
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Endocrinol., 15 May 2024
Sec. Cardiovascular Endocrinology
Volume 15 - 2024 | https://doi.org/10.3389/fendo.2024.1361447
 Ping-Ping Zhang1†
Ping-Ping Zhang1† You-Xin Wang2†
You-Xin Wang2† Jia-Yin Gu3
Jia-Yin Gu3 Miao Xu3
Miao Xu3 Ye Zhou3
Ye Zhou3 Hai-Jun Wang2
Hai-Jun Wang2 Patrick W C. Lau4,5
Patrick W C. Lau4,5 Hui Wang2*
Hui Wang2* Li Li3*
Li Li3*Background: Childhood obesity tends to persist into adulthood, predisposing individuals to cardiometabolic risk (CMR). This study aims to investigate the mediating role of cardiorespiratory fitness (CRF) in the associations between multiple fatness indicators and individual CMR markers and clustered CMR-score, and explore sex differences.
Methods: We recruited 1,557 children (age: 8 to 10, male/female: 52.7%/47.3%) in September 2022 in Ningbo, China. Physical examinations, overnight fasting blood test, and CRF was evaluated. The CMR-score was calculated by summing age- and sex-specific z scores of four CMR markers, including mean arterial blood pressure, triglycerides, the total cholesterol to high-density lipoprotein cholesterol ratio, and homeostatic model assessment for insulin resistance. Generalized linear mixed models were used to identify the associations, mediation analyses were performed to dissect the function of CRF.
Results: Partial correlation analyses revealed positive associations between high fatness indicators (including body mass index [BMI], BMI z score, body fat mass index [BFMI] and waist-to-height ratio [WHtR]) and increased CMR markers, whereas high CRF was associated with decreased CMR markers (all P < 0.05). In the mediation analyses, CRF emerged as a partial mediator, attenuating the relationship between four fatness indicators and CMR-score. Specifically, CRF mediated 6.5%, 7.7%, 5.3%, and 12.5% of the association between BMI, BMI z score, BFMI, WHtR and CMR-score (all P < 0.001). And the mediating effects of CRF between WHtR and four individual CMR markers was particularly robust, ranging from 10.4% to 21.1% (all P < 0.05). What’s more, CRF mediates the associations between WHtR and CMR-score more pronounced in girls than boys with a mediation effect size of 17.3% (P < 0.001).
Conclusion: In Chinese children, CRF partially mitigates the adverse effects of fatness on CMR, underscoring the significance of enhancing CRF in children.
The rising prevalence of obesity has emerged as a pressing public health concern (1, 2). Obesity that manifests in childhood tends to endure into adulthood, predisposing individuals to cardiovascular and metabolic risks (3), such as dyslipidemia, elevated glucose levels, and high blood pressure. Collectively, these factors contribute to over 30.0% of global mortality (4). Emerging evidence indicates that clusters of cardiometabolic risk (CMR) factors associated with obesity commence early in life, persisting from childhood into adulthood and potentially forecasting future occurrences of diabetes and CMR (5, 6). Investigating the factors associated with CMR during childhood is crucial for implementing proactive management and early-stage interventions.
Cardiorespiratory fitness (CRF), also known as cardiovascular fitness or aerobic fitness, is characterized by the maximum capacity of the cardiovascular and respiratory systems to deliver oxygen to the skeletal muscles during physical activity. As the importance of CRF is now well-established, it was identified as a fundamental indicator in the assessment of health in youth (7). It is widely accepted that higher CRF is beneficial for the prevention of cardiovascular and metabolic diseases in both children and adults (8, 9). Evidence in children demonstrated that even after adjusting for the impact of obesity, the protection effect of CRF on CMR persists (10).
To date, several studies conducted on children and adolescent have consistently demonstrated that fitness, in particularly CRF, is associated with lower CMR, even after accounting for the negative effects of excess body fat (11–15). Notably, boys generally have higher CRF than girls across all age groups (16), and ethnic disparities in CRF have also been highlighted (17). However, to our knowledge, few studies have delved into the sexual dimorphism in this context, and the majority of them have been conducted in Western countries, thus limiting their generalizability. While one study among Chinese children by Shang et.al (13) evaluated CRF through the 50m × 8 shuttle run test and explored its mediation effect, its comparability with other studies remains questionable, and the validity and reliability of this test have not gained widespread acceptance (7). In our study, the 20-m shuttle run test (20mSRT) will be employed, which is more widely used. Furthermore, there remains a gap in understanding the impact of various fatness exposures, how individual markers contribute to CMR as well as the clustered CMR-score, and it is imperative to explore these factors, particularly with regards to sexual differences.
Therefore, this study aims to explore the mediating role of CRF in the association between four fatness indicators and CMR-score with individual CMR markers in Chinese children, and explore sex differences.
The current study conducted a cross-sectional analysis using baseline data from the “Optimizing Intervention Effects in Children and Adolescents in Ningbo” program. This program is a cluster randomized controlled trial designed to evaluate the effect of a comprehensive intervention on weight management in third-grade primary students (Registration No. at clinicaltrials.gov: NCT05482165). Participants were recruited from six primary schools in the Haishu, Yinzhou, and Zhenhai districts of Ningbo city. The baseline assessment was conducted prior to the allocation of schools to either the treatment or control group and included data from physical examinations and CRF tests. Children aged between 8 and 10 years were recruited in September 2022. All third-grade students were recruited to participant this lifestyle intervention program. However, participants meeting the following criteria were excluded: those with a medical history of heart disease, hypertension, diabetes, asthma, viral hepatitis, or nephritis; individuals with obesity caused by endocrine diseases or drugs; those with abnormal physical development or physical deformity; students unable to participate in school sport activities; and individuals who experienced weight loss due to vomiting or taking drugs during the past 3 months (18).
The flowchart illustrating the selection of the study population in the current study is depicted in Figure 1. The program received approval from the Ethics Committee of the First Affiliated Hospital of Ningbo University (Approval No. 2021-R168). Written informed consent was obtained from all participating students and their primary guardians.
