
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Endocrinol., 05 December 2023
Sec. Thyroid Endocrinology
Volume 14 - 2023 | https://doi.org/10.3389/fendo.2023.1276992
This article is part of the Research TopicParathyroid Disorders: Updates of PTH / Serum Ca2+ Regulation and Therapeutic ProspectsView all 6 articles
 Yongliang Mu1†
Yongliang Mu1† Yishen Zhao1†
Yishen Zhao1† Jiannan Zhao2
Jiannan Zhao2 Qi Zhao1
Qi Zhao1 Yushuai Zhang1
Yushuai Zhang1 Yang Li1
Yang Li1 Jiedong Kou1
Jiedong Kou1 Gianlorenzo Dionigi3
Gianlorenzo Dionigi3 Xuehai Bian1*
Xuehai Bian1* Hui Sun1*
Hui Sun1*Background: Parathyroidectomy (PTX) is an effective treatment for primary hyperparathyroidism (PHPT) patients. Postoperative hypocalcemia is a common complication after PTX. This study aimed to analyze the factors influencing serum calcium levels and the incidence of hypocalcemia after parathyroidectomy in primary hyperparathyroidism patients.
Methods: The retrospective study included 270 PHPT patients treated with PTX and collected their demographic and clinical information and their laboratory indices. Factors influencing serum calcium levels and hypocalcemia after PTX in PHPT patients were analyzed using univariate and multifactorial analyses.
Results: First, in patients with normal preoperative serum calcium levels (2.20–2.74 mmol/L), the higher the preoperative alkaline phosphatase and serum phosphorus levels, the lower the postoperative serum calcium levels. Furthermore, the higher the preoperative serum calcium levels and the accompanying clinical symptoms, the higher the postoperative serum calcium levels. Low preoperative serum calcium levels were shown to be a risk factor for postoperative hypocalcemia (OR=0.022), and the optimal preoperative serum calcium threshold was 2.625 mmol/L (sensitivity and specificity were 0.587 and 0.712, respectively). Second, in the mild preoperative hypercalcemia group (2.75-3.00 mmol/L), the older the patient, the higher the preoperative and postoperative serum calcium levels, the higher the postoperative serum calcium; the lower the alkaline phosphatase and calcitonin levels, the higher the postoperative serum calcium levels. On the other hand, the younger the patient was, the more likely hypocalcemia blood was (OR=0.947), with an optimal age threshold of 47.5 years (sensitivity and specificity were 0.543 and 0.754, respectively). Third, in the preoperative moderate to severe hypercalcemia group (>3.0mmol/L), patients undergoing a combined contralateral thyroidectomy and a total thyroidectomy had low postoperative serum calcium levels.
Conclusion: Patients with different preoperative serum calcium levels had various factors influencing their postoperative serum calcium levels and postoperative hypocalcemia, which facilitated the assessment of their prognosis.
Primary hyperparathyroidism (PHPT) is a disease of the parathyroid glands, in which they produce excessive amounts of parathyroid hormone (PTH). Such excess results in elevated levels of serum calcium and decreased levels of serum phosphorus. Some patients experience bone pain, arthralgia, symptoms associated with urinary tract stones, and others (1). Parathyroidectomy (PTX) is the treatment of choice for PHPT (2). Hypocalcemia is a common postoperative complication in patients with PHPT. Severe hypocalcemia (including hypoparathyroidism and bone starvation syndrome) can cause muscle spasms in the hands and feet, cardiac arrhythmias, epilepsy, and even life-threatening symptoms (3, 4). The occurrence of these symptoms is the result of a rapid decline in PTH levels after surgery, after a long period of high PTH levels in PHPT (5). Vitamin D deficiency in preoperative patients leads to an increased probability of postoperative hypocalcemia (6).
Several studies have shown that the incidence of postoperative hypocalcemia after PHPT ranges from 4.1% to 21.3% (7–9), which shows that patients are at high risk of postoperative hypocalcemia. In order to effectively prevent and timely respond to the occurrence of postoperative hypocalcemia in PHPT patients, several research institutions have conducted research and concluded that the age, the preoperative alkaline phosphatase levels, and the preoperative blood calcium levels are related to postoperative hypocalcemia (10–12). With the introduction of routine serum calcium monitoring in several countries around the world, fewer patients with clinically significant primary hyperparathyroidism and moderate to severe preoperative serum calcium levels have been identified. Furthermore, increased numbers of patients with PHPT who are asymptomatic (or less symptomatic) and have normal or mildly hypercalcemic preoperative calcium have been diagnosed (13, 14). This phenomenon indicates that the preoperative serum calcium levels may represent a different disease stage in PHPT patients. However, no studies have stratified the factors influencing the patients’ postoperative serum calcium levels and hypocalcemia according to their preoperative serum calcium levels. Therefore, in this study, we collected clinical data from patients treated with PTX at the China–Japan Union Hospital of Jilin University (Changchun, Jilin, China). We performed a stratified analysis of the factors influencing the postoperative serum calcium levels and hypocalcemia in these patients, to investigate whether they were clinical or biochemical predictors. Our aim was to estimate the probability of postoperative hypocalcemia and to provide a more timely and effective postoperative management.
A total of 270 PHPT patients who underwent PTX at the Department of Thyroid Surgery, China–Japan Union Hospital of Jilin University (Changchun, Jilin, China), from June 2008 to October 2022 were enrolled in the present study. Participants included 157 patients who underwent parathyroidectomy and 113 patients who underwent parathyroidectomy combined with thyroidectomy (which was also combined with ipsilateral thyroidectomy, contralateral thyroidectomy, and total thyroidectomy).
