- 1College of Health Preservation and Rehabilitation, Chengdu University of Traditional Chinese Medicine, Chengdu, China
- 2Rehabilitation Department, Chengdu Second People’s Hospital, Chengdu, China
- 3Rehabilitation Department, Nuclear Industry 416 Hospital, Chengdu, China
- 4College of Sports and Health, Chengdu University of Traditional Chinese Medicine, Chengdu, China
- 5Acupuncture-Brain Science Research Center, Chengdu University of Traditional Chinese Medicine, Chengdu, China
Objective: To systematically summarize current evidence and determine the clinical effectiveness and safety of Tai Chi for type 2 diabetes mellitus (T2DM) in adults by conducting an overview of systematic reviews (SRs).
Methods: A systematic search encompassing five electronic databases was conducted until July 30, 2023, to identify relevant systematic reviews (SRs) based on randomized controlled trials (RCTs) concerning Tai Chi for T2DM. The methodological quality of the included SRs was assessed using the A MeaSurement Tool to Assess systematic Reviews (AMSTAR 2) and the Risk of Bias in Systematic Reviews (ROBIS) tool. The Preferred Reporting Items for Overview of Systematic Review (PRIO-harms) checklist was used to promote a more balanced reporting of benefits and harms in this overview. Corrected covered area (CCA) was used to calculate the degree of overlapping primary studies. Primary outcome measures were glycosylated hemoglobin (HbA1c) and fasting blood glucose (FBG), while secondary outcomes encompassed health-related quality measures. The GRADE (Grades of Recommendations, Assessment, Development, and Evaluation) framework was utilized to assess the quality of evidence for the outcome measures.
Results: A total of 17 eligible SRs were included in this overview. One SR reported negative conclusions, while the remaining 16 reported positive ones on different outcomes. A total of 4 SRs reported adverse events, either absent or minor. Most of the SRs exhibited critically low quality (15/17) and a high risk of bias (14/17), as indicated by AMSTAR2 and ROBIS, respectively. The CCA was 12.14%, indicating a high degree of primary study overlapping. Evidence from 135 results for 24 outcomes concerning Tai Chi for T2DM was evaluated using the GRADE approach, most of which were rated very low.
Conclusion: Tai Chi shows promise as a potentially effective and safe lifestyle intervention for adults with T2DM, particularly in improving HbA1c, FBG, BMI, and overall quality of life (QoL). However, these results should be cautiously interpreted due to methodological flaws observed in the current SRs and the low quality of the SRs based on GRADE. Furthermore, there is a compelling need for additional well-designed, high-quality RCTs and SRs to establish robust and conclusive evidence regarding the efficacy of Tai Chi for managing T2DM in the future.
Systematic Review Registration: https://www.crd.york.ac.uk/PROSPERO/, identifier CRD 42019140988.
1 Introduction
Diabetes mellitus is a chronic non-communicable disease of global significance, impacting 463 million adults aged 20-79 years, which accounts for approximately 9.3% of the world’s population of this age range (1). Among these cases, more than 90% are of Type 2 Diabetes Mellitus (T2DM) (1). According to the IDF Diabetes Atlas (10th edition) (1), the prevalence of T2DM is projected to escalate to 12.2% by 2045, affecting 783 million people worldwide. The global health expenditure amounted to USD 966 billion in 2021. A nationwide population-based cross-sectional study reported that China’s diabetes incidence stands at 11.2%, encompassing a population exceeding 100 million individuals with diabetes (2). Managing this health-threatening and financially challenging issue has become a major public concern worldwide.
A sedentary lifestyle and physical inactivity are significant contributing factors to the development of T2DM. Within the spectrum of therapeutic approaches, exercise-based lifestyle interventions are gaining increasing prominence in addressing various chronic conditions, including T2DM (3). This is particularly evident in the comprehensive management strategy for T2DM, where exercise therapy is accorded comparable importance alongside blood glucose monitoring and pharmacological therapy. Tai Chi, a holistic mind-body practice blending mindfulness and physical movement, has emerged as a noteworthy clinical intervention. Recent research has suggested its potential as a cognitive treatment for older adults dealing with both T2DM and mild cognitive impairment (4). Moreover, Tai Chi’s efficacy extends to conditions like metabolic syndrome (5), fibromyalgia (6), knee osteoarthritis (7), Parkinson’s disease (8), and insomnia after breast cancer (9), as substantiated by clinical validation. In a bibliometric analysis (10), diabetes ranks 4th among the top 10 conditions for which Tai Chi offers health-enhancing benefits. However, akin to any exercise regimen, Tai Chi is not devoid of potential adverse effects, such as falls, bruises, and even fractures due to sporting injuries.
As such, it is imperative to consider the safety implications of Tai Chi alongside investigating its manifold advantages.
Several systematic reviews (SRs) have investigated the efficacy and safety of Tai Chi as a lifestyle intervention for T2DM. Some of these SRs propose that, compared to other aerobic exercises, Tai Chi could better improve fasting blood glucose (FBG), glycated hemoglobin (HbA1c), balance, and quality of life (QoL) and reduce the high-density lipoprotein (HDL) and body mass index (BMI) of T2DM patients (11–13). Conversely, a different perspective has been presented by several other SRs (14–16), leading to unfavorable conclusions. A consensus among outcome measures remains elusive, and the quality of reporting and methodology in SRs themselves can significantly impact confidence in the derived evidence. As a promising and cost-effective exercise intervention for T2DM management, its effectiveness needs further validation. Hence, this overview of SRs was conducted and reported under the guidance of the checklist of Preferred Reporting Items for Overview of Systematic Reviews (PRIO-harms) (17), aiming to critically appraise the effectiveness, safety, and methodological rigor of currently published SRs based on RCTs that explore Tai Chi’s potential for adult patients with T2DM.
2 Method
2.1 Protocol and registration
The study protocol was registered on the PROSPRO platform (https://www.crd.york.ac.uk/PROSPERO/), with an assigned register: CRD 42019140988. The protocol was published in advance (18).
2.2 Literature search
A systematic search was conducted across five electronic databases: Web of Science, Cochrane Database of Systematic Reviews, MEDLINE via Pubmed, EMBASE via Ovid), and one Chinese electronic database, China National Knowledge Infrastructure (CNKI) from the inception of each database until July 30, 2023, without any language restrictions. The search terms employed included but were not limited to the following: (systematic review OR meta-analysis) AND (tai chi OR taiji OR tai chi chuan OR taijiquan OR chi, tai OR jiquan, tai OR quan, taiji OR chuan, taichi) AND (type 2 diabetes OR type 2 diabetes mellitus OR diabetes mellitus, type 2 OR diabetes mellitus OR noninsulin-dependent OR non-insulin dependent), (系统评价 OR meta分析) AND (太极拳 OR 太极) AND (糖尿病OR 消渴OR 脾瘅), with necessary adjustments made to accommodate the diverse syntax requirements of the respective databases. The full search strategy is listed in Appendix A. In addition, study registries in PROSPERO and gray literature like conference articles and dissertations were searched for supplementary information.
2.3 Inclusion and exclusion criteria
The Population, Intervention, Comparison, Outcome, and Study design (PICOS) strategy was employed in establishing the inclusion and exclusion criteria.
(1) Participants (P): Participants in the primary studies were diagnosed with T2DM according to recognized clinical guidelines.
(2) Intervention (I): Tai Chi (with no restriction on style), or Tai Chi with usual care were eligible interventions in this study. Usual care includes standard anti-diabetic agents (metformin, acarbose, insulin, etc.), nursing, and health education. Exclusions encompassed Tai Chi variations involving specific apparatus-based exercises like Tai Chi sword, Tai Chi ball, and similar adaptations derived from Tai Chi.
(3) Comparisons (C): The control interventions included usual care or treatment as usual and other exercise interventions apart from Tai Chi, such as walking, resistance training, yoga, dancing, etc., placebo (sham exercise), or waiting list. SRs comparing different styles of Tai Chi were excluded.
