- 1Faculty of Medicine, University of Geneva, Geneva, Switzerland
- 2Unit of Therapeutic Patient Education, WHO Collaborating Centre, Geneva University Hospitals, Geneva, Switzerland
- 3Department of Integrated Systems Engineering, The Ohio State University, Columbus, OH, United States
- 4Faculty Diabetes Centre, Faculty of Medicine, University of Geneva, Geneva, Switzerland
Aims: Adherence to therapeutic footwear is vital for effective diabetic foot ulcer prevention and treatment. Understanding the key adherence factors and potential barriers is important for footwear design and implementation. Our team is creating intelligent offloading footwear to prevent lower extremity amputations in people living with diabetes (PLwD). This exploratory study assessed the ability of the established Unified Theory of Acceptance and Use of Technology (UTAUT) model to predict behavioral intention to use or recommend this intelligent offloading footwear by PLwD, caregivers of PLwD, or medical professionals treating PLwD.
Methods: Online and paper questionnaires were implemented to assess the impact of the UTAUT model factors (performance expectancy, effort expectancy, social influence, facilitating conditions) and psychosocial factors (attitude, anxiety, self-efficacy) on the overall behavioral intention to use the footwear. Furthermore, factors influencing potential acceptance and rejection of the footwear were explored.
Results: Patients (4.0/5) and medical professionals (4.1/5) showed a behavioral intention to “agree” to use or recommend the footwear when it becomes available. Structural equation modeling showed that the UTAUT constructed model may not be the best indicator for behavioral intention here based on a lack of statistical significance. However, the logistic regression modeling showed that the social influence for PLwD (p=0.004) and the attitude toward the footwear for medical professionals (p=0.001) may be the most important when designing and implementing the footwear, though several other factors (performance expectancy, effort expectancy, facilitating conditions, and self-efficacy) were also important for one or both of these populations. Additionally, cost and clinician support were shown to be important factors influencing potential acceptance of the footwear.
Conclusions: The study found promising intention to use the intelligent footwear in the future. This highlights the need to continue future development and implementation of the footwear to incorporate these results, thus improving the likelihood of high adherence of the footwear.
1 Introduction
One in ten adults globally has diabetes (1). Diabetic foot ulcers affect 19-34% of people living with diabetes (PLwD) and are a leading cause of amputations in this population (2–5). Diabetes-related lower-extremity amputations lead to an increase in illness-related costs and a diminished quality of life compared to the general population (6). Studies have shown an increase in the prevalence of psychiatric disorders among this group of PLwD including depression and posttraumatic stress disorder (7). Lower-extremity amputations are also related to significant early and long-term post-operative mortality (8). There is a need to contribute to the currently available preventive modalities for these foot ulcers that can lead to amputations.
Diabetic foot ulcers are primarily due to peripheral neuropathy, or a lack of sensation in the extremities, coupled with high pressures under the foot (9). When the high pressures are not perceived by the patient and therefore not offloaded during walking, they can lead to callus formation, subcutaneous hemorrhaging, and then a foot ulcer which, if infected, can lead to an amputation. There are many ways to prevent and treat foot ulcers including surgical approaches (10, 11); however, the most prevalent approaches are pressure offloading interventions. Current methods include non-removable (e.g., total contact casts) and removable (e.g., removable cast walkers, custom insoles and footwear) interventions, with the former possibly increasing pre-existing challenges such as mobility and daily living activity impairments, low quality of life, and stigmatization (12–16). Removable interventions are often preferred by PLwD for convenience and adaptability to lifestyle (17); they have had varied success, but research has shown that using the interventions has positive effects (18, 19).
For removable interventions, one of the main limiting factors for ulcer healing is non-adherence. Higher adherence is associated with ulcer healing (20) and thus a lower risk for amputation. However, fewer than 50% of PLwD and neuropathy, who are especially at risk for ulceration, wear their therapeutic footwear (newly-prescribed, custom-made) for more than 60% of daytime hours (21, 22). Other studies have shown that 28-60% of patients adhere to footwear recommendations (23).
Among some of the most influential factors of footwear dissatisfaction and thus adherence in this population are footwear weight (21, 24), comfort (21), style (25), and the perceived opinions of others (26). Furthermore, Maslow’s Hierarchy of Needs, as described for product development research, maintains that these factors must be accounted for, especially to satisfy the need categories of social needs (e.g. belonging), esteem needs (e.g. positive self-evaluation and dignity) and self-actualization needs (e.g. self-fulfillment and beauty) (27, 28). Research has also shown that higher adherence is linked to the patient having paid employment, a current or previous foot ulcer, and an understanding of the risks associated with neuropathy along with the conviction that the footwear aids ulcer healing (29). In terms of the practical use of the footwear, important factors for adherence include the satisfaction level of the follow-up for the footwear, self-efficacy, storage location/type of footwear at home, and consistency of the type of footwear worn (29). Although these aesthetic needs may be considered by some to be less important than physiological needs for people with diabetes at risk for ulceration, they still greatly influence acceptability. Furthermore, it is essential to appeal to the patient themselves and address misconceptions regarding foot health, types of footwear, and footwear fit through therapeutic patient education to ensure that the overall foot care and footwear are appropriate (30–32). To address and design for all the needs of an individual, user-centered design principles such as user feedback assessments should be implemented during the design process.