Anthropometric measurements were conducted by trained staff from community healthcare centers following standard protocols at the participants’ schools. Diastolic blood pressure (DBP) and systolic blood pressure (SBP) were measured using an Omron digital sphygmomanometer (Omron HEM-7121, Kyoto, Japan) after the participants had rested for at least 5 minutes. Height was measured using a mechanical height meter with participants wearing no shoes. Waist circumference (WC) was measured as the circumference of the horizontal plane midway between the lowest rib and the iliac crest using a tape measure at the end of a normal expiration. Height and WC were all measured to the nearest 0.1cm. Weight and body fat mass were measured utilizing a bioimpedance analyzer (Inbody770, California, USA) with validity and reliability was demonstrated before (19, 20). The participants complied with the system commands by wearing only a single-layered shirt and shorts, standing barefooted on the electrode plates of the analyzer. They maintained a natural posture with both arms hanging down, holding the electrodes and placing their thumbs on them. Then the body composition test started and finished in 2 - 3 minutes.
Mean arterial blood pressure (MAP) was calculated as DBP + 1/3(SBP-DBP). The waist-to-height ratio (WHtR) was calculated as WC (cm) divided by height (cm). Body mass index (BMI) was calculated as weight (kg) divided by height (m) squared, and we calculated the age- and gender-specific BMI z score based on the WHO Child Growth Standards (21). Body fat mass index (BFMI) was calculated as body fat mass (kg) divided by height (m) squared. We selected BMI, BMI z score, BFMI and WHtR as the main fatness indicators in this study. BMI takes into account the relationship between height and weight, while BFMI considers body fat percentage, providing a more accurate reflection of obesity compared with BMI (22). We also used the z-score of BMI to eliminate the impact of age and gender, making BMI from different ages and genders comparable. WHtR is a good indicator of abdominal obesity and is closely related to cardiovascular disease risk (23). These indicators are complementary in assessing the impact of obesity on cardiovascular and metabolic risk.
Elbow vein blood samples (5mL) were obtained by trained nurses following a standard process during the morning of the physical examination at school. All blood parameters were collected after 10-14h of overnight fasting, and the collected blood was refrigerated at 4°C and transferred to examination on the same day. The blood was clotted for 20 - 30 min and centrifuged for10 - 15 min at 3,200 rpm, then the tests for different items were conducted with the remaining blood samples were divided and stored in -80°C refrigerator for further testing. Fasting insulin (FINS) levels were measured using a chemiluminescent method with an autoanalyzer (Roche Cobas E602 Immunology Analyzer, Basel, Switzerland). Fasting plasma glucose (FPG), triglycerides (TG), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), and total cholesterol (TC) were measured using an enzymatic method with another autoanalyzer (Beckman AU5800, California, USA). Homeostatic model assessment for insulin resistance (HOMA-IR) was calculated as [FINS (μU/L) * FPG (mg/dL)]/405. Additionally, the ratio of TC/HDL-C was calculated.
Different methods were employed to calculate continuous CMR-score, and nearly all computed scores incorporated some measure of adiposity, lipids, metabolism, and/or blood pressure (24). In the current study, CMR-score were calculated by summing age- and sex-specific z scores of four individual markers contribute to CMR, including MAP, TG, TC/HDL-C ratio, and HOMA-IR (24). Adiposity-related indicators such as WC or BMI were not included in this score, due to the high correlation between WC and BMI in the mediation analysis for fatness indicators and CRF with CMR-score. The z scores for each index mentioned above were calculated as (value-mean)/SD separately for boys and girls and for each 1-year age group. Higher values of CMR-score indicated a greater cardiovascular and metabolic risk.
CRF was assessed using the 20mSRT, organized by trained professional project staff. This test has been widely used for assessing CRF in children and youth (25). In the 20mSRT, children ran between two lines 20 m apart, keeping pace with audio signals. The test comprises several stages (also called levels), each lasting approximately 1 minute, with each stage consisting of a number of 20-m laps (also called shuttles), and the laps was used to estimate CRF for each child. The speed started at 8.5 km/h and increased by 0.5 km/h every minute (1 min equals 1 stage) (26). The test ended either when a child failed to reach the end line concurrently with the audio signals on two consecutive occasions or when a child stopped due to fatigue. The overall number of laps completed was recorded.
Descriptive analyses were conducted for the characteristics of the participants and presented as means (SD). Student’s t test was employed to compare the differences between sexes concerning anthropometric measures, CRF, and cardiometabolic markers. Partial correlation coefficients (r), adjusted for age, sex, and school, were used as a pre-analysis to examine the associations between four fatness indicators (BMI, BMI z score, BFMI, and WHtR), CRF, and CMR markers.
To determine the associations between four fatness indicators, CRF, and CMR -score/-markers, a generalized linear mixed (GLM) model was utilized. This model included school-level random intercepts to account for the correlation due to the clustering of children within schools, as the survey was conducted in units of schools. All GLM models were adjusted for age and sex. The mediation model pattern is presented in Figure 2. The total effect (TE) of fatness indicators on CMR-score is represented by a black line, and the equation can be expressed as follows: equation (1) CMR-score ~ c × Fatness + covariables. The direct effect (DE) of fatness indicators on CMR-score is represented by the red line. The indirect effect (IE) of fatness indicators on CRF and CMR-score is represented by the blue line. The mediation equation included two parts: equation (2) CRF ~ a × Fatness + covariables and equation (3) CMR-score ~ c’ × Fatness + b × CRF. According to the theory of Baron et al. (27), a significant “indirect role” (mediation) was established when coefficients a, b, and c were significant, and then the mediation effects could be expressed as IE = a×b. The bootstrapping method (5000 samples) was used to examine whether the association between fatness indicators and CMR-score was mediated by CRF (28). The mediation package in R was used to estimate the DE, IE, and TE. The proportion of mediation was calculated as the ratio of IE to TE. A P-value < 0.05 for the two-sided test was considered statistically significant. All statistical analyses were performed using R 4.3.0 (R Core Team).
