
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Endocrinol., 04 July 2024
Sec. Clinical Diabetes
Volume 15 - 2024 | https://doi.org/10.3389/fendo.2024.1342680
This article is part of the Research TopicCardiovascular Diseases Related to Diabetes and Obesity - Volume VView all 22 articles
Background: Microvascular complications are long-term complications that affect small blood vessels, usually developed in diabetes, and are primary causes of end-stage renal disease, several painful neuropathies, and blindness. Thus, this study aimed to determine diabetic microvascular complications and factors associated with them among patients with type 2 diabetes.
Methods: An institution-based cross-sectional study was conducted among 378 type 2 diabetes patients. The presence of at least one diabetic microvascular complications diagnosed by physicians and found on the record was considered to have microvascular complications. The data was collected by reviewing the medical records of T2DM patients who were on follow-up from January 1, 2012, to December 31, 2021. The collected data was entered into EpiData version 3.1 and analyzed by Stata version 14. Bivariate and multivariable logistic regression were used to identify statistically significant risk factors for diabetic microvascular complications at p-value < 0.05.
Results: Patients with type 2 diabetes mellitus had a prevalence of diabetic microvascular complications of 26.5% (95% CI: 22.0%, 30.9%). Diabetic neuropathy was the highest (13.2%), followed by diabetic nephropathy (12.4%), and diabetic retinopathy (6.4%). Increasing age, poor glycemic control, hypertension comorbidity, anemia, positive proteinuria, a longer duration of type 2 diabetes mellitus, and hypercholesterolemia were significantly associated factors with diabetic microvascular complications.
Conclusion: Diabetic microvascular complications were highly prevalent. Therefore, the study suggests that interventional strategies should be taken for poor glycemic control, hypertension comorbidity, anemia, positive proteinuria, and hypercholesterolemia to control the development of diabetic microvascular complications in patients with type 2 diabetes.
Diabetes mellitus (DM) is a chronic metabolic disease characterized by elevated levels of blood sugar, which over time leads to serious damage to the heart, blood vessels, eyes, kidneys, and nerves (1). It is found worldwide in every population in all regions, and its prevalence is continuously increasing (2). According to the International Diabetes Federation, in 2021, the prevalence of people living with diabetes was estimated at 537 million, or 10.5% of the global adult population aged 20–79 years, and it is projected to rise to 783 million in 2045 (3). Type 2 diabetes mellitus (T2DM) is the most common and accounts for more than 95% of people with diabetes (1, 4, 5). Globally, the rising tide of physical inactivity, energy-dense diets, and obesity has resulted in an unprecedented increase in the number of patients with T2DM (6).
The development of diabetic microvascular complications is significantly impacted by the rising prevalence of diabetes and the increase in life years spent with it. In addition to this, it places a huge burden on almost every health care system, both societal and financial (7). T2DM and its complications have made a significant global contribution to the burden of death and disability (8). Microvascular complications are long-term complications that affect small blood vessels, usually developed in diabetes. These typically include diabetic nephropathy, diabetic neuropathy, and diabetic retinopathy and are primary causes of end-stage renal disease, several painful neuropathies, and blindness respectively (9, 10). It also lowers the standard of living and increases medical expenses for T2DM patients (11, 12).
Microvascular complications are present in half of patients with T2DM (8). In previous studies conducted, the prevalence of microvascular complications was 18.0%-57.5% in Asia (13–16), 34.3%-48.4% in the Middle East (17–19), 47.8% in Nigeria (20), and 19.5%-42.6% in Ethiopia (21–26). Duration of diabetes, hypertension, triglycerides, age, dyslipidemia, poor glycemic control, sex, systolic blood pressure, and positive proteinuria were commonly associated factors with the development of diabetic microvascular complications in previous studies (13, 14, 16, 17, 21, 22, 24–27). Early detection of diabetic microvascular complications in patients with T2DM is important. In Ethiopia, complications from diabetes are a leading cause of morbidity and mortality, which has a knock-on effect on the economy (28). Even if studies have been conducted, diabetic microvascular complications continue to be a public health problem, and the significantly associated factors also vary in study settings. Thus, this study aimed to determine diabetic microvascular complications and factors associated with them among patients with type 2 diabetes at Hawassa University Comprehensive Specialized Hospital, Southern Ethiopia.
