- 1Department of Plastic Surgery and Burn Center, the Second Affiliated Hospital of Shantou University Medical College, Shantou, Guangdong, China
- 2Department of Plastic Surgery, Meizhou Clinical Institute of Shantou University Medical College, Meizhou, Guangdong, China
Objectives: The objective of this study was to evaluate the association between weight-adjusted waist index (WWI) and the prevalence of kidney stones among adults in the United States.
Methods: The cross-sectional study utilized data from the National Health and Nutrition Examination Survey (NHANES) spanning the years 2007-2018. A total of 31,344 participants were categorized into two groups: those with kidney stones and those without. WWI was determined by dividing waist circumference (cm) by the square root of body weight (kg). To examine the relationship between kidney stones and WWI, multivariate logistic regression models, smoothed curve fitting, and weighted generalized additive model (GAM) regression were employed. Subgroup analysis and interaction tests were conducted to explore the stability of this association across different groups.
Results: The final analysis comprised a total of 31,344 participants, including 2,928 individuals who had a history of kidney stones. In the fully adjusted model, an increase in WWI exhibited a positive correlation with the prevalence of kidney stones (OR=1.34, 95% CI: 1.18-1.51). When WWI was converted into quartiles (Q1-Q4), participants in the highest quartile (Q4) had a 69% greater risk of developing kidney stones compared to those in the lowest quartile (Q1) (OR=1.69, 95% CI: 1.28-2.25). This positive association was particularly notable among non-diabetic patients.
Conclusion: Our study demonstrates a significant positive association between weight-adjusted waist index levels and an elevated prevalence of kidney stones among US adults. Furthermore, this research highlights the potential utility of weight-adjusted waist index in the prevention of kidney stones in the overall population. This relationship is limited and further research is needed to test this hypothesis.
1 Introduction
Kidney stones (KS) is a disease caused by the formation of solid stones from solute deposits in the urinary tract, often presenting as painful renal colic or haematuria (1, 2). Research has indicated a significant rise in the prevalence and incidence of kidney stones in recent decades, with global estimates ranging from approximately 2% to 20%. It is estimated that kidney stones affect around 1–15% of the global population (2–5). Kidney stones may lead to irreversible damage such as ureteral blockage, urinary tract infection, cystitis, pyelonephritis or chronic pyelonephritis, and eventually end-stage renal failure (ESRF) (6). Most kidney stones require expensive surgical treatment (7), impose a significant medical burden on society as a whole and individuals, and have become a serious public health problem. Given the critical nature of the situation, enhancing early identification and preventive measures for kidney stones within the population becomes imperative.
Obesity represents a significant risk factor for kidney stone formation and substantially elevates the risk compared to individuals with normal weight. Existing studies indicate that the risk can be heightened by as much as 75% (8). In a comprehensive prospective cohort study examining the relationship between obesity, weight gain, and increased waist circumference, these factors were identified as novel risk factors for stone attacks in individuals with stone disease (9). Nevertheless, body mass index (BMI), waist circumference (WC), and waist-height ratio (WHtR), which are widely employed as indicators of obesity, possess inherent limitations, leading to increasing concerns and debate regarding their accuracy. The “obesity paradox” has emerged to varying degrees with inconsistent or contradictory results between these obesity indicators and mortality in different populations (10–12). Additionally, there exists a stronger correlation between body composition, body fat distribution, and unfavorable metabolic profiles. Conventional measures of obesity, such as body mass index (BMI) and waist circumference (WC), fail to differentiate between fat distribution and muscle mass (13).
As a result, researchers proposed a novel obesity index called the “weight-adjusted waist index(WWI) “ in their 2018 study (14). WWI is a novel biomarker that has recently been developed, with few pertinent studies, and its diagnostic and prognostic value is primarily in clinical studies in cardiovascular-related fields (15–17). WWI reduces the association with BMI and combines the benefits of waist circumference to better reflect body muscle and fat than traditional obesity metrics such as BMI. In addition, WWI shows greater stability compared to BMI and other factors, providing a more accurate representation of visceral fat and muscle mass, therefore, gaining interest (18, 19). Recent research indicates that WWI may also have implications for renal health. The findings indicate that the Weight-Adjusted Waist Index (WWI) can serve as a simple anthropometric index with the ability to accurately predict albuminuria (20). WWI, as a readily available and cost-effective measure of obesity, holds great potential for use across various healthcare settings, particularly in resource-limited areas or when extensive data analysis is required. In addition, WWI is linearly and positively correlated with cardiometabolic morbidity and mortality and has excellent predictive power in predicting cardiometabolic disease and cardiovascular disease (14), and in populations with high WWI, helping clinicians to assess target organ damage early and initiate treatment to minimize the risk of disease and improve prognosis. In a prospective cohort study, it was observed that weight-adjusted waist index (WWI) demonstrated superior predictive performance for cardiovascular disease (CVD) mortality when compared to BMI, WC, and waist-height ratio (WHtR). Notably, the association was found to be absent in the case of BMI and WC (14). The aforementioned studies propose the potential superiority of weight-adjusted waist index (WWI) as an obesity indicator. Nevertheless, the association between WWI and kidney stones remains uncertain.
Therefore, leveraging data acquired from the National Health and Nutrition Examination Survey (NHANES) spanning from 2007 to 2018, we explored the potential correlation between the WWI index and the probability of developing kidney stones. Our hypothesis posited that an elevated Weight-Adjusted Waist Index would be linked to an increased likelihood of kidney stones. To the best of our knowledge, this study is the first to investigate the correlation between WWI and the elevated prevalence of kidney stones.
