
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Endocrinol., 23 October 2023
Sec. Obesity
Volume 14 - 2023 | https://doi.org/10.3389/fendo.2023.1210371
This article is part of the Research TopicThe Role of Nutrition in Healthy AgingView all 10 articles
Background: Large population-based studies on the association between changes in body composition and the occurrence of heart failure (HF) are rare. We aimed to determine the association between changes in body composition, including the predicted body fat mass index (pBFMI), predicted appendicular skeletal muscle mass index (pASMI), and predicted lean body mass index (pLBMI), and the occurrence of HF.
Methods: For present study, 2,036,940 people who consecutively underwent national health examinations from 2010~2011 (baseline period) to 2012~2013 (follow-up period) were included. The pBFMI, pASMI, and pLBMI were indirectly investigated using validated anthropometric prediction equations from the Korean National Health and Nutrition Examination Survey cohort. The outcome was defined as at least two or more claims of HF.
Results: During a median of 7.59 years of follow-up, 22,172 participants (event rate, 1.09%) with HF were observed. Decreased changes in the pASMI and pLBMI were associated with the occurrence of HF among males (hazard ratio [HR] 0.966, 95% confidence interval (CI) [0.944-0.988]; HR 0.939, 95%CI [0.923-0.955], respectively) and females (HR 0.924, 95%CI [0.900-0.947]; HR 0.951, 95%CI [0.939-0.963], respectively). An increased change in the pBFMI was associated with the occurrence of HF in males (HR 1.017, 95%CI [1.001-1.034]). However, paradoxically, a change in the pBFMI was associated with the occurrence of HF in females (HR 0.925, 95%CI [0.909-0.942]).
Conclusion: Decreased skeletal muscle mass was related to the occurrence of HF. However, the relationship between a change in fat mass and the occurrence of HF was different and even paradoxical depending on sex.
Heart failure (HF) is a clinical syndrome that is related to decreased cardiac contractility accompanied by impairment of the ejection of blood or ventricular filling (1). HF is a common cardiovascular disease and a leading cause of hospitalization, especially in older adults. The economic burden and prevalence of HF have been increasing worldwide (2). Despite the development of treatment and prevention tools for HF, the morbidity and mortality rates associated with HF are still high (2). Therefore, it is important to identify the hidden risk factors associated with HF. To date, risk factors for HF, including hypertension, diabetes mellitus, coronary artery occlusive disease, aortic atheroma, poor oral hygiene, smoking, and cardiomyopathy, have been suggested. However, information regarding further modifiable associations or occurrence for HF is still lacking (3, 4).
Obesity is defined as an abnormal accumulation of health-impairing fat mass, commonly assessed as a determination of a body mass index (BMI) ≥30 kg/m2 (5). The prevalence of obesity has increased over the past few decades throughout the world, and the global burden of obesity is currently increasing rapidly (6). It is well known that obesity, especially greater levels of adiposity, is a well-established risk factor for cardiovascular disease and is associated with cardiovascular risk factors, including hypertension, insulin resistance, lipoprotein metabolism, and inflammation (7, 8). In a previous study, obesity and abdominal fat were found to be associated with an increased incidence of HF (9). However, when obesity was evaluated using BMI in patients with HF, the obesity paradox that obese patients have better long-term and short-term prognosis was observed (10). Furthermore, because BMI includes not only fat mass but also skeletal mass and lean body mass, cannot distinguish between lean body mass and fat mass, and provides no information on body fat distribution, it is necessary to check the correlation with HF using body composition rather than BMI (11).
Nevertheless, there have been few longitudinal studies targeting a general population of large sample sizes on the association of changes in body composition with the occurrence of HF. Therefore, we aimed to investigate the association between changes in body composition, including the predicted appendicular skeletal muscle mass index (pASMI), predicted body fat mass index (pBFMI), and predicted lean BMI (pLBMI), and the occurrence of HF in a longitudinal setting.
This study was performed using the National Health Insurance Service-Health Screening (NHIS-HEALS) dataset supplied by the Korean government. In South Korea, adults older than 40 years of age are advised to undergo free health examinations in alternate years. The Korean government combined the health screening dataset with age, sex, household income, and clinical information, including diagnostic codes, prescriptions, information on treatment or procedure, hospitalization, and mortality date (12, 13). For our study, 2,139,856 people who consecutively underwent national health examinations from 2010~2011 (baseline period) to 2012~2013 (follow-up period) were included (dataset number NHIS-2021-1-715) through an identification and validation process (14–16). Among 2,139,856 participants, those (n=85,947) with at least one missing data were excluded. Those with a previous history of HF (n=16,969) were excluded. Finally, 2,036,940 participants were included in the present study (Figure 1). The present study was approved by the Institutional Review Board of Ewha Womans University Seoul Hospital (Institutional Review Board approval number: SEUMC 2022-02-018).
