- 1Department of Pharmaceutical Care, Faculty of Pharmacy, Chiang Mai University, Chiang Mai, Thailand
- 2Pharmacoepidemiology and Statistics Research Center (PESRC), Faculty of Pharmacy, Chiang Mai University, Chiang Mai, Thailand
- 3Sansai Hospital, Ministry of Public Health, Chiang Mai, Thailand
- 4Division of Nephrology, Department of Internal Medicine, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand
- 5Ottawa Hospital Research Institute, Ottawa Hospital, Ottawa, ON, Canada
- 6Institute of Clinical and Evaluative Sciences (ICES), Ottawa, ON, Canada
- 7School of Epidemiology and Public Health, Faculty of Medicine, University of Ottawa, Ottawa, ON, Canada
Background: Although the national-based policy implemented an initiative program to offer diabetes care management in Thailand, there are limited time trends of evidence to gauge whether the quality of diabetes care in primary care practice is improving. As such, we aimed to identify temporal trends in the quality of diabetes care performance among type 2 diabetes mellitus (T2DM) patients in primary care practice.
Methods: Using assembled patient-level data from a suburban community in northern Thailand, this serial retrospective cross-sectional analytical study obtained adult T2DM patients from nine consecutive fiscal years 2013/14 (n = 976) to 2021/22 (n = 1,242). Based on international and national guidelines recommended, nine quality indicators were examined, namely, smoking cessation, hemoglobin A1c monitoring, foot and eye examinations, albuminuria testing, statin prescription, angiotensin-converting enzyme inhibitor/angiotensin II receptor blocker (ACEI/ARB) prescription for chronic kidney disease (CKD)/albuminuria, and blood pressure and glycemic control. Rates and time trends achieved in each quality indicator performance were estimated. Differences in the rates of patients who met each quality indicator across reimbursement schemes were explored.
Results: From 2013/14 to 2021/22, all quality indicators have increased over time (p for trend <0.05) except for smoking cessation, which remained steady. In 2021/22, only three out of nine quality indicators (i.e., smoking cessation, annual HbA1c monitoring, and annual foot examination) were successfully met at 70% or greater. Differences in quality indicators of diabetes performance were observed, particularly those under the Civil Servant Medical Benefit Scheme compared with other health insurance counterparts. For overall time trends analysis (compared with 2013/14), significant relative changes in the fiscal year 2021/22 were found in the annual foot examination (adjusted 12.1% increase; p = 0.048), annual albuminuria testing (adjusted 12.1% increase; p = 0.048), and ACEI/ARB prescription for persons with CKD or albuminuria (adjusted 22.2% increase; p = 0.025).
Conclusion: Among adult T2DM patients from 2013/14 to 2021/22, overall quality indicators for diabetes performance have substantially improved over time. However, health inequity regarding diabetes care performance was found across different reimbursement schemes. Sustainable policy implementation and innovative strategies to narrow health inequity are warranted to optimize diabetes care in primary care practice.
Introduction
According to the Global Burden of Diseases, Injuries, and Risk Factors Study, diabetes is one of the contributing causes of disability and has been recognized as a major cause of noncommunicable disease (NCD) deaths (1, 2). By 2050, it has been projected that more than 1.31 billion people will be living with diabetes worldwide, more than 90% of whom will have type 2 diabetes mellitus (T2DM) (2). People living with T2DM, particularly among those with diabetes-related complications, place immense strains on the disease burden, and they also experience impaired health-related quality of life (3). In addition, it is predicted that T2DM and its consequences consume approximately 12% of worldwide healthcare utilization (4). In Thailand, although the prevalence of diabetes has remained stable at 10% (ranging from 7.7% to 9.9%) over the last two decades (2, 4–7), it is lower in 43 countries and territories worldwide in 2021 (2), and diabetes remains a major public health burden in terms of morbidity, mortality, and healthcare expenditure.
In recent years, collaborative international societies [i.e., American Diabetes Association (ADA), American College of Cardiology/American Heart Association (ACC/AHA), and Kidney Disease: Improving Global Outcomes (KDIGO)] (8–10) and national professional societies (11, 12) have endorsed evidence-based clinical practice guidelines for entities of diabetes care, such as process of diabetes monitoring, optimal target for glycemic and blood pressure (BP) control, and medication optimization, to delivery of effective treatments and services and high-quality diabetes care. However, national and international literature evidence consistently underscores major gaps in delivering health services based on guideline recommendations and implementation in diabetes practice care (13–16).
Over a decade ago, the Ministry of Public Health in Thailand implemented an area health initiative program—Service Plan, which offers diabetes care management as part of the standard of care in NCD healthcare services for integrating and continuing care at primary care practices (11). Since 2013, this national policy framework has been employed at the local and regional levels in an effort to improve the quality of diabetes care, including expanded process of care and quality of measurement, adopted reporting quality of program performance, improved coverage for recommended services and therapy using evidence-based practice, and extension of transition of care across different level of services (11).
Despite these national policy efforts, there are limited time trends of evidence to gauge whether the quality of diabetes care in primary care practice is improving over time. Available studies to date in the Thai diabetes population have been limited by attention to only specific healthcare settings (e.g., elderly T2DM, specialist clinic, or tertiary care) (15, 17, 18) or limited generalizability by focusing on particular source services (5). Regarding studies in primary care settings, most of them have yielded only 1-year or short periods of diabetes care performance figures (16, 19, 20) or reporting before the implementation of the Service Plan—national policy (21), which precludes a temporal appraisal of change and remains a challenge in contemporary diabetes care practices.
To address this knowledge gap in primary care practice in Thailand, we measured nine simple quality indicators that are readily reported and available in primary care practices, involving preventive care, the process of care and testing, and medication utilization and disease control-based outcomes in the clinical entities of national and international guidelines’ recommended care. Based on a serial cross-sectional study between fiscal year 2013/14 and 2021/22 in a primary care setting within a suburban community in northern Thailand, we aimed to investigate whether national-based policy efforts for diabetes care performance using simple quality indicator metrics have been successful over time. Moreover, to address gaps in access to health services and coverage of important diabetic care, we investigated differences in diabetes care quality by health insurance status.
