- 1Department of Neurosurgery, Huazhong University of Science and Technology Union Shenzhen Hospital (Nanshan Hospital), Shenzhen, China
- 2Department of Neurosurgery, The First Hospital of China Medical University, Shenyang, China
- 3Department of Geriatrics, Shengjing Hospital of China Medical University, Shenyang, China
Background: Pituitary adenomas (PAs) present with clinical features such as neuroendocrine abnormalities and mass effects, common in the general morbidity population. However, in elderly patients, the disease progression renders some clinical features difficult to detect and identify in time. Consequently, elderly patients with PAs are often not identified and receive sufficient intervention on time to achieve a satisfactory outcome.
Methods: Clinical data were collected from 114 consecutive patients older than 70 years with PAs who had undergone surgery. Based on the average age, the patients were categorized into a younger group and an elder group, and were statistically analyzed and compared.
Results: Sixty-five males (57.0%) and 49 females (43.0%) were included in the study, with an average age of 73.2 years. Their common preoperative symptoms included vision impairment, followed by headache and vomiting, and visual field defect. The milder the preoperative visual impairment, the greater the possibility of post-operative visual improvement (P=0.001). The tumors were primarily non-functional pituitary adenomas (NFPAs, 73.7%), with a high degree of suprasellar invasion but a low degree of parasellar invasion (P<0.0001). For further analysis, based on the average age, we categorized the patients into younger (age< 73 years, 59 cases) and elder (age≥ 73 years, 55 cases) groups. The elder group was more likely to have preoperative vision impairment problems (P=0.044), whilst post-operative visual improvement was worse (P=0.001). The elder group also had a more severe suprasellar invasion (P=0.009), with a higher proportion of NFPA than the younger group (P=0.006). Compared to the younger group, the tumors in the elder group were larger (P=0.039), and had a higher rate of apoplexy (P=0.039), and were more likely to have comorbid postoperative complications (P=0.031), such as fever and cerebrospinal fluid (CSF) leakage, compared to the younger group.
Conclusions: Elderly patients with PA had specific clinical characteristics. Their relatively worse pre- and post-operative conditions and intraoperative findings illustrated the need for early surgery.
Introduction
Pituitary adenomas (PAs) are benign tumors originating from the anterior pituitary gland, with an incidence of 3.9 to 7.4 cases per 100,000 (1). PAs are typically detected as they cause abnormal hormone secretion or mass effect, producing clinical symptoms (2). The clinical features of PAs vary across different age groups. PAs have been found to be more likely to cause hormone-related symptoms in younger patients (3), while they are often mass effect or hypopituitarism in elderly patients (4, 5). PAs in the elderly account for 10-15% of all cases, with increasing detection rates as people aspire for a better quality of life (5–7). The detection of the mass effect or hypopituitarism in elderly patients with PA is often delayed, thus affecting prognosis (5, 7). In the elderly with PAs, transsphenoidal surgery (TSS) is generally considered to be the preferred and safe option; nonetheless, major controversies still exist regarding the improvement of preoperative symptoms (in terms of visual acuity) and the recovery of hypopituitarism and tumor recurrence (8–13). Therefore, this single-center retrospective study aimed to analyze the unique clinical characteristics of PA in elderly to facilitate better identification and timely intervention in such patients.
Methods
Patients
A total of 114 consecutive elderly patients (over 70 years old) diagnosed with PA underwent surgery in the Department of Neurosurgery, The First Hospital of China Medical University, between January 2011 and February 2019. All patients underwent transnasal endoscopic or microscopic surgery. Approval for this study was obtained from the institutional review board at The First Hospital of China Medical University. Written informed consent was obtained from each patient or their relatives for using their clinical data for a retrospective study.
Clinical examinations
A detailed medical history, including the history of previous illnesses, smoking, and alcohol consumption, of all patients was taken. On admission, pre-operative investigations were routinely performed, including hormone tests to determine the type of PA and magnetic resonance imaging (MRI) of the sellar region to determine tumor morphology. Visual disability included vision impairment as measured by an eye chart and visual field defect as measured by computerized perimetry. The visual impairment score (VIS) was used to evaluate visual disability caused by compression of the optic nerve and chiasma (14). The surgical risk was categorized by American Society of Anesthesiologists (ASA) score, scaled from I to VI, according to physical status and overall health of the patients. The degree of tumor invasion to the supra- and para-sellar region, were graded, respectively, through Hardy-Wilson classification and Knosp classification (15, 16). Further, tumor volume was approximated using the ellipsoid formula (V=πabc/6, a, b, c were anteroposterior diameter, transverse diameter, and axial diameter, respectively). Intraoperative information on clinical features, post-operative review of hormone levels, and post-operative complication data were also collected and analyzed. The intergroup comparisons were also made.
Near-total resection (NTR) means the removal of at least 90% of the tumor, whereas subtotal resection (STR) means that less than 90% of the tumor has been removed. Abnormal hormone levels were assessed based on baseline hormone levels with the following normal range: luteinizing hormone (LH): 6-34 mIU/mL; follicle-stimulating hormone (FSH): 2-22 mIU/mL; prolactin (PRL): 1.5-30 μg/L; growth hormone (GH): 0.05-8 μg/L; insulin-like growth factor-I (IGF-1): 10-500 ng/mL; adrenocorticotropic hormone (ACTH): 7.2-63.3 pg/mL; cortisol (COR): 171-536 nmol/L forenoon, and 64-327 nmol/L afternoon.
Tumor classification follows the World Health Organization 2017 classification (17) of tumors of the pituitary, and is combined with clinical symptoms and pre-operative hormone tests (18). Patients with preoperative PRL levels greater than 250 μg/L were diagnosed with lactotroph adenomas. Patients with elevated IGF-1 levels (>750 ng/mL) detected twice preoperatively, and lack of suppression of GH levels during an oral glucose tolerance test, were diagnosed with somatotroph adenomas. Patients, after underwent cortisol and dexamethasone suppression test to prove hypercortisolism, were diagnosed with corticotroph adenomas when sellar mass was detected as well as ectopic corticotropin secretion was excluded. Patients with one or more pituitary hormones deficiency measured by postoperative serum hormone level were diagnosed with hypopituitarism (19). Post-operative pathology and immunohistochemical analyses were conducted by the Department of Pathology, The First Hospital of China Medical University.
Statistical analysis
The chi-square test and t-test were used to identify statistical differences in the data of interest and to compare the two groups. Statistical analysis was performed using SPSS v25.0 (SPSS Inc., Chicago, IL). Differences were considered statistically significant at P<0.05.