The study was conducted at Hawassa University Comprehensive Specialized Hospital from January 1, 2012, to December 31, 2021. The hospital is located in Hawassa town, 278 kilometers from Addis Ababa, the capital city of Ethiopia. Hawassa University Comprehensive Specialized Hospital is the biggest hospital in southern Ethiopia, providing services like emergency, orthopedic, neonatal, ophthalmic, and medical referral clinic for more than 20 million people.
Institution based cross-sectional study was conducted. The source population was all T2DM patients who were attending the diabetic follow-up clinic at Hawassa University Comprehensive Specialized Hospital. All selected newly diagnosed T2DM patients who were enrolled from January 1, 2012, to December 31, 2021, were part of the study population.
The sample size was calculated by using the formula to estimate a single population proportion with the assumptions of a 95% confidence interval Zα/2 = 1.96, proportion (P) = 37.9% from a previous study conducted on the prevalence of microvascular complications (24), margin of error (d) = 0.05, and a 10% non-response rate.
By adding 10%, the final sample size was 398.
Study participants were selected by a simple random sampling technique.
Dependent variable.
Microvascular complications.
Independent variables.
Socio-demographic variables (age, sex, residence), clinical and treatment-related variables (anemia, hypertension, duration of diabetes, family history of diabetes mellitus, proteinuria, fasting blood sugar (FBS), high density lipoprotein (HDL), low density lipoprotein (LDL), total cholesterol, triglyceride, and type of anti-diabetic medication).
Microvascular complications: The presence of at least any one of the following diabetic microvascular complications: diabetic nephropathy, diabetic neuropathy, and diabetic retinopathy, diagnosed by physicians and found on the record. The absence of any diabetic microvascular complications was taken as no microvascular complications.
Hypertension defined as an average systolic blood pressure ≥140 mmHg, or diastolic blood pressure ≥ 90 mmHg, or both, or are on prescription medication for hypertension (29, 30).
The data extraction checklist had socio-demographic, clinical, and treatment-related factors. The tool was developed after reviewing different literature. The data was collected by reviewing the medical records of T2DM patients who were on follow-up from January 1, 2012, to December 31, 2021. Three nurses collected the data, which was facilitated by one supervisor.
One day of training was given to data collectors prior to actual data collection on how to retrieve records and the objective of the study. A pretest using 5% of the sample size was conducted on the same setting, and based on the result of the pretest; an adjustment was made to the data extraction checklist. During data collection, the extracted data were checked for completeness and consistency, and corrections were made accordingly.
The collected data was entered, coded, edited, and cleaned using EpiData version 3.1 and exported to Stata version 14 for analysis. Descriptive statistics, including frequencies with percentage, mean with standard deviation, and median with interquartile range were performed. A bivariate logistic regression analysis was performed between dependent and independent variables. A variable in bivariate analysis with a p-value < 0.25 was used as a candidate for multivariable logistic regression analysis. In multivariable logistic regression analysis, a p-value < 0.05 was considered statistically significant. Model was built by backward stepwise elimination. Multicolinearity was checked using the variance inflation factor with a mean cutoff value < 5. The model adequacy was checked by using the Hosmer and Lemeshow goodness of fit test, which had a P value > 0.05.
A study included a total of 378 T2DM patients, with a response rate of 94.97%. The study participants mean age was 49.5 years, with a standard deviation (SD) of ± 12.7 years. Two hundred ninety (76.72%) of the respondents were urban residents. More than four out of ten (44.44%) participants have hypertension, and 148 (39.15%) had a family history of T2DM. Of the study participants, nearly one-fourth (27.78%) of their HDL was less than 40 mg/dl. More than half (57.14%) of the participants used oral hypoglycemic agents (Table 1).