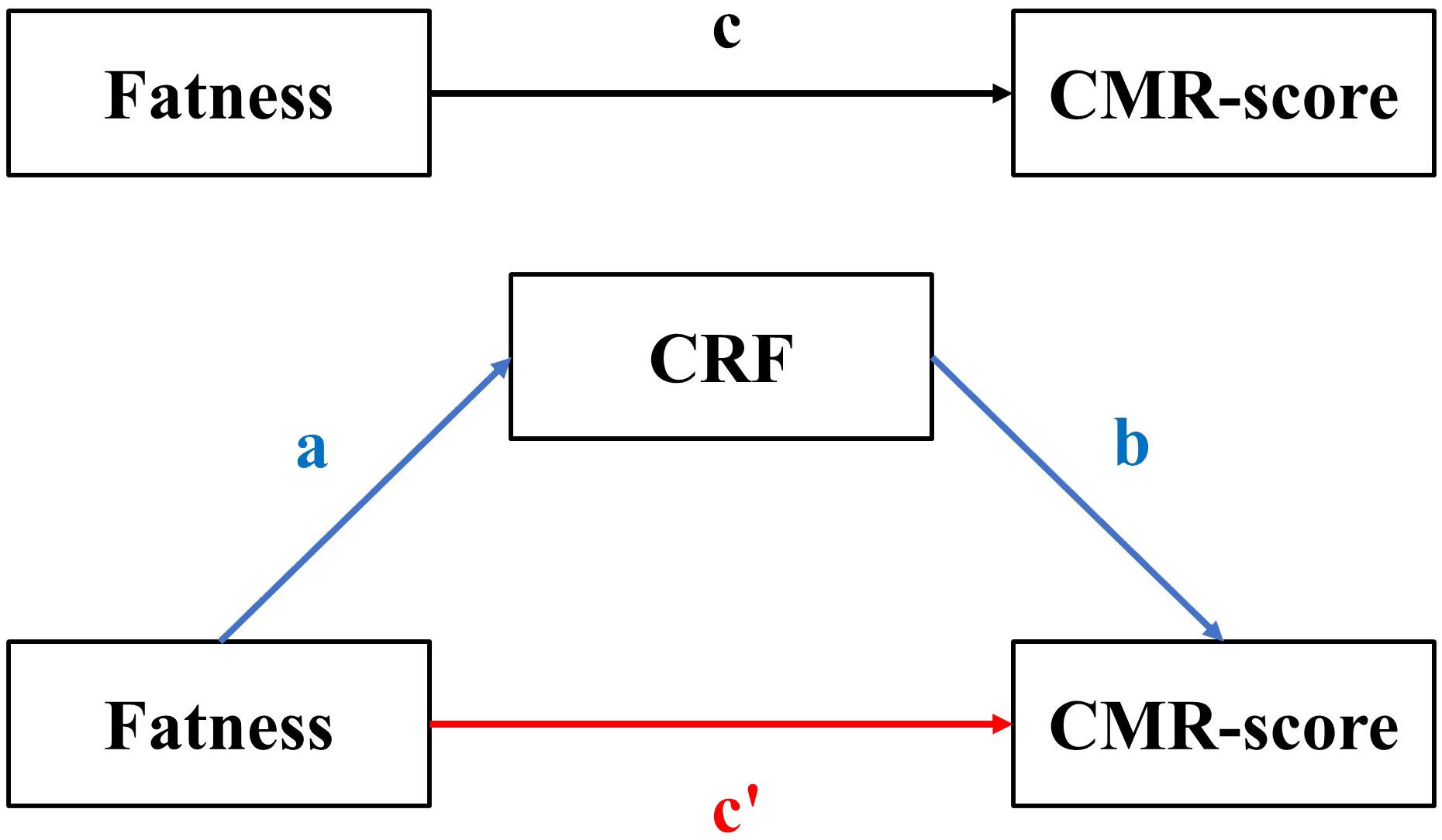
Figure 2 The mediation model pattern. The meaning of the lowecase letters were: c means the total effect, c’ means the direct effect, ab means the indirect effect.
We compared the characteristics of the 1,557 children included and 83 children excluded (Supplementary Table S1 in Supplementary Material), and the excluded participants only reported to have a higher FPG compared to the included (P < 0.05). Table 1 presents the basic characteristics of the participants. The children included in this study has an average age of 8.5 ± 0.3 years, 820 (52.7%) were boys. Notably, boys exhibited higher values in height, weight, WC, WHtR, BMI, body fat mass, BFMI, SBP, CRF, HDL-C, and FPG compared to girls (all P < 0.05). Conversely, girls demonstrated higher levels of TG and LDL-C (all P < 0.05). No significant differences in CMR-score were observed among genders (P = 0.789).
In the partial correlation analyses presented in Table 2, CRF was negatively associated with four fatness indicators (BMI, BMI z score, WHtR, BFMI) or individual CMR markers (MAP, TC/HDL-C, TG, HOMA-IR) after adjusting for age, sex, and school (all P < 0.05). Meanwhile, positive correlations were observed between multiple fatness indicators and CMR markers (all P < 0.05). The pre-analysis results of partial correlation coefficients fulfilled the prerequisites for mediating effect analyses. And the results of the between sexes analyses (Supplementary Tables S2, S3) were similar to the analyses of the entire population, the partial correlation of CRF and fatness indicator or CMR markers were significant (all P < 0.05) except for the association of MAP and CRF in boys.
