- Department of Pharmacy, Heyuan People’s Hospital, Heyuan, China
Aims: Obesity is detrimental to infertility. The association between weight-adjusted-waist index (WWI, a recently developed adiposity indicator) and infertility has not previously been confirmed.
Methods: The data for this study were obtained from the National Health and Nutrition Examination Survey (NHANES) 2013-2018. Each participant’s WWI was calculated as their waist circumference in centimeters by the square root of weight in kilograms. Multivariable logistic regression and generalized additive model were utilized to investigate the relationship between WWI with infertility. We used smoothed curve fitting to explore the non-linear relationship. Subgroup analysis and interaction tests were also conducted.
Results: A total of 3,526 participants with ages from18 to 45 were enrolled, 364 of whom were infertile. With the higher WWI, infertility was more prevalent (OR = 1.42, 95% CI: 1.22-1.65), and this association was still consistent in subgroups (all P for interaction> 0.05). Smoothed curve fitting showed a positive non-linear relationship between WWI and infertility. Furthermore, we discovered that WWI had a stronger connection with the risk of infertility than other markers of obesity including WC, body mass index (BMI) and a body shape index (ABSI).
Conclusions: Weight-adjusted-waist index levels were positively linked to an increased risk of infertility in American females and showed a stronger association than other markers of obesity. Our research indicated WWI could help identify women with infertility, and managing obesity as determined by WWI may help to reduce the risk of infertility.
1 Introduction
Infertility is the inability to conceive after routine unprotected sexual activity without the use of contraception for more than 12 months (1, 2). About 7% to 15.5% of women of reproductive age struggle with infertility in the United States (3, 4). It is reported that millions of families around the world, touching roughly one in seven couples in developed countries and one in every four couples in developing countries, were affected by infertility (5). Although infertility is a public health issue of worldwide concern, its determinants have not been fully elucidated.
Obesity, an increasingly widespread health burden in modern society, is increasingly common among women of reproductive age (6–8). This is pertinent since obesity is associated with certain risks, including irregular menstruation and endometrial pathology (9, 10). Obesity has been linked to an increased risk of prenatal diseases such as gestational hypertension and gestational diabetes (11, 12). Body mass index (BMI) was the traditionally recognized benchmark for determining obesity, however, it was unable to differentiate between lean mass and fat mass (13, 14). In 2018, Park et al. suggested a novel anthropometric index entitled the weight-adjusted-waist index (WWI), which can maximize the gains of WC and minimize the association with BMI (15, 16). Therefore, the weight-adjusted-waist index (WWI) reflects weight-independent centripetal obesity. Although WWI is a better predictor of obesity than BMI, its association with infertility has not been previously investigated.
In order to raise awareness of the detrimental consequences of obesity on infertility, it is imperative to identify the association between obesity assessed by WWI and infertility. Therefore, we used the National Health and Nutrition Examination Survey 2013–2018 (NHANES) to find out the association between WWI and infertility in the US female. We hypothesized that the prevalence of infertility was positively linked with the WWI level.
2 Materials and methods
2.1 Data source
The data for this study were obtained from the National Health and Nutrition Examination Survey (NHANES), a national program to assess the state of nutrition and health in the United States, which published by the National Center for Health Statistics (NCHS). To generate a nationally representative sample of non-institutionalized Americans, it was carried out using a sophisticated multistage probability design (17). An in-home interview was conducted by participants to collect data on their health, socioeconomic status, and other factors. A movable examination facility served as the setting for physical and laboratory exams.
All NHANES study methods were approved by the NCHS’s Research Ethics Review Board, and all survey respondents provided their written informed permission. On the website www.cdc.gov/nchs/nhanes/, all detailed NHANES research designs and data are accessible to the public. This cross-sectional study adhered to the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) reporting standards (18).
2.2 Study population
Infertility-related health questions were only included in the NHANES cycles from 2013 to 2018; hence, we used those cycles for our data. We included participants in our analysis who had comprehensive information regarding the infertility and WWI. Initially, a total of 29,400 participants were enrolled. After excluding male participants (n=14,452), those lacking data about the WII (n = 2,478), fertility information (n = 7,236), and women older than 45 and younger than 18 (n= 1,708), 3,526 eligible participants were included in our final analysis (Figure 1).
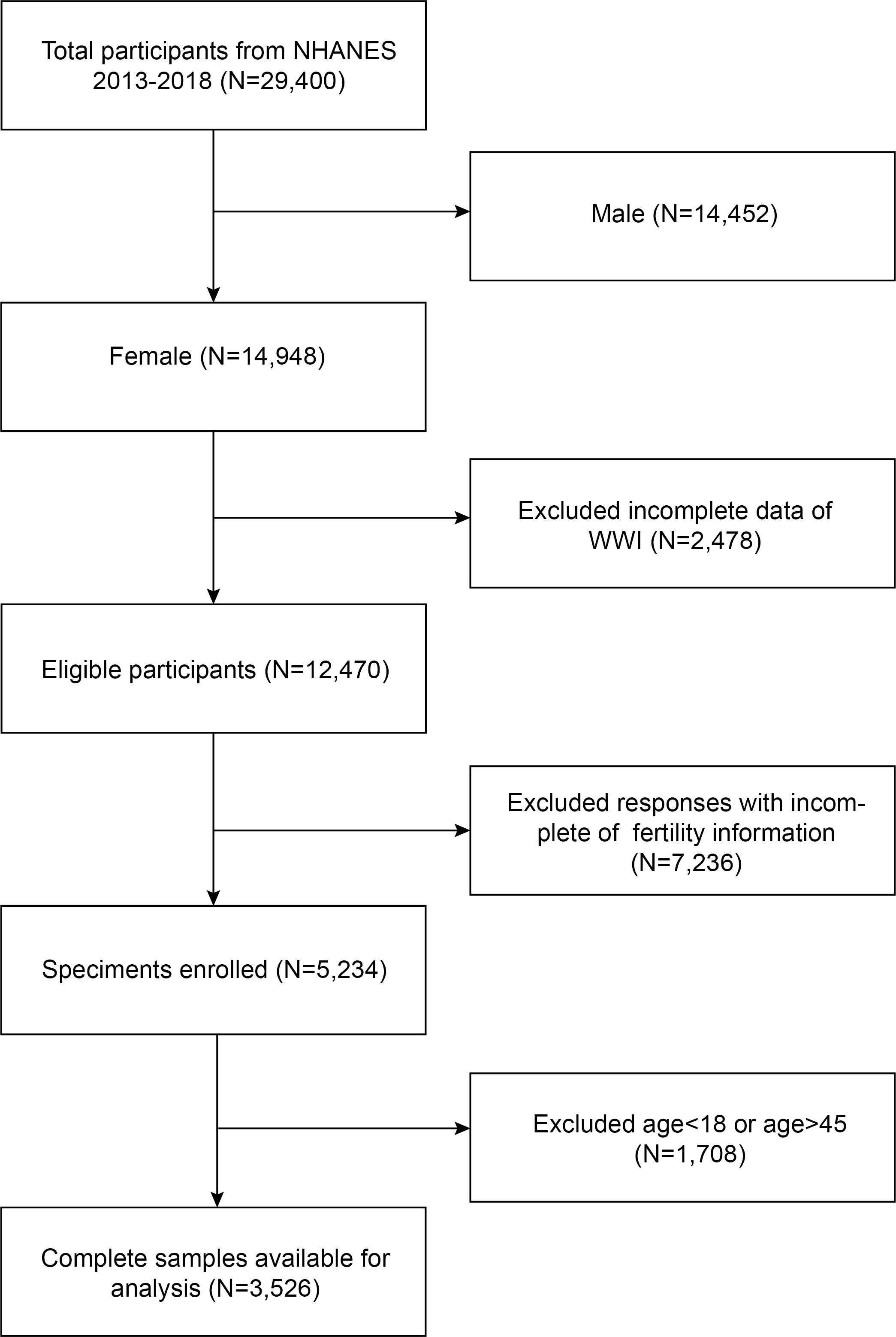
Figure 1 Flowchart of the sample selection from NHANES 2013–2018. A total of 29,400 participants were enrolled. After excluding male participants (n=14,452), those lacking data about the WII (n = 2,478), fertility information (n = 7,236), and women older than 45 and younger than 18 (n= 1,708), 3,526 eligible participants were included in our final analysis.