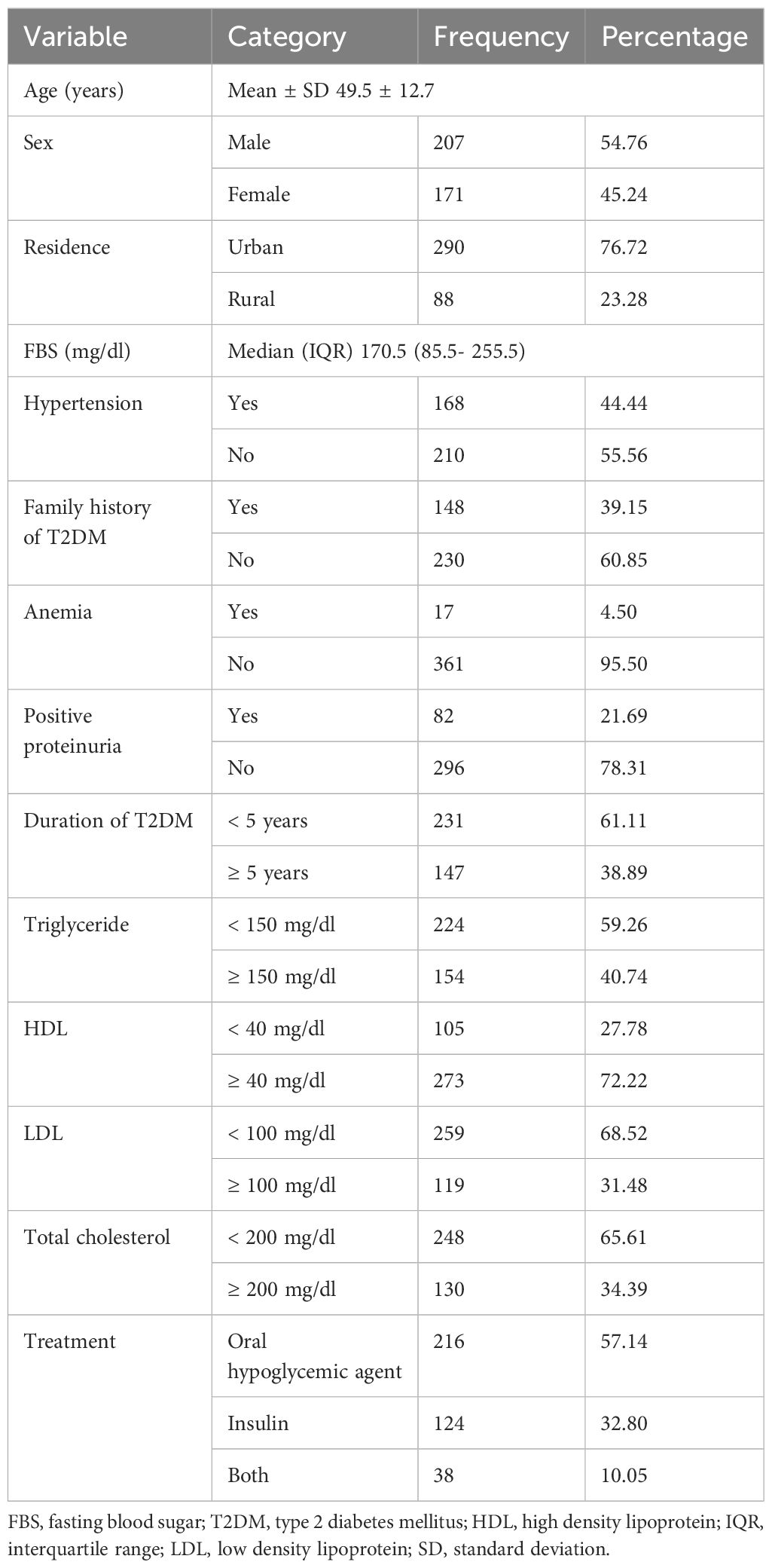
Table 1 Study participant characteristics of patients with type 2 diabetes in Southern Ethiopia (n=378).
According to this study, diabetic microvascular complications in patients with T2DM were 26.5% (95% CI: 22.0%, 30.9%). Diabetic neuropathy was the highest (13.2%), followed by diabetic nephropathy (12.4%), and diabetic retinopathy (6.4%). In bivariate logistic regression analysis, age, residence, FBS, hypertension, anemia, positive proteinuria, duration of T2DM, triglyceride, HDL, LDL, and total cholesterol were factors significantly associated at a p-value of 0.25. But, after adjusting for other variables in multivariable logistic regression, age, FBS, hypertension, anemia, positive proteinuria, duration of T2DM, and total cholesterol were statistically and significantly associated factors with diabetic microvascular complications in patients with T2DM. For each one year increases in age, the odds of developing microvascular complications increase by 4% (AOR, 1.04; 95% CI (1.02-1.06)). As FBS level increases by 1 mg/dl, the odds of developing microvascular complications increase by 1% (AOR, 1.01; 95% CI (1.00-1.01)). The odds of developing microvascular complications with hypertension comorbidity were 86% higher compared to diabetic patients with no comorbid hypertension (AOR, 1.86; 95% CI (1.08- 3.19)). Type 2 diabetic patients with anemia were 3.4 times more likely to develop microvascular complications as compared to their counterparts (AOR, 3.40; 95% CI (1.11- 10.44)). The odds of developing microvascular complications among type 2 diabetic patients were 86% higher in those with positive proteinuria than in those with negative proteinuria (AOR, 1.86; 95% CI (1.00- 3.44)). Type 2 diabetic patients who had a duration of diabetes ≥ 5 years were nearly 3 times more likely to develop microvascular complications than those who had a duration of diabetes less than 5 years (AOR, 2.93; 95% CI (1.72- 5.01)). The odds of developing microvascular complications among type 2 diabetic patients with total cholesterol ≥ 200 mg/dl were nearly 2 times higher compared to patients with total cholesterol less than 200 mg/dl (AOR, 1.93; 95% CI (1.13- 3.29)) (Table 2).