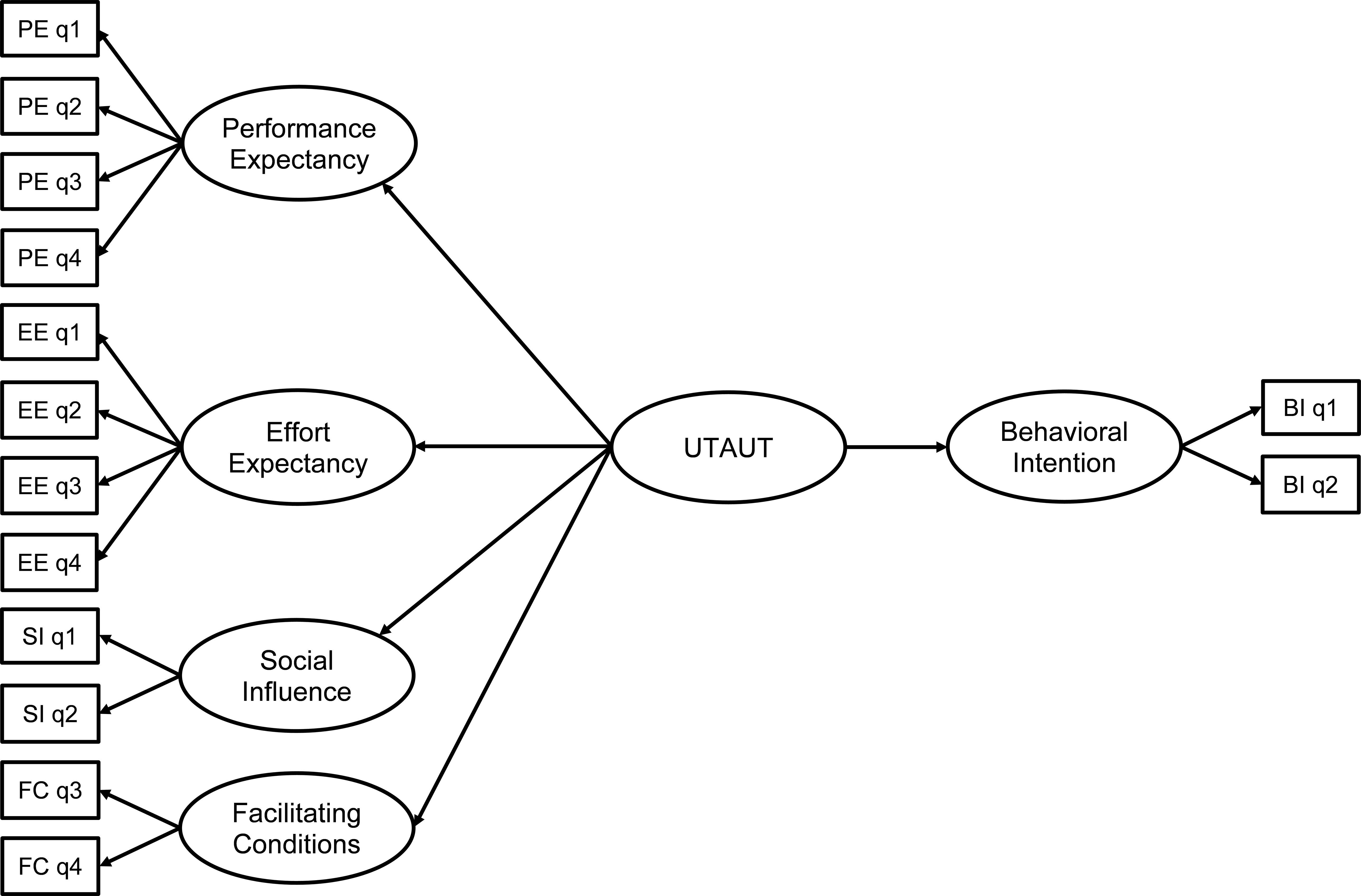
Assessments of technology acceptance and planned behavior provide effective methods for determining current usage and potential adherence (33). For products in any stage of design/development, from ideation to finishing, technology acceptance models may be especially useful for gauging usefulness and desirability, two topics that bridge the engineering, marketing, and design teams during the design process (27). A review of technology acceptance models has shown that a combination of previous methods may provide a more modern approach that is applicable in many fields (34–36); the Unified Theory of Acceptance and Use of Technology (UTAUT) pulls from eight other user acceptance models (35). Venkatesh, et al. (36) simplified the UTAUT model from 32 main effects and four moderators to one with four primary constructs that showed to be direct determinants of intention and usage behavior (35). In this previous study, these four determinants are defined: 1) performance expectancy (PE) as the perceived usefulness of the technology, 2) effort expectancy (EE) as the perceived ease of use of the technology, 3) social influence (SI) as the degree to which clinicians and caregivers support the use of the technology, and 4) facilitating conditions (FC) as the degree to which the user believes they possess the cognitive and physical ability to use the technology (35). These four constructs and the three associated psychosocial moderators of attitude (ATT), anxiety (ANX), and self-efficacy (SE) together have been used to estimate the perceived acceptance of healthcare-related technology along with potential barriers (34, 35, 37).
In this exploratory study, we present the UTAUT model with moderating psychosocial factors applied to intelligent offloading footwear (IOF) that is under development by our team at the University of Geneva, Geneva University Hospitals, and École Polytechnique Fédérale de Lausanne (38). The IOF is designed as an everyday shoe for PLwD and neuropathy who are at risk for developing ulcers; the footwear is designed to sense the location of high plantar pressures and then actively adjust the contour of the insole to reduce these high plantar pressures. The purpose of this exploratory study was to investigate the predictors from the UTAUT model and psychosocial factors analysis of behavioral intention to use the IOF by PLwD, caregivers, and medical professionals.
2 Materials and methods
2.1 Study summary
In this cross-sectional survey design study, a paper-and-pencil or an online questionnaire was given to PLwD (DM), caregivers of PLwD (CG), and medical professionals who care for PLwD (MP). The questionnaire employed general information and footwear preferences along with 26 questions to understand the predictive capability of the UTAUT model and moderating psychosocial factors to predict behavioral intention to use the IOF. The 26 questions relating to the UTAUT model were based on previous work (35, 37) and the other questions were designed for general understanding of design implications. The English language version was written by the first author (SH) – a native English speaker – based on previous work (35, 37). This version was translated into French by a native French speaker who also speaks English fluently and who was familiar with the work, but does not have topic-relevant expertise. The French and English versions were then compared by several other native French speakers who are fluent in English and have topic-relevant expertise (i.e., researchers with experience in movement and perception), in consultation with the first author (SH) until consensus was reached that the two versions were comparable. Furthermore, the French paper version was distributed to the patients prior to the distribution of the online questionnaire; this allowed for the investigating researchers to adjust the questionnaire according to any common questions which arose concerning the language. As there were no concerns for the translation after the paper version, the French version remained the same for the online version.
Hypothesis 1 (H1): The UTAUT model (PE, EE, SI, FC) predicts behavioral intention (BI) by DM to use and MP to prescribe the intelligent footwear when it becomes available.
Hypothesis 2 (H2): Attitude (ATT), anxiety (ANX), and self-efficacy (SE) moderate the impact of UTAUT on the behavioral intention prediction.
2.2 Questionnaire format
2.2.1 Pencil-and-paper version
PLwD in the Geneva University Hospitals (Department of Endocrinology, Diabetes, Nutrition and Therapeutic Patient Education) were recruited for a questionnaire to understand their perceptions of the proposed IOF (39). Questionnaires were conducted from June to August 2022. People with diabetes who had active or past foot ulcers and who were cognitively able to fill out a questionnaire in English or French were included in the study. Reasons for exclusion of data included those who did not complete the questionnaire. Ethical approval was granted by the University Commission for Ethical Research in Geneva for the paper and online versions (CUREG 2022-03-35).
2.2.2 Online version
A questionnaire similar to the paper questionnaire was made available online (LimeSurvey GmbH, Hamburg, Germany) from October 2022-January 2023 to DM, CG, and MP populations. As in the paper questionnaire, versions were made available in English and French.
2.2.3 Questionnaire sections
The paper and online questionnaires consisted of similar questions separated into 5 sections: 1) General description of the footwear, 2) person-specific information, 3) diabetes-specific questions, 4) UTAUT model and psychosocial moderators, 5) footwear design.
Section 1 stated that our team is developing IOF for people with diabetes with the intent to reduce the likelihood of ulcers and amputations. A brief description was given concerning how the footwear would sense the location and magnitude of high pressures under the foot and then actively adjust the insole to redistribute the high pressures to reduce the risk of ulceration. The respondents were then instructed that during the 15-20 minute questionnaire, they should imagine that they or the person for whom they care/oversee would 1) receive the footwear from a medical professional, 2) wear the shoes while walking around each day, 3) remove the shoes and plug them into the charger after each day of wear, and 4) unplug the shoes from the charger and put them on the next day.