2.3 Assessment of weight-adjusted-waist index
The WWI is a WC and weight-based anthropometric measure used to evaluate obesity. An increased level of obesity was indicated by a higher WWI score. Health technicians with training in body measurements took measurements of WC and weight in a mobile examination center (MEC). Each participant’s WWI was calculated as their waist circumference in centimeters divided by the square root of weight in kilograms. Participants were grouped according to their WWI tertiles for subsequent analysis, and additionally WWI was treated as a continuous variable in the analysis. In our study, WWI was intended as an exposure. Meanwhile, we used alternative obesity indices including WC, body mass index (BMI) and a body shape index (ABSI) as the exposures. Krakauer NY & Krakauer JC defined A Body Shape Index (ABSI) as (19). To avoid having large numbers for the regression coefficients of ABSI, we multiplied the ABSI values by 1000.
2.4 Assessment of infertility
Each woman’s self-report from the Reproductive Health Questionnaire served as the dependent variable for infertility (variable name in questionnaire: RHQ074). The researchers probed subjects with queries such as, “Tried for a year to become pregnant?” (20). If the answer was “yes,” it signaled an “infertile” situation; if not, it indicated that it was “fertile.”
2.5 Assessment of covariates of interest
Our study also took into account other factors, such as age (years), ratio of family income to poverty, race (Mexican American/other Hispanic/non-Hispanic White/non-Hispanic Black/other races), education level (less than high school/high school/more than high school/others), marital status (married or living with partner/living alone), smoked at least 100 cigarettes (yes/no), had at least 12 alcohol drinks/1 year(yes/no), age when first menstrual period occurred (Age<10/10≤Age<15/15≤Age ≤ 20), had regular periods in past 12 months (yes/no), ever treated for a pelvic infection/pelvic inflammatory disease (yes/no) and ever taken birth control pills (yes/no), which may have an impact on the relationship between WWI and infertility. The complete measurement procedures for these variables were made accessible to the public at www.cdc.gov/nchs/nhanes/.
2.6 Statistical analysis
In accordance with Centers for Disease Control and Prevention recommendations, all statistical analyses were carried out using the proper NHANES sampling weights and took into consideration intricate multistage cluster surveys.
In descriptive analyses, the two compared groups determined by infertility status were assessed using either a weighted Student’s t-test (for continuous variables) or a weighted Chi-square test (for categorical data). Categorical parameters are presented as proportions, whereas continuous variables are summarized as means with standard deviation. Multivariable regression models that took the NHANES complex sampling design (sampling weights) into account were utilized to investigate the association between WWI and infertility. In Model 1, covariates were not adjusted at all. In Model 2, age and race were adjusted. Model 3 were adjusted for age, ratio of family income to poverty, race, education level, marital status, smoked at least 100 cigarettes, had at least 12 alcohol drinks/1 year, age when first menstrual period occurred, ever treated for a pelvic infection/PID, ever taken birth control pills, had regular periods in past 12 months. Stratified multivariable logistic regression models with stratified covariates such as age, race (Mexican American/other Hispanic/non-Hispanic White/non-Hispanic Black/other races), education level (less than high school/high school/more than high school/others), marital status (married or living with partner/living alone), ratio of family income to poverty, smoked at least 100 cigarettes (yes/no), had at least 12 alcohol drinks/1 year(yes/no), had regular periods in past 12 months (yes/no) and age when first menstrual period occurred (Age<10/10≤Age<15/15≤Age ≤ 20) were used to conduct subgroup analysis. To assess its robustness, the continuous variable WWI was transformed into a categorical variable (tertiles) for sensitivity analysis. In order to address the non-linearity of WWI with infertility and each stratification, we additionally employed a generalized additive model (GAM) and smooth curve fittings. A two-piecewise linear regression model (segmented regression model) was used to fit each period and determine the threshold effect if a non-linear connection was showed. If a non-linear association was found, the threshold effect was determined by fitting each interval with a two-piecewise linear regression model (also known as a segmented regression model). The two-step recursive technique was applied to find the breakpoint (K) that connects the segments, which was based on the model that yields the maximum likelihood.
Similarly, the smooth curve fittings were employed to identify the non-linearity of BMI on infertility, and a two-piecewise linear regression model was utilized to further evaluate their threshold effects. All analyses were performed using R version 3.4.3 (http://www.R-project.org, The R Foundation) and Empower software (www.empowerstats.com; X&Y solutions, Inc., Boston, MA). P<0.05 was considered as the statistically significant level.