In this study, the variables analyzed were sex, age, Body Mass Index (BMI), the preoperative presence or absence of clinical symptoms, the preoperative and postoperative serum calcium levels, the preoperative serum phosphorus and PTH levels, the intraoperative levels of PTH, alkaline phosphatase, and calcitonin, and the operator, surgical procedure (either non-combined thyroidectomy or combined thyroidectomy), the postoperative paraffin pathology, the number of diseased paracrine glands (either single or multiple), and the location of the diseased parathyroid glands (either superior or inferior).
The postoperative serum calcium levels were defined on the first postoperative day. The intraoperative PTH levels were defined 30 min after the intraoperative removal of the diseased parathyroid gland. Clinical symptoms included bone pain, arthralgia, urinary stones, malignancy, vomiting, and depression. Hypocalcemia was determined as a minimum postoperative serum calcium value of <2.2 mmol/L.
The inclusion criteria were the following (1): patients surgically treated for PHPT and confirmed by postoperative pathology (2), patients with complete clinical data, and (3)≥ 18 years old patients.
The exclusion criteria were as follows (1): patients with combined severe renal insufficiency (2), patients with secondary and tertiary hyperparathyroidism, and (3) patients with incomplete clinical information.
According to their preoperative serum calcium values, all patients were divided into a preoperative normal serum calcium group (A group, 2.20–2.74 mmol/L), a preoperative mild hypercalcemia group (B group, 2.75–3.00 mmol/L), and a preoperative moderate to severe hypercalcemia group (C group, serum calcium ≥3.00 mmol/L) (4, 15).
On the day after surgery, patients are empirically supplemented with intravenous calcium gluconate. On the day after simple parathyroidectomy, patients received 3 g of intravenous calcium supplementation, which was adjusted on the first postoperative day, based on the intraoperative PTH and serum calcium values. The principle of calcium supplementation in patients with combined parathyroidectomy was the same; however, empirically, patients with combined thyroidectomy tended to have a more decreased parathyroid function. Therefore, the starting dosage of calcium supplementation was higher than in patients with simple parathyroidectomy. In summary, the overall calcium supplementation profile was empirically determined on the day of surgery and on the first postoperative day, being based on the intraoperative PTH and serum calcium levels. If the serum calcium levels were >2.2 mmol/L and no symptoms of hypocalcemia were diagnosed, the amount of intravenous calcium supplementation was reduced as appropriate.
Our center defines the parathyroid decline rate as the difference between preoperative PTH and intraoperative PTH levels, expressed as a percentage of preoperative PTH. Intraoperative PTH levels were measured by collecting venous blood 30 min after the intraoperative removal of the diseased parathyroid glands. The parathyroid hormone levels were measured in pg/mL. Laboratory tests included the levels of serum calcium (Ca; reference range, 2.00–2.60 mmol/L), serum phosphate (P; reference range, 0.81–1.45 mmol/L), alkaline phosphatase (ALP; reference range, 30.00–120.00 IU/L), and serum calcitonin (Cal; reference range, 0.50–6.00 pg/ml).
Statistical analysis was performed using the SPSS 27.0 software (IBM, Armonk, NY, USA). Statistics were expressed as the arithmetic mean standard deviation for continuous variables or the frequency and percentage (%) for categorical variables. The Kruskal–Wallis rank sum test was utilized to compare continuous variables, while the Pearson chi-square test was used for categorical variables. For single-factor analysis, Pearson product-difference correlation coefficients were used when all variables were continuous; chi-square coefficients were used when all variables were categorical. Spearman correlation coefficients were used when the variables were both ranked and continuous. For multifactor analysis, linear regression analysis was employed for the factors influencing the postoperative serum calcium levels. A binary logistic regression analysis was used for factors influencing postoperative hypocalcemia. A p<0.05 was regarded as statistically significant. Based on the binary logistic regression analysis, statistically significant variables were selected to investigate their predictive efficacy for hypocalcemia. A receiver operating characteristic curve (ROC) was established to determine the cutoff value, sensitivity, and specificity of statistically significant factors.
In this study, patients were divided into the preoperative normal serum calcium group, preoperative mild hypercalcemia group, and the preoperative moderate to severe hypercalcemia group. There were seven patients in the preoperative severe hypercalcemia group, who were incorporated into the preoperative moderate hypercalcemia group. The preoperative mild hypercalcemia group had the highest number of patients (104 patients, 38.5%), and the preoperative moderate to severe serum calcium group had the lowest number of patients (76 patients, 28.1%). The preoperative normal hypercalcemia group had the highest number of patients with postoperative hypocalcemia (58.9%) and the lowest number of patients with preoperative clinical symptoms (37.8%). The preoperative moderate to severe hypercalcemia group had a lower percentage of patients with postoperative hypocalcemia (22.4%) than the other two groups and also the highest rate of patients with preoperative clinical symptoms (61.8%). In all three patient groups, skeletal system symptoms were the most common (22.2%) of the preoperative concomitant clinical symptoms (Table 1).