Section 2 gathered demographical and other user-specific data (sex, age, country of residence, level of education) while Section 3 asked users to fill out diabetes-specific information (numbers of years since diagnosis, type of diagnosis, presence of a previous foot ulcer, active and shoe-wearing hours per day) for themselves (DM) or for the person for whom they are a caregiver (CG).
Section 4 consisted of questions regarding the UTAUT model and psychosocial factor (PE, EE, SI, FC, ATT, ANX, SE, and BI). These questions were adapted to the role of the person answering the questions. For example, a question such as “I would find the footwear useful for managing my foot health” was tailored such that “my” would be replaced with either “my care recipient’s” (for CG) or “my patient’s” for MP. For each of these questions, users were asked to rate their agreement with the question on a 5-point Likert scale (1=strongly disagree, 2=disagree, 3=neutral, 4=agree, 5=strongly agree; verbal descriptors were present at each number). Questions for ANX have the opposite connotation compared to the other categories; a smaller number denotes less anxiety toward using the footwear. Behavioral intention (BI) was measured by two questions which asked the participants to rate how likely they would be to wear or recommend the shoes when they became available (Table 1).
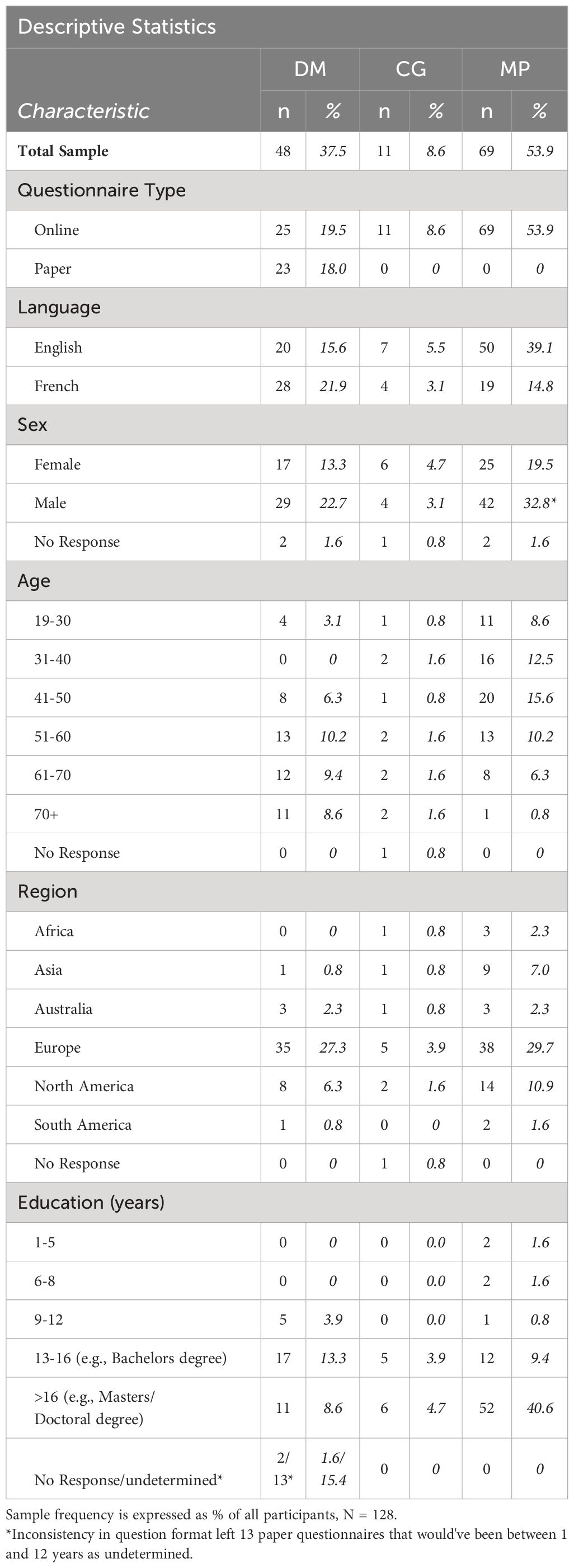
Table 1 Participant characteristics by questionnaire type, language, gender, age, region, and education.
Section 5 consisted of multiple-choice questions concerning why the person with diabetes might not want to use the footwear, what might change their mind in accepting the footwear, and preferences for footwear closure type, cost, and outer design.
2.3 Data analysis
The data were anonymized and statistical analyses were performed by the researchers including descriptive statistics (mean and SD), frequency counts, and percentages of total participants within each role. Further analyses were separated by role due to the nature of the question responses being perception-based. Therefore, for each group, Cronbach’s alpha measure of construct reliability with a threshold set at 0.7 or higher for acceptable reliability (40) was used to measure the reliability of the measures within the UTAUT model and within the general psychosocial factors. Multiple questions in each factor were accounted for by predicting a latent variable for each factor. Structural equation modeling (SEM) was used based on the work of Kohnke, et al. (35) to assess H1 (Figure 1). If the results for the SEM for H1 showed agreement, then linear regression analysis would be used for H2.
Factor loadings (FL) >0.7, Comparative Fit Index (CFI) ≥ 0.95, Root Mean Square Error of Approximation (RMSEA) ≤ 0.06, and the ratio of chi-square to the degrees of freedom (χ2/df) < 2 were used to evaluate the SEM (41–47). IBM SPSS (28.0.1.1 (14)) and AMOS (v29.0.0, SPSS) were used for all tests and Stata/SE 17.0 was used to calculate the predicted latent variables.
3 Results
3.1 Primary results
A total of 23 people (DM) completed the paper questionnaire and 105 people (DM, CG, and MP) completed the online questionnaire in French or English for a total of 128 responses (Table 1). For the paper questionnaire, there were 45 out of the 68 possible patients who did not complete the questionnaire or did not participate due to disinterest, language barriers, cognitive difficulties, or bilateral amputations that rendered footwear not useful. For the online questionnaire, as there was a low number of CG, this population was only included for descriptive statistics as shown in Table 1.
In total, the DM population was generally older than the MP population and there were generally more males than females in the DM and MP groups. The most responses for each population came from Europe and secondly from North America. The majority of respondents in all populations possessed at least a bachelor’s degree.