3 Results
3.1 Baseline characteristics of study participants
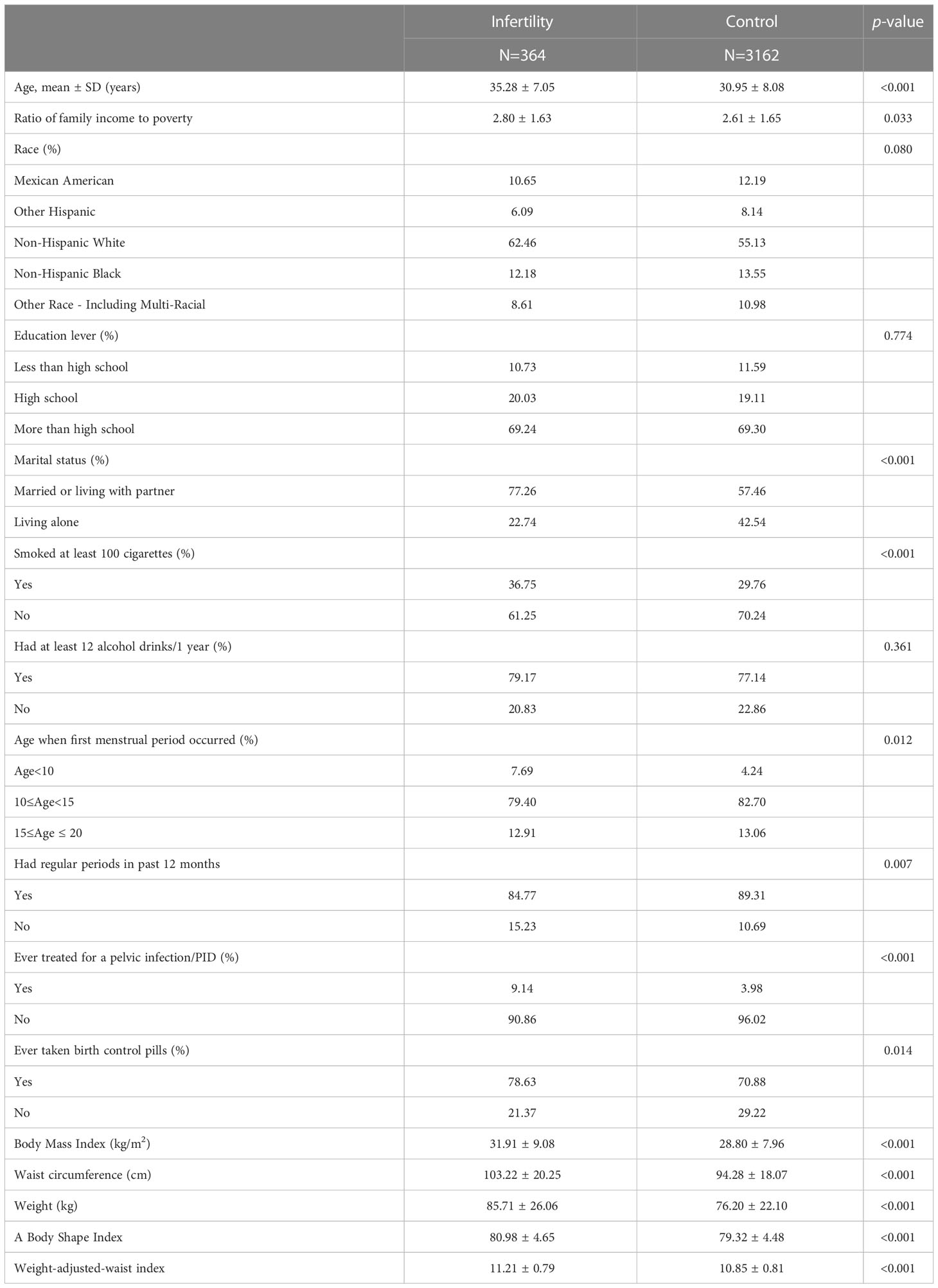
A total of 3,526 participants with ages from18 to 45 were enrolled, 364 of whom were infertile. Based on their infertile status, the research participants’ characteristics are shown in Table 1. Self-reported infertility was more prevalent in women who were older, had higher income to poverty ratios, were married/cohabiting, had smoked at least 100 cigarettes, had been treated for pelvic infection/PID, had taken the pill, or had higher weight, waist circumference and BMI. Besides, self-reported infertility was also significantly more prevalent among women who had higher WWI with an average of 11.21 ± 0.79 (cm/kg(^1/2)).
3.2 The association between weight-adjusted-waist index and infertility
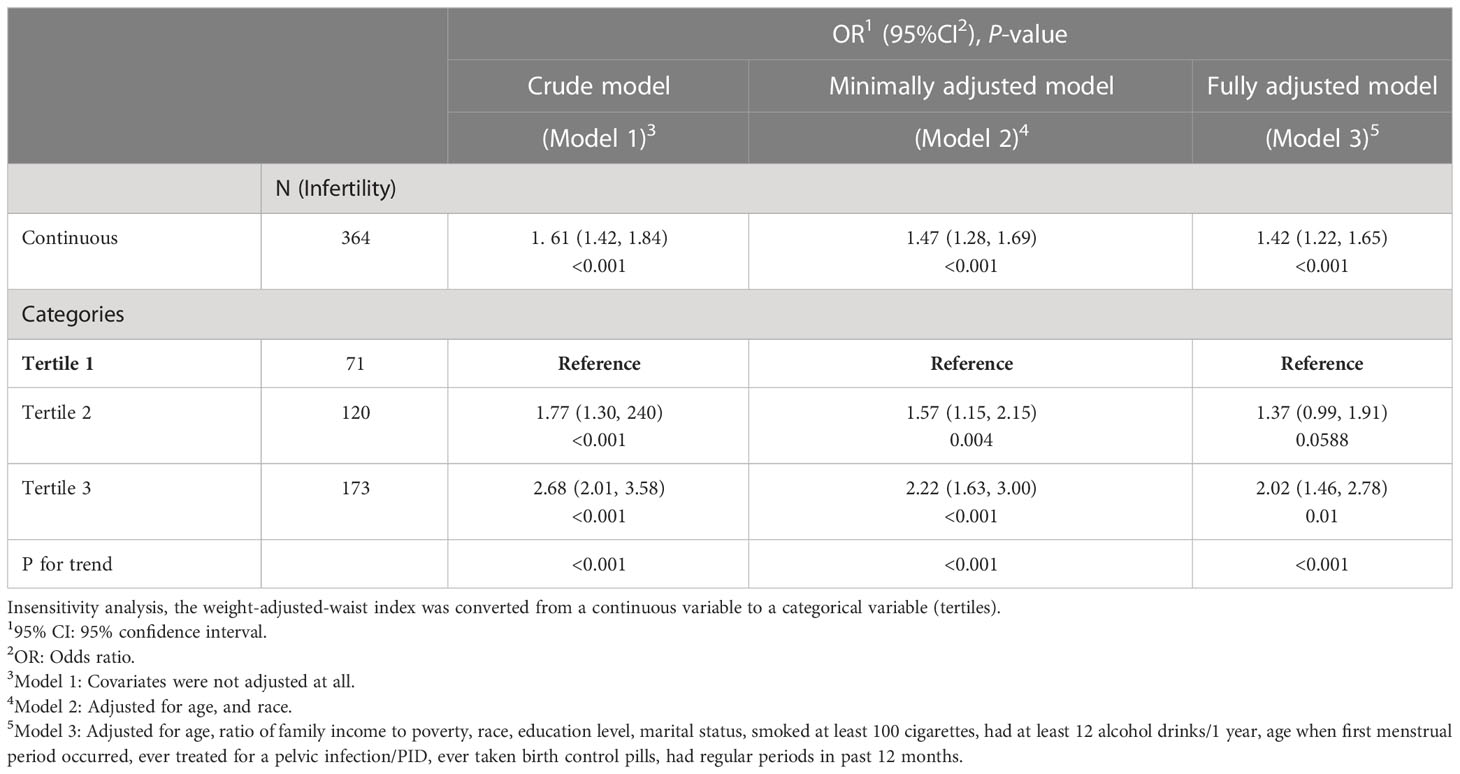
The association between WWI and infertility is seen in Table 2. Our findings indicated that a higher WWI was linked to a higher risk of infertility. Both the crude model and the minimally/fully adjusted model showed evidence of a positive correlation between WWI and infertility. When full adjustments were made, participants with a unit higher WWI had a 42% increased risk of infertility (Model 3: OR = 1.42, 95% CI: 1.22-1.65). After WWI was categorized as tertiles, this association maintained its statistical significance. In comparison to participants in the lowest WWI tertile, individuals in the highest WWI tertile had an importantly 102% increased risk (OR = 2.02, 95% CI: 1.46-2.78; P for trend < 0.001). (Table 2).