In general, all four fatness indicators were positively associated with CMR-score in our population, and the mediation analyses showed that CRF attenuated the association between fatness indicators and CMR-score (Figure 3). Of the four fatness indicators, CRF mediated 6.5% (95% CI: 3.3% to 9.6%, P < 0.001, Figure 3A), 7.7% (95% CI: 4.5% to 10.9%, P < 0.001, Figure 3B), 5.3% (95% CI: 1.5% to 9.0%, P = 0.007, Figure 3C) of the association between BMI, BMI z score, BFMI and CMR-score, and we found the largest mediating proportion of the association between WHtR and CMR-score (mediation effect: 12.5%, 95% CI: 8.4% to 16.6%, P < 0.001, Figure 3D). Table 3 presents the mediation effect stratified by sex. The mediation effect for CRF between BFMI and CMR-score was only significant in girls with a proportion of 5.8% (95% CI: 0.9% to 10.6%, P = 0.021). Meanwhile, the proportion of mediation for CRF between WHtR and CMR-score was 9.5% (95% CI: 4.8% to 14.2%, P < 0.001) in boys and more pronounced in girls, with a proportion of 17.3% (95% CI: 9.6% to 25.0%, P < 0.001).
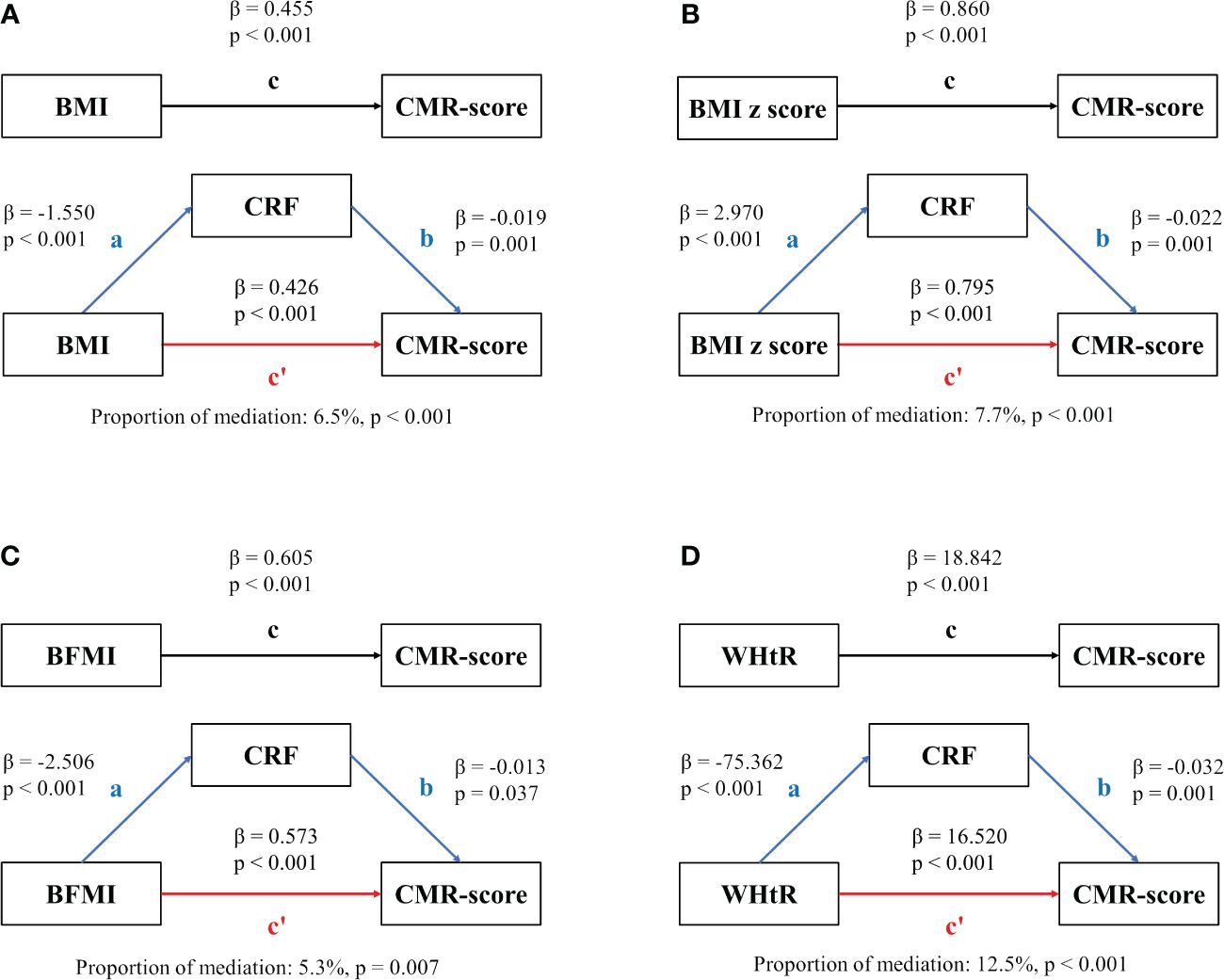
Figure 3 Mediation analysis. Contribution of CRF on the associations of fatness indicators and CMR-score. (A) The mediation between BMI and CMR-score; (B) The mediation between BMI z score and CMR-score; (C) The mediation between BFMI and CMR-score; (D) The mediation between WHtR and CMR-score. The meaning of the lowecase letters were: c means the total effect, c’ means the direct effect, ab means the indirect effect.