Materials and methods
Study design
We conducted a repeated retrospective cross-sectional analytical study from a single-center cohort of T2DM patients from the Sansai Hospital, a suburban community in northern Thailand, between 1 October 2012 and 30 September 2022. Because of the nature of retrospective data collection and the utilization of de-identified information, the requirement for informed consent was waived. We obtained institutional review board approval from the Chiang Mai Provincial Public Health Office (40/2563). We followed the Declaration of Helsinki and the amendments or comparable ethical standards and reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement guidelines (22).
Study population
We conducted a serial cross-sectional study that includes data on T2DM patients in primary care practices from nine consecutive fiscal years (October 1 to September 30), namely, 2013/14, 2014/15, 2015/16, 2016/17, 2017/18, 2018/19, 2019/20, 2020/21, and 2021/22. Within the measurement fiscal year, we included adult patients (≥18 years of age) diagnosed with T2DM and enlisted at least two consecutive outpatients in primary care practice encounters during that fiscal year. We identified patients with T2DM diagnosis within the following fiscal year based on the International Statistical Classification of Diseases, Ninth Revision (ICD-9) and Tenth Revision (ICD-10) Clinical Modification codes. To minimize the missing values and ensure adequate ascertainment of information, we excluded patients who had periods of medical and pharmacy coverage less than 365 days before the index date of the following fiscal years.
Clinical variables
Variables regarding T2DM patients and diabetes care were based on the information available at primary care practice. These datasets included electronic health record (EHR)—outpatient and inpatient data, administrative data on pharmacy claims, laboratory results, and patient-level data on primary care practice on diabetes and complications. Based on public health protection schemes, we categorized health insurance status into three groups: the Universal Coverage Scheme (UCS) by the National Health Security Office, the Civil Servant Medical Benefit Scheme (CSMBS), and the Social Security Scheme (SSS)/others. We combined those with other health insurance (e.g., self-payment and private insurance) with the SSS group because of the small number of patients, which would preclude the analyses. Smoking status and diabetes care testing [i.e., hemoglobin A1c (HbA1c), foot and eye examination, and urine dipstick/urine albumin–creatinine ratio (UACR)] were extracted from EHR data and primary care practice on diabetes and complications routinely reported data.
Regarding the KDIGO guideline (10), we considered T2DM patients with chronic kidney disease (CKD) using serum creatinine measurements for calculating an estimated glomerular filtration rate (eGFR) based on the Chronic Kidney Disease—Epidemiology Collaboration (CKD-EPI) equation. Those with an eGFR value <60 mL/min/1.73 m2 (stage 3–5) for more than 3 months before the index fiscal year were classified as having comorbid CKD. History of comorbid conditions (i.e., hypertension, coronary heart disease, and cerebrovascular disease) was ascertained based on the ICD-9/10 revision.
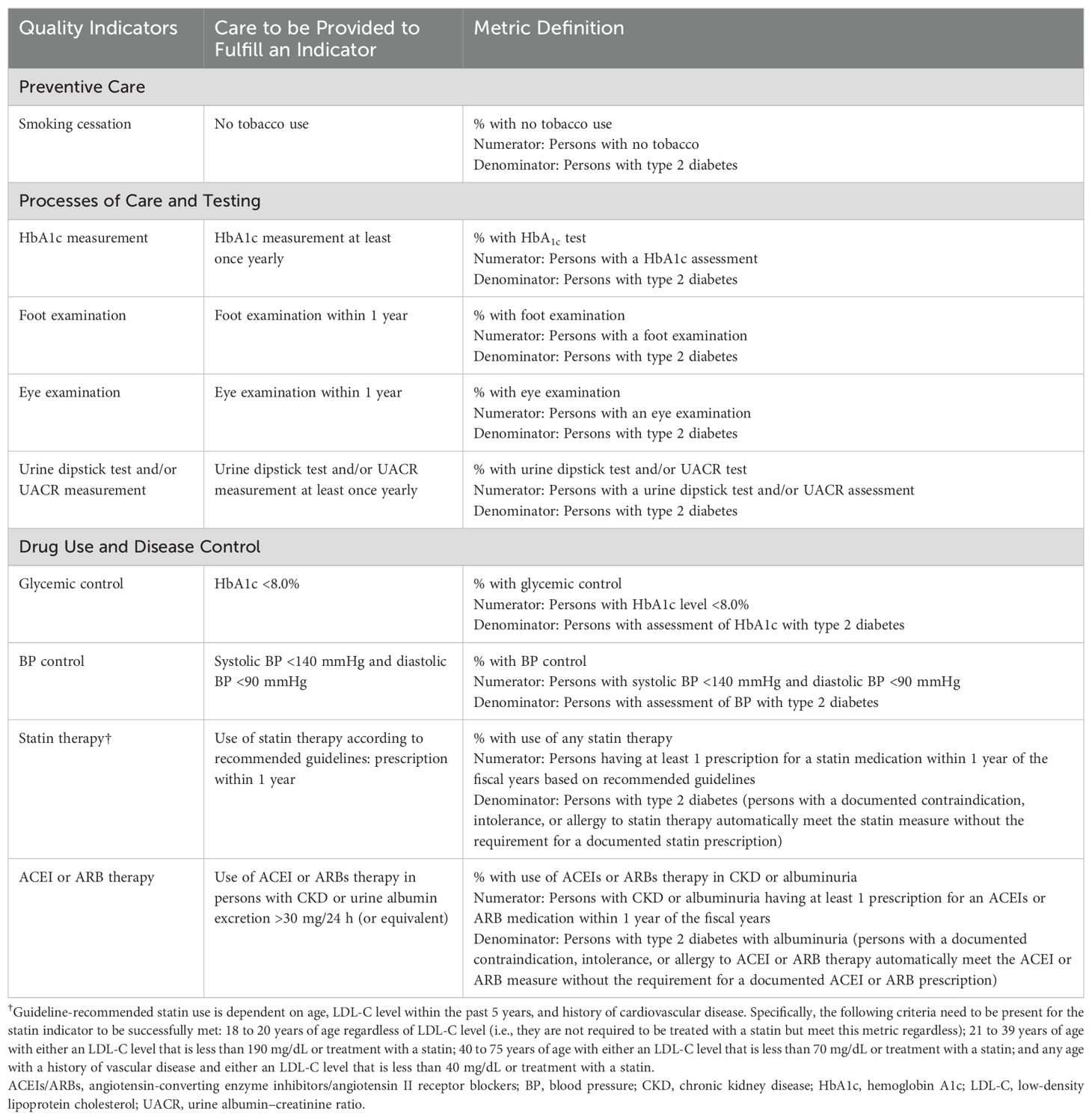
Outcomes: quality indicators performance