(4) Outcome measures (O): Primary outcomes were HbA1c and FBG. Secondary outcomes included postprandial blood glucose (PBG), fasting serum insulin (FINS), index of homeostasis model assessment of insulin resistance (HOMA-IR), body mass index (BMI), the Short-Form Health Survey (SF-36), BMI, lipids-related indices (total cholesterol (TCh), triglycerides (TG), high-density lipoprotein (HDL), low-density lipoprotein (LDL)), cognition, balance, and emotion. Safety was measured by adverse events (AEs) such as falls, fainting, bruises, etc.
(5) Study design (S): In this overview, only SRs that encompassed more than one RCT were included. Furthermore, SR protocols, duplicates, network SRs, or SRs lacking complete data or whose full text was unavailable were excluded.
2.4 Eligibility assessment and data extraction
All retrieved citations were imported into Endnote X9 software, and duplicates were filtered and removed by the software. Two independent reviewers (Z-FR and C-XX) screened all the titles and abstracts for relevance, followed by a meticulous assessment of full-text eligibility. A cross-verification process was executed to ensure consistency. The exclusion list with corresponding justifications was provided in Appendix B. A predefined template for data extraction was used to collect the following information from each eligible SR: study features (first author, year of publication, country and region, language and publication type, number of included RCTs and patients recruited), methodological features (participants, interventions, controls, outcomes, and RCT quality assessment tools), and main conclusions of SRs. In instances involving duplicated data, priority was accorded to the most recent iteration due to its heightened methodological rigor and encompassment of a larger number of RCTs. For any instances of missing or incomplete data, the corresponding author was contacted via email. Any disagreements were settled by introducing a third reviewer (J-RJ).
2.5 Assessment of methodological quality and risk of bias
A MeaSurement Tool to Assess systematic Reviews (AMSTAR 2) (19) was used to assess the methodological quality of included SRs. AMSTAR is a popular methodological quality assessment tool for RCT-based SRs (19). AMSTAR 2, an update of AMSTAR released in 2017, incorporates an expansion from 11 items to 16, with a focus on 7 critical domains (items 2, 4, 7, 9, 11, 13, and 15). This updated version accommodates the assessment of both randomized and non-randomized controlled trials, utilizing predefined key items to establish a quality rating. Risk of Bias in Systematic reviews (ROBIS) (20) was applied to evaluate the risk of bias of the included SRs. ROBIS operates through three distinct phases (1): assess relevance (optional) (2), identify concerns with the review process, and (3) judge the risk of bias. Phase 2 includes 4 domains by which bias may be involved in an SR: study eligibility criteria; identification and selection of studies; data collection and study appraisal; and synthesis and findings (20). The evaluation of all included systematic reviews was conducted independently by two reviewers (L-XC, S-XY) in accordance with previously outlined instructions (21). Likewise, in case of any discrepancies, a consensus was reached through group discussion.
2.6 Reporting quality and overlapping assessment
We employed the checklist with PRIO-harms (17) to promote a more balanced reporting of benefits and harms in this overview. Developed from the PRISMA, PRISMA harms, and PRISMA-P statements, and guidelines from related methodological review articles (17), the checklist has a set of 27 items (56 subitems) for reporting benefits and harms in overviews of healthcare interventions (see Appendix C). It is noteworthy that the PRIO-harms checklist encompasses a dedicated segment for addressing overlaps (instances where primary studies are encompassed within multiple eligible systematic reviews, potentially leading to a duplication of outcomes). To tackle this, we employed the concept of Corrected Covered Area (CCA) as a recommended approach for evaluating overlapping effects.
While overviews based on SRs provide evidence with a broader summary of the current information available, their statistical power can become disproportionate when primary studies (usually RCTs) are incorporated into multiple SRs (22). Therefore, in conjunction with the PRIO-harms checklist (17), the CCA (22) was used to quantify the extent of overlap in this overview. This overlap was further visualized using an upset plot. The calculation formula was as follows: CCA=(N-r)/(rc-r) (22), where N represents the number of included publications (RCTs in this study, including double counting); r stands for the number of included index publications (rows in the citation matrix) defined as the first appearance of a primary publication; c is the number of included SRs (columns in the citation matrix). The CCA values were categorized as follows: 0 to 5 for slight overlap, 6 to 10 for moderate overlap, 11 to 15 for high overlap, and exceeding 15 for very high overlap (22). The upset plot was made by the online tool Bioladder (https://www.bioladder.cn/web/#/chart/16).
2.7 Evidence quality assessment
The Grades of Recommendations, Assessment, Development, and Evaluation (GRADE) (23) framework was used to assess the evidence quality regarding the main outcomes of the meta-analysis. This assessment encompassed five key domains: study limitations (risk of bias), inconsistency, indirectness, imprecision, and publication bias. The evaluation process was conducted using the GRADEpro GDT online (http://www.guidelinedevelopment.org/) by two authors (Z-FR and C-XX) separately. Any discrepancies that arose were resolved through group discussions to achieve a consensus.
2.8 Data synthesis and presentation
The SRs included in the overview were descriptively analyzed. Characteristics of each SR including methodology quality (AMSTAR 2 and ROBIS), interventions, outcomes, and conclusions were summarized in tables and figures. The reporting quality of this overview was demonstrated in the PRIO-harms checklist (see Appendix C). The result of the overlapping assessment was displayed in an upset plot. The evidence profile and summary of findings were generated using the GRADEpro GDT online software.
2.9 Patient and public involvement
Given that this is a literature review, no patient participation was involved in this overview. Beyond the inclusion in peer-reviewed journals, the insights derived from the study findings are intended for dissemination across medical and nursing institutions and communities including patients affected by T2DM.
3 Results
3.1 Results of literature search and selection
The search yielded a total of 192 citations. A total of 71 duplicates were removed and an additional 87 citations were excluded through the initial screening of titles and abstracts. A comprehensive full-text assessment was conducted on 34 citations, resulting in the exclusion of 17. Consequently, 17 SRs were ultimately included in this study. The flowchart of the study selection is shown in Figure 1. The exclusion list with explanations is shown in Appendix B.
Figure 1 Flow diagram of literature search and study selection. The search yielded a total of 192 citations; 71 duplicates were removed and another 87 were excluded through initial screening of titles and abstracts. A total of 34 underwent full-text assessment, with 17 excluded, and finally, 17 SRs were included. The flowchart of the study selection is shown in Figure 1.
