this observed relationship was found to be modifiable through interventions with aloe-emodin or aspirin (22). Contrarily, Massimi I et al. conducted an investigation revealing upregulated expression of multidrug resistance-associated protein 4(MRP4) mRNA and MRP4 protein in a peroxisome proliferator-activated receptor-alpha (PPAR-α) dependent manner (23).
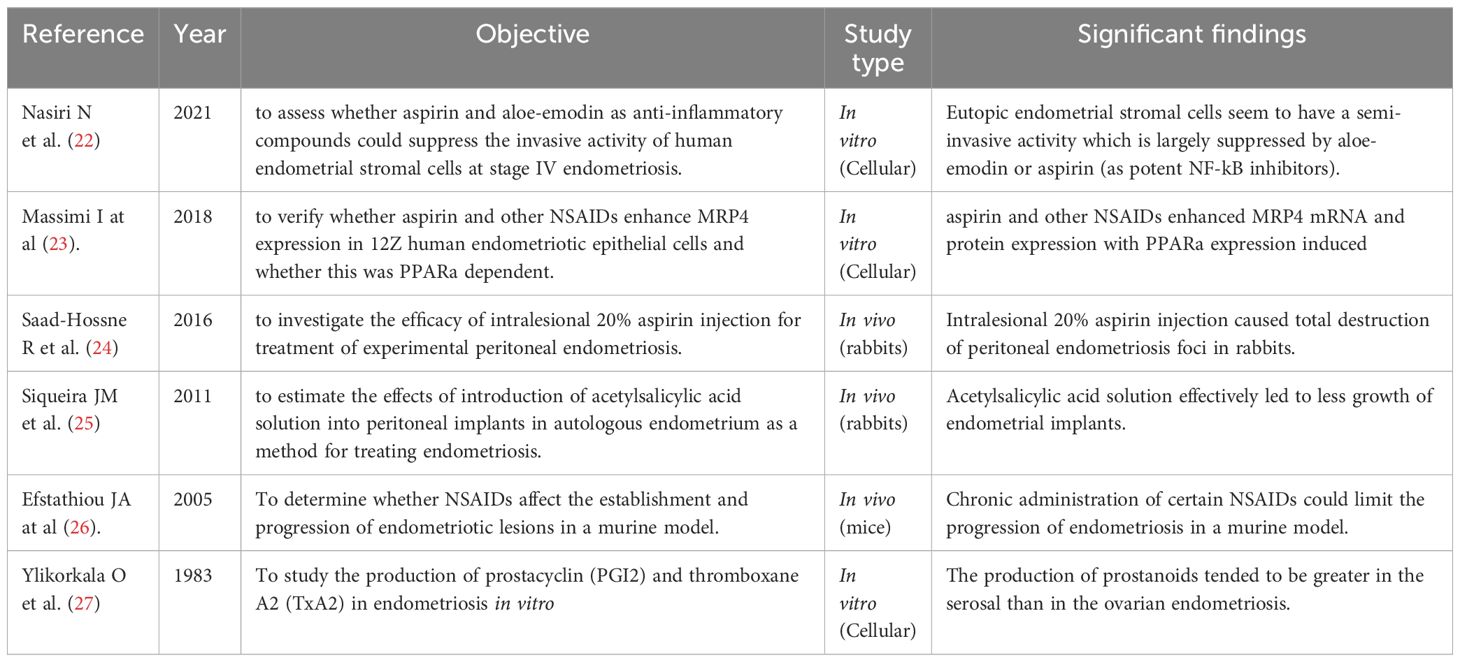
In a comprehensive investigation conducted by Saad-Hossne R et al., the therapeutic efficacy of intralesional aspirin administration in mitigating endometriosis was rigorously assessed utilizing an established rabbit model of peritoneal endometriosis. Histological evaluations post-treatment revealed notable alterations within the endometriotic lesions, characterized by pronounced necrosis, hemorrhage, apoptosis, and fibrotic changes. Intriguingly, a substantial reduction in endometrial tissue foci, and in certain instances, complete eradication of endometrial tissue, was evident compared to the saline control cohort (24), Notably, these observations are congruent with earlier investigations by Siqueira JM et al (25). In an insightful study conducted by Efstathiou JA et al., utilizing a murine model, the differential impacts of various NSAIDs on the initiation and progression of endometriotic lesions were systematically evaluated. Comparative analysis revealed that among the NSAIDs investigated, celecoxib exerted the most pronounced reduction in lesion burden, followed by indomethacin, naproxen, sulindac, rofecoxib, and ibuprofen, respectively. Contrastingly, aspirin did not elicit any statistically significant impact on lesion burden compared to the control group (26) (Table 1).