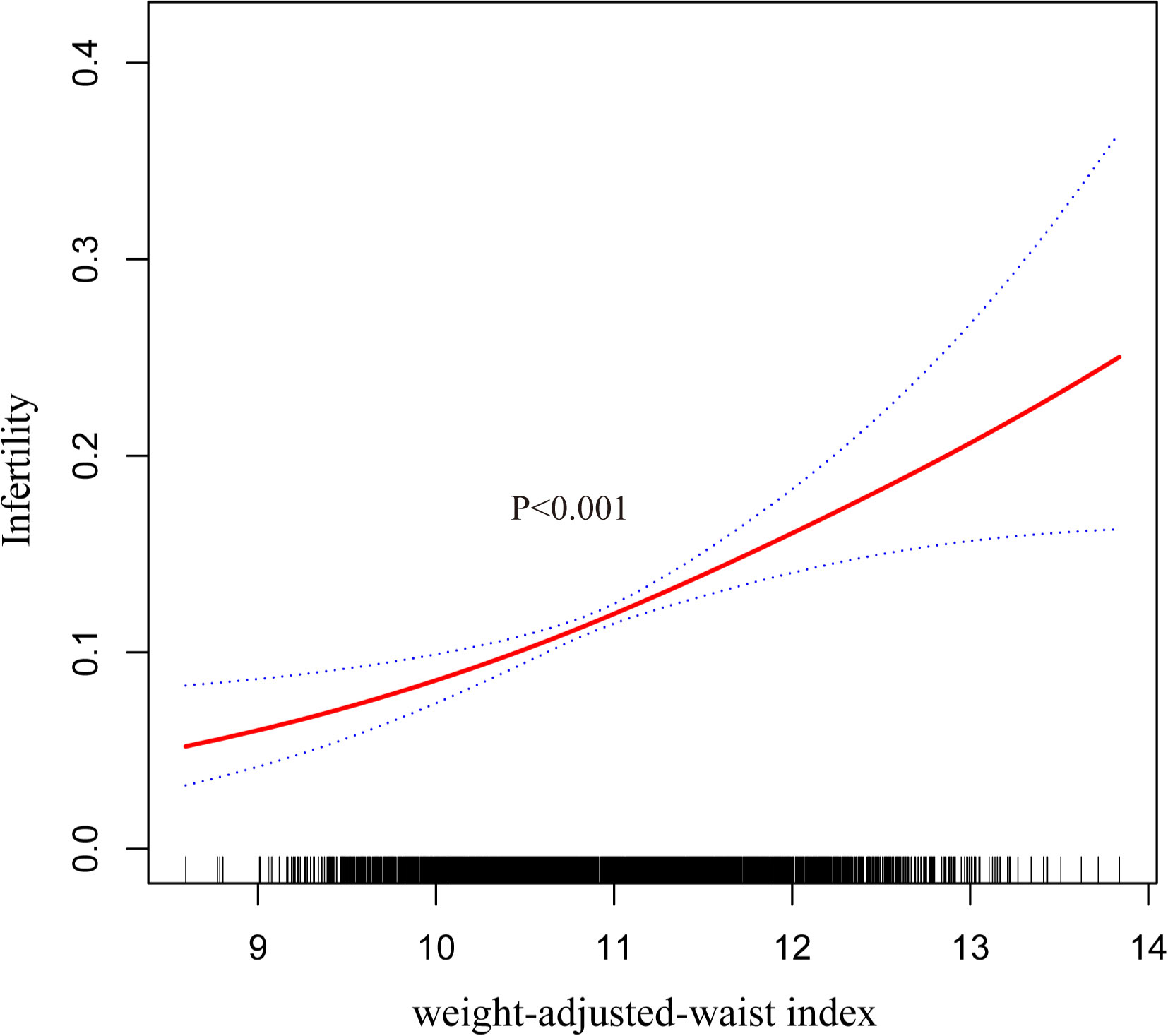
In addition, we further investigated the relationship between WWI and the risk of infertility using smoothed curve fitting, which showed a positive non-linear relationship (Figure 2).
