
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Endocrinol., 06 February 2024
Sec. Bone Research
Volume 15 - 2024 | https://doi.org/10.3389/fendo.2024.1323595
This article is part of the Research TopicWomen in Bone ResearchView all 16 articles
We aimed to evaluate the clinical efficacy of five traditional Chinese fitness exercises (Baduanjin, Taijiquan, Wuqinxi, Yijinjing, and Liuzijue), as well as their efficacy when combined with drug therapy, in the treatment of decreased bone mineral density in postmenopausal women
Methods: This study strictly followed the evaluation guidelines of PRISMA and followed the “PICOS” principle outlined in the Cochrane Handbook. We performed a systematic search on Web of Science, Springer Link, Scopus, EMBASE, EBSCO, PubMed, the Cochrane Library, CNKI, Wanfang, CBMdisc, and the VIP Database, and we targeted RCTs studying the effect of TCE on BMD in postmenopausal women published prior to September 2023. The quality of the literature and the risk of bias of the included studies were assessed according to ROB2 and GRADE criteria, and data analysis was performed using Stata 14.
Results: A total of 33 RCTs (3658 post-menopausal women) were included. Network meta-analysis showed that Taiji (SMD=0.72, 95% CI: 0.22, 1.21, P<0.01) and Yijinjing (SMD=0.51, 95% CI: 0.03, 0.99, P<0.05) were significantly superior to conventional rehabilitation in lumbar BMD. In terms of improvement of femoral neck BMD, Baduanjin (SMD=1.63, 95% CI: -3.58, 6.85, P<0.001) and Taiji (SMD=0.46, 95% CI: 0.14, 0.79, P<0.05) had statistically different outcomes to conventional rehabilitation. Regarding Ward’s triangle BMD, Taiji (SMD= 0.32, 95% CI: 0.14, 0.50, P< 0.05) had statistically different outcomes to conventional rehabilitation. The results of the SUCRA probability ranking showed that Baduanjin + drug interventions achieved the most significant improvement in lumbar BMD (SUCRA=83.6%) and femoral neck BMD (SUCRA=90.2%). Taiji + drug interventions most effectively improved Ward’s triangle BMD (SUCRA=86.0%). In terms of traditional Chinese fitness exercises alone, Taiji was the most effective in improving lumbar BMD (SUCRA=64.4%) and Ward’s triangle BMD (SUCRA=46.8%), and Baduanjin was the most effective in treating femoral neck BMD (SUCRA=89.9%).
Conclusion: Traditional Chinese fitness exercises can significantly improve the BMD levels of postmenopausal women. Taiji, Yijinjing, and Baduanjin combined with medication showed better intervention effects overall. However, due to the limitations of the number of studies and sample sizes of individual interventions, definitive conclusions need to be verified by more high-quality studies.
As women age, they experience degeneration of ovarian function. A lack of estrogen leads to reduced bone mass, decreased bone density, and structural changes in bone tissue, which increases bone fragility and fracture susceptibility (1–4). In an observational study, lack of estrogen increased osteoporosis-related fractures by about 50% (5). An estimated 32 million people in Europe had osteoporosis in 2019, with around 80% of cases involving postmenopausal women (6), where the residual lifetime risk of a hip fracture at the age of 50 years ranged from 7.0% (Romania) to 25.1% (Sweden) (7). As human life expectancy increases and the global aging process accelerates, the prevalence of postmenopausal osteoporosis will increase in the coming decades (8, 9). The data show that the rate of bone loss in older women is significantly accelerated 1–10 years after menopause, with an annual loss rate of 1.5–2.5% and a reduction in BMD, which increases the risk of fracture by 2.6 times (10). Recently, European data showed that menopausal women are 40% more likely to experience fractures (11). In summary, postmenopausal osteoporosis and the accompanying loss of bone density have become a severe public health problem and a threat to older women’s health.
Given the prevalence of postmenopausal osteoporosis and the many disadvantages of pharmacological treatment, such as long cycle times, high costs, adverse effects, and poor compliance, exercise therapy is gaining increasing attention as a complementary therapy to pharmacological treatment, due to its advantages of being economical and having few side effects (12). In recently years, traditional Chinese exercise (TCE), including Taiji, Yijinjing, Baduanjin, Wuqinxi, and Liuzijue, has played a significant role in the treatment of osteoporosis, and has been widely and flexibly used in clinical practice (13–15). Compared to other exercises, TCEs are easy to learn and are not restricted by exercise venues. They impact personal health and disease prevention by improving body balance (16), strengthening lower limb muscles (17, 18), and preventing postmenopausal osteoporosis (19).
Despite differences in the design of experiments testing this, TCE is a safe option for the prevention and treatment of primary osteoporosis or bone loss. Recent meta-analyses have shown that Taiji interventions prevent further osteoporotic BMD decline in elderly female patients with osteopenia or osteoporosis (20). Another meta-analysis showed that, of a range of exercises, Baduanjin was most effective in inhibiting or even reversing BMD in older adults with osteoporosis (21). However, there has been a lack of systematic reviews of TCE’s effects on BMD in older postmenopausal adults, other than Taiji. Furthermore, a recent meta-analysis suggested that different exercise patterns may affect BMD in older adults (10). Therefore, it is crucial to systematically determine the pathways of BMD influence of TCE in postmenopausal women.
Therefore, we aimed to integrate the relevant clinical evidence of the direct and indirect comparative relationships between different TCEs using a network analysis. The effect of different TCEs on BMD at different sites was assessed using a network analysis, based on a probability ranking of the superiority of the index efficacy in postmenopausal women.
This study followed the international guidelines for writing meta-analyses (PRISMA) (22). The registration number for our study is INPLASY2022110030 (DOI number 10.37766/inplasy2022.11.0030). The literature was obtained from Web of Science, Springer link, Scopus EMBASE, Cochrane Library, EBSCO, PubMed, CNKI, Wanfang, CBMdisc, and VIPdatabases. Our study aimed to identify published RCTs on the effects of TCE on BMD in postmenopausal women, with a deadline of 30 September 2023. The words used in the search of databases included “Taiji (Tai Chi or Tai Ji Quan or Taijiquan, etc.) or Health Qigong or Qigong or Qi Gong or Chi Kung or Baduanjin or Wuqinxi or Yijinjing or Liuzijue or traditional Chinese exercise AND bone density or bone mass or osteoporosis AND menopause or postmenopausal or women or female. Taking PubMed, Embase, and China Knowledge as examples, Appendix I outlines the specific search strategies.
Two researchers (S.J.L. and W.L.) independently determined the relevant research data. The degree of agreement between the two researchers was quantified using Cohen’s Kappa; the Cohen’s Kappa value of the two researchers was 0.679, indicating good agreement (23).
Two independent reviewers (S.J.L. and W.L.) examined the titles and abstracts of the retrieved articles and performed the primary screening based on inclusion and exclusion criteria. After obtaining the full text of the RCTs, the full text of the first selected studies was rechecked, and the studies to be analyzed were finalized. A Cohen’s Kappa value of 0.655 was obtained between the researchers, indicating moderate agreement. The studies were further reviewed by the two independent researchers until a consensus was reached. The third reviewer’s opinion (S.J.W.) was adopted without a contract.