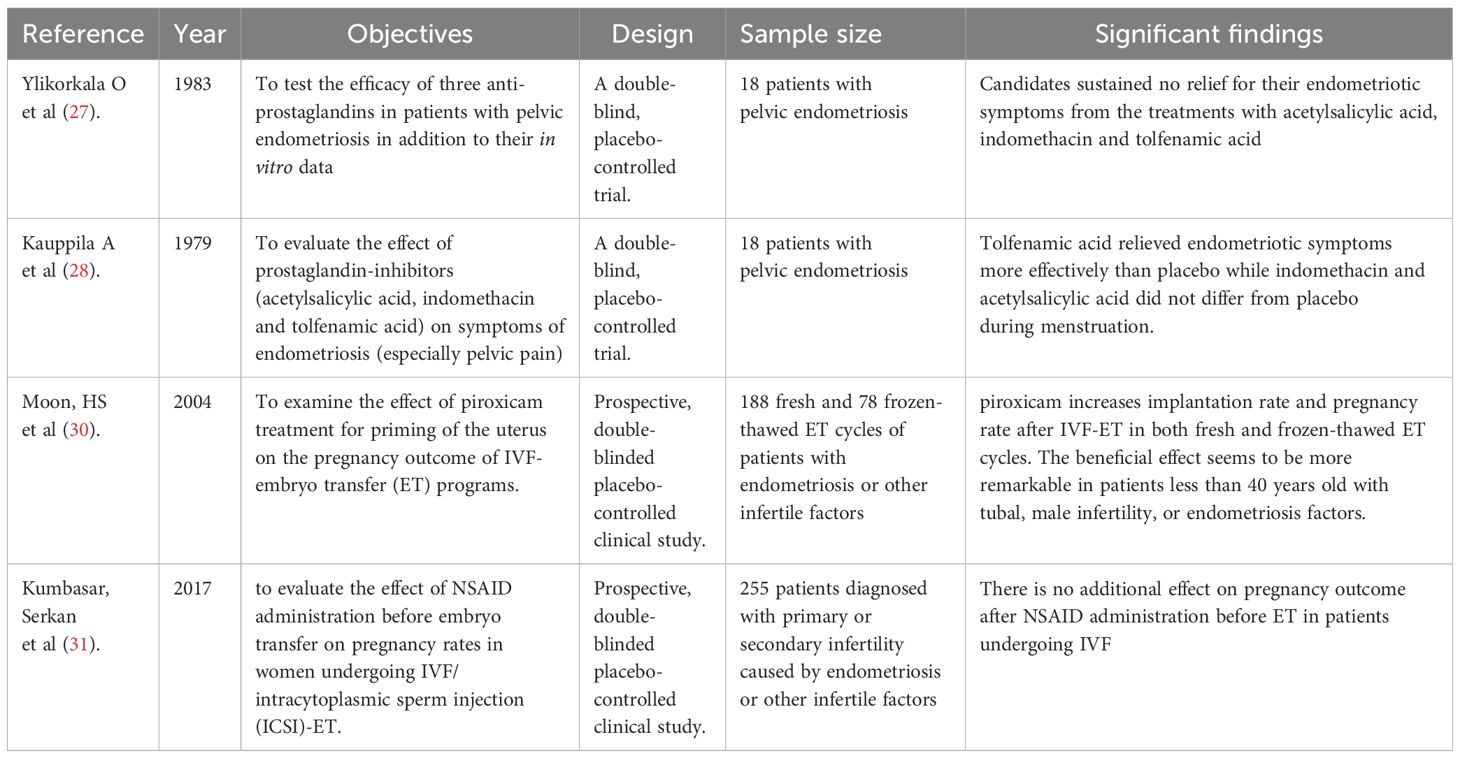
In a meticulously designed double-blind, placebo-controlled clinical trial orchestrated by Ylikorkala O et al., a cohort of 18 patients afflicted with pelvic endometriosis was subjected to therapeutic regimens involving aspirin (acetylsalicylic acid), indomethacin, and tolfenamic acid. Surprisingly, the study outcomes diverged from anticipated results, revealing no substantial alleviation in endometriotic symptoms subsequent to NSAID administration, when compared to placebo treatments (27). Subsequently, in a similarly designed clinical trial by Kauppila A et al. in 1997, the impact of prostaglandin biosynthesis inhibitors, including aspirin, indomethacin, and tolfenamic acid, on endometriosis-associated symptoms was systematically assessed. Notably, the findings unveiled that tolfenamic acid exhibited heightened efficacy in mitigating endometriotic symptoms particularly during the menstrual phase. Conversely, both indomethacin and aspirin did not manifest any notable disparity in symptom relief compared to the placebo control group (28). In a pioneering pilot study published by Flannagan KS et al. in 2019, compelling evidence was presented for the first time suggesting that short-term therapy with aspirin and pravastatin, an HMG-CoA reductase inhibitor employed for lipid level reduction, could effectively attenuate high-sensitivity C-reactive protein levels. Furthermore, the combination of these pharmacological agents demonstrated promising potential in enhancing the outcomes of infertility treatments (29). Concurrently, Moon HS et al. conducted an exploratory pilot study to assess the effects of oral administration of piroxicam, at a dosage of 10 mg administered 1 to 3 hours prior to embryo transplant, on the in vitro fertilization-embryo transfer (IVF-ET) and frozen embryo transfer (FET) outcomes in patients presenting with endometriosis, tubal, and male infertility factors. Intriguingly, their findings elucidated that the piroxicam treatment group exhibited significantly elevated implantation and pregnancy rates compared to the control group. Specifically, the implantation and pregnancy rates were approximately doubled in patients with endometriosis factors following piroxicam treatment, as compared to the control (P<0.05) (30). In contrast, a study by Kumbasar S et al. presented divergent results. Their investigation encompassed 255 patients with primary or secondary infertility attributed to endometriosis, tubal, or male factors. The administration of either piroxicam (10 mg orally) or indomethacin (100 mg rectal suppository) prior to ET was assessed for its impact on implantation rates, miscarriage rates, and clinical pregnancy rates in patients undergoing IVF. Surprisingly, their data revealed that neither piroxicam nor indomethacin conferred any additional benefit in terms of implantation rates (P = 0.842), miscarriage rates (P = 0.964), or clinical pregnancy rates (P = 0.887) compared to the control group (31) (Table 2).