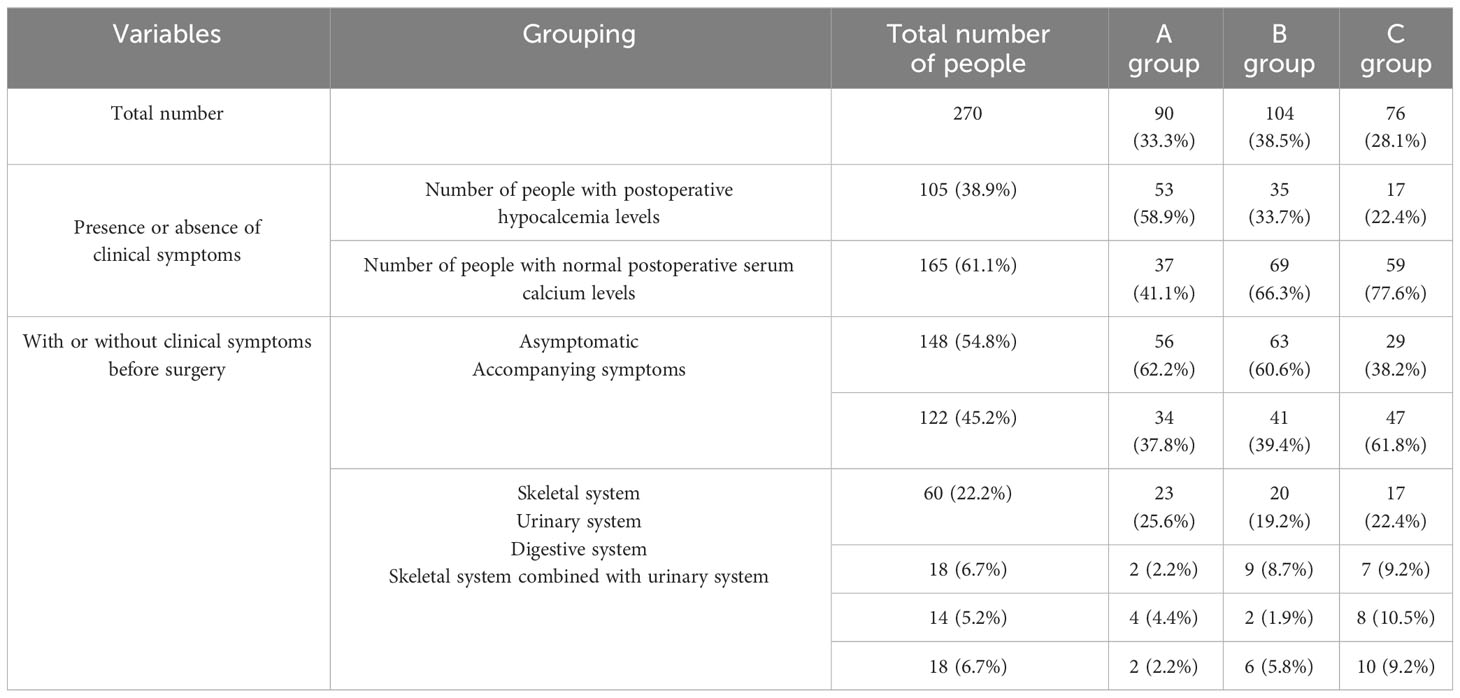
Table 1 Distribution of the number of patients with postoperative serum calcium levels, preoperative serum calcium levels, and clinical symptoms.
There were statistically significant differences (p<0.05) among the three groups concerning the preoperative and postoperative serum calcium levels, the decline rate in serum calcium levels, the preoperative serum phosphorus and alkaline phosphatase levels, the preoperative and intraoperative PTH levels, the decrease rate in PTH, and calcitonin levels (Table 2). The differences in demographic characteristics, preoperative clinical symptoms, and laboratory parameters among the three groups of patients required their division into groups.
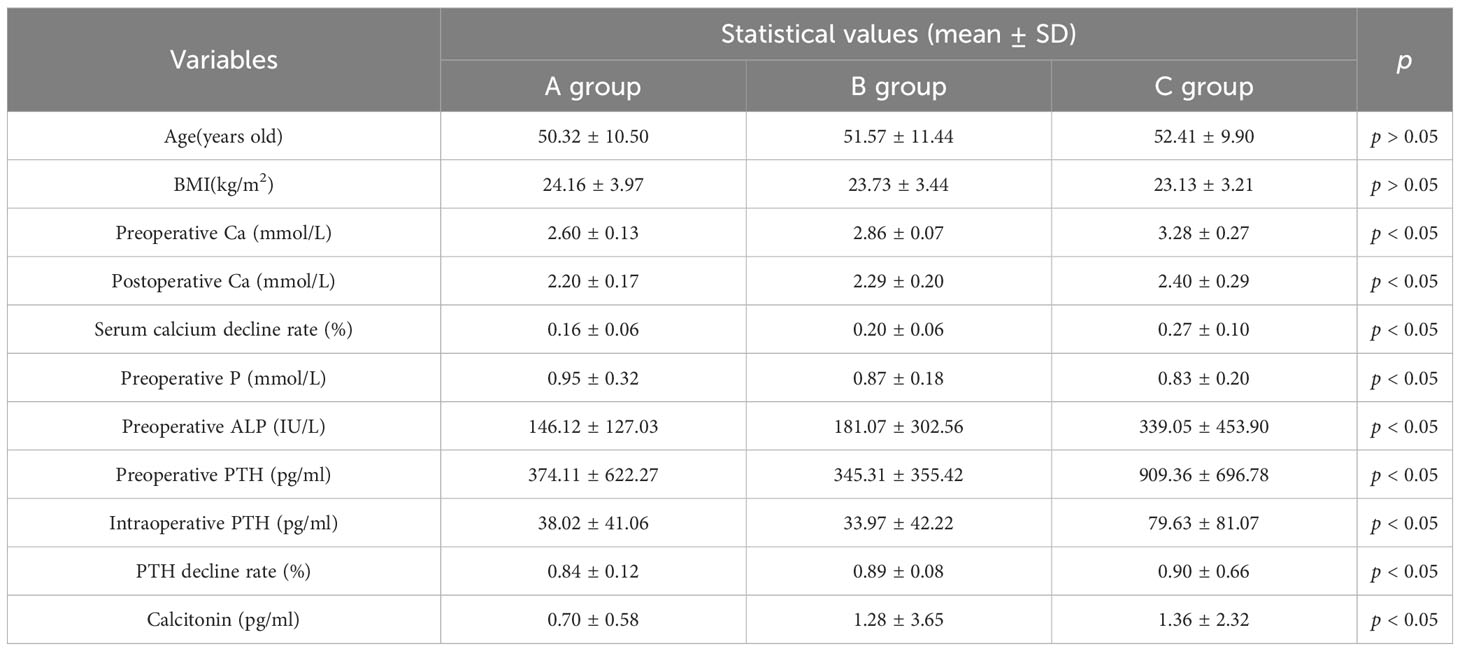
Table 2 Basic information and statistical values of laboratory indicators for the three groups of patients.