2 Materials and methods
2.1 Study participants
The National Health and Nutrition Examination Survey (NHANES) is an extensive survey of the US population, employing intricate, multi-stage, and probabilistic sampling techniques to gather a comprehensive range of data on nutrition and health among the general population in the United States. This survey makes use of the NHANES dataset for the United States from 2007 to 2018. There were 59,842 participants in this round. After excluding individuals with missing laboratory and demographic information, the analysis encompassed a total of 31,344 subjects. Figure 1 illustrates the flowchart depicting the process of sample selection. The overall protocol was approved by the ethical review committee at the National Center for Health Statistics (NCHS), and all participants provided informed consent by signing the consent form.

Figure 1 Flow chart of participants selection. NHANES, National Health and Nutrition Examination Survey.
2.2 Exposure and outcome definitions
As an exposure variable, each participant’s WWI was calculated as the square root of waist circumference (cm) divided by body weight (kg). At baseline, this was recorded as a continuous variable. Kidney stone occurrence (variable name: KIQ 026) was designed as an outcome variable. The participant was considered to have a kidney stone if he or she answered yes to the question, “Have you or the sample person (SP) ever had a kidney stone?” Previous research has established the reliability of self-reported kidney stone status (21).
2.3 Study variables
The covariates chosen for this study were age, sex (male or female), race, education level, moderate activity, marital status, smoking status, diabetes, hypertension, alcohol consumption, household income to poverty ratio (household PIR), weight, Waist circumference, body mass index(BMI), total cholesterol, high-density lipoprotein cholesterol (HDL-C), and low-density lipoprotein cholesterol (LDL-C). These were based on prior knowledge of the weight-adjusted index and factors associated with kidney stones. The NHANES Survey Methodology and Analysis Guide offers in-depth details on the methods used to gather the variables. You can find more specific information on the aforementioned variables in the NHANES Methodology and Analysis Guide (https://wwwn.cdc.gov/nchs/nhanes/AnalyticGuidelines).
2.4 Statistical analysis