The pBFMI, pASMI, and pLBMI were indirectly evaluated by validated anthropometric prediction equations from the Korean National Health and Nutrition Examination Survey cohort (11). A previous study suggested that body fat mass, appendicular skeletal muscle mass, and lean body mass were identified using dual-energy X-ray absorptiometry, and then a prediction equation was composed using different combinations of age, anthropometric measurements (weight, height, waist circumference), serum creatinine levels, physical activity, smoking status, and alcohol intake (11). These predictive equations were validated as having high predictive power, a moderate agreement rate, and low bias in the Korean general population (11). In the present study, these prediction equations were applied to evaluate the participants’ body composition. Body fat mass, appendicular skeletal muscle mass, and lean body mass were presented as indices (weight [kg] divided by height squared [m2]); thus, pBFMI, pASMI, and pLBMI, respectively (Supplementary Methods 1). The change in the pBFMI, termed ΔpBFMI, was calculated from the difference between the baseline and follow-up periods pBFMI, and the changes in the pASMI and pLBMI (ΔpASMI and ΔpLBMI) were also calculated similarly.
The detailed definitions of covariates were demonstrated in Supplementary Methods 2 and previous studies (17–19). Variables including age, sex, BMI, household income (first, second, third, or fourth quartile), smoking status (never, former, or current), alcohol intake (0, 1-2, 3-4, or ≥5 times per week), physical activity (0, 1-2, 3-4, or ≥5 times per week), comorbid disease (hypertension, diabetes mellitus, dyslipidemia, atrial fibrillation, cancer, and renal disease), systolic blood pressure, fasting serum glucose, total cholesterol, estimated glomerular filtration rate, and Charlson Comorbidity Index (CCI) which is a commonly used method for evaluating comorbidities were collected (3, 18, 20). Comorbidities were defined considering the International Classification of Diseases, Tenth Revision (ICD-10) codes, history of prescriptions, and laboratory findings from the health examinations (3, 18).
The index date was defined as the date of the national health examination. The most recent health examination data were used for statistical analysis if more than one examination was performed during the period. Outcomes were defined as two or more claims for HF (21). Previously, the diagnostic accuracy of the ICD-10 code (I50) for HF using the NHIS dataset has been validated (3, 21). Monitoring was conducted until December 31, 2020, or the first occurrence of death or HF.
Chi-square and paired t-tests were used to compare categorical and continuous variables according to sex. The Cox proportional hazards model presented with a hazard ratio (HR) with a 95% confidence interval (CI) was used to evaluate the effect of changes in body composition (1 kg/m2 increments in the ΔpBFMI, ΔpASMI, and ΔpLBMI) between the baseline and follow-up periods on the occurrence of HF after adjusting for all potential confounding factors. In addition, we performed an additional multivariable analysis after adjusting for all potential confounding factors, except for variables used in the prediction equations to calculate the predicted body composition, including age, smoking status, alcohol intake, and physical activity. Furthermore, we provided restricted cubic splines of change in the predicted body composition to visually estimate the association between the change in the predicted body composition (ΔpBFMI, ΔpASMI, and ΔpLBMI) and the occurrence of HF. Four knots were placed at the 5th, 35th, 65th, and 95th percentiles of the change in the predicted body composition. Stratified analyses of the effects of changes in body composition on the occurrence of HF were conducted according to the subgroups of age, household income, alcohol intake, smoking status, physical activity, systolic blood pressure, fasting serum glucose, total cholesterol, CCI, and BMI at baseline and the follow-up categories: normal weight (18.5-24.9 kg/m2), overweight (25-29.9 kg/m2), and obese (≥ 30 kg/m2). To evaluate the combined effects of changes in the BMI, pASMI, pBFMI, and pLBMI, stratified analysis was additionally performed to evaluate the effect of changes in BMI during the two health examinations on the occurrence of HF according to changes in body composition. Statistical analyses were performed using R software, version 3.3.3 (R Foundation for Statistical Computing, Vienna, Austria) and SAS version 9.4 (SAS Inc., Cary, NC, USA). Two-sided P-values less than 0.05 were considered significant.
Table 1 shows the results of comparing the baseline characteristics of the 2,036,940 participants according to sex (n=1,070,377 for males, n=966,563 for females). During a median of 7.59 years of follow-up, 22,172 participants (event rate, 1.09%) with HF were observed. The mean age of males was 49.60 ± 13.45 years, and of females was 52.32 ± 13.65 years. Significant differences in the BMI at baseline and follow-up, household income, smoking status, alcohol intake, physical activity, systolic blood pressure, fasting serum glucose, total cholesterol, estimated glomerular filtration rate, and CCI were observed between males and females (Table 1). In the baseline period, the pASMI (23.67 ± 3.19 kg/m2 for males vs. 15.17 ± 1.85 kg/m2 for females), pBFMI (16.11 ± 4.27 kg/m2 for males vs. 19.16 ± 4.61 kg/m2 for females), and pLBMI (53.41 ± 6.52 kg/m2 for males vs. 37.25 ± 3.96 kg/m2 for females) were significantly different according to sex (P<0.001). In the follow-up period, the pASMI (23.68 ± 3.26 kg/m2 for males vs. 15.13 ± 1.86 kg/m2 for females), pBFMI (16.17 ± 4.34 kg/m2 for males vs. 19.22 ± 4.66 kg/m2 for females), and pLBMI (53.53 ± 6.66 kg/m2 for males vs. 37.23 ± 4.04 kg/m2 for females) were also significantly different according to sex (P<0.001, Table 1).