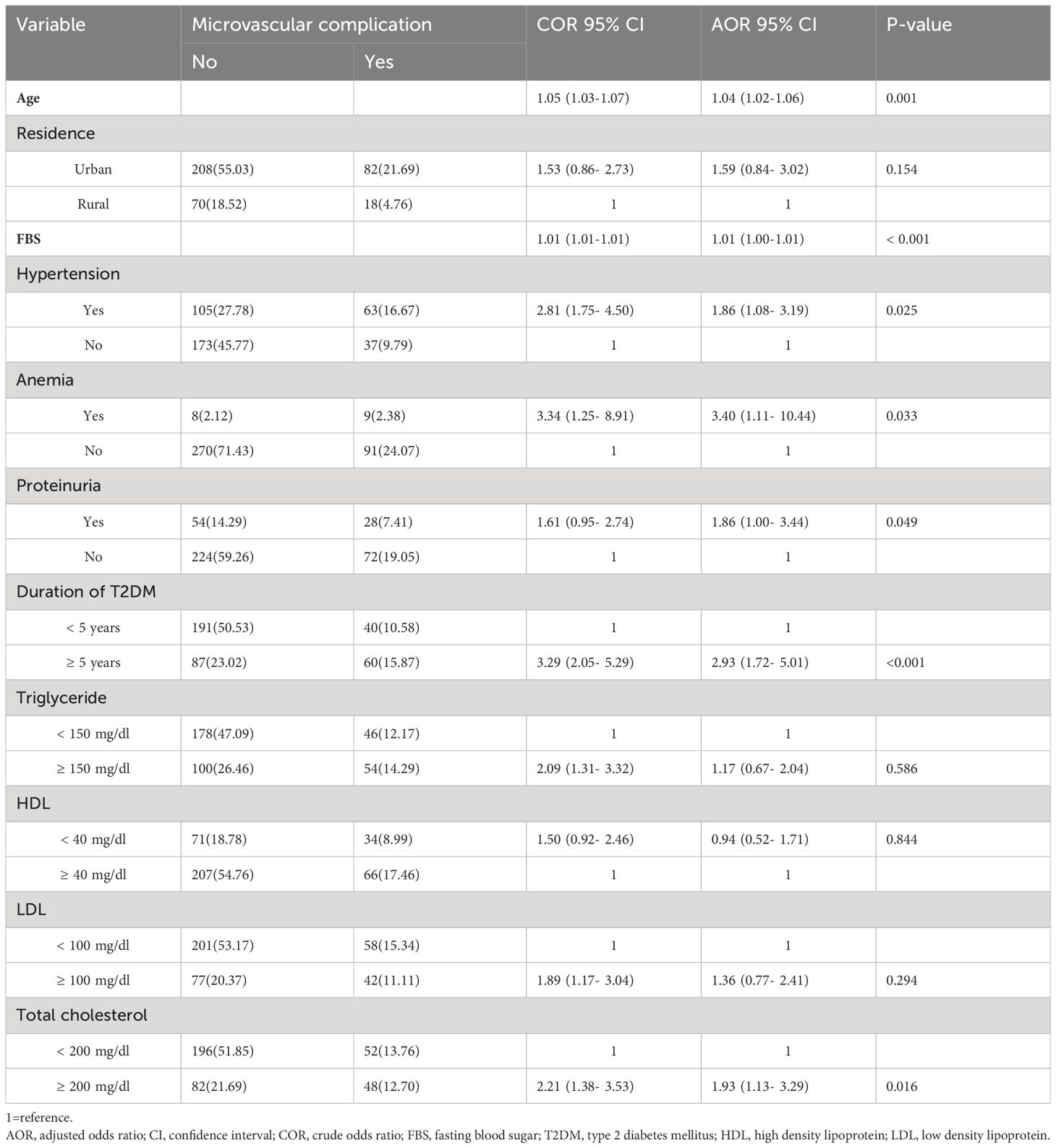
Table 2 Multivariable logistic regression analysis for factors associated to diabetic microvascular complications among patients with type 2 diabetes in Southern Ethiopoia (n=378).
