- 1School of Humanities and Management, Zhejiang Chinese Medical University, Hangzhou, Zhejiang, China
- 2Department of Quality Management, Jining N0.1 People’s Hospital, Jining, Shandong, China
Objective: This study aimed to comprehensively analyze the incidence of amputation in Chinese patients with diabetic foot ulcers (DFUs).
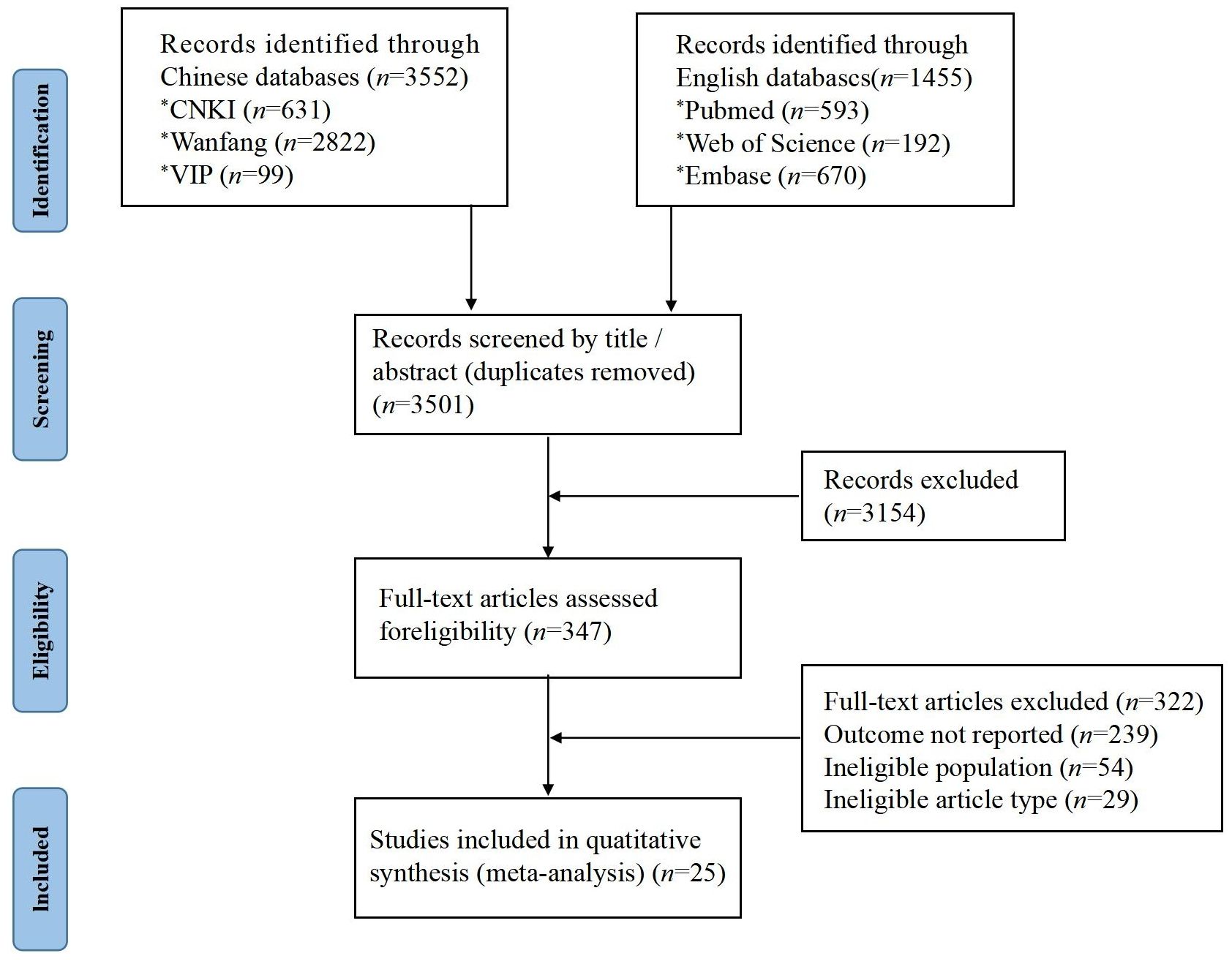
Methods: The Preferred Reporting Items for a Systematic Review and Meta-analysis (PRISMA) guidelines were used. The CNKI, Wanfang Data, VIP, PubMed, Web of Science, and Embase databases were searched to collect relevant literature on the incidence of amputation in Chinese patients with DFUs. Two researchers independently screened the literature, extracted data, and evaluated the risk of bias. The data were systematically analyzed using Stata 17.0 software to determine the incidence of amputation in this patient population.
Results: A total of 25 papers were included in the study, revealing an incidence of amputation in Chinese patients with DFUs of 22.4% (95% confidence interval: 18.3–26.5%). The subgroup analysis revealed that a history of ulcers, Wagner grade >3, and diabetic peripheral vascular disease were the primary risk factors associated with a higher incidence of amputation in Chinese patients with DFUs (P<0.05). Among Chinese patients with DFUs, the amputation group and the non-amputation group showed significant differences in body mass index, duration of DFUs, total cholesterol, triglyceride, fasting blood glucose, white blood cell count, hemoglobin A1c, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, high-sensitivity C-reactive protein, and uric acid (P<0.05).
Conclusion: The high incidence of amputation among Chinese patients with DFUs indicates that interventions should be implemented to prevent or minimize amputations.
Systematic review registration: https://www.crd.york.ac.uk/prospero, identifier CRD42023463976.
Introduction
Diabetes mellitus is a global public health threat that has increased in incidence over the last 20 years (1, 2). Currently, 537 million adults are affected by diabetes. Patients with diabetes are prone to several complications, among which diabetic foot ulcers (DFUs) are particularly prevalent (3). Each year, approximately 18.6 million people with diabetes experience foot ulcers worldwide (4). DFUs are characterized by infection or destruction of the soft tissues of the foot and are classified based on the affected area and extent of the lesions (5). They tend to heal poorly and require long-term, intensive treatment (6). DFUs are currently treated with a variety of therapies, including local surgical debridement (7), dressings to maintain a moist wound environment (8), wound offloading (9), vascular assessment (9), treatment of active infections, and glycemic control (10).
Studies have found the incidence rates of patients with a single occurrence of DFU in the United Kingdom, the United States, Spain, Denmark, and Australia to be 8.22% (11), 8.45% (12), 11.90% (13), 4.49% (14), and 5.35% (15), respectively. In Asia, the incidence rates of DFUs in Japan and Korea were 0.95% (16) and 4.90% (17), respectively. Meanwhile, a meta-analysis revealed that the incidence of recurrent DFUs among patients with diabetes was 38.01% (18). In China, the incidence of DFUs ranges from 17.03% to 42.84% (19–22), which is notably higher than in other countries.