Eligibility criteria for inclusion in the study were as follows: (1) RCTs; (2) the participants were diagnosed as postmenopausal women with osteopenia, or with normal bone mass, and had no serious complications or other diseases; (3) the experimental group included traditional Chinese fitness exercises (e.g., Taiji, Baduanjin, Wuqinxi, Yijinjing, and Liuzijue), and was compared with control groups (e.g., drugs, usual care, and exercise training); (4) outcome indicators included BMD in the lumbar spine or femoral neck, or Ward’s triangle BMD, as one of the outcome indicators; (5) before the test, each group of indicators showed a consistent baseline among subjects; (6) the study data were in the form of mean ± standard deviation or could be transformed into M ± SD (if the data in the literature were presented as the standard error (SE), then SD=SE× (N is the sample size) was used for transformation); and (7) the studies were published in Chinese or English.
The exclusion criteria were: (1) duplicated studies; (2) no major TCE interventions; (3) abstract-only articles and non-RCT studies; (4) conference emails not able to be contacted; and (5) no data or data not clearly reported for analysis.
We followed the PICO model in the reporting, design, and descriptive data extraction, including the following: first author, country, and year of publication, sample size (attrition rate), mean age or age range, years of menopause, bone mass of participant, intervention design (intervention, time, frequency), and main outcome indicators. Detailed information for inclusion in the study is shown in Table 1.
This study assessed the methodological quality of the randomized controlled trials included in the survey using RoB2, which considered the following domains: bias during randomization, inclination to deviate from established interventions (including the effect of intervention allocation and the impact of intervention adherence), bias related to missing outcome data, bias related to measurement of outcomes, and prejudice related to reporting the results selectively. Under each domain, there are multiple “signaling questions”, each of which provides five answers: Yes, Probably Yes, Probably No, No, and No Information, and based on the answers to the signaling questions, RoB2 generates a recommended risk assessment outcome.
Two independent reviewers (S.J.L. and W.L.) performed a quality assessment of the literature, and based on the RoB2 risk assessment, the included randomized controlled trials were classified as “high risk of bias”, “some concerns”, and “low risk of bias”.
In addition, we invited the first two independent reviewers to review the literature in which there was inconsistency in opinion until a consensus was reached. In the absence of agreement, the third reviewer’s opinion (S.J.W.) was adopted.
A traditional meta-analysis was performed by applying the MetaXL program (version 5.3). Given the small sample size of the screened and suitable literature and the slight differences in evaluation tools and units used in individual studies, the standardized mean difference (SMD) and its 95% confidence interval (CI) calculated by the Hedges’g method were used to estimate the relative effect of each intervention. For each direct comparison, effect sizes were aggregated using an inverse heterogeneity (IVhet) model, which corrects for heterogeneity and generates more robust results relative to traditional fixed- and random-effects models.
Both the Q-test and I2 results determined heterogeneity in the literature. The meta-analysis was performed using a fixed-effects model when P≥0.1 for the Q-test and I2<50% indicated that inter-study heterogeneity was within acceptable limits, and vice versa using the random-effects model. The outcomes were categorized as either very low (<25%), low 25–50%), moderate (50–75%), or significant (>75%) (56). Furthermore, publication bias was measured using Doi plots with the LFK index, which has been shown to have higher accuracy than traditional funnel plots with the egger test, especially when the number of studies is small. Finally, sources of heterogeneity were sought through sensitivity analyses (rejected one by one) and subgroup analyses.
A network meta-analysis was performed using Stata 14.0 in a frequency-based framework. A grid relationship diagram was drawn by network meta-analysis (in the diagram, each node indicates the intervention, the size of the area of the node indicates the number of samples corresponding to the intervention, and the thickness of the line connecting the nodes indicates the number of studies included for the intervention) (57). When there was a closed-loop structure between interventions, inconsistency tests were required, and the model type was selected accordingly. If the lower limit of the 95% CI of the inconsistency factor’s (IF) value was zero (or close to zero), this indicated that the direct evidence and indirect evidence were consistent (58). Finally, the area under the cumulative ranked probability curve (surface under the cumulative, SUCRA) showed the magnitude of the likelihood of each intervention being the best intervention (56).
The Grading Recommendations to Assess Development and Evaluation system (GRADE) is an evidence evaluation system, and is one of the international standards for evidence quality and the classification of recommendation strength (13). We evaluated the quality of the evidence for each outcome using the GRADE classification with four possible levels: I (high), where the real effect is similar to a credible estimate; II (moderate), where the true effect is closest to the estimated effect; III (low), where the actual effect may be significantly different from the estimated effect; and IV (very low), where the actual effect is likely to be significantly different from the estimated effect. Five factors can cause the quality of the evidence to decrease: (1) risk of bias; (2) imprecision; (3) inconsistency; (4) indirectness; and (5) publication bias (59).
A total of 585 articles were found from 11 databases (Figure 1), and 490 were removed by title and abstract. The remaining 95 articles were further screened by reading the complete text, and 62 records were excluded as they were non-RCTs (n=21), they had no reported data for analysis (n = 14), they were reviews (n = 6), they had no major TCE interventions (n = 13), and conference emails were not provided (n = 8). Finally, 33 studies were included in our network analysis.
In total, there were 3658 participants [the smallest sample was 30 (60) and the largest sample was 800 (37)]. The ages of the participants ranged from 50 to 70 years old. Three studies had an intervention period of 12 weeks (27, 40, 48), and 13 studies had an intervention period of 48 weeks, in addition to one study with an intervention period of 96 weeks (42). The experimental group involved 62 cases of traditional Chinese fitness exercises in a single treatment protocol, of which 15, 3, 5, 2, and 1 group used Taiji, Baduanjin, Wuqinxi, Yijinjing, and Liuzijue techniques as interventions, respectively. The protocols using Taiji, Baduanjin, and Wuqinxi in combination with medication included 5, 6, and 3 groups, respectively. The control groups were treated with usual care or drug therapy. Furthermore, 32 articles metrics measured lumbar spine BMD, 20 articles measured femoral neck BMD, and 13 articles measured Ward’s triangle BMD. During the intervention period, 11 articles (30, 31, 34, 37, 38, 41, 44, 51–53, 61) reported the follow-up status.
The results of the risk of bias evaluation of the RCTs are shown in Figure 2. Thirty-three articles in our study reported the random allocation method as a random number table method/computer randomized generation, sixteen articles reported deviation from the intended intervention, one paper was missing outcome data, and no selective outcomes were reported in any article.
Based on the criteria of GRADE, the assessment of the certainty of the evidence regarding the significant impact of traditional Chinese fitness exercises on bone mineral density in postmenopausal women was carried out separately (Table 2). Specifically, traditional Chinese fitness exercises has medium-high quality evidence for the lumbar spine, femoral neck, and Ward’s triangle BMD of postmenopausal women, indicating that the quality assessment of this study had a high degree of credibility.
