- 1Sheffield Endocrine Surgery Unit, Sheffield Teaching Hospitals, Sheffield, United Kingdom
- 2School of Medicine and Biomedical Sciences, University of Sheffield, Sheffield, United Kingdom
Objective: To report findings of pilot study using a novel point of care (POC) intraoperative parathyroid hormone (IOPTH) assay for parathyroid hormone (PTH) using whole blood during surgery for primary hyperparathyroidism (PHPT).
Methods: Patients undergoing surgery for primary hyperparathyroidism from March to November 2022 where intraoperative PTH assay was performed using the NBCL CONNECT IOPTH and the laboratory PTH assay were included (group 1). The biochemistry results were reviewed to determine concordance between NBCL and lab PTH values and diagnostic test parameters of the NBCL CONNECT assay. ‘In-theatre’ times were then compared with a historical cohort (group 2) where the lab-based IOPTH assay alone was used.
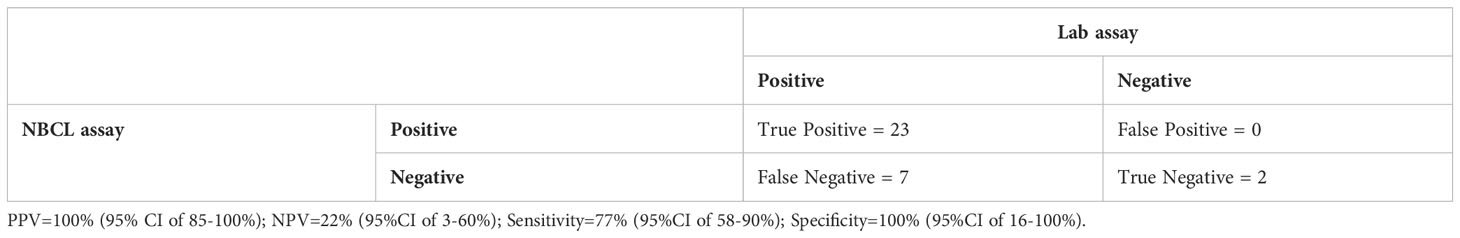
Results: Of the 141 paired samples in group I, correlation between NBCL and the lab assay was high (rho=0.82; p<0.001). PTH levels using the NBCL assay dropped satisfactorily (>50% of the basal or 0 min sample; whichever was lower – i.e. positive test) in 23 patients; giving a positive predictive value of 100%. Of the 9 patients that did not demonstrate a drop, two were true negative (negative predictive value of 22%) leading to cure after excision of another gland. Group 1 (150 mins) had a significantly shorter ‘in-theatre’ time compared to group 2 (167 mins) (p=0.007); despite much higher use of near infra-red autofluorescence (NIRAF) (72% vs 11.6% in group I and 2 respectively).
Conclusion: The NBCL CONNECT POC IOPTH assay gives comparable results to lab based PTH assays and can be performed without need for a centrifuge or qualified technicians. Surgeons, however, need to be aware of the potential for false-negative results.
Introduction
Parathyroidectomy (parathyroid surgery) is the definitive treatment for primary hyperparathyroidism (PHPT) and is curative in around 95% of patients (1). The primary pathology is usually benign and may affect one (single gland disease – SGD) or multiple (multi gland disease – MGD) parathyroid glands; although SGD accounts for ~ 80% of patients (2). The traditional procedure of bilateral neck exploration (BNE) has now largely given way to a targeted or unilateral neck exploration (TP/UNE) in a significant proportion of patients. Currently, TP/UNE accounts for well over 50% of parathyroid surgery in the UK(BAETS) (3). However, this figure is slightly lower (~40-50%) in tertiary centres (2); probably due to the higher proportion of scan negative disease.