This study’s main goal was to determine diabetic microvascular complications and factors associated with patients with T2DM. The overall prevalence of diabetic microvascular complications was 26.5%. Multivariable logistic regression analysis revealed that age, FBS, hypertension, anemia, positive proteinuria, duration of T2DM, and total cholesterol were the factors associated with the development of diabetic microvascular complications. The study findings would have implications for clinical and management practices to have strategies targeting old age, poor glycemic control, hypertension comorbidity, being anemic, having positive proteinuria, a longer duration of T2DM, and hypercholesterolemia for diabetes care to prevent or delay the development of diabetic microvascular complications.
The study found that 26.5% of study participants had diabetic microvascular complications. The finding was in line with a study conducted in the North West, Ethiopia 26.3% (22). However, the finding was higher than the finding of studies from Northern Ethiopia 19.5%, and Chandigarh, India 18.04% (13, 21). The finding of this study was lower than the finding of the studies conducted in Jimma, Ethiopia 41.5%, Dessie, Ethiopia 37.9%, Gondar, Ethiopia 31.33%, Ayder, Ethiopia 42.6%, Jos, Nigeria 47.8%, Tabuk, Saudi Arabia 34.3%, Doha, Qatar 48.4%, South India 52.1%, Tianjin, China 34.5%, and Ningbo, China 57.5% (14–17, 19, 20, 23–26). This discrepancy might be due to differences in diagnostic methods or criteria, sample size, and healthcare systems.
In this study, increased age was found to increase the risk of diabetic microvascular complications. The finding is consistent with a study conducted in Ethiopia, Nigeria, India, China, and Ireland (13, 16, 20, 24, 26, 27). This could be due to a combination effect of insulin resistance and predominately a loss of beta cells in advanced age, which results in poor glycemic control and greater microvascular damage (31). Higher FBS levels showed a significant association with the development of diabetic microvascular complications, as has been observed in previous studies conducted in Ethiopia and Saudi Arabia (22, 26). This might be associated with the high blood sugar level for longer periods effect of cell damage mainly occurs in capillary endothelial cells of the retina, mesangial cells of the renal glomerulus, neurons, and Schwann cells of peripheral nerves, causing diabetic microvascular complications (32).
According to the findings of this study, the risk of microvascular complications was higher in T2DM patients with hypertension. The study finding is in line with the studies done in Ethiopia, Saudi Arabia, Qatar, China, and Ireland (14, 16, 17, 19, 24, 27). The possible explanation might be due to increasing intracellular hyperglycemia through upregulation of the glucose transporter 1 (33). For every 10 mm Hg of higher systolic blood pressure, the risk of diabetic microvascular complications increased by 9% (34). Therefore, blood pressure control decreases the onset and development of microvascular complications in patients with T2DM (35). The finding of this study showed that T2DM patients with anemia have an increased risk of developing diabetic microvascular complications, which might be due to tissue hypoxia and hemodynamic effects in diabetic tissues (36). Previous studies showed an association between anemia and microvascular complications in patients with T2DM (37, 38).
The present study revealed that positive proteinuria were significantly associated factor of diabetic microvascular complications. The finding is similar with the previous studies conducted in Ethiopia (21, 22). Proteinuria itself could lead to the progression of diabetic nephropathy, which is indicative of damage to the glomerular filtration barrier (39, 40). Furthermore, in this study, the risk of diabetic microvascular complications was higher in patients with a T2DM duration ≥ 5 years. The finding is in accordance with the studies conducted in Ethiopia, Nigeria, Saudi Arabia, China, and Ireland (14, 16, 17, 20, 24). Moreover, the finding that the risk of diabetic microvascular complications was higher in patients with T2DM whose total cholesterol ≥ 200 mg/dl is consistent with previous studies done in Saudi Arabia and China (14, 17). The explanation may be that dyslipidemia may cause or exacerbate diabetic microvascular complications through alterations in the coagulation-fibrinolytic system, changes in membrane permeability, damage to endothelial cells, and increased atherosclerosis. Diabetes patients with hypercholesterolemia experienced a faster decline in their glomerular filtration rate (41). Mean total cholesterol levels for diabetics with microvascular complications were significantly higher (42). Thus, appropriate measures should be undertaken with regular monitoring of total cholesterol levels.