Multivariate analysis showed a relationship between the occurrence of HF and changes in body composition (Table 2; Supplementary Table 1). In males, with a 1 kg/m2 increase in the ΔpBFMI, the HR for the occurrence of HF was 1.017 (95%CI: 1.001-1.034), and the HRs for a 1 kg/m2 increase in the ΔpASMI and ΔpLBMI were 0.924 (95%CI: 0.900-0.947) and 0.951 (95%CI: 0.939-0.963), respectively. In females, with a 1 kg/m2 increase in the ΔpBFMI, the HR for the occurrence of HF was 0.925 (95%CI: 0.909-0.942), for a 1 kg/m2 increase in the ΔpASMI and ΔpLBMI were 0.966 (95%CI: 0.944-0.988), and 0.939 (95%CI: 0.923-0.955), respectively. In contrast, decreases in the ΔpASMI and ΔpLBMI were associated with an increased incidence of HF in both sexes. Furthermore, a decrease in the ΔpBFMI was associated with a decreased HF incidence in males, whereas a decrease in the ΔpBFMI was associated with an increased HF incidence in females (Table 2; Supplementary Table 1 and Figure 2). For the stratified analysis, these trends and results were similar regardless of the BMI status at baseline. The occurrence-reducing effects of increased ΔpLBMI and ΔpASMI on the occurrence of HF were more prominent when the participants were less obese. Furthermore, the occurrence-reducing effect of an increased ΔpBFMI on the occurrence of HF was more prominent when female participants were less obese. In contrast to females, the occurrence-increasing effect of increased ΔpBFMI on the occurrence of HF was more prominent when male participants were less obese (Table 3; Supplementary Table 2).
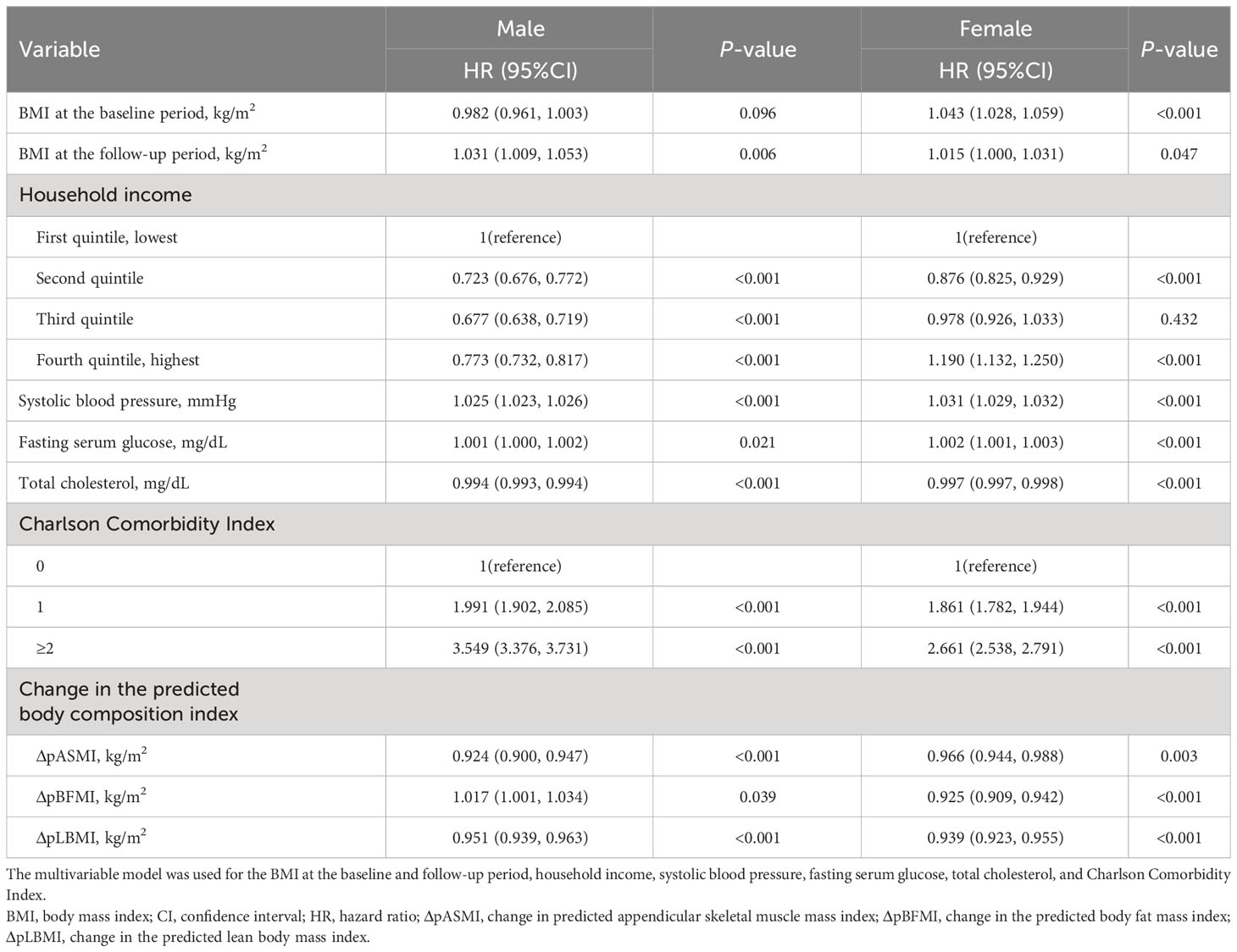
Table 2 Hazard ratios and 95%CI of heart failure per 1 kg/m2 increase in the change in the predicted body composition index.
