
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Endocrinol., 28 August 2023
Sec. Clinical Diabetes
Volume 14 - 2023 | https://doi.org/10.3389/fendo.2023.1238399
 Chun Xing Li1†
Chun Xing Li1† Li Yan Liu1†
Li Yan Liu1† Chen Xiao Zhang2
Chen Xiao Zhang2 Xu Hua Geng3
Xu Hua Geng3 Si Meng Gu1
Si Meng Gu1 Yu Qiao Wang1
Yu Qiao Wang1 Hua Liu1*
Hua Liu1* Qing Xie1*
Qing Xie1* Shuo Liang1*
Shuo Liang1*Backgrounds: The safety of different sodium-glucose transporter 2 (SGLT-2) inhibitors remains uncertain due to the lack of head-to-head comparisons.
Methods: This network meta-analysis (NMA) was performed to compare the safety of nine SGLT-2 inhibitors in patients with type 2 diabetes (T2DM). PubMed, Embase, Cochrane Central Register of Controlled Trials and ClinicalTrials.gov were searched for studies published in English before August 30, 2022. Published and unpublished randomized controlled trials (RCTs) comparing the safety of individual SGLT-2 inhibitors in patients with T2DM were included. A Bayesian NMA with random effects model was applied. Subgroup and sensitivity analyses were performed. The quality of the evidence was evaluated using the Confidence in Network Meta-Analysis framework.
Results: Nine SGLT-2 inhibitors were evaluated in 113 RCTs (12 registries) involving 105,293 adult patients. Reproductive tract infections (RTIs) were reported in 1,967 (4.51%) and 276 (1.01%) patients in the SGLT-2 inhibitor and placebo groups, respectively. Furthermore, pollakiuria was reported in 233 (2.66%) and 45 (0.84%) patients, respectively. Compared to placebo, a significantly higher risk of RTIs was observed with canagliflozin, ertugliflozin, empagliflozin, remogliflozin, dapagliflozin, and sotagliflozin, but not with luseogliflozin and ipragliflozin, regardless of gender. An increased risk of pollakiuria was observed with dapagliflozin [odds ratio (OR) 10.40, 95% confidence interval (CI) 1.60-157.94) and empagliflozin (OR 5.81, 95%CI 1.79-32.97). Remogliflozin (OR 6.45, 95%CI 2.18-27.79) and dapagliflozin (OR 1.33, 95%CI 1.10-1.62) were associated with an increased risk of urinary tract infections (UTIs). Instead, the included SGLT-2 inhibitors had a protective effect against acute kidney injury (AKI). No significant differences were found for hypovolemia, renal impairment or failure, fracture, diabetic ketoacidosis (DKA), amputation, and severe hypoglycemia between the SGLT-2 inhibitor and the placebo groups.
Conclusion: In patients with T2DM, dapagliflozin was associated with an increased risk of RTIs, pollakiuria, and UTIs. Empagliflozin increased the risk of RTIs and pollakiuria. Remogliflozin increased the risk of UTIs. None of the SGLT-2 inhibitors showed a significant difference from the placebo for hypovolemia, renal impairment or failure, fracture, DKA, amputation, and severe hypoglycemia. The findings guide the selection of SGLT-2 inhibitors for patients with T2DM based on the patient’s profiles to maximize safety.
Systematic review registration: https://www.crd.york.ac.uk/prospero, identifier CRD42022334644.
Sodium-glucose transporter 2 (SGLT2) inhibitors are a new class of oral anti-diabetic drugs with evidence of improvement in metabolic syndrome and cardiovascular outcomes. SGLT2 inhibitors are recommended as first-line treatment in patients with type 2 diabetes mellitus (T2DM) and heart failure, especially heart failure with decreased ejection fraction (1). SGLT2 inhibitors may be associated with an increased risk of reproductive tract infections (RTIs), pollakiuria, hypovolemia, urinary tract infections (UTIs), and other adverse effects. However, the evidence differed between trials (2–6), all of which compared a single SGLT2 inhibitor with a placebo. Head-to-head comparisons were published only in three studies and one registry, which found that empagliflozin had a lower risk of urinary and genital infection than dapagliflozin (7, 8) A network meta-analysis (NMA) conducted in 2016 showed that dapagliflozin (10 mg) was associated with an increased risk of UTI compared to empagliflozin (25 mg) (6) Furthermore, concerns have been raised about the potential safety of individual SGLT2 inhibitors.
Although three NMAs analyzed the safety differences between SGLT2 inhibitors, the number of drugs and related adverse reactions included was limited (6, 9, 10). Whether the class safety profiles can represent individual SGLT2 inhibitors remains to be clarified. Therefore, this systematic review and NMA of randomized controlled trials (RCTs) aimed to evaluate the relative safety of nine SGLT2 inhibitors regarding RTIs, pollakiuria, hypovolemia, renal impairment/failure, acute kidney injury (AKI), UTIs, fracture, diabetic ketoacidosis (DKA), amputation, and severe hypoglycemia in patients with T2DM.
This NMA followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) extension statement (11). The protocol was registered in the International Prospective Register of Systematic Review (PROSPERO, registration number CRD42022334644).
We searched PubMed, Cochrane Central Register of Controlled Trials, Embase, and ClinicalTrials.gov for RCTs comparing SGLT2 inhibitors to placebo or other SGLT2 inhibitors in T2DM patients from the inception to August 30, 2022. The search consisted of three domains: intervention (SGLT2 inhibitor class or individual drugs), adverse events of particular interest, and RCTs. Details of the search strategy are provided in Appendix 2.
The literature screening used PICOS (participants, intervention, comparison, outcomes and characteristics, and study design). RCTs were included if they met the following criteria: 1) T2DM patients ≥ 18 years old; 2) patients who received SGLT2 inhibitors (canagliflozin, dapagliflozin, empagliflozin, ertugliflozin, tofogliflozin, luseogliflozin, ipragliflozin, remogliflozin, or sotagliflozin) with doses equal or greater than the approved doses for at least 12 weeks; 3) the comparator was placebos or any of the nine SGLT2 inhibitors; and 4) studies evaluated safety outcomes. Only RCTs with a sample size in the single group (sum of all dose groups) greater than 50 were included.
Primary outcomes were the risks of RTIs and pollakiuria. Secondary outcomes were the risks of hypovolemia, renal impairment and failure, AKI, UTI, fracture, DKA, amputation, and severe hypoglycemia. Two authors (LY Liu and CX Zhang) independently performed the literature search and study selection using Endnote 18.0. Disagreements were resolved by a third author (CX Li).
Two authors (LY Liu and CX Zhang) independently completed the data extraction using a standardized form and verified by the third author. The following data were extracted: study characteristics (first author, year of publication, countries/regions, follow-up time, details of the interventions, number of patients, and outcomes) and participants’ characteristics [mean or median age, percentage of women, baseline body mass index (BMI), median hemoglobin A1c level, and stage of renal impairment].
Two authors independently assessed the risk of bias in eligible studies using the revised Cochrane Collaboration Risk of Bias 2 (RoB2) tool for RCTs (12). Any discrepancies were resolved by consensus with a third author. We assessed all endpoints from the five domains, and the overall risk of bias was rated as “low risk,” “some concerns,” and “high risk.”
We used the Confidence in Network Meta-Analysis (CINeMA) framework and the Web application to evaluate confidence in the NMA results. CINeMA offers a more comprehensive approach to assessing the quality of evidence in NMA (13). CINeMA considers six domains that affect the confidence level in the NMA results: within-study bias, reporting bias, indirectness, imprecision, heterogeneity, and incoherence. The level of concern for each relative treatment effect of NMA gives rise to “no concerns,” “some concerns,” or “major concerns” in each of the six domains. Then, the judgments in all domains are summarized into a single confidence rating (“high,” “moderate,” “low,” or “very low”). The percentage contribution matrix and the weighted average risk of bias were applied to assess the within-study bias and the indirectness of each comparison.
We performed Bayesian random-effects NMA of all outcomes. Dichotomous outcomes were calculated as odds ratios (OR) and 95% confidence intervals (CI). Model convergence was monitored and visualized using trace, density, and Brooks-Gelman-Rubin diagnosis plots. Good model convergence was when the potential scale reduction factor (PSRF), the median value of the shrink factor, and the 97.5% value simultaneously approached 1. The network graphs scaled by the number of patient studies by each treatment node and the risk of bias were presented graphically.
The I2 estimates and their 95% CIs were used to assess heterogeneity: low (0-29%), moderate (30-59%), substantial (60-89%), and high (>89%). Subgroup analyses were used to address heterogeneity. For inconsistency, we looked at the results of node splitting. The consistency was assessed by considering direct and indirect evidence separately with node splitting. Treatment rankings were evaluated using the surface under the cumulative ranking curve (SUCRA). SUCRA values range from 0 to 100%. The higher the SUCRA value, and the closer to 100%, the higher the probability that a therapy is in the top rank or one of the top ranks.
All analyses were performed using four Markov chains (50,000 iterations after a burn-in of 10,000 and a thinning of 10). For further verification, the results were reproduced by implementing the R software (version 4.0.3) with the gemtc package (version 0.8-8) and the JAGS software (version 4.3.0). The RTIs were calculated separately for males and females. Studies focusing on T2DM with chronic kidney disease (CKD) and studies that reported extended follow-ups (≥48 weeks) were not included in the overall analysis. They were only included in the subgroup analysis. Trials with zero events in both groups were omitted from the NMA.
The dose-specific network model was conducted. Subgroup analyses were performed according to renal function (estimated glomerular filtration rate (eGFR) < 90 mL/min/m2), study countries/regions (Asia, Japan, or China), types of SGLT2 inhibitor treatment (an add-on to metformin-based therapy or monotherapy in drug-naïve patients), and duration of follow-up.
The initial screening identified 113 RCTs (n=105,293) for inclusion in the systematic review (2–5, 7, 8, 14–119) (Appendix 1). Twelve trials were published in registries (107, 108, 110–119). After reviewing data collection, 21 RCTs were excluded from NMA: 13 focused on T2DM and CKD (96–106, 108, 120), and 11 reported extended follow-ups (21, 28, 69, 89–95, 121). Among the 11 studies, 8 had only extended follow-up data, and 3 had short (24-28 weeks) and extended follow-up results (only extended follow-up outcomes were excluded).
Appendix 4 shows the characteristics of the included studies, including 78 (69.0%) multinational studies, 25 (22.1%) Japanese studies, and 6 (5.3%) conducted in other Asia regions. The median number of patients was 133 [33-8,582, interquartile range (IQR) 140], and the median age was 57.4 years (48.7-70.5). Twenty-three studies (20.35%) enrolled 50% or more women. The patients were primarily overweight, with a median baseline BMI of 30.7 (23.36-36.04). Most patients had a baseline median hemoglobin A1c of 8.1% (6.87-10.10). Among these studies, 90 (79.7%) studies were patients with T2DM alone, 13 (11.5%) were patients with T2DM with CKD, and 10 (8.9%) were patients with T2DM with cardiovascular disease and/or hypertension. Seventy-five studies (66.4%) (n=53,658) reported the average time since diabetes diagnosis, with a median of 7.2 years (0.25-20.70, IQR 5.67).
SGLT-2 inhibitors were used as monotherapy in drug-naive patients (20 trials; 5,714 patients) or as an addition to metformin-based therapy (25 trials; 9,957 patients). A total of 109 (96.5%) of the studies were placebo-controlled, and 4 (3.5%) had an active SGLT-2 inhibitor as a comparator. The types of intervention were dapagliflozin (5-50 mg/d, 34 studies), empagliflozin (10-50 mg/d, 26 studies), ipragliflozin (50-300 mg/d, 18 studies), canagliflozin (100-600 mg/d, 17 studies), sotagliflozin (200-400 mg/d, 11 studies), ertugliflozin (5-25 mg/d, 8 studies), luseogliflozin (2.5-10 mg/d, 8 studies), tofogliflozin (20-40 mg/d, 3 studies), and remogliflozin (200-2000 mg/d, 3 studies). The median duration of the intervention was 24 weeks (12-338). Eleven studies had a short follow-up of 24 to 28 weeks and an extended follow-up of 48 to 102 weeks.