3.3 Subgroup analysis
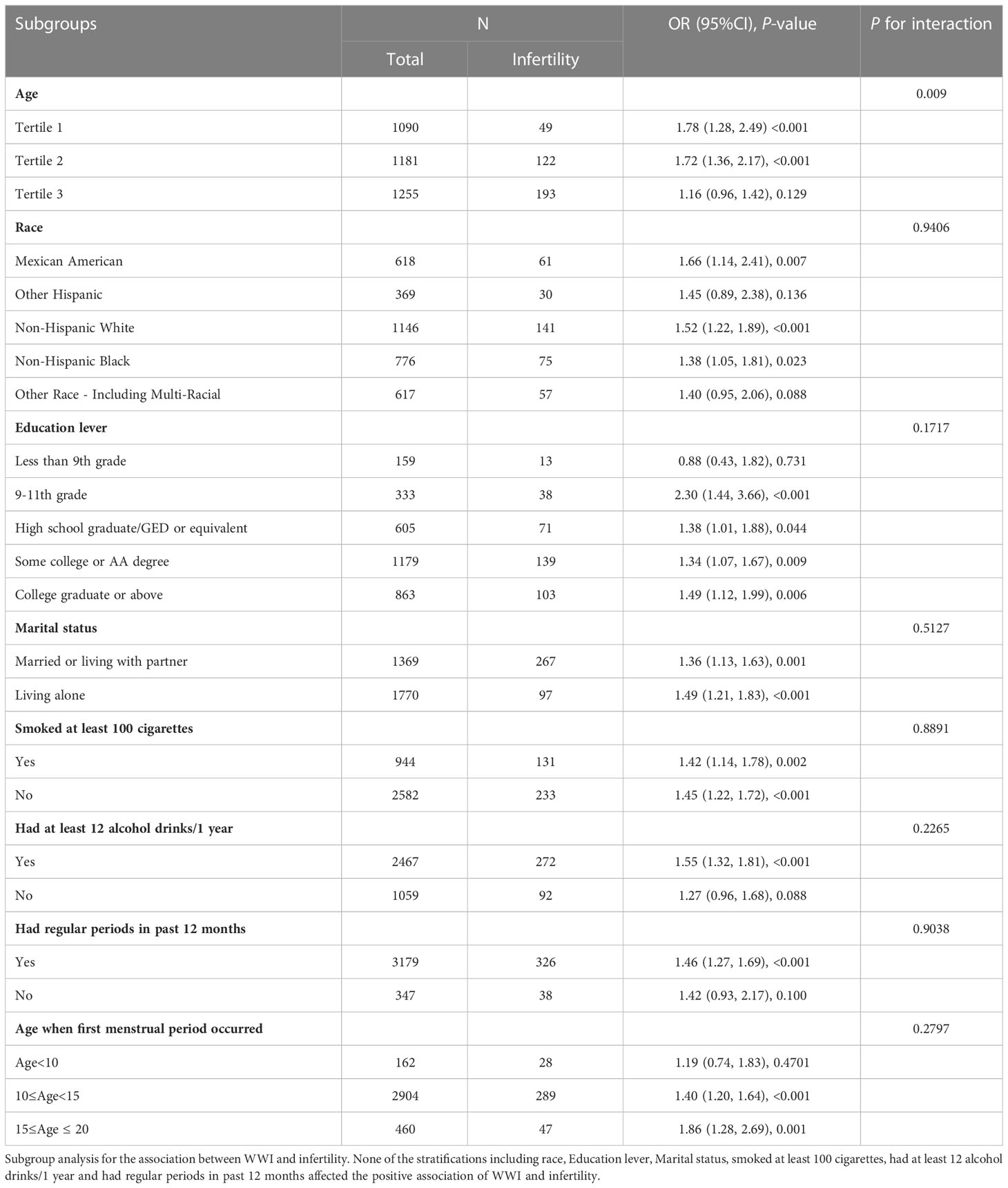
We then conducted subgroup analysis to assess whether the relationship between WWI and infertility was stable across various demographic situations. According to our findings, there was no dependency on the relationship between WWI and infertility. As shown in Table 3, none of the stratifications, including race, education lever, marital status, smoke at least 100 cigarettes, had at least 12 alcohol drinks/1 year, age when first menstrual period occurred and had regular periods in past 12 months significantly affected the positive association between WWI and infertility (all P for interaction> 0.05).
3.4 Weight-adjusted-waist index showed a stronger correlation than other markers of obesity including WC, body mass index and a body shape index for infertility
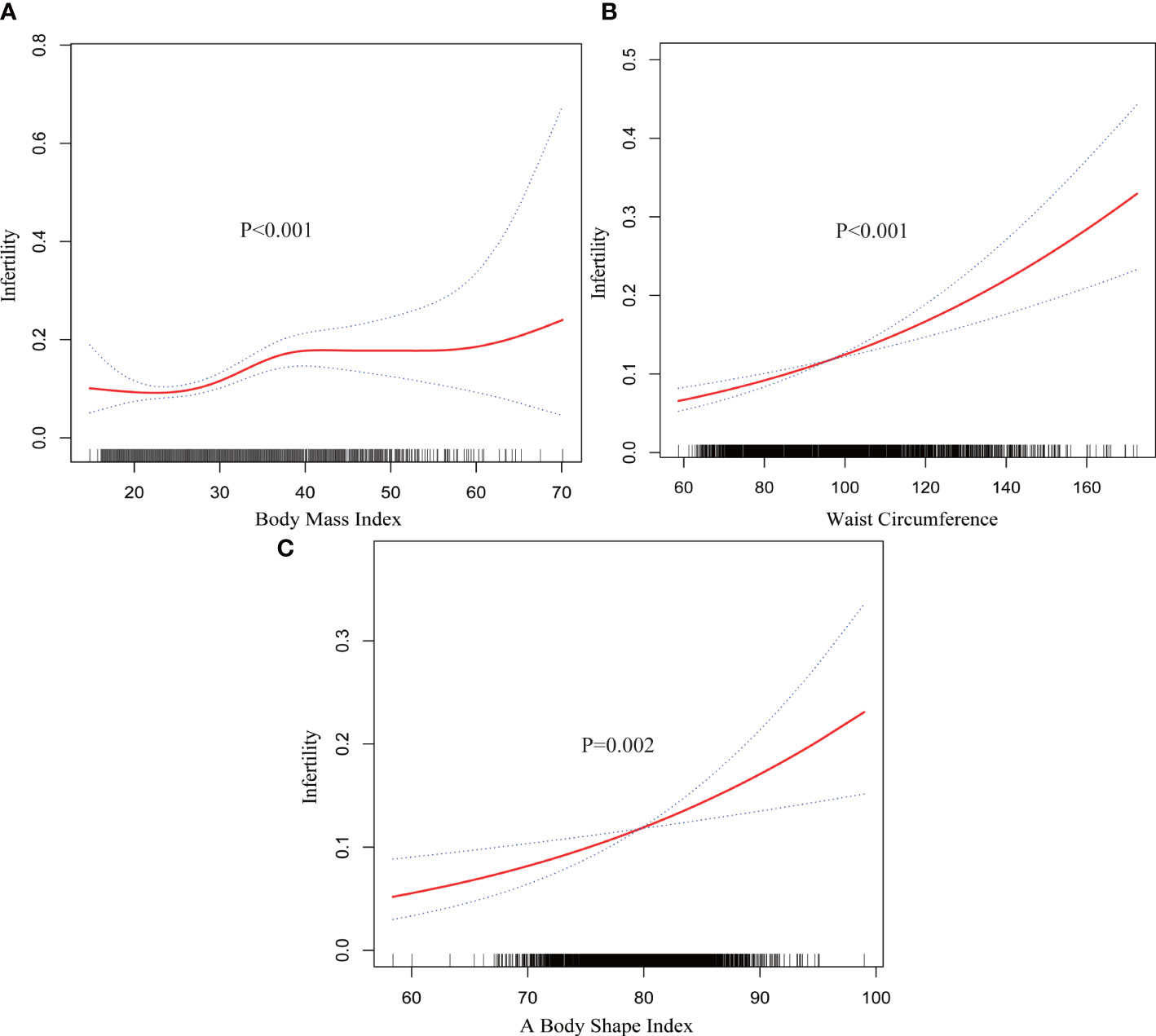
Smooth curve fitting revealed non-linearity in the relationships between other markers of obesity including WC, body mass index (BMI) and a body shape index (ABSI) and infertility (Figure 3). Then, each interval was fitted using the segmented regression model, and the threshold effect was calculated (Table 4).