The incidence of postoperative hypocalcemia was higher in patients with combined thyroidectomy (p=0.041; Table 3).
In this study, there were more female (75.9%) than male (24.1%) participants. More patients had a single-lesion parathyroidectomy (96.7%) than multiple-lesion parathyroidectomies (3.3%). Most patients (79.6%) had a parathyroid lesion located in the inferior thyroid gland. Of the patients, 41.9% had a parathyroidectomy combined with a thyroidectomy (Table 4).
In this study, 14 factors were selected, which could influence the postoperative serum calcium levels in patients with primary hyperparathyroidism. These factors included the gender, age, BMI, presence of clinical symptoms before surgery, the preoperative serum calcium, serum phosphorus, and PTH levels; the intraoperative PTH, alkaline phosphatase, and calcitonin levels; the operator, the surgical procedure; and the number and location of diseased parathyroid glands. A value of 1 was assigned to male and 0 to female participants. A value of 0 was assigned to a single diseased parathyroid gland and 1 to multiple diseased parathyroid glands. A value of 1 was assigned to the superior and 2 to the inferior location of diseased parathyroid glands. A value of 1 was assigned to combined thyroidectomy and 0 to non-combined thyroidectomy. A value of 1 was assigned to the presence of preoperative clinical symptoms and 0 to their absence.
Correlation analysis showed that the alkaline phosphatase (r=−0.240), preoperative PTH (r=−0.318), and the preoperative serum phosphorus (r=−0.258) levels were all negatively correlated with the postoperative serum calcium levels. These parameters were combined with low postoperative serum calcium levels in patients undergoing thyroidectomy (r=−0.242), preoperative serum calcium levels (r=0.369), patients having preoperative clinical symptoms (r=0.296), and postoperative serum calcium levels, which were positively correlated (Table 5).
Furthermore, statistically significant factors were selected for regression analysis. In the patient group with normal preoperative serum calcium levels, higher alkaline phosphatase and preoperative serum phosphorus levels were associated with lower postoperative serum calcium levels. Patients with high preoperative serum calcium levels and clinical symptoms were associated with higher postoperative serum calcium levels (Table 6). The regression model was expressed as postoperative serum calcium levels = 1.212 − 0.0004 × alkaline phosphatase levels + 0.423 × preoperative serum calcium levels − 0.102× preoperative serum phosphorus levels + 0.091× presence or absence of clinical symptoms.
Correlation analysis revealed that the alkaline phosphatase levels (r=−0.326), the preoperative levels of PTH (r=−0.234), and calcitonin (r=-0.204) were all negatively correlated with the preoperative and postoperative serum calcium levels (r=0.310) and the age (r=0.333), which were positively correlated with the postoperative serum calcium levels (Table 5).
Regression analysis of selected statistically significant factors revealed that older age and higher preoperative serum calcium levels were associated with higher postoperative serum calcium levels. Lower alkaline phosphatase and calcitonin levels were associated with higher postoperative serum calcium levels (Table 6). The regression model used was the follows: postoperative serum calcium levels = 0.831 × preoperative serum calcium levels − 0.0002 × alkaline phosphatase levels − 0.010 × calcitonin levels.
Correlation analysis revealed that a combined thyroidectomy was negatively associated with the postoperative serum calcium levels (r=−0.340), while other variables were not statistically significant (Table 5).
Regression analysis revealed that the postoperative serum calcium levels were low in patients with combined contralateral and total thyroidectomy (Table 6).
A value of 1 was assigned to the occurrence of postoperative hypocalcemia and 0 to the absence of postoperative hypocalcemia. Correlation analysis showed that the preoperative serum calcium levels were negatively correlated with postoperative hypocalcemia (r=−0.221), while other variables were not statistically significant (Table 7).
Regression analysis revealed that the lower the preoperative serum calcium levels, the more likely hypocalcemia would occur postoperatively (OR=0.022) (Table 8). ROC curves were produced to further investigate the efficacy of the preoperative serum calcium levels in predicting the occurrence of hypocalcemia in this group (Figure 1A). The results showed a statistically significant AUC=0.629 and p=0.038 at a preoperative serum calcium level of 2.625 mmol/L. The sensitivity and specificity at this point were 0.587 and 0.712, respectively (Table 9), which had predictive values.