The limitation of this study is that the findings may not be generalizable to the total population because of the institution-based nature of the study, and some variables like socioeconomic status, alcohol use, and body mass index were incomplete in the patient’s medical records. As the study was cross-sectional, the cause-and-effect relationship between the associated factors and diabetic microvascular complications was impossible to determine. The strength of this study was that longer-term data were used.
According to this study, diabetic microvascular complications were highly prevalent. Increasing age, poor glycemic control, hypertension comorbidity, anemia, positive proteinuria, longer duration of T2DM, and hypercholesterolemia were factors independently associated with diabetic microvascular complications in patients with T2DM. Therefore, microvascular complications need to be identified early, and interventional strategies should be taken to control the modifiable risk factors poor glycemic control, hypertension comorbidity, anemia, positive proteinuria, and hypercholesterolemia associated with the development of diabetic microvascular complications in patients with T2DM.
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
The studies involving humans were approved by Institutional Review Board of Arab Minch University, College of Medicine and Health Sciences. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
FM: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Resources, Software, Visualization, Writing – original draft, Writing – review & editing. FG: Methodology, Supervision, Validation, Writing – review & editing. HE: Methodology, Supervision, Validation, Writing – review & editing. TG: Formal analysis, Methodology, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
We would like acknowledge all medical referral staffs for their support during data collection.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. WHO. Diabetes (2022). Available online at: https://www.who.int/health-topics/diabetes.
3. International Diabetes Federation. IDF Diabetes Atlas. 10th edn. Brussels, Belgium: International Diabetes Federation (2021). Available at: https://www.diabetesatlas.org.
4. World Health Organization. Diabetes . Available online at: https://www.who.int/news-room/fact-sheets/detail/diabetes.
5. Lin X, Xu Y, Pan X, Xu J, Ding Y, Sun X, et al. Global, regional, and national burden and trend of diabetes in 195 countries and territories: an analysis from 1990 to 2025. Sci Rep. (2020) 10:14790. doi: 10.1038/s41598-020-71908-9
6. Chatterjee S, Khunti K, Davies MJ. Type 2 diabetes. Lancet (London England). (2017) 389:2239–51. doi: 10.1016/S0140-6736(17)30058-2
7. Crasto W, Patel V, Davies MJ, Khunti K. Prevention of microvascular complications of diabetes. Endocrinol Metab Clinics North America. (2021) 50:431–55. doi: 10.1016/j.ecl.2021.05.005
8. Zheng Y, Ley SH, Hu FB. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev endocrinology. (2018) 14:88–98. doi: 10.1038/nrendo.2017.151
10. Zimmerman RS. Diabetes mellitus: management of microvascular and macrovascular complications. J Cleveland Clinic: Centers Continuing Educ. (2016).