A meta-analysis revealed that the prevalence of depression among patients with DFUs was 47%, with nearly half of the patients experiencing depressive symptoms (23). DFUs impose a heavy financial burden, with a direct cost of treatment estimated to be between 9 billion and 13 billion USD in the United States (24). Additionally, DFUs negatively impact patients’ quality of life (25). Notably, lower limb amputation is the most feared consequence of the disease (26). Given that DFUs significantly increase the risk of amputation, its adverse effects on individuals and society require urgent attention.
Worldwide, approximately 1.6 million people undergo amputations each year, of which approximately 33% are severe amputations. DFUs are the leading cause of nontraumatic amputations (4, 27), with more than 1 million diabetic patients undergoing nontraumatic lower extremity amputations each year, nearly 85% of which are due to DFUs (28). Crude estimates of 5-year mortality after amputation range from 39% to 68%, which is higher than the mortality rates of some common tumors (29). Therefore, it is crucial to implement effective interventions to prevent amputations in patients with DFUs.
A search of the Chinese and international literature revealed a lack of systematic reviews and meta-analysis studies on the incidence of amputation in Chinese patients with DFUs. Among three similar studies, two focused on the incidence and risk factors of lower limb amputation in patients with DFUs (30, 31), with only English-language studies being selected. Some differences were observed between the two studies, including variations in the reported incidence of combined lower extremity amputations. One of the studies lacked a quantitative analysis of the risk factors, while the other explored the epidemiology of diabetic foot amputation and its risk factors in the Middle East (31).
The incidence of amputation in Chinese patients with DFUs cannot be effectively characterized at present due to certain differences in the survey area, survey time, sample size, and other factors. Therefore, this systematic review and meta-analysis aimed to clarify the incidence of amputation in Chinese patients with DFUs and identify the factors influencing this incidence. This information can provide an evidence-based reference for early identification, diagnosis, and intervention to prevent amputation in these patients.
Methods
Protocol
The meta-analysis was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (32). Please see the checklist in Supplementary Material 8. Our research protocol was registered with PROSPERO (CRD42023463976).
Search strategy
The Chinese databases included in the study were CNKI, Wanfang Data, and VIP, while the English databases included were PubMed, Web of Science, and Embase. The search timeframe extended from the inception of the databases to December 2023. The search terms used were (“diabetic foot” OR “diabetic feet” OR “diabetic foot ulcer” OR “diabetic ulcer” OR “diabetic wound” OR “DF” OR “DFU”) AND (“amputation” OR “limb amputation” OR “limb loss”) AND (“China” OR “Chinese”). The researchers used subjects, article titles, or keywords to gather literature on the incidence of amputation in Chinese patients with DFUs and employed a literature tracing method to identify additional relevant literature.
Study selection
The following inclusion criteria were adopted in the study. (1) Population: Chinese patients with DFUs. (2) Intervention and comparison: Whether patients with DFUs in China had undergone amputations. (3) Outcome: Accurate extraction of the incidence of amputation in Chinese patients with DFUs from the literature, or through indirect conversion based on the data in the text. (4) Study design: The study type was observational. We excluded the following studies: (1) reviews and conference abstracts, (2) repetitive publications or literature with data from the same study, and (3) literature with unavailable or untransformed data.
Data extraction
Two researchers independently screened the literature, excerpted relevant information, and cross-checked it. The literature was screened twice—first by reading the title and abstract, and then by examining the full text—to ensure compliance with the inclusion and exclusion criteria, Relevant literature meeting all criteria was included. Specific data excerpts primarily included the following elements. (1) Basic characteristics: first author, survey time, survey area, average age of patients, etc. (2) Outcome indicators: incidence of amputation in Chinese patients with DFUs. If the amputation incidence rate was not specified, it was calculated using the formula: amputation incidence rate = (number of amputations/total sample size)×100. (3) Potential influencing factors: sex, smoking history, drinking history, hypertension, coronary artery disease, ulcer history, duration of DFUs, Wagner grade, neuropathy, peripheral vascular disease (PVD), retinopathy, nephropathy, age, duration of diabetes, body mass index (BMI), total cholesterol (TC), triglyceride (TG), fasting blood glucose (FBG), white blood cell (WBC) count, hemoglobin A1c (HbA1c), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), high-sensitivity C-reactive protein (hs-CRP), and uric acid (Ua).
Quality assessment
The nine-point Newcastle–Ottawa Scale (NOS) (33) was used to assess the quality of cohort and case-control studies. This scale evaluates cohort studies based on eight entries, categorized into three major modules: selection, comparability, and exposure/outcome. The NOS evaluates the quality of the literature using the semi-quantitative principle of the star rating system. With the exception of comparability, which has a maximum two-star rating, the maximum rating for the entries is one star. A full score is 9 stars, with entries having a score of ≥7 being considered high-quality literature.
Statistical analysis
The information from the included literature was entered into a database, and chi-square tests were conducted. Meta-analysis was performed using Stata 17.1 and RevMan 5.3 software. I2 was used to test the heterogeneity of the included studies. If I2<50%, the fixed-effects model was used; if I2>50%, the random-effects model was used. If heterogeneity was detected, subgroup and sensitivity analyses were performed to further investigate its sources. Publication bias was assessed using a funnel plot, Egger’s test, and Begg’s test.
Results
Selection of studies and basic characteristics
A total of 5,007 relevant articles were retrieved. After eliminating duplicates, the titles and abstracts were initially screened, followed by a full-text screening (Figure 1). The 25 included studies were all cohort studies published between 2000 and 2023. The effective sample size included 11,902 cases and 2,140 patients with DFUs who had experienced amputation. The incidence of amputation ranged from 5.10% to 57.03% (Table 1).
The NOS scores of the included studies ranged from 7 to 9, indicating high quality. However, most studies lacked follow-up time and completeness of follow-up (Supplementary Material 1).
Incidence of amputation in Chinese patients with DFUs
The heterogeneity test for the included studies showed I2 = 97.4% (P<0.01), so the random-effects model was chosen for the meta-analysis. The results showed that the incidence of amputation in Chinese patients with DFUs was 22.4% (95% CI 18.3–26.5%) (Figure 2).