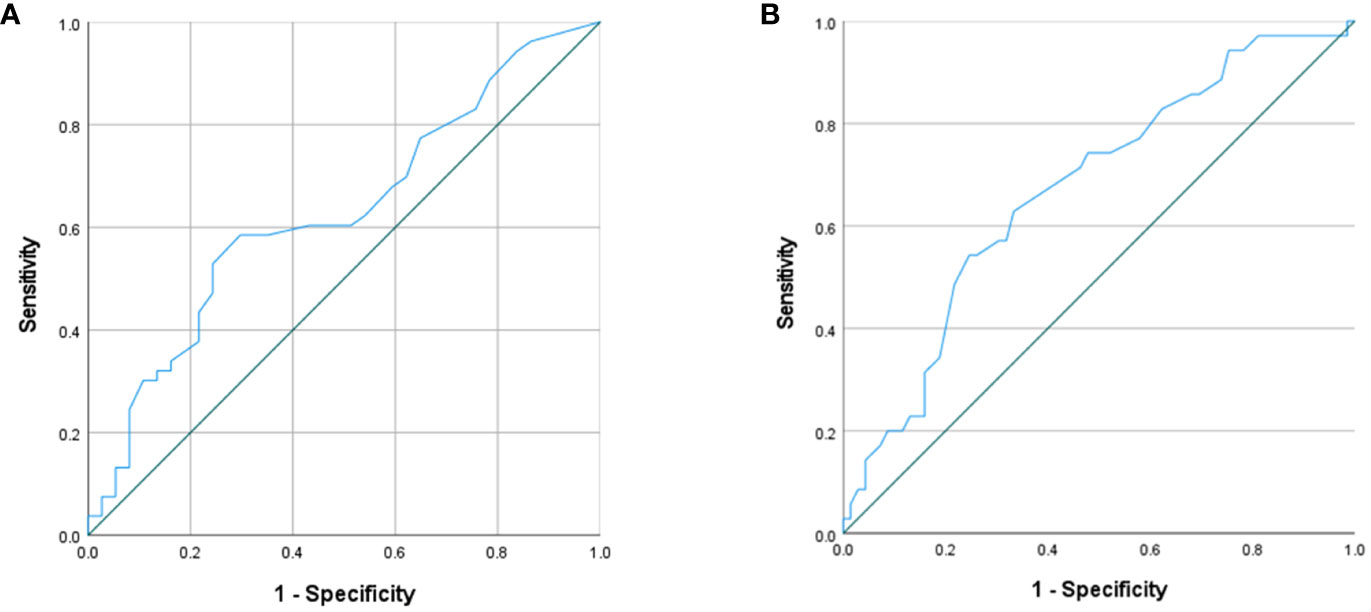
Figure 1 (A) ROC curves for preoperative serum calcium predicting postoperative hypocalcemia in the preoperative standard serum calcium group; (B) ROC curve for age prediction of postoperative hypocalcemia in the preoperative mildly high serum calcium group.
Correlation analysis showed that age (r=−0.280) and the preoperative serum calcium levels (r=−0.252) were negatively associated with the occurrence of postoperative hypocalcemia. Furthermore, alkaline phosphatase levels (r=0.241) were positively associated with the occurrence of postoperative hypocalcemia (Table 7).
Regression analysis revealed that age was an independent influencing factor on the occurrence of postoperative hypocalcemia (Table 8), being younger patients more likely to develop hypocalcemia (OR=0.947). ROC curves were produced to further investigate efficacy of age as a factor in predicting the occurrence of hypocalcemia in this group (Figure 1B). The results showed that when the patient’s age was 47.5 years, AUC = 0.671, p = 0.004, sensitivity and specificity were 0.543 and 0.754, respectively (Table 9), with predictive value.
Correlation analysis revealed that the location of the diseased paracrine gland was associated with postoperative hypocalcemia; other variables were not statistically significant (Table 7).
The results of the regression analysis did not indicate any factors influencing the occurrence of postoperative hypocalcemia (Table 8).
In this study, 270 patients were divided into three groups, according to their preoperative serum calcium levels. Statistical analysis revealed that (1) the incidence of postoperative hypocalcemia was different in each group (2), many biochemical indexes were different among the groups, and (3) the proportion of patients with or without concomitant clinical symptoms and the proportion of specific types of concomitant clinical symptoms were different among the groups. From these three observations, we conclude that the different preoperative serum calcium levels may reflect, to some extent, the stage of disease development of PHPT patients. The factors influencing the postoperative serum calcium levels and postoperative hypocalcemia in the patient groups need to be discussed. We evaluated 14 factors that could be associated with the postoperative serum calcium levels and postoperative hypocalcemia in PHPT patients. We concluded that the factors influencing the postoperative serum calcium levels and the factors influencing postoperative hypocalcemia differed among groups.
Preoperative serum calcium, serum phosphorus, and alkaline phosphatase levels affected the postoperative serum calcium levels differently, in different subgroups of patients. Possible causes were the following (1): calcium and phosphorus are the basic components of bone tissue, where both are stored as hydroxyapatite (16). Furthermore, excessive levels of PTH lead to bone destruction and to an internal environment of high serum calcium, low serum phosphorus, and increased calcitonin (17), with clinical symptoms such as bone pain and skin pruritus. Large amounts of calcium and phosphorus are required for bone remineralization after surgery (18) (2). The preoperative internal environment of high serum calcium and low serum phosphorus levels could make bone remineralization partially dependent on serum phosphorus (19). This could modify the postoperative serum calcium levels among the three groups of patients. The mean values of postoperative serum calcium levels in the three groups of patients from this study were 2.20 ± 0.17, 2.29 ± 0.20, and 2.40 ± 0.29, respectively. These values may further indicate that preoperative serum calcium and serum phosphorus levels could affect the postoperative serum calcium levels of the patients. Patients with high preoperative serum calcium levels may also maintain a relatively high serum calcium concentration postoperatively (3). The long-term bone destruction and high calcium levels, which cause some clinical symptoms in the body, also activate osteoblasts. Alkaline phosphatase is secreted by osteoblasts, which, accordingly, leads to elevated alkaline phosphatase levels, absorbing serum calcium into the bone and lowering serum calcium levels (20).