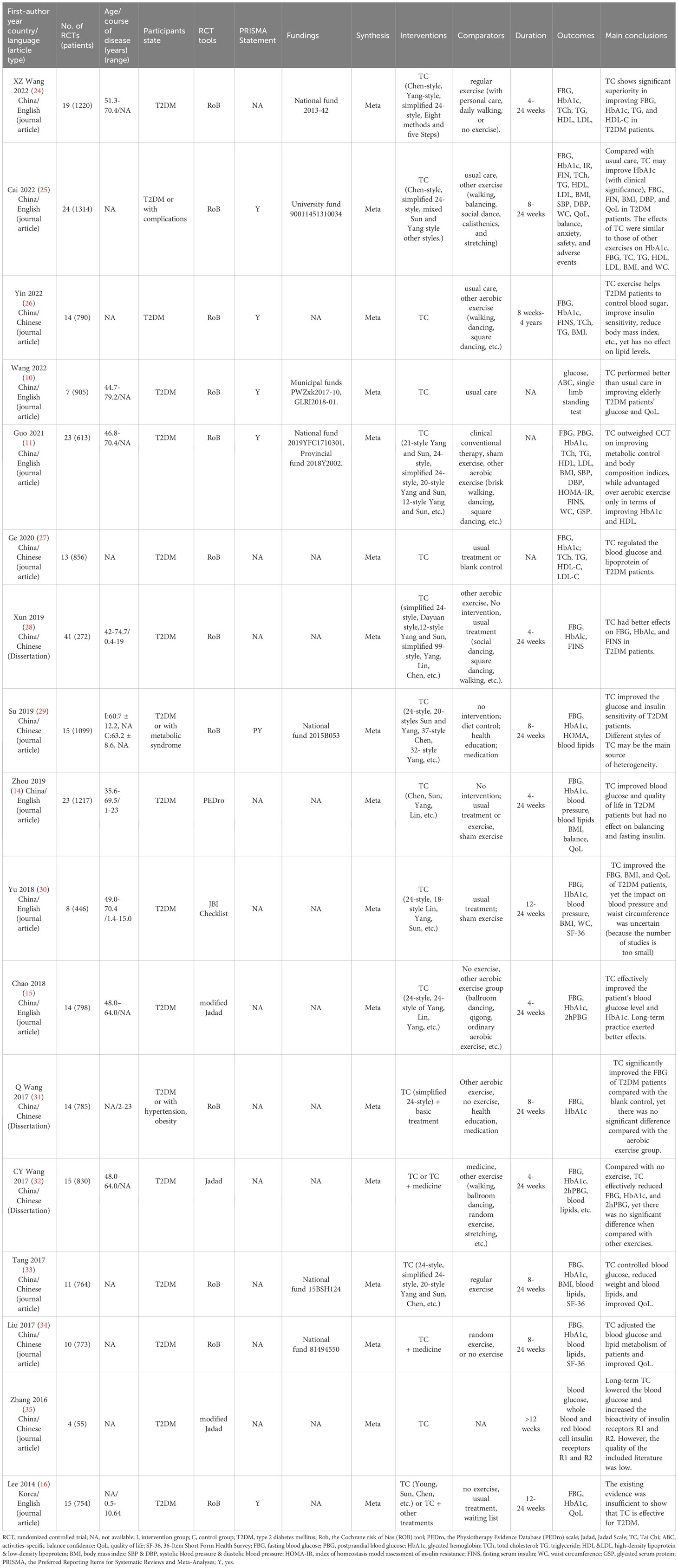
3.2 Characteristics of included SRs
The basic characteristics of the included SRs are presented in Table 1. A total of 17 SRs (11, 14–16, 24–36) published between 2014 and 2022 were included in this overview. Among these, 10 SRs were reported in Chinese and the remaining 7 were in English. Dissertations accounted for 3 of the SRs (28, 31, 32) and the remaining 14 were all journal articles. The majority of these SRs (16 out of 17) were authored by researchers based in China, with the remaining one being from South Korea (16). The number of RCTs included in the SRs ranged from 4 to 24, encompassing patient cohorts ranging from 55 to 1314 individuals. The age of enrolled T2DM patients ranged from 35.6 to 79.2 years old, and the disease duration ranged from 0.4 to 23 years. Four tools were employed to assess the methodological quality of RCTs across the SRs. Specifically, the Cochrane Collaboration Risk of Bias tool was employed in 12 SRs, the (modified) Jadad scale in 3 SRs (15, 35, 36), the PEDro scale in 1 SR (14), and the key evaluation list of JBI RCT in 1 SR (30). Only 1 SR (25) used the GRADE system to assess the evidence quality and 6 SRs (11, 16, 25, 26, 29, 36) were reported under the guidance of the PRISMA Statement.
A total of 7 SRs (11, 24, 25, 29, 33, 34, 36) reported their funding sources, predominantly deriving support from national and provincial entities. All 17 SRs applied meta-analysis. The interventions included Tai Chi, either as a standalone intervention or in conjunction with usual care, while the control groups mainly received treatment as usual or usual care, sham exercises, no treatment or waiting list, and other exercises (walking, dancing, etc.). The duration of interventions varied between 4 weeks and 4 years. The main outcomes included indices related to glucose metabolism, insulin sensitivity, blood lipid profiles, and indicators of QoL. In terms of the results and conclusions, the SR published in 2014 (16) reported a negative conclusion that the existing evidence was insufficient to show that TC is effective for T2DM; while the remaining SRs consistently indicated favorable outcomes for Tai Chi, often demonstrating superior efficacy compared to control conditions, which encompassed usual care alone, waiting lists, and alternative aerobic exercises.
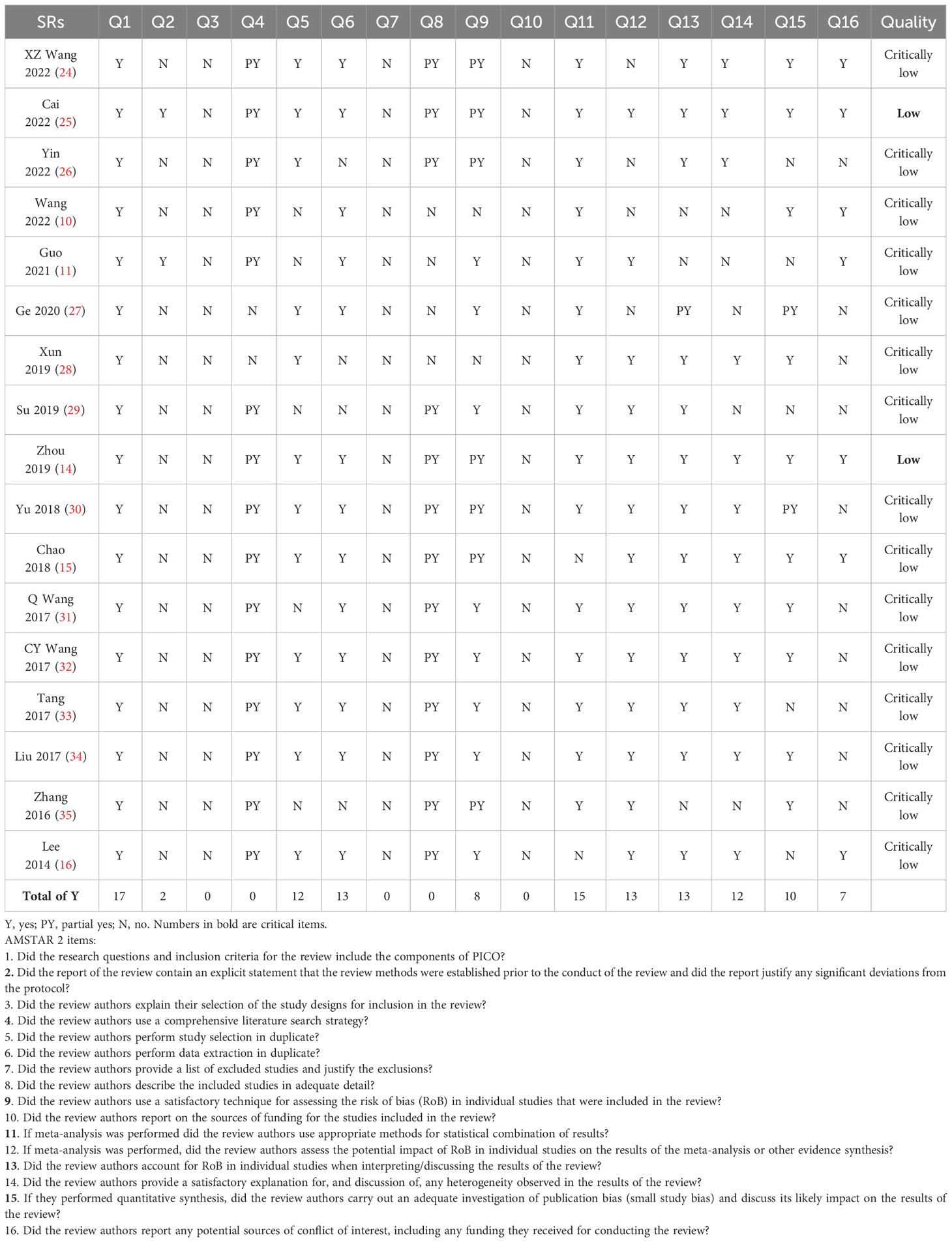
3.3 Methodological appraisal results of included SRs by AMSTAR 2
The findings of AMSTAR 2 methodological quality assessment are shown in Table 2. Among the 17 SRs under evaluation, 15 were rated critically low quality due to the identification of multiple critical weaknesses (items 2, 4, 7, 9, 11, 13, and 15). Additionally, 2 SRs (14, 25) were rated low quality. The majority of the included SRs excelled in implementing the PICO components, study selection, and data extraction in duplicate, followed by choosing appropriate methods for data pooling, assessing the risk of bias with proper tools, and providing appropriate explanations for the results. However, only 2 SRs (11, 25) reported study protocols. Moreover, none of the SRs explained the choice of RCT as the study design, provided a list of excluded studies with justifications, or disclosed funding information.