Regarding the international guidelines and the initiative Service Plan—a program by the Ministry of Public Health of Thailand (8–12), we adapted and employed nine quality indicators for diabetes care performance in the primary care practice based on preventive care (one indicator), process of care and testing (four indicators), and medication use and disease control (four indicators). These quality indicators for diabetes care included (i) smoking cessation (no tobacco use), (ii) annual HbA1c monitoring, (iii) annual diabetic foot examination, (iv) annual eye examination (digital fundus camera), (v) annual urine dipstick test and/or UACR, (vi) diabetes control (HbA1c <8.0%), (vii) BP control (<140/90 mmHg), (viii) statin prescription according to recommended guidelines, and (ix) angiotensin-converting enzyme inhibitors/angiotensin II receptor blockers (ACEIs/ARBs) prescription for persons with CKD or urine albumin excretion >30 mg/24 h (or equivalent). Each quality indicator was captured using merged EHR, pharmacy claims, laboratory results, and patient-level data on primary care practice on diabetes and complications within the measurement fiscal year. Details of each quality indicator and operational definitions for diabetes care outcome performance are described in Table 1.
Statistical analysis
Analyses were conducted using Stata version 14.0 (StataCorp LLC, TX). A two-sided test with a p-value <0.05 was considered the statistical significance threshold. For descriptive data of patient demographic characteristics, we summarized categorical and continuous variables as the number (percentages) and means ± standard deviations (SDs) or median (min–max).
The unadjusted proportion of T2DM patients who met the diabetes care performance criteria for each quality indicator over the nine consecutive fiscal years (2013/14 to 2021/22) was estimated with 95% confidence intervals (CIs). Using a nonparametric analysis (an extension of the Wilcoxon rank-sum test) for trends across fiscal years, we examined trends in the proportion of patients who met each quality indicator over time. With respect to age- and sex-adjusted analysis, we also estimated diabetes care performance stratified by reimbursement scheme status (i.e., UCS, CSMBS, and SSS/others) to explore inequalities in health benefit package and coverage, which may operate differently among health insurance status. Moreover, the relative change with 95% CIs for each quality indicator performance adjusted for age, sex, and reimbursement scheme was estimated to estimate the temporal trends for change in diabetes care practice between fiscal years 2013/14 and 2021/22.
Results
Description of study population
Overall, sociodemographic and clinical characteristics of T2DM were generally similar across study periods (the proportion of female patients ranged from 56.5% to 57.3%, and the proportion with UCS health insurance ranged from 74.6% to 74.9%), with the noticeable difference in mean age increased from 57.9 to 61.4 years. Based on the recent fiscal year (2021/22) data, a total of 1,242 T2DM patients met the inclusion criteria. Characteristics of patients with T2DM in the fiscal year 2021/22 are described in Table 2 (mean ± SD age, 61.4 ± 10.8 years; 56.5% female; mean body mass index ± SD, 24.7 ± 4.9 kg/m2; mean HbA1c ± SD, 8.2 ± 2.1%). Generally, patient characteristics and medication for glycemic and BP control were different between reimbursement schemes (Table 2). For example, patients undergoing CSMBS health insurance had a significant difference in a higher proportion of elderly, a higher proportion of long-standing diabetes (>10 years), and a higher level of low-density lipoprotein cholesterol than the other health insurance counterparts (Table 2).

Table 2. Demographic characteristics of persons with type 2 diabetes according to sex, fiscal year 2021/22.