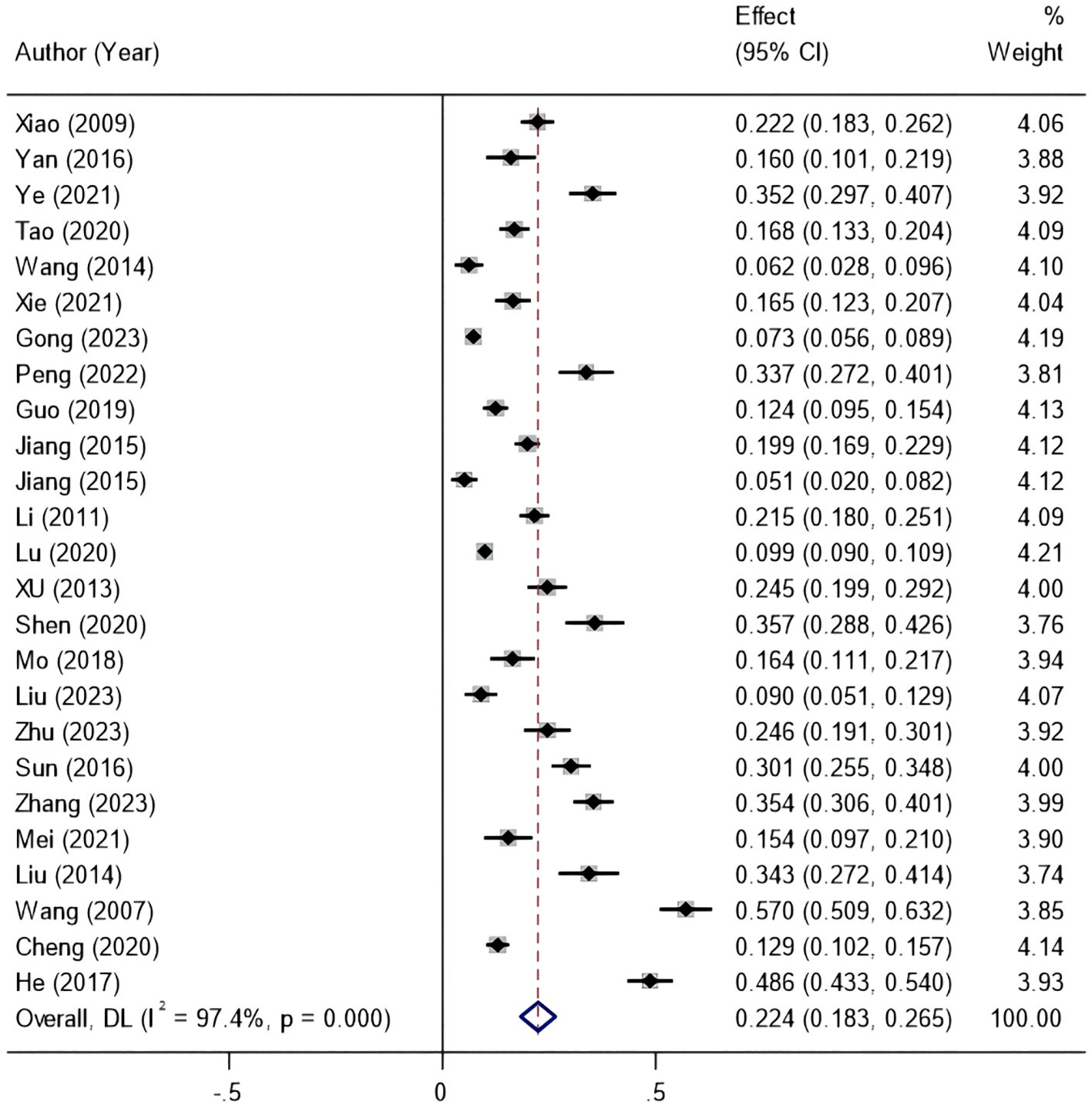
Figure 2. Forest plot of the incidence of amputation in patients with diabetic foot ulcers based on the random-effects model.
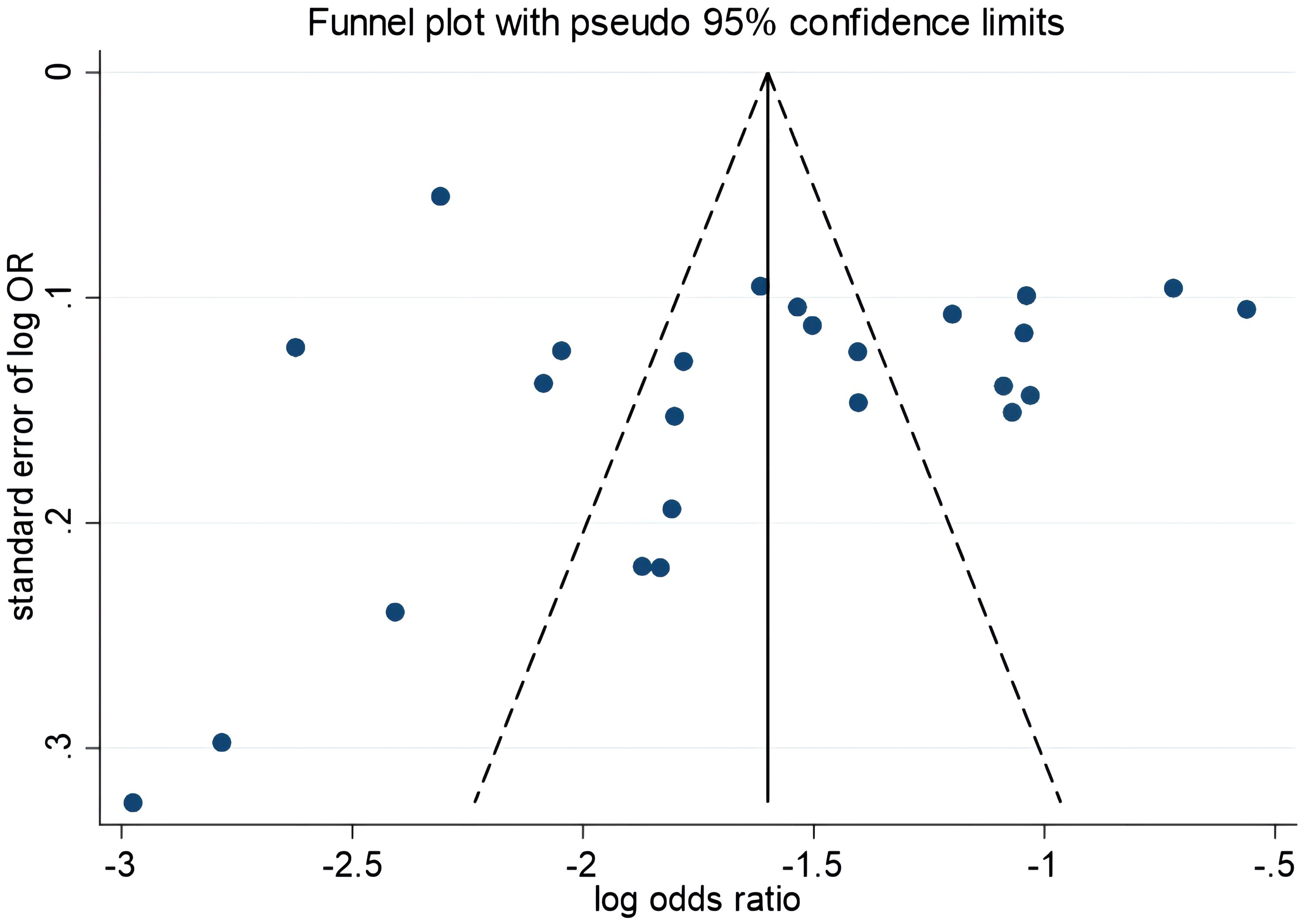
Publication bias
The funnel plot results showed symmetry in the graphical distribution on both sides (Figure 3). Egger’s and Begg’s tests were used to evaluate publication bias. P>0.05 indicated no significant publication bias. Egger’s test (P=0.792) and Begg’s test (P=0.059) suggested that the possibility of publication bias was small.