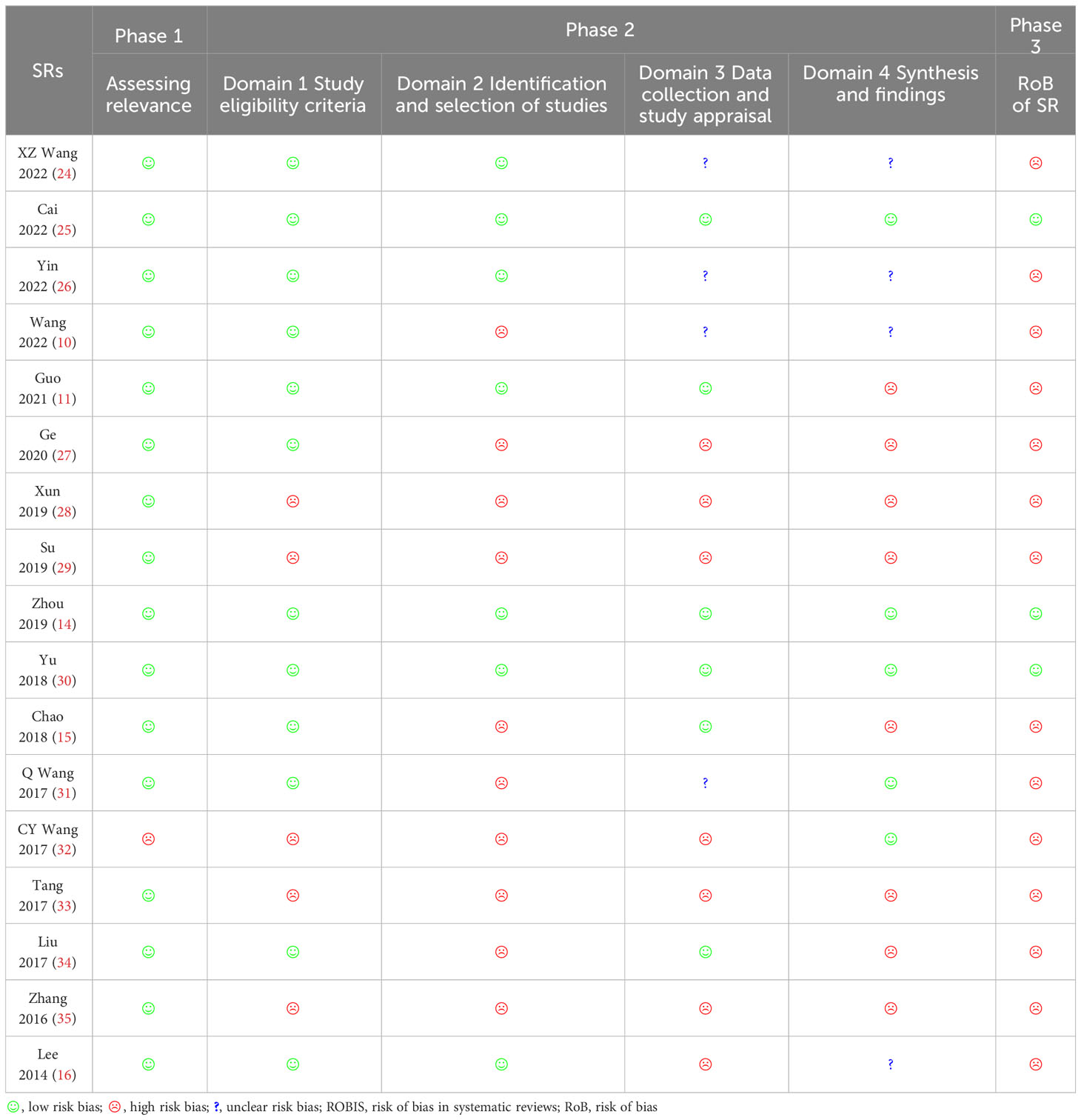
3.4 Risk of bias appraisal results of included SRs
Among the 17 SRs, 3 SRs (11, 14, 25, 30) were rated low risk of bias, and the remaining 14 were assigned a high risk of bias rating. The detailed results are shown in Figure 2 and Table 3. In the assessment of bias risk using ROBIS, 16 SRs (94%) were rated low risk in Phase 1 (assessing relevance). For Phase 2, four domains were investigated. In Domain 1 (study eligibility criteria), 12 SRs (71%) were rated low risk, 7 SRs (41%) low risk in Domain 2 (identification and selection of studies), 6 (35%) low risk in Domain 3 (collection and study appraisal), and 5 (29%) low risk in Domain 4 (synthesis and findings). Three SRs (18%) were rated low risk in Phase 3 (risk of bias in the review).
Figure 2 Results of risk bias of SRs included assessed by ROBIS. For Phase 2, four domains were investigated. In Domain 1 (study eligibility criteria), 12 SRs (71%) were rated low risk, 7 SRs (41%) were rated low risk in Domain 2 (identification and selection of studies), 6 (35%) were rated low risk in Domain 3 (collection and study appraisal), and 5 (29%) were rated low risk in Domain 4 (synthesis and findings). In Phase 3 (risk of bias in the review), 3 SRs (18%) were rated low risk.
3.5 Reporting quality results of this overview
The reporting quality of this overview was demonstrated in the PRIO-harms checklist (see Appendix C).
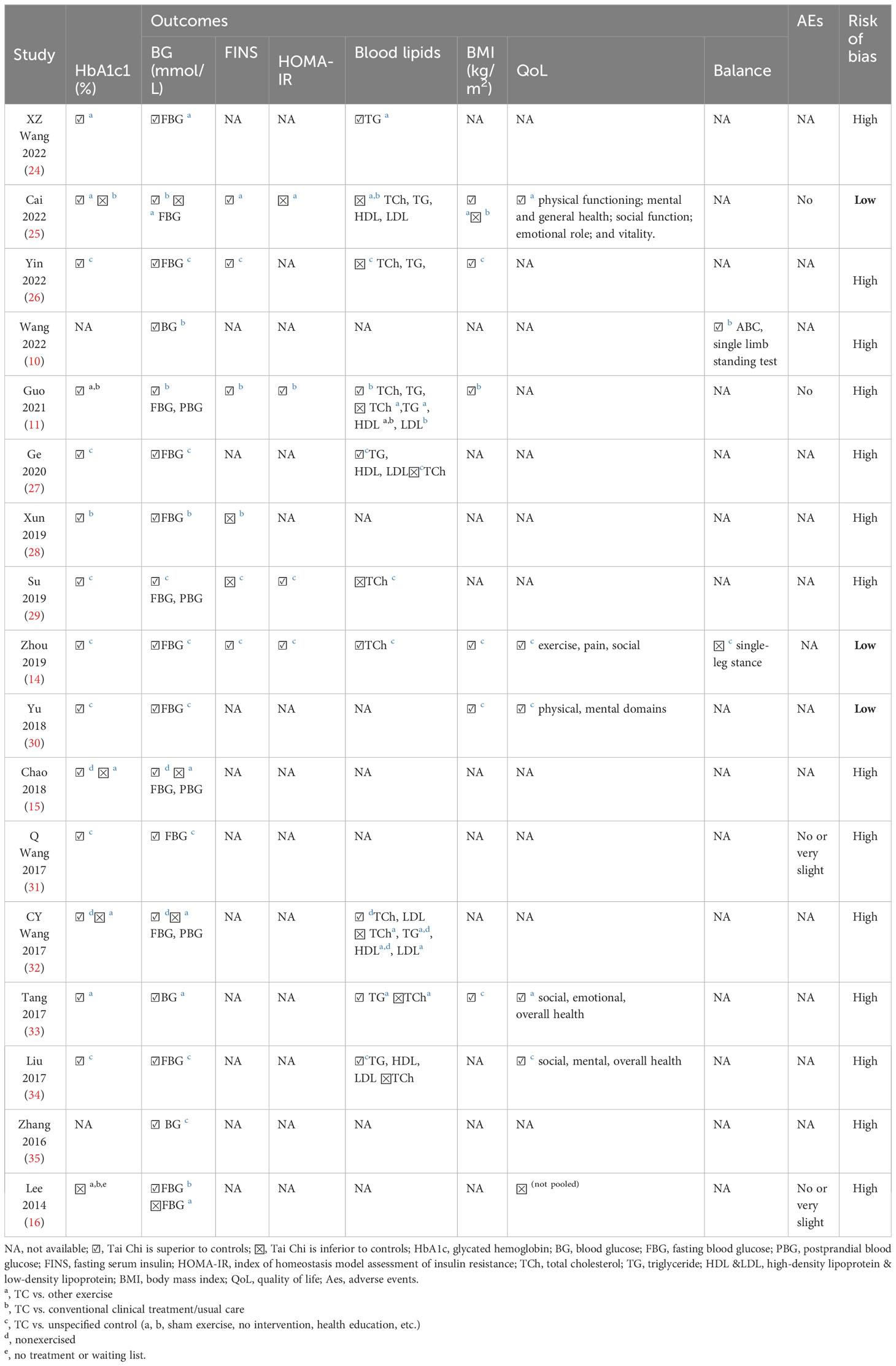
3.6 Effectiveness of Tai Chi for adult patients with T2DM
The effectiveness indices of Tai Chi for adult patients with T2DM are summarized in Table 4. Out of the 17 SRs, 16 (including 3 with low risk of bias) arrived at affirmative conclusions, while the earliest study by Lee in 2014 (16) reported a negative one.