In a bilateral neck exploration, dissection to locate/identify all 4 glands has the potential to damage normal glands, increase risk of recurrent laryngeal nerve injury, increase operating time and is reliant on operator experience and judgment to distinguish normal from abnormal glands. This can lead to higher rates of post-surgical hypoparathyroidism (POSH) with significant short-term and long-term morbidity (2). Minimally invasive parathyroidectomy (MIP), in the form of unilateral neck exploration (UNE) or targeted parathyroidectomy (TP) is guided by preoperative identification of an enlarged gland on imaging and appeals to both surgeons and patients given that ~85% of patients have single gland disease (4). This approach may potentially be associated with lower morbidity (5) and reduces hypoparathyroidism to negligible levels. The main limitations of this approach are the potential to miss multi gland disease and increasing failure rate; unless accompanied by frozen section or intra-operative PTH assay (IOPTH) (6).
Failure to cure PHPT is well-recognised (5, 7) potentially due to inability to identify an enlarged gland(s) in eutopic or ectopic locations, failure to recognise presence or extent of multi gland disease (7). Prediction of multi gland disease using defined criteria have been proposed as a solution (8–10). However, published evidence from this unit has shown that these criteria based on pre- and/or intra-operative features do not accurately differentiate single from multi gland disease (2).
Intra-operative parathyroid hormone monitoring (IOPTH) may improve success rates and reduce need for extensive dissection (11, 12). The failure of PTH to drop after excision of a single large parathyroid is a clear indicator of multi gland disease and may reduce failure rates of MIP (5). IOPTH may also be an alternative to frozen section confirmation of parathyroid tissue. Minimally invasive parathyroidectomy utilising IOPTH has been shown to improve cure rates and reduce morbidity in some (13), but not all studies (14–16). Potential limitations include increase in cost and the variably reported risk of false positive and false negative results, which may in turn be due to variations in half-life of PTH (17), definition of baseline value (18) and timing of post-excision assessment (19). The UK National Institute for Health and Care Excellence (NICE) guidance on surgery for PHPT in 2019 (20) did not support routine use of IOPTH given its cost, despite noting a ‘marginal benefit’. However, several UK centres use IOPTH and a recent study has demonstrated cost savings (20), challenging the current NICE guidance. In a recent meta-analysis that demonstrated MIP to be associated with similar success but lower complication rates and operating time compared to BNE (21); however, most (84%) of studies in this review used IOPTH. The shorter operating time in the MIP arm (facilitated by IOPTH) has also enabled the adoption of parathyroidectomy as a day case procedure (13).
The intact PTH hormone has a very short half-life (2-4 minutes) while C-terminal fragments (which account for 80% of total circulating PTH have a much longer half-life (22). There are three generations of PTH assays (23), but currently, most labs use the second-generation assay.
Several ‘lab based’ and ‘point of care’ systems are now available to enable intraoperative assessment of PTH levels. All these assays typically require blood to be collected in a EDTA vial, centrifuged and the serum used to assay PTH. The reported time for the results to be available ranges from 8-16 minutes (24).
Numerous guidelines help define an ‘adequate’ PTH fall that guide the decision to terminate the operation; thereby avoiding the need for further dissection (25). The guidance varies in how to define baseline values, the number and timing of measurements and the definition of an adequate fall in PTH (25).
The standard practice in Sheffield Teaching Hospitals was to obtain a baseline (after induction, but prior to incision) measurement, a further measurement just prior to gland excision and a sample 15 minutes after excision. These three blood samples were sent together to the central lab for PTH assessments. A ‘positive’ result would be a >50% fall of PTH in the 15-minute sample compared to the pre-incision or pre-excision value. This was left to the discretion of the surgeon and depended on consideration of imaging, patient, and disease related factors.
The Novel Biomarkers Catalyst Lab (NBCL) CONNECT analyser enables an intraoperative assessment of PTH levels available withing a few minutes using an intact PTH (second-generation) assay in a single step (sandwich immunoassay), performed on whole blood. This pilot study aims to evaluate the results of surgery for primary hyperparathyroidism following the implementation of the NCBL CONNECT assay in one centre. The objectives of this study include:
1. Determine the accuracy of the results of the NBCL CONNECT assay by comparison with the lab ‘IOPTH’ assay and postoperative adjusted calcium and PTH levels.