11. Arnold SV, Khunti K, Tang F, Chen H, Nicolucci A, Gomes MB, et al. Impact of micro- and macrovascular complications of type 2 diabetes on quality of life: insights from the DISCOVER prospective cohort study. Endocrinology Diabetes Metab. (2022) 5:e00321. doi: 10.1002/edm2.321
12. Visaria J, Iyer NN, Raval AD, Kong SX, Hobbs T, Bouchard J, et al. Healthcare costs of diabetes and microvascular and macrovascular disease in individuals with incident type 2 diabetes mellitus: a ten-year longitudinal study. ClinicoEconomics outcomes research: CEOR. (2020) 12:423–34. doi: 10.2147/CEOR.S247498
13. Bansal D, Gudala K, Esam HP, Nayakallu R, Vyamusani RV, Bhansali A. Microvascular complications and their associated risk factors in newly diagnosed type 2 diabetes mellitus patients. Int J chronic diseases. (2014) 2014:201423. doi: 10.1155/2014/201423
14. Bui HDT, Jing X, Lu R, Chen J, Ngo V, Cui Z, et al. Prevalence of and factors related to microvascular complications in patients with type 2 diabetes mellitus in Tianjin, China: a cross-sectional study. Ann Trans Med. (2019) 7:325. doi: 10.21037/atm
15. Govindarajan Venguidesvarane A, Jasmine A, Varadarajan S, Shriraam V, Muthuthandavan AR, Durai V, et al. Prevalence of vascular complications among type 2 diabetic patients in a rural health center in South India. J primary Care Community Health. (2020) 11:2150132720959962. doi: 10.1177/2150132720959962
16. Li J, Chattopadhyay K, Xu M, Chen Y, Hu F, Chu J, et al. Prevalence and associated factors of vascular complications among inpatients with type 2 diabetes: a retrospective database study at a tertiary care department, Ningbo, China. PloS One. (2020) 15:e0235161. doi: 10.1371/journal.pone.0235161
17. Saiyed NS, Yagoub U, Al Qahtani B, Al Zahrani AM, Al Hariri I, Syed MJ, et al. Risk factors of microvascular complications among type 2 diabetic patients using cox proportional hazards models: a cohort study in tabuk Saudi Arabia. J Multidiscip healthcare. (2022) 15:1619–32. doi: 10.2147/JMDH.S367241
18. Dweib M, El Sharif N. Diabetes-related microvascular complications in primary health care settings in the west bank, Palestine. J Clin Med. (2023) 12:6719. doi: 10.3390/jcm12216719
19. Cheema S, Maisonneuve P, Zirie M, Jayyousi A, Alrouh H, Abraham A, et al. Risk factors for microvascular complications of diabetes in a high-risk middle east population. J Diabetes Res. (2018) 2018:7. doi: 10.1155/2018/8964027
20. Jasper U, Opara M, Pyiki E. Prevalence and clinical pattern of acute and chronic complications in African diabetic patients. Br J Med Med Res. (2014) 4:4908. doi: 10.9734/BJMMR
21. Gebremedhine H, Gidey B. micro-vascular-complications-and-associated-factors-among-type-two-diabetic-patients-in-adigrat-and-wkuro-general-hospit. J Diabetes Metab. (2020) 11:856. doi: 10.35248/2155-6156.20.11.856
22. Gashaye Shita N, Sharew Iyasu A. Predictors of blood glucose change and microvascular complications of type 2 diabetes mellitus patients in Felege Hiwot and Debre Markos referral hospital, North West Ethiopia. BMC Endocrine Disord. (2022) 22:1–13. doi: 10.1186/s12902-022-01047-x
23. Fasil A, Biadgo B, Abebe M. Glycemic control and diabetes complications among diabetes mellitus patients attending at University of Gondar Hospital, Northwest Ethiopia. Diabetes Metab syndrome obesity: Targets Ther. (2019) 12:75–83. doi: 10.2147/DMSO
24. Seid MA, Akalu Y, Gela YY, Belsti Y, Diress M, Fekadu SA, et al. Microvascular complications and its predictors among type 2 diabetes mellitus patients at Dessie town hospitals, Ethiopia. Diabetol Metab syndrome. (2021) 13:86. doi: 10.1186/s13098-021-00704-w
25. Tilahun A, Waqtola C, Tewodros G, Amare D, Yohannis M. Major micro vascular complications and associated risk factors among diabetic outpatients in Southwest Ethiopia. Endocrinol Metab Syndr. (2017) 6:272. doi: 10.4172/2161-1017.1000272
26. Berihun L, Muluneh EK. Correlates of time to microvascular complications among diabetes mellitus patients using parametric and non-parametric approaches: a case study of Ayder referral hospital, Ethiopia. Ethiopian J Sci Technology. (2017) 10:65–80. doi: 10.4314/ejst.v10i1.5
27. Tracey ML, McHugh SM, Fitzgerald AP, Buckley CM, Canavan RJ, Kearney PM. Risk factors for macro- and microvascular complications among older adults with diagnosed type 2 diabetes: findings from the irish longitudinal study on ageing. J Diabetes Res. (2016) 2016:5975903. doi: 10.1155/2016/5975903
28. Bishu KG, Jenkins C, Yebyo HG, Atsbha M, Wubayehu T, Gebregziabher M. Diabetes in Ethiopia: a systematic review of prevalence, risk factors, complications, and cost. Obes Med. (2019) 15:100132. doi: 10.1016/j.obmed.2019.100132
29. Passarella P, Kiseleva TA, Valeeva FV, Gosmanov AR. Hypertension management in diabetes: 2018 update. Diabetes Spectrum. (2018) 31:218–24. doi: 10.2337/ds17-0085
30. Organization WH. Noncommunicable disease education manual for primary health care professionals and patients. World Health Organization (2017). Available at: https://iris.who.int/handle/10665/254746.