3.6.1 Glycated hemoglobin A1c
HbA1c, a stable glycated hemoglobin molecule, serves as a reflective measure of average blood glucose levels over the past 2 to 3 months, and it assumes a pivotal role in both the management and diagnosis of diabetes mellitus (37, 38). The HbA1c results were presented in 15 SRs. Except for Lee’s 2014 study (16), the remaining 14 SRs (11, 14, 15, 24–34) concurred that Tai Chi demonstrated significant efficacy in reducing HbA1c levels among T2DM patients when compared to controls (mean difference [MD]: -1.48 to -0.59).
3.6.2 Blood glucose indices
All 17 SRs reported the results of blood glucose indices and 14 SRs (11, 14–16, 24–36) reported inconsistent results on FBG outcome. While Tai Chi exhibited superior efficacy in reducing FBG when compared to usual care, no statistically significant differences were observed in comparison to other exercise interventions (15, 16). A total of 3 SRs (15, 29, 32) reported a lower 2hPBG and another 3 (33, 35, 36) demonstrated lower blood glucose levels in the Tai Chi group.
3.6.3 Insulin resistance indices
Five SRs (11, 14, 25, 26, 28) reported lower FINS (mean difference [MD]: -3.00 to -0.28) levels in the Tai Chi group, of which, fouR (11, 14, 25, 29) reported HOMA-IR and one (25) reported a negative result.
3.6.4 Blood lipids
Blood lipids indices mainly include TCh, TG, HDL, and LDL. A total of 10 SRs (11, 14, 24–27, 29, 32, 33, 35) reported results of blood lipids. With the exception of 2 SRs (25, 26), the remaining reviews uniformly indicated that Tai Chi yielded superior reductions in blood lipid indices compared to usual care or no treatment control. See Appendix D for details.
3.6.5 BMI
BMI, calculated as an individual’s weight in kilograms divided by the square of their height in meters (kg/m²), serves as an established metric for gauging body fat. In the evaluation of BMI outcomes, six SRs (11, 14, 25, 26, 30, 33) reported results of BMI (MD:-1.64 to -0.39), reaching a consensus that Tai Chi could reduce BMI more effectively than usual care. Compared with other exercise, Tai Chi did not show an advantage in reducing BMI (25).
3.6.6 Quality of life
Six SRs (14, 16, 25, 30, 33, 34) reported outcomes on QoL as evaluated by SF-36, diabetes-specific QoL (DSQoL) instruments. These evaluations encompassed domains such as physical functioning, physical role, pain, general health, vitality, social function, emotional role, and mental health. Lee’s study in 2014 (16) reported no difference between Tai Chi and the control group in promoting the QoL of T2DM patients. Conversely, the remaining five indicated Tai Chi’s capacity to augment QoL in aspects relating to physiology (physical functioning, bodily pain), psychology (mental/emotional health), sociality (social participation), and overall health. Yu’s investigation in 2018 (30) reported Tai Chi practice for at least 150 min per week could improve the mental domain of QoL (MD=6.54; 95%CI [0.77, 12.3]; I2 = 61%, p = 0.03), indicating a dose-effect relation of Tai Chi for the QoL of T2DM patients.
3.6.7 Balance
Two SRs (14, 36) reported outcomes on balance, evaluated by the activities-specific balance confidence (ABC), single-limb standing test with eyes open or closed, and single-leg stance assessments. Zhou’s study in 2019 (14) found no difference between Tai Chi and the control group in increasing the duration of single-leg stance (MD=2.71; 95% CI (–3.29, 8.71); p=0.376; I2 = 63.8%, p=0.063). Conversely, Wang’s research in 2022 (36) demonstrated that their Tai Chi group had higher ABC scale scores (MD=9.26, 95%CI [6.68, 11.83], p < 0.001) and single limb standing test scores (MD=8.38, 95%CI [4.02, 12.74], p <0.001) than the controls.
3.7 Safety of Tai Chi for T2DM
The safety is mainly measured by the adverse events reported in the SRs, as evidenced in Table 4. Four SRs (11, 16, 25, 31) reported adverse events characterized as minimal or negligible adverse reactions or injuries, with no instances of severe adverse effects reported. Moreover, a 14-SRs-based overview reported that Tai Chi may be beneficial for improving balance and reducing falls in older people and patients with Parkinson’s disease (39). Consequently, the consensus within the available evidence suggests that Tai Chi remains a favorable safety intervention for individuals with T2DM.
3.8 Results of overlapping assessment by CCA
The total number (N) of included publications was 292 (including double counting), the number of index publications (without double counting) r was 96, and the number of SRs c was 17. Based on the formula CCA=(N-r)/(rc-r)*100%, the CCA of this overview was 12.14%, indicating a high degree of overlap (22). The upset plot is shown in Figure 3.
Figure 3 Upset plot of overlapping assessment. RCTs shared among all included SRs. Upset plot of the intersection of different RCTs across SRs. The horizontal bar graph (set size) on the left shows the number of RCTs included in each SR. The upper bar graph shows the number of RCTs for each overlapping combination. Black connected circles indicate which SRs are involved in each intersection.
3.9 Evidence quality based on GRADE framework
The GRADE evidence profile and GRADE summary of the findings of the included SRs are displayed in Supplementary Table 1 and Table 5, respectively. Evidence from 135 results concerning 24 outcomes of Tai Chi for adults wit`h T2DM was summarized. The quality assessment indicated that all the evidence was appraised as being of low or very low quality. Among the five contributing factors leading to downgrading, the foremost consideration was limitation (risk of bias), followed by impression (not reaching the optimal information size), inconsistency (o great heterogeneity), and potential publication bias.
4 Discussion
4.1 Summary of study findings
This overview has summarized the effectiveness and safety of Tai Chi for adult patients with T2DM, based on 17 SRs of RCTs. Only 1 SR (16) drew negative conclusions, while the remaining 16 reported positive conclusions on different outcomes. Most SRs were critically low quality (15/17), with a high risk of bias (14/17), according to the AMSTAR2 and ROBIS, respectively. The CCA (12.14%) indicated a high degree of overlap, possibly suggesting redundant reviews. GRADE assessment rated all evidence as low or very low quality.
4.2 Effects of Tai Chi for T2DM and possible ways to probe its working mechanisms
The current study’s findings highlight Tai Chi’s effectiveness in regulating blood glucose and BMI and enhancing the Quality of Life (QoL) of Type 2 Diabetes Mellitus (T2DM) patients, particularly when compared to usual care or no treatment. However, outcomes regarding insulin resistance, blood lipids, and balance exhibit inconsistency. Notably, Tai Chi demonstrates the potential to ameliorate social function in T2DM patients. Social participation is an important component of the International Classification of Functioning, Disability, and Health (ICF) framework (40), the very basics of rehabilitation. Facilitating the diffusion of Tai Chi exercise under different backgrounds and cultural contexts serves as a way to promote socialization among T2DM patients and participation in the Tai Chi programs themselves (13).