2. Compare ‘in-theatre’ time in groups of patients operated using the lab ‘IOPTH’ assay and the ‘NBCL CONNECT’ assay.
3. Explore the ‘false positive’ and ‘false negative’ results obtained by the NBCL CONNECT assay.
Methods
Patients with primary hyperparathyroidism operated using the NBCL CONNECT assay in one UK centre were initially considered for inclusion in the study (Group I). These patients were later compared to a historical cohort (Group II) where the lab IOPTH assay was used. The duration of recruitment was from March 2022 to November 2022 for the NBCL cohort. The pre-operative work up and surgery was performed in a manner consistent with local practice. The operations were performed by or under the supervision of a single consultant surgeon. For all included patients, after intubation and positioning, an ultrasound scan was usually performed to confirm the findings of preoperative imaging and determine the relationship of any enlarged parathyroid glands to the thyroid, carotid artery and internal jugular vein. Following this a bilateral superficial plexus nerve block was performed under ultrasound guidance.
During surgery, samples of venous blood were taken and tested for PTH using both the NBCL CONNECT assay and standard laboratory (Roche) assay simultaneously. The NBCL CONNECT assay was done immediately and used to guide the extent of surgery; while the lab assay was performed later and did not guide surgical decision making. Both these assays are 2nd generation PTH assays.
In general, the timing of blood tests was baseline or pre-incision (after intubation prior to skin incision), time zero or pre-excision (at identification of the enlarged parathyroid gland), 5 minutes and 10 minutes after devascularization and/or excision or the enlarged parathyroid gland. However, in some instances, the timings varied based on the operative findings and the judgement of the operating surgeon.
A positive test result on the NBCL CONNECT assay was defined as a drop in PTH of >50% of the lower of the baseline or ‘0-minute PTH’. A negative test result (unsatisfactory drop in PTH) was defined as a drop in the PTH <50% of the higher of the baseline or ‘0-minute PTH’. If the drop in 10-minute PTH was >50% of the higher of the two pre-excision values but <50% of the lower of the two pre-excision values, the test was considered equivocal.
A positive test result warranted termination of neck exploration. A negative result warranted further neck exploration and search for enlarged parathyroid glands. In the equivocal test results the decision to terminate the operation was made by the operating surgeon based on the clinical circumstances. All these decisions were based on the results of the NCBL assay.
After surgery, postoperative care depended on whether patients were managed as ‘day case’ or whether they were admitted for overnight stay. Patients who were able to go home the same day in accordance with a local ‘day case’ protocol went home on calcium and vitamin D supplements and had a telephone appointment the day after surgery. Patients managed as ‘inpatients’ had serum calcium and PTH measurements the day after surgery and were sent home with supplements dependent on the results of these blood tests.
The primary endpoints were cure rates and correlation between the PTH levels assessed by the NBCL CONNECT and the laboratory assays. Cure was defined as normalisation of PTH and adjusted calcium in postoperative blood samples. Secondary endpoints included assessment of true-positive and true-negative results of the NBCL assay; the gold standard being the laboratory values. Additional endpoints included in-theatre times for patients which was recorded from the operating theatre database where-in the times are logged in by staff in the theatre room. These times were compared to times in another historical cohort of patients in where the laboratory PTH assay was used to guide surgical decision making. Due to the short-term nature of the study, data on longer term follow up was not available.
Demographics, perioperative biochemistry and surgical details were collected, and data was anonymised before analysis. Descriptive analyses included frequencies and percentages for qualitative data, mean and standard deviation for quantitative data that was normally distributed and median and range for quantitative data that was not normally distributed. Inferential methods include the use of Pearson rho correlation coefficient for the correlation of the NBCL CONNECT and the lab PTH assays. Diagnostic parameters of true and false positive and negative tests were calculated for the NBCL CONNECT in comparison to the lab PTH assays. Comparisons of in-theatre times between the two groups were done using the Mann-Whitney U test.