The presence or absence of clinical symptoms and calcitonin also have an impact on a patient’s postoperative calcium levels. Over the past 50 years, with the routine implementation of serum calcium monitoring, the clinical features of PHPT patients have changed from moderately severe hypercalcemia, with skeletal or renal system symptoms, to normal or mild serum calcium, with few or no symptoms (13, 14). This alteration indicates that clinical symptoms represent, to some extent, the degree of disease in patients with PHPT. As evidenced by the statistics of this study, patients with clinical symptoms have relatively high preoperative and postoperative blood calcium levels. In some institutions, calcitonin has been used to control hypercalcemia caused by PHPT, and improved results have been achieved (21, 22). This achievement may explain the effects of the levels of preoperative serum calcium, serum phosphorus (with or without clinical symptoms), and calcitonin on the postoperative levels of serum calcium. Several studies (11, 17, 23) had the same or similar results as the present study.
According to this study, we found that in the preoperative moderate to severe hypercalcemia group, patients undergoing a combined contralateral thyroidectomy and a total thyroidectomy had lower postoperative serum calcium levels than those subjected only to parathyroidectomy. Concerning the incidence of postoperative hypocalcemia, patients undergoing a combined parathyroidectomy and thyroidectomy had a higher incidence than those subjected only to parathyroidectomy (46.02% vs. 33.76%). Possible reasons for this difference could be the complex and delicate process of blood supply to the parathyroid glands and the challenge of combined thyroidectomy to achieve in situ preservation of the non-lesioned parathyroid glands. Moreover, the arteries and veins supplying the parathyroid glands are subjected to mechanical, electrical, and thermal injuries, which affect the blood supply to the remaining parathyroid glands (24, 25). Pradhan et al. (26) verified that combined thyroidectomy was an independent influence on postoperative hypocalcemia, which is consistent with the findings of the present study.
The younger the patients, the more likely they are to suffer from hypocalcemia. In PHPT patients, PTH overproduction leads to bone destruction and osteodystrophy (27, 28). After PTX, osteoclast activity is markedly reduced, osteoblast activity is delayed, the bone formation rate exceeds its destruction rate, calcium is transferred from the blood to the bone, and postoperative hypocalcemia occurs (29). Compared to younger individuals, older people have significantly reduced expression levels of many osteogenic genes and significantly fewer osteoblasts (30). This difference suggests that younger patients have a more evident ability to transfer calcium from the blood to the bone after PTX than older adults. Furthermore, they are more likely to develop hypocalcemia after surgery, which explains the relationship between hypocalcemia and age after PTX. Several studies have also demonstrated that patients who develop hypocalcemia tend to be younger (31, 32).
However, some studies have shown that patients with preoperative serum calcium levels >2.75 mmol/L were more likely to develop postoperative hypocalcemia than patients with normal preoperative serum calcium levels (11). The patient’s age, the preoperative serum calcium levels, and the presence or absence of clinical symptoms were not associated with the development of postoperative hypocalcemia, which contrasts with the findings of this study (33, 34). Possible causes could be the different exclusion criteria and grouping. Another study concluded that the preoperative PTH levels were associated with postoperative hypocalcemia, which has not been confirmed in the statistics of this study (35).
This study has the following shortcomings: it is a single-center retrospective study, which could have a bias in patient selection and did not exclude any potential single-center effects. The sample size was insufficient, as the number of patients in the preoperative severe serum calcium group was low and insufficient for data analysis. To assess its accuracy, the model constructed in the present study needs to be validated using additional data. Moreover, the sensitivity of the predictors was relatively low, but it can be used as a reference for all experts and scholars. Second, a long-term follow-up of the patients was not conducted in time, and the incidence of hypocalcemia in discharged patients was also not included. Therefore, larger samples, multicenter, and numerous prospective studies are needed in the future.
In the present study, for the first time, PHPT patients were stratified according to their initial serum calcium levels. The influencing factors of the postoperative serum calcium levels and postoperative hypocalcemia in patients with different preoperative serum calcium were analyzed. Different conclusions were obtained for different levels of preoperative serum calcium groups. Such differences are beneficial for the preoperative prognosis of the postoperative serum calcium levels and hypocalcemia in PHPT patients. They are also beneficial for a timely formulation of more accurate and individualized calcium supplementation regimens after surgery, in order to shorten the patients’ hospital stay and reduce their treatment costs.
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board of China–Japan Union Hospital of Jilin University (approval number: 20220904014). A detailed informed consent form is signed by the patients or their legal guardians prior to surgery.
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding authors.
The studies involving humans were approved by Institutional Review Board of China-Japan Union Hospital of Jilin University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board of China–Japan Union Hospital of Jilin University (approval number: 20220904014). A detailed informed consent form is signed by the patients or their legal guardians prior to surgery.
YM: Data curation, Investigation, Methodology, Software, Writing – original draft, Writing – review & editing. YiZ: Funding acquisition, Methodology, Supervision, Writing – original draft. JZ: Formal Analysis, Methodology, Writing – review & editing. QZ: Investigation, Methodology, Writing – original draft. YuZ: Data curation, Investigation, Writing – original draft. YL: Data curation, Investigation, Writing – original draft. JK: Data curation, Investigation, Writing – original draft. GD: Methodology, Supervision, Visualization, Writing – review & editing. XB: Funding acquisition, Resources, Supervision, Validation, Writing – review & editing. HS: Conceptualization, Funding acquisition, Supervision, Visualization, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by Science and Technology Research Project of Education Department of Jilin Province, China, No.JJKH20221065KJ; Jilin Province Health Research Talent Special Project (No.2020SCZ03); Beijing Cihua Medical Development Foundation (J2023107004).