Beyond its impact on physical health, Tai Chi’s influence on motor ability, cognition, and balance in T2DM patients warrants further exploration in future investigations. Attention to the dose-effect relationship of Tai Chi is crucial, as prolonged engagement yields greater benefits (6, 30). While two SRs (14, 36) were inconsistent on balance, Tai Chi still holds promise as a valuable intervention for improving balance, a critical concern for elderly patients, particularly those with diabetic peripheral neuropathy and a high fall risk. In alignment with recommendations by the American Diabetes Association, Tai Chi is suggested as a biweekly to triweekly exercise regimen for older adults with diabetes, specifically for enhancing flexibility and balance (41). Substantiating these claims, an SR published in 2020 (13) also supported Tai Chi’s capacity to enhance balance in T2DM patients.
While Tai Chi may not exhibit unparalleled performance compared to other forms of exercise, it presents distinct advantages in certain aspects. Recent research underscores Tai Chi’s potential as a viable cognitive treatment for older adults grappling with T2DM and mild cognitive impairment (4). Despite sharing aerobic traits with other exercises, Tai Chi’s efficacy cannot be solely attributed to its moderate intensity and energy expenditure. Rooted in traditional Chinese practice, Tai Chi combines dynamic movement and meditation, encapsulating the principles of body regulation (Tiaoshen), mind regulation (Tiaoxin), and respiration regulation (Tiaoxi), as elucidated in prior reviews (42, 43). Researchers are increasingly intrigued by its operational mechanisms and are undertaking mechanism-oriented investigations. Physiologically, elder Tai Chi practitioners exhibit heightened cutaneous microcirculatory function compared to sedentary controls, partly attributed to augmented nitric oxide release (44). Individuals with chronic conditions like T2DM usually have alterations in brain function (45); therefore, Tai Chi’s impact might be rooted in central nervous system modulation. Neuroimaging methods, including functional magnetic resonance imaging (fMRI) and functional near-infrared spectroscopy (fNIRS), have delved into Tai Chi’s mind-regulation potential, including cognitive impairment (46) and subthreshold depression (47). Tai Chi’s body-regulating effects have been explored via omics-based approaches like metagenomics and metabolomics, particularly in systematic ailments like metabolic syndrome, diabetes, and hypertension. Biomechanical analyses employing motion analysis systems and electromyography have investigated its influence on posture control, balance, and coordination (48). Respiratory conditions like chronic obstructive pulmonary disease have been a focal point for understanding Tai Chi’s respiratory regulation. In summary, Tai Chi operates holistically, with a multifaceted mechanism instead of singular elucidation. Given its triad of distinctive attributes, future studies should integrate diverse technologies to unravel Tai Chi’s mechanisms from multifarious perspectives.
4.3 Suggestions for better reporting and methodological quality of SRs and overview of Tai Chi
As commonly acknowledged, the PRISMA guideline serves as a tool for authors to enhance reporting quality and should ideally be consulted prior to or during the conduct of an SR, rather than solely as a post-hoc assessment tool. In this overview, five SRs (11, 16, 25, 26, 36) were reported along with the PRISMA statement. A previous analysis of Tai Chi studies (39) highlighted deficiencies in certain PRISMA items, notably encompassing protocol and registration, search strategy, risk of bias across studies, additional analysis, and funding details. Addressing these areas is imperative for bolstering the overall reporting quality of SRs.
Methodological appraisal was executed through both AMSTAR 2 and ROBIS assessments. The majority of the SRs demonstrated critically low quality (15/17) and exhibited a high risk of bias (14/17). Concerning AMSTAR 2, several SRs fell short in delineating study protocols or registrations, justifying the choice of Randomized Controlled Trials (RCTs) as the selected study design, explaining exclusions with rationales, and detailing study funding sources.
The significance of preregistration and protocol in SRs cannot be understated; they substantially diminish reporting bias, enhance study transparency, curtail redundant publication, and economize authors’ time and effort. Emphasizing formal and standardized preregistration and protocol for SRs contributes to their reliability and should be actively advocated and adopted by SR authors. To ensure coherence and consistency, this overview specifically focused on SRs based solely on RCTs, thereby mitigating the heterogeneity stemming from divergent study types. Additionally, it is crucial for funding sources and potential conflicts of interest to be unequivocally disclosed, thereby augmenting confidence in both RCTs and SRs.
For the ROBIS results, deficiencies predominantly emerged in the identification and selection of studies (Domain 2), collection and study appraisal (Domain 3), and synthesis and findings (Domain 4), largely encompassing methodological aspects. It is worth noting that many SRs included in this overview employed the original version of the RoB tool, rather than the updated RoB 2. While RoB 2 accommodates a broader spectrum of study types, including cluster RCTs and crossover RCTs, it entails a more intricate evaluation process. Consequently, if an SR encompasses study types beyond parallel RCTs, the adoption of RoB 2 is recommended.
SRs have recently gained considerable popularity in recent years, yet the quality of many published SRs falls below optimal standards, with methodology being a prevalent contributing factor. Enhancing reporting and methodology quality necessitates the integration of tools such as PRISMA, as well as assessment instruments like AMSTAR 2 and ROBIS. Raising awareness among SR authors regarding the pivotal role of refining methodology and reporting quality is fundamental to ensuring robust evidence generation from study findings.
Safety concerns related to exercise therapy for Tai Chi have been inadequately reported in many SRs. Given the potential for harm from sports injuries during exercise, heightened attention is warranted toward AEs associated with Tai Chi interventions. Regrettably, only four SRs (11, 16, 25, 31) reported AEs related to Tai Chi exercise therapy for T2DM. To comprehensively evaluate the safety profile of Tai Chi interventions, an increased number of studies, with meticulous AE reporting, is indispensable.
Additionally, due to the nature of Tai Chi exercise, designing and conducting a placebo-controlled RCT poses considerable challenges, particularly in locales where traditional exercises like Tai Chi are prevalent, as in China. Consequently, numerous RCTs on Tai Chi suffer from a heightened risk of bias, particularly concerning blinding, sequence generation, and allocation concealment. For future refinement, specialized guidelines and tools tailored to RCTs on Tai Chi could be pivotal in elevating study quality. In the future, guidelines and tools tailored for RCTs on Tai Chi may be necessary to improve study quality. Drawing inspiration from the Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA) for RCTs on acupuncture could serve as a useful model for developing such resources.
Overviews have been categorized as SRs, and the previous reporting checklist for SRs like PRISMA is also applicable to overviews. However, existing standards have not adequately addressed the issue of overlapping content, despite the potential indication of excessive duplication of SRs (22). This concern has been specifically tackled in the PRIO-harms checklist (17), which incorporates a dedicated section for assessing overlap within this context. To quantify the extent of overlap, the CCA metric has been proposed as a suitable method for evaluating overlap in overviews. The utility of the PRIO-harms checklist has been demonstrated in various studies. It has been successfully applied to overviews of acupuncture and moxibustion (49), traditional Chinese medicine for ulcerative colitis (50), and the application of artificial intelligence for prognostics and health management (51). For the enhancement of reporting standards in overviews or umbrella reviews, we strongly advocate the adoption of the PRIO-harms checklist.
4.4 Strengths and limitations
This comprehensive overview presents the most up-to-date evidence regarding the use of Tai Chi for T2DM, providing a reference for clinical practice. Furthermore, the pilot version of the PRIO-harms checklist, which incorporates assessments of overlapping content, was employed to enhance the reporting quality of this overview. Derived in 2018 from the PRISMA, PRISMA harms, and PRISMA-P guidelines, this checklist aims to ensure balanced reporting of both benefits and harms in overviews.