Diabetes care performance according to quality indicators
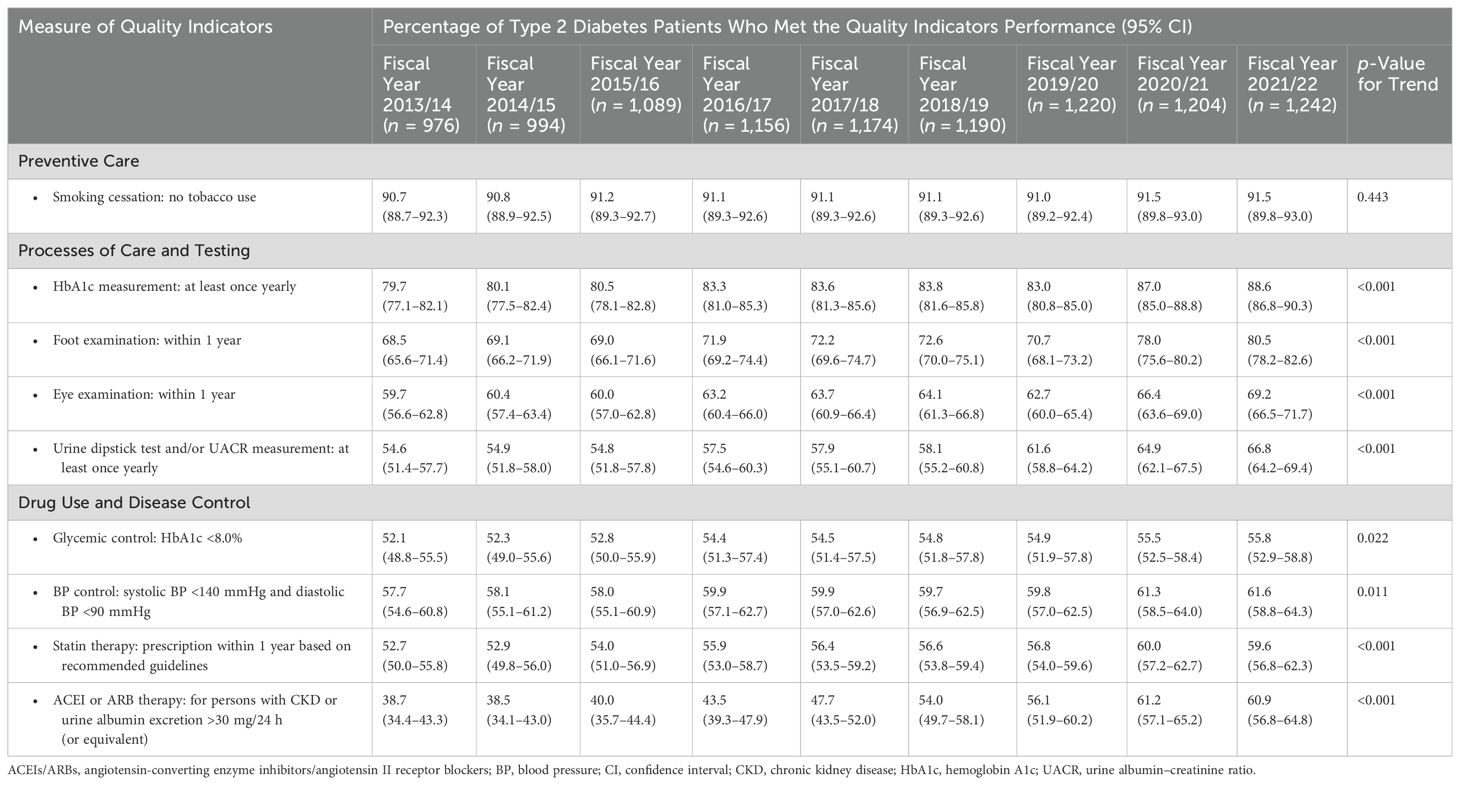
Temporal trends in the unadjusted proportion of T2DM patients who met each quality indicator of diabetes care performance are illustrated in Table 3. All quality indicators have been increased over time except for the domain of prevention care—smoking cessation (p for trend <0.05; Table 3). Overall, only three out of nine quality indicators (i.e., smoking cessation, annual HbA1c monitoring, and annual foot examination) successfully met 70% or greater in the fiscal year 2021/22.
For smoking cessation criteria (Table 3), consistent time trends of T2DM patients with no tobacco use were found, ranging from 90.7% (95% CI, 88.7–92.3) in 2013/14 to 91.5% (95% CI, 89.8–93.0). For the domain of process of care and testing, the proportion of T2DM patients who met diabetes care performance was highest among the criteria of annual HbA1c monitoring (ranging from 79.7% to 88.6%) and lowest among the criteria of annual urine dipstick test and/or UACR measurement (ranging from 54.6% to 66.8%). Of these, during the fiscal year 2019/20, there was a slight drop in the prevalence rate of annual HbA1c monitoring and annual foot and eye examinations.
Likewise, there was an increase in medication use and disease control during the fiscal year 2013/14 to 2021/22: 52.1% to 55.8% for the criteria of HbA1c <8.0%; 57.7% to 61.6% for the criteria of systolic and diastolic BP <140/90 mmHg, and 52.7% to 59.6% for the use of statin therapy based on recommended guidelines (Table 3). Interestingly, the use of ACEI/ARBs therapy for persons with CKD or urine albumin excretion >30 mg/24 h (or equivalent) had dramatically increased from 38.7% (95% CI, 34.4–43.3) in 2013/14 to 60.9% (95% CI, 56.8–64.8) in 2021/22.