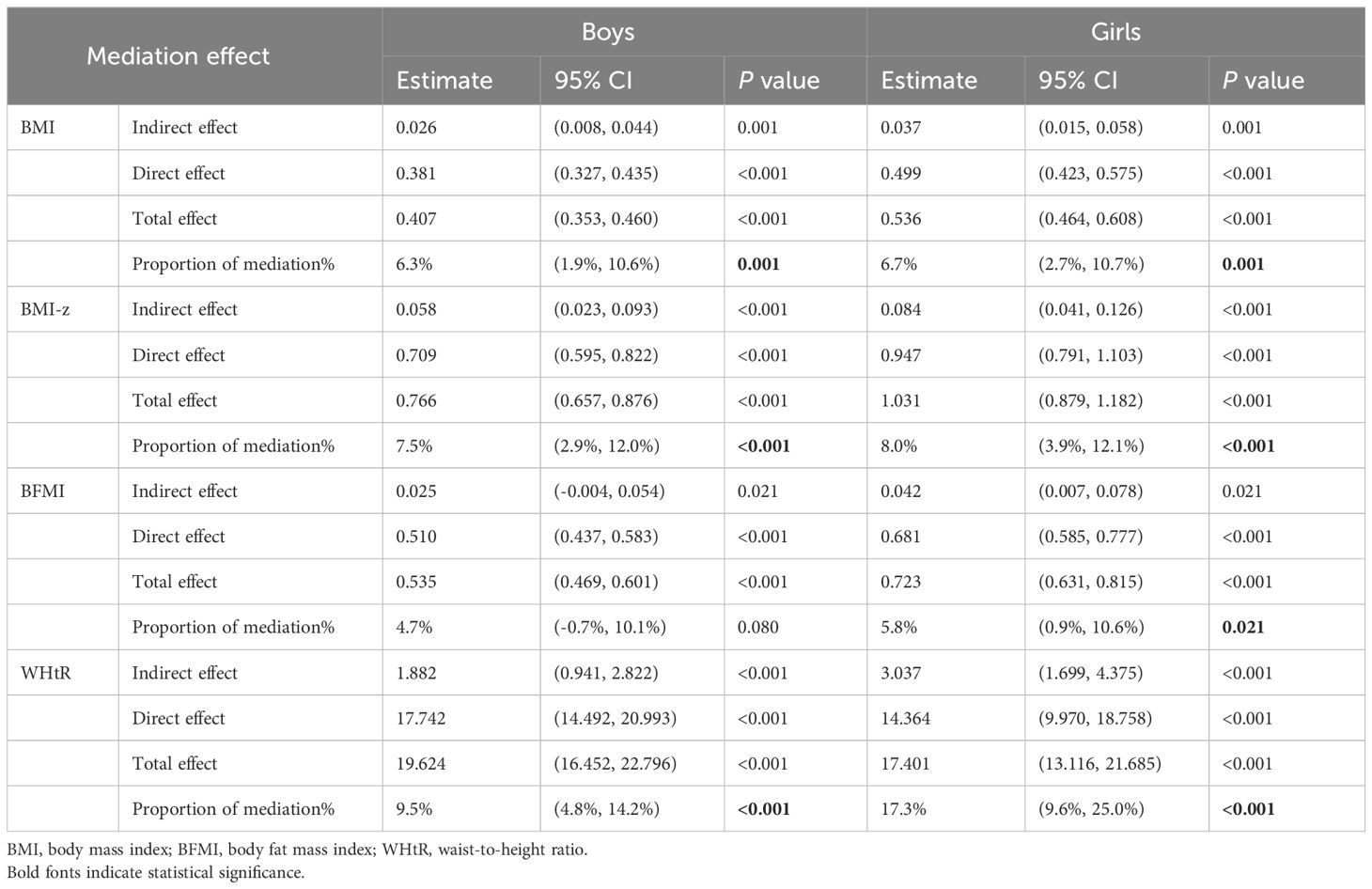
Table 3 Mediation effect of CRF on the associations between fatness indicators and CMR-score among sex.
Additionally, we explored the mediating effect of CRF between four fatness indicators and four individual CMR markers (detailed in Tables 4, 5). We found that the mediating effect sizes of CRF between one of the fatness indicators “WHtR” and all four markers contribute to CMR were particularly robust, ranging from 10.4% to 21.1% (all P < 0.05). And in the further between sexes analyses, the mediation effect for the association between fatness indicators and MAP/TG were more remarkable in girls (Supplementary Tables S4, S6).
To the best of our knowledge, this study is the first to use the 20mSRT to assess CRF and illustrate the extent to which CRF may act as a mediator in the relationship between fatness indicators and CMR in Chinese children. This study revealed that CRF partially attenuate the associations between multiple fatness indicators and individual CMR markers and clustered CMR-score in Chinese children, with the mediation effect size for WHtR and CMR-markers/CMR-score being the largest. Meanwhile, the proportion of mediation were larger in girls, indicating that girls may benefit more from improvements in CRF.
Both obesity and CRF are crucial factors influencing cardiovascular health in childhood. We observed that higher fatness indicators were associated with a worse CMR level, while elevated CRF levels were linked to a better CMR level. These findings align with previous studies (29–32). Childhood obesity is a well-established marker for the clustering of metabolic risk factors, including high triglycerides, low HDL-C, high blood pressure, and dysglycemia (32). Although some therapeutic advances have emerged to address this global problem (33), longitudinal studies with comprehensive data, especially in children with obesity, are still essential to pinpoint the optimal timing for implementing mitigation strategies in children. These studies also suggest that defining a CRF threshold in children may help providers identify those at high risk of cardiometabolic disease, which could be considered in future study.
CRF has been recognized as a predictor of CMR and can be assessed through maximal or submaximal exercise tests. While maximal exercise tests, analyzed for gases, are considered the gold standard, they often require expensive equipment and well-trained staff, which may not always be readily available. In Chinese students aged 7 to 12 years old, the 50m × 8 shuttle run has traditionally been used to assess cardiorespiratory endurance. However, due to its test duration of less than 5 minutes, it may not accurately reflect the actual CRF level. The 20mSRT is currently the most widely used test in school settings worldwide to estimate CRF in children (26). In a review of 73 studies, it demonstrated moderate to high validity against the gold standard for CRF estimation (34). However, it should be concerned that evidence indicated performance in the 20mSRT has a shared variance with body size and fatness (8, 35), which may introduce confounding.