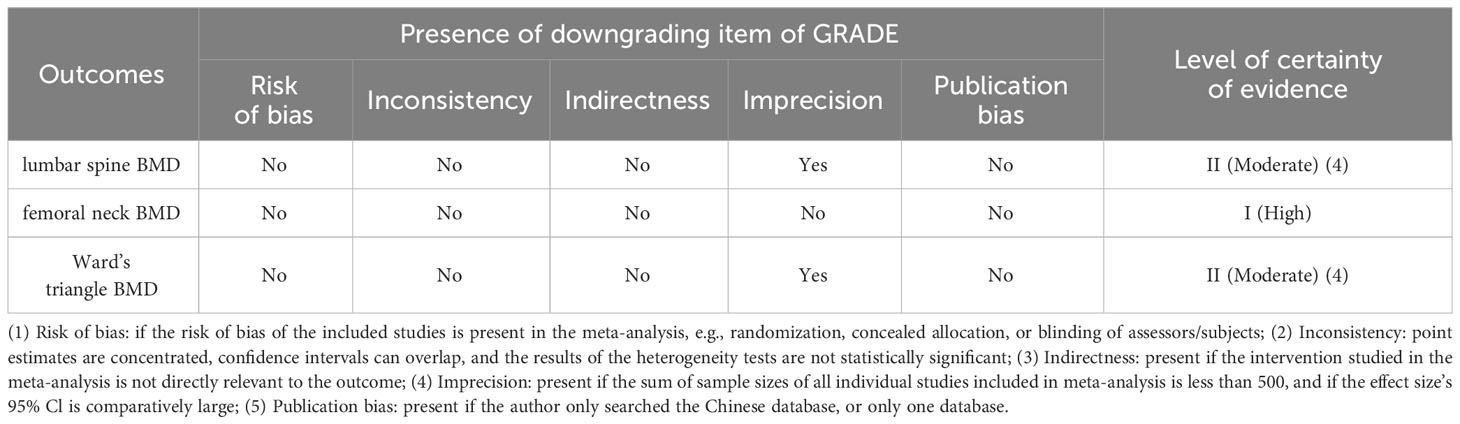
Table 2 Grading Recommendations to Assess Development and Evaluation system (GRADE) assessment of the evidence of certainty for traditional Chinese fitness exercises.
A total of 33 articles were included in the traditional meta-analysis, which used Doi plots and the LFK index. The LFK index in the ±1 interval suggests that there may have been minimal publication bias, in the ±2 interval suggests that there may have been a slight publication bias, and outside the ±2 interval suggests that there may have been a significant publication bias (62). Specifically, as shown in Table 3, in the Lumbar Spine BMD and Femoral Neck BMD indexes, the publication bias of the interventions involving Baduanjin was more significant, and in general, the studies on the effects of Baduanjin on each index of BMD in postmenopausal women had a significant bias. In contrast, the bias of studies of other Chinese traditional fitness exercises was negligible. Further heterogeneity analysis revealed that the heterogeneity of Lumbar Spine BMD and Femoral Neck BMD was significant (I2 > 50%, P< 0.1), and the heterogeneity of Ward’s triangle BMD was weak (I2< 50%, P > 0.1). Based on the data in this study, subgroup analyses were conducted by classifying different exercise forms, and sensitivity analyses (article-by-article elimination) were performed to find the source of heterogeneity (Table 4), which showed that except for the subgroups of Taiji and Baduanjin, which were still heterogeneous, the rest of the groups were homogeneous. A random effects model was used for the analysis to ensure the study’s accuracy.
Traditional Chinese fitness exercises significantly improved L-BMD (SMD = 0.58, 95% CI -0.34 to 0.82, p< 0.01) and Femoral Neck BMD (SMD = 0.63, 95% CI 0.28 to 0.98, p< 0.01) in postmenopausal women, with some statistically significant improvement in Ward’s triangle BMD (SMD=0.26, 95% CI 0.15 to 0.36, p< 0.05) (Table 5). Subgroup analyses based on different exercise modalities showed that Taiji had a high effect size for improvement in L-BMD (SMD=0.72, 95% CI 0.22 to 1.21, p< 0.01) and a medium effect size for improvement in Femoral Neck BMD (SMD=0.46, 95% CI 0.14 to 0.79, p< 0.01) and Ward’s triangle BMD (SMD = 0.32, 95% CI 0.14 to 0.50, p< 0.01). Baduanjin had a high effect size for the improvement effect on Femoral Neck BMD (SMD = 1.63, 95% CI -3.58 to 6.85, p< 0.01) in postmenopausal women, and small effect sizes for both Ward’s triangle BMD (SMD = 0.19, 95% CI - 0.39 to 0.78, p< 0.05), and L-BMD (SMD = 0.03, 95% CI - 1.05 to 1.10, p > 0.05), which were not statistically different. Wuqinxi had a slight effect size for improvement on all BMD indicators in postmenopausal women (p< 0.05). Yijinjing had a significant improvement effect in L-BMD (SMD = 0.51, 95% CI 0.03 to 0.99, p< 0.01) and a minor improvement effect in Femoral Neck BMD (SMD=0.23, 95% CI 0.35 to 0.80, p< 0.05).
The overall inconsistency test showed that the L-BMD outcome indicator P > 0.05, which indicated that the overall consistency was good. Further tests of the consistency of each closed loop showed that the value of the inconsistency factor (IF) ranged from 0.06 to 0.14, and the lower limit of the 95% CI all contained 0, which indicated that the consistency of each closed loop was better, so the consistency model was used for analysis.
In total, 32 RCT studies reported changes in L-BMD pretest-posttest intervention in 2771 subjects; 14 studies included drug therapy as the control group and 18 studies had usual care as the control group, with three studies reporting both drug therapy and usual care, incorporating a web of relationships between studies (Figure 3). The pairwise comparison between the two found that Taiji was superior to exercise training (SMD=-0.05, 95% CI -0.10 to -0.02, p<0.05) and Wuqinxi (SMD=-0.05, 95% CI -0.13 to -0.01, p<0.05) and Baduanjin (SMD=-0.06, 95% CI -0.16 to -0.02, p<0.05). It is worth noting that the Baduanjin+drug group was better than Baduanjin (SMD=-0.11, 95% CI -0.24 to -0.04, p<0.05), and the drug group (SMD=-0.08, 95% CI -0.14 to -0.02, p<0.05) (Table 6).
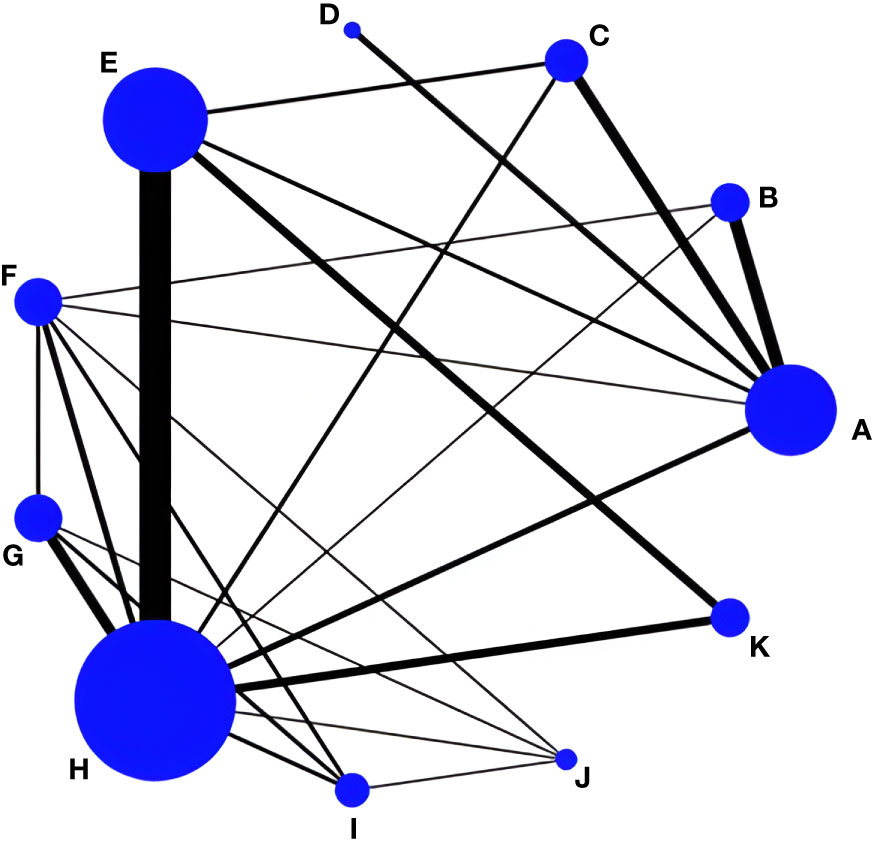
Figure 3 Network evidence for L-BMD. (A) Drug group; (B) Baduanjin+Drug group; (C) Taiji+Drug group; (D) Wuqinxi+Drug group; (E) Taiji; (F) Baduanjin; (G) Wuqinxi; (H) Usual care; (I) Yujinjin; (J) Liuzijue; (K) Exercise training.