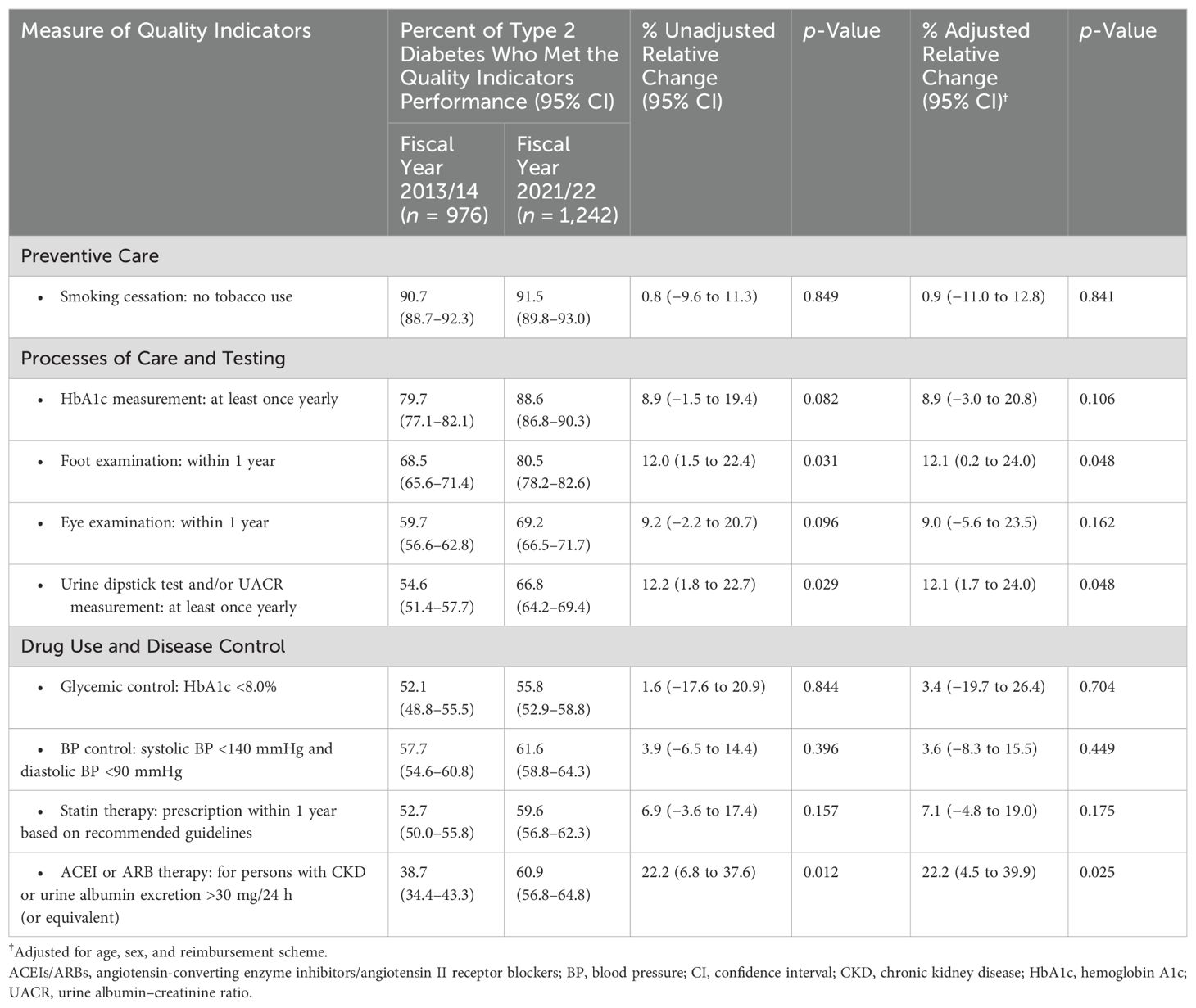
After adjusting for age and sex, T2DM patients with CSMBS health insurance revealed time trends in a greater proportion of patients who met each quality indicator of diabetes care performance compared with UCS or SSS/other groups, particularly for foot and eye examination, glycemic control, and statin therapy (Figure 1). Compared with the inception of study period (2013/14; Table 4), significant relative change in the fiscal year 2021/22 were found in the quality indicator of annual foot examination (adjusted 12.1% increase; 95% CI, 0.2% to 24.0%; p = 0.048), annual urine dipstick test and/or UACR measurement (adjusted 12.1% increase; 95% CI, 1.7% to 24.0%; p = 0.048), and use of ACEI/ARB therapy for persons with CKD or urine albumin excretion >30 mg/24 h (or equivalent) (adjusted 22.2% increase; 95% CI, 4.5% to 39.9%; p = 0.025).
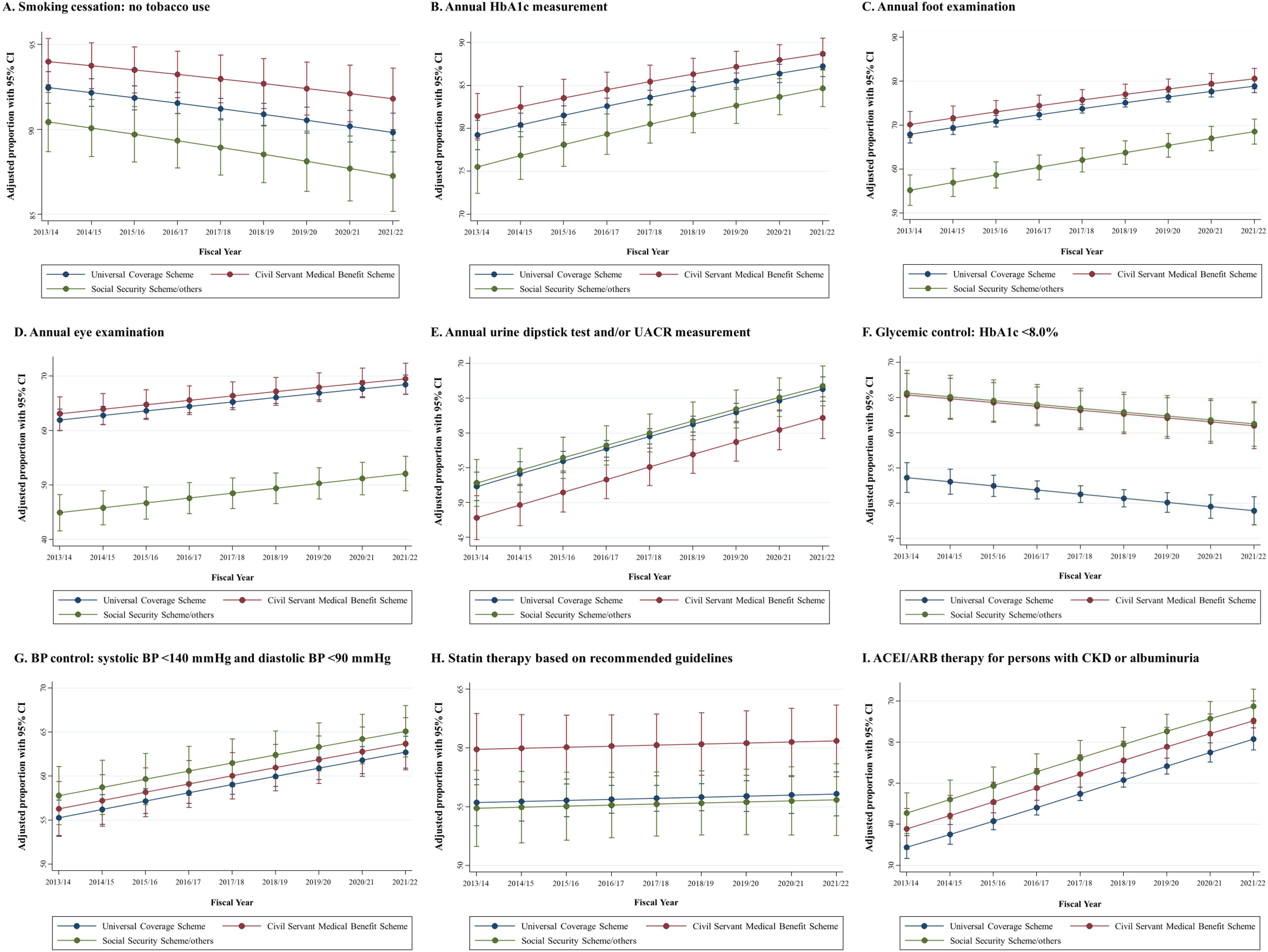
Figure 1. (A–I) Age-, sex-, and reimbursement-adjusted of trends quality indicators of diabetes care performance between the fiscal year 2013/14 and 2021/22. ACEI/ARB, angiotensin-converting enzyme inhibitors/angiotensin II receptor blockers; BP, blood pressure; CI, confidence interval; CKD, chronic kidney disease; HbA1c, hemoglobin A1c.