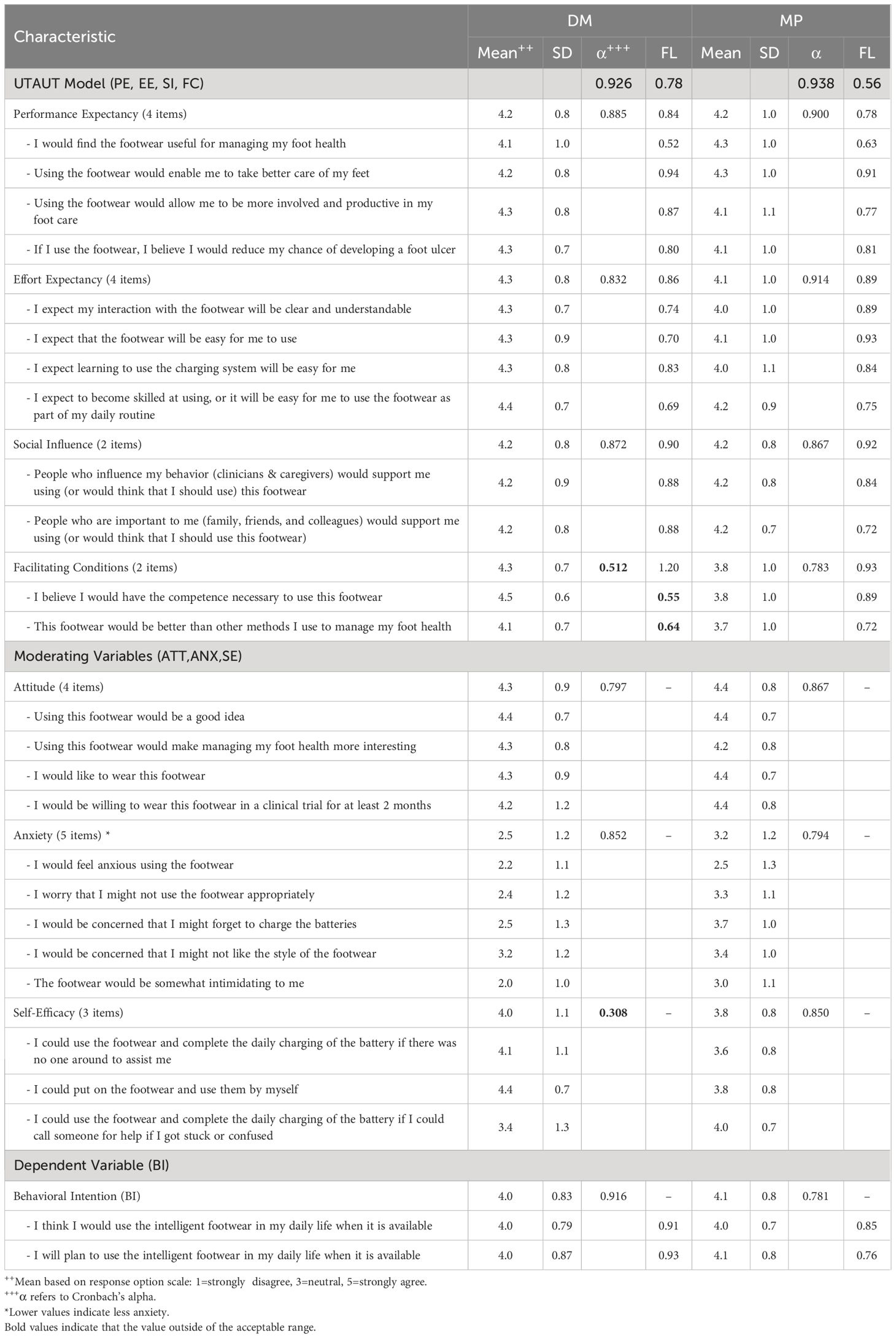
The mean value for all question groups in the UTAUT model was above 4.0 (agree) except for the facilitating conditions for the MP populations (Table 2). Within the UTAUT factors, the scores for the DM group were generally higher than the MP group scores. Within the psychosocial factors, the general attitude was positive (>4.0) and the anxiety level was nearly neutral for DM and MP groups. The self-efficacy scores were less than 4.0 for both groups. Cronbach’s alpha was above the threshold of 0.7 for all categories except for facilitating conditions and self-efficacy in the DM group.
In the SEM model, the factor loadings for the UTAUT model, as a whole, were 0.8 for the DM group and 0.56 for the MP group. The CFI and RMSEA were 0.863 and 0.134 for the DM group and 0.881 and 0.130 for the MP group. The ratio of chi-square to the degrees of freedom (χ2/df) was 1.862 for the DM group and 2.144 for the MP group.
3.2 Exploratory analysis
The results of the parameters as shown in Section 2.3 – Data Analysis showed that the UTAUT may not be an effective model to examine the relationships among the variables. To explore these relationships, the following exploratory analysis was conducted similar to previous work (48–50).
3.2.1 Exploratory methods
Previously established methods of using logistic regression modeling were modeled to explore the relationships between all categories and the behavioral intention to use the footwear (48–50).
Step 1: The predicted latent variable for each UTAUT model factor and psychosocial factor was determined. In each population, a univariate logistic regression model was tested for each factor in relation to the behavioral intention (BI) to use the footwear. BI was converted into a binary factor with the average of the Likert values less than 4 indicated as negative responses to BI and values of 4 and above were indicated as positive responses to BI. A predicted variable could not be created for the FC factor in the MP group due to a lack of responses for the two questions. Therefore, univariate logistic regression was conducted for the remaining predicted factors for a total of 13 models tested (2 populations * 7 factors [4 UTAUT and 3 psychosocial]). Any factor that was not determined to be statistically significant with a Wald test p-value >0.20 was excluded from further analysis. Multicollinearity between the statistically significant factors in each population was tested by performing linear regression analyses including the BI as the dependent variable and the significant factors in each group as the independent factors (in all possible combinations).
Step 2: The factors that proved significant in Step 1 were incorporated into a backward selection multivariate logistic regression to select important factors to keep (p-value < 0.10). A categorical backward selection was not used as there were too few variables to conduct this analysis as in previous work (48, 50).