Discussion
With evolving theories attempting to elucidate its origins, the precise etiology of endometriosis remains elusive. Though Sampson’s theory positing that menstrual debris flows backward through the fallopian tubes, implanting and proliferating within the pelvic cavity holds sway and remains prevalent in contemporary discourse, the paradigm of inflammation has emerged as a pivotal determinant in the pathophysiology of endometriosis, and its role in the context of endometriosis has attracted significant attention and empirical validation. Inflammatory processes are now increasingly recognized as central to the initiation, progression, and perpetuation of endometriotic lesions. -
Endometriosis is increasingly acknowledged not merely as a pelvic disorder but as a systemic condition (11, 32) with a dysregulated immune system and a proinflammatory environment (33). Neutrophils, pivotal granulocytes renowned for their role in combating bacterial invasions and preserving tissue integrity, have been implicated in the pathogenesis of endometriosis. This association is substantiated by strong evidence demonstrating heightened chemotactic activity in neutrophils derived from women with endometriosis compared to their counterparts in healthy control individuals. Concurrently, macrophages, serving as the vanguard of our primary immune defense, display increased activation of the proinflammatory transcription factor NF-κB and have been identified increased in the peritoneal fluid of women with endometriosis (34). However, while an elevation in macrophage numbers has been observed in the peritoneal fluid of women with endometriosis, these cells exhibit compromised phagocytic capabilities, culminating in inhibiting apoptosis and fostering proliferation of endometrial stromal cells, consistently, co-culture experiments have elucidated that macrophages can augment the proliferation and invasive potential of endometrial stromal cells (35, 36). Notably, estradiol, necessary for endometriosis development, has been identified as a crucial mediator of macrophage function in the context of endometriosis (35). Regulatory T cells (Tregs), a pivotal subset of T cells essential for modulating immune responses and sustaining maternal-fetal tolerance, elevated presence of which was detected in ectopic endometrial tissues and peritoneal fluid of endometriosis patients, suggesting that Tregs within the local microenvironment may contribute to the expansion and progression of endometriotic lesions (37, 38) (Figure 1).
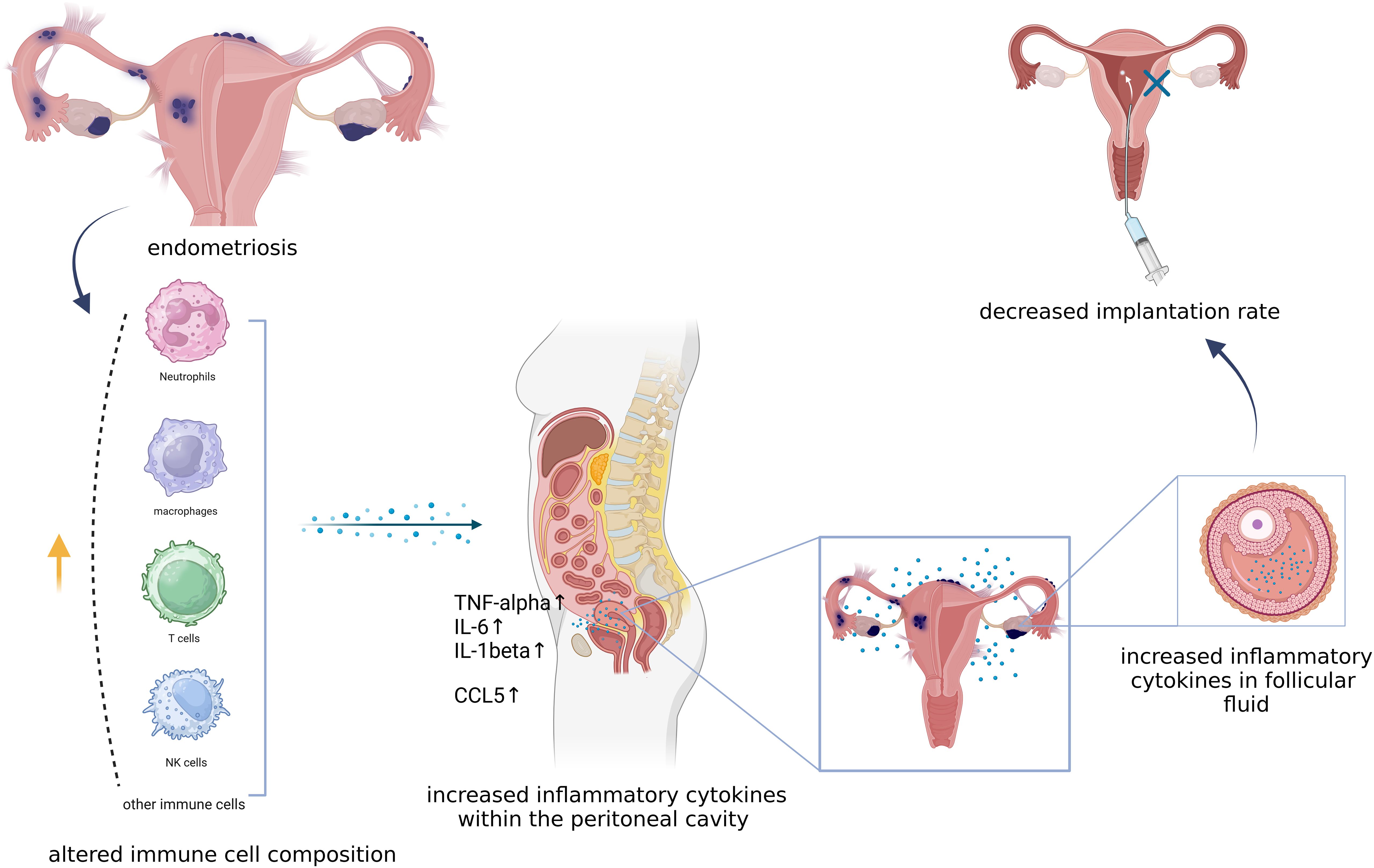
Figure 1. The relationship between immune cells and inflammation in endometriosis. this figure illustrates that neutrophils, macrophages, T cells and NK cells are all contributing to the pro-inflammatory environment both systematically and pelvically by secrecting TNF-alhpa, IL-6, IL-6beta as well as CCL5. Pro-inflammatory environment not only promotes the progression of endometriosis but also affects follicular fluid microenvironment and endometrial receptivity which might result in an unfavorable implantation. Created with BioRender.com.