Discussion
In this serial cross-section study of Thai individuals with T2DM, we found an increase in the quality indicator metrics over the nine consecutive fiscal years (2013/14 to 2021/22), reflecting a health system response to the Service Plan, national-based policy efforts for diabetes care management at primary care practices. However, we identified the disparities and gaps in health insurance status for diabetes care quality-based reimbursement in relation to diabetes monitoring and testing, as well as medication utilization based on recommended guidelines and disease control.
Regarding our findings, we underscore a need to understand reasons and identify factors associated with appropriate or poor performance in each diabetes quality indicator. Based on the nine quality indicators metrics measured, we found only three indicators that illustrated satisfactory performance, with criteria fulfilled at 70% or over in recent years. Specifically, the three indicators that illustrated satisfactory performance were in the domains of preventive care (i.e., smoking cessation: no tobacco use) and the process of care and testing (i.e., annual HbA1c monitoring and annual foot examination). However, inadequate quality indicator metrics performance was concerned within the domains of processes of care and testing (i.e., annual eye examination and urine dipstick test and/or UACR measurement at least once yearly) and medication use and disease control [i.e., HbA1c <8.0%, systolic and diastolic BP <140/90 mmHg, use of statin therapy based on recommended guidelines, and use of ACEI/ARBs therapy for persons with CKD or urine albumin excretion >30 mg/24 h (or equivalent)]. In this circumstance, there are substantial opportunities to improve the quality of diabetes care performance, particularly in the domains of processes of care and testing, medication optimization, and disease control.
Collectively, we found that the quality indicators of diabetes care performance among adult Thai T2DM patients have improved over time compared to the previous studies in the past decade (15, 16, 18, 19, 21, 23). Not surprisingly, during the early COVID-19 pandemic, March 2020 in Thailand, the performance rates of quality indicators requiring in-center testing (i.e., HbA1c measurement, foot examination, and eye examination) appeared to be slightly decreased in the fiscal year 2019/20 compared to the previous fiscal year. However, after that, the overall quality indicator metrics rebounded and continued to increase in 2020/21 and 2021/22. We postulate that rapid responses and social community buffer through hospital preparedness with primary care units and village health volunteers may help mitigate the impact of this unprecedented public health event.
In our study, after adjusting for age, sex, and reimbursement scheme, substantial relative changes in quality indicators over the periods of policy implemented were found in the rate of annual foot examination (12.1% increase), annual urine dipstick test and/or UACR measurement (12.1% increase), and a prescription filled for ACEI/ARB therapy among those with CKD or albuminuria (22.2% increase). Although the performance of the process of care delivery and measurement testing has improved over nearly a decade, lower achievement of disease outcome-based performance in terms of BP and glycemic control (<140/90 mmHg and HbA1c <8.0%) remains observed. Notably, these suggested that only attention to the process of care delivery may be inadequate in isolation regarding the burden of diabetes care. Ultimately, upstream interventions that address both individuals (e.g., modifiable risk factors or social determinants of health) and healthcare system levels (e.g., health information systems, innovative health technologies, and integrative care services and resource delivery) may help further mitigate to achieve high-quality diabetes care.
More importantly, despite the fact that Thailand has implemented UCS health insurance since 2002 and covered over 99% of the population, the unmet attrition to the diabetes care continuum was observed (total unmet need was 70%) among persons under the UCS health insurance in recent years (5). Our findings expanded to the previous study by identifying the disparities and gaps in the quality indicators of diabetes care performance among the different reimbursement schemes. Apparently, we found that those under the CSMBS health insurance had fulfilled and met each quality indicator metric more than UCS or SSS/other counterparts. Of these, persons with CSMBS health insurance were more likely to have annual diabetes foot and eye examination, more likely to have glycemic control with HbA1c <8.0%, and more likely to have filled a prescription for statin therapy than persons with UCS or SSS/other health insurance counterparts. However, the reasons for the inequality in access to the standard of diabetes care are unclear and not fully elucidated by sex and age in this study. Unmeasured or residual confounders regarding multifactorial clinical characteristics and healthcare system environment remain a possible explanation. Based on different health benefit packages in healthcare coverage, we postulated that CSMBS health insurance populations may have access to high-quality diabetes care in terms of measurement testing, monitoring, medication optimization, or referral and collaborative care with a specialist professional (i.e., endocrinologist or nephrologist) compared to UCS or SSS/other health insurance counterparts. To improve diabetes care delivery across all health insurance, strategies or innovative policy-based interventions are needed to narrow health inequity across multiple reimbursement schemes.