Results
Clinical features
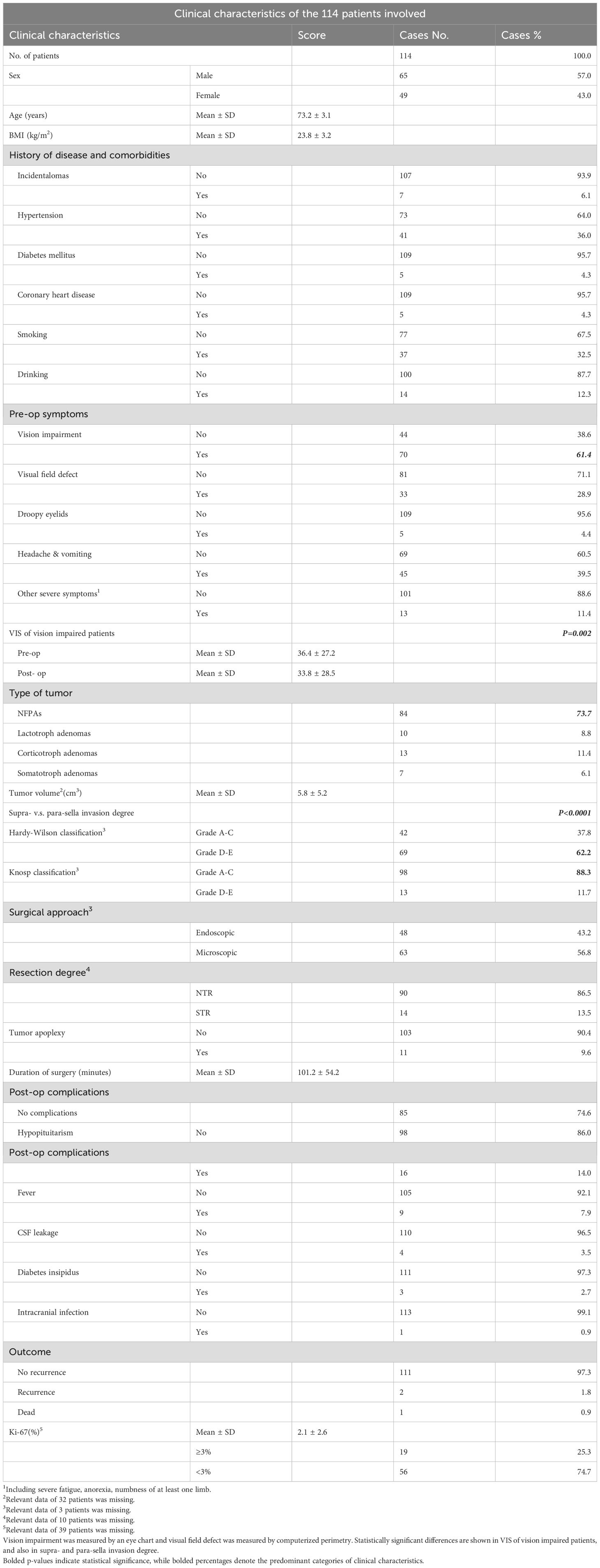
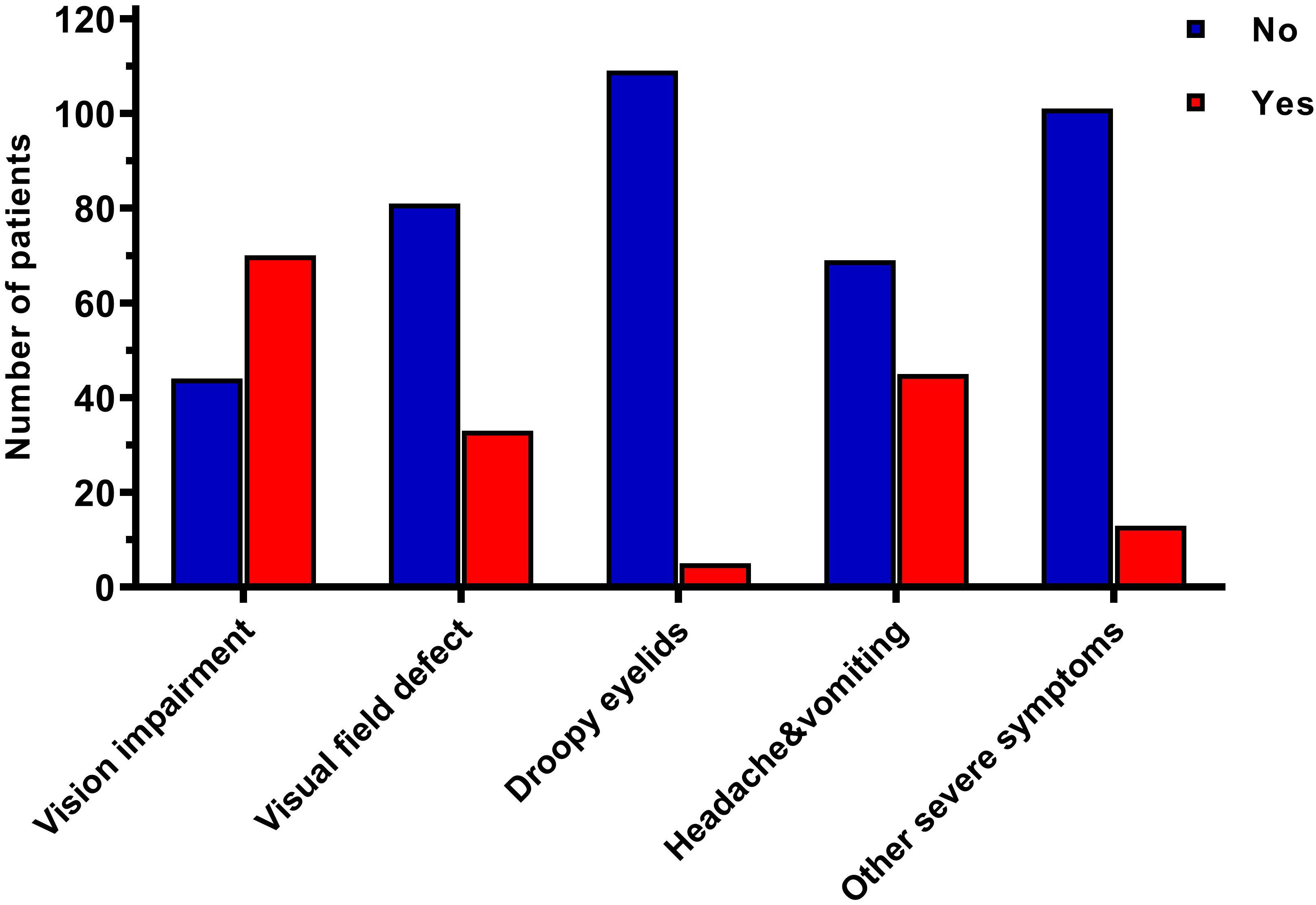
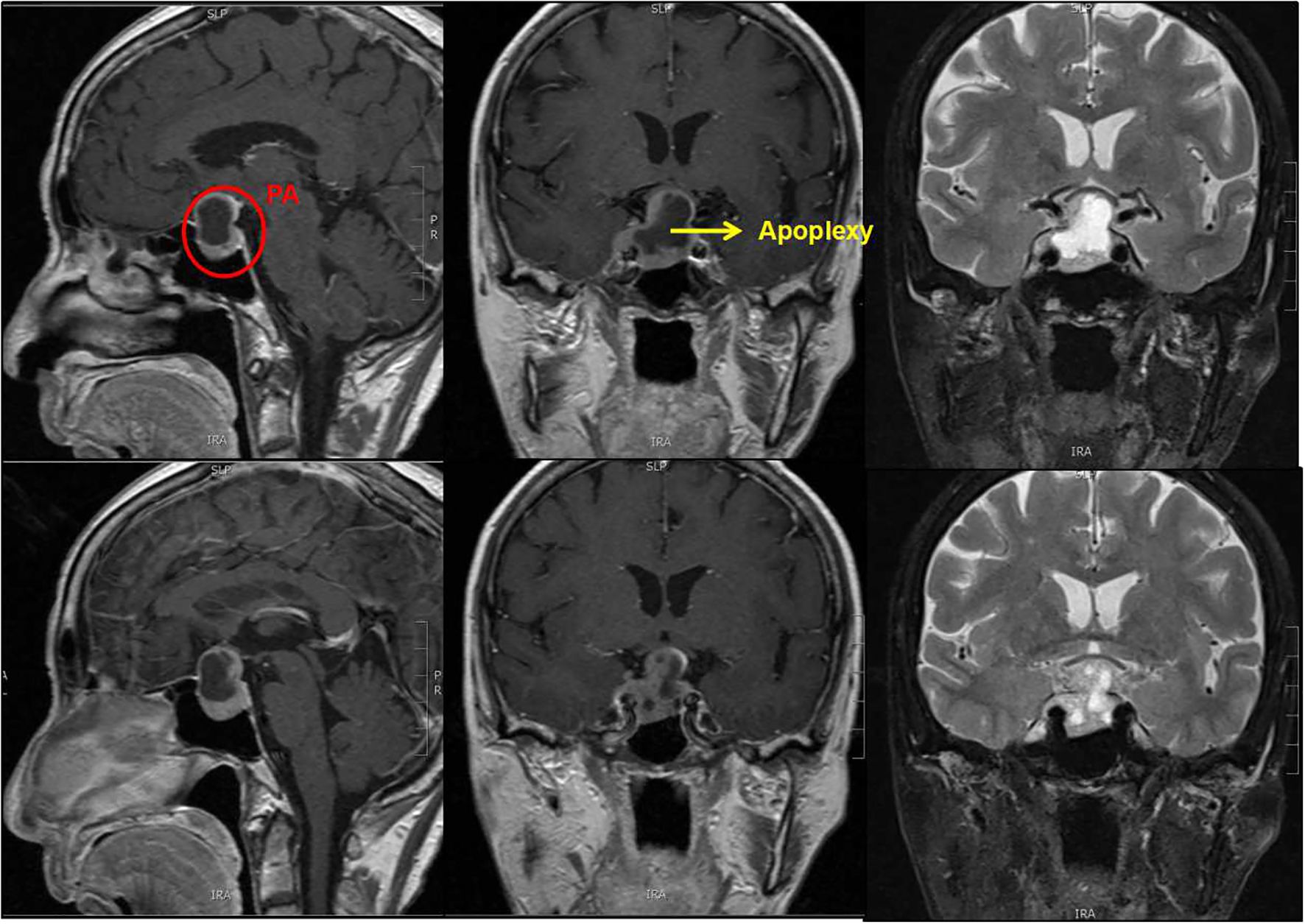
A total of 65 males (57.0%) and 49 females (43.0%), with an average age of 73.2 years, were included in the study (Table 1). Among these, 41 (36%) had a history of hypertension, and 37 (32.5%) had a history of smoking. Most preoperative symptoms included vision impairment (70 patients, 61.4%), followed by headache and vomiting (45 patients, 39.5%), and visual field defect (33 patients, 28.9%), (Figure 1). There were 84 (73.7%) non-functional pituitary adenomas (NFPAs), 10 (8.8%) lactotroph adenomas (six of whom had preoperative visual acuity loss and visual field defects, two had severe preoperative headache, dizziness, and vomiting, one had cranial nerve III palsy and one experienced consciousness disturbance), 13 (11.4%) corticotroph adenomas, and 7 (6.1%) somatotroph adenomas, (Figure 2A). The average tumor volume was 5.8 cm3, with the average longest diameter of 2.5 cm (mean ± standard deviation [SD]: 2.5 ± 0.9 cm). The study also documented seven pituitary microadenomas, seventy-one pituitary macroadenomas, and four giant pituitary adenomas. The degree of tumor aggressiveness towards the suprasellar area was quantified using the Hardy-Wilson classification. There were 42 (37.8%) patients with Grade A-C and 69 (62.2%) with Grade D-E. Likewise, the Knosp classification was used to quantify the degree of para-sellar invasion. The results showed 98 (88.3%) patients with Grade A-C and 13 (11.7%) with Grade D-E of para-sellar invasion. The degree of suprasellar invasion in the young group was significantly higher than that of parasellar invasion in these elderly patients (P<0.0001, Figure 2B).