In addition, the final ranking of the five single modulation interventions, the three-drug combination interventions, and the three control groups was performed using SUCRA, with percentages indicating that the more significant the portion of the area under the SUCRA curve, the better the treatment effect (Figure 4). The final ranking was as follows: Baduanjin+drug (83.6%) > Taiji+drug (78.7%) > Taiji (64.4%) > drug (59.3%) > Yijinjin (49.7%) > Liuzijue (48.2%) > exercise training (47.1%) > Wuqinxi+drug (46.9%) > Wuqinxi (35%) > Baduanjin (32%) > usual care (5.2%).
Twenty RCT studies reported changes in femoral neck BMD before and after the intervention, amounting to 2593 subjects; six included drug therapy as the control group and 13 included usual care, of which one study reported both drug therapy and usual care, and the reticulation between the included studies was performed as in Figure 5. Subsequently, the overall inconsistency test showed the femoral neck BMD outcome indicator P<0.05 and the overall consistency was poor, so the inconsistency model was used for analysis.
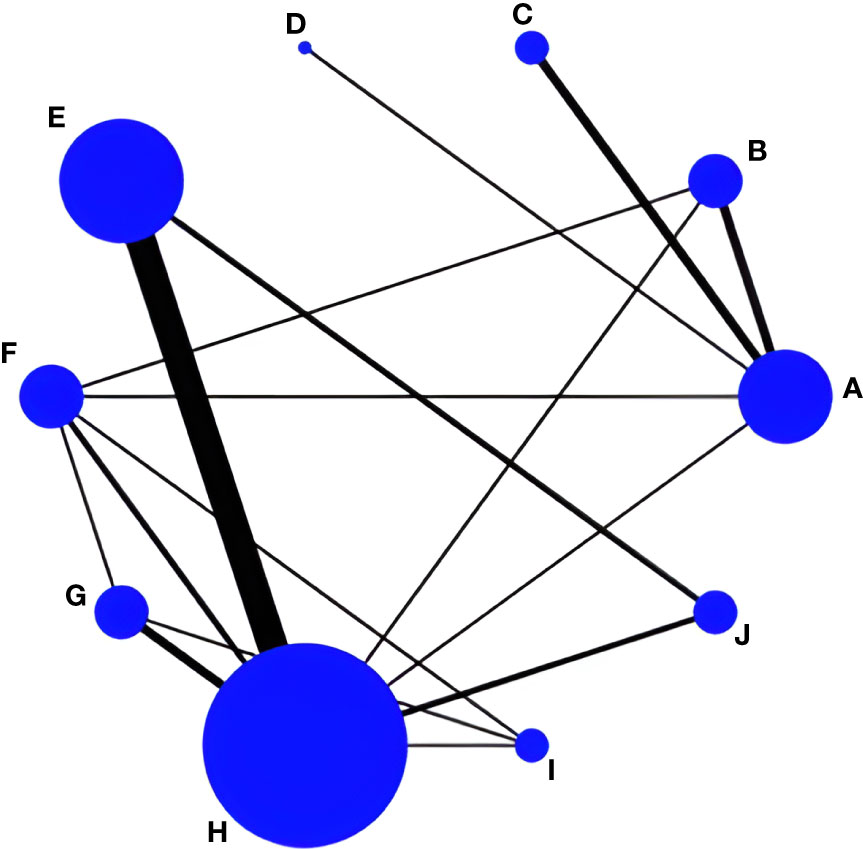
Figure 5 Network evidence for femoral neck BMD. (A) Drug group; (B) Baduanjin+Drug group; (C) Taiji+Drug group; (D) Wuqinxi+Drug group; (E) Taiji; (F) Baduanjin; (G) Wuqinxi; (H) Usual care; (I) Yujinjin; (J) Exercise training.
An indirect comparison between the two found that Taiji was superior to Yinjin (SMD= -0.07, 95% CI -0.12 to -0.05, p<0.05) and Wuqinxi (SMD= -0.07, 95% CI -0.13 to -0.04, p<0.05), but compared with Baduanjin and Baduanjin+drug, the Taiji+drug intervention effect was slightly worse. In addition, Baduanjin was superior to Taiji (SMD= 0.12, 95% CI 0.08 to 0.16, p<0.05) and Wuqinxi (SMD= -0.02, 95% CI -0.09 to -0.05, p<0.05), and the difference was statistically significant. Moreover, the Baduanjin+drug group (SMD= -0.14, 95%CI -0.23 to -0.05, p<0.01) was superior to the Baduanjin and the Taiji+drug group (SMD= -0.10, 95%CI -0.18 to -0.01, p<0.05), which was superior to Taiji (Table 7).
The final ranking using SUCRA was as follows (Figure 6): Baduanjin+drug (90.2%) > Baduanjin (89.9%) > Taiji+drug (84.5%) > drug (66.7%) > Taiji (51.3%) > Yijinjin (42.4%) > Wuqinxi+drug (39.4%) > exercise training (19%) > Wuqinxi (14.8%) > usual care (1.9%).
LI tests and a net meta-analysis of the included data showed IF values ranging from 0.01 to 0.10 and a lower 95% CI of 0, indicating no significant inconsistency across the closed loop analyses using the consistency model. Thirteen RCT studies reported changes in Ward’s triangle bone density before and after the intervention, amounting to 1324 subjects; one included drug therapy as the control group, and 12 had usual care as the control group, with a mesh relationship between the included studies (Figure 7).
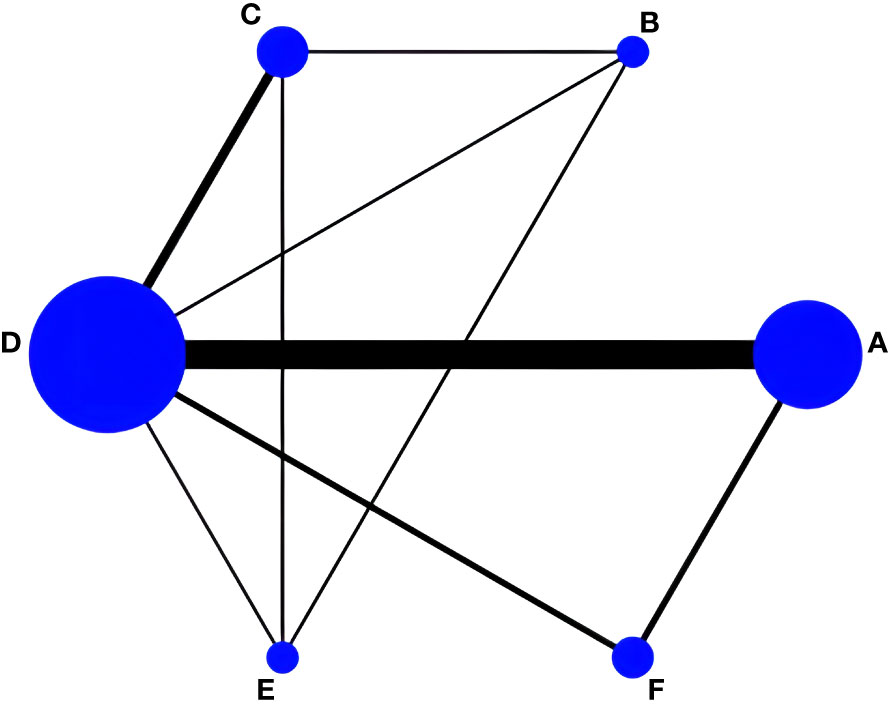
Figure 7 Network evidence for Ward’s triangle BMD. (A) Drug group; (B) Taiji+Drug group; (C) Taiji; (D) Baduanjin; (E) Wuqinxi; (F) Usual care.