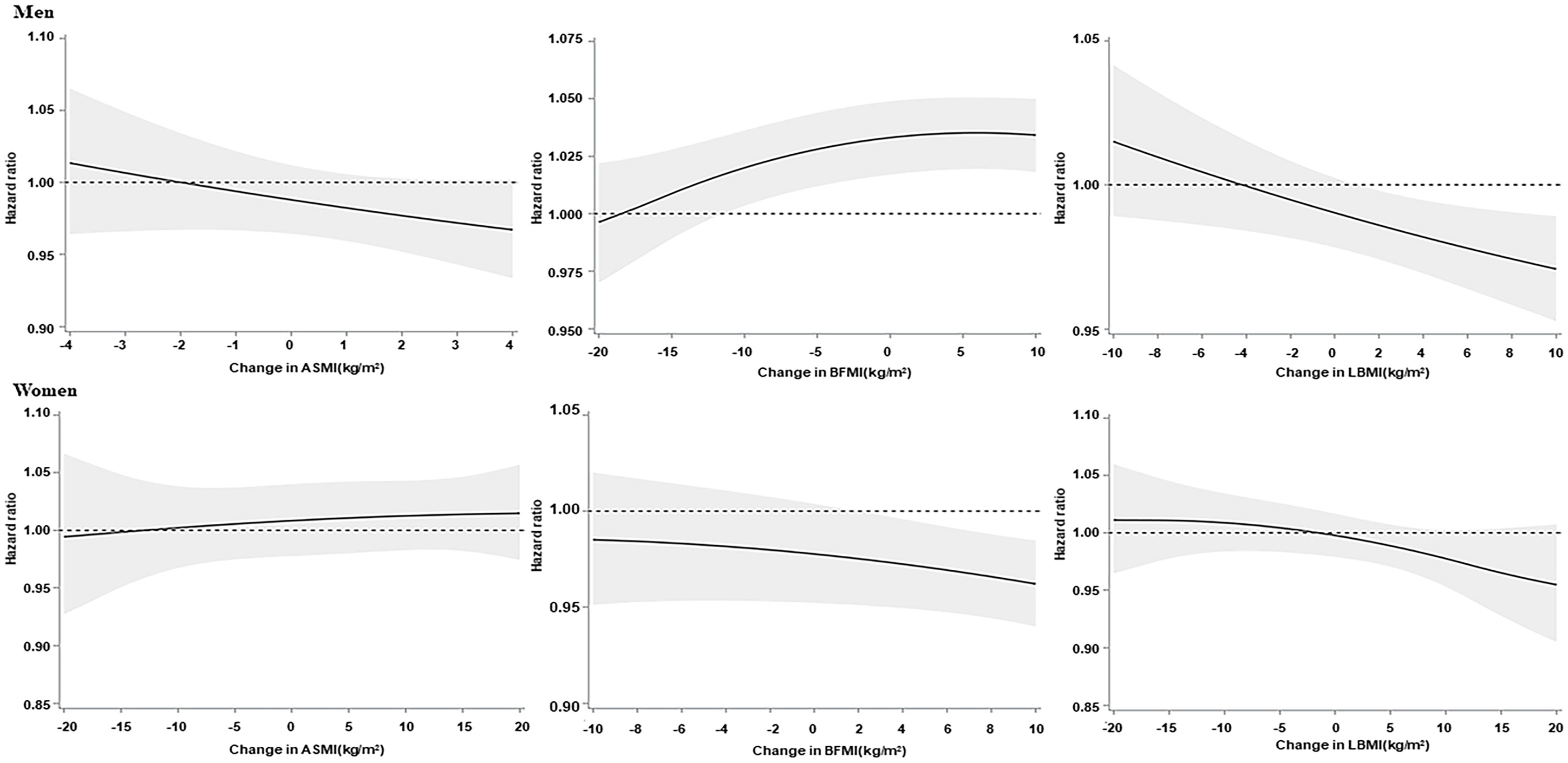
Figure 2 Association of the changes in the predicted body composition index with heart failure. Association of the changes in the predicted appendicular skeletal muscle mass index, body fat mass index, and lean body mass index (BMI) with heart failure. The solid lines indicate the hazard ratios, and the shaded regions show 95% confidence intervals from restricted cubic spline regression. Restricted cubic splines were constructed with four knots placed at the 5th, 35th, 65th, and 95th percentiles of the change in the predicted appendicular skeletal muscle mass index, body fat mass index, and lean BMI. The hazard ratios (95% confidence interval) were calculated by Cox proportional hazards regression analysis after adjusting for age, BMI at baseline and follow-up, household income, smoking status, alcohol intake, physical activity, systolic blood pressure, fasting serum glucose, total cholesterol, and Charlson Comorbidity Index.