The quality of the studies varied (Appendix 5). No studies had high risks of bias for the randomization process, deviations from the intended intervention, the measurement of the outcome, and the selection of the reported result. Two studies (1.9%) had a high risk of missing outcome data. Overall, 77 studies (73.3%) had a low risk of bias (overall bias score of 1), 26 (24.8%) had some concerns (overall bias score of 2), and 2 (1.9%) had a high risk of bias (overall bias score of 1) (Appendix 5.1). The risk of bias for each outcome is shown in the RoB chart (Appendix 5.2).
Seventy-nine RCTs (n=70,850) (2–5, 7, 8, 14–24, 26–32, 34–76, 78–80, 83, 85–88, 112, 115, 117, 118) (four published in registries) reported 2, 243 (3.2%) cases of RTIs: 1,967 (4.5%) in the SGLT-2 inhibitor group and 276 (1.0%) in the placebo group. RTIs were reported in patients treated with canagliflozin (552, 6.7%), ertugliflozin (385, 5.5%), empagliflozin (536, 5.1%), sotagliflozin (21, 3.3%), remogliflozin (23, 2.9%), dapagliflozin (412, 2.9%), ipragliflozin (26, 2.2%), tofogliflozin (5, 1.3%), and luseogliflozin (7, 1.3%). Details are shown in Table 1.
The pooled OR of tofogliflozin had a wide 95% CI, which reduced the confidence of the results. Therefore, related studies were excluded from the NMA (2, 14, 15). Head-to-head comparative studies (sotagliflozin and empagliflozin, empagliflozin and dapagliflozin, remogliflozin and dapagliflozin) are shown in the network plot (Figure 1), which contributed 6.3%, 2.5%, and 8.1% to the entire network, respectively (Appendix 12.1). The trace and density plots showed good model convergence (Appendix 6.1). The PSRF was 1.01 on the Brooks-Gelman-Rubin diagnosis plot (Appendix 6.1).
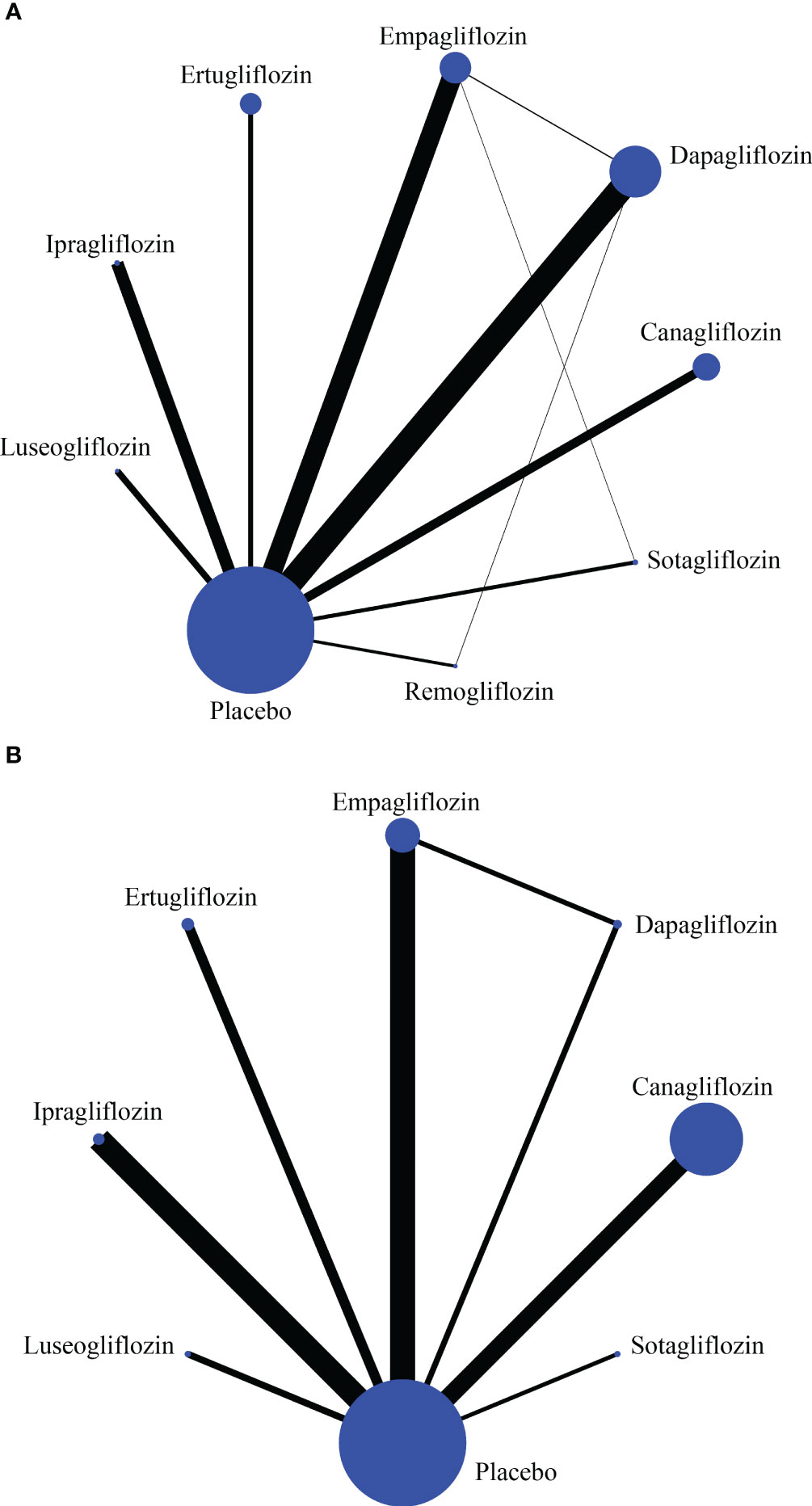
Figure 1 The network plot of reproductive tract infections (A) and pollakiuria (B). Each circle indicates a treatment node. Lines connecting 2 nodes represent direct comparisons between 2 treatments. The size of the nodes is proportional to the number of trials evaluating each treatment. The thickness of the lines is proportional to the number of trials directly comparing the 2 connected treatments.
Canagliflozin, ertugliflozin, empagliflozin, remogliflozin, dapagliflozin, and sotaglifozin were associated with a significant increase in RTIs compared to placebo. In contrast, luseogliflozin and ipragliflozin were unrelated to the risk of RTIs (Figure 2A; Table 2). The certainty of the evidence was low to high (Appendix 17.1). Compared to sotagliflozin or luseogliflozin, the risk of RTIs was not significantly different between individual SGLT-2 inhibitors (Figure 2B; Table 2).
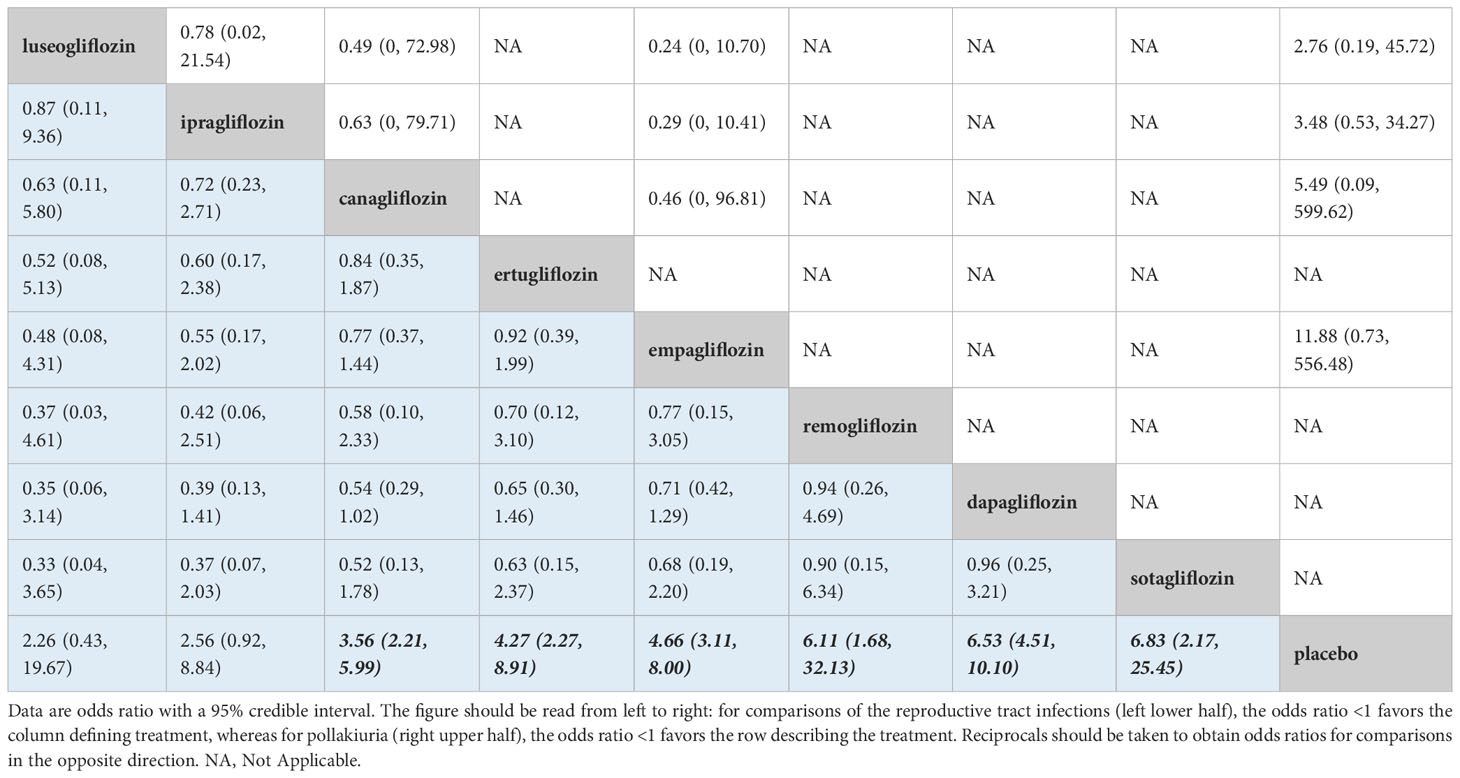
Table 2 Network meta-analysis results for reproductive tract infections (left lower half) and pollakiuria (right upper half).
There was moderate heterogeneity between the studies (I2 pairwise and consistency was 35.60% and 36.41%, and the P-value of inconsistency was > 0.1) (Appendix 11.1). The SUCRA value of dapagliflozin, sotagliflozin, remogliflozin, empagliflozin, ertugliflozin, canagliflozin, luseogliflozin, ipragliflozin, and placebo was 0.81, 0.76, 0.70, 0.59, 0.54, 0.41, 0.32, 0.31, and 0.03, respectively. Dapagliflozin was ranked highest for the increased risk of RTIs (Figure 3A). Comparison-adjusted funnel plots did not suggest the presence of small study bias (Appendix 14.1).