Of the six pairwise comparisons produced in the reticulated network analysis (Table 8), they were not statistically significantly different from the Taiji+drug group (SMD= -0.01,95%CI -0.06 to 0.04, p >0.05), Taiji (SMD= 0.02, 95%CI -0.01 to 0.05, p>0.05), and Wuqinxi (SMD= 0.03, 95%CI -0.04 to 0.09, p>0.05), but the drug group was superior to Baduanjin (SMD= 0.03, 95%CI 0.02 to 0.05, p<0.05). In addition, Taiji was superior to usual care (SMD= -0.06, 95%CI -0.13 to -0.03, p<0.05). In an indirect comparison, only Taiji was superior to Baduanjin (SMD= -0.02, 95% CI -0.04 to -0.01, p<0.05). The final SUCRA ranking was as follows (Figure 8): Taiji+drug (86%) > drug (68.7%) > Taiji (46.8%) > Baduanjin (41.2%) > Wuqinxi (39.8%) > usual care (15.5%).
To our knowledge, this article is the first to compare the effects of TCE (including drug treatment, usual care, exercise training, Taiji, Baduanjin, Wuqinxi, Yijinjin, and their combinations) on BMD in postmenopausal women by network analysis, using direct and indirect evidence to compare the effect of L-BMD, femoral neck BMD, and Ward’s triangle BMD in 33 randomized controlled trials (3658 postmenopausal women). The results showed that, compared with drug treatment, routine nursing, and exercise training, Taiji, Baduanjin, and Yijinjin can effectively prevent bone loss, and the effect of Wuqinxi needs to be further explored. Further, we distinguished between TCE and drug interventions to prevent the combined intervention from potentially exaggerating the impact of the intervention and causing bias in the experimental design.
In this study, all the traditional Chinese fitness exercise interventions improved the L-BMD status of postmenopausal women. Baduanjin+drug, Taiji+drug, Taiji, drug, and Yijinjin had better intervention effects. From the point of view of Chinese traditional fitness exercise alone (without combining their use with drugs), Taiji and Yijinjin achieved a more significant improvement in L-BMD and femoral neck BMD.
Many of the movements in Taiji required the subjects to adopt a semi-squatting posture, such as the Wild Horse Splitting Mane, Knee-Wrapping Reversing Stance, and Left and Right Ranging Sparrow’s Tail, etc. During the practice process, the subjects are required to adjust the stability of their body postures continuously. Moreover, when practicing, the subjects are required to sink their qi into the dantian and adopt abdominal breathing, which plays a role in exercising the core muscles of the torso, and long-term practice produces stress changes and increases bone mass of the lumbar spine (63), which in turn has a positive effect on L-BMD and femoral neck BMD. In Ward’s triangle BMD, Taiji+drug, drug, and Taiji were the optimal approaches for improving BMD symptoms in postmenopausal women, and this intervention was better than the control group, suggesting that Taiji has some muscle-strengthening effects. This finding was similar to previous studies by Zou, which showed that Taiji could improve L- BMD, femoral neck BMD, and Ward’s triangle BMD (18).
The effect of Yijinjing intervention was consistent with previous studies that concluded that Yijinjing was the best method for improving lumbar spine and femoral bone density via TCE (64). A previous study also showed that Yijinjing may be more beneficial for bone formation to improve BMD (65). A recent meta-analysis on osteoporosis in older people showed that, for femoral neck BMD and L-BMD, Yijinjing was better than Baduanjin and Wuqinxi, which yielded results of 0.02-0.05 g/cm2 and 0.07-0.08 g/cm2 (15). This was because the practice of Yijinjing uses the torso to drive the limbs to complete stretching, spreading, retracting, and rotating movements, which leads to the bones, muscles, ligaments, and joints moving from multiple angles, increasing the stimulation of the bones and improving their metabolic capacity (64). Through static stretching of the muscles and synergistic movement of the joints, we can stretch the tendons and bones, improve microcirculation and muscle mobility, and increase the body’s potential for change, thus strengthening the spleen, kidneys, and blood, as well as the tendons and bones. Furthermore, studies have shown that the estradiol level in older women increases significantly after Yijinjing, which positively affects bone density (66). However, considering the small number of studies focused on Yijinjing, its effectiveness in improving BMD in postmenopausal women has yet to be confirmed. Therefore, future high-quality original studies or systematic evaluations of the above interventions are needed.
In this study we identified a novel phenomenon: the effect of Baduanjin combined with medication on postmenopausal women’s L-BMD and femoral neck BMD was highly effective. Previous meta-analyses did not identify this, and we believe that this is because postmenopausal women were considered in this study. Related research confirms our other view that long-term regular Baduanjin exercises combined with medication can alleviate the lower back pain caused by osteoporosis in postmenopausal women and improve bone density. This is because the loss of bone density in postmenopausal women occurs mainly due to a decrease in the level of hormones synthesized by the ovaries, which disrupts the equilibrium of bone metabolism in the patient’s body, with more bone resorption than bone formation, thus accelerating the rate of bone loss in the patient. Pharmacological treatment supplements the hormones or may utilize osteoclast-inhibiting drugs (e.g., calcitonin, vitamin D, aluminophosphates, and calcium supplements) (14, 67). For this reason, postmenopausal women who choose Baduanjin+drug as an intervention should follow it long-term to treat L-BMD and femoral neck BMD. However, Taiji is relatively backward in overall alignment in L-BMD and femoral neck BMD. Some studies have pointed out that Taiji’s foot movements are variable in direction, slower, and lighter, similar to “stirring the feet” and “pointing the ground with a false toe step”, and that the ground reaction force on the soles of the feet is low during Taijiquan practice (68). However, previous studies have pointed to a positive correlation between the load applied to the bone and bone density, with the maximum force significantly increasing bone density. Therefore, compared to the Baduanjin interventions, Taiji is slightly less effective in decreasing BMD loss in postmenopausal women.