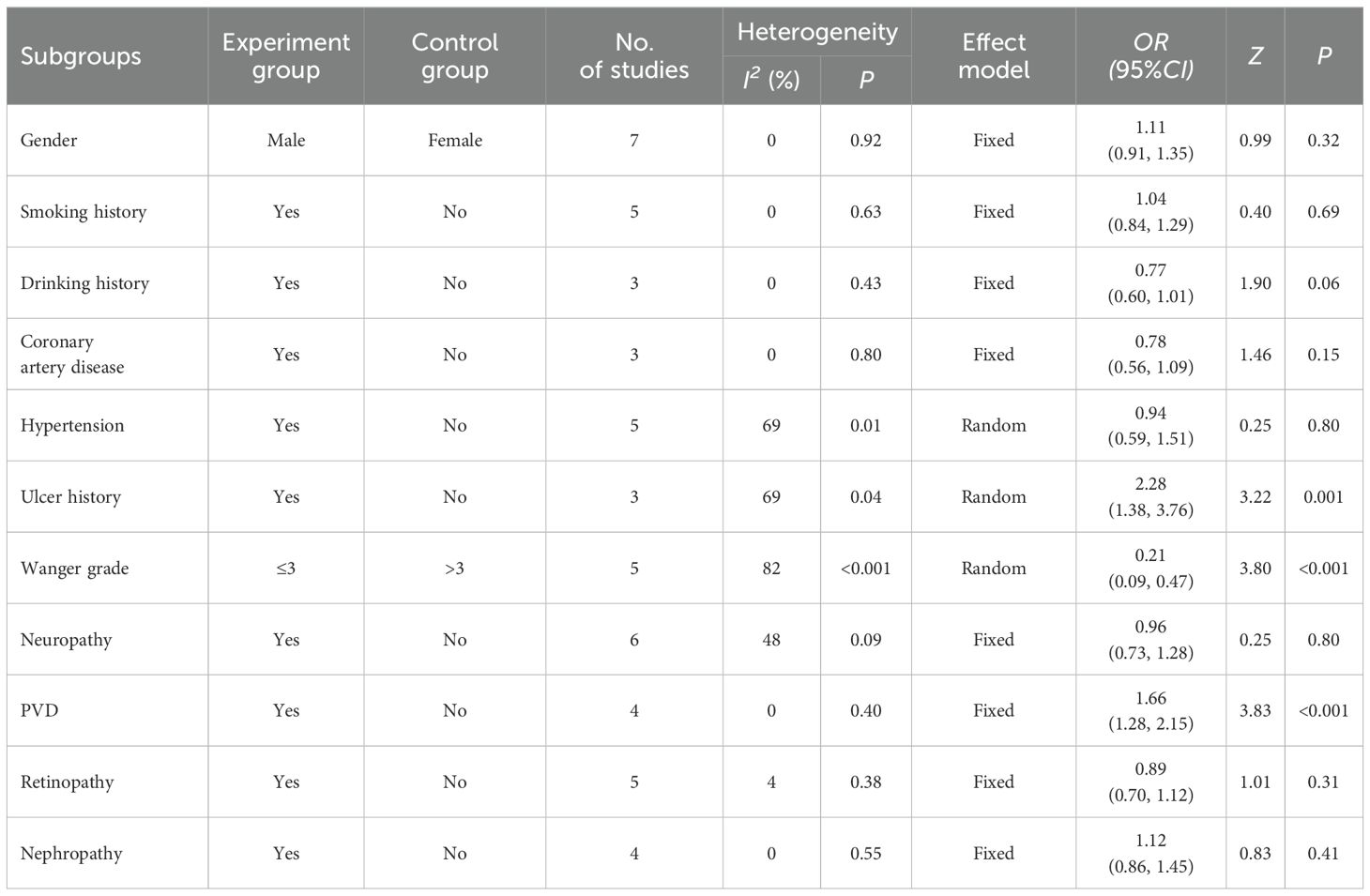
Subgroup analysis
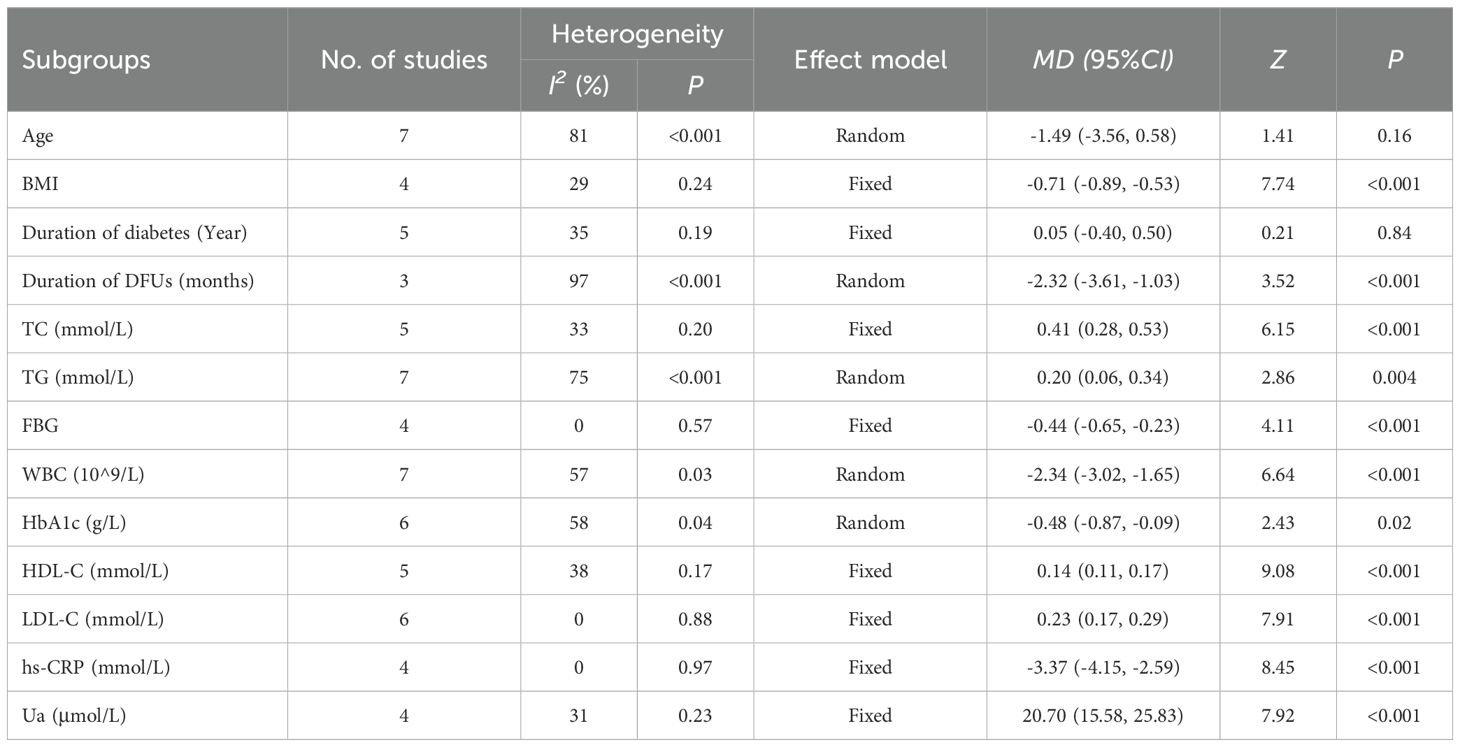
The heterogeneity test results showed that the literature mentioning hypertension, ulcer history, Wagner grade, age, duration of DFUs, TG, WBC, and HbA1c was highly heterogeneous (I2>50%), so a random-effects model was chosen. Sex, smoking history, drinking history, coronary artery disease, neuropathy, PVD, retinopathy, nephropathy, BMI, duration of diabetes, TC, FBG, HDL-C, LDL-C, hs-CRP, and Ua factors were more homogeneous (I2<50%); thus, a fixed-effects model was applied.
Subgroup analysis showed that the incidence of amputation was higher among Chinese patients with DFUs who had an ulcer history, Wagner grade >3, and diabetic peripheral vascular disease (P<0.05) (Table 2) (Supplementary Material 3). Statistically significant differences were found between the amputation and non-amputation groups of Chinese patients with DFUs in terms of BMI, duration of DFUs, TC, TG, FBG, WBC, HbA1c, HDL-C, LDL-C, hs-CRP, and Ua (P<0.05) (Table 3) (Supplementary Material 4-7).
Sensitivity analysis
Sensitivity analyses were performed using the article-by-article exclusion method. The variables for coronary heart disease and BMI showed considerable changes in heterogeneity after excluding Ye’s study (36). Similarly, the variables for diabetes duration and HDL-C showed substantial changes in heterogeneity after excluding Wang’s (37) and Jiang’s (43) studies, respectively. This suggests that these studies may be sources of heterogeneity, leading to their exclusion.
After these exclusions, the sensitivity analysis was performed again with the adjusted analytical model. The OR or MD values and 95% CI from the two analysis models for each subgroup variable were similar (Supplementary Material 2), indicating that the sensitivity of this study was low and the results were more stable.
Discussion
Our meta-analysis showed that the incidence of amputation in patients with DFUs was 22%. In comparison, a meta-analysis showed that the incidence of amputation in patients with DFUs was 19% (57). However, a meta-analysis of Middle Eastern countries found that the incidence of amputation in patients with DFUs was 33% (31). China’s developing economy and vigorous promotion of medical science popularization has led to improved health literacy and increased health awareness. Disease awareness has been increasing among patients with DFUs, and they have gained understanding of potential health hazards such as amputation. However, the incidence of amputation among patients with DFUs in China remains high overall.