All statistical analyses in this study adhered to the guidelines set forth by the Centers for Disease Control and Prevention (CDC). Continuous variables were summarized using means and standard deviations, while categorical variables were presented as percentages. To evaluate differences between groups categorized by the presence or absence of kidney stones, weighted Student’s t-tests (for continuous variables) and weighted chi-square tests (for categorical variables) were employed. The independent association between the WWI index and kidney stones was investigated using multifactor logistic regression models. Three models were utilized: Model 1, without any adjustment variables; Model 2, adjusted for sex, age, and race; and Model 3, adjusted for all covariates except BMI, waist circumference, and weight, which exhibited a significant impact on the exposure factors. To further investigate the non-linear relationship between the WWI index and kidney stones, smoothed curve fitting and weighted generalized additive model (GAM) regression techniques were employed. To explore heterogeneous associations between study subgroups, stratified factors were analyzed in subgroups by sex, age, race, education level, smoking status, diabetes, and hypertension. The heterogeneity of associations between subgroups was assessed using a log-likelihood ratio test model, which included an interaction term. Statistical analyses were performed using R (version 4.2) and EmpowerStats (version 4.1), statistical computing, and graphing software. A p-value of less than 0.05 was deemed statistically significant.
3 Results
3.1 Characteristics of the study population
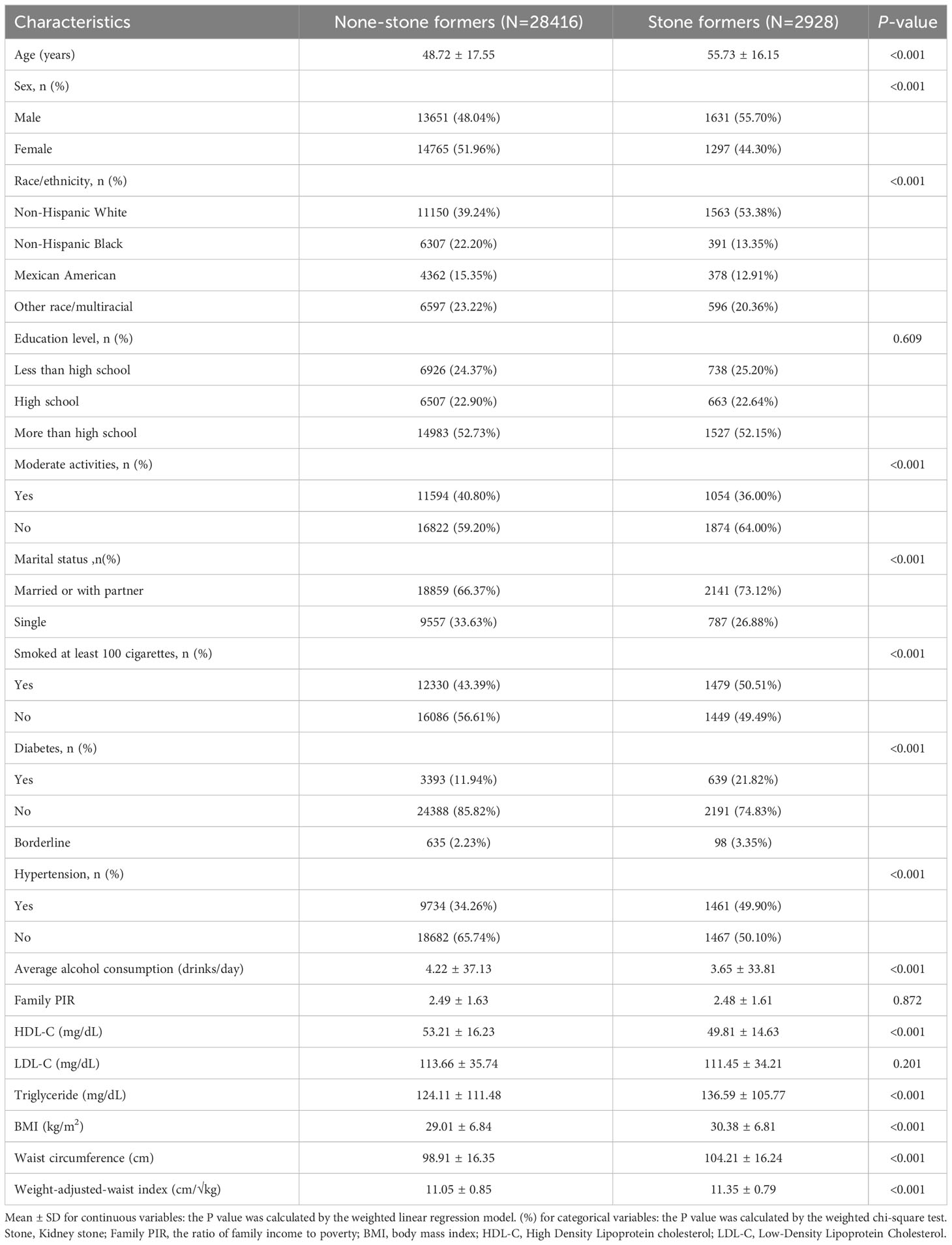
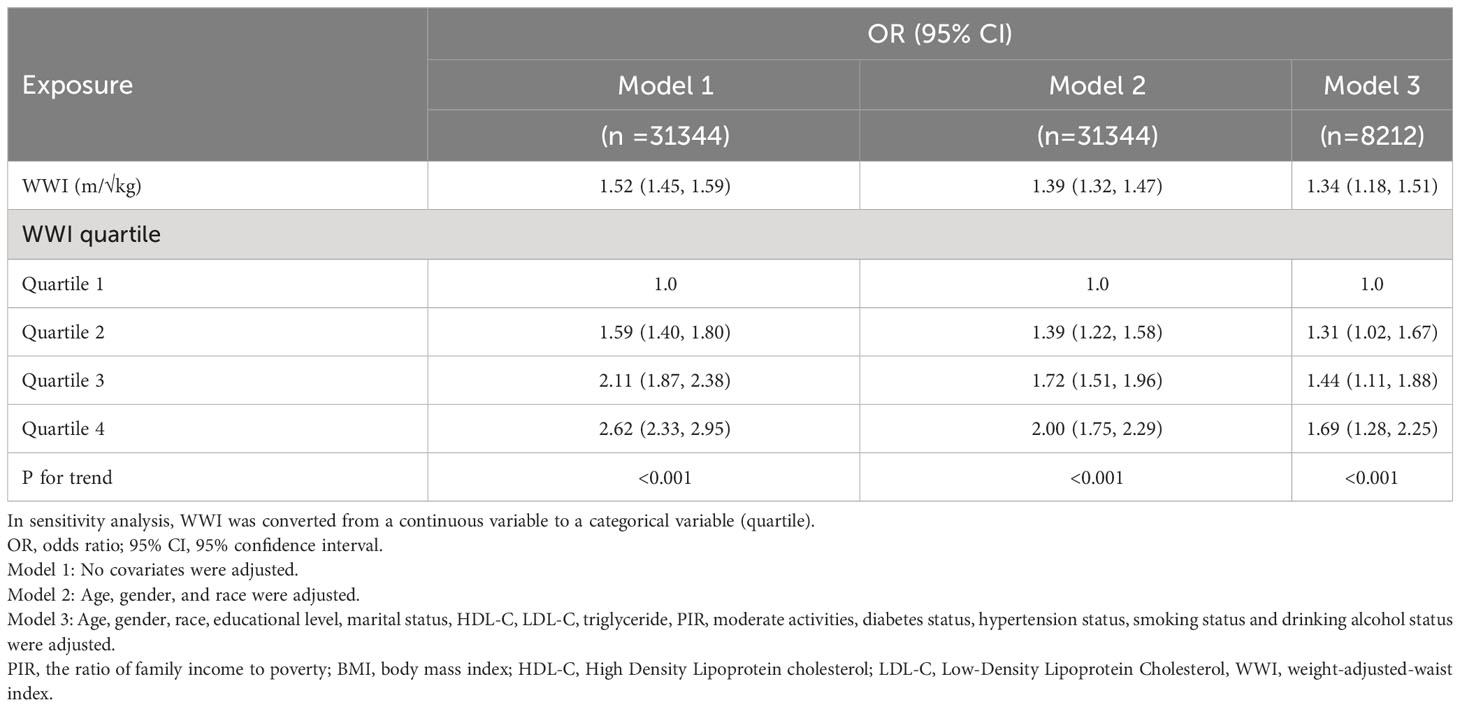
The study encompassed a total of 31,344 participants. Table 1 presents the overall characteristics of the study population based on the presence or absence of kidney stones. Patients with kidney stones exhibited a mean age of 55.73 ± 16.15 years, with 55.70% being male. On the other hand, patients without kidney stones had a mean age of 48.72 ± 17.55 years, with 48.04% being male. Participants with kidney stones, when compared to the non-kidney stone population, exhibited a higher prevalence of male gender, non-Hispanic white ethnicity, sedentary lifestyle, marital or partnered status, higher frequency of smoking, lower alcohol consumption, lower HDL-C levels, elevated total cholesterol levels, increased waist circumference, and BMI levels, and higher prevalence of high blood pressure and diabetes. In this study, the mean WWI was 11.35 ± 0.79 for individuals with kidney stones and 11.05 ± 0.85 for those without kidney stones. WWI was significantly different between the two groups (p < 0.001).