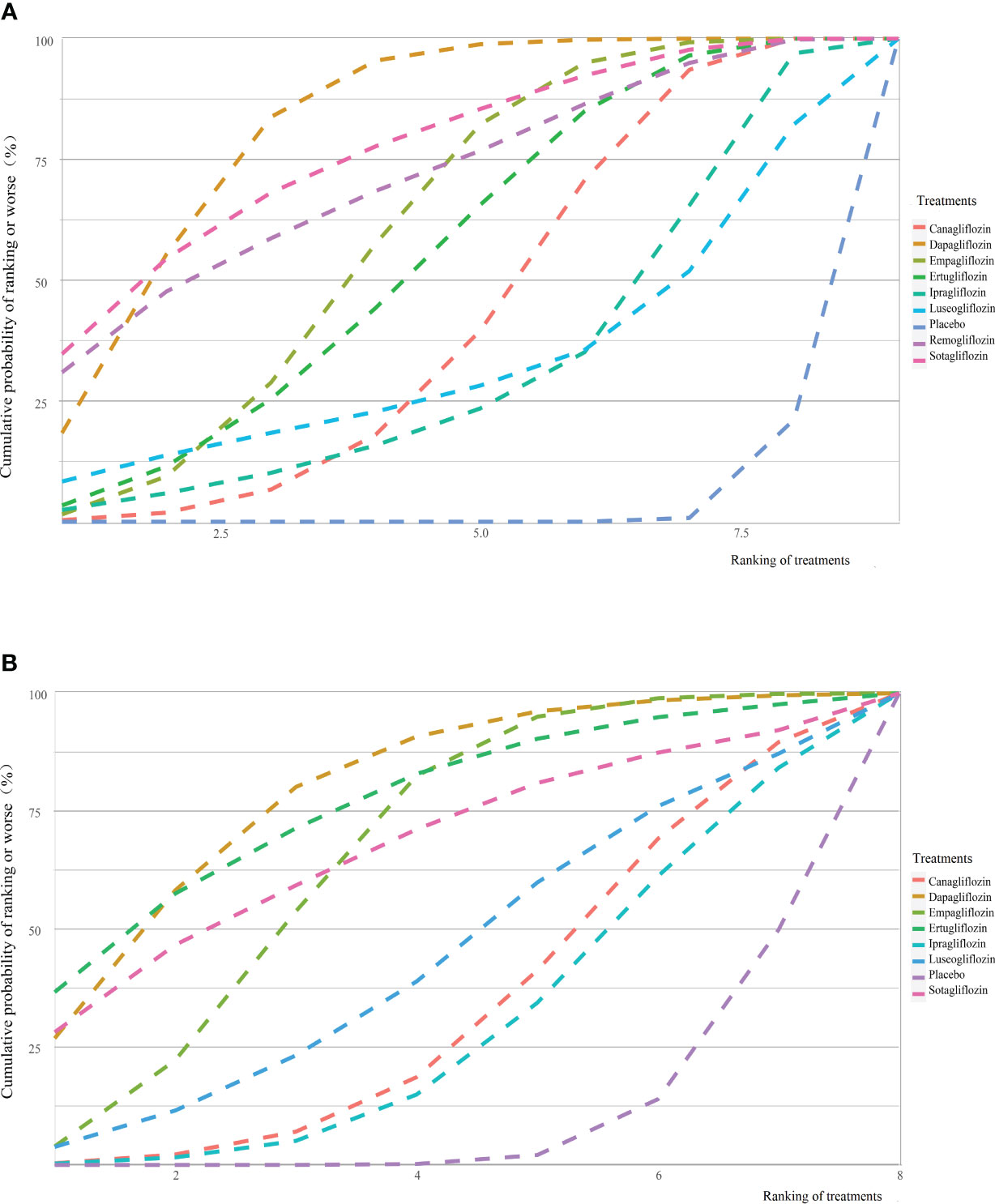
Figure 3 Cumulative ranking curves for reproductive tract infections (A) and pollakiuria (B). Graphs show the cumulative probability of each intervention ranking, from worst (rank 1) to best (rank 9 or 8 depending on the number of treatments) for each outcome. A rank indicates the probability that an intervention is worst, second worst etc. For example, dapagliflozin probably ranked worst for increasing the risk of reproductive tract infections.
RTIs were reported in 519 (4.1%) of the men in the SGLT-2 inhibitor group compared to 61 (1.0%) in the placebo group. In contrast, 635 (8.4%) of the women reported RTIs in the SGLT-2 inhibitor group compared to 85 (2.22%) in the placebo group. Women had the same risk of RTIs between ipragliflozin, ertugliflozin, canagliflozin, empagliflozin, and dapagliflozin. However, higher ORs in RTIs were observed in men compared to women (Appendices 7.1-7.2 and 8.1-8.2).
Twenty-five RCTs (n=14,117) (4, 7, 8, 14, 17, 18, 20, 24, 26, 27, 32, 56, 59, 65, 66, 69, 71, 75, 77, 79–81, 110, 117, 119) (three published in the registries) reported 278 (1.9%) cases of pollakiuria: 233 (2.7%) in the SGLT-2 inhibitor group and 45 (0.8%) in the placebo group. Among the 233 cases in the SGLT-2 inhibitor group, the number of pollakiuria cases was luseogliflozin (17, 7.1%), dapagliflozin (22, 6.7%), ipragliflozin (33, 5.9%), sotagliflozin (10, 4.0%), empagliflozin (95, 3.9%), ertugliflozin (12, 1.7%), tofogliflozin (2, 1.5%), and canagliflozin (42, 1.0%) (Table 1).
The 95% CI of the tofogliflozin combined OR was wide, so the related study (14) was excluded from the NMA. Finally, 24 RCTs were included. Head-to-head comparative studies between empagliflozin and dapagliflozin were found in the network plot (Figure 1). The direct comparison contributed 88.5% and 12.4% to the mixed estimates and the entire network, respectively (Appendix 12.2).
The trace and density plots showed good model convergence, and the PSRF was 1.00 in the Brooks-Gelman-Rubin diagnosis plot (Appendix 6.2). Dapagliflozin (OR 10.40, 95%CI 1.60-157.94) and empagliflozin (OR 5.81, 95%CI 1.79-32.97) increased the risk of pollakiuria compared to placebo (Figure 2C; Table 2). The certainty of the evidence was low to high (Appendix 17.2). Canagliflozin, ertugliflozin, sotagliflozin, luseogliflozin, and ipragliflozin were not associated with the risk of pollakiuria (Figure 2C; Table 2). Compared to dapagliflozin, other SGLT-2 inhibitors had the same risk of pollakiuria (Figure 2D; Table 2).
There was moderate heterogeneity between the studies (I2 pairwise and consistency was 41.40% and 45.56%, and the P-value of inconsistency was > 0.1) (Appendix 11.2). The SUCRA value of dapagliflozin, ertugliflozin, sotagliflozin, empagliflozin, luseogliflozin, canagliflozin, ipragliflozin, and placebo was 0.79, 0.76, 0.67, 0.65, 0.43, 0.33, 0.28, and 0.09, respectively. Dapagliflozin ranked highest for an increased risk of pollakiuria (Figure 3B).
The numbers of cases reported for secondary outcomes were: hypovolemia [824 (2.4%) vs. 477 (2.0%)], renal impairment or failure [177 (1.7%) vs. 97 (1.2%)], AKI [506 (2.0%) vs. 420 (2.2%)], UTIs [3,133 (6.8%) vs. 1,457 (5.1%)], fracture [957 (3.4%) vs. 670 (3.3%)], DKA [73 (0.3%) vs. 18 (0.1%)], amputation [238 (1.6%) vs. 160 (1.4%)], and severe hypoglycemia [434 (1.9%) vs. 292 (1.9%)] in the SGLT-2 inhibitor and placebo groups, respectively. Appendix 7.3–7.10 shows the network plot. The trace, density, and Brooks-Gelman-Rubin diagnosis plots showed good model convergence (Appendix 6.3–6.10). The details are shown in Table 1. The contribution graphs are shown in Appendix 12.3–12.10.
The SGLT-2 inhibitors included were not associated with the risk of hypovolemia, renal impairment or failure, fracture, DKA, amputation, or severe hypoglycemia compared to the placebo (Appendices 8.3-8.10 and 9.3–9.10). The certainty of the evidence was very low to low (Appendix 17.3–17.10). Furthermore, canagliflozin, dapagliflozin, empagliflozin, ertugliflozin, and sotagliflozin demonstrated a protective effect on AKI, but the difference was not statistically significant compared to placebo(Appendices 8.5 and 9.5).
Remogliflozin (OR 6.45, 95%CI 2.18-27.79) and dapagliflozin (OR 1.33, 95%CI 1.10-1.62) were associated with an increased risk of UTIs compared to placebo. In contrast, empagliflozin, sotagliflozin, canagliflozin, ertugliflozin, ipragliflozin, and tofogliflozin did not show significant differences with placebo. The certainty of the evidence was low to high (Appendix 17.6). Remogliflozin (OR 4.86, 95%CI 1.66-20.88) increased the risk of UTIs, while empagliflozin (OR 0.78, 95%CI 0.61-0.99) decreased the risk of UTIs when compared to dapagliflozin (Appendices 8.6 and 9.6).
Tofogliflozin and luseogliflozin ranked the worst for hypovolemia, with a value of SUCRA of 0.68 and 0.81, respectively. Dapagliflozin ranked worst for renal impairment or failure with a SUCRA value of 0.84. Remogliflozin and dapagliflozin ranked worst for UTIs, with a value of SUCRA 1.00 and 0.75, respectively (Appendix 13.1).
The risk of RTIs increased with increasing doses of dapagliflozin (5 to 50 mg/d) and ertugliflozin (5 to 20 mg/d, except 10 mg/d). The certainty of the evidence was very low to high. In split-dose studies, subgroup analysis of canagliflozin 600 mg/d (24), empagliflozin 50 mg/d (59, 61), ertugliflozin 10 mg/d (19), remogliflozin 250 mg/d (87), and remogliflozin 1000 mg/d (86, 87) was inconsistent with the overall analysis, suggesting that there was no increased risk of RTIs at these drug doses. Canagliflozin 200 mg/d in women (29, 61) and empagliflozin 50 mg/d (61) in men showed opposite results compared to the overall analysis (Appendix 15.1).
Subgroup analyses showed that, in split-dose studies, the risks of pollakiuria (except empagliflozin 50 mg/d (59) and ertugliflozin 15 mg/d (4, 20)), UTIs (except high dose dapagliflozin 20 mg/d (5, 35) and 50 mg/d (5), remogliflozin low dose 200 mg/d (86, 88) and 250 mg/d (87)), and fracture were consistent with the overall analyses. The certainty of the evidence was low to high (Appendix 15.1).
Subgroup analyses showed that the risks of hypovolemia (except canagliflozin 300 mg/d), AKI, and severe hypoglycemia were consistent with the overall analyses. The certainty of the evidence was low. Low- to moderate-quality evidence showed the same renal impairment or failure results. Very low to low-quality evidence showed similar results regarding DKA and amputation.
Twenty-five RCTs (n=7,162) reported 113 (2.2%) and 11(0.5%) cases of RTIs in Asia treated with SGLT-2 inhibitors and placebo, respectively (2, 3, 7, 8, 15–18, 22, 29, 31, 32, 41, 42, 49, 52, 53, 61, 69, 71, 76, 78–80, 88). NMA with 23 RCTs suggested empagliflozin and dapagliflozin were associated with an increased risk of RTIs, but not for luseogliflozin, ipragliflozin, canagliflozin, ertugliflozin, and remogliflozin. Similar results were obtained from NMA with 17 RCTs conducted in Japan (2, 3, 15–18, 29, 32, 41, 49, 61, 69, 71, 76, 78–80). Two RCTs from China (22, 42) suggested that dapagliflozin but not ertugliflozin was associated with an increased risk of RTIs (Appendix 15.2).