China currently lacks medical institutions for diabetes, and hospitals lack specialized departments and clinicians for DFUs. This results in a shortage of medical resources that prevents residents from accessing timely and effective diagnosis and treatment for foot ulcers (58). While patients’ awareness of diabetic foot disease has increased, significant misconceptions still remain (59). Some patients recognize their condition, but delay seeking consultation because of their low economic status. For example, alcohol and trauma stickers are sometimes used to self-treat wounds without proper medical guidance, thus missing the optimal time for treatment, and eventually leading to lower limb amputation (60, 61).
The incidence of amputation is higher among patients with DFUs, who have a ulcer and Wagner >3 grade (P<0.05). A significant difference was also observed in the duration of diabetic foot disease between the amputation and non-amputation groups (P<0.05). This is consistent with the studies by Jiang (43) and Gong (39). All three indicators reflect the severity of the disease, with amputation rates typically increasing with disease severity. Foot ulcers with Wagner grade 1 to 2 generally heal because they do not involve bone tissue. However, a Wagner grade of 3 or higher indicates that the infection involves bone, and the amputation rate is 11 times higher (62).
Our results showed a significant difference in BMI between the amputation and non-amputation groups (P<0.05). BMI is influenced by a patient’s lifestyle, and a high BMI may reflect deficiencies in disease awareness. This highlights the importance of improving patients’ disease-related knowledge and awareness. WBC and hs-CRP were significantly higher in the amputation group compared to the non-amputation group (P<0.05), consistent with findings from Xie’s study (35). High WBC and hs-CRP levels in patients in the amputation group suggest a persistent and severe infection in diabetic foot patients, which correlates with a poor prognosis (34).
Significant differences were observed between the amputation and non-amputation groups in terms of TC, TG, HDL-C, and LDL-C (P<0.05). Nutritional indicators are important for determining the effect and prognosis of DFU treatment, as they are essential for evaluating the nutritional status of patients. Li’s study (21) showed that these indicators are important factors in preventing amputation. LDL-C can cause malnutrition and increased mortality, while HDL-C has anti-atherosclerotic properties (61, 63). Together, these factors can exacerbate the patient’s nutritional status and affect the healing of foot ulcers. This highlights the need for enhanced nutritional support therapy for patients with DFUs.
Studies have demonstrated that intensive glycemic control can reduce the risk of amputation among patients with DFUs (64, 65). Our results showed that FBG and HbA1c levels were significantly higher among patients in the amputation group (P<0.05). A meta-analysis of randomized controlled trials demonstrated that intensive glycemic control reduces the risk of amputation by 35% in patients with diabetic foot syndrome (66). This suggests that poor glycemic control is associated with a higher likelihood of healing difficulties and an increased risk of amputation.