3.2 Association between weight-adjusted waist index and kidney stones
In this study, as presented in Table 2, the unadjusted (Model 1) multifactorial logistic regression analysis revealed a positive association between WWI and the risk of kidney stones, with an odds ratio (OR) of 1.52 (95% CI: 1.45, 1.59). This association was consistently observed in Models 2 and 3 as well. In the fully adjusted model (Model 3) that accounted for all confounding factors, the correlation between WWI and kidney stones remained stable, with an odds ratio (OR) of 1.34 (95% CI: 1.18, 1.51). This suggests that for every unit increase in WWI, there was a 34% increased risk of developing kidney stones. Additionally, we obtained reliable findings even after categorizing the continuous variables into quartiles. The OR (95% CI) for Q2, Q3, and Q4 are displayed in Table 2 and were 1.31 (1.02, 1.67), 1.44 (1.11, 1.88), and 1.69 (1.28, 2.25), respectively. The WWI index was 69% higher for Q4 than for Q1 (OR = 1.69, 95% CI: 1.28–2.25). indicating a potential non-linearity in this relationship. GAM and smoothing curves were employed to further explore the non-linear association between WWI and kidney stones, revealing a non-linear positive correlation (Figures 2, 3).
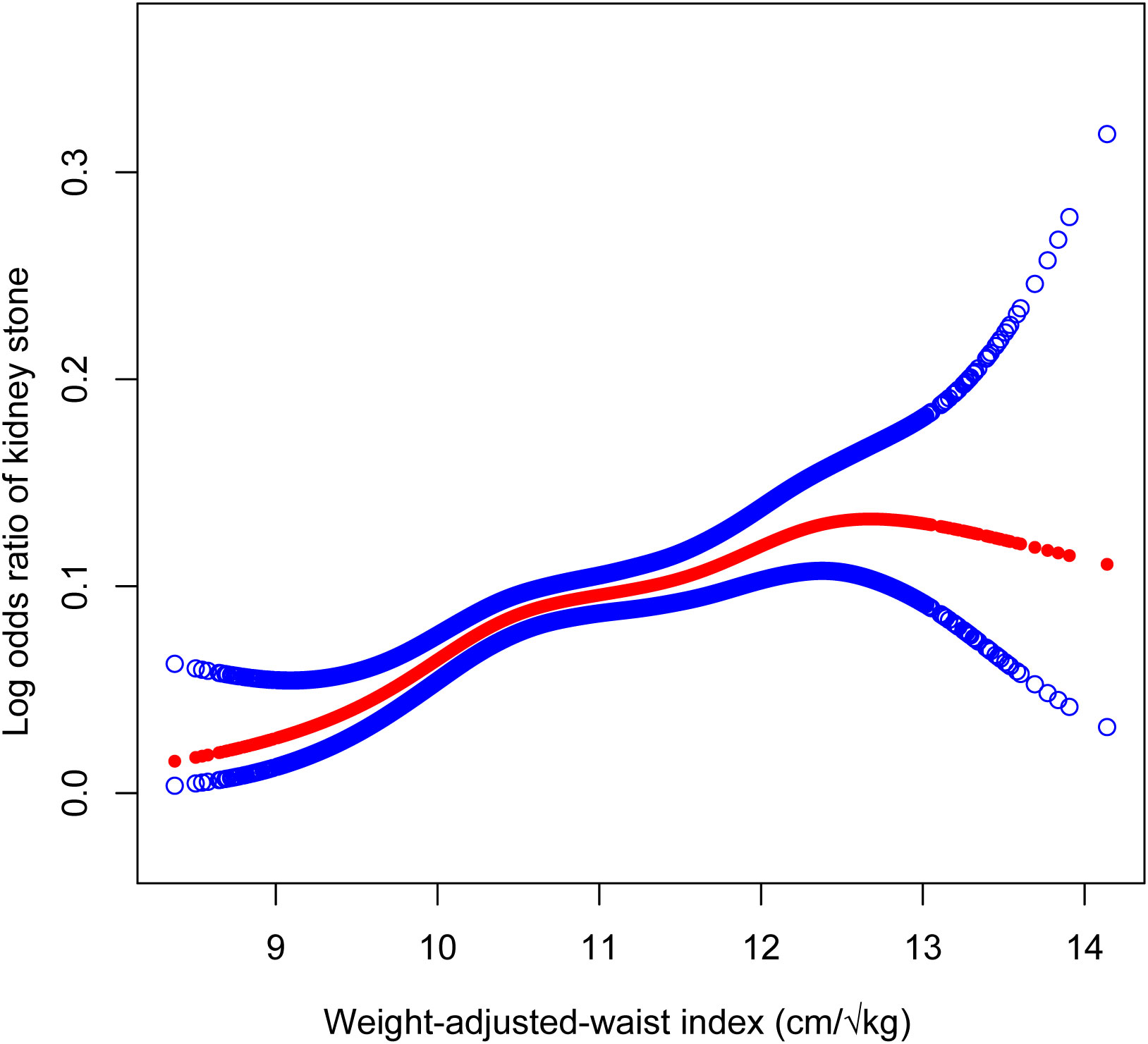
Figure 2 The association between Weight-Adjusted-Waist Index and Kidney Stones prevalence. Age, gender, race, educational level, marital status, HDL-C, LDL-C, triglyceride, PIR, moderate activities, diabetes status, hypertension status, smoking status and drinking alcohol status were adjusted.