The NBCL CONNECT assay is currently approved for clinical use in the UK and is being introduced in several UK centres. This project was undertaken as a service evaluation project in one UK centres. For this reason, it was not deemed necessary to apply for ethics approval. Permission was however obtained from the directorate of general surgery in Sheffield Teaching Hospitals. No patient identifiable data was accessed by anyone outside the clinical teams. For this reason, informed patient consent was not deemed necessary.
Results
In Group I, 32 patients where the NBCL assay was used during surgery for primary hyperparathyroidism were included during the period March 2022 to November 2022. These included 26 females and 6 males. The median (interquartile range) age of the included patients was 60 (48-72) years. MIBI and USS were performed on all patients. Majority of patients had imaging lateralizing to one side (84% on ultrasound and 75% on MIBI). Concordance between MIBI scan and pre-op USS was 75.0% (24/32). Of these 24 patients, localization was found to be incorrect in one patient.
This study included 141 paired samples from 32 patients for comparative analysis. Of these, correlation between NBCL and the lab assay was high (rho=0.82; p<0.001). PTH levels using the NBCL assay dropped satisfactorily (>50% of the basal or 0 min sample; whichever was lower – i.e. positive test) in 23 patients; giving a positive predictive value of 100% as seen in Table 1. Of the 9 patients that did not demonstrate a drop, two were true negative (negative predictive value of 22%) leading to cure after excision of a further gland. Of the 7 patients with false negative results, further exploration was performed in 5 of them. Sensitivity of the NBCL assay was 77% (95%CI of 58-90%), while specificity was 100% (95%CI of 16-100%). The decision to proceed with further exploration was based on intraoperative findings (including the finding of a second normal gland on that side) and surgical judgement (of the likelihood of single versus multi-gland disease), in combination with the intraoperative PTH results. Biochemical cure with normalization of serum calcium and PTH was achieved in all patients using the NBCL CONNECT assay.
The patients in Group I (n=32) where the NBCL assay was used from March 2022 to November 2022 were compared with a historical cohort of 47 patients prior to the availability of the NBCL assay (group 2) where the lab assay was used. Patients from group 2 underwent their respective procedures from April 2019 to 2021. The baseline characteristics of the two groups of patients are shown in Table 2. Statistically different demographics between both cohorts were noted in the concordance of dual imaging and the use of autofluorescence; both of which were higher in group one. In-theatre times were significantly shorter (p=0.007) in Group I compared to Group II as shown in Table 2.