In our study, we observed that the mediation effect size was largest in the associations between one of the fatness indicators “WHtR” and CMR-score and CMR markers. Stoner et. al (14) also found the CRF as mediators in the fatness indicators (BMI, BFMI, and WHtR) and CMR-score in European adolescents (age: 14.1 ± 1.1 years old), the mediation effect sizes were all about 10.0%. Another study from European with children aged 8-11 years also concluded the similar mediation effect, with the fatness evaluated by BMI (15). Our study highlights the largest effect size for WHtR, possibly indicating that abdominal fat may be more important than total body fat, given that WHtR is frequently utilized as a proxy for central adiposity and has been validated as a significant predictor of morbidity (36). In comparison with BMI, WHtR demonstrates a stronger association with cardiovascular disease and provides a more accurate reflection of cardiovascular and metabolic risks (37).
Additionally, we noted that the mediation effect was more pronounced in girls than boys This suggests that interventions aimed at improving CRF may yield greater benefits in girls. In general, girls exhibit higher levels of abdominal fat than boys throughout childhood and adolescence (38). Consequently, improving CRF may potentially lead to easier reduction of abdominal fat in girls. Further research is warranted to investigate the biological mechanisms underlying this gender difference. Our analysis used BMI, BFMI, and WHtR as continuous variables rather than relying on specific clinical cut-offs, which allowed us to examine the dose-response relationships between fatness and CMR, as well as the mediating role of CRF. While our use of continuous variables provides valuable insights, future research could consider the use of clinical cut-offs.
The “fat-but-fit” hypothesis suggests that the risk of all-cause and cardiovascular disease mortality in individuals with obesity but who are fit (i.e., having CRF levels above the age-specific and sex-specific 20th percentile) is not significantly different from that of their normal-weight and fit counterparts (39). Musa et al. (40) found that both fatness and fitness (estimated through the 20mSRT) are independent predictors of blood pressure in Nigerian children. Of these two factors, fatness plays a more important role. Additionally, compared with fat-unfit children, participants with higher CRF had more favorable BP profiles. In our study, we observed that all four fatness indicators (BMI, BMI z score, BFMI and WHtR) partially attenuate the association between fatness and CMR-score in children, with the mediation effect of WHtR being the most substantial, accounting for 12.5%. WHtR is considered an accurate and simpler index for evaluating obesity in children and adolescents (41). To some extent, these findings lend support to the “fat-but-fit” hypothesis. Being fit plays a major role in cardiovascular health, and children benefit from both improved fitness and weight loss. Given that intervention during childhood potentially benefit most, it is critical to conduct relevant intervention studies in children as early as possible in future research.
Several limitations need to be considered of this study. Firstly, we did not estimate the pubertal status of the participants, however, all participant were from grade 3 in primary school with age of 8.5 years, for Chinese children, puberty starts at 9.65 years for boys and 10.65 years for girls (42). Secondly, the cross-sectional design inherently cannot eliminate bidirectional causality, and the narrow age range (8–10 years old) of the participants limit the generalizability, in that large and longitudinal studies may offer more conclusive evidence. Thirdly, there is a concern whether CRF measured by 20mSRT being confounded by body size and composition, but 20mSRT is applicable, convenient and was recommended in large-scale childhood population (43).
In summary, our study results support the promotion that children with excess fatness should pay attention to improving CRF to reduce the harm of fatness to the cardiometabolic system. The more pronounced mediation effect observed in girls suggests potential benefits of CRF interventions. For children and adolescents, addressing both short-term and long-term cardiovascular risks necessitates not only weight management but also the enhancement of cardiopulmonary fitness.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Ethics Committee of the First Affiliated Hospital of Ningbo University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
P-PZ: Data curation, Formal analysis, Investigation, Software, Writing – original draft. Y-XW: Data curation, Formal analysis, Investigation, Methodology, Software, Validation, Writing – original draft. J-YG: Investigation, Methodology, Project administration, Resources, Writing – review & editing. MX: Data curation, Investigation, Supervision, Writing – review & editing. YZ: Data curation, Investigation, Supervision, Writing – review & editing. H-JW: Conceptualization, Resources, Writing – review & editing. PL: Conceptualization, Writing – review & editing. HW: Conceptualization, Data curation, Funding acquisition, Methodology, Resources, Writing – review & editing. LL: Conceptualization, Data curation, Funding acquisition, Investigation, Project administration, Resources, Supervision, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study received funding from the Major Science and Technology Projects for Health of Zhejiang Province (WKJ-ZJ-2216), the Cyrus Tang Foundation for Young Scholar 2022 (2022-B126) and Ningbo public welfare science and technology project (2022S182).
We thank all the children, parents, school teachers in this study for their support, and thank other investigators for their help and advice throughout this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2024.1361447/full#supplementary-material
BMI, body mass index; BFMI, body fat mass index; CMR, cardiometabolic risk; CRF, cardiorespiratory fitness; DBP, diastolic blood pressure; DE, direct effect; FINS, fasting insulin; FPG, fasting plasma glucose; GLM, generalized linear mixed; HDL-C, high-density lipoprotein cholesterol; HOMA-IR, homeostatic model assessment for insulin resistance; IE, indirect effect; LDL-C, low-density lipoprotein cholesterol; MAP, mean arterial blood pressure; SBP, systolic blood pressure; TC, total cholesterol; TE, total effect; TG, triglyceride; WC, waist circumference; WHtR, waist-to-height ratio; 20mSRT, 20-m shuttle run test.
1. Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. (2014) 384:766–81. doi: 10.1016/S0140-6736(14)60460-8
2. China, T.S.C.I.O.o.t.P.s.R.o. Press briefing for the Report on Chinese Residents’ Chronic Diseases and Nutrition 2020 (in Chinese)(2020). Available online at: http://www.gov.cn/xinwen/2020-12/24/content_5572983.htm.