Limitations
This study has some limitations. First, the meta-analysis primarily included cross-sectional single-arm studies, where respondents were susceptible to subjective factors, leading to significant heterogeneity between studies. Second, the limited number of included studies, and the fact that the minimum number of studies included in each subgroup analysis was three, might have impacted the results. Third, relatively few studies were from the central and western regions of China. Fourth, our study was restricted to publications in Chinese and English. This implies that important local studies published in journals in other languages may have been overlooked, which could have led to bias in our findings. Therefore, the primary scope of the investigation was limited to certain provinces and cities, which might have affected the comprehensiveness and representativeness of the results.
Conclusions
We systematically evaluated the incidence of amputation and associated risk factors through meta-analysis. We found a high incidence of amputation, with ulcer history, BMI, TC, TG, FBG, leukocytes, and glycosylated hemoglobin being important factors. Therefore, timely and appropriate interventions for these patients are necessary. We must actively encourage patients to adopt healthier lifestyles and improve their health literacy. Additionally, effectively control of blood glucose levels and infections, improvement in blood supply to the lower limbs, and provision of nutritional support are crucial to effectively reduce the incidence of amputation among Chinese patients with DFUs.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
YZ: Conceptualization, Data curation, Project administration, Software, Writing – original draft, Writing – review & editing. HL: Data curation, Writing – review & editing. YY: Data curation, Writing – review & editing. CF: Data curation, Writing – review & editing. LC: Conceptualization, Data curation, Project administration, Software, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2024.1405301/full#supplementary-material
References
1. Ramachandran A, Snehalatha C, Shetty AS, Nanditha A. Trends in prevalence of diabetes in Asian countries. World J Diabetes. (2012) 3:110–7. doi: 10.4239/wjd.v3.i6.110
2. Shahbazian H, Yazdanpanah L, Latifi SM. Risk assessment of patients with diabetes for foot ulcers according to risk classification consensus of International Working Group on Diabetic Foot (IWGDF). Pak J Med Sci. (2013) 29:730–4. doi: 10.12669/pjms.293.3473
3. Schaper NC, Apelqvist J, Bakker K. The international consensus and practical guidelines on the management and prevention of the diabetic foot. Curr Diabetes Rep. (2003) 3:475–9. doi: 10.1007/s11892-003-0010-4
4. Zhang Y, Lazzarini PA, McPhail SM, van Netten JJ, Armstrong DG, Pacella RE. Global disability burdens of diabetes-related lower-extremity complications in 1990 and 2016. Diabetes Care. (2020) 43:964–74. doi: 10.2337/dc19-1614
5. Schaper NC, van Netten JJ, Apelqvist J, Bus SA, Hinchliffe RJ, Lipsky BA. Practical guidelines on the prevention and management of diabetic foot disease (IWGDF 2019 update). Diabetes Metab Res Rev. (2020) 36 Suppl 1:e3266. doi: 10.1002/dmrr.3266
6. Tong T, Yang C, Tian W, Liu Z, Liu B, Cheng J, et al. Phenotypes and outcomes in middle-aged patients with diabetic foot ulcers: a retrospective cohort study. J Foot Ankle Res. (2020) 13:24. doi: 10.1186/s13047-020-00386-z
7. Biz C, Belluzzi E, Crimi A, Bragazzi NL, Nicoletti P, Mori F, et al. Minimally invasive metatarsal osteotomies (Mimos) for the treatment of plantar diabetic forefoot ulcers (pdfus): A systematic review and meta-analysis with meta-regressions. Appl Sci. (2021) 11:9628. doi: 10.3390/app11209628
8. Jiang P, Li Q, Luo Y, Luo F, Che Q, Lu Z, et al. Current status and progress in research on dressing management for diabetic foot ulcer. Front Endocrinol (Lausanne). (2023) 14:1221705. doi: 10.3389/fendo.2023.1221705
9. Lazzarini PA, Armstrong DG, Crews RT, Gooday C, Jarl G, Kirketerp-Moller K, et al. Effectiveness of offloading interventions for people with diabetes-related foot ulcers: A systematic review and meta-analysis. Diabetes Metab Res Rev. (2024) 40:e3650. doi: 10.1002/dmrr.3650
10. Everett E, Mathioudakis N. Update on management of diabetic foot ulcers. Ann N Y Acad Sci. (2018) 1411:153–65. doi: 10.1111/nyas.13569
11. Anderson SG, Shoo H, Saluja S, Anderson CD, Khan A, Livingston M, et al. Social deprivation modifies the association between incident foot ulceration and mortality in type 1 and type 2 diabetes: a longitudinal study of a primary-care cohort. Diabetologia. (2018) 61:959–67. doi: 10.1007/s00125-017-4522-x
12. Boyko EJ, Ahroni JH, Cohen V, Nelson KM, Heagerty PJ. Prediction of diabetic foot ulcer occurrence using commonly available clinical information: the Seattle Diabetic Foot Study. Diabetes Care. (2006) 29:1202–7. doi: 10.2337/dc05-2031
13. Arrieta F, Piñera M, Iglesias P, Nogales P, Salinero-Fort MA, Abanades JC. Metabolic control and chronic complications during a 3-year follow-up period in a cohort of type 2 diabetic patients attended in primary care in the Community of Madrid (Spain). Endocrinol Nutr. (2014) 61:11–7. doi: 10.1016/j.endonu.2013.09.002
14. Rasmussen A, Almdal T, Anker Nielsen A, Nielsen KE, Jørgensen ME, Hangaard S. Decreasing incidence of foot ulcer among patients with type 1 and type 2 diabetes in the period 2001-2014. Diabetes Res Clin Pract. (2017) 130:221–8. doi: 10.1016/j.diabres.2017.05.025
15. Kästenbauer T, Sauseng S, Sokol G, Auinger M, Irsigler K. A prospective study of predictors for foot ulceration in type 2 diabetes. J Am Podiatr Med Assoc. (2001) 91:343–50. doi: 10.7547/87507315-91-7-343
16. Iwase M, Fujii H, Nakamura U, Ohkuma T, Ide H, Jodai-Kitamura T, et al. Incidence of diabetic foot ulcer in Japanese patients with type 2 diabetes mellitus: the Fukuoka diabetes registry. Diabetes Res Clin Pract. (2018) 137:183–9. doi: 10.1016/j.diabres.2018.01.020
17. Yun JS, Cha SA, Lim TS, Lee EY, Song KH, Ahn YB, et al. Cardiovascular autonomic dysfunction predicts diabetic foot ulcers in patients with type 2 diabetes without diabetic polyneuropathy. Med (Baltimore). (2016) 95:e3128. doi: 10.1097/MD.0000000000003128
18. Huang ZH, Li SQ, Kou Y, Huang L, Yu T, Hu A. Risk factors for the recurrence of diabetic foot ulcers among diabetic patients: a meta-analysis. Int Wound J. (2019) 16:1373–82. doi: 10.1111/iwj.13200