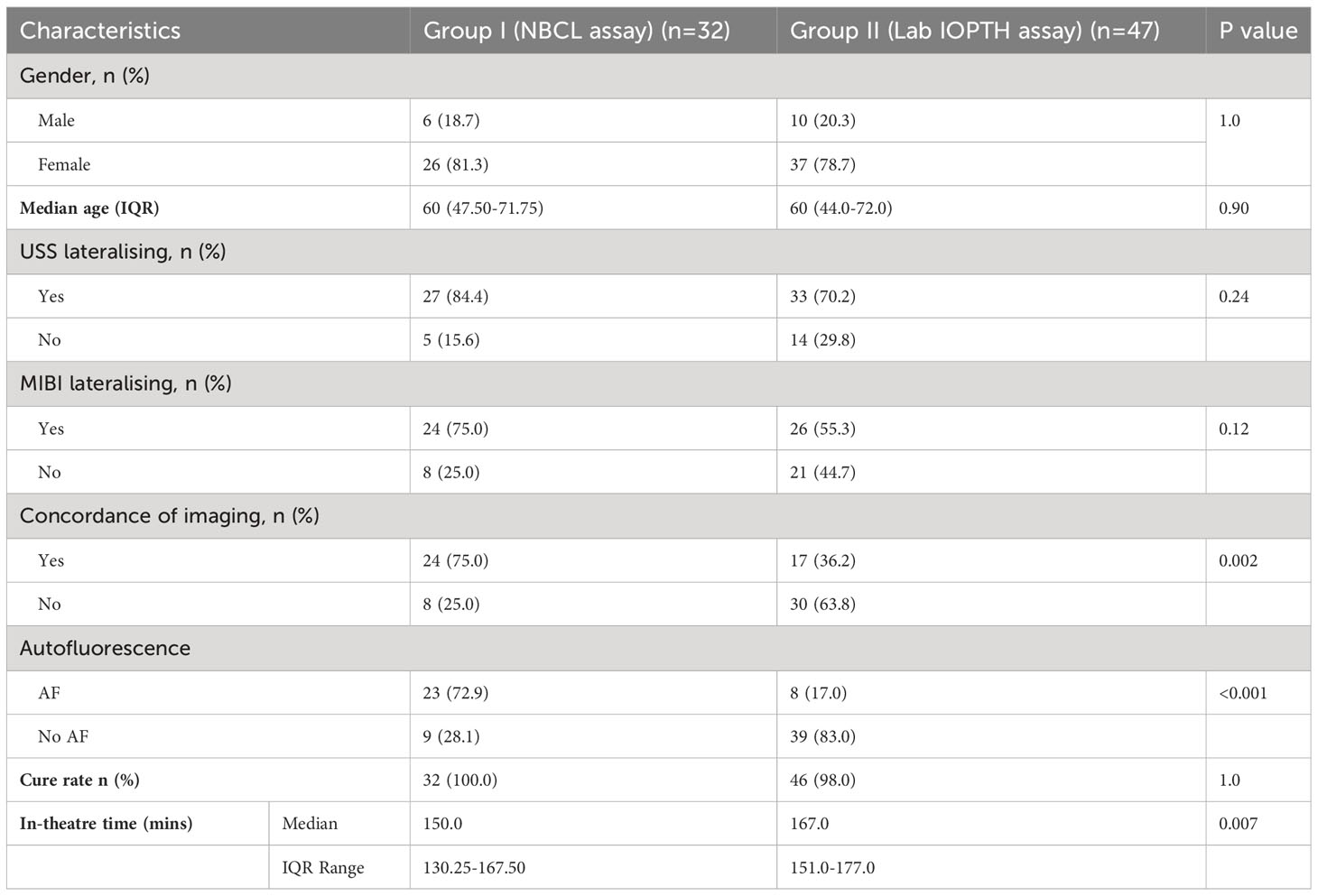
Table 2 Comparison of demographics, radiology findings and clinical outcomes in the NBCL assay cohort (Group I) and the lab assay cohort (Group II).
Discussion
Intra-operative parathyroid hormone (IOPTH) assay is an intraoperative tool which aids in detecting a significant fall in PTH levels during surgery predicting cure of primary hyperparathyroidism, while reducing the need for extensive four-gland dissection and associated post-operative complications (26, 27). Arguments against IOPTH are based on the costs of routine implementation, risks of false positive and false negative test results and uncertain effectiveness in improving patient outcomes (28). However, this view has been challenged, with evidence showing that IOPTH may be cost effective by increasing cure rates and reduce operating times; by reducing the costs of investigations and monitoring in patients with failed operations, complications relating to extensive dissection and prolonged operating times (20).
Results from this pilot study using the NBCL CONNECT assay has shown a high correlation with lab assay in 141 paired samples. In addition, no false positive results have been observed in this small cohort. This positive correlation and performance of the assay in predicting biochemical cure has recently been demonstrated in another study (29); which has not yet been published.
However, within the cohort of 32 patients, there were 7 instances of false negative results. It is expected that ongoing improvements in the technology and software will result in reduction in these false negative results.