Twelve RCTs (n=2,602) reported 106 (5.9%) and 20 (2.5%) cases of pollakiuria in Asia treated with SGLT-2 inhibitors and placebo, respectively (7, 8, 17, 18, 32, 69, 71, 75, 77, 79–81). NMA with 12 RCTs from Asia and 9 RCTs from Japan (17, 18, 32, 69, 71, 75, 77, 79, 80) suggested that the SGLT-2 inhibitors (empagliflozin and dapagliflozin in Asia and empagliflozin in Japan) were not associated with an increased risk of pollakiuria. Subgroup analyses of other SGLT-2 inhibitors were consistent with the overall analysis (Appendix 15.2).
Fifteen RCTs (n=4,429) reported 52 (1.7%) and 13 (0.9%) cases of hypovolemia (2, 3, 8, 15–17, 22, 29, 31, 53, 61, 69, 71, 80, 84), five RCTs (n=1,450) reported 17 (1. 9%) and 15 (2.7%) cases of renal impairment or failure (18, 42, 49, 52, 53), and 27 RCTs (n=7,411) reported 172 (3.3%) and 63 (2.9%) cases of UTIs (2, 7, 8, 15, 17, 22, 29, 31–33, 41, 42, 49, 52, 53, 61, 69, 71, 75, 76, 78–82, 84, 88) in Asians treated with SGLT-2 inhibitors and placebo, respectively. NMAs of 26 RCTs in Asia and 16 from Japan demonstrated that dapagliflozin and remogliflozin were not associated with an increased risk of UTIs. Other outcomes in Asia and Japan were consistent with the overall analysis (Appendix 15.2).
Subgroup analyses were performed for the 13 studies focusing on T2DM with CKD (eGFR<90 ml/min/1.73m2) (96–106, 108, 120). Similar results were obtained regarding pollakiuria, renal impairment or failure, fracture, and severe hypoglycemia compared to the overall analyses. However, opposite results were obtained regarding RTIs for empagliflozin, dapagliflozin, and sotagliflozin; hypovolemia for ertugliflozin and luseogliflozin; AKIs for dapagliflozin and sotagliflozin; and UTIs, DKA, and amputation for dapagliflozin in the subgroup analyses compared to the overall analyses (Appendix 15.3).
Sensitivity analyses of SGLT-2 inhibitors as an add-on therapy to metformin-based treatment showed similar results for hypovolemia and renal impairment or failure compared to the overall analyses. Fewer included SGLT-2 inhibitors (canagliflozin, dapagliflozin, empagliflozin, ertugliflozin, ipragliflozin, and remogliflozin) were associated with risk of RTIs [dapagliflozin (OR 5.06, 95%CI 1.21-54.57) and empagliflozin (OR 10.86, 95%CI 2.52-116.23)]. All included SGLT-2 inhibitors were not associated with a risk of pollakiuria (canagliflozin, empagliflozin, and ipragliflozin) and UTIs (canagliflozin, dapagliflozin, empagliflozin, ertugliflozin, ipragliflozin, sotaglifozin, tofogliflozin, and remogliflozin). Details are shown in Appendix 16.1.
Subgroup analyses of drug-naive patients showed similar outcome results for pollakiuria, hypovolemia, and renal impairment or failure as the overall analysis. The results were similar to metformin-based treatment (Appendix 16.1).
The risks of RTIs (canagliflozin, dapagliflozin, ertugliflozin, empagliflozin), pollakiuria (canagliflozin and empagliflozin), hypovolemia (canagliflozin, dapagliflozin, ertugliflozin, empagliflozin) and UTIs (canagliflozin, dapagliflozin, ertugliflozin, empagliflozin, expect dapagliflozin in short-term follow-up studies) of the included SGL-2 inhibitors were consistent with the overall analysis regardless of the follow-up time (Appendix 16.2).
Only four head-to-head RCTs (7, 8, 88, 112) compared individual SGLT-2 inhibitors in T2DM. The comparative safety of specific SGLT-2 inhibitors remains unclear. NMA is an increasingly popular tool for comparative effectiveness or safety research. Three NMAs have compared the safety profiles of different SGLT-2 inhibitors regarding UTIs, focusing mainly on canagliflozin, empagliflozin, and dapagliflozin (6, 9, 10). A study compared the risk of RTIs, UTIs, and hypoglycemia among dapagliflozin, canagliflozin, and empagliflozin in patients with T2DM (6). Another study compared the risk of hypovolemia among dapagliflozin, canagliflozin, and empagliflozin in T2DM (10). The third study compared the risk of UTIs among dapagliflozin, canagliflozin, empagliflozin, ertugliflozin, bexagliflozin, and sotagliflozin in T2DM patients with CKD (9). This is the first comprehensive analysis comparing safety evidence of nine SGLT-2 inhibitors in patients with T2DM regarding ten adverse events (especially new outcomes: pollakiuria, renal impairment or failure, and AKI).
Most of the included studies reported RTIs (79 studies), pollakiuria (25 studies), hypovolemia (42 studies), renal impairment or failure (21 studies), and UTIs (89 studies). Few included studies reported AKI (9 studies), fracture (20 studies), DKA (7 studies), amputation (4 studies), and severe hypoglycemia (15 studies). Most patients were treated with canagliflozin, dapagliflozin, empagliflozin, ipragliflozin, and ertugliflozin. Few included studies enrolled patients treated with remogliflozin, sotagliflozin, tofogliflozin, and luseogliflozin. Therefore, outcomes based on a few studies, especially those with wider confidence intervals, should be interpreted cautiously. Further verification from more high-quality and large-sample studies is necessary.
Luseogliflozin and ipragliflozin were not associated with an increased risk of RTIs. Therefore, not all SGLT-2 inhibitors increased the risk of RTIs, which differed from a previous study (6). The participants in the luseogliflozin trial were all Japanese, and most of the participants included in the ipragliflozin trial were Japanese. SGLT-2 inhibitors seem safer in the Asian population, and the association of luseogliflozin and ipragliflozin with the risk of RTIs should be studied in more ethnic groups. The subgroup analysis indicated that individual SGLT-2 inhibitors were not associated with the risk of RTIs in Asia. A meta-analysis also showed that SGLT-2 inhibitors were associated with a similar risk of RTIs compared to placebo in Japanese patients with T2DM (122).
The subgroup analysis showed that the risk of RTIs increased with increasing doses of dapagliflozin or ertugliflozin. Due to the few included studies and the few events, several doses of SGLT-2 inhibitors showed inconsistent results with wide confidence intervals and, therefore, should be interpreted cautiously.
Dapagliflozin and empagliflozin increased the risk of pollakiuria in T2DM compared to placebo (with incidence rates of 6.73% and 3.89%). Similar results were also shown in the subgroup analyses of CKD and drug-naive patients. However, individual SGLT-2 inhibitors were not associated with a risk of pollakiuria in Asia. Several real-world studies from Asia have also shown lower pollakiuria rates in patients treated with SGLT-2 inhibitors. A Korean post-marketing surveillance study of empagliflozin (10 and 25 mg) revealed that the most common adverse event was pollakiuria, with incidence rates of 0.59% (123). A Japanese post-marketing surveillance study of 100 mg of canagliflozin showed that the most common adverse event was pollakiuria, with an incidence rate of 0.79% (124). A 36-month post-marketing surveillance study found that the pollakiuria incidence rate of tofogliflozin was 1.3% in Japanese patients (125). A study found that the increase in urine output was transient, with a return to baseline on day 2 to day 5 of treatment (126). Therefore, pollakiuria may be tolerated over time.
The nine SGLT-2 inhibitors were not associated with the risk of hypovolemia, renal impairment or failure, fracture, DKA, amputation, and severe hypoglycemia compared to the placebo. Two meta-analyses found that the SGLT-2 inhibitor class was associated with an increased risk of hypovolemia, which differs from our study (127, 128). The subgroup analysis showed that canagliflozin 300 mg was associated with a significantly increased risk of hypovolemia, consistent with a previous meta-analysis (10).
Remogliflozin and dapagliflozin were associated with an increased risk of UTIs. Dapagliflozin 10 mg/d increased the risk of UTIs compared to placebo and empagliflozin 25 mg/d (6). However, a meta-analysis of three RCTs suggested that remogliflozin was not associated with UTIs. Differences may be caused by effect sizes (relative risk versus OR) (129). The subgroup analysis indicated that individual SGLT-2 inhibitors were not associated with the risk of UTIs in Asia.
A 3-year Japanese post-marketing surveillance study showed that drug-naive patients had significantly lower incidences of adverse events (10.81% vs. 20.87%; P < 0.001) and serious adverse events (0.86% vs. 2.09%; P < 0.001) compared to non-naive patients, as well as significantly lower incidences of pollakiuria, volume depletion-related events, and kidney disorders (130). Sensitivity analysis showed that adverse drug reactions were similar between SGLT-2 inhibitor monotherapy and add-on therapies to metformin. Few SGLT-2i were associated with the risk of RTIs, pollakiuria and UTIs compared to overall analysis, which should be interpreted with caution, as it could be affected by the number of studies and sample sizes.
Although the included studies had follow-up times ranging from 12 to 338 weeks, the median duration was 24 weeks. The sensitivity analysis based on the follow-up time showed broadly consistent results. The incidence of related adverse events in extended follow-up studies was higher than in short-term studies because the sample size was unchanged and the number of events accumulated. A 3-year Japanese post-marketing surveillance study showed that the long-term safety profile of ipragliflozin treatment in routine clinical practice was consistent with previously reported interim data at 12 or 24 months and pre-approval clinical trials (131).
The present NMA included all available evidence on the safety outcomes of all SGLT-2 inhibitors in patients with T2DM. Considering the homogeneity of the included studies, we deliberately excluded studies that focus on specific populations (such as T2DM with heart failure or BMI≥35 kg/m2 or years of age > 65 or with CKD). Meanwhile, studies with a sample size of less than 50 or with a study period of fewer than 12 weeks were excluded. Our study has several limitations. First, most of the included studies were individual SGLT-2 inhibitors versus placebo, and only four studies were conducted to compare different SGLT-2 inhibitors. Direct comparisons contributed little to these NMA results, resulting in wider CIs, greater uncertainty, and lower confidence in the evidence evaluated by CINeMA. Second, most of the included studies had a relatively small number of patients (less than 300), only ten studies had a larger sample size of 500-9,000. Third, given the limited availability of data on individual SGLT-2 inhibitors or subgroup analysis, caution is recommended when interpreting these results.
Not all SGLT-2 inhibitors increased the risk of RTIs. Luseogliflozin and ipragliflozin were not associated with an increased risk of RTIs. Dapagliflozin ranked first in increasing the risk of RTIs. Dapagliflozin and empagliflozin increased the risk of pollakiuria. Remogliflozin and dapagliflozin increased the risk of UTIs, and remogliflozin ranked first. SGLT-2 inhibitors were not associated with the risk of hypovolemia, renal impairment or failure, fracture, DKA, amputation, and severe hypoglycemia compared to placebo. Active-controlled trials comparing SGLT2 inhibitors are urgently needed to validate the estimates of the comparative safety produced in this network meta-analysis.
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.
CXL, HL, LYL and SL designed the study. CXL, LYL and CXZ set up the database. LYL, CXZ, XHG, QX, SMG, and YQW screened the literature search, acquired reports of relevant trials, selected included studies, and extracted data. CXL, LYL and CXZ did all statistical analyses, analyzed and interpreted the data and drafted the report. All authors critically reviewed the report for important intellectual content and approved the final submitted version.