However, it is worth noting that this study found no improvement effect of Baduanjin on L-BMD in direct and indirect comparisons. As a traditional Chinese medicine fitness qigong, Baduanjin has slow and gentle movements, mainly used to regulate qi and blood, dredge meridians and channels, and then restrict the body’s internal organs and meridians. The movement of the joints needs to combine qi regulation and static force to play a role in strengthening the bones (69). Our findings may have been related to the differences in the trial subjects, the duration of the trial intervention, and the frequency of practice of Baduanjin. From the three articles included, it was found that the length and frequency of the intervention were short, which may have contributed to the poor results for the Baduanjin intervention in L-BMD in postmenopausal women. In contrast to the L-BMD results, the Baduanjin intervention alone significantly affected femoral neck BMD. The reasons for this phenomenon may be that the intervention used was a modified version of Baduanjin, the eighth stance of which in traditional Baduanjin is known as the toe posture, which can stimulate the immune system and enhance osteogenesis through the vertical pressure generated by the body’s gravity. However, the modified eighth stance of Baduanjin adds two training movements, such as tiptoeing and clapping. When the heel is suddenly put down, combined with the palm clapping action, the ankle, knee, and femur joints will increase the body’s gravity, hitting the ground and creating a reaction force, which will lead to vibration. Secondly, fewer studies were included, and it is possible that further research will confirm its effectiveness in improving femoral neck BMD in postmenopausal women. Therefore, future high-quality original studies or systematic evaluations of the above interventions based are needed.
Wuqinxi had a particular mitigating effect on BMD in postmenopausal women, and this finding was similar to the findings in previous studies (38, 70). Some studies have concluded that in elderly patients, Wuqinxi significantly improves BMD and prevents POP fractures compared with control groups, as it can enhance the bone formation index, reduce the rate of bone resorption, and achieve a dynamic and positive balance between osteogenesis and osteoblast genesis (35).
Some scholars have also shown that when older women practiced Wuqinxi for 24 weeks, lumbar spine L2-4, greater trochanter, Ward’s triangle, and femoral neck BMD improved to varying degrees. While not statistically significant, the static and dynamic balance in the left and right directions were improved, and the risk of falling was reduced (33). The reasons for these findings may be related to the duration, frequency, and intensity of Wuqinxi practice and the small sample size. A previous study showed that the protective BMD effect was difficult to observe in a 12-week intervention trial, as the bone remodeling cycle usually takes at least 24 weeks (71). However, there has yet to be a longitudinal study to demonstrate the effect of long-term exercise on changes in bone mineral density in older adults over time. Therefore, the comparison between different durations suggests interesting future directions for exploring protective bone density loss, and further research is needed.
This study has several limitations: (1) although we used 11 electronic databases, they were limited to Chinese and English articles, which may have led to a specific language bias; (2) we did not include VAS and serum ALP, as the number of studies on VAS and serum ALP were insufficient for network analysis, which may have weakened the strength of the evidence; (3) most of the studies were assigned inappropriately and non-double-blinded to exaggerate the effects of the treatment; (4) most studies lacked follow-up information, resulting in incomplete data on the effectiveness and safety of treatment regimens; and (5) this study focused on TCE interventions and discussed mainly single exercise interventions, distinguishing between combined TCE and drug interventions to avoid exaggerating or reducing the degree of effect of these interventions, but it remains unclear by which mechanism the combination of TCE and different medications affects BMD. Given the limitations of this study, there is a need to objectify and standardize the study design in this field to support the development of more high-quality literature, such as large-scale, prospective, double-blind RCTs.
The results of the reticulated network analysis showed that all five traditional gong methods (Wuqinxi, Taiji, Baduanjin, Yijinjin, and Liuzijue) were effective in addressing BMD in postmenopausal women. The probability ranking showed that Taiji and Yijinjing alone have significant advantages, while Baduanjin still needs more studies to testify that it has substantial benefits if combined with medication. Therefore, Taiji or Baduanjin combined with medication may be preferred to effectively prevent and treat osteoporosis in postmenopausal women in clinical practice at this stage. However, the specific disease should be considered, along with the patient’s actual situation, to choose the patient’s recommended fitness qigong rationally and discriminatively.
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
SL: Conceptualization, Data curation, Resources, Visualization, Writing – original draft. SW: Data curation, Formal analysis, Methodology, Software, Writing – review & editing. JQ: Data curation, Software, Supervision, Validation, Writing – review & editing. LW: Data curation, Funding acquisition, Supervision, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by Fundamental Research Funds for the Central Universities (WUT: 2021VI034), the 2023 Undergraduate Teaching Reform Research Project of Wuhan University of Technology (W2023048), and the Fundamental Research Funds for the Central Universities (WUT: 2024IVA084).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2024.1323595/full#supplementary-material
1. Tella SH, Gallagher JC. Prevention and treatment of postmenopausal osteoporosis. J Steroid Biochem Mol Biol (2014) 6(142):155–70. doi: 10.1016/j.jsbmb.2013.09.008
2. Panel NI. Osteoporosis prevention, diagnosis, and therapy. JAMA (2001) 285(6):785–95. doi: 10.1001/jama.285.6.785
3. Silva I, Branco JC. Denosumab: recent update in postmenopausal osteoporosis. Acta Reumatolgica Portuguesa (2012) 37(4):302–13.
4. Sanchez-Rodriguez D, Bergmann P, Body JJ, Cavalier E, Gielen E, Goemaere S, et al. The Belgian bone club 2020 guidelines for the management of osteoporosis in postmenopausal women. Maturitas (2020) 139:69–89. doi: 10.1016/j.maturitas.2020.05.006
5. Dalal PK, Agarwal M. Postmenopausal syndrome. Indian J Psychiat (2015) 57:S222–32. doi: 10.4103/0019-5545.161483
6. Mornar M, Novak A, Bozic J. Quality of life in postmenopausal women with osteoporosis and osteopenia: associations with bone microarchitecture and nutritional status. Qual Life Res (2023) 32(2):1–20. doi: 10.1007/s11136-023-03542-7
7. Kanis JA, Norton N, Harvey NC. Scope 2021: A new scorecard for osteoporosis in Europe. Arch Osteoporos (2021) 16:82–9. doi: 10.1007/s11657-020-00871-9
8. David L, Nichols E. Bone health and osteoporosis. Clinics Sports Med (2000) 23(1):466–70. doi: 10.1016/S0278-5919(05)70201-5