The complex interplay of inflammatory mediators, cytokines, and immune cells orchestrates a pro-inflammatory microenvironment that fosters the adhesion, invasion, and survival of ectopic endometrial tissue outside the uterine cavity. Elevated levels of pro-inflammatory cytokines, such as interleukin-6 (IL-6), interleukin-1beta (IL-1β), tumor necrosis factor-alpha (TNF-α), and prostaglandin E2 (PGE2) have been consistently identified in women diagnosed with endometriosis (39, 40). PGE2 plays a crucial role in reproductive functions such as ovulation, implantation, parturition, and lactation. Elevated levels of prostaglandins can disrupt peritoneal function, leading to pain and interfering with essential processes like oocyte maturation, ovulation, and fertilization (41). These cytokines play pivotal roles in modulating inflammatory responses, immune cell activation, and tissue remodeling, thereby contributing to the pathophysiology of the disease. Additionally, the CCL5, also referred to as regulated upon activation normal T-cell expressed and secreted (RANTES), has been observed to be markedly increased in both endometrial tissues and follicular fluid of women with endometriosis. CCL5/RANTES functions as a chemoattractant for immune cells and has been implicated in the recruitment and activation of inflammatory cells at the ectopic endometrial sites, further perpetuating the inflammatory milieu characteristic of endometriosis (42–44). The gene encoding CCL5 receptor, known as CCR5, has already been proposed as a potential candidate gene for diagnosing endometriosis (45).
Abnormal high levels of COX-2 isoform and prostaglandins are presented in women suffering from endometriosis (46). Aspirin, however, targeting at cyclooxygenases therefore restricting the production of prostaglandins, has been testified in quite numbers of research to be effective in reducing endometrial lesion size and overall disease burden. Paradoxically, MRP4 expression, elevated of which may result in increased extracellular PGE2, has been found to be triggered in a PPAR-α dependent manner in endometrial cells treated with aspirin (23).
As it is the most commonly prescribed NSAID, aspirin ranks the highest among other NSAIDs in term of annual cost, for instance, Ibuprofen costs £0.86 for 24 tablets of 400 mg, leading to an annual expense of £40.05 (47). Low dose of aspirin, irreversibly targeting platelet cyclooxygenase, leading to decreased production of thromboxane A2, a potent platelet aggregator, is generally used to treat ischemic cardiomyopathy, atrial fibrillation, artificial heart valves, and arteriovenous fistulas in order to reduce the risk of cardiovascular events such as myocardial infarction and stroke. It also has carved out a notable niche in the realm of obstetrics and gynecology, particularly in the prevention of preeclampsia—a serious complication of pregnancy characterized by high blood pressure that might cause multiple organ damage and lead to both fetal and maternal mortality. Patients identified as being at high risk for developing preeclampsia are often prescribed oral low-dose aspirin, typically 50 to 100 mg daily, as a prophylactic measure to mitigate the risk and improve maternal and fetal outcomes (48, 49). Low-dose aspirin plays a pivotal role in the management of antiphospholipid antibody-associated recurrent spontaneous abortion, too (50), basing on antiplatelet properties of aspirin which is believed to help improve blood flow to the placenta and reduce the risk of miscarriage. In addition, aspirin also shows promise in improving the outcomes of IVF/ICSI procedures in women with endometriosis-associated infertility, as testified in previous clinical studies (30).