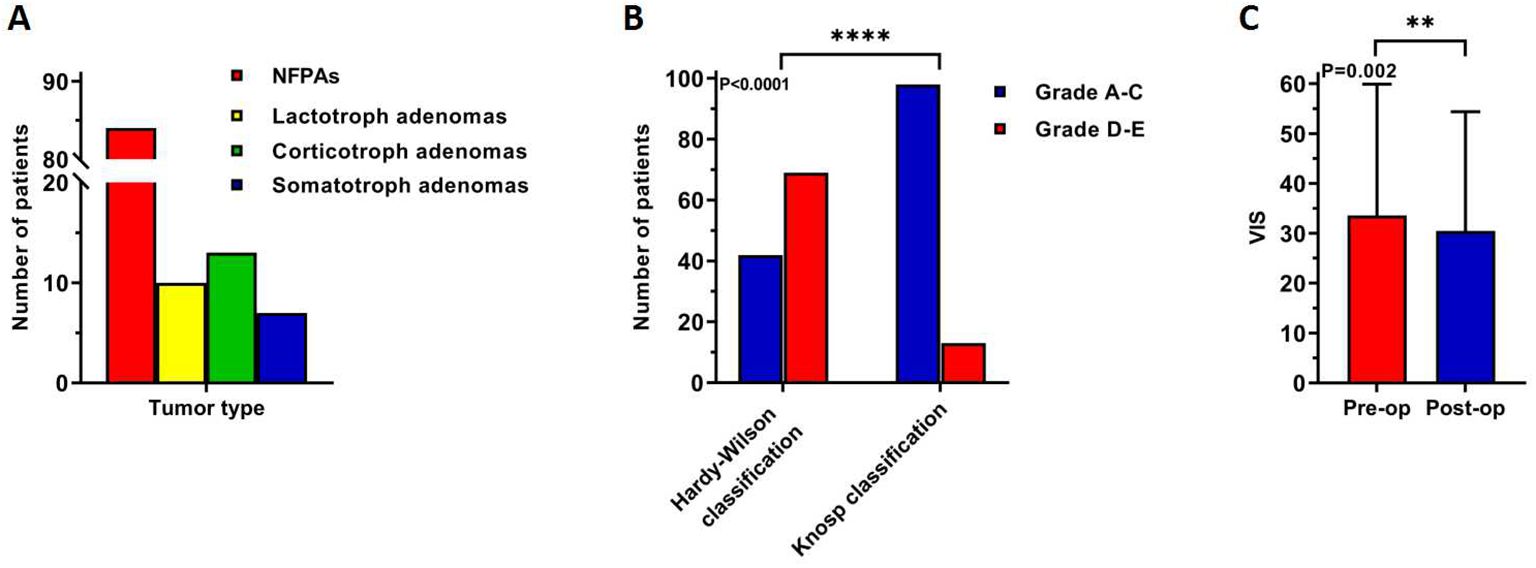
Figure 2. Difference in clinical characteristics of 114 elderly patients: (A) tumor type, (B) a high degree of suprasellar invasion while a low degree of parasellar invasion, (C) post-operative visual impairment was improved. **: P<0.01; ****: P<0.0001.
Forty-eight (43.2%) patients underwent endoscopic surgery, while 63 (56.8%) underwent microscopic surgery. NTR of the tumor was achieved in 90 (86.5%) and STR in 14 (13.5%) patients. Visual improvement was observed in 20/74 patients with visual impairment and visual field defect. Preoperative VIS of these 74 patients was 36.4 ± 27.2, while post-operative VIS was 33.8 ± 28.5, and the difference was statistically significant (P=0.002, Figure 2C). Eleven (9.6%) patients experienced tumor apoplexy, but it did not affect preoperative and postoperative VIS (P=0.087 and P=0.151, respectively). The main post-operative complications were hypopituitarism, fever, cerebrospinal fluid (CSF) leakage, diabetes insipidus and intracranial infection. Sixteen (14.0%) patients had post-operative hypopituitarism, nine (7.9%) had a post-operative fever, four (3.5%) had post-operative nasal leakage of CSF, three (2.7%) had post-operative diabetes insipidus, and one (0.9%) had post-operative intracranial infection. The standard treatment protocol for post-operative hypopituitarism included oral hormone replacement therapy. Patients with post-operative fever were routinely managed through physical cooling and, antibiotics was administered in case of infection diagnosis. Patients with post-operative CSF nasal leakage were treated at an early stage of detection by placing the lumbar puncture and fluid drainage system which was combined with antibiotics application to prevent meningitis. Anti-diuretic treatment was given to patients who developed post-operative diabetes insipidus. One patient in the younger group required long-term oral hormone replacement therapy, while each of the above-mentioned post-operative complications was effectively managed and resolved without delay or serious consequences. Most patients (111 cases, 97.3%) had a good prognosis, however, tumor recurrence was observed in the other two patients, and one patient died due to respiratory circulatory accident during post-operative hospitalization.
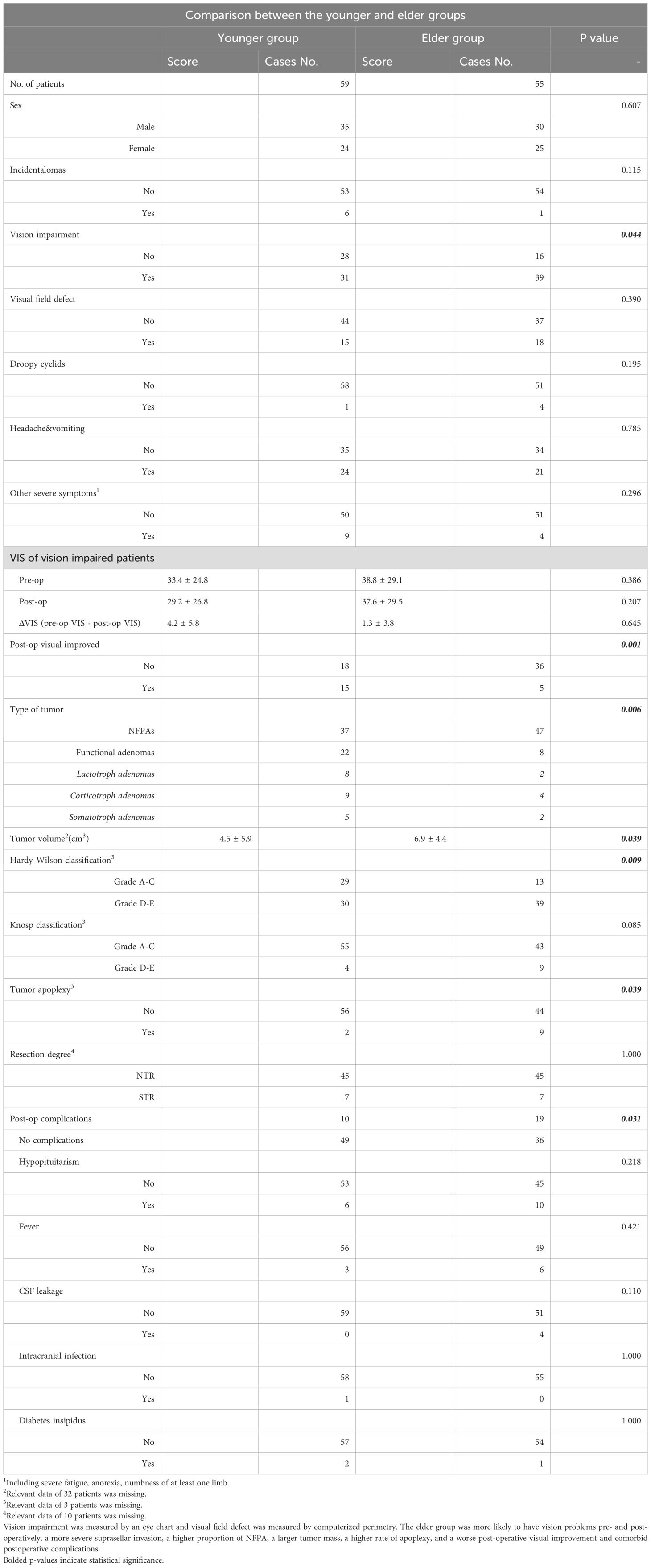
Comparison between the two groups
We performed a normality test on the age distribution. The skewness and peakness values were 1.324 and 1.922, respectively. Thus, based on the average age, we divided the patients were categorized into younger (age < 73 years, 59 cases) and elder (age ≥ 73 years, 55 cases) groups and statistical analysis was performed again. The results are presented in Table 2 and Figure 3. Compared to the younger group, patients in the elderly group were more likely to have larger tumor volume (P=0.039), preoperative vision impairment (P=0.044, Figure 3A), and higher grades in the Hardy-Wilson classification (P=0.009, Figure 3B). Further, the post-operative visual recovery in the elderly group was effective to a lesser degree than in the younger group (P=0.001, Figure 3C). NFPAs in the elderly group were more common compared to the younger group (P=0.006, Figure 3D), as were tumor apoplexy (P=0.039, Figure 3E), and post-operative complications (P=0.031, Figure 3F). A statistical comparison revealed that no complication was more likely to occur in the elderly group (post-op hypopituitarism, P=0.218; post-op fever, P=0.421; post-op CSF leakage, P=0.110; post-op intracranial infection, P=1.000; post-op diabetes insipidus, P=1.000). However, all four patients experiencing CSF leakage were in the elderly group.