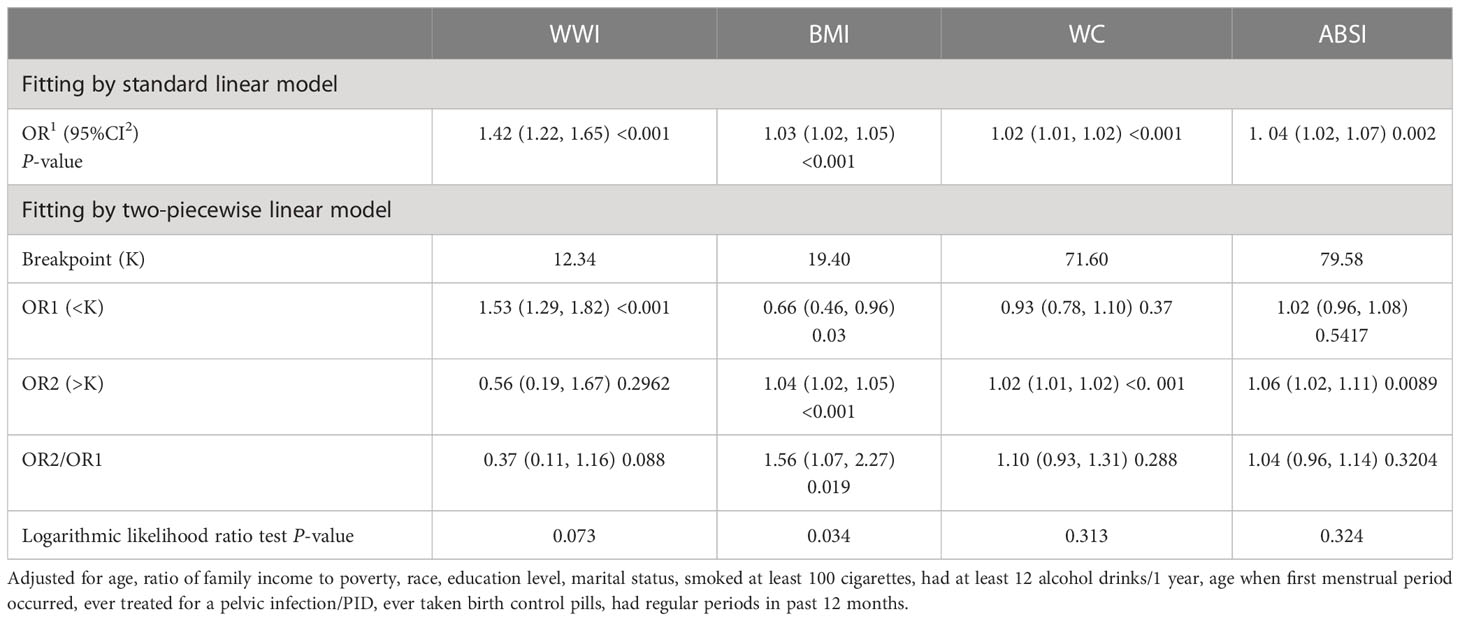
Table 4 Threshold effect analysis of WWI, BMI, WC and ABSI on infertility using a two-piecewise linear regression model.
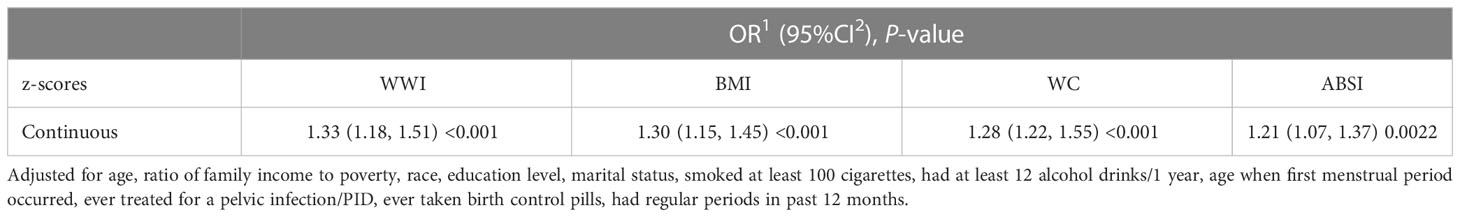
Furthermore, to be able to comment on the OR for WWI in comparison to the OR for other markers of obesity, we calculated their z-scores and used these in the linear models (Table 5). Compared with other markers of obesity including WC, body mass index (BMI) and a body shape index (ABSI), WWI had a stronger connection with the risk of infertility (WWI: OR = 1.33; BMI: OR =1.30; WC: OR =1.28; ABSI: OR =1.21), suggesting that it may be a better predictor of the likelihood of infertility than other markers of obesity.
4 Discussion
This investigation examined the association between Weight-adjusted-waist index and infertility in non-institutionalized Americans. We discovered that individuals with higher WWI demonstrated an increased probability of infertility in our cross-sectional analysis, which included 3,526 females. Subgroup analysis and interaction test showed that this association between WWI and infertility was stable across various demographic situations. Additionally, we further found a stronger association between WWI and infertility than other markers of obesity, indicating that WWI may be a more accurate predictor of infertility than other obesity-related indicators. According to our research, WWI may be able to predict the prevalence of infertility, and managing obesity as determined by WWI may help to reduce the risk of infertility.