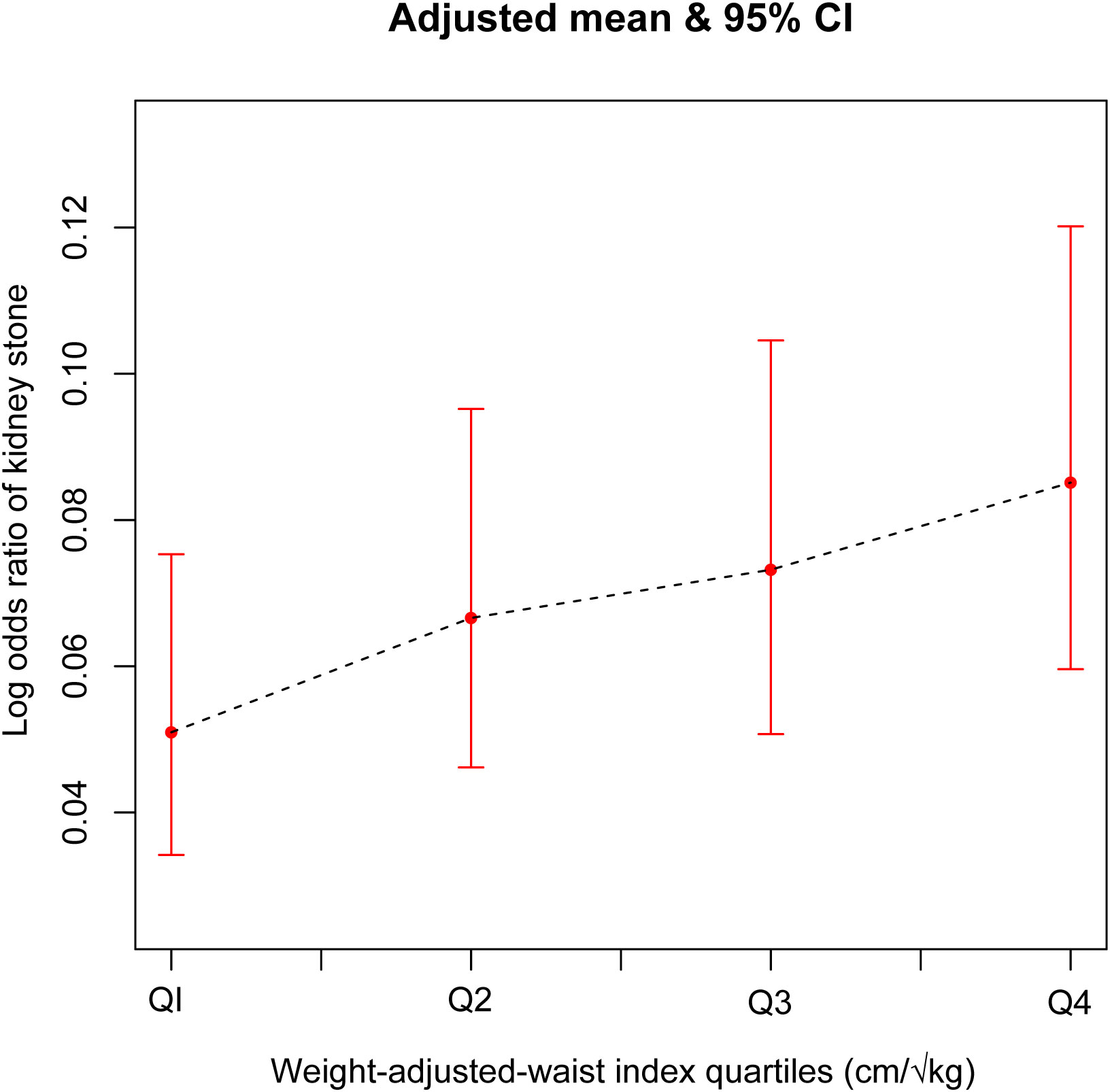
Figure 3 The association between Weight-Adjusted-Waist Index quartiles and Kidney Stones prevalence. Age, gender, race, educational level, marital status, HDL-C, LDL-C, triglyceride, PIR, moderate activities, diabetes status, hypertension status, smoking status and drinking alcohol status were adjusted.
3.3 Subgroup analysis
Subgroup analysis was conducted to assess the consistency of the correlation between WWI and kidney stones across different populations. Subgroup analysis (Figure 4) revealed that the correlation between WWI and the occurrence of kidney stones was not significantly influenced by age, gender, race/ethnicity, education level, smoking status, or diabetes status (p<0.05). Furthermore, we observed a significant interaction between the Hypertension status (Yes/No) groups and the correlation between WWI and kidney stones (interaction P < 0.05). In the non-hypertensive population, each 1-unit increase in WWI was associated with a 48% increase in the risk of kidney stones. However, in the hypertensive population, the correlation between WWI and the risk of kidney stones was found to be nonsignificant.