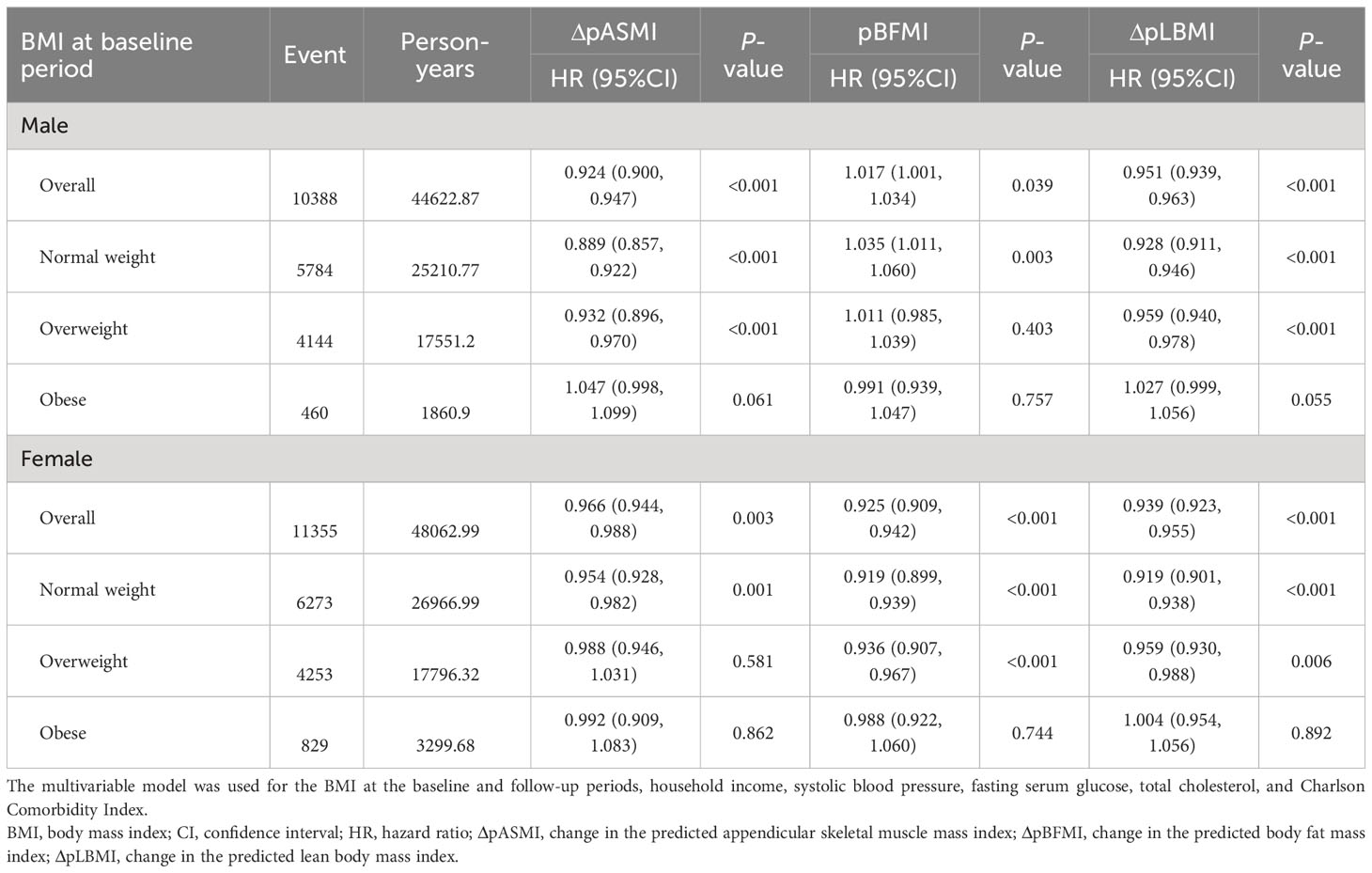
Table 3 Hazard ratios and 95%CI of heart failure per 1 kg/m2 increase in the change in the predicted body composition index stratified by the BMI group.
Table 4 shows the effect of BMI changes during the two health examinations on the occurrence of HF according to changes in body composition. Participants who maintained a stable weight (change in BMI ± 1 kg/m2) had a reduced incidence of HF occurrence per 1 kg/m2 increase in ΔpLBMI and ΔpASMI for males (HR:0.928, 95%CI 0.911-0.946; HR:0.894, 95%CI 0.863-0.927, respectively) and females (HR:0.923, 95%CI 0.904-0.943; HR:0.963, 95%CI 0.935-0.993, respectively). Male participants had an increased incidence of HF per 1 kg/m2 increase in ΔpBFMI (HR: 1.028; 95%CI: 1.005-1.050). However, female participants had a decreased incidence of HF per 1 kg/m2 increase in ΔpBFMI (HR: 0.918; 95%CI: 0.899-0.937; Table 4).