A few studies have investigated the association between central obesity and infertility, and the findings vary from study to study (21–23). According to a prospective cohort of black women (21), greater WC (>84 cm) or WHR (>0.85) was linked to lower fecundity independently of BMI. After adjusting for BMI, a different American prospective cohort discovered that the negative correlations between WC and WHR and fecundity were attenuated (22). In contrast, a multiethnic prospective cohort revealed no correlations for WC, WHR, WHtR or ABSI with fecundability (23). In this population-based study, we found positive associations for WWI, WC and ABSI with infertility. Therefore, it is essential to explore whether abdominal adipocytes have dissimilar hormonal activity in different populations.
To our knowledge, this is the first study to evaluate the association between WWI and infertility, highlighting the relationship between a higher WWI level and increased infertile risks. Compared to conventional equations based on BMI, WWI is a newly developed metric of obesity that more correctly predicts whole-body fat percentage and that has been explored in various fields (15, 24). According to Park et al., WWI was strongly correlated with cardiometabolic morbidity and cardiovascular death among 465,629 participants, which were not evident in BMI (15). Similarly, Ding et al. discovered a non-linear positive correlation between WWI levels and the risk of cardiovascular and all-cause mortality that was independent of BMI and WC (25). Moreover, Xie F et al. uncovered that WWI was strongly linked with higher abdominal aortic calcification (AAC) scores [= 0.95, 95% confidence interval (CI): 0.65-1.25, P< 0.001] and an increased likelihood of severe AAC [odds ratio (OR) = 1.82; 95% CI: 1.20-2.75; P = 0.005] (26). Additionally, Qin Z et al. observed that the prevalence of albuminuria was significantly correlated with WWI (OR = 1.28; BMI: OR = 1.02; WC: OR = 1.01), suggesting that WWI may be a more accurate predictor of the incidence of albuminuria than other obesity indicators like BMI (27). In our analysis, we found out a positive non-linear association of WWI with infertility both in crude model and adjusted model. A dose-response association between WWI and infertility was also revealed by the sensitivity analysis using WWI as a tertile. And more importantly, WWI exhibited a substantially stronger association with the likelihood of infertility than other markers of obesity (WWI: OR = 1.33; BMI: OR =1.30; WC: OR =1.28; ABSI: OR =1.21). In conclusion, it has been widely claimed that WWI might be used as a predictor of obesity-related disorders, and our research supports this claim.
Infertility is a common issue that has an enormous effect on women, families, and communities (28). It is significant to note that obesity may affect the chances of conceiving and delivering a baby. Obesity has a detrimental influence on a person’s ability to conceive, which is mostly attributed to a functional change in the hypothalamic-pituitary-ovarian (HPO) axis (29–31). Other studies have shown that obese women experience longer pregnancy wait times (32, 33). Contrary to popular belief, obese women tend to be infertile even in the absence of ovulatory disorders (34, 35). Obesity also appears to influence the results of assisted reproductive technology (ART), since obese women have smaller oocytes that are less likely to fertilize normally (26, 36, 37). Therefore, it is of great importance to accurately assess obesity to reduce the risk of infertility. However, BMI, the traditional obesity-related anthropometric index, have intrinsic limitations as its inability to discriminate between muscle mass and fat mass (13, 14). WWI, a new obesity index based on weight and WC, may be a complete and superior indication of obesity and might be used to predict problems associated with obesity.
Our study has some limitations to be declared. First, temporality cannot be determined since this research is cross-sectional. Furthermore, despite adjusting for a number of pertinent confounders, we were incapable to completely exclude the influence of other confounding variables, thus our results should be taken with care. Additionally, because our results were based on only one country, it is yet unknown if they apply to nations. Despite these limitations, our research work has a number of advantages. Since sample weights were taken into consideration and national data were used for our study, the results are generally relevant to the whole population of the United States. We used subgroup analyses to confirm the robustness of the regression analysis after adjusting for confounders due to the large sample size. Finally, we further explored that weight-adjusted-waist index showed a stronger correlation than body mass index for infertility.
5 Conclusion
This investigation revealed that elevated WWI levels were linked to an increased risk of infertility, and that the association between WWI and infertility was stronger than that between other markers of obesity and infertility, suggesting that WWI may serve as a simple anthropometric index to predict infertility.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the National Health and Nutrition Examination Survey. The patients/participants provided their written informed consent to participate in this study.
Author contributions
ZW and XL designed the research. ZW collected, analyzed the data, and drafted the manuscript. ZW and XL revised the manuscript. All authors contributed to the article and approved the submitted version.