Thanks to all the members of the Pathology Department of China–Japan Union Hospital of Jilin University and Chengdu Zhitu Intelligent Technology Cooperation & Dr. Yijun Liu for their strong support to this study. The authors would like to express their gratitude to EditSprings (https://www.editsprings.cn) for the expert linguistic services provided.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Bilezikian JP, Khan AA, Silverberg SJ, Fuleihan GE, Marcocci C, Minisola S, et al. Evaluation and management of primary hyperparathyroidism: summary statement and guidelines from the fifth international workshop. J Bone Miner Res (2022) 37(11):2293–314. doi: 10.1002/jbmr.4677
2. Perrier N, Lang BH, Farias LCB, Poch LL, Sywak M, Almquist M, et al. Surgical aspects of primary hyperparathyroidism. J Bone Miner Res (2022) 37(11):2373–90. doi: 10.1002/jbmr.4689
3. Wilhelm SM, Wang TS, Ruan DT, Lee JA, Asa SL, Duh QY, et al. The american association of endocrine surgeons guidelines for definitive management of primary hyperparathyroidism. JAMA Surg (2016) 151(10):959–68. doi: 10.1001/jamasurg.2016.2310
4. Walker MD, Shane E. Hypercalcemia:A review. JAMA (2022) 328(16):1624–36. doi: 10.1001/jama.2022.18331
5. Carsote M, Nistor C. Forestalling hungry bone syndrome after parathyroidectomy in patients with primary and renal hyperparathyroidism. Diagnostics (Basel) (2023) 13(11):1953. doi: 10.3390/diagnostics13111953
6. Acharya R, Kopczynska M, Goodmaker C, Mukherjee A, Doran H. Vitamin D repletion in primary hyperparathyroid patients undergoing parathyroidectomy leads to reduced symptomatic hypocalcaemia and reduced length of stay: a retrospective cohort study. Ann R Coll Surg Engl (2022) 104(1):41–7. doi: 10.1308/rcsann.2021.0078
7. Miah MS, Mahendran S, Mak C, Leese G, Smith D. Pre-operative serum alkaline phosphatase as a predictive indicator of post-operative hypocalcaemia in patients undergoing total thyroidectomy. J Laryngol Otol (2015) 129(11):1128–32. doi: 10.1017/S0022215115002352
8. Fonseca-Correa JI, Nava-Santana C, Tamez-Pedroza L, Paz-Cortes A, Santillan-Ceron A, Rojas-Concha LJ, et al. Clinical factors associated with early and persistent hypocalcaemia after parathyroidectomy in patients on dialysis with severe hyperparathyroidism. Nephrol (Carlton) (2021) 26(5):408–19. doi: 10.1111/nep.13854
9. Kaya C, Tam AA, Dirikoç A, Kılıçyazgan A, Kılıç M, Türkölmez Ş, et al. Hypocalcemia development in patients operated for primary hyperparathyroidism: Can it be predicted preoperatively? Arch Endocrinol Metab (2016) 60(5):465–71. doi: 10.1590/2359-3997000000207
10. Järhult J, Landerholm K. Outcome of hypocalcaemia after thyroidectomy treated only in symptomatic patients. Br J Surg (2016) 103(6):676–83. doi: 10.1002/bjs.10086
11. Sun L, He X, Liu T. Preoperative serum alkaline phosphatase: a predictive factor for early hypocalcaemia following parathyroidectomy of primary hyperparathyroidism. Chin Med J (Engl) (2014) 127(18):3259–64.
12. Kidwai SM, Parasher AK, Ho YW, Teng MS, Genden EM. Risk stratification for outpatient parathyroidectomy and predictors of postoperative complications. Am J Otolaryngol (2017) 38(1):26–30. doi: 10.1016/j.amjoto.2016.09.006
13. Muñoz-Torres M, García-Martín A. Primary hyperparathyroidism. Hiperparatiroidismo primario. Med Clin (Barc) (2018) 150(6):226–32. doi: 10.1016/j.medcli.2017.07.020
14. Walker MD, Silverberg SJ. Primary hyperparathyroidism. Nat Rev Endocrinol (2018) 14(2):115–25. doi: 10.1038/nrendo.2017.104
15. Payne RB, Little AJ, Williams RB, Milner JR. Interpretation of serum calcium in patients with abnormal serum proteins. Br Med J (1973) 4(5893):643–6. doi: 10.1136/bmj.4.5893.643
16. Ciosek Ż, Kot K, Kosik-Bogacka D, Łanocha-Arendarczyk N, Rotter I. The effects of calcium, magnesium, phosphorus, fluoride, and lead on bone tissue. Biomolecules (2021) 11(4):506. doi: 10.3390/biom11040506
17. Han CH, Fry CH, Sharma P, Han TS. A clinical perspective of parathyroid hormone related hypercalcaemia. Rev Endocr Metab Disord (2020) 21(1):77–88. doi: 10.1007/s11154-019-09529-5
18. Brasier AR, Nussbaum SR. Hungry bone syndrome: clinical and biochemical predictors of its occurrence after parathyroid surgery. Am J Med (1988) 84(4):654–60. doi: 10.1016/0002-9343(88)90100-3
19. Pal R, Gautam A, Bhadada SK. Role of bisphosphonates in the prevention of postoperative hungry bone syndrome in primary hyperparathyroidism: A meta-analysis and need for randomized controlled trials. Drug Res (Stuttg) (2021) 71(2):108–9. doi: 10.1055/a-1325-0351