3.2.2 Exploratory results
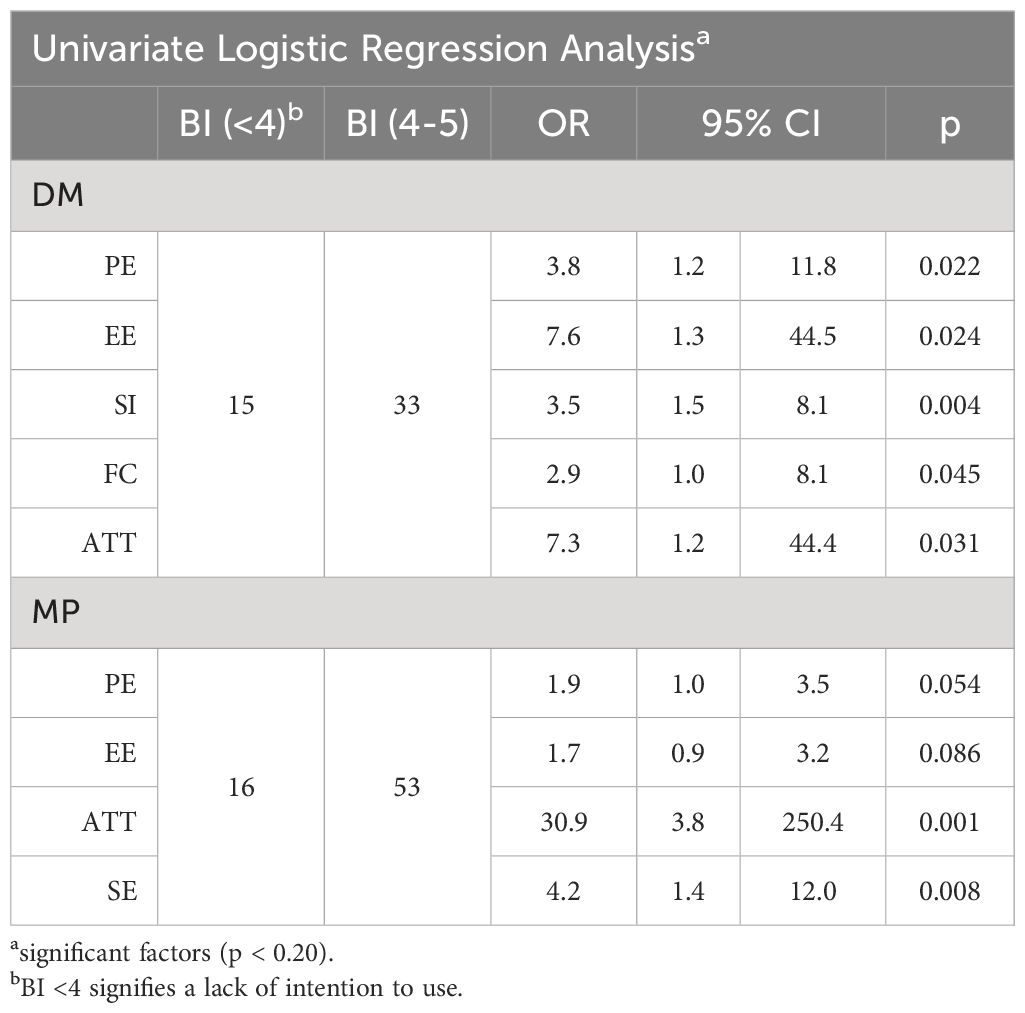
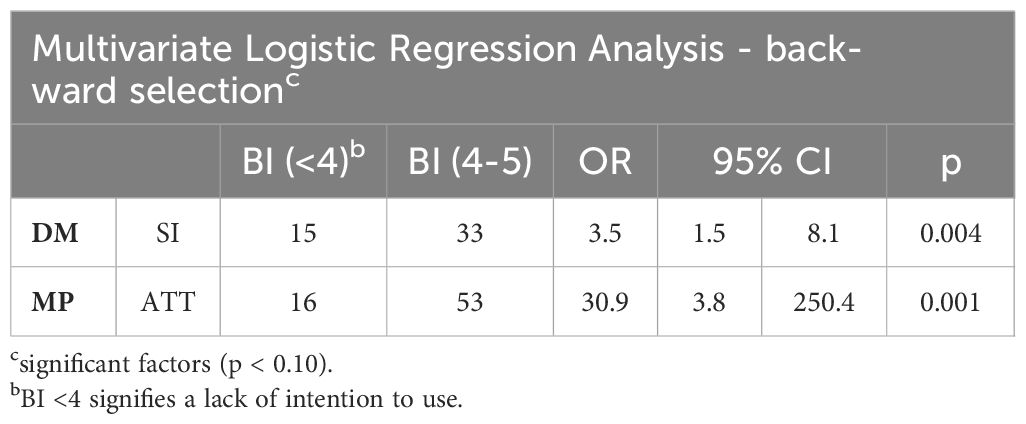
In the DM and MP groups respectively, there were 33/48 and 53/69 responses indicating a positive intention to use the IOF when considering BI as a binary variable (Table 3). Univariate logistic regression analysis showed that for the DM group, PE, EE, SI, FC, and ATT were significant (p<0.20) and that for the MP group, PE, EE, ATT, and SE were significant. Both groups showed no multicollinearity among the significant factors (DM: VIF [1.13-2.57], Tolerance [0.39-0.89], r [.385-.468]; MP: VIF [1.09-2.25], Tolerance [0.45-0.92], r [.265-.496]) (51). Therefore, each of these factors was carried over to the multivariate logistic regression for the respective group (Table 4). Backward selection showed that the multivariate regressions were eventually reduced to having only one factor (univariate regressions) with the significance level set to p < 0.10 (Wald test). SI (OR=3.5, p=0.004) was the only remaining factor in the DM group and ATT (OR=30.9, p=0.001) was the remaining factor in the MP group.
The most predominant concern by all roles for why PLwD may not wear the footwear was described as the cost (Table 5). However, the main reason stated by DMs and MPs as to why a patient may change their mind to accept the footwear was also if the cost of the footwear was covered by insurance. The amount of money that someone would be willing to spend annually on footwear was recorded. For the paper questionnaire, the conversion rate from CHF to USD was based on the start date of the first survey. As there was a maximum of 5% fluctuation in the exchange rate in this period, the risk of error was small. For the online questionnaire, an error prevented the collection of currency type for the responses. Therefore, the currency was defaulted to the country location of the respondent and was limited to the following countries: USA [USD], Canada [CAD], European countries using the Euro [EUR], Switzerland [CHF], United Kingdom [GBP], and Australia [AUS]. Other currencies and amounts were excluded from the analysis. Currency was converted to USD for the online questionnaires according to the conversion rate of the date the questionnaire was received. Across the paper and online questionnaires, the average cost (in USD) that PLwD may be willing to pay annually for the footwear was estimated to be $322 for DMs, $158 for CGs and $448 for MPs.