Over the past 15 years, research has documented the systemic effects of endometriosis. Women diagnosed with endometriosis are increasingly recognized as being predisposed to a higher risk of developing cardiovascular complications like stroke and coronary artery disease (51–53). The underlying pathophysiological mechanisms linking endometriosis to these cardiovascular conditions remain an area of active research but may involve chronic inflammation (53, 54). In addition to cardiovascular implications, endometriosis exerts a notable influence on metabolic processes, particularly within the liver and adipose tissue. This metabolic dysregulation can lead to alterations in body composition and energy metabolism. As a consequence, women with endometriosis often present with a lower body mass index (BMI) compared to individuals without (32, 55). Pain is the most debilitating and common symptom of endometriosis. Women diagnosed with endometriosis often experience cyclic and aggressing pelvic pain, typically during menstruation. Apart from acute pain during menstruation, women may also experience chronic pelvic pain, painful sexual intercourse, and pain associated with bowel and bladder functions. For many women, pain is persistent or chronic. ˄Due to its rapid analgesic effects and lack of suppression on ovarian function, in comparison to hormonal treatment, aspirin demonstrates its own superiority, which may provide an alternative treating strategy.
However, as an antiplatelet drug, long-term use of aspirin could increase the risk of gastrointestinal or other major extracranial bleeds, too. This potential risk presents a limitation for the use of aspirin in the treatment of endometriosis. The current guidelines for occlusive vascular disease still largely recommended that in primary prevention, aspirin be used widely in patients at moderately raised of coronary heart disease, despite the possible bleeding risk (56). The management of bleeding disorders related to long-term use of aspirin involves a combination of strategies aimed at reducing bleeding risk (for example, prescribing the lowest effective dose of aspirin, using combination therapy with PPIs, etc.), monitoring for complications regularly (like a routinely endoscopy, regular follow-up of CBC, etc.), and treating any bleeding events that occur effectively.
Nevertheless, due to the lack of clinical data on long-term use of aspirin in endometriosis patients, the evidence for the effectiveness of NSAIDs in treating endometriosis was weak and contradictory, partly because of the vagueness regarding the exact analgesic used by individuals, for its handy accessibility (47). While there is ongoing research exploring the potential benefits of aspirin in managing endometriosis, its widespread adoption as a therapeutic agent for this condition has yet to be realized. Subsequently, in endometriosis patients, the long-term use of aspirin as primary prevention or therapeutic strategy should be evaluated, for example, assessing the risk of bleeding propensity relative to its preventive or therapeutic benefits. And more dedicated studies focusing on efficacy and safety of long-term use of aspirin in endometriosis patients are urgently needed. There are quite small number of research on the association between aspirin and endometriosis, so the correlation between aspirin and endometriosis remains elusive. More research is needed to explore the role of aspirin in the development and progression of endometriosis, aiming to identify new treatment targets and alternative medications for patients suffering from it.
The complex interplay of these pathological characteristics underscores the multifaceted nature of endometriosis and highlights the importance of targeting inflammatory pathways and cellular mechanisms in the development of novel therapeutic strategies for this debilitating condition (57). Both in vitro and in vivo studies have suggested that aspirin may exert curative effects on ectopic endometrial lesions by reducing cell infiltration and growth, but it is not substantial enough to state that aspirin shall be an effective therapeutic choice for endometriosis, and its long-term utilization necessitates careful evaluation, vigilant monitoring, and individualized patient management strategies to ensure both safety and therapeutic efficacy in clinical practice.
Future directions
There is still need for further experimental research to elucidate the underlying mechanisms of action, optimal dosing regimens, and potential long-term effects of aspirin in endometriosis management. Moreover, there is also a pressing need for the design and execution of rigorously controlled and well-designed clinical trials to provide robust evidence regarding the efficacy, safety, and potential benefits of aspirin-based interventions in endometriosis patients.