3. Freedman DS, Khan LK, Serdula MK, Dietz WH, Srinivasan SR, Berenson GS. The relation of childhood BMI to adult adiposity: the Bogalusa Heart Study. Pediatrics. (2005) 115:22–7. doi: 10.1542/peds.2004-0220
4. GBD 2015 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. (2016) 388:1659–724. doi: 10.1016/S0140-6736(16)31679-8
5. Kelly AS, Steinberger J, Jacobs DR, Hong CP, Moran A, Sinaiko AR. Predicting cardiovascular risk in young adulthood from the metabolic syndrome, its component risk factors, and a cluster score in childhood. Int J Pediatr Obes. (2011) 6:e283–9. doi: 10.3109/17477166.2010.528765
6. Berenson GS, Srinivasan SR, Bao W, Newman WP, Tracy RE, Wattigney WA. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. N Engl J Med. (1998) 338:1650–6. doi: 10.1056/NEJM199806043382302
7. Raghuveer G, Hartz J, Lubans DR, Takken T, Wiltz JL, Mietus-Snyder M, et al. Cardiorespiratory fitness in youth: an important marker of health: A scientific statement from the American heart association. Circulation. (2020) 142:e101–18. doi: 10.1161/CIR.0000000000000866
8. Haapala EA, Tompuri T, Lintu N, Viitasalo A, Savonen K, Lakka TA, et al. Is low cardiorespiratory fitness a feature of metabolic syndrome in children and adults? J Sci Med Sport. (2022) 25:923–9. doi: 10.1016/j.jsams.2022.08.002
9. dos Santos FK, Prista A, Gomes TN, Santos D, Damasceno A, Madeira A, et al. Body mass index, cardiorespiratory fitness and cardiometabolic risk factors in youth from Portugal and Mozambique. Int J Obes (Lond). (2015) 39:1467–74. doi: 10.1038/ijo.2015.110
10. Zaqout M, Michels N, Bammann K, Ahrens W, Sprengeler O, Molnar D, et al. Influence of physical fitness on cardio-metabolic risk factors in European children. The IDEFICS study. Int J Obes (Lond). (2016) 40:1119–25. doi: 10.1038/ijo.2016.22
11. Andersen LB, Sardinha LB, Froberg K, Riddoch CJ, Page AS, Anderssen SA. Fitness, fatness and clustering of cardiovascular risk factors in children from Denmark, Estonia and Portugal: the European Youth Heart Study. Int J Pediatr Obes. (2008) 3 Suppl 1:58–66. doi: 10.1080/17477160801896366
12. Cristi-Montero C, Courel-Ibáñez J, Ortega FB, Castro-Piñero J, Santaliestra-Pasias A, Polito A, et al. Mediation role of cardiorespiratory fitness on the association between fatness and cardiometabolic risk in European adolescents: The HELENA study. J Sport Health Sci. (2021) 10:360–7. doi: 10.1016/j.jshs.2019.08.003
13. Shang X, Li Y, Xu H, Zhang Q, Hu X, Liu A, et al. Independent and interactive associations of fitness and fatness with changes in cardiometabolic risk in children: A longitudinal analysis. Front Endocrinol (Lausanne). (2020) 11:342. doi: 10.3389/fendo.2020.00342
14. Stoner L, Pontzer H, Barone Gibbs B, Moore JB, Castro N, Skidmore P, et al. Fitness and fatness are both associated with cardiometabolic risk in preadolescents. J Pediatr. (2020) 217:39–45.e1. doi: 10.1016/j.jpeds.2019.09.076
15. Nyström CD, Henriksson P, Martínez-Vizcaíno V, Medrano M, Cadenas-Sanchez C, Arias-Palencia NM, et al. Does cardiorespiratory fitness attenuate the adverse effects of severe/morbid obesity on cardiometabolic risk and insulin resistance in children? A pooled analysis. Diabetes Care. (2017) 40:1580–7. doi: 10.2337/dc17-1334
16. Tomkinson GR, Lang JJ, Tremblay MS, Dale M, LeBlanc AG, Belanger K, et al. International normative 20 m shuttle run values from 1 142 026 children and youth representing 50 countries. Br J Sports Med. (2017) 51:1545–54. doi: 10.1136/bjsports-2016-095987
17. Bettiol H, Rona RJ, Chinn S. Variation in physical fitness between ethnic groups in nine year olds. Int J Epidemiol. (1999) 28:281–6. doi: 10.1093/ije/28.2.281
18. Zhang PP, Wang YX, Shen FJ, Xing YF, Gu JY, Li XY, et al. Lifestyle intervention in children with obesity and nonalcoholic fatty liver disease (NAFLD): study protocol for a randomized controlled trial in Ningbo city (the SCIENT study). Trials. (2024) 25:196. doi: 10.1186/s13063-024-08046-4
19. Buch A, Ben-Yehuda A, Rouach V, Maier AB, Greenman Y, Izkhakov E, et al. Validation of a multi-frequency bioelectrical impedance analysis device for the assessment of body composition in older adults with type 2 diabetes. Nutr Diabetes. (2022) 12:45. doi: 10.1038/s41387-022-00223-1
20. Hurt RT, Ebbert JO, Croghan I, Nanda S, Schroeder DR, Teigen LM, et al. The comparison of segmental multifrequency bioelectrical impedance analysis and dual-energy X-ray absorptiometry for estimating fat free mass and percentage body fat in an ambulatory population. JPEN J Parenter Enteral Nutr. (2021) 45:1231–8. doi: 10.1002/jpen.1994