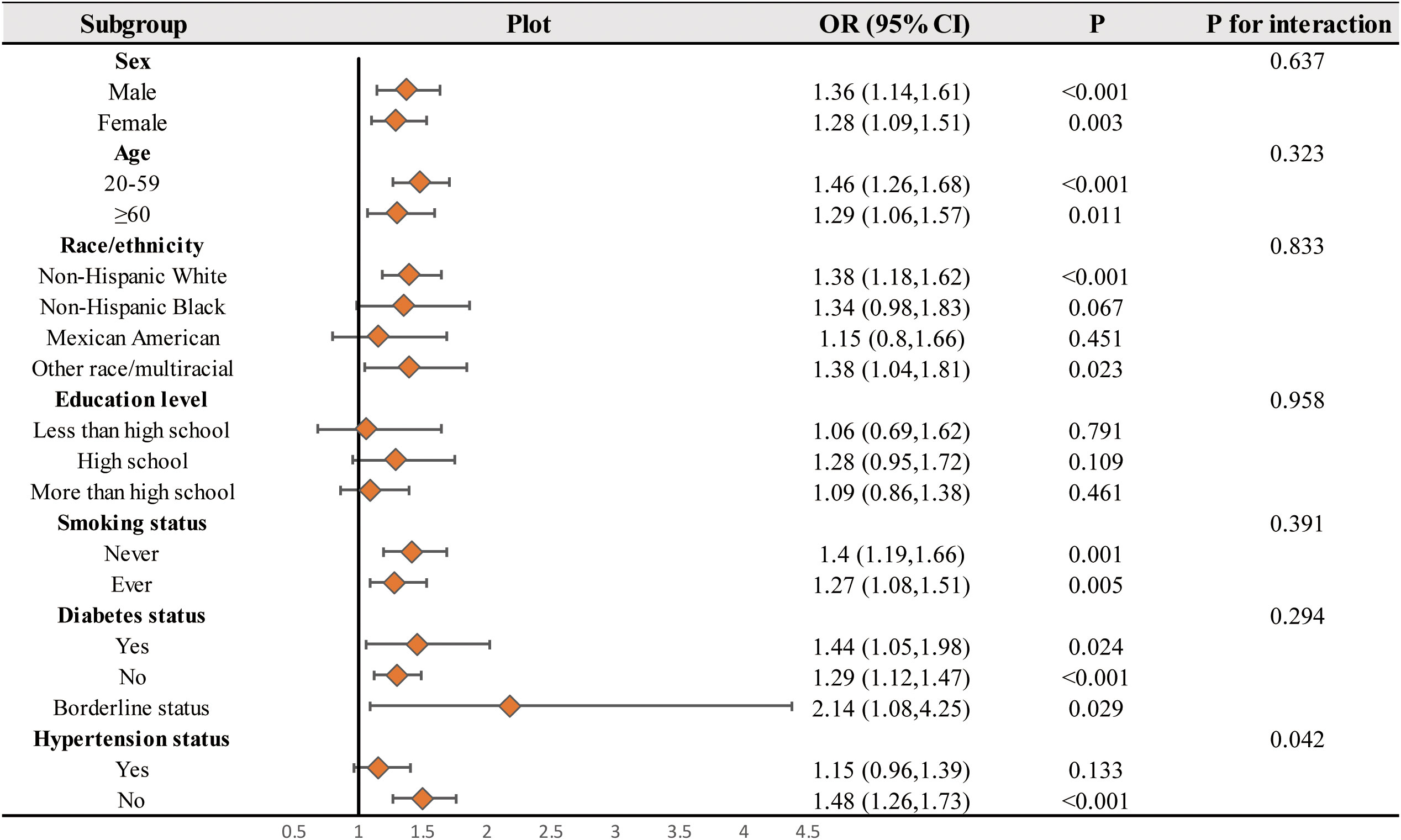
Figure 4 Subgroups analyses. In the subgroup analysis stratified by sex, age, Race/ethnicity, Education levels, Smoking status, Moderate activities, Diabetes status, and Hypertension status, the model is not adjusted for sex, age, Race/ethnicity, Education levels, Smoking status, Moderate activities, Diabetes status, and Hypertension status, respectively.
4 Discussion
The primary objective of this study was to evaluate the association between the weight-adjusted waist index (WWI) and the incidence of kidney stones. This cross-sectional study enrolled 31,344 adult participants over six consecutive NHANES 2-year cycles (2007–2018), and we observed an association between WWI and an increased likelihood of developing kidney stones. Subgroup analyses and interaction tests further demonstrated a significant dependence of hypertension (yes or no) and on this association. This suggests that higher levels of WWI may lead to an increased risk of developing kidney stones, particularly in those who are not hypertensive. The development and recurrence of kidney stones are known for their complexity. Understanding the risk factors associated with kidney stones is crucial for effective prevention and treatment strategies. Therefore, the weight-adjusted waist index (WWI) holds promise in the diagnosis of kidney stones.
Preliminary research has indicated the significant involvement of obesity in the development of kidney stones. Moreover, obesity has been shown to increase the risk of kidney stones, irrespective of whether the study participants have metabolic syndrome (22–24). A prospective study conducted by Taylor et al. investigated three large cohorts and found a significant association between obesity, weight gain, and the risk of kidney stone formation. Furthermore, the study revealed that women had a higher increased risk compared to men (25). In addition, Lee et al. discovered an association between obesity, metabolic changes, and the recurrence of urinary stones in their analysis of 704 patients, particularly in those who had previously formed stones (24). A retrospective study conducted by Kim et al. demonstrated a strong association between visceral fat obesity and uric acid stones. The study also indicated that visceral fat obesity had superior predictive value compared to BMI or urine pH in classifying stone type (26). A previous report indicated that the association between risk factors for uric acid stone formation and total body fat and trunk fat was stronger compared to body weight (27). The Android region, which includes the liver, pancreas, and kidneys, has been linked to an increased incidence of kidney stones, and an increase in the A/G ratio denotes an increase in the fat content of the Android region (21). On the other hand, Abufaraj et al. discovered that, even after controlling for various confounding variables, total body fat and trunk fat were associated with a significantly higher prevalence of kidney stones in adult women and men aged 40 years (28), and Bos et al. discovered that body fat distribution was also linked to the recurrence of kidney stones (29). Interestingly, earlier research has shown that WWI is a better predictor of body fat, especially concerning visceral fat (18). Similar to the findings of earlier studies, we discovered in this one that there is a correlation between the composite obesity index WWI and kidney stones, indicating that individuals with high levels of the weight-adjusted waist index (WWI) may be more likely to experience kidney stone formation. In addition, in our subgroup analysis, the association between WWI and kidney stones was more pronounced in non-hypertensive patients, and a series of earlier studies suggesting that hypertension (30, 31) is an independent risk factor for the development of kidney stones fits with previous findings.
One plausible explanation is that the accumulation of fat in the renal parenchyma may result in lipotoxicity. Specifically, the buildup of non-esterified fatty acids in renal cells, particularly in proximal tubular cells, could disrupt cellular metabolism, leading to a decreased production of ammonia. This reduction in ammonia output may contribute to renal damage, consequently promoting the development of kidney stones (32). On the other hand, it may be that increased fat is associated with elevated urinary oxalate, which contributes to the development of kidney stones through enhanced intestinal absorption of oxalate and increased endogenous synthesis of oxalate (26). In addition, obesity or fat gain can lead to inflammation and fibrosis of the kidney parenchyma or urinary tract infection, which is also a possible mechanism to induce the development of kidney stones (33–35).