20. Sarac F, Saygili F. Causes of high bone alkaline phosphatase. Biotechnol Biotechnol Equip (2007) 21(2):194–7. doi: 10.1080/13102818.2007.10817444
21. Pyram R, Mahajan G, Gliwa A. Primary hyperparathyroidism: Skeletal and non-skeletal effects, diagnosis and management. Maturitas (2011) 70(3):246–55. doi: 10.1016/j.maturitas.2011.07.021
22. Kuchay MS, Mathew A, Kaur P, Mishra SK. Denosumab can be used successfully as a bridge to surgery in patients with severe hypercalcemia due to primary hyperparathyroidism. Arch Endocrinol Metab (2021) 65(5):669–73. doi: 10.20945/2359-3997000000408
23. Carvalho GB, Giraldo LR, Lira RB, Macambira IBM, Tapia MA, Kohler HF, et al. Preoperative vitamin D deficiency is a risk factor for postoperative hypocalcemia in patients undergoing total thyroidectomy: retrospective cohort study. Sao Paulo Med J (2019) 137(3):241–7. doi: 10.1590/1516-3180.2018.0336140319
24. Falch C, Hornig J, Senne M, Braun M, Konigsrainer A, Kirschniak A, et al. Factors predicting hypocalcemia after total thyroidectomy - A retrospective cohort analysis. Int J Surg (2018) 55:46–50. doi: 10.1016/j.ijsu.2018.05.014
25. Orloff LA, Wiseman SM, Bernet VJ, Fahey TJ 3rd, Shaha AR, Shindo ML, et al. American thyroid association statement on postoperative hypoparathyroidism: diagnosis, prevention, and management in adults. Thyroid (2018) 28(7):830–41. doi: 10.1089/thy.2017.0309
26. Pradhan MC, Young CD, Thomas SM, Stang MT, Kazaure HS, Scheri RP. Outcomes of concurrent parathyroidectomy and thyroidectomy among CESQIP surgeons. Am J Surg (2022) 224(5):1190–6. doi: 10.1016/j.amjsurg.2022.03.041
27. El-Hajj Fuleihan G, Chakhtoura M, Cipriani C, Eastell R, Karonova T, Liu JM, et al. Classical and nonclassical manifestations of primary hyperparathyroidism. J Bone Miner Res (2022) 37(11):2330–50. doi: 10.1002/jbmr.4679
28. Eller-Vainicher C, Battista C, Guarnieri V, Muscarella S, Palmieri S, Salcuni AS, et al. Factors associated with vertebral fracture risk in patients with primary hyperparathyroidism. Eur J Endocrinol (2014) 171(3):399–406. doi: 10.1530/EJE-14-0343
29. Yajima A, Inaba M, Tominaga Y, Nishizawa Y, Ikeda K, Ito A. Increased osteocyte death and mineralization inside bone after parathyroidectomy in patients with secondary hyperparathyroidism. J Bone Miner Res (2010) 25(11):2374–81. doi: 10.1002/jbmr.126
30. Becerikli M, Jaurich H, Schira J, Schulte M, Döbele C, Wallner C, et al. Age-dependent alterations in osteoblast and osteoclast activity in human cancellous bone. J Cell Mol Med (2017) 21(11):2773–81. doi: 10.1111/jcmm.13192
31. Sutton W, Canner JK, Shank JB, Fingeret AL, Karzai S, Segev DL, et al. The impact of patient age on practice patterns and outcomes for primary hyperparathyroidism. Am J Surg (2022) 224(1 Pt B):400–7. doi: 10.1016/j.amjsurg.2022.03.007
32. Yu Q, Liu K, Ma D, Xie C, Wu Y, Dai W, et al. Do symptoms and serum calcium levels affect the results of surgical treatment of primary hyperparathyroidism? BioMed Res Int (2019) 2019:2150159. doi: 10.1155/2019/2150159
33. Jakubauskas M, Beisa V, Strupas K. Risk factors of developing the hungry bone syndrome after parathyroidectomy for primary hyperparathyroidism. Acta Med Litu (2018) 25(1):45–51. doi: 10.6001/actamedica.v25i1.3703
34. Jannasch O, Voigt C, Reschke K, Lippert H, Mroczkowski P. Comparison of outcome between older and younger patients following surgery for primary hyperparathyroidism. Pol Przegl Chir (2013) 85(10):598–604. doi: 10.2478/pjs-2013-0089
Keywords: primary hyperparathyroidism, parathyroidectomy, hypocalcemia, age, alkaline phosphatase
Citation: Mu Y, Zhao Y, Zhao J, Zhao Q, Zhang Y, Li Y, Kou J, Dionigi G, Bian X and Sun H (2023) Factors influencing serum calcium levels and the incidence of hypocalcemia after parathyroidectomy in primary hyperparathyroidism patients. Front. Endocrinol. 14:1276992. doi: 10.3389/fendo.2023.1276992
Received: 13 August 2023; Accepted: 13 November 2023;
Published: 05 December 2023.
Edited by:
Chenyu Sun, AMITA Health, United StatesReviewed by:
Mara Carsote, Carol Davila University of Medicine and Pharmacy, RomaniaCopyright © 2023 Mu, Zhao, Zhao, Zhao, Zhang, Li, Kou, Dionigi, Bian and Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xuehai Bian, YmlhbnhoQGpsdS5lZHUuY24=; Hui Sun, c19oQGpsdS5lZHUuY24=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.