9. Zolfaroli I, Ortiz E, Garcia-Perez M-A, Jose Hidalgo-Mora J, Tarin JJ, Cano A. Positive association of high-density lipoprotein cholesterol with lumbar and femoral neck bone mineral density in postmenopausal women. Maturitas (2021) 147:41–6. doi: 10.1016/j.maturitas.2021.03.001
10. Zhang SF, Huang XX, Zhao XR. Effect of exercise on bone mineral density among patients with osteoporosis and osteopenia: A systematic review and network meta-analysis. J Clin Nurs (2021) 31(15):2100–11. doi: 10.1111/jocn.16101
11. Kanis JA, Cooper C, Rizzoli R, R JY. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int (2019) 30(1):3–44. doi: 10.1007/s00198-018-4704-5
12. Center JR, Bliuc D, Nguyen ND, Nguyen TV, Eisman JA. Osteoporosis medication and reduced mortality risk in elderly women and men. J Clin Endocrinol Metab (2011) 96(4):1006–14. doi: 10.1210/jc.2010-2730
13. Zhang YJ, Loprinzi PD, Yang L. The beneficial effects of traditional Chinese exercises for adults with low back pain: A meta-analysis of randomized controlled trials. Medicina (2019) 55(5):118. doi: 10.3390/medicina55050118
14. Liu J, Wu WZ, Xu DM. Clinical research progress of traditional exercises in the treatment of primary osteoporosis. Chin J Osteoporosis (2019) 25(12):1817–20. doi: 10.3969/j.issn.1006−7108
15. Li YJ, Niu XR, Hu S. Efficacy evaluation of different forms of traditional Chinese health-preservation exercises for osteoporosis: A network meta-analysis. J Acupunct Tuina Sci (2021) 19(4):258–70. doi: 10.1007/s11726-021-1256-6
16. Zou LY, Wang CY. Baduanjin exercise for stroke rehabilitation: A systematic review with meta-analysis of randomized controlled trials. Int J Environ Res Public Health (2018) 15(1):322–42. doi: 10.3390/ijerph15040600
17. Zou L, Zhang Y, Liu Y, Tian X, Xiao T, Liu X, et al. The effects of Tai Chi Chuan versus core stability training on lower-limb neuromuscular function in aging individuals with non-specific chronic lower back pain. Medicina (2019) 55(3):345–75. doi: 10.3390/medicina55030060
18. Zou L, Han J, Li C, Yeung AS, Hui SC, Tsang WWN, et al. The effects of tai chi on lower limb proprioception in adults aged over 55: A systematic review and meta-analysis article type: systematic/meta-analytic reviews. Arch Phys Med Rehabil (2018) 16(7):168–83. doi: 10.1016/j.apmr.2018.07.425
19. Wei X, Xu A, Yin Y, Zhang R. The potential effect of Wuqinxi exercise for primary osteoporosis: A systematic review and meta-analysis. Maturitas (2015) 82(4):346–54. doi: 10.1016/j.maturitas.2015.08.013
20. Pan YR, Wang MD. The influence of Taijiquan on bone mineral density of natural menopausal women. Sichuan Sports Sci (2021) 40(6):26–30+61. doi: 10.13932/j.cnki.sctykx
21. Varahra I. Exercise to improve functional outcomes in persons with osteoporosis: A systematic review and meta-analysis. Osteoporosis Int (2018) 29(2):265–86. doi: 10.1007/s00198-017-4339-y
22. Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M. Preferred reporting items for systematic review and meta-analysis protocols (Prisma-P) 2015: elaboration and explanation. Bmj-British Med J (2015) 349(21):489–99. doi: 10.1136/bmj.g7647
23. Bangshi X, Jinhua W. Kappa consistency test in test medicine research. Chin J Lab Med (2006) 1(1):83–4. doi: 10.3760/j:issn:1009-9158.2006.01.030
24. Cai YX, Li XL, Zhao JJ. A clinical observation on prevention of postmenopausal osteoporosis in 30 cases with Baduanjin combined with Calcine D. Chin Ethnic Folk Med (2018) 27(23):130–2. doi: 10.19664/j.cnki.1002-2392.180090
25. Chen C. Effects of exercise therapy on bone density, lean body weight and fat content in postmenopausal osteoporosis. Nanjing Univ Chin Med (2016) 32:42–8.
26. Su JH, Deng Q. Clinical study of baduanjin combined with anti osteoporosis drugs in the treatment of postmenopausal osteoporosis. J Traditional Chin Med (2018) 46(3):84–8. doi: 10.19664/j.cnki.1002-2392.180090
27. Cheng L, Lei Y, Hu Y, Kang KL, Wang XY. Effect of Baduan Jin exercise on bone mineral density in community perimenopausal women. Chin foreign Med Res (2017) 15(1):135–7. doi: 10.14033/j.cnki.cfmr.2017.1.076
28. Peng RD, Deng Q. The effect of Baduanjin on glucose and bone metabolism indicators in postmenopausal type 2 diabetes patients with osteoporosis. J Traditional Chin Med (2019) 25(23):53–6. doi: 10.13862/j.cnki.cn43-1446/r.2019.23.013
29. Zhou Y. Effect of traditional sports on bone mineral density of menopausal women. J Beijing Sport Univ (2014) 3(1):354–5+60. doi: 10.19582/j.cnki.11-3785/g8.2014.03.024
30. Dan X, Kang JW. Effects of Taijiquan in the adjuvant therapy of postmenopausal osteoporosis. Chin J modern Nurs (2015) 21(31):3729–31. doi: 10.3760/cma.j.issn.1674-2907.2015.31.003
31. Liu BX, Chen SP, Li YD, Wang J, Zhang B, Lin Y, et al. The effect of the modified eighth section of eight-section brocade on osteoporosis in postmenopausal women: A prospective randomized trial. Medicine (2015) 94(25):e991. doi: 10.1097/MD.0000000000000991
32. Chen WL, Mao YF, Zhang JF, Liu Z, Xiao WL. Observation on the clinical efficacy of Yiqi Wenjing prescription in combination with the newly compiled Wuqinxi on postmenopausal patients with bone loss. Chin J Osteoporosis (2018) 24(7):954–8. doi: 10.3969/j.issn.1006-7108
33. Wang FH, Zhang JM, Xu HX. The influence of the newly compiled Wuqinxi exercise on the balance ability and bone density of elderly women. China J Osteoporosis (2018) 24(12):1577–81. doi: 10.3969/j.issn.1006-7108
34. Li JW, Pan DQ, He KH, Shi XL. Improved Wuqinxi I Prevention and treatment of primary osteoporosis clinical application experience. Chin J osteoporosis (2014) 20(8):920–3. doi: 10.3969/j.issn.1006-7108
35. Shen MR, Feng YJ, Wang T. Effect of Wuqin exercise on lumbar vertebra density in postmenopausal women. J integrated traditional Chin western Med (2012) 22(8):804–5+20. doi: 10.3969/j.issn.1006-7108
36. Gu L, Liu Y. The effect of the new Wuqinxi on bone mineral density of elderly women. Chin J Gerontology (2021) 41(1):79–82. doi: 10.3969/j.issn.1005-9202
37. Shi ZY, Liu Z, Chen WL. Multi-center clinical study on the prevention and treatment of postmenopausal bone mass reduction by integrated therapy of traditional Chinese medicine. Chin Bone setting (2017) 29(4):1–7. doi: 10.3969/j.issn.1006-7108.2017.07.017
38. Li J. Effects of three exercises on bone density in elderly women. Chin J osteoporosis (2019) 25(3):339–42+50. doi: 10.3969/j.issn.1006-7108
39. Miao FS, Wang M. Effect of fitness qigong on bone density and bone metabolism in postmenopausal women. J jilin Phys Educ Univ (2012) 28(3):107–9. doi: 10.21203/rs.2.23049/v1
40. Kuo LT, Hsu RWW, Hsu WH, R. LZ. The comparison of impact of circuit exercise training and Tai-Chi exercise on multiple fracture-related risk factors in postmenopausal osteopenic women. J Clin Densitometry (2014) 17(1):427–8. doi: 10.1016/j.jocd.2014.04.102
41. Liu SF, Huang SY. An analysis of the effect of Taijiquan combined with resistance training on bone mineral density in women aged 55-60 years. J Anyang Normal Univ (2019) 23(3):82–6. doi: 10.16140/j.cnki.1671-5330.2019.05.021
42. Liu CJ, Liu G. Effects of regular taijiquan exercise on serum lipids, leptin levels and bone mineral density in retired women. Liaoning sports Sci Technol (2014) 36(3):55–8. doi: 10.13940/j.cnki.lntykj.2014.03.019
43. Mao HN. Effect of Taijiquan combined with calcium supplement on bone mineral density in postmenopausal women. Chin J Rehabil Med (2009) 24(9):814–6.