This study has some advantages. It is a cross-sectional study using a broadly representative national representative sample. The study also employs a sophisticated multi-stage probability sampling design and makes extensive covariate adjustments, which significantly boosts the precision of statistical inference. In addition to the novel findings of the study, there are some shortcomings in our study. Firstly, as this study was cross-sectional, the relationship between WWI and kidney stones was limited. Also, more specific data were not included in the NHANES database, and due to the limitations of the questionnaire, such as the specific dose, specific type, site, and complications of kidney stones were information that we could not obtain. This affected the results to some extent. Thirdly, a lot of our data, including that on kidney stones, is self-reported and may be biased by recall. Given these limitations, further research is necessary. For example, study details such as the type of renal stone dose should be included to validate the findings of this study and to examine the relationship between WWI and renal stones in more detail.
5 Conclusion
Through the analysis of a nationally representative sample, this study revealed a significant association between high WWI and an increased incidence of kidney stones. We hypothesize that this has important implications for the prevention and treatment of kidney stones. Given the current sample of studies, this relationship is limited and this finding needs to be supported by further research to test this hypothesis.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by National Center for Health Statistics (NCHS) Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. The manuscript presents research on animals that do not require ethical approval for their study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
HL and LS designed the research. HL, YM, and LS collected and analyzed the data. HL and YM drafted the manuscript. LS revised the manuscript. All authors contributed to the article and approved the submitted version.
Funding
The authors declare financial support was received for the research, authorship, and/or publication of this article. This work was funded by the Natural Science Foundation of Guangdong Province, China (grant nos. 2022A1515012150 and 2018A030307010).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
Kidney stones, KS; The weight-adjusted-waist-index, WWI; National Health and Nutrition Examination Survey, NHANES; Mobile Examination Center, MEC; Body mass index, BMI; The ratio of family income to poverty, PIR; High Density Lipoprotein cholesterol, HDL-C; Low-Density Lipoprotein Cholesterol, LDL-C; Vibration-controlled transient elastography, VCTE.
References
1. Boyce CJ, Pickhardt PJ, Lawrence EM, Kim DH, Bruce RJ. Prevalence of urolithiasis in asymptomatic adults: objective determination using low dose noncontrast computerized tomography. J Urol (2010) 183:1017–21. doi: 10.1016/j.juro.2009.11.047
2. Soucie JM, Thun MJ, Coates RJ, McClellan W, Austin H. Demographic and geographic variability of kidney stones in the United States. Kidney Int (1994) 46:893–9. doi: 10.1038/ki.1994.347
3. Buchholz NPN, Abbas F, Afzal M, Khan R, Rizvi I, Talati J. The prevalence of silent kidney stones–an ultrasonographic screening study. J Pak Med Assoc (2003) 53:24–5.
4. Indridason OS, Birgisson S, Edvardsson VO, Sigvaldason H, Sigfusson N, Palsson R. Epidemiology of kidney stones in Iceland: a population-based study. Scand J Urol Nephrol (2006) 40:215–20. doi: 10.1080/00365590600589898
5. Romero V, Akpinar H, Assimos DG. Kidney stones: a global picture of prevalence, incidence, and associated risk factors. Rev Urol (2010) 12:e86–96.
6. Ziemba JB, Matlaga BR. Epidemiology of kidney stones in Iceland: a population-based study. Scand J Urol Nephrol (2006) 40:215–20. doi: 10.4111/icu.2017.58.5.299
7. Lingeman JE, Saywell RM, Woods JR, Newman DM. Cost analysis of extracorporeal shock wave lithotripsy relative to other surgical and nonsurgical treatment alternatives for urolithiasis. Med Care (1986) 24:1151–60. doi: 10.1097/00005650-198612000-00007
8. Wong YV, Cook P, Somani BK. The association of metabolic syndrome and urolithiasis. Int J Endocrinol (2015) 2015:570674. doi: 10.1155/2015/570674
9. Taylor EN, Stampfer MJ, Curhan GC. The association of metabolic syndrome and urolithiasis. Int J Endocrinol (2015) 2015:570674. doi: 10.1155/2015/570674
10. Carnethon MR, De Chavez PJD, Biggs ML, Lewis CE, Pankow JS, Bertoni AG, et al. Association of weight status with mortality in adults with incident diabetes. JAMA (2012) 308:581–90. doi: 10.1001/jama.2012.9282
11. Kim NH, Lee J, Kim TJ, Kim NH, Choi KM, Baik SH, et al. Body mass index and mortality in the general population and in subjects with chronic disease in Korea: A nationwide cohort study (2002-2010). PloS One (2015) 10:e0139924. doi: 10.1371/journal.pone.0139924
12. Clark AL, Fonarow GC, Horwich TB. Waist circumference, body mass index, and survival in systolic heart failure: the obesity paradox revisited. J Card Fail (2011) 17:374–80. doi: 10.1016/j.cardfail.2011.01.009