Table 4 Hazard ratios and 95%CI of heart failure per 1 kg/m2 increase in the change in the predicted body composition index stratified by a change in the BMI group.
The occurrence-reducing effects of the increase in ΔpASMI and ΔpLBMI were observed in male participants whose BMI increased from normal to obese or overweight and from overweight to obese. The occurrence-reducing effect of the increase in the ΔpASMI and ΔpLBMI was also observed in female participants whose BMI increased from normal to overweight and obese. The decrease in the ΔpBFMI showed an occurrence-reducing effect in male participants whose BMI decreased from overweight or obese to normal and from obese to overweight. However, the increase in the ΔpBFMI showed an occurrence-reducing effect in female participants whose BMI increased from normal to obese or overweight and from overweight to obese (Table 4; Supplementary Table 3). In the subgroup analysis, there was no heterogeneity among the groups, except for age (Supplementary Table 4).
In this large-scale cohort study, we found that decreased ΔpASMI and ΔpLBMI were negatively correlated with the occurrence of HF, regardless of sex. The occurrence-reducing effects of increased ΔpASMI and ΔpLBMI on the occurrence of HF were alleviated when the participants were more obese and when their BMI increased. In males, an increased ΔpBFMI showed a positive relationship with the occurrence of HF. The occurrence-increasing effect of increased ΔpBFMI on the occurrence of HF was more prominent when male participants were less obese and when the BMI of participants decreased. In contrast, decreased ΔpBFMI showed a negative relationship with the occurrence of HF in females. The occurrence-reducing effect of increased ΔpBFMI on the occurrence of HF was alleviated when the female participants were obese and when their BMI increased.
Previous studies showed that sarcopenia, which is primarily characterized by a progressive and widespread decline in skeletal muscle mass and muscle dysfunction, is common in patients with HF (about 10%) and is strongly related to the prognosis of HF (22). Also, loss of lean body mass was related to the occurrence of HF, particularly among older males (23). Various mechanisms, including malnutrition and anorexia, physical inactivity, and insulin resistance, cause an increase in muscle protein catabolism, resulting in a loss of muscle or body weight, which is associated with HF (24). Although present study could not confirm the causal relationship, in other hand, some studies suggested that muscle wasting is a consequence of HF and HF lead to several complications including musculoskeletal abnormalities and sarcopenia (25, 26). The present study showed that increased change in muscle mass had a negative relationship with the occurrence of HF, and the negative correlation was more attenuated when the participants were more obese and when the BMI of participants increased.
This study investigated sex-related differences in the association between changes in body fat mass and HF. Although the fat distribution varies according to sex, the role of obesity in the occurrence of HF in females may differ from that in males. Generally, males store sufficient fat in a visceral distribution, while females store sufficient fat in a peripheral subcutaneous distribution (27). These differences in location for stocking excessive fat have been shown to persist even after menopause. In males, visceral fat mass is associated with adiposopathy, which includes fat cell hypertrophy, increased circulating free fatty acids, and inflammatory and immune responses, leading to common metabolic diseases and HF (28, 29). The present study showed that an increased change in the body fat mass had a positive relationship with the occurrence of HF, and the occurrence-increasing effect of the increased change in body fat mass was more noticeable when the male participants were less obese and when the BMI of participants decreased. In females, peripherally distributed fat has a negative impact on exercise intolerance (30). Also, female patients with HF were found to be in a catabolic state and have more metabolic reserves. If patients experienced malnutrition, the burden of morbidity and mortality for HF increased, and loss of muscle mass occurred, leading to advanced HF (31). In contrast, obese patients showed low adiponectin levels and a decreased catecholamine response, which led to improved HF (32). Finally, obese females showed higher fatty acid uptake and less myocardial glucose utilization compared with obese males, which resulted in differences in myocardial metabolism (33, 34). The present study showed that increased changes in the body fat mass had a negative relationship with the occurrence of HF, and the occurrence-reducing effect of the increased change in body fat mass was more alleviated when the female participants were obese and when the BMI of participants increased.
The strength of our study is that it showed an association between changes in the body composition indices and the occurrence of HF in a large sample of the Korean general population in a longitudinal setting. However, our study has several limitations. First, present study has been conducted using anthropometric prediction equations to estimate body composition. Due to time constraint and cost, measurement of body composition using accurate modalities remains challenging issue in large epidemiological studies. Therefore, we decided to proceed with present study based on previous study which developed prediction equations to indirectly assess body composition using data obtained with dual-energy X-ray absorptiometry as reference (11). These anthropometric prediction equations from the Korean National Health and Nutrition Examination Survey cohort was validated, but it is major limitation of our study. Second, the equation for predicted body composition was estimated for the Korean population aged > 19 years; therefore, these findings may not be generalizable to other ethnicities and may not be directly applicable to different geographic and/or demographic settings. Third, although it was conducted with a longitudinal design, this is a retrospective study; therefore, we could not confirm the causal relationship or exclude confounders. Finally, because this is an epidemiologic study, our study cannot explain the basic mechanism of the association between changes in body composition and HF.