When comparing theatre times between the NBCL CONNECT and lab assays, a significant reduction in ‘in-theatre’ times was demonstrated in Group I. As previously highlighted, the NBCL connect analyser doesn’t require centrifugation, can be used by theatre staff and is able to provide results using whole blood within minutes. Conversely, the lab assay would require transport to the laboratory and subsequent analysis by a trained technician, this process is eliminated when using the NBCL CONNECT and may explain the reduction in comparative theatre times.
However, it must be highlighted that in the period in which patients from group 2 underwent their operations, IOPTH was not routinely used for all cases and specifically selected for cases deemed to be challenging by the surgeon. It could be argued that this is a more difficult patient cohort, therefore, prolonging theatre time. A counterpoint to this would be the increased use of auto-fluorescence in group 1 (72.9%) vs group 2 (17.0%) which also would increase ‘theatre-time’.
Limitations
This study has a small sample size, is observational in nature and has a control arm that is historical. Given the retrospective nature of this study, elements of selection bias such as the potential use of IOPTH in ‘more difficult cases’ in the control arm were unavoidable. In addition, the increased use of NIRAF in the NBCL CONNECT arm could potentially confound the outcomes. This study has not compared the use of NBCL assay with currently available ‘in-theatre’ assays; as these are currently not available. Despite this, the results of this pilot study are important and highlight the potential utility of this technology and the concern about false negative results.
Conclusion
The NBCL CONNECT assay showed high correlation with compared with lab based PTH assays. Its advantages over other assays lie in its potential to reduce theatre time and shorter turnaround times. However, surgeons must be aware of the potential of false negatives results, consider intraoperative findings and assess the potential for multi-gland disease; prior to making decisions on further exploration. Further work is ongoing to reduce the risk of false negative results.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Author contributions
RM: substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work. Writing and submission of final manuscript. AP: substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work. EM: substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work. MS: substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work. SB: substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work. Writing and submission of final manuscript.
Funding
Funding of publication by the University of Sheffield Institutional Open Access Fund. For the purpose of open access, the author has applied a Creative Commons Attribution (CC BY) licence to any Author Accepted Manuscript version arising.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Guerrero MA, Clark OH. A comprehensive review of intraoperative parathyroid hormone monitoring. World J Endocrine Surg (2010) 2(1):21–7. doi: 10.5005/jp-journals-10002-1016
2. Bergenfelz A, Lindblom P, Tibblin S, Westerdahl J. Unilateral versus bilateral neck exploration for primary hyperparathyroidism: A prospective randomized controlled trial. Ann Surg (2002) 236(5):543–51. doi: 10.1097/00000658-200211000-00001
3. Aspinall S, Mihai R, Walton P, Kinsman R. British Association of Endocrine & Thyroid Surgeons Sixth National Audit Report 2021. (United Kingdom: Dendrite Clinical Systems Ltd) (2021).