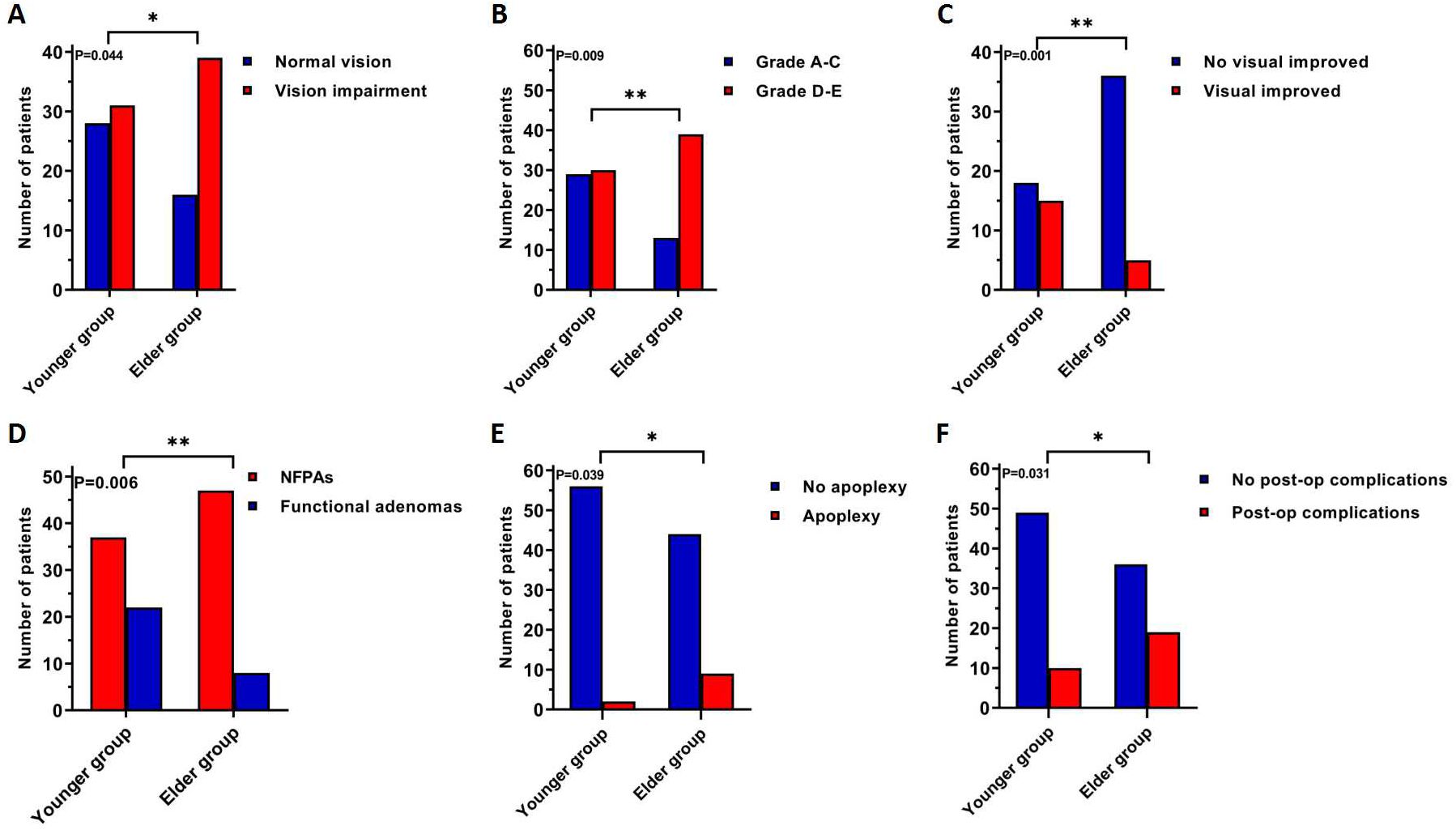
Figure 3. A comparison of clinical characteristics shows statistically significant differences between younger and elder groups, patients in the elderly group were more likely to have: (A) pre-operative visual impairment, (B) pre-operative supra-sella invasion (C) post-operative visual improvement, (D) NFPAs, (E) tumor apoplexy, (F) post-operative complications. *: P<0.05; **: P<0.01.
Discussion
Visual issues
The incidence of PA in the elderly has been reported at the rate of 4%-10% (3, 20). With the increased emphasis on life expectancy, the detection of pituitary tumors in the elderly is also increased. Nearly half of patients with NFPAs have been reported to potentially experience comorbid visual impairment, as can some hormone-secreting PAs, and a small number of patients with pituitary microadenomas (21). Elderly patients with PAs are more likely to experience symptoms of preoperative visual loss (61.4% in our study) and headache and vomiting (39.5% in our study); further, older patients were more likely to have symptoms of visual loss, which may be related to chiasmatic compression due to prolonged presence of the tumor (11–13, 22–24) and the gradual increase in symptoms was misdiagnosed as other diseases, such as cataract (3, 24–26), leading to delayed treatment (5, 9, 20). We found a correlation between the degree of preoperative visual impairment and the degree of postoperative visual improvement in elderly patients, with patients with mild preoperative visual impairment more likely to achieve postoperative improvement. The degree of visual improvement was not related to age, however, patients in the younger group were more likely to achieve visual improvement, which is consistent with the previous study (28, 29).