21. World Health, O. WHO child growth standards: training course on child growth assessment. Genev (2008).
22. Alpízar M, Frydman TD, Reséndiz-Rojas JJ, Trejo-Rangel MA, Aldecoa-Castillo JM. Fat mass index (FMI) as a trustworthy overweight and obesity marker in Mexican pediatric population. Children (Basel). (2020) 7(3):19. doi: 10.3390/children7030019
23. Lee HJ, Shim YS, Yoon JS, Jeong HR, Kang MJ, Hwang IT. Distribution of waist-to-height ratio and cardiometabolic risk in children and adolescents: a population-based study. Sci Rep. (2021) 11:9524. doi: 10.1038/s41598-021-88951-9
24. Kamel M, Smith BT, Wahi G, Carsley S, Birken CS, Anderson LN. Continuous cardiometabolic risk score definitions in early childhood: a scoping review. Obes Rev. (2018) 19:1688–99. doi: 10.1111/obr.12748
25. Lang JJ, Belanger K, Poitras V, Janssen I, Tomkinson GR, Tremblay MS. Systematic review of the relationship between 20m shuttle run performance and health indicators among children and youth. J Sci Med Sport. (2018) 21:383–97. doi: 10.1016/j.jsams.2017.08.002
26. Tomkinson GR, Lang JJ, Blanchard J, Léger LA, Tremblay MS. The 20-m shuttle run: assessment and interpretation of data in relation to youth aerobic fitness and health. Pediatr Exercise Sci. (2019) 31:152–63. doi: 10.1123/pes.2018-0179
27. Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. (1986) 51:1173–82. doi: 10.1037/0022-3514.51.6.1173
28. Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysi: A Regression-Based Approach. New York 732. (2022).
29. Agbaje AO, Haapala EA, Lintu N, Viitasalo A, Barker AR, Takken T, et al. Peak oxygen uptake cut-points to identify children at increased cardiometabolic risk - The PANIC Study. Scand J Med Sci Sports. (2019) 29:16–24. doi: 10.1111/sms.13307
30. Agostinis-Sobrinho C, Ruiz JR, Moreira C, Abreu S, Lopes L, Oliveira-Santos J, et al. Cardiorespiratory fitness and blood pressure: A longitudinal analysis. J Pediatr. (2018) 192:130–5. doi: 10.1016/j.jpeds.2017.09.055
31. Chung ST, Krenek A, Magge SN. Childhood obesity and cardiovascular disease risk. Curr Atheroscler Rep. (2023) 25:405–15. doi: 10.1007/s11883-023-01111-4
32. Magge SN, Goodman E, Armstrong SC. The metabolic syndrome in children and adolescents: shifting the focus to cardiometabolic risk factor clustering. Pediatrics. (2017) 140(2):e20171603. doi: 10.1542/peds.2017-1603
33. Smith JD, Fu E, Kobayashi MA. Prevention and management of childhood obesity and its psychological and health comorbidities. Annu Rev Clin Psychol. (2020) 16:351–78. doi: 10.1146/annurev-clinpsy-100219-060201
34. Castro-Piñero J, Artero EG, España-Romero V, Ortega FB, Sjöström M, Suni J, et al. Criterion-related validity of field-based fitness tests in youth: a systematic review. Br J Sports Med. (2010) 44:934–43. doi: 10.1136/bjsm.2009.058321
35. Fairchild TJ, Klakk H, Heidemann MS, Andersen LB, Wedderkopp N. Exploring the relationship between adiposity and fitness in young children. Med Sci Sports Exerc. (2016) 48:1708–14. doi: 10.1249/MSS.0000000000000958
36. Żegleń M, Kryst Ł, Kowal M, Woronkowicz A. Sexual dimorphism of adiposity and fat distribution among children and adolescents (8-18 year olds) from Poland. Am J Hum Biol. (2024):e24046. doi: 10.1002/ajhb.24046
37. Zong X, Kelishadi R, Hong YM, Schwandt P, Matsha TE, Mill JG, et al. Establishing international optimal cut-offs of waist-to-height ratio for predicting cardiometabolic risk in children and adolescents aged 6-18 years. BMC Med. (2023) 21:442. doi: 10.1186/s12916-023-03169-y
38. Staiano AE, Katzmarzyk PT. Ethnic and sex differences in body fat and visceral and subcutaneous adiposity in children and adolescents. Int J Obes (Lond). (2012) 36:1261–9. doi: 10.1038/ijo.2012.95
39. Ortega FB, Ruiz JR, Labayen I, Lavie CJ, Blair SN. The Fat but Fit paradox: what we know and don’t know about it. Br J Sports Med. (2018) 52:151–3. doi: 10.1136/bjsports-2016-097400
40. Musa DI, Williams CA. Cardiorespiratory fitness, fatness, and blood pressure associations in Nigerian youth. Med Sci Sports Exerc. (2012) 44:1978–85. doi: 10.1249/MSS.0b013e31825ae19d
41. Lo K, Wong M, Khalechelvam P, Tam W. Waist-to-height ratio, body mass index and waist circumference for screening paediatric cardio-metabolic risk factors: a meta-analysis. Obes Rev. (2016) 17:1258–75. doi: 10.1111/obr.12456
42. Liang X, Huang K, Dong G, Chen R, Chen S, Zheng R, et al. Current pubertal development in Chinese children and the impact of overnutrition, lifestyle, and perinatal factors. J Clin Endocrinol Metab. (2023) 108:2282–9. doi: 10.1210/clinem/dgad102
43. Lang JJ, Tremblay MS, Léger L, Olds T, Tomkinson GR. International variability in 20 m shuttle run performance in children and youth: who are the fittest from a 50-country comparison? A systematic literature review with pooling of aggregate results. Br J Sports Med. (2018) 52:276. doi: 10.1136/bjsports-2016-096224
Keywords: obesity, metabolism, fitness, children, mediator
Citation: Zhang P-P, Wang Y-X, Gu J-Y, Xu M, Zhou Y, Wang H-J, Lau PWC, Wang H and Li L (2024) Cardiorespiratory fitness attenuates the association between fatness and cardiometabolic risk in Chinese children. Front. Endocrinol. 15:1361447. doi: 10.3389/fendo.2024.1361447
Received: 26 December 2023; Accepted: 17 April 2024;
Published: 15 May 2024.
Edited by:
Rudolf Lucas, Augusta University, United StatesReviewed by:
Alan R. Barker, University of Exeter, United KingdomCopyright © 2024 Zhang, Wang, Gu, Xu, Zhou, Wang, Lau, Wang and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Li Li, bGlseW5pbmdib0AxNjMuY29t; Hui Wang, aHVpd2FuZ0Biam11LmVkdS5jbg==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.