Strengths and limitations
As part of a continuous quality improvement program, our findings were based on routinely available serial data collection, reflecting the primary care practice service patterns on diabetes care performance. We highlight the quality indicators of the process of care, health services, and outcome-based performance under the area health initiative strategy that implemented comprehensive diabetes care in primary care centers.
Nevertheless, our study has several limitations. Firstly, this study was based on a single center and unique practice of the Sansai Hospital, which integrated services delivery and coordinated with primary care units and village health volunteers for continuity of care in the community. Thus, the generalizability of these findings to settings other than primary care should be interpreted with caution. However, to the best of our knowledge, we utilize longitudinal data to assess the quality of diabetes care in primary care practice, and some of it may shed light on Thai health policies over time. Secondly, on the basis of our study design, we could not establish whether changes in diabetes care treatment, particularly for medication optimization, were reflected in changes in individuals’ practice of prescribers or due to a policy driven by the Ministry of Public Health. Moreover, we also lacked information regarding the specialties of prescribers (i.e., general physician, endocrinologist, or nephrologist), which may differ in prescribing practice and behavior. Thirdly, based on measurements available in primary care, we limited comorbid CKD to only T2DM patients with moderate to advanced stages (stages 3–5 of CKD) because quantifying eGFR using serum creatinine-based methods cannot identify patients with early stages of CKD. Moreover, urinary protein tests for UACR monitoring were not routinely available in our primary care practice, especially in the early phase of the Service Plan—policy implemented, resulting in the rate of use of ACEI/ARB therapy in persons with CKD being underestimated. Fourthly, on the basis of a temporal trends analysis, medication use for T2DM patients may not be fully elucidated in some clinical situations, for instance, withholding of ACEI/ARB in the clinical entities of hypotension, hyperkalemia, or acute kidney injury. Moreover, we do not include the new treatments, such as glucagon-like peptide-1 receptor agonists or sodium-glucose cotransporter-2 inhibitors, which reduce the risk of CKD progression and mortality among persons with T2DM (8). As such, these promising drugs need to be prioritized in this area for further studies regarding the quality of diabetes in primary care practices. Finally, although we found inequalities in terms of health insurance status, an individual’s level of social determinants of health gradients (e.g., socioeconomic position, education, working life conditions, food insecurity, and access to affordable health services of decent quality) was not fully investigated in this study, which may explain the differences in the proportion of success in each quality indicator of diabetes care performance over time. In this regard, further studies should pay attention to the influence of non-medical factors such as social health inequalities and access to effective diabetes care services.
Conclusions and policy implications
We found that the overall diabetes care performance among adult T2DM patients has substantially improved over time for preventive care, process of care and testing, and medication use and disease control in a primary care practice from the fiscal years 2013/14 to 2021/22. Based on our findings, the relative change in diabetes care practice patterns reflected a shift in the continuous quality improvement system and the impact of the area health initiative program offering diabetes care at primary care centers. However, inequalities in health insurance status were observed; compared with UCS or SSS/other counterparts, T2DM patients undergoing the CSMBS health benefits package were more likely to have foot and eye examinations, achieve glycemic control, and have statin therapy.
Given prominent health insurance status disparities, we underscore that the unmet need for collaborative care remains a challenge for improving quality indicators of diabetes care and minimizing inequality in access to the standard healthcare system. We propose that proactive interprofessional collaborative teams and long-term holistic care services will bring highly effective coverage care to improve diabetes care performance, particularly for diabetes control and medication optimization. Moreover, the sustainable policy that implemented and incorporated innovative approaches driven by evidence-based decisions will be necessary to optimize diabetes care in primary care practice.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Institutional review board approval from the Chiang Mai Provincial Public Health Office (40/2563). The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because this study involved analysis based on the nature of retrospective data collection.
Author contributions
RA: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Project administration, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization. WK: Writing – review & editing, Resources, Project administration, Investigation, Data curation. CR: Writing – review & editing, Validation, Software, Methodology, Investigation, Formal analysis, Conceptualization. KN: Writing – review & editing, Validation, Software, Methodology, Investigation, Formal analysis, Conceptualization. KT: Writing – review & editing, Validation, Methodology, Investigation, Formal analysis, Conceptualization. SN: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Project administration, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was partially supported by Chiang Mai University, Thailand. The funder of the study had no role in the study design collection, analysis, or interpretation of the data or writing of the report.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. NCD Countdown 2030 collaborators. Ncd countdown 2030: worldwide trends in non-communicable disease mortality and progress towards sustainable development goal target 3.4. Lancet. (2018) 392:1072–88. doi: 10.1016/s0140-6736(18)31992-5
2. GBD 2021 Diabetes Collaborators. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: A systematic analysis for the global burden of disease study 2021. Lancet. (2023) 402:203–34. doi: 10.1016/s0140-6736(23)01301-6
3. Zheng Y, Ley SH, Hu FB. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol. (2018) 14:88–98. doi: 10.1038/nrendo.2017.151