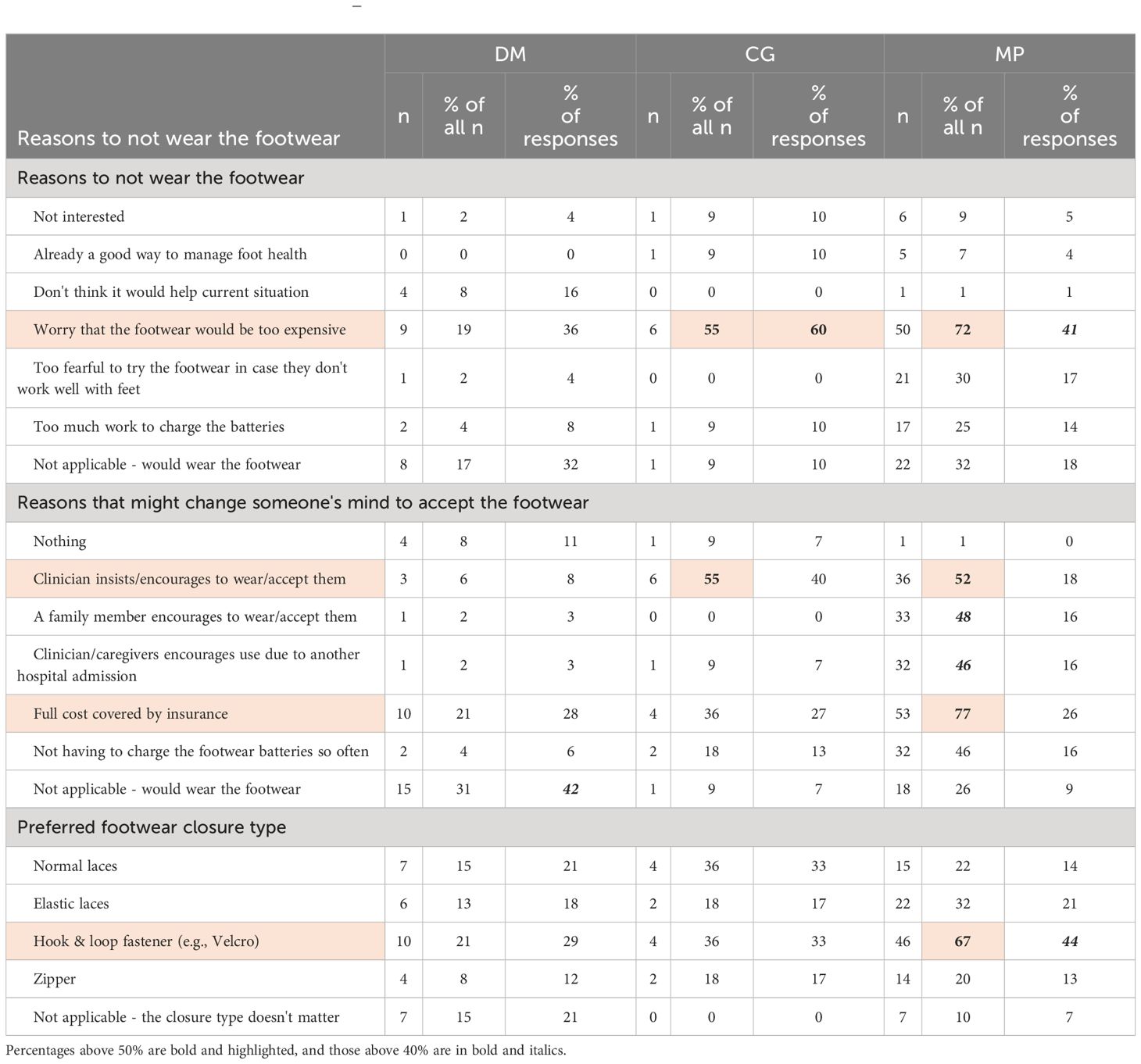
Table 5 Reported multiple choice questions – reasons for potential rejection or acceptance of the footwear and preferred style.
The potential cost of the footwear was the largest perceived prohibitor to acquisition and subsequent use of the shoes. Otherwise, the general, open-ended questions as to why people would not wear the footwear fell into 2 main categories: aesthetics and usability. The main concerns for people with diabetes were the style (aesthetics) and that the footwear would not fit their feet or that the battery in the shoe could be dangerous (usability). For the MPs, the main concerns were centered around being able to effectively encourage use of the footwear and durability (usability), along with the importance of the style for PLwD (aesthetics).
The aesthetic preferences of the participants were varied. In general, the preferred type of closure was stronger for medical professionals as a hook and loop fastener (Velcro®). In the questionnaire, participants were shown two images of potential aesthetic designs: one sport and one formal. The sport design was preferred by most of the DMs (20/24 respondents), while the preferences of the MPs were split between the formal (29/65 respondents) and the sport (36/65 respondents).
4 Discussion
The high potential usage scores based on the UTAUT model suggest that there could be high adoption of the new IOF when it becomes available. Based on established thresholds, the Structural Equation Modeling showed that a UTAUT model may not be the most indicative of behavioral intention for PLwD nor with medical professionals. However, the supplementary, exploratory analysis showed that for PLwD, all the UTAUT model factors (PE, EE, SI, FC) may individually positively influence Behavioral Intention (BI) with Social Influence (of caregivers, medical professionals, and family members) being the most influential factor in predicting BI (based on multivariate backward selection). For the Medical Professional (MP) group, univariate analysis showed the significance of Performance Expectancy and Effort Expectancy, from the UTAUT model, as well as Attitude and Self-Efficacy in predicting BI. In the MP group, the Attitude toward the shoes was the prominent factor for predicting BI in the multivariate analysis. Apart from the UTAUT model, cost/affordability of the footwear was also identified by participants as an important factor that could influence adoption of the footwear.
The results from this study align with previous findings. In the current study, for PLwD, the impact of external opinions and the advice of medical professionals (Social Influence) was shown to be an important factor for wearing this footwear (multivariate backward selection regression). This is consistent with previous work that showed that stigmatization and confirmation from MPs that recommended footwear is helpful and important for adherence (26, 29). Furthermore, for MPs in the current study, the Attitude toward the footwear proved to be the most influential factor for them recommending the footwear to their PLwD. This result is consistent with previous results that showed that there must be buy-in and a positive attitude of a device from an MP before recommending the device to a patient (52–55). The cost was shown to be an influential part of the potential wear of the shoes which is consistent with previous work indicating that this topic is important for understanding potential adherence (56).
Certain limitations to this research should be stated as well. Our intelligent footwear was presented as a concept and as such was only described and not shown in physical form to the participants. This may have limited responses, though it may have also avoided certain biases. For those who were invited to complete the questionnaire online, there was no option for completing a paper copy of the questionnaire. As such, some potential participants who did not have internet access or were uncomfortable using technology may not have participated. This could be an important missing group, given that the shoes being developed are “high tech”. Therefore, the study pool may have been limited for this reason and because of the missed patients in the paper questionnaire study. The study population does not represent global opinions, because most of the participants were located in Europe or North America. A larger sample size could also aid in the use of the UTAUT which was limited due to the number of participants. Furthermore, in this study, Cronbach’s alpha assumptions were not met for the FC and SE questions in the DM group which was primarily due to the small number of questions. Therefore, this set of questions may not be the most influential for future design considerations. Due to limited resources, forward translation followed by a sort of expert committee and pilot testing were conducted as mentioned in the methods for the translation from English to French. With a larger target audience and more available resources, a rigid structure for the translation validation could be performed in the future (57).
Future designs of the questionnaire may incorporate more comprehensive imagery or use description of the footwear to provide respondents with a more realistic understanding of the footwear and in turn that will allow respondents to provide a more accurate perception of the footwear. Implementation of the footwear should include a focus on ensuring that there is a positive attitude instilled in potential end-users (persons with diabetes) and those who care for them (Medical Professionals), to affect the overall attitude toward the footwear and the social influence parameter. Furthermore, attention to shoe affordability will address an important potential barrier for many prospective end users.