4. Bilezikian JP, Bandeira L, Khan A, Cusano NE. Hyperparathyroidism. Lancet (2018) 391(10116):168–78. doi: 10.1016/S0140-6736(17)31430-7
5. Wilhelm SM, Wang TS, Ruan DT, Lee JA, Asa SL, Duh QY, et al. The American association of endocrine surgeons guidelines for definitive management of primary hyperparathyroidism. JAMA Surg (2016) 151(10):959–68. doi: 10.1001/jamasurg.2016.2310
6. Ishii H, Mihai R, Watkinson JC, Kim DS. Systematic review of cure and recurrence rates following minimally invasive parathyroidectomy. BJS Open (2018) 2(6):364–70. doi: 10.1002/bjs5.77
7. Bagul A, Patel HP, Chadwick D, Harrison BJ, Balasubramanian SP. Primary hyperparathyroidism: an analysis of failure of parathyroidectomy. World J Surg (2014) 38(3):534–41. doi: 10.1007/s00268-013-2434-6
8. Kavanagh DO, Fitzpatrick P, Myers E, Kennelly R, Skehan SJ, Gibney RG, et al. A predictive model of suitability for minimally invasive parathyroid surgery in the treatment of primary hyperparathyroidism [corrected]. World J Surg (2012) 36(5):1175–81. doi: 10.1007/s00268-011-1377-z
9. Kebebew E, Hwang J, Reiff E, Duh QY, Clark OH. Predictors of single-gland vs multigland parathyroid disease in primary hyperparathyroidism: a simple and accurate scoring model. Arch Surg (2006) 141(8):777–82; discussion 82. doi: 10.1001/archsurg.141.8.777
10. Mazeh H, Chen H, Leverson G, Sippel RS. Creation of a "Wisconsin index" nomogram to predict the likelihood of additional hyperfunctioning parathyroid glands during parathyroidectomy. Ann Surg (2013) 257(1):138–41. doi: 10.1097/SLA.0b013e31825ffbe1
11. Calo PG, Pisano G, Loi G, Medas F, Barca L, Atzeni M, et al. Intraoperative parathyroid hormone assay during focused parathyroidectomy: the importance of 20 minutes measurement. BMC Surg (2013) 13:36. doi: 10.1186/1471-2482-13-36
12. Paek SH, Kim SJ, Choi JY, Lee KE. Clinical usefulness of intraoperative parathyroid hormone monitoring for primary hyperparathyroidism. Ann Surg Treat Res (2018) 94(2):69–73. doi: 10.4174/astr.2018.94.2.69
13. Udelsman R, Lin Z, Donovan P. The superiority of minimally invasive parathyroidectomy based on 1650 consecutive patients with primary hyperparathyroidism. Ann Surg (2011) 253(3):585–91. doi: 10.1097/SLA.0b013e318208fed9
14. Helbrow J, Owais AE, Sidwell AG, Frank LM, Lucarotti ME. The use of intraoperative parathyroid hormone monitoring in minimally invasive parathyroid surgery. Ann R Coll Surg Engl (2016) 98(7):516–9. doi: 10.1308/rcsann.2016.0201
15. Nair CG, Babu MJ, Jacob P, Menon R, Mathew J. Is intraoperative parathyroid hormone monitoring necessary in symptomatic primary hyperparathyroidism with concordant imaging? Indian J Endocrinol Metab (2016) 20(4):512–6. doi: 10.4103/2230-8210.183451
16. Soyder A, Unubol M, Omurlu IK, Guney E, Ozbas S. Minimally invasive parathyroidectomy without using intraoperative parathyroid hormone monitoring or gamma probe. Ulus Cerrahi Derg (2015) 31(1):9–14. doi: 10.5152/UCD.2014.2572
17. Libutti SK, Alexander HR, Bartlett DL, Sampson ML, Ruddel ME, Skarulis M, et al. Kinetic analysis of the rapid intraoperative parathyroid hormone assay in patients during operation for hyperparathyroidism. Surgery (1999) 126(6):1145–50; discussion 50-1. doi: 10.1067/msy.2099.101835
18. Riss P, Kaczirek K, Heinz G, Bieglmayer C, Niederle B. A "defined baseline" in PTH monitoring increases surgical success in patients with multiple gland disease. Surgery (2007) 142(3):398–404. doi: 10.1016/j.surg.2007.05.004