4. International Diabetes Federation. IDF Diabetes Atlas. 7th ed. (Brussels: International Diabetes Federation) (2015).
5. Yan LD, Hanvoravongchai P, Aekplakorn W, Chariyalertsak S, Kessomboon P, Assanangkornchai S, et al. Universal Coverage but Unmet Need: National and Regional Estimates of Attrition across the Diabetes Care Continuum in Thailand. PLoS One. (2020) 15:e0226286. doi: 10.1371/journal.pone.0226286
6. Aekplakorn W, Chariyalertsak S, Kessomboon P, Assanangkornchai S, Taneepanichskul S, Putwatana P. Prevalence of diabetes and relationship with socioeconomic status in the thai population: national health examination survey, 2004-2014. J Diabetes Res. (2018) 2018:1654530. doi: 10.1155/2018/1654530
7. Aekplakorn W, Stolk RP, Neal B, Suriyawongpaisal P, Chongsuvivatwong V, Cheepudomwit S, et al. The prevalence and management of diabetes in Thai adults: the international collaborative study of cardiovascular disease in Asia. Diabetes Care. (2003) 26:2758–63. doi: 10.2337/diacare.26.10.2758
8. American Diabetes Association. Standard of care in diabetes–2024. Diabetes Care. (2024) 47:S1–S321. doi: 10.2337/dc24-SREV
9. Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task force on clinical Practice Guidelines. J Am Coll Cardiol. (2019) 73:e285–350. doi: 10.1016/j.jacc.2018.11.003
10. Levin A, Stevens PE, Bilous RW, Coresh J, De Francisco AL, De Jong PE, et al. Kdigo 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. (2013) 3:1–150. doi: 10.1038/kisup.2012.73
11. Division of Non Communicable Diseases. Thailand: NCD Clinic Plus.Department of Disease Control, Ministry of Public Health: Nonthaburi (2023).
12. Diabetes Association of Thailand. Clinical Practice Guideline for Diabetes 2023. Diabetes Association of Thailand: Bangkok (2023).
13. Cheung A, Stukel TA, Alter DA, Glazier RH, Ling V, Wang X, et al. Primary care physician volume and quality of diabetes care: A population-based cohort study. Ann Intern Med. (2017) 166:240–7. doi: 10.7326/m16-1056
14. Kurani SS, Lampman MA, Funni SA, Giblon RE, Inselman JW, Shah ND, et al. Association between area-level socioeconomic deprivation and diabetes care quality in us primary care practices. JAMA Netw Open. (2021) 4:e2138438. doi: 10.1001/jamanetworkopen.2021.38438
15. Sieng S, Hurst C. A Combination of Process of Care and Clinical Target among Type 2 Diabetes Mellitus Patients in General Medical Clinics and Specialist Diabetes Clinics at Hospital Levels. BMC Health Serv Res. (2017) 17:533. doi: 10.1186/s12913-017-2486-7
16. Puangpet T, Pongkunakorn T, Chulkarat N, Bunlangjit C, Surawit A, Pinsawas B, et al. Control and complications of diabetes in urban primary care units in Thailand: A cross-sectional study. BMC Prim Care. (2022) 23:212. doi: 10.1186/s12875-022-01823-7
17. Wongrith P, Thirarattanasunthon P, Kaewsawat S. Glycemic control outcome in patients with type 2 diabetes mellitus: chronic care management support of family care team in Thailand. J Diabetes Metab Disord. (2021) 20:1269–79. doi: 10.1007/s40200-021-00851-x
18. Kaewput W, Thongprayoon C, Mungthin M, Jindarat S, Varothai N, Suwannahitatorn P, et al. Temporal trends in optimal diabetic care and complications of elderly type 2 diabetes patients in Thailand: A nationwide study. J Evid Based Med. (2019) 12:22–8. doi: 10.1111/jebm.12318
19. Somanawat J, Saramunee K, Chanasopon S. Process, quality and challenges of diabetes care in primary care: A study of district health network in Thailand. Prim Health Care Res Dev. (2020) 21:e46. doi: 10.1017/s1463423620000468
20. Sonthon P, Promthet S, Changsirikulchai S, Rangsin R, Thinkhamrop B, Rattanamongkolgul S, et al. The impact of the quality of care and other factors on progression of chronic kidney disease in thai patients with type 2 diabetes mellitus: A nationwide cohort study. PLoS One. (2017) 12:e0180977. doi: 10.1371/journal.pone.0180977
21. Nitiyanant W, Chetthakul T, Sang AKP, Therakiatkumjorn C, Kunsuikmengrai K, Yeo JP. A survey study on diabetes management and complication status in primary care setting in Thailand. J Med Assoc Thai. (2007) 90:65–71.
22. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (Strobe) statement: guidelines for reporting observational studies. Lancet. (2007) 370:1453–7. doi: 10.1016/s0140-6736(07)61602-x
Keywords: quality indicator, patterns, practice care, primary care, time trends, type 2 diabetes
Citation: Awiphan R, Kowatcharakul W, Ruengorn C, Noppakun K, Thavorn K and Nochaiwong S (2024) Temporal trend in quality indicators of diabetes care performance among persons with type 2 diabetes in primary care practice: a serial cross-sectional analytical study, 2013/14 to 2021/22. Front. Endocrinol. 15:1359904. doi: 10.3389/fendo.2024.1359904
Received: 22 December 2023; Accepted: 30 September 2024;
Published: 23 October 2024.
Edited by:
Åke Sjöholm, Gävle Hospital, SwedenReviewed by:
Fatjona Kamberi, University of Vlorë, AlbaniaIchiro Sakuma, Hokko Memorial Hospital, Japan
Copyright © 2024 Awiphan, Kowatcharakul, Ruengorn, Noppakun, Thavorn and Nochaiwong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Surapon Nochaiwong, c3VyYXBvbi5ub2NoYWl3b25nQGdtYWlsLmNvbQ==
†ORCID: Ratanaporn Awiphan, orcid.org/0000-0003-3628-0596
Chidchanok Ruengorn, orcid.org/0000-0001-7927-1425
Kajohnsak Noppakun, orcid.org/0000-0002-5783-8766
Kednapa Thavorn, orcid.org/0000-0003-4738-8447
Surapon Nochaiwong, orcid.org/0000-0003-1100-7171
 Ratanaporn Awiphan
Ratanaporn Awiphan Woravut Kowatcharakul3
Woravut Kowatcharakul3 Chidchanok Ruengorn
Chidchanok Ruengorn Kajohnsak Noppakun
Kajohnsak Noppakun Kednapa Thavorn
Kednapa Thavorn Surapon Nochaiwong
Surapon Nochaiwong