19. Chuan F, Tang K, Jiang P, Zhou B, He X. Reliability and validity of the perfusion, extent, depth, infection and sensation (PEDIS) classification system and score in patients with diabetic foot ulcer. PloS One. (2015) 10:e0124739. doi: 10.1371/journal.pone.0124739
20. Blumberg SN, Warren SM. Disparities in initial presentation and treatment outcomes of diabetic foot ulcers in a public, private, and veterans administration hospital. J Diabetes. (2014) 6:68–75. doi: 10.1111/1753-0407.12050
21. Li X, Xiao T, Wang Y, Gu H, Liu Z, Jiang Y, et al. Incidence, risk factors for amputation among patients with diabetic foot ulcer in a Chinese tertiary hospital. Diabetes Res Clin Pract. (2011) 93:26–30. doi: 10.1016/j.diabres.2011.03.014
22. Aydin K, Isildak M, Karakaya J, Gürlek A. Change in amputation predictors in diabetic foot disease: effect of multidisciplinary approach. Endocrine. (2010) 38:87–92. doi: 10.1007/s12020-010-9355-z
23. Jiang FH, Liu XM, Yu HR, Qian Y, Chen HL. The incidence of depression in patients with diabetic foot ulcers: a systematic review and meta-analysis. Int J Low Extrem Wounds. (2022) 21:161–73. doi: 10.1177/1534734620929892
24. Rice JB, Desai U, Cummings AK, Birnbaum HG, Skornicki M, Parsons NB. Burden of diabetic foot ulcers for medicare and private insurers. Diabetes Care. (2014) 37:651–8. doi: 10.2337/dc13-2176
25. Khunkaew S, Fernandez R, Sim J. Health-related quality of life among adults living with diabetic foot ulcers: a meta-analysis. Qual Life Res. (2019) 28:1413–27. doi: 10.1007/s11136-018-2082-2
26. Jupiter DC, Thorud JC, Buckley CJ, Shibuya N. The impact of foot ulceration and amputation on mortality in diabetic patients. I: from ulceration to death, a systematic review. Int Wound J. (2016) 13:892–903. doi: 10.1111/iwj.12404
27. Behrendt CA, Sigvant B, Szeberin Z, Beiles B, Eldrup N, Thomson IA, et al. International variations in amputation practice: A VASCUNET Report. Eur J Vasc Endovasc Surg. (2018) 56:391–9. doi: 10.1016/j.ejvs.2018.04.017
28. Caravaggi C, Ferraresi R, Bassetti M, Sganzaroli AB, Galenda P, Fattori S, et al. Management of ischemic diabetic foot. J Cardiovasc Surg (Torino). (2013) 54:737–54.
29. Monge L, Gnavi R, Carnà P, Broglio F, Boffano GM, Giorda CB. Incidence of hospitalization and mortality in patients with diabetic foot regardless of amputation: a population study. Acta Diabetol. (2020) 57:221–8. doi: 10.1007/s00592-019-01412-8
30. Lin C, Liu J, Sun H. Risk factors for lower extremity amputation in patients with diabetic foot ulcers: a meta-analysis. PloS One. (2020) 15:e0239236. doi: 10.1371/journal.pone.0239236
31. Bandarian F, Qorbani M, Nasli-Esfahani E, Sanjari M, Rambod C, Larijani B. Epidemiology of diabetes foot amputation and its risk factors in the Middle East region: a systematic review and meta-analysis. Int J Low Extrem Wounds. (2022) Jun 21:15347346221109057. doi: 10.1177/15347346221109057
32. Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. (2015) 4:1. doi: 10.1186/2046-4053-4-1
33. Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses (2019). Available online at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (Accessed January 12, 2024).
34. Xiao T, Wang AH, Xu ZR, Wang YZ, Jiang YF, Gu HB, et al. Analysis of amputation risk factors in 436 patients with diabetic foot ulcers. Chin J Endocrinol Metab. (2009) 25:591–4. doi: 10.3760/cma.j.issn.1000-6699.2009.06.002
35. Yan L, Ma CH, Zhang JX, Zhang MH, Wang ZP. Logistic regression analysis of risk factors of amputation among inpatients with diabetic foot and intervention. Chin J Nosocomiol. (2016) 26:824–6. doi: 10.11816/cn.ni.2016-152341
36. Ye L, Deng JX, Cao DS, Xie J, Pan FM. Risk factors for amputation in patients with diabetic foot ulcer. Acta Universitatis Medicinalis Anhui. (2021) 56:608–12. doi: 10.19405/j.cnki.issn1000-1492.2021.04.020
37. Wang A, Sun X, Wang W, Jiang K. A study of prognostic factors in Chinese patients with diabetic foot ulcers. Diabetes Foot Ankle. (2014) 5:10. doi: 10.3402/dfa.v5.22936
38. Xie P, Deng B, Zhang X, Li YY, Du CZ, Rui SL, et al. Time in range in relation to amputation and all-cause mortality in hospitalised patients with diabetic foot ulcers. Diabetes Metab Res Rev. (2022) 38:e3498. doi: 10.1002/dmrr.3498
39. Gong H, Ren Y, Li Z, Zha PP, Bista R, Li Y, et al. Clinical characteristics and risk factors of lower extremity amputation in the diabetic inpatients with foot ulcers. Front Endocrinol (Lausanne). (2023) 14:1144806. doi: 10.3389/fendo.2023.1144806
40. Peng X, Gou D, Zhang L, Wu HM, Chen Y, Shao X, et al. Status and influencing factors of lower limb amputation in patients with diabetic foot ulcer. Int Wound J. (2023) 20:2075–81. doi: 10.1111/iwj.14076
41. Guo Z, Yue C, Qian Q, He H, Mo Z. Factors associated with lower-extremity amputation in patients with diabetic foot ulcers in a Chinese tertiary care hospital. Int Wound J. (2019) 16:1304–13. doi: 10.1111/iwj.13190
42. Jiang Y, Ran X, Jia L, Yang C, Wang P, Ma J. Epidemiology of type 2 diabetic foot problems and predictive factors for amputation in China. Int J Low Extrem Wounds. (2015) 14:19–27. doi: 10.1177/1534734614564867
43. Jiang Y, Wang X, Xia L, Fu X, Xu Z, Ran X, et al. A cohort study of diabetic patients and diabetic foot ulceration patients in China. Wound Repair Regen. (2015) 23:222–30. doi: 10.1111/wrr.12263
44. Lu Q, Wang J, Wei X, Wang G, Xu Y, Lu Z, et al. Cost of diabetic foot ulcer management in China: A 7-year single-center retrospective review. Diabetes Metab Syndr Obes. (2020) 13:4249–60. doi: 10.2147/DMSO.S275814
45. Xu L, Qian H, Gu J, Shi J, Gu X, Tang Z. Heart failure in hospitalized patients with diabetic foot ulcers: clinical characteristics and their relationship with prognosis. J Diabetes. (2013) 5:429–38. doi: 10.1111/1753-0407.12062
46. Shen JF, Jiang RM, Wang ZQ, Li M, Li J, Xie SY, et al. Recurrence and influencing factors of diabetic foot ulcer in patients with type 2 diabetes mellitus. Chin J Burns. (2020) 36:947–52. doi: 10.3760/cma.j.cn501120-20190726-00315
47. Mo ZW, Chen DX, Gao YY, Quan HB, Chen CR, Wang F, et al. Risk factors for foot ulcer recurrence in diabetic patients with new-onset foot ulcers. Chin Trop Med. (2018) 18:716–9. doi: 10.13604/j.cnki.46-1064/r.2018.07.21
48. Liu WJ. Analysis of factors influencing recurrent diabetic foot ulcers. Nanchang, China:Nanchang University (2023). doi: 10.27232/d.cnki.gnchu.2023.000720
49. Zhu JJ, Li SM. Study on limb infection in diabetic patients and risk factor analysis of amputation. Chin J Health Lab Tec. (2023) 33:1892–6.