Hormonal features of pituitary adenomas in the elderly
PAs in elderly patients often present as non-functional or hypopituitarism, which is usually underestimated (3, 5, 9, 11, 12, 20, 22, 25, 27, 29). NFPAs account for 1/3 of all PAs (2). The current consensus indicates that a high proportion of PAs in the elderly are NFPAs (20), consistent with the findings of the present study. According to the latest PA pathological classification, about 3/4 of the number of elderly patients had these adenomas; however, this proportion did not increase with age, possibly because the age of the study population was more than 70 years, during which the hormonal and other body functions decline, for the anterior pituitary gland undergoes fibrosis and vascular alterations (5). As a result, the proportion of functional PAs in this group was lower than in the general population. Besides, hormonal PAs are often detected in young patients because of clinical symptoms due to abnormal hormone levels; in contrast, they are usually detected in older people because of the mass effect, often caused by NFPAs (20).
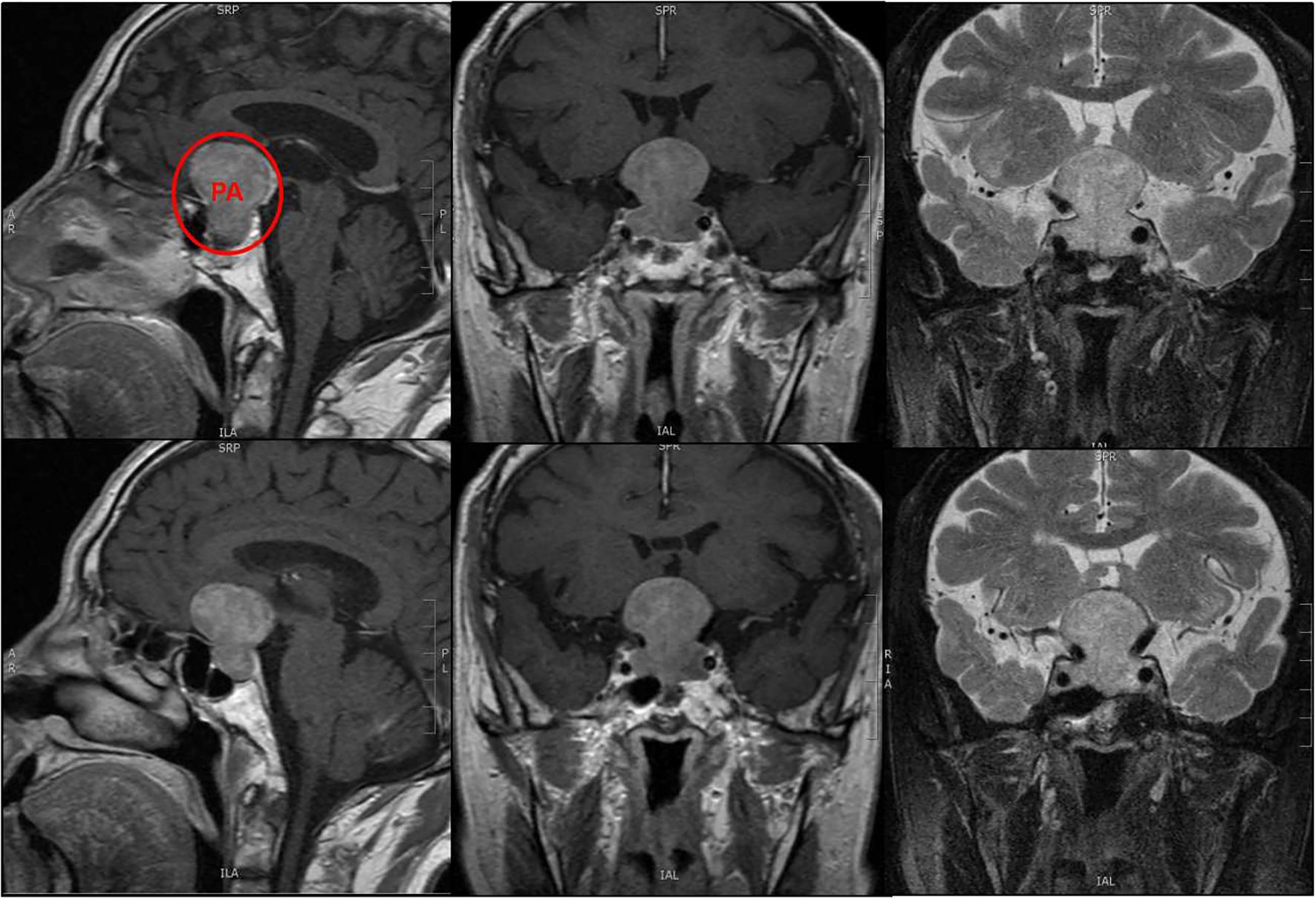
Suprasellar and parasellar invasion
In the current study, tumor invasion to the suprasellar region was generally higher in elderly patients (Figure 4), while that to the para-sellar region was generally lower, in accordance with earlier published studies (9, 30, 31). Nonetheless, with age, tumor growth to the para-sellar region begins to occur, which may subsequently lead to palsy of the oculomotor nerves post-operatively, with prolonged post-operative recovery time (11, 12). Although vision impairment was more severe in the elderly age group, we did not find any correlation between this and the degree of suprasellar invasion of the tumor, as reported in a previous study (30). Similarly, the increase in the degree of parasellar invasion with age did not lead to any significant difference in clinical symptoms. We hypothesize that this was because the number of patients with suprasellar invasion was generally larger than those with parasellar invasion (69 cases vs. 13 cases), as a result, older patients usually consulted more for optic nerve function impairment. Increased incidence of headaches has been reported (12) in the elderly age group, considering that the mass effect of the tumor is associated with increasing age, which is in contrast to our findings and those reported in other studies (27, 32).
Other comorbidities and complications
Consistent with the previous studies (5, 11, 23, 28, 31), there was a low probability of tumor apoplexy (9.6%, Figure 5), however, the risk of apoplexy increased with age (20). The mechanism of tumor apoplexy is complex, the exact factor could not be identified in this study, although previous studies have suggested that this may be associated with hypertension, coronary heart disease, or the use of anticoagulants (5, 20).