The project supported by Youth Innovation Fund of Aerospace Center Hospital (grant number 2022QN08)
We thank all study authors who responded to our data requests. We thank Suying Yan, Hao Lu and Tiantian Liu for help in the article polishing.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2023.1238399/full#supplementary-material
SGLT-2, sodium-glucose transporter 2; NMA, network meta-analysis; T2D, type 2 diabetes; RCTs, randomized controlled trials; CINeMA, Confidence In Network Meta-Analysis; RTIs, reproductive tract infections; UTIs, urinary tract infections; AKI, acute kidney injury; DKA, diabetic ketoacidosis; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; PICOS, participants, intervention, comparison, outcomes and characteristics and study design; OR, odds ratio; CI, confidence interval; PSRF, potential scale reduction factor; SUCRA, the surface under the cumulative ranking scores; CKD, chronic kidney disease; eGFR, estimated glomerular filtration rate; ADRs, adverse drug reactions; oGLD, the other glucose-lowering drug.
1. Buse JB, Wexler DJ, Tsapas A, Rossing P, Mingrone G, Mathieu C, et al. 2019 update to: management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American diabetes association (ADA) and the European association for the study of diabetes (EASD). Diabetes Care (2020) 43(2):487–93. doi: 10.2337/dc20–er07
2. Kaku K, Watada H, Iwamoto Y, Utsunomiya K, Terauchi Y, Tobe K, et al. Efficacy and safety of monotherapy with the novel sodium/glucose cotransporter–2 inhibitor tofogliflozin in Japanese patients with type 2 diabetes mellitus: a combined Phase 2 and 3 randomized, placebo–controlled, double–blind, parallel–group comparative study. Cardiovasc Diabetol (2014) 13(1):65. doi: 10.1186/1475–2840–13–65
3. Seino Y, Sasaki T, Fukatsu A, Sakai S, Samukawa Y. Efficacy and safety of luseogliflozin monotherapy in Japanese patients with type 2 diabetes mellitus: a 12–week, randomized, placebo–controlled, phase II study. Curr Med Res Opin (2014) 30(7):1219–30. doi: 10.1185/03007995.2014.901943
4. Rosenstock J, Frias J, Pall D, Charbonnel B, Pascu R, Saur D, et al. Effect of ertugliflozin on glucose control, body weight, blood pressure and bone density in type 2 diabetes mellitus inadequately controlled on metformin monotherapy (VERTIS MET). Diabetes Obes Metab (2018) 20(3):520–9. doi: 10.1111/dom.13103
5. List JF, Woo V, Morales E, Tang W, Fiedorek FT. Sodium–glucose cotransport inhibition with dapagliflozin in type 2 diabetes. Diabetes Care (2009) 32(4):650–7. doi: 10.2337/dc08–1863
6. Zaccardi F, Webb DR, Htike ZZ, Youssef D, Khunti K, Davies MJ. Efficacy and safety of sodium–glucose co–transporter–2 inhibitors in type 2 diabetes mellitus: systematic review and network meta–analysis. Diabetes Obes Metab (2016) 18(8):783–94. doi: 10.1111/dom.12670
7. Hussain M, Atif M, Babar M, Akhtar L. Comparison of efficacy and safety profile of empagliflozin versus dapagliflozin as add on therapy in type 2 diabetic patients. J Ayub Med College Abbottabad (2021) 33(4):593–7.
8. Hussain M, Elahi A, Iqbal J, Bilal Ghafoor M, Rehman H, Akhtar S. Comparison of efficacy and safety profile of sodium–glucose cotransporter–2 inhibitors as add–on therapy in patients with type 2 diabetes. Cureus (2021) 13(4):e14268. doi: 10.7759/cureus.14268
9. Lin J, Wang S, Wen T, Zhang X. Renal protective effect and safety of sodium–glucose cotransporter–2 inhibitors in patients with chronic kidney disease and type 2 diabetes mellitus: a network meta–analysis and systematic review. Int Urol Nephrol (2022) 54(9):2305–16. doi: 10.1007/s11255–022–03117–4
10. Jiang Y, Yang P, Fu L, Sun L, Shen W, Wu Q. Comparative cardiovascular outcomes of SGLT2 inhibitors in type 2 diabetes mellitus: A network meta–analysis of randomized controlled trials. Front Endocrinol (Lausanne) (2022) 13:802992. doi: 10.3389/fendo.2022.802992
11. Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta–analyses of health care interventions: checklist and explanations. Ann Intern Med (2015) 162(11):777–84. doi: 10.7326/M14–2385
12. Sterne JAC SJ, Page MJ, Elbers RG, Blencowe NS, Boutron I, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ (2019) 28:366. doi: 10.1136/bmj.l4898
13. Nikolakopoulou A, Higgins JPT, Papakonstantinou T, Chaimani A, Del Giovane C, Egger M, et al. CINeMA: An approach for assessing confidence in the results of a network meta–analysis. PloS Med (2020) 17(4):e1003082. doi: 10.1371/journal.pmed.1003082
14. Ikeda S, Takano Y, Cynshi O, Tanaka R, Christ AD, Boerlin V, et al. A novel and selective sodium–glucose cotransporter–2 inhibitor, tofogliflozin, improves glycaemic control and lowers body weight in patients with type 2 diabetes mellitus. Diabetes Obes Metab (2015) 17(10):984–93. doi: 10.1111/dom.12538
15. Terauchi Y, Tamura M, Senda M, Gunji R, Kaku K. Efficacy and safety of tofogliflozin in Japanese patients with type 2 diabetes mellitus with inadequate glycaemic control on insulin therapy (J–STEP/INS): results of a 16–week randomized, double–blind, placebo–controlled multicentre trial. Diabetes Obes Metab (2017) 19(10):1397–407. doi: 10.1111/dom.12957
16. Seino Y, Sasaki T, Fukatsu A, Ubukata M, Sakai S, Samukawa Y. Dose–finding study of luseogliflozin in Japanese patients with type 2 diabetes mellitus: a 12–week, randomized, double–blind, placebo–controlled, phase II study. Curr Med Res Opin (2014) 30(7):1231–44. doi: 10.1185/03007995.2014.909390
17. Seino Y, Sasaki T, Fukatsu A, Imazeki H, Ochiai H, Sakai S. Efficacy and safety of luseogliflozin added to insulin therapy in Japanese patients with type 2 diabetes: a multicenter, 52–week, clinical study with a 16–week, double–blind period and a 36–week, open–label period. Curr Med Res Opin (2018) 34(6):981–94. doi: 10.1080/03007995.2018.1441816
18. Seino Y, Sasaki T, Fukatsu A, Ubukata M, Sakai S, Samukawa Y. Efficacy and safety of luseogliflozin as monotherapy in Japanese patients with type 2 diabetes mellitus: a randomized, double–blind, placebo–controlled, phase 3 study. Curr Med Res Opin (2014) 30(7):1245–55. doi: 10.1185/03007995.2014.912983
19. Amin NB, Wang X, Jain SM, Lee DS, Nucci G, Rusnak JM. Dose–ranging efficacy and safety study of ertugliflozin, a sodium–glucose co–transporter 2 inhibitor, in patients with type 2 diabetes on a background of metformin. Diabetes Obes Metab (2015) 17(6):591–8. doi: 10.1111/dom.12460
20. Terra SG, Focht K, Davies M, Frias J, Derosa G, Darekar A, et al. efficacy and safety study of ertugliflozin monotherapy in people with type 2 diabetes mellitus inadequately controlled with diet and exercise alone. Diabetes Obes Metab (2017) 19(5):721–8. doi: 10.1111/dom.12888
21. Dagogo–Jack S, Liu J, Eldor R, Amorin G, Johnson J, Hille D, et al. Efficacy and safety of the addition of ertugliflozin in patients with type 2 diabetes mellitus inadequately controlled with metformin and sitagliptin: the VERTIS SITA2 placebo–controlled randomized study. Diabetes Obes Metab (2018) 20(3):530–40. doi: 10.1111/dom.13116
22. Ji L, Liu Y, Miao H, Xie Y, Yang M, Wang W, et al. Safety and efficacy of ertugliflozin in Asian patients with type 2 diabetes mellitus inadequately controlled with metformin monotherapy: VERTIS Asia. Diabetes Obes Metab (2019) 21(6):1474–82. doi: 10.1111/dom.13681
23. Cannon CP, Pratley R, Dagogo–Jack S, Mancuso J, Huyck S, Masiukiewicz U, et al. Cardiovascular outcomes with ertugliflozin in type 2 diabetes. New Engl J Med (2020) 383(15):1425–35. doi: 10.1056/NEJMoa2004967
24. Rosenstock J, Aggarwal N, Polidori D, Zhao Y, Arbit D, Usiskin K, et al. Dose–ranging effects of canagliflozin, a sodium–glucose cotransporter 2 inhibitor, as add–on to metformin in subjects with type 2 diabetes. Diabetes Care (2012) 35(6):1232–8. doi: 10.2337/dc11–1926
25. Inagaki N, Kondo K, Yoshinari T, Maruyama N, Susuta Y, Kuki H. Efficacy and safety of canagliflozin in Japanese patients with type 2 diabetes: a randomized, double–blind, placebo–controlled, 12–week study. Diabetes Obes Metab (2013) 15(12):1136–45. doi: 10.1111/dom.12149
26. Bode B, Stenlöf K, Sullivan D, Fung A, Usiskin K. Efficacy and safety of canagliflozin treatment in older subjects with type 2 diabetes mellitus: a randomized trial. . Hosp Pract (1995) 41(2):72–84. doi: 10.3810/hp.2013.04.1020
27. Stenlöf K, Cefalu WT, Kim KA, Alba M, Usiskin K, Tong C, et al. Efficacy and safety of canagliflozin monotherapy in subjects with type 2 diabetes mellitus inadequately controlled with diet and exercise. Diabetes Obes Metab (2013) 15(4):372–82. doi: 10.1111/dom.12054
28. Wilding JP, Charpentier G, Hollander P, González–Gálvez G, Mathieu C, Vercruysse F, et al. Efficacy and safety of canagliflozin in patients with type 2 diabetes mellitus inadequately controlled with metformin and sulphonylurea: a randomised trial. Int J Clin Pract (2013) 67(12):1267–82. doi: 10.1111/ijcp.12322
29. Inagaki N, Kondo K, Yoshinari T, Takahashi N, Susuta Y, Kuki H. Efficacy and safety of canagliflozin monotherapy in Japanese patients with type 2 diabetes inadequately controlled with diet and exercise: A 24–week, randomized, double–blind, placebo–controlled, Phase III study. Expert Opin Pharmacother (2014) 15(11):1501–15. doi: 10.1517/14656566.2014.935764
30. Qiu R, Capuano G, Meininger G. Efficacy and safety of twice–daily treatment with canagliflozin, a sodium glucose co–transporter 2 inhibitor, added on to metformin monotherapy in patients with type 2 diabetes mellitus. J Clin Trans Endocrinol (2014) 1(2):54–60. doi: 10.1016/j.jcte.2014.04.001
31. Ji L, Han P, Liu Y, Yang G, Dieu Van NK, Vijapurkar U, et al. Canagliflozin in Asian patients with type 2 diabetes on metformin alone or metformin in combination with sulphonylurea. Diabetes Obes Metab (2015) 17(1):23–31. doi: 10.1111/dom.12385
32. Inagaki N, Harashima SI, Maruyama N, Kawaguchi Y, Goda M, Iijima H. Efficacy and safety of canagliflozin in combination with insulin: a double–blind, randomized, placebo–controlled study in Japanese patients with type 2 diabetes mellitus. Cardiovasc Diabetol (2016) 5:89. doi: 10.1186/s12933–016–0407–4
33. Kadowaki T, Inagaki N, Kondo K, Nishimura K, Kaneko G, Maruyama N, et al. Efficacy and safety of canagliflozin as add–on therapy to teneligliptin in Japanese patients with type 2 diabetes mellitus: results of a 24–week, randomized, double–blind, placebo–controlled trial. Diabetes Obes Metab (2017) 19(6):874–82. doi: 10.1111/dom.12898
34. Bailey CJ, Gross JL, Pieters A, Bastien A, List JF. Effect of dapagliflozin in patients with type 2 diabetes who have inadequate glycaemic control with metformin: a randomised, double–blind, placebo–controlled trial. Lancet (2010) 375(9733):2223–33. doi: 10.1016/S0140–673610()60407–2
35. Ferrannini E, Ramos SJ, Salsali A, Tang W, List JF. Dapagliflozin monotherapy in type 2 diabetic patients with inadequate glycemic control by diet and exercise: A randomized, double–blind, placebo–controlled, phase 3 trial. Diabetes Care (2010) 33(10):2217–24. doi: 10.2337/dc10–0612