In conclusion, changes in body composition are associated with the occurrence of HF. Decreased ΔpASMI and ΔpLBMI are associated with the occurrence of HF. Furthermore, in males, increased ΔpBFMI was associated with the occurrence of HF. However, in females, decreased ΔpBFMI was associated with the occurrence of HF.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Institutional Review Board approval number: SEUMC 2022-02-018. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
T-JS had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. HW, D-HK, HL, MKK, and T-JS conceived of and designed the study. T-JS and HL conducted the data acquisition and statistical analyses. HW, D-HK, MKK, and T-JS interpreted data and drafted the manuscript. T-JS reviewed and edited the manuscript. All authors contributed to the article and approved the submitted version.
This work was supported by the Institute of Information & Communications Technology Planning & Evaluation (IITP) grant funded by the Korean government (MSIT) (2022–0-00621 to T-JS, Development of artificial intelligence technology that provides dialog-based multi-modal explainability). This research was supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI22C073600, RS-2023-00262087 to T-JS). The funding source had no role in the design, conduct, or reporting of this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2023.1210371/full#supplementary-material
1. Tan LB, Williams SG, Tan DK, Cohen-Solal A. So many definitions of heart failure: are they all universally valid? A critical appraisal. Expert Rev Cardiovasc Ther (2010) 8(2):217–28. doi: 10.1586/erc.09.187
2. Savarese G, Lund LH. Global public health burden of heart failure. Card Fail Rev (2017) 3(1):7–11. doi: 10.15420/cfr.2016:25:2
3. Chang Y, Woo HG, Park J, Lee JS, Song TJ. Improved oral hygiene care is associated with decreased risk of occurrence for atrial fibrillation and heart failure: A nationwide population-based cohort study. Eur J Prev Cardiol (2020) 27(17):1835–45. doi: 10.1177/2047487319886018
4. Inamdar AA, Inamdar AC. Heart failure: diagnosis, management and utilization. J Clin Med (2016) 5(7):62. doi: 10.3390/jcm5070062
5. Obesity WHOCo, World Health O. Obesity : Preventing and Managing the Global Epidemic : Report of a WHO Consultation. Geneva: World Health Organization (2000).
6. Dai H, Alsalhe TA, Chalghaf N, Ricco M, Bragazzi NL, Wu J. The global burden of disease attributable to high body mass index in 195 countries and territories, 1990-2017: An analysis of the Global Burden of Disease Study. PloS Med (2020) 17(7):e1003198. doi: 10.1371/journal.pmed.1003198
7. Ortega FB, Lavie CJ, Blair SN. Obesity and cardiovascular disease. Circ Res (2016) 118(11):1752–70. doi: 10.1161/CIRCRESAHA.115.306883
8. Krauss RM, Winston M, Fletcher BJ, Grundy SM. Obesity : impact on cardiovascular disease. Circulation (1998) 98(14):1472–6. doi: 10.1161/01.CIR.98.14.1472
9. Aune D, Sen A, Norat T, Janszky I, Romundstad P, Tonstad S, et al. Body mass index, abdominal fatness, and heart failure incidence and mortality: A systematic review and dose-response meta-analysis of prospective studies. Circulation (2016) 133(7):639–49. doi: 10.1161/CIRCULATIONAHA.115.016801
10. Hall ME. Body mass index and heart failure mortality: more is less? JACC Heart Fail (2018) 6(3):243–5. doi: 10.1016/j.jchf.2017.12.013
11. Lee G, Chang J, Hwang SS, Son JS, Park SM. Development and validation of prediction equations for the assessment of muscle or fat mass using anthropometric measurements, serum creatinine level, and lifestyle factors among Korean adults. Nutr Res Pract (2021) 15(1):95–105. doi: 10.4162/nrp.2021.15.1.95
12. Park MS, Jeon J, Song TJ, Kim J. Association of periodontitis with microvascular complications of diabetes mellitus: A nationwide cohort study. J Diabetes Complications (2022) 36(2):108107. doi: 10.1016/j.jdiacomp.2021.108107
13. Chang Y, Lee JS, Woo HG, Ryu DR, Kim JW, Song TJ. Improved oral hygiene care and chronic kidney disease occurrence: A nationwide population-based retrospective cohort study. Med (Baltimore) (2021) 100(47):e27845. doi: 10.1097/MD.0000000000027845
14. Kim J, Kim HJ, Jeon J, Song TJ. Association between oral health and cardiovascular outcomes in patients with hypertension: a nationwide cohort study. J Hypertens (2022) 40(2):374–81. doi: 10.1097/HJH.0000000000003022
15. Chang Y, Lee JS, Lee KJ, Woo HG, Song TJ. Improved oral hygiene is associated with decreased risk of new-onset diabetes: a nationwide population-based cohort study. Diabetologia (2020) 63(5):924–33. doi: 10.1007/s00125-020-05112-9
16. Woo HG, Chang YK, Lee JS, Song TJ. Association of Periodontal Disease with the Occurrence of Unruptured Cerebral Aneurysm among Adults in Korea: A Nationwide Population-Based Cohort Study Medicina (Kaunas), Basel, Switzerland: Licensee MDPI, Vol. 57. (2021).