Conclusion
Based on the research available currently, it is not substantial enough to address the conclusion that aspirin shall be an effective therapeutic choice for endometriosis, although aspirin as an anti-inflammation drug targeting the COX enzymes, itself or its derivatives might help prevent/lower the risk of endometriosis development in the near future. Thus, further studies are needed to elucidate the efficacy, safety profile, and optimal dosing regimens of aspirin in the context of endometriosis treatment.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Author contributions
YY: Investigation, Methodology, Writing – original draft, Writing – review & editing. HL: Formal analysis, Investigation, Validation, Writing – original draft. ZL: Formal analysis, Investigation, Validation, Writing – original draft. JZ: Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Giudice LC. Clinical practice. Endometriosis. N Engl J Med. (2010) 362:2389–98. doi: 10.1056/NEJMcp1000274
2. Gao X, Outley J, Botteman M, Spalding J, Simon JA, Pashos CL. Economic burden of endometriosis. Fertil Steril. (2006) 86:1561–72. doi: 10.1016/j.fertnstert.2006.06.015
3. Dunselman GA, Vermeulen N, Becker C, Calhaz-Jorge C, D'Hooghe T, De Bie B, et al. ESHRE guideline: management of women with endometriosis. Hum Reprod. (2014) 29:400–12. doi: 10.1093/humrep/det457
4. Chapron C, Marcellin L, Borghese B, Santulli P. Rethinking mechanisms, diagnosis and management of endometriosis. Nat Rev Endocrinol. (2019) 15:666–82. doi: 10.1038/s41574-019-0245-z
5. Parazzini F, Esposito G, Tozzi L, Noli S, Bianchi S. Epidemiology of endometriosis and its comorbidities. Eur J Obstet Gynecol Reprod Biol. (2017) 209:3–7. doi: 10.1016/j.ejogrb.2016.04.021
6. Sampson JA. Peritoneal endometriosis due to the menstrual dissemination of endometrial tissue into the peritoneal cavity. Am Jour Obst Gynec. (1927) 14:422–69. doi: 10.1016/S0002-9378(15)30003-X
7. Matsuzaki S, Darcha C. Epithelial to mesenchymal transition-like and mesenchymal to epithelial transition-like processes might be involved in the pathogenesis of pelvic endometriosis. Hum Reprod. (2012) 27:712–21. doi: 10.1093/humrep/der442
8. Sampson JA. Metastatic or Embolic Endometriosis, due to the Menstrual Dissemination of Endometrial Tissue into the Venous Circulation. Am J Pathol. (1927) 3:93–110 43.
9. Koninckx PR, Ussia A, Adamyan L, Wattiez A, Gomel V, Martin DC. Pathogenesis of endometriosis: the genetic/epigenetic theory. Fertil Steril. (2019) 111:327–40. doi: 10.1016/j.fertnstert.2018.10.013
10. Sourial S, Tempest N, Hapangama DK. Theories on the pathogenesis of endometriosis. Int J Reprod Med. (2014) 2014:179515. doi: 10.1155/2014/179515
11. Saunders PTK, Horne AW. Endometriosis: Etiology, pathobiology, and therapeutic prospects. Cell. (2021) 184:2807–24. doi: 10.1016/j.cell.2021.04.041
12. Buggio L, Somigliana E, Barbara G, Frattaruolo MP, Vercellini P. Oral and depot progestin therapy for endometriosis: towards a personalized medicine. Expert Opin Pharmacother. (2017) 18:1569–81. doi: 10.1080/14656566.2017.1381086
13. Patel BG, Rudnicki M, Yu J, Shu Y, Taylor RN. Progesterone resistance in endometriosis: origins, consequences and interventions. Acta Obstet Gynecol Scand. (2017) 96:623–32. doi: 10.1111/aogs.13156
14. McKinnon B, Mueller M, Montgomery G. Progesterone resistance in endometriosis: an acquired property? Trends Endocrinol Metab. (2018) 29:535–48. doi: 10.1016/j.tem.2018.05.006
15. Varghese M, Lockey RF. Aspirin-exacerbated asthma. Allergy Asthma Clin Immunol. (2008) 4:75–83. doi: 10.1186/1710-1492-4-2-75
16. Ugurlucan M, Caglar IM, Caglar FN, Ziyade S, Karatepe O, Yildiz Y, et al. Aspirin: from a historical perspective. Recent Pat Cardiovasc Drug Discovery. (2012) 7:71–6. doi: 10.2174/157489012799362377
17. Wang L, Zhang J, Zhang H, Li R, Li C, Zhao X, et al. Low-dose aspirin can downregulate progesterone resistance and increase the expression of LIF in endometriosis during the implantation window. Gynecol Endocrinol. (2021) 37:725–9. doi: 10.1080/09513590.2021.1918663
18. Hayes EC, Rock JA. COX-2 inhibitors and their role in gynecology. Obstet Gynecol Surv. (2002) 57:768–80. doi: 10.1097/00006254-200211000-00023
19. MaChado DE, Berardo PT, Landgraf RG, Fernandes PD, Palmero C, Alves LM, et al. A selective cyclooxygenase-2 inhibitor suppresses the growth of endometriosis with an antiangiogenic effect in a rat model. Fertil Steril. (2010) 93:2674–9. doi: 10.1016/j.fertnstert.2009.11.037