36. Strojek K, Yoon KH, Hruba V, Elze M, Langkilde AM, Parikh S. Effect of dapagliflozin in patients with type 2 diabetes who have inadequate glycaemic control with glimepiride: A randomized, 24–week, double–blind, placebo–controlled trial. Diabetes Obes Metab (2011) 13(10):928–38. doi: 10.1111/j.1463–1326.2011.01434.x
37. Bailey CJ, Iqbal N, T'Joen C, List JF. Dapagliflozin monotherapy in drug–naïve patients with diabetes: a randomized–controlled trial of low–dose range. Diabetes Obes Metab (2012) 14(10):951–9. doi: 10.1111/j.1463–1326.2012.01659.x
38. Bolinder J, Ljunggren Ö, Kullberg J, Johansson L, Wilding J, Langkilde AM, et al. Effects of dapagliflozin on body weight, total fat mass, and regional adipose tissue distribution in patients with type 2 diabetes mellitus with inadequate glycemic control on metformin. J Clin Endocrinol Metab (2012) 97(3):1020–31. doi: 10.1210/jc.2011–2260
39. Rosenstock J, Vico M, Wei L, Salsali A, List JF. Effects of dapagliflozin, an SGLT2 inhibitor, on HbA(1c), body weight, and hypoglycemia risk in patients with type 2 diabetes inadequately controlled on pioglitazone monotherapy. Diabetes Care (2012) 35(7):1473–8. doi: 10.2337/dc11–1693
40. Wilding JP, Woo V, Soler NG, Pahor A, Sugg J, Rohwedder K, et al. Dapagliflozin 006 Study Group. Long–term efficacy of dapagliflozin in patients with type 2 diabetes mellitus receiving high doses of insulin: a randomized trial. . Ann Intern Med (2012) 156(6):405–15. doi: 10.7326/0003–4819–156–6–201203200–00003
41. Kaku K, Inoue S, Matsuoka O, Kiyosue A, Azuma H, Hayashi N, et al. Efficacy and safety of dapagliflozin as a monotherapy for type 2 diabetes mellitus in Japanese patients with inadequate glycaemic control: A phase II multicentre, randomized, double–blind, placebo–controlled trial. Diabetes Obes Metab (2013) 15(5):432–40. doi: 10.1111/dom.12047
42. Ji L, Ma J, Li H, Mansfield TA, T'Joen CL, Iqbal N, et al. Dapagliflozin as monotherapy in drug–naive Asian patients with type 2 diabetes mellitus: a randomized, blinded, prospective phase III study. Clin Ther (2014) 36(1):84–100.e109. doi: 10.1016/j.clinthera.2013.11.002
43. Leiter LA, Cefalu WT, De Bruin TWA, Gause–Nilsson I, Sugg J, Parikh SJ, et al. Dapagliflozin added to usual care in individuals with type 2 diabetes mellitus with preexisting cardiovascular disease: A 24–week, multicenter, randomized, double–blind, placebo–controlled study with a 28–week extension. J Am Geriatrics Soc (2014) 62(7):1252–62. doi: 10.1111/jgs.12881
44. Bailey CJ, Morales Villegas EC, Woo V, Tang W, Ptaszynska A, List JF. Efficacy and safety of dapagliflozin monotherapy in people with Type 2 diabetes: a randomized double–blind placebo–controlled 102–week trial. Diabetes Med (2015) 32(4):531–41. doi: 10.1111/dme.12624
45. Cefalu WT, Leiter LA, De Bruin TWA, Gause–Nilsson I, Sugg J, Parikh SJ, et al. Dapagliflozin's effects on glycemia and cardiovascular risk factors in high–risk patients with type 2 diabetes: A 24–week, multicenter, randomized, double–blind, placebo–controlled study with a 28–week extension. Diabetes Care (2015) 38(7):1218–27. doi: 10.2337/dc14–0315
46. Mathieu C, Ranetti AE, Li D, Ekholm E, Cook W, Hirshberg B, et al. Randomized, double–blind, phase 3 trial of triple therapy with dapagliflozin add–on to saxagliptin plus metformin in type 2 diabetes. Diabetes Care (2015) 38(11):2009–17. doi: 10.2337/dc15–0779
47. Matthaei S, Bowering K, Rohwedder K, Grohl A, Parikh S. Study 05 Group. Dapagliflozin improves glycemic control and reduces body weight as add–on therapy to metformin plus sulfonylurea: a 24–week randomized, double–blind clinical trial. Diabetes Care (2015) 38(3):365–72. doi: 10.2337/dc14–0666
48. Schumm–Draeger PM, Burgess L, Korányi L, Hruba V, Hamer–Maansson JE, de Bruin TW. Twice–daily dapagliflozin co–administered with metformin in type 2 diabetes: a 16–week randomized, placebo–controlled clinical trial. Diabetes Obes Metab (2015) 17(1):42–51. doi: 10.1111/dom.12387
49. Araki E, Onishi Y, Asano M, Kim H, Ekholm E, Johnsson E, et al. Efficacy and safety of dapagliflozin in addition to insulin therapy in Japanese patients with type 2 diabetes: Results of the interim analysis of 16–week double–blind treatment period. J Diabetes Invest (2016) 7(4):555–64. doi: 10.1111/jdi.12453
50. Weber MA, Mansfield TA, Alessi F, Iqbal N, Parikh S, Ptaszynska A. Effects of dapagliflozin on blood pressure in hypertensive diabetic patients on renin–angiotensin system blockade. Blood Press (2016) 25(2):93–103. doi: 10.3109/08037051.2015.1116258
51. Weber MA, Mansfield TA, Cain VA, Iqbal N, Parikh S, Ptaszynska A. Blood pressure and glycaemic effects of dapagliflozin versus placebo in patients with type 2 diabetes on combination antihypertensive therapy: a randomised, double–blind, placebo–controlled, phase 3 study. Lancet Diabetes Endocrinol (2016) 4(3):211–20. doi: 10.1016/S2213–858715()00417–9
52. Yang W, Han P, Min KW, Wang B, Mansfield T, T'Joen C, et al. Efficacy and safety of dapagliflozin in Asian patients with type 2 diabetes after metformin failure: A randomized controlled trial. J Diabetes (2016) 8(6):796–808. doi: 10.1111/1753–0407.12357
53. Yang W, Ma J, Li Y, Li Y, Zhou Z, Kim JH, et al. Dapagliflozin as add–on therapy in Asian patients with type 2 diabetes inadequately controlled on insulin with or without oral antihyperglycemic drugs: A randomized controlled trial. J Diabetes (2018) 10(7):589–99. doi: 10.1111/1753–0407.12634
54. Wiviott SD, Mosenzon O, Moist L. Dapagliflozin reduced cardiorenal outcomes but not MACE in T2 diabetes with or at risk for atherosclerotic CVD. Ann Internal Med (2019) 171(8):JC43. doi: 10.7326/ACPJ201910150–043
55. Frías JP, Guja C, Hardy E, Ahmed A, Dong F, Öhman P, et al. Exenatide once weekly plus dapagliflozin once daily versus exenatide or dapagliflozin alone in patients with type 2 diabetes inadequately controlled with metformin monotherapy (DURATION–8): a 28 week, multicentre, double–blind, phase 3, randomised controlled trial. Lancet Diabetes Endocrinol (2016) 41(2):1004–16. doi: 10.1016/S2213–858716()30267–4
56. Ferrannini E, Seman L, Seewaldt–Becker E, Hantel S, Pinnetti S, Woerle HJ. A Phase IIb, randomized, placebo–controlled study of the SGLT2 inhibitor empagliflozin in patients with type 2 diabetes. Diabetes Obes Metab (2013) 15(8):721–8. doi: 10.1111/dom.12081
57. Häring HU, Merker L, Seewaldt–Becker E, Weimer M, Meinicke T, Woerle HJ, et al. EMPA–REG METSU Trial Investigators. Empagliflozin as add–on to metformin plus sulfonylurea in patients with type 2 diabetes: a 24–week, randomized, double–blind, placebo–controlled trial. Diabetes Care (2013) 36(11):3396–404. doi: 10.2337/dc12–2673
58. Roden M, Weng J, Eilbracht J, Delafont B, Kim G, Woerle HJ, et al. EMPA–REG MONO trial investigators. Empagliflozin monotherapy with sitagliptin as an active comparator in patients with type 2 diabetes: a randomised, double–blind, placebo–controlled, phase 3 trial. . Lancet Diabetes Endocrinol (2013) 1(3):208–19. doi: 10.1016/S2213–858713()70084–6
59. Rosenstock J, Seman LJ, Jelaska A, Hantel S, Pinnetti S, Hach T, et al. Efficacy and safety of empagliflozin, a sodium glucose cotransporter 2 (SGLT2) inhibitor, as add–on to metformin in type 2 diabetes with mild hyperglycaemia. Diabetes Obes Metab (2013) 15(12):1154–60. doi: 10.1111/dom.12185
60. Häring HU, Merker L, Seewaldt–Becker E, Weimer M, Meinicke T, Broedl UC, et al. EMPA–REG MET Trial Investigators. Empagliflozin as add–on to metformin in patients with type 2 diabetes: a 24–week, randomized, double–blind, placebo–controlled trial. Diabetes Care (2014) 37(6):1650–9. doi: 10.2337/dc13–2105
61. Kadowaki T, Haneda M, Inagaki N, Terauchi Y, Taniguchi A, Koiwai K, et al. Empagliflozin monotherapy in Japanese patients with type 2 diabetes mellitus: A randomized, 12–week, double–blind, placebo–controlled, phase II trial. Adv Ther (2014) 31(6):621–38. doi: 10.1007/s12325–014–0126–8
62. Kovacs CS, Seshiah V, Swallow R, Jones R, Rattunde H, Woerle HJ, et al. EMPA–REG PIO™ trial investigators. Empagliflozin improves glycaemic and weight control as add–on therapy to pioglitazone or pioglitazone plus metformin in patients with type 2 diabetes: a 24–week, randomized, placebo–controlled trial. Diabetes Obes Metab (2014) 16(2):147–58. doi: 10.1111/dom.12188
63. Merker L, Häring HU, Christiansen AV, Roux F, Salsali A, Kim G, et al. Empagliflozin as add–on to metformin in people with Type 2 diabetes. Diabetes Med (2015) 32(12):1555–67. doi: 10.1111/dme.12814
64. Rosenstock J, Jelaska A, Zeller C, Kim G, Broedl UC, Woerle HJ, et al. Impact of empagliflozin added on to basal insulin in type 2 diabetes inadequately controlled on basal insulin: A 78–week randomized, double–blind, placebo–controlled trial. Diabetes Obes Metab (2015) 17(10):936–48. doi: 10.1111/dom.12503
65. Ross S, Thamer C, Cescutti J, Meinicke T, Woerle HJ, Broedl UC. Efficacy and safety of empagliflozin twice daily versus once daily in patients with type 2 diabetes inadequately controlled on metformin: a 16–week, randomized, placebo–controlled trial. Diabetes Obes Metab (2015) 17(7):699–702. doi: 10.1111/dom.12469
66. Tikkanen I, Narko K, Zeller C, Green A, Salsali A, Broedl UC, et al. EMPA–REG BP Investigators. Empagliflozin reduces blood pressure in patients with type 2 diabetes and hypertension. Diabetes Care (2015) 38(3):420–8. doi: 10.2337/dc14–1096
67. Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. New Engl J Med (2015) 373(22):2117–28. doi: 10.1056/NEJMoa1504720
68. Søfteland E, Meier JJ, Vangen B, Toorawa R, Maldonado–Lutomirsky M, Broedl UC. Empagliflozin as add–on therapy in patients with type 2 diabetes inadequately controlled with linagliptin and metformin: A 24–week randomized, double–blind, parallel–group trial. Diabetes Care (2017) 40(2):201–9. doi: 10.2337/dc16–1347
69. Kawamori R, Haneda M, Suzaki K, Cheng G, Shiki K, Miyamoto Y, et al. Empagliflozin as add–on to linagliptin in a fixed–dose combination in Japanese patients with type 2 diabetes: glycaemic efficacy and safety profile in a 52–week, randomized, placebo–controlled trial. Diabetes Obes Metab (2018) 20(9):2200–9. doi: 10.1111/dom.13352
70. Ferdinand KC, Izzo JL, Lee J, Meng L, George J, Salsali A, et al. Antihyperglycemic and blood pressure effects of empagliflozin in black patients with type 2 diabetes mellitus and hypertension. Circulation (2019) 139(18):2098–109. doi: 10.1161/CIRCULATIONAHA.118.036568
71. Sone H, Kaneko T, Shiki K, Tachibana Y, Pfarr E, Lee J, et al. Efficacy and safety of empagliflozin as add–on to insulin in Japanese patients with type 2 diabetes: A randomized, double–blind, placebo–controlled trial. Diabetes Obes Metab (2020) 22(3):417–26. doi: 10.1111/dom.13909