Nevertheless, certain limitations exist within this overview. Firstly, the inclusion criteria were confined to RCT-based SRs, thereby excluding other types of literature. To expand the scope of analysis, it is advisable to consider incorporating various study designs related to Tai Chi for T2DM in future aggregated analyses. Secondly, the studied population exclusively encompassed adult patients diagnosed with T2DM, potentially neglecting other age groups such as children and teenagers in forthcoming research endeavors. Additionally, a notable proportion of the included SRs exhibited suboptimal methodological quality, displaying a high susceptibility to bias. Consequently, the overall quality of evidence, as evaluated by the GRADE framework, was classified as low or very low, thereby restraining the confidence level of the overview’s concluding remarks. Lastly, while the inclusion of the PRIO-harms checklist represents a notable aspect of this study, it is imperative to acknowledge that the checklist is currently in a pilot phase. The validation of this checklist through rigorous assessments across diverse SRs spanning various subject areas remains relatively limited. Furthermore, its dissemination through established platforms, such as the EQUATOR Network (https://www.equator-network.org/), has been somewhat constrained, which in turn could potentially hinder its broader accessibility to the public.
5 Conclusions
Tai Chi shows promise as a potentially effective and safe lifestyle intervention for adults with T2DM, particularly in improving HbA1c, FBG, BMI, and overall quality of life (QoL). However, these results should be cautiously interpreted due to methodological flaws observed in the current SRs and the low quality of the SRs based on GRADE. Furthermore, there is a compelling need for additional well-designed, high-quality RCTs and SRs to establish robust and conclusive evidence regarding the efficacy of Tai Chi for managing T2DM in the future.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.
Author contributions
FRZ, XC, and XL contributed equally to this manuscript. Study conceptualization: RJ and FRZ. Literature search, and data collection and analysis: FRZ, XC, XL, XS, and TL. Manuscript preparation: FRZ, XC, and XL. Manuscript revision: FZ and RJ. All authors contributed to the article and approved the submitted version.
Funding
This study was financially supported by grants from the National Key Research and Development Project of China (grant number 2019YFC1710302), the National Natural Science Foundation of China (grant number 81873356, 82374559 and 82305360), and the Xinglin Promotion Program for Post-doctorates of Chengdu University of Traditional Chinese Medicine (grant number BSH202020029). The funders had no role in study design, data collection and analysis, report writing, or decision-making for publication.
Acknowledgments
All authors thank Dr. Yunzhou Shi from Chengdu University of Traditional Chinese Medicine for his help with the GRADE methodology.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2023.1208202/full#supplementary-material
References
1. Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, et al. IDF diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract (2021) 183:109119. doi: 10.1016/j.diabres.2021.109119
2. Li YZ, Teng D, Shi XG, Qin GJ, Qin YF, Quan HB, et al. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: national cross sectional study. Bmj-Brit Med J (2020) 369:m997. doi: 10.1136/bmj.m997
3. Luan X, Tian X, Zhang H, Huang R, Li N, Chen P, et al. Exercise as a prescription for patients with various diseases. J Sport Health Sci (2019) 8:422–41. doi: 10.1016/j.jshs.2019.04.002
4. Chen Y, Qin J, Tao L, Liu Z, Huang J, Liu W, et al. Effects of tai chi chuan on cognitive function in adults 60 years or older with type 2 diabetes and mild cognitive impairment in China: A randomized clinical trial. JAMA Netw Open (2023) 6:e237004. doi: 10.1001/jamanetworkopen.2023.7004
5. Siu PM, Yu AP, Yu DS, Hui SS, Woo J. Effectiveness of Tai Chi training to alleviate metabolic syndrome in abdominal obese older adults: a randomised controlled trial. Lancet (2017) 390:S11. doi: 10.7326/M20-7014
6. Wang C, Schmid CH, Fielding RA, Harvey WF, Reid KF, Price LL, et al. Effect of tai chi versus aerobic exercise for fibromyalgia: comparative effectiveness randomized controlled trial. BMJ (2018) 360:k851. doi: 10.1136/bmj.k851
7. Wang CC, Schmid CH, Iversen MD, Harvey WF, Fielding RA, Driban JB, et al. Comparative effectiveness of tai chi versus physical therapy for knee osteoarthritis. Ann Internal Med (2016) 165:77. doi: 10.7326/M15-2143
8. Fuzhong L, Peter H, Kathleen F, Elizabeth E, Ronald S, Johnny G, et al. Tai chi and postural stability in patients with Parkinso’'s disease. N Engl J Med (2012) 366:511–9. doi: 10.1056/NEJMoa1107911
9. Irwin MR, Olmstead R, Carrillo C, Sadeghi N, Nicassio P, Ganz PA, et al. Tai chi chih compared with cognitive behavioral therapy for the treatment of insomnia in survivors of breast cancer: A randomized, partially blinded, noninferiority trial. J Clin Oncol (2017) 35:2656–65. doi: 10.1200/JCO.2016.71.0285
10. Yang GY, Sabag A, Hao WL, Zhang LN, Jia MX, Dai N, et al. Tai Chi for health and well-being: A bibliometric analysis of published clinical studies between 2010 and 2020. Complement Ther Med (2021) 60:102748. doi: 10.1016/j.ctim.2021.102748
11. Guo S, Xu Y, Qin J, Chen Y, You Y, Tao J, et al. Effect of tai chi on glycaemic control, lipid metabolism and body composition in adults with type 2 diabetes: A meta-analysis and systematic review. J Rehabil Med (2021) 53:jrm00165. doi: 10.2340/16501977-2799
12. Qin J, Chen Y, Guo S, You Y, Xu Y, Wu J, et al. Effect of tai chi on quality of life, body mass index, and waist-hip ratio in patients with type 2 diabetes mellitus: A systematic review and meta-analysis. Front Endocrinol (Lausanne) (2021) 11:543627. doi: 10.3389/fendo.2020.543627
13. Palermi S, Sacco AM, Belviso I, Marino N, Gambardella F, Loiacono C, et al. Effectiveness of tai chi on balance improvement in type 2 diabetes patients: A systematic review and meta-analysis. J Aging Phys Activity (2020) 28:787–97. doi: 10.1123/japa.2019-0242
14. Zhou Z, Zhou R, Li K, Zhu Y, Zhang Z, Luo Y, et al. Effects of tai chi on physiology, balance and quality of life in patients with type 2 diabetes: A systematic review and meta-analysis. J Rehabil Med (2019) 51:405–17. doi: 10.2340/16501977-2555
15. Chao M, Wang C, Dong X, Ding M. The effects of tai chi on type 2 diabetes mellitus: A meta-analysis. J Diabetes Res (2018) 2018:7350567. doi: 10.1155/2018/7350567
16. Lee MS, Jun JH, Lim HJ, Lim HS. A systematic review and meta-analysis of tai chi for treating type 2 diabetes. Maturitas (2014) 80:14–23. doi: 10.1016/j.maturitas.2014.09.008
17. Bougioukas KI, Liakos A, Tsapas A, Ntzani E, Haidich A-B. Preferred reporting items for overviews of systematic reviews including harms checklist: a pilot tool to be used for balanced reporting of benefits and harms. J Clin Epidemiol (2018) 93:9–24. doi: 10.1016/j.jclinepi.2017.10.002
18. Chen XX, Zhang FR, Li J, Zhou XJ, Sun MS, Liu XC, et al. Tai Chi for type 2 diabetes mellitus A protocol for systematic review. Medicine (2020) 99:4. doi: 10.1097/MD.0000000000018853
19. Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 358 (2017) 358:j4008. doi: 10.1136/bmj.j4008
20. Whiting P, Savovic J, Higgins JP, Caldwell DM, Reeves BC, Shea B, et al. ROBIS: A new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol (2016) 69:225–34. doi: 10.1016/j.jclinepi.2015.06.005
21. Zhang FR, Sun MS, Han SS, Shen XY, Luo YA, Zhong DL, et al. Acupuncture for primary dysmenorrhea: an overview of systematic reviews. Evidence-Based Complement Altern Med 2018 (2018) 2018:8791538. doi: 10.1155/2018/8791538
22. Pieper D, Antoine SL, Mathes T, Neugebauer EA, Eikermann M. Systematic review finds overlapping reviews were not mentioned in every other overview. J Clin Epidemiol (2014) 67:368–75. doi: 10.1016/j.jclinepi.2013.11.007
23. Pollock A, Farmer SE, Brady MC, Langhorne P, Mead GE, Mehrholz J, et al. An algorithm was developed to assign GRADE levels of evidence to comparisons within systematic reviews. J Clin Epidemiol (2016) 70:106–10. doi: 10.1016/j.jclinepi.2015.08.013
24. Xinzheng W, Fanyuan J, Xiaodong W. The effects of Tai Chi on glucose and lipid metabolism in patients with diabetes mellitus: A meta-analysis. Complement Ther Med (2022) 71:102871. doi: 10.1016/j.ctim.2022.102871
25. Cai Y, Liu X, Zhao A, Mao J, Guo X, Li G, et al. Effects of Tai Chi on health outcomes in patients with type 2 diabetes mellitus: A systematic review and meta-analysis. J Traditional Chin Med Sci (2022) 9:108–20. doi: 10.1016/j.jtcms.2022.04.001
26. Yin TT, Deng SL, Zhang JM, Chen SS. The influence of Tai Chi exercise on physical functioning in patients with type 2 diabetes: a meta-analysis. Bull Sport Sci (2022) 30:68–72. doi: 10.19379/j.cnki.issn.1005-0256.2022.11.022
27. Ge Y, Qin C, Gu XX, Xue YZ. A meta-analysis of the effect of Taijiquan on blood glucose and lipoprotein metabolism in T2DM patients. J Taishan Med College (2020) 41:103–5.