31. Zoungas S, Woodward M, Li Q, Cooper ME, Hamet P, Harrap S, et al. Impact of age, age at diagnosis and duration of diabetes on the risk of macrovascular and microvascular complications and death in type 2 diabetes. Diabetologia. (2014) 57:2465–74. doi: 10.1007/s00125-014-3369-7
32. Giri B, Dey S, Das T, Sarkar M, Banerjee J, Dash SK. Chronic hyperglycemia mediated physiological alteration and metabolic distortion leads to organ dysfunction, infection, cancer progression and other pathophysiological consequences: an update on glucose toxicity. Biomedicine pharmacotherapy = Biomedecine pharmacotherapie. (2018) 107:306–28. doi: 10.1016/j.biopha.2018.07.157
33. Hurst C, Thinkhamrop B. The association between hypertension comorbidity and microvascular complications in type 2 diabetes patients: a nationwide cross-sectional study in Thailand. Diabetes Metab J. (2015) 39:395–404. doi: 10.4093/dmj.2015.39.5.395
34. Li C, Yu H, Zhu Z, Shang X, Huang Y, Sabanayagam C, et al. Association of blood pressure with incident diabetic microvascular complications among diabetic patients: Longitudinal findings from the UK Biobank. J Global Health. (2023) 13:13. doi: 10.7189/jogh.13.04027
35. Climie RE, van Sloten TT, Bruno R-M, Taddei S, Empana J-P, Stehouwer CD, et al. Macrovasculature and microvasculature at the crossroads between type 2 diabetes mellitus and hypertension. Hypertension. (2019) 73:1138–49. doi: 10.1161/HYPERTENSIONAHA.118.11769
36. Thomas MC, Cooper ME, Rossing K, Parving HH. Anaemia in diabetes: is there a rationale to TREAT? Diabetologia. (2006) 49:1151–7. doi: 10.1007/s00125-006-0215-6
37. Hosseini MS, Rostami Z, Saadat A, Saadatmand SM, Naeimi E. Anemia and microvascular complications in patients with type 2 diabetes mellitus. Nephro-urology monthly. (2014) 6:e19976. doi: 10.5812/numonthly
38. Nasrat M, Samar MY, Esheba NE, Mohammed HE. The relation between anemia and microvascular complications in patients with type 2 diabetes mellitus. Med J Cairo Univ. (2018) 86:947–54. doi: 10.21608/mjcu.2018.55761
39. Zelmanovitz T, Gerchman F, Balthazar AP, Thomazelli FC, Matos JD, Canani LH. Diabetic nephropathy. Diabetol Metab syndrome. (2009) 1:10. doi: 10.1186/1758-5996-1-10
40. Raja P, Maxwell AP, Brazil DP. The potential of albuminuria as a biomarker of diabetic complications. Cardiovasc Drugs Ther. (2021) 35:455–66. doi: 10.1007/s10557-020-07035-4
41. Misra A, Kumar S, Kishore Vikram N, Kumar A. The role of lipids in the development of diabetic microvascular complications: implications for therapy. Am J Cardiovasc drugs: drugs devices other interventions. (2003) 3:325–38. doi: 10.2165/00129784-200303050-00004
Keywords: microvascular complications, prevalence, associated factors, T2DM, southern Ethiopia
Citation: Merid F, Getahun F, Esubalew H and Gezahegn T (2024) Diabetic microvascular complications and associated factors in patients with type 2 diabetes in Southern Ethiopia. Front. Endocrinol. 15:1342680. doi: 10.3389/fendo.2024.1342680
Received: 22 November 2023; Accepted: 20 June 2024;
Published: 04 July 2024.
Edited by:
Lu Cai, University of Louisville, United StatesReviewed by:
Shiferaw Letta, Haramaya University, EthiopiaCopyright © 2024 Merid, Getahun, Esubalew and Gezahegn. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fasika Merid, bWVyaWRmMjAwNUBnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.