72. Rodbard HW, Seufert J, Aggarwal N, Cao A, Fung A, Pfeifer M, et al. Efficacy and safety of titrated canagliflozin in patients with type 2 diabetes mellitus inadequately controlled on metformin and sitagliptin. Diabetes Obes Metab (2016) 18(8):812–9. doi: 10.1111/dom.12684
73. Fonseca VA, Ferrannini E, Wilding JP, Wilpshaar W, Dhanjal P, Ball G, et al. Active– and placebo–controlled dose–finding study to assess the efficacy, safety, and tolerability of multiple doses of ipragliflozin in patients with type 2 diabetes mellitus. J Diabetes Complications (2013) 27(3):268–73. doi: 10.1016/j.jdiacomp.2012.11.005
74. Wilding JP, Ferrannini E, Fonseca VA, Wilpshaar W, Dhanjal P, Houzer A. Efficacy and safety of ipragliflozin in patients with type 2 diabetes inadequately controlled on metformin: a dose–finding study. Diabetes Obes Metab (2013) 15(5):403–9. doi: 10.1111/dom.12038
75. Kashiwagi A, Kazuta K, Yoshida S, Nagase I. Randomized, placebo–controlled, double–blind glycemic control trial of novel sodium–dependent glucose cotransporter 2 inhibitor ipragliflozin in Japanese patients with type 2 diabetes mellitus. J Diabetes Invest (2014) 5(4):382–91. doi: 10.1111/jdi.12156
76. Kashiwagi A, Akiyama N, Shiga T, Kazuta K, Utsuno A, Yoshida S, et al. Efficacy and safety of ipragliflozin as an add–on to a sulfonylurea in Japanese patients with inadequately controlled type 2 diabetes: results of the randomized, placebo–controlled, double–blind, phase III EMIT study. Diabetol Int (2015) 6(2):125–38. doi: 10.1007/s13340–014–0184–9
77. Kashiwagi A, Kazuta K, Goto K, Yoshida S, Ueyama E, Utsuno A. Ipragliflozin in combination with metformin for the treatment of Japanese patients with type 2 diabetes: ILLUMINATE, a randomized, double–blind, placebo–controlled study. Diabetes Obes Metab (2015) 17(3):304–8. doi: 10.1111/dom.12331
78. Kashiwagi A, Kazuta K, Takinami Y, Yoshida S, Utsuno A, Nagase I. Ipragliflozin improves glycemic control in Japanese patients with type 2 diabetes mellitus: the BRIGHTEN study: BRIGHTEN: double–blind randomized study of ipragliflozin to show its efficacy as monotherapy in T2DM patients. Diabetol Int (2015) 6(1):8–18. doi: 10.1007/s13340–014–0164–0
79. Kashiwagi A, Shiga T, Akiyama N, Kazuta K, Utsuno A, Yoshida S, et al. Efficacy and safety of ipragliflozin as an add–on to pioglitazone in Japanese patients with inadequately controlled type 2 diabetes: a randomized, double–blind, placebo–controlled study (the SPOTLIGHT study). Diabetol Int (2015) 6(2):104–16. doi: 10.1007/s13340–014–0182–y
80. Ishihara H, Yamaguchi S, Nakao I, Okitsu A, Asahina S. Efficacy and safety of ipragliflozin as add–on therapy to insulin in Japanese patients with type 2 diabetes mellitus (IOLITE): a multi–centre, randomized, placebo–controlled, double–blind study. Diabetes Obes Metab (2016) 18(12):1207–16. doi: 10.1111/dom.12745
81. Lu CH, Min KW, Chuang LM, Kokubo S, Yoshida S, Cha BS. Efficacy, safety, and tolerability of ipragliflozin in Asian patients with type 2 diabetes mellitus and inadequate glycemic control with metformin: Results of a phase 3 randomized, placebo–controlled, double–blind, multicenter trial. J Diabetes Investig (2016) 7(3):366–73. doi: 10.1111/jdi.12422
82. Han KA, Chon S, Chung CH, Lim S, Lee KW, Baik S, et al. Efficacy and safety of ipragliflozin as an add–on therapy to sitagliptin and metformin in Korean patients with inadequately controlled type 2 diabetes mellitus: A randomized controlled trial. Diabetes Obes Metab (2018) 20(10):2408–15. doi: 10.1111/dom.13394
83. Shestakova MV, Wilding JPH, Wilpshaar W, Tretter R, Orlova VL, Verbovoy AF. A phase 3 randomized placebo–controlled trial to assess the efficacy and safety of ipragliflozin as an add–on therapy to metformin in Russian patients with inadequately controlled type 2 diabetes mellitus. Diabetes Res Clin Pract (2018) 146:240–50. doi: 10.1016/j.diabres.2018.10.018
84. Kaku K, Kadowaki T, Seino Y, Okamoto T, Shirakawa M, Sato A, et al. Efficacy and safety of ipragliflozin in Japanese patients with type 2 diabetes and inadequate glycaemic control on sitagliptin. Diabetes Obes Metab (2021) 23(9):2099–108. doi: 10.1111/dom.14448
85. Rosenstock J, Cefalu WT, Lapuerta P, Zambrowicz B, Ogbaa I, Banks P, et al. Greater dose–ranging effects on A1C levels than on glucosuria with LX4211, a dual inhibitor of SGLT1 and SGLT2, in patients with type 2 diabetes on metformin monotherapy. Diabetes Care (2015) 38(3):431–8. doi: 10.2337/dc14–0890
86. Sykes AP, O'Connor–Semmes R, Dobbins R, Dorey DJ, Lorimer JD, Walker S, et al. Randomized trial showing efficacy and safety of twice–daily remogliflozin etabonate for the treatment of type 2 diabetes. Diabetes Obes Metab (2015) 17(1):94–7. doi: 10.1111/dom.12391
87. Sykes AP, O'Connor–Semmes R, Dobbins R, Dorey DJ, Lorimer JD, Walker S, et al. Randomized trial showing efficacy and safety of twice–daily remogliflozin etabonate for the treatment of type 2 diabetes. Diabetes Obes Metab (2015) 17(1):94–7. doi: 10.1111/dom.12391
88. DharMalingam M, Aravind SR, Thacker H, Paramesh S, Mohan B, Chawla M, et al. Efficacy and safety of remogliflozin etabonate, a new sodium glucose co–transporter–2 inhibitor, in patients with type 2 diabetes mellitus: a 24–week, randomized, double–blind, active–controlled trial. Drugs (2020) 80(6):587–600. doi: 10.1007/s40265–020–01285–0
89. Bailey CJ, Gross JL, Hennicken D, Iqbal N, Mansfield TA, List JF, et al. Dapagliflozin add–on to metformin in type 2 diabetes inadequately controlled with metformin: a randomized, double–blind, placebo–controlled 102–week trial. BMC Med (2013) 11(43):1–10. doi: 10.1186/1741–7015–11–43
90. Strojek K, Yoon KH, Hruba V, Sugg J, Langkilde AM, Parikh S, et al. Dapagliflozin added to glimepiride in patients with type 2 diabetes mellitus sustains glycemic control and weight loss over 48 weeks: A randomized, double–blind, parallel–group, placebo–controlled trial. Diabetes Ther (2014) 5(1):267–83. doi: 10.1007/s13300–014–0072–0
91. Wilding JPH, Woo V, Rohwedder K, Sugg J, Parikh S. Dapagliflozin in patients with type 2 diabetes receiving high doses of insulin: Efficacy and safety over 2 years. Diabetes Obes Metab (2014) 16(2):124–36. doi: 10.1111/dom.12187
92. Jabbour SA, Frías JP, Ahmed A, Hardy E, Choi J, Sjöström CD, et al. Efficacy and safety over 2 years of exenatide plus dapagliflozin in the DURATION–8 study: A multicenter, double–blind, phase 3, randomized controlled trial. Diabetes Care (2020) 43(10):2528–36. doi: 10.2337/dc19–1350
93. Haering HU, Merker L, Christiansen AV, Roux F, Salsali A, Kim G, et al. Empagliflozin as add–on to metformin plus sulphonylurea in patients with type 2 diabetes. Diabetes Res Clin Pract (2015) 110(1):82–90. doi: 10.1016/j.diabres.2015.05.044
94. Kovacs CS, Seshiah V, Merker L, Christiansen AV, Roux F, Salsali A, et al. Empagliflozin as add–on therapy to pioglitazone with or without metformin in patients with type 2 diabetes mellitus. Clin Ther (2015) 37(8):1773–1788.e1771. doi: 10.1016/j.clinthera.2015.05.511
95. Roden M, Merker L, Christiansen AV, Roux F, Salsali A, Kim G, et al. Safety, tolerability and effects on cardiometabolic risk factors of empagliflozin monotherapy in drug–naïve patients with type 2 diabetes: A double–blind extension of a Phase III randomized controlled trial. Cardiovasc Diabetol (2015) 14:154. doi: 10.1186/s12933–015–0314–0
96. Haneda M, Seino Y, Inagaki N, Kaku K, Sasaki T, Fukatsu A, et al. Influence of renal function on the 52–week efficacy and safety of the sodium glucose cotransporter 2 inhibitor luseogliflozin in Japanese patients with type 2 diabetes mellitus. Clin Ther (2016) 38(1):66–88.e20. doi: 10.1016/j.clinthera.2015.10.025
97. Grunberger G, Camp S, Johnson J, Huyck S, Terra SG, Mancuso JP, et al. Ertugliflozin in patients with stage 3 chronic kidney disease and type 2 diabetes mellitus: the VERTIS RENAL randomized study. Diabetes Ther (2018) 9(1):49–66. doi: 10.1007/s13300–017–0337–5
98. Yale JF, Bakris G, Cariou B, Nieto J, David–Neto E, Yue D, et al. Efficacy and safety of canagliflozin over 52 weeks in patients with type 2 diabetes mellitus and chronic kidney disease. Diabetes Obes Metab (2014) 16(10):1016–27. doi: 10.1111/dom.12348
99. Perkovic V, Jardine MJ, Neal B, Bompoint S, Heerspink HJL, Charytan DM, et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. New Engl J Med (2019) 380(24):2295–306. doi: 10.1056/NEJMoa1811744
100. Fioretto P, Del Prato S, Goldenberg R, Giorgino F, Reyner D, Reyner D, et al. Eficacy and safety of dapagliflozin in patients with type 2 diabetes and moderate renal impairment (chronic kidney disease Stage 3A): the DERIVE Study. Diabetes Obes Metab (2018) 20(11):2532–40. doi: 10.1111/dom.13413
101. Pollock C, Stefánsson B, Reyner D, Rossing P, Sjöström CD, Wheeler DC, et al. Albuminuria–lowering effect of dapagliflozin alone and in combination with saxagliptin and effect of dapagliflozin and saxagliptin on glycaemic control in patients with type 2 diabetes and chronic kidney disease (DELIGHT): a randomised, double–blind, placebo–controlled trial. Lancet Diabetes Endocrinol (2019) 7(6):429–44. doi: 10.1016/S2213–858719()30086–5
102. Barnett AH, Mithal A, Manassie J, Jones R, Rattunde H, Woerle HJ, et al. Efficacy and safety of empagliflozin added to existing antidiabetes treatment in patients with type 2 diabetes and chronic kidney disease: a randomised, double–blind, placebo–controlled trial. Lancet Diabetes Endocrinol (2014) 2(5):369–84. doi: 10.1016/S2213–858713()70208–0
103. Wanner C, Inzucchi SE, Lachin JM, Fitchett D, von Eynatten M, Mattheus M, et al. Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med (2016) 37(54):323–34. doi: 10.1056/NEJMoa1515920
104. Kashiwagi A, Takahashi H, Ishikawa H, Yoshida S, Kazuta K, Utsuno A, et al. A randomized, double–blind, placebo–controlled study on long–term efficacy and safety of ipragliflozin treatment in patients with type 2 diabetes mellitus and renal impairment: Results of the Long–Term ASP1941 Safety Evaluation in Patients with Type 2 Diabetes with Renal Impairment (LANTERN) study. Diabetes Obes Metab (2015) 17(2):152–60. doi: 10.1111/dom.12403
105. Cherney DZI, Ferrannini E, Umpierrez GE, Peters AL, Rosenstock J, Carroll AK, et al. Efficacy and safety of sotagliflozin in patients with type 2 diabetes and severe renal impairment. Diabetes Obes Metab (2021) 23(12):2632–42. doi: 10.1111/dom.14513
106. Bhatt DL, Szarek M, Pitt B, Cannon CP, Leiter LA, McGuire DK, et al. Sotagliflozin in patients with diabetes and chronic kidney disease. N Engl J Med (2021) 384(2):129–39. doi: 10.1056/NEJMoa2030186
107. Efficacy and Safety of Sotagliflozin Versus Placebo in Patients With Type 2 Diabetes Mellitus Not Currently Treated With Antidiabetic Therapy. Available at: https://clinicaltrials.gov/ct2/show/NCT02926937?term=NCT02926937&draw=2&rank=1.