Overall, this study showed that the UTAUT model, as a whole, and three previously identified psychosocial factors did not necessarily predict stakeholder behavioral intention, but rather specific factors in the model predicted the intention to use or recommend the footwear for people with diabetes and medical professionals, respectively. In attracting future patients with diabetes and their medical professionals to use new footwear, this work suggests that information given should focus on targeting a positive social influence and attitude toward the footwear. The work is useful not only for the design of the presented IOF, but also for future intelligent footwear that may emerge with advances in technology.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by University Commission for Ethical Research in Geneva. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
SH: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Visualization, Writing – original draft, Writing – review & editing. CS: Conceptualization, Formal analysis, Methodology, Validation, Visualization, Writing – review & editing. JC: Investigation, Writing – review & editing. ZP: Conceptualization, Funding acquisition, Methodology, Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was funded by the Swiss National Science Foundation (BRIDGE Discovery Grant #40B2-0_181020).
Acknowledgments
The authors would like to acknowledge Nuria Flores Vuffray for assistance in questionnaire translation, the diabetic podiatric team at the HUG for administration of the paper questionnaire, and Antoine Poncet and Dr. Cyril Jaksic for their statistical support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
2. Armstrong DG, Boulton AJM, Bus SA. Diabetic foot ulcers and their recurrence. New Engl J Med. (2017) 376:2367–75. doi: 10.1056/NEJMra1615439
3. Reiber GE, Boyko EJ, Smith DG. Lower extremity foot ulcers and amputations in diabetes. Diabetes America. (1995) 2:409-27.
4. Palumbo P, Melton L. Peripheral vascular disease and diabetes (1985). In: Diabetes in America (1984). p. 1. Data compiled.
5. Pecoraro RE, Reiber GE, Burgess EM. Pathways to diabetic limb amputation: basis for prevention. Diabetes Care. (1990) 13:513–21. doi: 10.2337/diacare.13.5.513
6. Lo ZJ, Surendra NK, Saxena A, Car J. Clinical and economic burden of diabetic foot ulcers: A 5-year longitudinal multi-ethnic cohort study from the tropics. Int Wound J. (2021) 18:375–86. doi: 10.1111/iwj.13540
7. Pedras S, Preto I, Carvalho R, Graça Pereira M. Traumatic stress symptoms following a lower limb amputation in diabetic patients: a longitudinal study. Psychol Health. (2019) 34:535–49. doi: 10.1080/08870446.2018.1545907
8. Gurney JK, Stanley J, Rumball-Smith J, York S, Sarfati D. Postoperative death after lower-limb amputation in a national prevalent cohort of patients with diabetes. Diabetes Care. (2018) 41:1204–11. doi: 10.2337/dc17-2557
9. Armstrong DG, Lipsky BA. Diabetic foot infections: stepwise medical and surgica management. Int Wound J. (2004) 1:123–32. doi: 10.1111/j.1742-4801.2004.00035.x
10. Biz C, Belluzzi E, Crimì A, Bragazzi NL, Nicoletti P, Mori F, et al. Minimally invasive metatarsal osteotomies (MIMOs) for the treatment of plantar diabetic forefoot ulcers (PDFUs): A systematic review and meta-analysis with meta-regressions. Appl Sci. (2021) 11:9628. doi: 10.3390/app11209628
11. Biz C, Ruggieri P. Minimally invasive surgery: osteotomies for diabetic foot disease. Foot Ankle Clinics. (2020) 25:441–60. doi: 10.1016/j.fcl.2020.05.006
12. Crews RT, King AL, Yalla SV, Rosenblatt NJ. Recent advances and future opportunities to address challenges in offloading diabetic feet: A mini-review. Gerontology. (2018) 64:309–17. doi: 10.1159/000486392
13. Kanade RV, Van Deursen RWM, Harding K, Price P. Walking performance in people with diabetic neuropathy: benefits and threats. Diabetologia. (2006) 49:1747–54. doi: 10.1007/s00125-006-0309-1
14. Wu SC, Jensen JL, Weber AK, Robinson DE, Armstrong DG. Use of pressure offloading devices in diabetic foot ulcers. Diabetes Care. (2008) 31:2118–9. doi: 10.2337/dc08-0771
15. Armstrong DG, Nguyen HC, Lavery LA, Van Schie CHM, Boulton AJM, Harkless LB. Off-loading the diabetic foot wound. Diabetes Care. (2001) 24:1019–22. doi: 10.2337/diacare.24.6.1019
16. Khunkaew S, Fernandez R, Sim J. Health-related quality of life among adults living with diabetic foot ulcers: a meta-analysis. Qual Life Res. (2019) 28:1413–27. doi: 10.1007/s11136-018-2082-2
17. Health Quality Ontario. Fibreglass total contact casting, removable cast walkers, and irremovable cast walkers to treat diabetic neuropathic foot ulcers: a health technology assessment. Vol. 17. Ontario, Canada: Ontario health technology assessment series (2017). p. 1.
18. Piaggesi A, Goretti C, Iacopi E, Clerici G, Romagnoli F, Toscanella F, et al. Comparison of removable and irremovable walking boot to total contact casting in offloading the neuropathic diabetic foot ulceration. Foot Ankle Int. (2016) 37:855–61. doi: 10.1177/1071100716643429
19. Jorgetto JV, Gamba MA, Kusahara DM. Evaluation of the use of therapeutic footwear in people with diabetes mellitus – a scoping review. J Diabetes Metab Disord. (2019) 18:613–24. doi: 10.1007/s40200-019-00428-9
20. Crews RT, Shen B-J, Campbell L, Lamont PJ, Boulton AJM, Peyrot M, et al. Role and determinants of adherence to off-loading in diabetic foot ulcer healing: A prospective investigation. Diabetes Care. (2016) 39:1371–7. doi: 10.2337/dc15-2373
21. Arts ML, de Haart M, Bus SA, Bakker JP, Hacking HG, Nollet F. Perceived usability and use of custom-made footwear in diabetic patients at high risk for foot ulceration. J Rehabil Med. (2014) 46:357–62. doi: 10.2340/16501977-1272