20. Matsuzaki S, Canis M, Darcha C, Dallel R, Okamura K, Mage G. Cyclooxygenase-2 selective inhibitor prevents implantation of eutopic endometrium to ectopic sites in rats. Fertil Steril. (2004) 82:1609–15. doi: 10.1016/j.fertnstert.2004.07.946
21. Ota H, Igarashi S, Sasaki M, Tanaka T. Distribution of cyclooxygenase-2 in eutopic and ectopic endometrium in endometriosis and adenomyosis. Hum Reprod. (2001) 16:561–6. doi: 10.1093/humrep/16.3.561
22. Nasiri N, Babaei S, Moini A, Eftekhari-Yazdi P. Controlling semi-invasive activity of human endometrial stromal cells by inhibiting NF-kB signaling pathway using aloe-emodin and aspirin. J Reprod Infertil. (2021) 22:227–40. doi: 10.18502/jri.v22i4.7648
23. Massimi I, Pulcinelli FM, Piscitelli VP, Alemanno L, Maltese T, Guarino ML, et al. Non-steroidal anti-inflammatory drugs increase MRP4 expression in an endometriotic epithelial cell line in a PPARa dependent manner. Eur Rev Med Pharmacol Sci. (2018) 22:8487–96. doi: 10.26355/eurrev_201812_16549
24. Saad-Hossne R, Barretto AB, Siqueira JM, Denadai R. Evaluation of peritoneal endometriosis treatment using intralesional acetylsalicylic acid injection in rabbits. Acta Cir Bras. (2016) 31:227–34. doi: 10.1590/S0102-865020160040000002
25. Siqueira JM, Barreto AB, Saad-Hossne R. Treatment of endometriosis with local acetylsalicylic acid injection: experimental study in rabbits. J Minim Invasive Gynecol. (2011) 18:800–6. doi: 10.1016/j.jmig.2011.08.721
26. Efstathiou JA, Sampson DA, Levine Z, Rohan RM, Zurakowski D, Folkman J, et al. Nonsteroidal antiinflammatory drugs differentially suppress endometriosis in a murine model. Fertil Steril. (2005) 83:171–81. doi: 10.1016/j.fertnstert.2004.06.058
27. Ylikorkala O, Viinikka L. Prostaglandins and endometriosis. Acta Obstet Gynecol Scand Suppl. (1983) 113:105–7. doi: 10.3109/00016348309155209
28. Kauppila A, Puolakka J, Ylikorkala O. Prostaglandin biosynthesis inhibitors and endometriosis. Prostaglandins. (1979) 18:655–61. doi: 10.1016/0090-6980(79)90033-9
29. Flannagan KS, Sjaarda LA, Hill MJ, Connell MT, Zolton JR, Perkins NJ, et al. Pilot randomized trial of short-term changes in inflammation and lipid levels during and after aspirin and pravastatin therapy. Reprod Health. (2019) 16:132. doi: 10.1186/s12978-019-0794-6
30. Moon HS, Park SH, Lee JO, Kim KS, Joo BS. Treatment with piroxicam before embryo transfer increases the pregnancy rate after in vitro fertilization and embryo transfer. Fertil Steril. (2004) 82:816–20. doi: 10.1016/j.fertnstert.2004.02.140
31. Kumbasar S, Gul O, Sik A. Evaluation of the effect of indomethacin and piroxicam administration before embryo transfer on pregnancy rate. J Obstet Gynaecol Res. (2017) 43:536–42. doi: 10.1111/jog.13244
32. Taylor HS, Kotlyar AM, Flores VA. Endometriosis is a chronic systemic disease: clinical challenges and novel innovations. Lancet. (2021) 397:839–52. doi: 10.1016/S0140-6736(21)00389-5
33. Symons LK, Miller JE, Kay VR, Marks RM, Liblik K, Koti M, et al. The immunopathophysiology of endometriosis. Trends Mol Med. (2018) 24:748–62. doi: 10.1016/j.molmed.2018.07.004
34. Lousse JC, Van Langendonckt A, Gonzalez-Ramos R, Defrere S, Renkin E, Donnez J. Increased activation of nuclear factor-kappa B (NF-kappaB) in isolated peritoneal macrophages of patients with endometriosis. Fertil Steril. (2008) 90:217–20. doi: 10.1016/j.fertnstert.2007.06.015
35. Chan RWS, Lee CL, Ng EHY, Yeung WSB. Co-culture with macrophages enhances the clonogenic and invasion activity of endometriotic stromal cells. Cell Prolif. (2017) 50. doi: 10.1111/cpr.12330
36. Shao J, Zhang B, Yu JJ, Wei CY, Zhou WJ, Chang KK, et al. Macrophages promote the growth and invasion of endometrial stromal cells by downregulating IL-24 in endometriosis. Reproduction. (2016) 152:673–82. doi: 10.1530/REP-16-0278
37. Braundmeier A, Jackson K, Hastings J, Koehler J, Nowak R, Fazleabas A. Induction of endometriosis alters the peripheral and endometrial regulatory T cell population in the non-human primate. Hum Reprod. (2012) 27:1712–22. doi: 10.1093/humrep/des083
38. Olkowska-Truchanowicz J, Bocian K, Maksym RB, Bialoszewska A, Wlodarczyk D, Baranowski W, et al. CD4(+) CD25(+) FOXP3(+) regulatory T cells in peripheral blood and peritoneal fluid of patients with endometriosis. Hum Reprod. (2013) 28:119–24. doi: 10.1093/humrep/des346
39. Gazvani R, Templeton A. Peritoneal environment, cytokines and angiogenesis in the pathophysiology of endometriosis. Reproduction. (2002) 123:217–26. doi: 10.1530/rep.0.1230217