108. Safety and Efficacy Study of Sotagliflozin on Glucose Control in Participants With Type 2 Diabetes, Moderate Impairment of Kidney Function, and Inadequate Blood Sugar Control (SOTA–CKD3). Available at: https://clinicaltrials.gov/ct2/show/NCT03242252?term=NCT03242252&draw=2&rank=1.
109. Efficacy and Bone Safety of Sotagliflozin 400 and 200 mg Versus Placebo in Participants With Type 2 Diabetes Mellitus Who Have Inadequate Glycemic Control (SOTA–BONE). Available at: https://clinicaltrials.gov/ct2/show/NCT03386344?term=NCT03386344&draw=2&rank=1.
110. Efficacy and Safety of Sotagliflozin Versus Placebo in Patients With Type 2 Diabetes Mellitus on Background of Metformin. Available at: https://clinicaltrials.gov/ct2/show/NCT02926950?term=NCT02926950&draw=2&rank=1.
111. Efficacy and Safety of Sotagliflozin Versus Placebo and Empagliflozin in Participants With Type 2 Diabetes Mellitus Who Have Inadequate Glycemic Control While Taking a DPP4 Inhibitor Alone or With Metformin (SOTA–EMPA). Available at: https://clinicaltrials.gov/ct2/show/NCT03351478?term=NCT03351478&draw=1&rank=1.
112. Efficacy and Safety of Sotagliflozin Versus Placebo in Participants With Type 2 Diabetes Mellitus Who Have Inadequate Glycemic Control While Taking Insulin Alone or With Other Oral Antidiabetic Agents (SOTA–INS) . Available at: https://clinicaltrials.gov/ct2/show/NCT03285594?term=NCT03285594&draw=2&rank=1.
113. Efficacy and Safety of Sotagliflozin Versus Placebo in Participants With Type 2 Diabetes Mellitus on Background of Sulfonylurea Alone or With Metformin. Available at: https://clinicaltrials.gov/ct2/show/NCT03066830?term=NCT03066830&draw=2&rank=1.
114. Efficacy and Safety of Sotagliflozin Versus Glimepiride and Placebo in Participants With Type 2 Diabetes Mellitus That Are Taking Metformin Monotherapy (SOTA–GLIM). Available at: https://clinicaltrials.gov/ct2/show/NCT03332771?term=NCT03332771&draw=1&rank=1.
115. A 16 Weeks Study on Efficacy and Safety of Two Doses of Empagliflozin (BI 10773) (Once Daily Versus Twice Daily) in Patients With Type 2 Diabetes Mellitus and Preexisting Metformin Therapy. Available at: https://clinicaltrials.gov/ct2/show/NCT01649297?term=NCT01649297&draw=2&rank=1.
116. A Study of the Effects of Canagliflozin (JNJ–28431754) on Renal Endpoints in Adult Participants With Type 2 Diabetes Mellitus (CANVAS–R). Available at: https://clinicaltrials.gov/ct2/show/NCT01989754?term=NCT01989754&draw=2&rank=1.
117. A Study of the Effects of Canagliflozin (JNJ–28431754) on Renal Endpoints in Adult Participants With Type 2 Diabetes Mellitus (CANVAS–R) . Available at: https://clinicaltrials.gov/ct2/show/NCT01989754?term=NCT01989754&draw=2&rank=1.
118. Dapagliflozin Effects on Epicardial Fat. Available at: https://clinicaltrials.gov/ct2/show/NCT02235298?term=NCT02235298&draw=2&rank=1.
119. Kohan DE, Fioretto P, Tang W, List JF. Long–term study of patients with type 2 diabetes and moderate renal impairment shows that dapagliflozin reduces weight and blood pressure but does not improve glycemic control. . Kidney Int (2014) 85(4):962–71. doi: 10.1038/ki.2013.356
120. Bode B, Stenlof K, Harris S, Sullivan D, Fung A, Usiskin K, et al. Long–term efficacy and safety of canagliflozin over 104 weeks in patients aged 55–80 years with type 2 diabetes. Diabetes Obes Metab (2015) 17(3):294–330. doi: 10.1111/dom.12428
121. Tanaka H, Takano K, Iijima H, Maruyama N, Hashimoto T, Hashimoto T, et al. Factors affecting canagliflozin–induced transient urine volume increase in patients with type 2 diabetes mellitus. Adv Ther (2017) 34(2):436–51. doi: 10.1007/s12325–016–0457–8
122. Moon JS, Kim NH, Na JO, Jeong IK, Lee SH, Mok JO, et al. Safety and effectiveness of empagliflozin in korean patients with type 2 diabetes mellitus: results from a nationwide post–marketing surveillance. Diabetes Metab J (2023) 47(1):82–91. doi: 10.4093/dmj.2021.0356
123. Inagaki N, Nangaku M, Sakata Y, Sasaki K, Mori–Anai K, Iwasaki T, et al. Real–world safety and effectiveness of canagliflozin treatment for type 2 diabetes mellitus in Japan: SAPPHIRE, a long–term, large–scale post–marketing surveillance. Adv Ther (2022) 39(1):674–91. doi: 10.1007/s12325–021–01984–4
124. Utsunomiya K, Koshida R, Kakiuchi S, Senda M, Fujii S, Kurihara Y, et al. Safety and effectiveness of tofogliflozin in Japanese patients with type 2 diabetes mellitus treated in real–world clinical practice: Results of a 36–month post–marketing surveillance study (J–STEP/LT). J Diabetes Investig (2021) 12(2):184–99. doi: 10.1111/jdi.13333
125. Maegawa H, Tobe K, Nakamura I, Uno S. Real–world evidence for long–term safety and effectiveness of ipragliflozin in treatment–naive versus non–naive Japanese patients with type 2 diabetes mellitus: subgroup analysis of a 3–year post–marketing surveillance study (STELLA–LONG TERM). Diabetol Int (2021) 12(4):430–44. doi: 10.1007/s13340–021–00501–w
126. Lin DS, Lee JK, Chen WJ. Clinical adverse events associated with sodium–glucose cotransporter 2 inhibitors: A meta–analysis involving 10 randomized clinical trials and 71 553 individuals. J Clin Endocrinol Metab (2021) 106(7):2133–45. doi: 10.1210/clinem/dgab274
127. Menne J, Dumann E, Haller H, Schmidt BMW. Acute kidney injury and adverse renal events in patients receiving SGLT2–inhibitors: A systematic review and meta–analysis. PloS Med (2019) 16(12):e1002983. doi: 10.1371/journal.pmed.1002983
128. Dutta D, Jindal R, Mehta D, Khandelwal D, Sharma M. Efficacy and safety of novel sodium glucose cotransporter–2 inhibitor remogliflozin in the management of type 2 diabetes mellitus: A systematic review and meta–analysis. Diabetes Metab Syndr (2021) 15(6):102315. doi: 10.1016/j.dsx.2021.102315
129. Mukai J, Kanno S, Kubota R. A literature review and meta–analysis of safety profiles of SGLT2 inhibitors in Japanese patients with diabetes mellitus. . Sci Rep (2021) 11(1):13472. doi: 10.1038/s41598–021–92925–2
130. Qiu M, Ding LL, Zhang M, Zhou HR. Safety of four SGLT2 inhibitors in three chronic diseases: A meta–analysis of large randomized trials of SGLT2 inhibitors. Diabetes Vasc Dis Res (2021) 18(2):14791641211011016. doi: 10.1177/14791641211011016
131. Nakamura I, Maegawa H, Tobe K, Uno S. Real–world evidence for long–term safety and effectiveness of ipragliflozin in Japanese patients with type 2 diabetes mellitus: final results of a 3–year post–marketing surveillance study (STELLA–LONG TERM). Expert Opin Pharmacother (2021) 22(3):373–87. doi: 10.1080/14656566.2020.1817388
Keywords: sodium-glucose transporter 2 inhibitors, reproductive tract infections, pollakiuria, hypovolemia, network meta-analysis
Citation: Li CX, Liu LY, Zhang CX, Geng XH, Gu SM, Wang YQ, Liu H, Xie Q and Liang S (2023) Comparative safety of different sodium-glucose transporter 2 inhibitors in patients with type 2 diabetes: a systematic review and network meta-analysis of randomized controlled trials. Front. Endocrinol. 14:1238399. doi: 10.3389/fendo.2023.1238399
Received: 11 June 2023; Accepted: 26 July 2023;
Published: 28 August 2023.
Edited by:
Shusen Sun, Western New England University, United StatesReviewed by:
Kefeng Liu, First Affiliated Hospital of Zhengzhou University, ChinaCopyright © 2023 Li, Liu, Zhang, Geng, Gu, Wang, Liu, Xie and Liang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hua Liu, emZsaHpmbGhAc2luYS5jb20=; Qing Xie, eGllX3FpbmcxMjNAMTI2LmNvbQ==; Shuo Liang, MTI4MDY3OTMwNkBxcS5jb20=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.