50. Sun XX, Wang PH, Zhang JH, Hou XL, Zhao RY, Li XW. Could antibiotics be stopped after symptoms disappear in patients with diabetic foot infection? Chin J Diabetes Mellitus. (2016) 8:346–50. doi: 10.3760/cma.j.issn.1674-5809.2016.06.007
51. Zhang J, Li HF, Li XM, Yao M, Ma HZ, Ma Q. Construction of recurrence risk prediction model for diabetic foot ulcer on the basis of Logistic regression, support vector machine and BP neural network model. Chin Gen Pract. (2023) 26:4013–9. doi: 10.12114/j.issn.1007-9572.2023.0175
52. Mei T. Study on the status and influencing factors of ulcer-free survival days in diabetic foot ulcer patients. Wuhan, China: Huazhong University of Science and Technology (2021). doi: 10.27157/d.cnki.ghzku.2021.001910
53. Liu CB, Huang Y, Ye JN, Ni PW, Lu SL. Prognostic factors for diabetic foot ulcer. Chin J Trauma. (2014) 30:291–7. doi: 10.3760/cma.j.issn.1001-8050.2014.04.002
54. Wang PH, Yu DM, Chu YJ, Song ZQ, Wang JC, Xu J, et al. Research on the clinical features and effective factors of 249 diabetic patients with deep foot infection. Chin J Med. (2007) 87:1828–31.
55. Cheng Y, Zu P, Zhao J, Shi L, Shi H, Zhang M, et al. Differences in initial versus recurrent diabetic foot ulcers at a specialized tertiary diabetic foot care center in China. J Int Med Res. (2021) 49:300060520987398. doi: 10.1177/0300060520987398
56. He Y, Qian H, Xu L, Zhang S, Gu X, Gu J, et al. Association between estimated glomerular filtration rate and outcomes in patients with diabetic foot ulcers: a 3-year follow-up study. Eur J Endocrinol. (2017) 177:41–50. doi: 10.1530/EJE-17-0070
57. Rodrigues BT, Vangaveti VN, Urkude R, Biros E, Malabu UH. Prevalence and risk factors of lower limb amputations in patients with diabetic foot ulcers: a systematic review and meta-analysis. Diabetes Metab Syndr. (2022) 16:102397. doi: 10.1016/j.dsx.2022.102397
58. Li J, Zhang LL, Xu ZR. Construction and development of diabetic foot centers and multidisciplinary approaches for patients with diabetic foot disease. Chin J Diabetes. (2024) 16:28–33. doi: 10.3760/cma.j.cn115791-20230918-00162
59. Wang HL, Ye Y, Zhou J, Li N, Li XY, Dai WW, et al. Need for an intelligent management platform for diabetic foot: a qualitative descriptive study. Chin J Diabetes. (2023) 15:1280–5. doi: 10.3760/cma.j.cn115791-20230915-00143
60. Gershater MA, Löndahl M, Nyberg P, Larsson J, Thörne J, Eneroth M, et al. Complexity of factors related to outcome of neuropathic and neuroischaemic/ischaemic diabetic foot ulcers: a cohort study. Diabetologia. (2009) 52:398–407. doi: 10.1007/s00125-008-1226-2
61. Zhang Y, Lei S, Yang F. Meta-analysis of delay rate in patients with diabetic foot in China. Mod Prev Med. (2023) 50:3197–202. doi: 10.20043/j.cnki.MPM.202302321
62. Wang YZ, Wang AH, Zhao S, Li Q, Wang PH, Yan L, et al. Differences in risk factors of diabetic foot in the patients in South and North China. Zhonghua Yi Xue Za Zhi. (2007) 87:1817–20.
63. Liu Y, Coresh J, Eustace JA, Longenecker JC, Jaar B, Fink NE, et al. Association between cholesterol level and mortality in dialysis patients: role of inflammation and malnutrition. JAMA. (2004) 291:451–9. doi: 10.1001/jama.291.4.451
64. Goldman MP, Clark CJ, Craven TE, Davis RP, Williams TK, Velazquez-Ramirez G, et al. Effect of intensive glycemiccontrol on risk of lower extremity amputation. J Am Coll Surg. (2018) 227:596–604. doi: 10.1016/j.jamcollsurg.2018.09.021
65. Imran S, Ali R, Mahboob G. Frequency of lower extremity amputation in diabetics with reference to glycemic control and Wagner’s grades. J Coll Phys Surg Pakistan. (2006) 16:124–7.
Keywords: amputation, diabetic foot ulcers, meta-analysis, risk factors, systematic review
Citation: Zhang Y, Liu H, Yang Y, Feng C and Cui L (2024) Incidence and risk factors for amputation in Chinese patients with diabetic foot ulcers: a systematic review and meta-analysis. Front. Endocrinol. 15:1405301. doi: 10.3389/fendo.2024.1405301
Received: 08 May 2024; Accepted: 15 August 2024;
Published: 30 August 2024.
Edited by:
Carlo Biz, University of Padua, ItalyReviewed by:
Nicola Luigi Bragazzi, University of Parma, ItalyElisa Belluzzi, University of Padua, Italy
Copyright © 2024 Zhang, Liu, Yang, Feng and Cui. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Liwei Cui, bXNjdWkwNTUyQDE2My5jb20=
 Yujie Zhang
Yujie Zhang Hui Liu2
Hui Liu2