The extent of tumor resection was not affected by age (P=1.000) and the majority of patients in this study (97.3%) had no recurrence; this confirmed the effectiveness of transnasal surgery for the treatment of PAs in the elderly, as reported in other studies (3, 26, 33, 34). The probability of post-operative complications may increase with age; in fact, a relatively high level of cranial complications has been reported in elderly patients (11, 12, 31, 35), suggesting the need for aggressive early surgical treatment for symptomatic PAs in the elderly. However, this statement remains controversial (10, 13, 25, 29, 33). Transnasal endoscopic or microscopic approaches have been demonstrated to be safe and effective (7, 9, 23, 25, 30, 33), or even better in the elderly group (9, 27), while another study showed frequently increased anesthesia risk in elderly patients due to other medical conditions (3, 32). In our study, 62 (54.3%) patients had coexisting physical problems such as hypertension, diabetes mellitus, coronary heart disease, or a history of drinking and smoking that may cause pulmonary and liver function abnormalities. All patients had the ASA score in the range of I to III (39 patients were ASA I, 44 patients were ASA II, and 31 patients were ASA III, respectively). Three patients (2.7%) in our study had post-operative diabetes insipidus, all of which were transient. As there were no patients with pre-operative diabetes insipidus in earlier reports, we suggest that the presence of diabetes insipidus in this study may be related to local stimulation of the hypothalamus and/or pituitary stalk as a result of intraoperative manipulation. Post-operative diabetes insipidus is associated with injury to the hypothalamus or posterior pituitary, leading to impaired production and transport of antidiuretic hormone (33, 36). All cases of post-operative CSF leak were low-flowing, and originated from the elderly group, but the difference was not statistically significant, consistent with the previous study (7, 11, 20, 33, 34). We did not analyze the causes of CSF leaks as only four cases occurred in our study; however previous studies have shown that surgical technique is the primary causes of this complication (11, 33), in addition to the late healing of wounds in elder patients (23). Careful intra-operative manipulation to prevent the perforation of saddle septum and skull base reconstruction minimizes post-operative CSF leakage.
Limitations
This study had a few limitations: It was a single-center retrospective study, and, given the specificity of the population, long-term follow-up could not be conducted. Therefore, subsequent multi-center prospective studies with long-term follow-up are still needed to validate the results.
Conclusions
In this study, we found that in elderly patients with PA, visual impairment was the majority of preoperative symptoms. The tumors were frequently non-functional and associated with hypopituitarism, often showing a high degree of suprasellar invasion but minimal parasellar invasion. The correlation between post-operative visual improvement and preoperative visual acuity highlights the importance for early surgical intervention to salvage vision in elderly patients.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by The First Hospital of China Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
RW: Data curation, Formal analysis, Writing – original draft, Writing – review & editing. XH: Data curation, Writing – review & editing. CX: Data curation, Writing – review & editing. QZ: Conceptualization, Funding acquisition, Writing – review & editing. LK: Methodology, Supervision, Writing – review & editing. SH: Conceptualization, Funding acquisition, Methodology, Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was funded by grants from the LiaoNing Revitalization Talents Program (no. XLYC1807253) and Clinical Key Disciplines of Nanshan District.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Daly AF, Beckers A. The epidemiology of pituitary adenomas. Endocrinol Metab Clin North Am. (2020) 49:347–55. doi: 10.1016/j.ecl.2020.04.002
2. Molitch ME. Diagnosis and treatment of pituitary adenomas: A review. Jama. (2017) 317:516–24. doi: 10.1001/jama.2016.19699
3. Wang R, Wang Z, Song Y, Li L, Han X, Han S. Comparative analysis of pituitary adenoma with and without apoplexy in pediatric and adolescent patients: a clinical series of 80 patients. Neurosurgical Rev. (2022) 45:491–8. doi: 10.1007/s10143-021-01551-z
4. Hong J, Ding X, Lu Y. Clinical analysis of 103 elderly patients with pituitary adenomas: transsphenoidal surgery and follow-up. J Clin Neurosci. (2008) 15:1091–5. doi: 10.1016/j.jocn.2007.11.003
5. Minniti G, Esposito V, Piccirilli M, Fratticci A, Santoro A, Jaffrain-Rea ML. Diagnosis and management of pituitary tumours in the elderly: a review based on personal experience and evidence of literature. Eur J Endocrinol. (2005) 153:723–35. doi: 10.1530/eje.1.02030
6. Tatsi C, Stratakis CA. Aggressive pituitary tumors in the young and elderly. Rev Endocrine Metab Disord. (2020) 21:213–23. doi: 10.1007/s11154-019-09534-8
7. Pereira MP, Oh T, Joshi RS, Haddad AF, Pereira KM, Osorio RC, et al. Clinical characteristics and outcomes in elderly patients undergoing transsphenoidal surgery for nonfunctioning pituitary adenoma. Neurosurgical Focus. (2020) 49:E19. doi: 10.3171/2020.7.FOCUS20524
8. Choo YH, Seo Y, Kim OL. The outcomes of surgical treatment via transsphenoidal approach for patients with nonfunctioning pituitary adenoma: a single institution's experience. Ann Med. (2022) 54:3136–45. doi: 10.1080/07853890.2022.2140449
9. Villar-Taibo R, Díaz-Ortega C, Sifontes-Dubon M, Fernández-Pombo A, Serramito-García R, Martínez-Capoccioni G, et al. Pituitary surgery in elderly patients: a safe and effective procedure. Endocrine. (2021) 72:814–22. doi: 10.1007/s12020-021-02665-6
10. Biamonte E, Betella N, Milani D, Lasio GB, Ariano S, Radice S, et al. Impact of age on postsurgical outcomes of nonfunctioning pituitary adenomas. Endocrine. (2021) 72:915–22. doi: 10.1007/s12020-020-02554-4
11. Tardivo V, Penner F, Garbossa D, Di Perna G, Pacca P, Salvati L, et al. Surgical management of pituitary adenomas: does age matter? Pituitary. (2020) 23:92–102. doi: 10.1007/s11102-019-01014-1
12. Memel Z, Chesney K, Pangal DJ, Bonney PA, Carmichael JD, Zada G. Outcomes following transsphenoidal pituitary surgery in the elderly: A retrospective single-center review. Operative Neurosurg (Hagerstown Md). (2019) 16:302–9. doi: 10.1093/ons/opy109
13. Chen SH, Sprau A, Chieng L, Buttrick S, Alam ES, Ali SC, et al. Transsphenoidal approach for pituitary adenomas in elderly patients. World Neurosurg. (2019) 121:e670–e4. doi: 10.1016/j.wneu.2018.09.187
14. Fahlbusch R, Schott W. Pterional surgery of meningiomas of the tuberculum sellae and planum sphenoidale: surgical results with special consideration of ophthalmological and endocrinological outcomes. J Neurosurg. (2002) 96:235–43. doi: 10.3171/jns.2002.96.2.0235
15. Wilson CB. Neurosurgical Management of Large and Invasive Pituitary Tumors. In: Tindall GT, Collins WF, editors. Clinical Management of Pituitary Disorders. Raven Press, New York (1979). p. 335–42.