22. Knowles E, Boulton A. Do people with diabetes wear their prescribed footwear? Diabetic Med. (1996) 13:1064–8.
23. Racaru S, Bolton Saghdaoui L, Roy Choudhury J, Wells M, Davies AH. Offloading treatment in people with diabetic foot disease: A systematic scoping review on adherence to foot offloading. Diabetes Metab Syndrome: Clin Res Rev. (2022) 16:102493. doi: 10.1016/j.dsx.2022.102493
24. Keukenkamp R, Van Netten JJ, Busch-Westbroek TE, Nollet F, Bus SA. Users’ needs and expectations and the design of a new custom-made indoor footwear solution for people with diabetes at risk of foot ulceration. Disability Rehabil. (2021) 44:8493–500. doi: 10.1080/09638288.2021.2003878
25. Williams A, Nester C. Patient perceptions of stock footwear design features. Prosthetics orthotics Int. (2006) 30:61–71. doi: 10.1080/03093640600574425
26. Van Netten JJ, Dijkstra PU, Geertzen JHB, Postema K. What influences a patient’s decision to use custom-made orthopaedic shoes? BMC Musculoskeletal Disord. (2012) 13:92. doi: 10.1186/1471-2474-13-92
27. Sanders EBN. Converging perspectives: product development research for the 1990s. Design Manage J (Former Series). (1992) 3:49–54. doi: 10.1111/j.1948-7169.1992.tb00604.x
28. Desmet P, Fokkinga S. Beyond Maslow’s pyramid: Introducing a typology of thirteen fundamental needs for human-centered design. Multimodal Technol Interact. (2020) 4:38. doi: 10.3390/mti4030038
29. Jarl G, Tranberg R, Johansson U, Alnemo J, Lundqvist L-O. Predictors of adherence to wearing therapeutic footwear among people with diabetes. J Foot Ankle Res. (2020) 13. doi: 10.1186/s13047-020-00413-z
30. Correia JC, Waqas A, Huat TS, Gariani K, Jornayvaz FR, Golay A, et al. Effectiveness of therapeutic patient education interventions in obesity and diabetes: A systematic review and meta-analysis of randomized controlled trials. Nutrients. (2022) 14:3807. doi: 10.3390/nu14183807
31. Dorresteijn JA, Kriegsman DM, Assendelft WJ, Valk GD. Patient education for preventing diabetic foot ulceration. Cochrane Database Syst Rev. (2014). doi: 10.1002/14651858
32. Jones PJ, Bibb RJ, Davies MJ, Khunti K, McCarthy M, Fong DTP, et al. A fitting problem: Standardising shoe fit standards to reduce related diabetic foot ulcers. Diabetes Res Clin Pract. (2019) 154:66–74. doi: 10.1016/j.diabres.2019.05.017
33. Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. (1989) p:319–40. doi: 10.2307/249008
34. Macdonald EM, Perrin BM, Hyett N, Kingsley MIC. Factors influencing behavioural intention to use a smart shoe insole in regionally based adults with diabetes: a mixed methods study. J Foot Ankle Res. (2019) 12. doi: 10.1186/s13047-019-0340-3
35. Kohnke A, Cole ML, Bush R. Incorporating UTAUT predictors for understanding home care patients’ and clinician’s acceptance of healthcare telemedicine equipment. J Technol Manage Innovation. (2014) 9:29–41. doi: 10.4067/S0718-27242014000200003
36. Venkatesh V, Morris MG, Davis GB. User Acceptance of Information Technology: Toward a Unified View. Vol. 27. Management Information Systems Research Center, University of Minnesota (2003). p. 425.
37. Macdonald EM, Perrin BM, Kingsley MIC. Factors influencing Australian podiatrists’ behavioural intentions to adopt a smart insole into clinical practice: a mixed methods study. J Foot Ankle Res. (2020) 12. doi: 10.1186/s13047-020-00396-x
38. Hemler SL, Ntella SL, Jeanmonod K, Köchli C, Tiwari B, Civet Y, et al. Intelligent plantar pressure offloading for the prevention of diabetic foot ulcers and amputations. Front Endocrinol. (2023) 14:1166513. doi: 10.3389/fendo.2023.1166513
39. Hemler SL, Sommerich CM, Pataky Z. User Perceptions of Intelligent Footwear for Preventing Amputations in People with Diabetes. In: International Symposium on Human Factors and Ergonomics in Health Care. Orlando, FL, USA (2023).
41. Bentler PM. On tests and indices for evaluating structural models. Pers Individ Dif. (2007) 42:825–9. doi: 10.1016/j.paid.2006.09.024
42. Schumacker RE, Lomax RG. A beginner’s guide to structural equation modeling. New York: psychology press (2004). doi: 10.4324/9781410610904
43. Hu L-t, Bentler PM. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychol Methods. (1998) 3:424. doi: 10.1037/1082-989X.3.4.424
44. Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equation Modeling: A Multidiscip J. (1999) 6:1–55. doi: 10.1080/10705519909540118
45. Alavi M, Visentin DC, Thapa DK, Hunt GE, Watson R, Cleary M, et al. Chi-square for model fit in confirmatory factor analysis. J Advanced Nurs. (2020) 76:2209–11. doi: 10.1111/jan.14399
46. Cole DA. Utility of confirmatory factor analysis in test validation research. J consulting Clin Psychol. (1987) 55:584. doi: 10.1037/0022-006X.55.4.584
47. Wheaton B, Muthen B, Alwin DF, Summers GF. Assessing reliability and stability in panel models. Sociological Method. (1977) 8:84–136. doi: 10.2307/270754
48. Roquelaure Y, Ha C, Rouillon C, Fouquet N, Leclerc A, Descatha A, et al. Risk factors for upper-extremity musculoskeletal disorders in the working population. Arthritis Care Res. (2009) 61:1425–34. doi: 10.1002/art.24740
49. Li J, Sommerich CM, Chipps E, Lavender SA, Stasny EA. A framework for studying risk factors for lower extremity musculoskeletal discomfort in nurses. Ergonomics. (2020) 63:1535–50. doi: 10.1080/00140139.2020.1807615
50. Evans KD, Sommerich CM, Stigall-Weikle AN, Stokes AD, Klatt MD. Work-related musculoskeletal disorders among radiographers: an exploration of self-reported symptoms. Radiologic Technol. (2021) 93:161–76.
51. Kim JH. Multicollinearity and misleading statistical results. Korean J Anesthesiol. (2019) 72:558. doi: 10.4097/kja.19087
52. Hu X, Fang H, Wang P. Factors affecting doctor’s recommendation for mobile health services. Digital Health. (2022) 8:20552076221125976. doi: 10.1177/20552076221125976
53. Zhou C, Chen J, Tan F, Lai S, Li X, Pu K, et al. Relationship between self-care compliance, trust, and satisfaction among hypertensive patients in China. Front Public Health. (2023) 10. doi: 10.3389/fpubh.2022.1085047
54. Kerse N. Physician-patient relationship and medication compliance: A primary care investigation. Ann Family Med. (2004) 2:455–61. doi: 10.1370/afm.139
55. Deniz S, Akbolat M, Çimen M, Ünal Ö. The mediating role of shared decision-making in the effect of the patient–physician relationship on compliance with treatment. J Patient Exp. (2021) 8:237437352110180. doi: 10.1177/23743735211018066
56. Jarl G, Lundqvist L-O. Adherence to wearing therapeutic shoes among people with diabetes: a systematic review and reflections. Patient Prefer Adherence (2016) 10:1521–8. doi: 10.2147/PPA
Keywords: adherence, diabetic foot, foot pressure, footwear, off-loading
Citation: Hemler SL, Sommerich CM, Correia JC and Pataky Z (2024) User perceptions of intelligent offloading diabetic footwear. Front. Endocrinol. 15:1380525. doi: 10.3389/fendo.2024.1380525
Received: 01 February 2024; Accepted: 15 July 2024;
Published: 07 August 2024.
Edited by:
Christina Parker, Queensland University of Technology, AustraliaCopyright © 2024 Hemler, Sommerich, Correia and Pataky. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sarah L. Hemler, c2FyYWguaGVtbGVyQHVuaWdlLmNo
 Sarah L. Hemler
Sarah L. Hemler Carolyn M. Sommerich3
Carolyn M. Sommerich3