44. Song JL, Cheng L, Chang SW. Effects of 48-week shadowboxing, brisk walking and square dancing on bone density in elderly women. J Shandong Institute Phys Educ (2018) 34(6):105–8. doi: 10.14104/j.cnki.1006-2076.2018.06.018
45. Xu F. Effect of 24 style simplified Taijiquan on bone mineral density in postmenopausal women. J Pract Chin Med (2017) 33(12):1428–9.
46. Ye CQ, Wang CW, Wang GY. The influence of Taijiquan on the health status of middle-aged and old women. Chin J Health Med (2016) 18(6):494–5. doi: 10.3969/.issn.1674-3245.2016.06.022
47. Yu DH, Wang HR, Xie YL. Effects of Tai Chi calisthenics on bone mineral density in postmenopausal women. J Shanghai institute Phys Educ (2014) 38(6):100–4. doi: 10.16099/j.cnki.jsus.2014.06.019
48. Zhao J, Cheng L. Effects of different types of long-term exercise on bone mineral density in elderly women. Chin J osteoporosis (2020) 26(1):50–3. doi: 10.3969/j.issn.1006-7108
49. Zhao MY, Li N, Fan C, Yuan SH. Influence of Tai Chi push-hand exercise combined with nutritional intervention on rehabilitation of patients with primary osteoporosis. Liaoning sports Sci Technol (2015) 37(3):44–6. doi: 10.13940/j.cnki.lntykj.2015.03.013
50. Zhou Y. LIJ, Chen YB, Jia JY. Effects of Tai Chi push-hand exercise and calcium supplementation on bone mineral density in postmenopausal women. Chin J Sports Med (2015) 2(1):106–8. doi: 10.13940/j.cnki.lntykj.2015.03.013
51. Chan KM, Qin L, Lau MC, Woo J, Au S, Choy WY, et al. A randomized, prospective study of the effects of Tai Chi Chun exercise on bone mineral density in postmenopausal women. Arch Phys Med Rehabil (2004) 85(5):717–22. doi: 10.1016/j.apmr.2003.08.091
52. Wayne PM, Kiel DP, Buring JE, Connors EM, Davis RB. Impact of Tai Chi exercise on multiple fracture-related risk factors in post-menopausal osteopenic women: A pilot pragmatic, randomized trial. BMC Complementary Altern Med (2012) 12(1):7. doi: 10.1186/1472-6882-12-7
53. Wang HR, Yu B, Chen WH. Simplified Tai Chi resistance training versus traditional Tai Chi in slowing bone loss in postmenopausal women. Evidence-Based Complementray Altern Med (2015) 2015(2):1–6. doi: 10.1155/2015/379451
54. Liu GL, Liu XQ. The influence of Taijiquan exercise on bone mineral density and bone metabolism indicators of postmenopausal women. Contemp Sports Sci Technol (2021) 11(24):19–21. doi: 10.16655/j.cnki.2095-2813.2012-1579-1245
55. Li KQ, Yu HG, Lin XJ. The effects of Er Xian decoction combined with Baduanjin exercise on bone mineral density, lower limb balance function, and mental health in women with postmenopausal osteoporosis: A randomized controlled trial. Evidence-Based Complementary Altern Med (2022) 2022(1):13. doi: 10.1155/2022/8602753
56. Salanti G, Ades AE. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol (2011) 64(2):163. doi: 10.1016/j.jclinepi.2010.03.016
57. Hutton B, Salanti G, Caldwell DM. The prisma extension statement for reporting of systematic reviews inCorporating network meta-analyses of health care interventions: checklist and explanations. Ann Internal Med (2015) 162(11):777. doi: 10.7326/M14-2385
58. Zhang C, Yan JZ, Sun F. Methods for identification and treatment of consistency of reticular meta-analysis. Chin J Evidence Based Med (2014) 14(7):884. doi: 10.7507/1672-2531.20140146
59. Liu SJ, Yu Q, Li ZM, Cunha PM, Zhang Y, Kong ZW, et al. Effects of acute and chronic exercises on executive function in children and adolescents: A systemic review and meta-analysis. Front Psychol (2020) 11:554915. doi: 10.3389/fpsyg.2020.554915
60. Du XL, Zhao XH. Clinical observation on the improvement of osteoporosis symptoms in postmenopausal women with traditional Chinese medicine combined with Eight Duan Jingong. Chin Health standards Manage (2014) 5(5):65–8. doi: 10.3969/J.ISSN.1674-9316.2014.05.038
61. Sun W, Wang JN, Yang CR. A follow-up study on the effects of Taijiquan and fast walking exercise on bone density and bone metabolism in elderly women. Chin J osteoporosis (2017) 23(8):1034–40. doi: 10.3969/j.issn.1006-7108
62. Furuya-Kanamori L, Barendregt JJ, Doi SA. A new improved graphical and quantitative method for detecting bias in meta-analysis. J Int J Evid Based Healthc (2018) 53:1–23. doi: 10.1097/XEB.0000000000000141
63. Li JY, Cheng L. Effects of tai chi exercise with different frequencies on bone mineral density in elderly women for 48 weeks. Chin J Osteoporosis (2017) 23(10):1309–12. doi: 10.3969/j.issn.1006-7108.2017.10.010
64. Yu Y. Net meta-analysis of four traditional Chinese fitness exercise therapy on osteoporosis in middle-aged and elderly people. China sports Sci Technol (2020) 56(9):37–44. doi: 10.16470/j.csst.2020115
65. Jing FJ, Z J. Effect of tendon changing exercise on bone mineral density of patients with primary osteoporosis. China Sports Sci Technol (2008) 1(2):88–90+102. doi: 10.16470/j.csst.2008.02.002
66. Robinson JA, Riggs BL, Spelsberg TC. Osteoclasts and transforming growth factor-beta: estrogen-mediated inform-specific regulation of production. Endocrinology (1996) 137(2):615–21. doi: 10.1210/ENDO.137.2.8593810
67. Chen J. Clinical observation on the improvement of postmenopausal women’s osteoporosis symptoms with traditional Chinese medicine diet and Baduanjingong. Asia Pacific Traditional Med (2015) 11(7):104–5. doi: 10.1089/jwh.2017.6706
68. Mao DW, Li JX, Hong Y. The duration and plantar pressure distribution during one-leg stance in Tai Chi exercise. Clin biomechanics (Bristol Avon) (2008) 21(6):640–5. doi: 10.1016/J.CLINBIOMECH.2006.01.008
69. Li H, Ge D, Liu S, Zhang W, Wang J, Si J, et al. Baduanjin exercise for low back pain: A systematic review and meta-analysis. Complementary Therapies Med (2019) 43:109–16. doi: 10.1016/j.ctim.2019.01.021
70. Wang XW, Chen GQ. Research progress of traditional health and modern sports in prevention and treatment of primary osteoporosis. Int J Geriatr (2022) 43(6):755–8.
Keywords: traditional Chinese fitness exercises, BMD, network meta-analysis, postmenopausal, women
Citation: Liu S, Wu S, Qi J and Wang L (2024) Effect of traditional Chinese fitness exercises on bone mineral density in postmenopausal women: a network meta-analysis of randomized controlled trials. Front. Endocrinol. 15:1323595. doi: 10.3389/fendo.2024.1323595
Received: 18 October 2023; Accepted: 15 January 2024;
Published: 06 February 2024.
Edited by:
Katherine A. Staines, University of Brighton, United KingdomReviewed by:
Lifei Liu, The People’s Hospital of Liaoning Province, ChinaCopyright © 2024 Liu, Wu, Qi and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lin Wang, d2FuZ2xpbjEyM0AxMjYuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.