28. Xun CY. Tai Chi for the prevention and treatment of type 2 diabetes: a meta-analyses [master’s thesis]. China: Yangtze University (2019).
29. Su ZJ, Hong P. Meta-analysis of effects of Tai Chi exercise on glycometabolism to the pathoglycermia populations. J Shaanxi Normal Univ (Natural Sci Edition) (2019) 47(3):38–47. doi: 10.15983/j.cnki.jsnu.2019.03.235
30. Yu X, Chau JPC, Huo L. The effectiveness of traditional Chinese medicine-based lifestyle interventions on biomedical, psychosocial, and behavioral outcomes in individuals with type 2 diabetes: A systematic review with meta-analysis. Int J Nurs Stud (2018) 80:165–80. doi: 10.1016/j.ijnurstu.2018.01.009
31. Wang Q. Tai Chi exercise for type 2 diabetes: a systematic review and meta-analyses of RCTs [master’s thesis]. China: Beijing Sports University (2017).
32. Wang CY. Traditional exercise for the rehabilitation of diabetes: a systematic review and meta-analyses[master’s thesis]. China: Shangdong Normal University (2017).
33. Tang Q, Guo YJ, Li P, Yang L, Xiang JZ. Meta-analysis of the effect of Tai Chi in patients with type 2 diabetes mellitus. Modern Prev Med (2017) 44(14):2516–21.
34. Liu YJ, Du B, Huang BW, Yang LQ, Huang SP. Systematic review on effect of Tai Chi regarding to glucolipid metabolism and life quality of type 2 diabetes mellitus. Rehabil Med (2017) 27(4):55–9,64. doi: 10.3724/SP.J.1329.2017.04055
35. Zhang YT, Zhu B, Li CK. Effects of Taiji Exercise on Type 2 diabetes: a meta-analyses. Bull Sport Sci Technol (2019) 24(8):135–6.
36. Wang Y, Yan J, Zhang P, Yang P, Zhang W, Lu M. Tai chi program to improve glucose control and quality of life for the elderly with type 2 diabetes: A meta-analysis. Inquiry (2022) 59:469580211067934. doi: 10.1177/00469580211067934
37. Rooney MR, Tang O, Pankow JS, Selvin E. Glycaemic markers and all-cause mortality in older adults with and without diabetes: the Atherosclerosis Risk in Communities (ARIC) study. Diabetologia (2021) 64:339–48. doi: 10.1007/s00125-020-05285-3
38. American Diabetes Association. 6. Glycemic targets: standards of medical care in diabetes-2021. Diabetes Care (2021) 44:S73–s84. doi: 10.2337/dc21-S006
39. Zhong DL, Xiao QW, Xiao XL, Li YX, Ye J, Xia LN, et al. Tai Chi for improving balance and reducing falls: An overview of 14 systematic reviews. Ann Phys Rehabil Med (2020) 63:505–17. doi: 10.1016/j.rehab.2019.12.008
40. World Health Organization. International classification of functioning, disability and health (ICF) (World Health Organization). (2007).
41. American Diabetes A. Standards of medical care in diabetes-2019 abridged for primary care providers. Clin Diabetes (2019) 37:11–34. doi: 10.2337/cd18-0105
42. Zhang F, Chen X, Shen X, Jin R. Taijiquan in der klinischen Rehabilitation – Teil II. Chinesische Med / Chin Med (2021) 36:93–100. doi: 10.1007/s00052-021-00013-5
43. Zhang F, Chen X, Shen X, Jin R. Taijiquan in der klinischen Rehabilitation – Teil I. Chinesische Med / Chin Med (2021) 36:23–9. doi: 10.1007/s00052-021-00005-5
44. Wang JS, Lan C, Wong MK. Tai Chi Chuan training to enhance microcirculatory function in healthy elderly men. Arch Phys Med Rehabil (2001) 82:1176–80. doi: 10.1053/apmr.2001.24305
45. Crisostomo J, Duarte JV, Moreno C, Gomes L, Castelo-Branco M. A novel morphometric signature of brain alterations in type 2 diabetes: Patterns of changed cortical gyrification. Eur J Neurosci (2021) 54:6322–33. doi: 10.1111/ejn.15424
46. Zhong XY, Yan XH, Liang H, Xia R, Chen B, Zhao HJ. Evaluation of eight-style Tai chi on cognitive function in patients with cognitive impairment of cerebral small vessel disease: study protocol for a randomised controlled trial. BMJ Open (2021) 11:e042177. doi: 10.1136/bmjopen-2020-042177
47. Xie XT, Song J, Zhu JF, Han MY, He YZ, Huang J, et al. The effectiveness of Tai Chi on the depressive symptom of young adults with subthreshold depression: a study protocol for a randomized controlled trial. Trials (2021) 22:106. doi: 10.1186/s13063-021-05054-6
48. Chan SP, Luk TC, Hong Y. Kinematic and electromyographic analysis of the push movement in tai chi. Br J Sports Med (2003) 37:339–44. doi: 10.1136/bjsm.37.4.339
49. Wang LJ, Zeng Q, Xie YJ, Chen D, Yao DY, Chen X, et al. [Normativity of overview report of the systematic review of acupuncture and moxibustion at home and abroad based on PRIO-harms scale]. Zhongguo Zhen Jiu (2020) 40:793–8. doi: 10.13703/j.0255-2930.20190508-k0004
50. Shen ZF, Wu HH, Zhu L, Zhou Q, Shen H. [Traditional Chinese medicine for ulcerative colitis: systematic reviews based on PRIO-harms]. Zhongguo Zhong Yao Za Zhi (2020) 45:674–82. doi: 10.19540/j.cnki.cjcmm.20190624.501
Keywords: Tai Chi, type 2 diabetes, overview, AMSTAR2, PRIO-harms checklist, GRADE
Citation: Zhang F, Chen X, Liu X, Shen X, Liu T, Zeng F and Jin R (2024) Lifestyle intervention Tai Chi for adult patients with type 2 diabetes mellitus: a PRIO-harms based overview of 17 systematic reviews. Front. Endocrinol. 14:1208202. doi: 10.3389/fendo.2023.1208202
Received: 18 April 2023; Accepted: 06 December 2023;
Published: 17 January 2024.
Edited by:
Hamid Reza Baradaran, Iran University of Medical Sciences, IranReviewed by:
Sakib Mohammad Moinuddin, East Bay Institute for Research and Education, United StatesYouhua Wang, Shanghai University of Traditional Chinese Medicine, China
Farzaneh Barzkar, Iran University of Medical Sciences, Iran
Copyright © 2024 Zhang, Chen, Liu, Shen, Liu, Zeng and Jin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fang Zeng, emVuZ2ZhbmdAY2R1dGNtLmVkdS5jbg==; Rongjiang Jin, anJqMTMzQDEyNi5jb20=
†These authors have contributed equally to this work
 Furong Zhang
Furong Zhang Xixi Chen1†
Xixi Chen1† Tianyu Liu
Tianyu Liu Fang Zeng
Fang Zeng Rongjiang Jin
Rongjiang Jin