17. Park J, Shin JI, Kim DH, Park J, Jeon J, Kim J, et al. Association of atrial fibrillation with infectivity and severe complications of COVID-19: A nationwide cohort study. J Med Virol (2022) 94(6):2422–30. doi: 10.1002/jmv.27647
18. Kim HJ, Park MS, Shin JI, Park J, Kim DH, Jeon J, et al. Associations of heart failure with susceptibility and severe complications of COVID-19: A nationwide cohort study. J Med Virol (2022) 94(3):1138–45. doi: 10.1002/jmv.27435
19. Lee K, Lee JS, Kim J, Lee H, Chang Y, Woo HG, et al. Oral health and gastrointestinal cancer: A nationwide cohort study. J Clin Periodontol (2020) 47(7):796–808. doi: 10.1111/jcpe.13304
20. Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol. (2004) 57(12):1288–94. doi: 10.1016/j.jclinepi.2004.03.012
21. Choi EK. Cardiovascular research using the korean national health information database. Korean Circ J (2020) 50(9):754–72. doi: 10.4070/kcj.2020.0171
22. Sato R, Vatic M, da Fonseca GWP, von Haehling S. Sarcopenia and frailty in heart failure: is there a biomarker signature? Curr Heart Fail Rep (2022) 19(6):400–11. doi: 10.1007/s11897-022-00575-w
23. Forman DE, Santanasto AJ, Boudreau R, Harris T, Kanaya AM, Satterfield S, et al. Impact of incident heart failure on body composition over time in the health, aging, and body composition study population. Circ Heart Fail (2017) 10(9):e003915. doi: 10.1161/CIRCHEARTFAILURE.117.003915
24. Springer J, Springer JI, Anker SD. Muscle wasting and sarcopenia in heart failure and beyond: update 2017. ESC Heart Fail (2017) 4(4):492–8. doi: 10.1002/ehf2.12237
25. Chandrashekhar Iyer L, Vaishali K, Babu AS. Prevalence of sarcopenia in heart failure: A systematic review. Indian Heart J (2023) 75(1):36–42. doi: 10.1016/j.ihj.2022.12.004
26. Fülster S, Tacke M, Sandek A, Ebner N, Tschöpe C, Doehner W, et al. Muscle wasting in patients with chronic heart failure: results from the studies investigating co-morbidities aggravating heart failure (SICA-HF). Eur Heart J (2012) 34(7):512–9. doi: 10.1093/eurheartj/ehs381
27. Lemieux S, Prud'homme D, Bouchard C, Tremblay A, Despres JP. Sex differences in the relation of visceral adipose tissue accumulation to total body fatness. Am J Clin Nutr (1993) 58(4):463–7. doi: 10.1093/ajcn/58.4.463
28. Clark AL, Chyu J, Horwich TB. The obesity paradox in men versus women with systolic heart failure. Am J Cardiol (2012) 110(1):77–82. doi: 10.1016/j.amjcard.2012.02.050
29. Snijder M, van Dam R, Visser M, Seidell J. What aspects of body fat are particularly hazardous and how do we measure them? Int J Epidemiol (2005) 35(1):83–92. doi: 10.1093/ije/dyi253
30. Haykowsky MJ, Kouba EJ, Brubaker PH, Nicklas BJ, Eggebeen J, Kitzman DW. Skeletal muscle composition and its relation to exercise intolerance in older patients with heart failure and preserved ejection fraction. Am J Cardiol (2014) 113(7):1211–6. doi: 10.1016/j.amjcard.2013.12.031
31. Lavie CJ, De Schutter A, Alpert MA, Mehra MR, Milani RV, Ventura HO. Obesity paradox, cachexia, frailty, and heart failure. Heart Fail Clin (2014) 10(2):319–26. doi: 10.1016/j.hfc.2013.12.002
32. Kistorp C, Faber J, Galatius S, Gustafsson F, Frystyk J, Flyvbjerg A, et al. Plasma adiponectin, body mass index, and mortality in patients with chronic heart failure. Circulation (2005) 112(12):1756–62. doi: 10.1161/CIRCULATIONAHA.104.530972
33. Peterson LR, Soto PF, Herrero P, Mohammed BS, Avidan MS, Schechtman KB, et al. Impact of gender on the myocardial metabolic response to obesity. JACC Cardiovasc Imaging (2008) 1(4):424–33. doi: 10.1016/j.jcmg.2008.05.004
Keywords: body composition, body mass index, obesity, skeletal mass, fat mass, heart failure
Citation: Woo HG, Kim D-H, Lee H, Kang MK and Song T-J (2023) Association between changes in predicted body composition and occurrence of heart failure: a nationwide population study. Front. Endocrinol. 14:1210371. doi: 10.3389/fendo.2023.1210371
Received: 22 April 2023; Accepted: 03 October 2023;
Published: 23 October 2023.
Edited by:
Roberta Zupo, University of Bari Aldo Moro, ItalyReviewed by:
Andrea Milzi, University Hospital RWTH Aachen, GermanyCopyright © 2023 Woo, Kim, Lee, Kang and Song. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tae-Jin Song, a25zdGFyQGV3aGEuYWMua3I=
†ORCID: Tae-Jin Song, orcid.org/0000-0002-9937-762X
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.