19. Riss P, Dunkler D, Selberherr A, Brammen L, Heidtmann J, Scheuba C. Evaluating a shortened interpretation criterion for intraoperative parathyroid hormone monitoring in patients with primary hyperparathyroidism: 5-minutes criterion in primary hyperparathyroidism and intraoperative algorithm. Head Neck (2018) 40(12):2664–9. doi: 10.1002/hed.25453
20. Zammit M, Pierce K, Bailey L, Rowland M, Waghorn A, Shore S. Challenging NICE guidelines on parathyroid surgery. Surgeon (2021) 20(4):e105–11. doi: 10.1016/j.surge.2021.04.008
21. Jinih M, O'Connell E, O'Leary DP, Liew A, Redmond HP. Focused versus bilateral parathyroid exploration for primary hyperparathyroidism: A systematic review and meta-analysis. Ann Surg Oncol (2017) 24(7):1924–34. doi: 10.1245/s10434-016-5694-1
22. Evenepoel P, Bover J, Urena Torres P. Parathyroid hormone metabolism and signaling in health and chronic kidney disease. Kidney Int (2016) 90(6):1184–90. doi: 10.1016/j.kint.2016.06.041
23. Cavalier E, Delanaye P, Nyssen L, Souberbielle JC. Problems with the PTH assays. Ann Endocrinol (Paris) (2015) 76(2):128–33. doi: 10.1016/j.ando.2015.03.018
24. Bornhorst JA, Franco AT, Hinson AM. Laboratory testing, PTH measurement of needle aspirates, and intra operative PTH technologies. In: Stack BC, Bodenner DL, editors. Medical and Surgical Treatment of Parathyroid Diseases An evidence-based approach. Switzerland: Springer International Publishing (2017). p. 517–28.
25. Bhangu JS, Riss P. The role of intraoperative parathyroid hormone (IOPTH) determination for identification and surgical strategy of sporadic multiglandular disease in primary hyperparathyroidism (pHPT). Best Pract Res Clin Endocrinol Metab (2019) 33(5):101310. doi: 10.1016/j.beem.2019.101310
26. Medas F, Cappellacci F, Canu GL, Noordzij JP, Erdas E, Calò PG. The role of Rapid Intraoperative Parathyroid Hormone (ioPTH) assay in determining outcome of parathyroidectomy in primary hyperparathyroidism: A systematic review and meta-analysis. Int J Surg (2021) 92:106042–. doi: 10.1016/j.ijsu.2021.106042
27. Walsh NJ, Sullivan BT, Duke WS, Terris DJ. Routine bilateral neck exploration and four-gland dissection remains unnecessary in modern parathyroid surgery. Laryngoscope Investig Otolaryngol (2019) 4(1):188–92. doi: 10.1002/lio2.223
28. National Institute for Health and Care Excellence aQIfHaCE. Hyperparathyroidism (primary) : diagnosis, assessment and initial management. Hyperparathyroidism (2019) 132:28.
Keywords: parathyroid hormone (PTH), Intraoperative PTH (IOPTH), parathyroidectomy, NBCL CONNECT, point of care (POC)
Citation: Mohan Kumar R, Pannu A, Metcalfe E, Senbeto M and Balasubramanian SP (2023) Findings of pilot study following the implementation of point of care intraoperative PTH assay using whole blood during surgery for primary hyperparathyroidism. Front. Endocrinol. 14:1198894. doi: 10.3389/fendo.2023.1198894
Received: 02 April 2023; Accepted: 09 August 2023;
Published: 25 August 2023.
Edited by:
Terry Francis Davies, Icahn School of Medicine at Mount Sinai, United StatesReviewed by:
Anna Eremkina, Endocrinology Research Center, RussiaSudhaker D. Rao, Henry Ford Hospital, United States
Ana Valea, Iuliu Hatieganu University of Medicine and Pharmacy Cluj-Napoca, Romania
Copyright © 2023 Mohan Kumar, Pannu, Metcalfe, Senbeto and Balasubramanian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rahul Mohan Kumar, cmFodWwubW9oYW5rdW1hcjFAbmhzLm5ldA==
 Rahul Mohan Kumar
Rahul Mohan Kumar Arslan Pannu
Arslan Pannu Emily Metcalfe1
Emily Metcalfe1 Mesfin Senbeto
Mesfin Senbeto Saba P. Balasubramanian
Saba P. Balasubramanian