40. Scholl B, Bersinger NA, Kuhn A, Mueller MD. Correlation between symptoms of pain and peritoneal fluid inflammatory cytokine concentrations in endometriosis. Gynecol Endocrinol. (2009) 25:701–6. doi: 10.3109/09513590903159680
41. Dawood MY, Khan-Dawood FS, Wilson L Jr. Peritoneal fluid prostaglandins and prostanoids in women with endometriosis, chronic pelvic inflammatory disease, and pelvic pain. Am J Obstet Gynecol. (1984) 148:391–5. doi: 10.1016/0002-9378(84)90713-0
42. Bersinger NA, von Roten S, Wunder DM, Raio L, Dreher E, Mueller MD. PAPP-A and osteoprotegerin, together with interleukin-8 and RANTES, are elevated in the peritoneal fluid of women with endometriosis. Am J Obstet Gynecol. (2006) 195:103–8. doi: 10.1016/j.ajog.2005.12.010
43. Hornung D, Ryan IP, Chao VA, Vigne JL, Schriock ED, Taylor RN. Immunolocalization and regulation of the chemokine RANTES in human endometrial and endometriosis tissues and cells. J Clin Endocrinol Metab. (1997) 82:1621–8. doi: 10.1210/jc.82.5.1621
44. Xu H, Schultze-Mosgau A, Agic A, Diedrich K, Taylor RN, Hornung D. Regulated upon activation, normal T cell expressed and secreted (RANTES) and monocyte chemotactic protein 1 in follicular fluid accumulate differentially in patients with and without endometriosis undergoing in vitro fertilization. Fertil Steril. (2006) 86:1616–20. doi: 10.1016/j.fertnstert.2006.05.043
45. Antinolo G, Fernandez RM, Noval JA, Molini JL, Borrego S. Analysis of the involvement of CCR5-Delta32 and CCR2-V64I variants in the development of endometriosis. Mol Hum Reprod. (2004) 10:155–7. doi: 10.1093/molehr/gah026
46. Liu Y, Hu J, Shen W, Wang J, Chen C, Han J, et al. Peritoneal fluid of patients with endometriosis promotes proliferation of endometrial stromal cells and induces COX-2 expression. Fertil Steril. (2011) 95:1836–8. doi: 10.1016/j.fertnstert.2010.11.039
47. Endometriosis: diagnosis and management. London: National Institute for Health and Care Excellence. (2017).
48. Dekker GA, Sibai BM. Low-dose aspirin in the prevention of preeclampsia and fetal growth retardation: rationale, mechanisms, and clinical trials. Am J Obstet Gynecol. (1993) 168:214–27. doi: 10.1016/S0002-9378(12)90917-5
49. US Preventive Services Task Force, Davidson KW, Barry MJ, Mangione CM, Cabana M, Caughey AB, et al. Aspirin use to prevent preeclampsia and related morbidity and mortality: US preventive services task force recommendation statement. JAMA. (2021) 326:1186–91. doi: 10.1001/jama.2021.14781
50. Kutteh WH. Antiphospholipid antibody-associated recurrent pregnancy loss: treatment with heparin and low-dose aspirin is superior to low-dose aspirin alone. Am J Obstet Gynecol. (1996) 174:1584–9. doi: 10.1016/S0002-9378(96)70610-5
51. Zheng M, Zheng S. Endometriosis increases the risk of stroke: A mendelian randomization study. Stroke. (2023) 54:e30–e3. doi: 10.1161/STROKEAHA.122.041163
52. Poeta do Couto C, Policiano C, Pinto FJ, Brito D, Caldeira D. Endometriosis and cardiovascular disease: A systematic review and meta-analysis. Maturitas. (2023) 171:45–52. doi: 10.1016/j.maturitas.2023.04.001
53. Farland LV, Degnan WJ 3rd, Bell ML, Kasner SE, Liberman AL, Shah DK, et al. Laparoscopically confirmed endometriosis and risk of incident stroke: A prospective cohort study. Stroke. (2022) 53:3116–22. doi: 10.1161/STROKEAHA.122.039250
54. Li PC, Yang YC, Wang JH, Lin SZ, Ding DC. Endometriosis is associated with an increased risk of coronary artery disease in asian women. J Clin Med. (2021) 10. doi: 10.3390/jcm10184173
55. Goetz TG, Mamillapalli R, Taylor HS. Low body mass index in endometriosis is promoted by hepatic metabolic gene dysregulation in mice. Biol Reprod. (2016) 95:115. doi: 10.1095/biolreprod.116.142877
56. Antithrombotic Trialists C, Baigent C, Blackwell L, Collins R, Emberson J, Godwin J, et al. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet. (2009) 373:1849–60. doi: 10.1016/S0140-6736(09)60503-1
Keywords: endometriosis, inflammation, aspirin, endometriosis-related symptoms, endometriosis treatments
Citation: Yang Y, Lai H, Li Z and Zhang J (2024) Endometriosis and aspirin: a systematic review. Front. Endocrinol. 15:1409469. doi: 10.3389/fendo.2024.1409469
Received: 30 March 2024; Accepted: 05 August 2024;
Published: 27 August 2024.
Edited by:
Francesca de Michele, Chirec Delta Hospital, BelgiumReviewed by:
Angelo Finelli, ULSS2 Marca Trevigiana, ItalyHao Wang, Shenzhen University General Hospital, China
Copyright © 2024 Yang, Lai, Li and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jun Zhang, emhhbmcuanVuMkBzemhvc3BpdGFsLmNvbQ==
 Yi Yang
Yi Yang HanHong Lai1
HanHong Lai1 ZhengJuan Li
ZhengJuan Li