16. Knosp E, Steiner E, Kitz K, Matula C. Pituitary adenomas with invasion of the cavernous sinus space: A magnetic resonance imaging classification compared with surgical findings. Neurosurg. (1993) 33:610–8. doi: 10.1227/00006123-199310000-00008
17. Lloyd RV, Osamura RY, Kloppel G, Rosai J. WHO Classification of Tumours of the Endocrine Organs. 4th edn. Lyon: InternationalAgency for Research on Cancer (2017).
18. Tritos NA, Miller KK. Diagnosis and management of pituitary adenomas: A review. JAMA. (2023) 329:1386–98. doi: 10.1001/jama.2023.5444
19. Fleseriu M, Christ-Crain M, Langlois F, Gadelha M, Melmed S. Hypopituitarism. Lancet. (2024) 403:2632–48. doi: 10.1016/S0140-6736(24)00342-8
20. Liu J, Li C, Xiao Q, Gan C, Chen X, Sun W, et al. Comparison of pituitary adenomas in elderly and younger adults: clinical characteristics, surgical outcomes, and prognosis. J Am Geriatrics Soc. (2015) 63:1924–30. doi: 10.1111/jgs.2015.63.issue-9
21. Butenschoen VM, Schwendinger N, von Werder A, Bette S, Wienke M, Meyer B, et al. Visual acuity and its postoperative outcome after transsphenoidal adenoma resection. Neurosurgical Rev. (2021) 44:2245–51. doi: 10.1007/s10143-020-01408-x
22. Turner HE, Wass JA. Pituitary tumours in the elderly. Bailliere's Clin Endocrinol Metab. (1997) 11:407–22. doi: 10.1016/S0950-351X(97)80377-1
23. Kurosaki M, Lüdecke DK, Flitsch J, Saeger W. Surgical treatment of clinically nonsecreting pituitary adenomas in elderly patients. Neurosurgery. (2000) 47:843–8. doi: 10.1097/00006123-200010000-00009
24. Locatelli M, Bertani G, Carrabba G, Rampini P, Zavanone M, Caroli M, et al. The trans-sphenoidal resection of pituitary adenomas in elderly patients and surgical risk. Pituitary. (2013) 16:146–51. doi: 10.1007/s11102-012-0390-z
25. Watanabe T, Uehara H, Takeishi G, Chuman H, Azuma M, Yokogami K, et al. Characteristics of preoperative visual disturbance and visual outcome after endoscopic endonasal transsphenoidal surgery for nonfunctioning pituitary adenoma in elderly patients. World Neurosurg. (2019) 126:e706–e12. doi: 10.1016/j.wneu.2019.02.132
26. Azab MA, O'Hagan M, Abou-Al-Shaar H, Karsy M, Guan J, Couldwell WT. Safety and outcome of transsphenoidal pituitary adenoma resection in elderly patients. World Neurosurg. (2019) 122:e1252–e8. doi: 10.1016/j.wneu.2018.11.024
27. Zhao Y, Lian W, Xing B, Feng M, Liu X, Wang R, et al. The clinical characteristics and microsurgical therapy of pituitary adenomas in elderly patients: A retrospective study of 130 cases. J Clin Neurosci. (2017) 46:13–6. doi: 10.1016/j.jocn.2017.08.038
28. Robenshtok E, Benbassat CA, Hirsch D, Tzvetov G, Cohen ZR, Iraqi HM, et al. Clinical course and outcome of nonfunctioning pituitary adenomas in the elderly compared with younger age groups. Endocrine Pract. (2014) 20:159–64. doi: 10.4158/EP13182.OR
29. Spina A, Losa M, Mortini P. Pituitary adenomas in elderly patients: clinical and surgical outcome analysis in a large series. Endocrine. (2019) 65:637–45. doi: 10.1007/s12020-019-01959-0
30. Rosinha P, Fonseca L, Amaral C, Ribeiro I, Cardoso MH. Pituitary adenomas in the elderly: Retrospective comparative analysis of clinical/tumor features and surgical data by age group. Medicine. (2022) 101:e30825. doi: 10.1097/MD.0000000000030825
31. Gondim JA, Almeida JP, de Albuquerque LA, Gomes E, Schops M, Mota JI. Endoscopic endonasal transsphenoidal surgery in elderly patients with pituitary adenomas. J Neurosurg. (2015) 123:31–8. doi: 10.3171/2014.10.JNS14372
32. Kinoshita Y, Kurisu K, Arita K. Nonfunctioning pituitary adenomas in elderly patients. J Clin Neurosci. (2018) 53:127–31. doi: 10.1016/j.jocn.2018.04.054
33. Zhan R, Ma Z, Wang D, Li X. Pure endoscopic endonasal transsphenoidal approach for nonfunctioning pituitary adenomas in the elderly: surgical outcomes and complications in 158 patients. World Neurosurg. (2015) 84:1572–8. doi: 10.1016/j.wneu.2015.08.035
34. Chinezu R, Fomekong F, Lasolle H, Trouillas J, Vasiljevic A, Raverot G, et al. Risks and benefits of endoscopic transsphenoidal surgery for nonfunctioning pituitary adenomas in patients of the ninth decade. World Neurosurg. (2017) 106:315–21. doi: 10.1016/j.wneu.2017.06.151
35. Wilson PJ, Omay SB, Kacker A, Anand VK, Schwartz TH. Endonasal endoscopic pituitary surgery in the elderly. J Neurosurg. (2018) 128:429–36. doi: 10.3171/2016.11.JNS162286
Keywords: pituitary adenomas, elderly patients, visual impairment, tumor apoplexy, retrospective study
Citation: Wang R, Han X, Xie C, Zhang Q, Kan L and Han S (2024) Comparative analysis of clinical characteristics of symptomatic pituitary adenomas in elderly patients: a consecutive series of 114 patients. Front. Endocrinol. 15:1385813. doi: 10.3389/fendo.2024.1385813
Received: 01 March 2024; Accepted: 20 November 2024;
Published: 06 December 2024.
Edited by:
Xiang'En Shi, Capital Medical University, ChinaReviewed by:
Peizhi Zhou, Sichuan University, ChinaMaria Eugenia Sabatino, Instituto de Ciencia y Tecnología de Alimentos Córdoba (ICyTAC-CONICET), Argentina
Yuan Shan, Baylor Scott and White Health, United States
Copyright © 2024 Wang, Han, Xie, Zhang, Kan and Han. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sheng Han, aGFuc2hlbmcyMDAxX3hAYWxpeXVuLmNvbQ==; Liang Kan, a2FubGlhbmczMWNtdUAxNjMuY29t; Qinghua Zhang, ZG9jdG9yemhhbmdodWFAMTYzLmNvbQ==
 Run Wang
Run Wang Xiaodi Han2
Xiaodi Han2 Liang Kan
Liang Kan Sheng Han
Sheng Han