13. Antonopoulos AS, Oikonomou EK, Antoniades C, Tousoulis D. From the BMI paradox to the obesity paradox: the obesity-mortality association in coronary heart disease. Obes Rev (2016) 17:989–1000. doi: 10.1111/obr.12440
14. Park Y, Kim NH, Kwon TY, Kim SG. A novel adiposity index as an integrated predictor of cardiometabolic disease morbidity and mortality. Sci Rep (2018) 8:16753. doi: 10.1038/s41598-018-35073-4
15. Qin Z, Du D, Li Y, Chang K, Yang Q, Zhang Z, et al. The association between weight-adjusted-waist index and abdominal aortic calcification in adults aged ≥ 40 years: results from NHANES 2013-2014. Sci Rep (2022) 12:20354. doi: 10.1038/s41598-022-24756-8
16. Ding C, Shi Y, Li J, Li M, Hu L, Rao J, et al. Association of weight-adjusted-waist index with all-cause and cardiovascular mortality in China: A prospective cohort study. Nutr Metab Cardiovasc Dis (2022) 32:1210–7. doi: 10.1016/j.numecd.2022.01.033
17. Zhang D, Shi W, Ding Z, Park J, Wu S, Zhang J. Association between weight-adjusted-waist index and heart failure: Results from National Health and Nutrition Examination Survey 1999-2018. Front Cardiovasc Med (2022) 9:1069146. doi: 10.3389/fcvm.2022.1069146
18. Kim NH, Park Y, Kim NH, Kim SG. Weight-adjusted waist index reflects fat and muscle mass in the opposite direction in older adults. Age Ageing (2021) 50:780–6. doi: 10.1093/ageing/afaa208
19. Nuttall FQ. Body mass index: obesity, BMI, and health: A critical review. Nutr Today (2015) 50:117–28. doi: 10.1097/NT.0000000000000092
20. Qin Z, Chang K, Yang Q, Yu Q, Liao R, Su B. The association between weight-adjusted-waist index and increased urinary albumin excretion in adults: A population-based study. Front Nutr (2022) 9:941926. doi: 10.3389/fnut.2022.941926
21. Li G, Liang H, Hao Y, Huang Q, Shen X, Chen Y, et al. Association between body fat distribution and kidney stones: Evidence from a US population. Front Endocrinol (Lausanne) (2022) 13:1032323. doi: 10.3389/fendo.2022.1032323
22. Inci M, Demirtas A, Sarli B, Akinsal E, Baydilli N. Association between body mass index, lipid profiles, and types of urinary stones. Ren Fail (2012) 34:1140–3. doi: 10.3109/0886022X.2012.713298
23. Hess B. Metabolic syndrome, obesity and kidney stones. Arab J Urol (2012) 10:258–64. doi: 10.1016/j.aju.2012.04.005
24. Lee S-C, Kim Y-J, Kim T-H, Yun S-J, Lee NK, Kim W-J. Impact of obesity in patients with urolithiasis and its prognostic usefulness in stone recurrence. J Urol (2008) 179:570–4. doi: 10.1016/j.juro.2007.09.040
25. Taylor EN, Stampfer MJ, Curhan GC. Obesity, weight gain, and the risk of kidney stones. JAMA (2005) 293:455–62. doi: 10.1001/jama.293.4.455
26. Pigna F, Sakhaee K, Adams-Huet B, Maalouf NM. Body fat content and distribution and urinary risk factors for nephrolithiasis. Clin J Am Soc Nephrol (2014) 9:159–65. doi: 10.2215/CJN.06180613
27. Kim JH, Doo SW, Cho KS, Yang WJ, Song YS, Hwang J, et al. Which anthropometric measurements including visceral fat, subcutaneous fat, body mass index, and waist circumference could predict the urinary stone composition most? BMC Urol (2015) 15:17. doi: 10.1186/s12894-015-0013-x
28. Abufaraj M, Siyam A, Xu T, Imm K, Cao C, Waldoer T, et al. Association between body fat mass and kidney stones in US adults: analysis of the national health and nutrition examination survey 2011-2018. Eur Urol Focus (2022) 8:580–7. doi: 10.1016/j.euf.2021.03.010
29. Bos D, Dason S, Matsumoto E, Pinthus J, Allard C. A prospective evaluation of obesometric parameters associated with renal stone recurrence. Can Urol Assoc J (2016) 10:234–8. doi: 10.5489/cuaj.3876
30. Soligo M, Morlacco A, Zattoni F, Valotto C, DE Giorgi G, Beltrami P. Metabolic syndrome and stone disease. Panminerva Med (2022) 64:344–58. doi: 10.23736/S0031-0808.21.04517-1
31. Wong Y, Cook P, Roderick P, SOmani BK. Metabolic syndrome and kidney stone disease: A systematic review of literature. J Endourol (2016) 30:246–53. doi: 10.1089/end.2015.0567
32. Soligo M, Morlacco A, Zattoni F, Valotto C, DE Giorgi G, Beltrami P. Body Mass Index: Obesity, BMI, and Health: A Critical Review. Nutr Today (2015) 50:117–28. doi: 10.1097/NT.0000000000000092
33. Gorbachinsky I, Akpinar H, Assimos DG. Metabolic syndrome and urologic diseases. Rev Urol (2010) 12:e157–180. doi: 10.1089/end.2015.0567
34. Reisin E, Jack AV. Obesity and hypertension: mechanisms, cardio-renal consequences, and therapeutic approaches. Med Clin North Am (2009) 93:733–51. doi: 10.1016/j.mcna.2009.02.010
Keywords: weight-adjusted waist index, kidney stone, NHANES, obese, cross-sectional study
Citation: Liu H, Ma Y and Shi L (2023) Higher weight-adjusted waist index is associated with increased likelihood of kidney stones. Front. Endocrinol. 14:1234440. doi: 10.3389/fendo.2023.1234440
Received: 04 June 2023; Accepted: 29 August 2023;
Published: 20 September 2023.
Edited by:
Long Nguyen, The University of Sydney, AustraliaReviewed by:
Jayanta Gupta, Florida Gulf Coast University, United StatesAmani Alrasheedi, King Abdulaziz University, Saudi Arabia
Copyright © 2023 Liu, Ma and Shi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lungang Shi, bHVuZ2FuZ3NoaUAxNjMuY29t
 Hangyu Liu
Hangyu Liu Yang Ma
Yang Ma Lungang Shi2*
Lungang Shi2*