Acknowledgments
We are grateful for the information provided by the National Health and Nutrition Examination Survey (2013–2018) of the United States, which is used in epidemiological research and health science research to aid in the development of sound public health policies, direct and design health plans and services, and advance health knowledge.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Broughton DE, Moley KH. Obesity and female infertility: potential mediators of obesity's impact. Fertil Steril (2017) 107:840–7. doi: 10.1016/j.fertnstert.2017.01.017
2. Caballero B. Humans against obesity: who will win? Adv Nutr (2019) 10:S4–9. doi: 10.1093/advances/nmy055
3. Ding C, Shi Y, Li J, Li M, Hu L, Rao J, et al. Association of weight-adjusted-waist index with all-cause and cardiovascular mortality in China: A prospective cohort study. Nutr Metab Cardiovasc Dis (2022) 32:1210–7. doi: 10.1016/j.numecd.2022.01.033
4. Gesink Law DC, Maclehose RF, Longnecker MP. Obesity and time to pregnancy. Hum Reprod (2007) 22:414–20. doi: 10.1093/humrep/del400
5. Greil AL, Johnson KM, McQuillan J, Lacy N. Are prior pregnancy outcomes relevant for models of fertility-specific distress or infertility helpseeking? Hum Fertil (Camb) (2011) 14:160–6. doi: 10.3109/14647273.2011.587229
6. Gualdani E, Di Cianni G, Seghieri M, Francesconi P, Seghieri G. Pregnancy outcomes and maternal characteristics in women with pregestational and gestational diabetes: a retrospective study on 206,917 singleton live births. Acta Diabetol (2021) 58:1169–76. doi: 10.1007/s00592-021-01710-0
7. Kim JY, Choi J, Vella CA, Criqui MH, Allison MA, Kim NH, et al. Associations between weight-adjusted waist index and abdominal fat and muscle mass: multi-ethnic study of atherosclerosis. Diabetes Metab J (2022) 46:747–55. doi: 10.4093/dmj.2021.0294
8. Knight M, Kurinczuk JJ, Spark P, Brocklehurst P, U. K. O. S. System. Extreme obesity in pregnancy in the United Kingdom. Obstet Gynecol (2010) 115:989–97. doi: 10.1097/AOG.0b013e3181da8f09
9. Lam BC, Koh GC, Chen C, Wong MT, Fallows SJ. Comparison of Body Mass Index (BMI), Body Adiposity Index (BAI), Waist Circumference (WC), Waist-To-Hip Ratio (WHR) and Waist-To-Height Ratio (WHtR) as predictors of cardiovascular disease risk factors in an adult population in Singapore. PloS One (2015) 10:e0122985. doi: 10.1371/journal.pone.0122985
10. Li Q, Qie R, Qin P, Zhang D, Guo C, Zhou Q, et al. Association of weight-adjusted-waist index with incident hypertension: The Rural Chinese Cohort Study. Nutr Metab Cardiovasc Dis (2020) 30:1732–41. doi: 10.1016/j.numecd.2020.05.033
11. Luke B, Brown MB, Stern JE, Missmer SA, Fujimoto VY, Leach R, et al. Female obesity adversely affects assisted reproductive technology (ART) pregnancy and live birth rates. Hum Reprod (2011) 26:245–52. doi: 10.1093/humrep/deq306
12. Macaluso M, Wright-Schnapp TJ, Chandra A, Johnson R, Satterwhite CL, Pulver A, Berman SM,, et al. A public health focus on infertility prevention, detection, and management. Fertil Steril (2010) 93:16 e11–10. doi: 10.1016/j.fertnstert.2008.09.046
13. Marquard KL, Stephens SM, Jungheim ES, Ratts VS, Odem RR, Lanzendorf S, et al. Polycystic ovary syndrome and maternal obesity affect oocyte size in in vitro fertilization/intracytoplasmic sperm injection cycles. Fertil Steril (2011) 95:2146–2149, 2149 e2141. doi: 10.1016/j.fertnstert.2010.10.026
14. Mascarenhas MN, Flaxman SR, Boerma T, Vanderpoel S, Stevens GA. National, regional, and global trends in infertility prevalence since 1990: a systematic analysis of 277 health surveys. PloS Med (2012) 9:e1001356. doi: 10.1371/journal.pmed.1001356
15. Park Y, Kim NH, Kwon TY, Kim SG. A novel adiposity index as an integrated predictor of cardiometabolic disease morbidity and mortality. Sci Rep (2018) 8:16753. doi: 10.1038/s41598-018-35073-4
16. Qin Z, Chang K, Yang Q, Yu Q, Liao R, Su B. The association between weight-adjusted-waist index and increased urinary albumin excretion in adults: A population-based study. Front Nutr (2022) 9:941926. doi: 10.3389/fnut.2022.941926
17. Curtin LR, Mohadjer LK, Dohrmann SM, Kruszon-Moran D, Mirel LB, Carroll MD, et al. National Health and Nutrition Examination Survey: sample design, 2007-2010. Vital Health Stat (2013) 2:1–23. doi: 10.1002/9781118190180.ch20
18. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet (2007) 370:1453–7. doi: 10.1016/S0140-6736(07)61602-X
19. Krakauer NY, Krakauer JC. A new body shape index predicts mortality hazard independently of body mass index. PloS One (2012) 7:e39504. doi: 10.1371/journal.pone.0039504
20. McGuire S. Frayar, D.C., Ervin, R.B. Caloric intake from fast food among adults: United States, 2007-2010. NCHS Data Brief, No. 114, February 2013. Hyattsville, MD: National Center for Health Statistics, 2013. Adv Nutr (2013) 4:578. doi: 10.3945/an.113.003889
21. Wise LA, Palmer JR, Rosenberg L. Body size and time-to-pregnancy in black women. Hum Reprod (2013) 28:2856–64. doi: 10.1093/humrep/det333
22. McKinnon CJ, Hatch EE, Rothman KJ, Mikkelsen EM, Wesselink AK, Hahn KA, et al. Body mass index, physical activity and fecundability in a North American preconception cohort study. Fertil Steril (2016) 106:451–9. doi: 10.1016/j.fertnstert.2016.04.011
23. Loy SL, Cheung YB, Soh SE, Ng S, Tint MT, Aris IM, et al. Female adiposity and time-to-pregnancy: a multiethnic prospective cohort. Hum Reprod (2018) 33:2141–9. doi: 10.1093/humrep/dey300
24. Rachon D, Teede H. Ovarian function and obesity–interrelationship, impact on women's reproductive lifespan and treatment options. Mol Cell Endocrinol (2010) 316:172–9. doi: 10.1016/j.mce.2009.09.026
25. Ramlau-Hansen CH, Thulstrup AM, Nohr EA, Bonde JP, Sørensen TI, Olsen J, et al. Subfecundity in overweight and obese couples. Hum Reprod (2007) 22:1634–7. doi: 10.1093/humrep/dem035
26. Xie F, Xiao Y, Li X, Wu Y. Association between the weight-adjusted-waist index and abdominal aortic calcification in United States adults: Results from the national health and nutrition examination survey 2013-2014. Front Cardiovasc Med (2022) 9:948194. doi: 10.3389/fcvm.2022.948194
27. Romero-Corral A, Somers VK, Sierra-Johnson J, Thomas RJ, Collazo-Clavell ML, Korinek J, et al. Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes (Lond) (2008) 32:959–66. doi: 10.1038/ijo.2008.11
28. Sandelowski M. On infertility. J Obstet Gynecol Neonatal Nurs (1994) 23:749–52. doi: 10.1111/j.1552-6909.1994.tb01949.x
29. Shah DK, Missmer SA, Berry KF, Racowsky C, Ginsburg ES. Effect of obesity on oocyte and embryo quality in women undergoing in vitro fertilization. Obstet Gynecol (2011) 118:63–70. doi: 10.1097/AOG.0b013e31821fd360
30. Thoma ME, McLain AC, Louis JFs, King RB, Trumble AC, Sundaram R, et al. Prevalence of infertility in the United States as estimated by the current duration approach and a traditional constructed approach. Fertil Steril (2013) 99:1324–1331 e1321. doi: 10.1016/j.fertnstert.2012.11.037
31. Tortoriello DV, McMinn J, Chua SC. Dietary-induced obesity and hypothalamic infertility in female DBA/2J mice. Endocrinology (2004) 145:1238–47. doi: 10.1210/en.2003-1406
32. Tortoriello DV, McMinn JE, Chua SC. Increased expression of hypothalamic leptin receptor and adiponectin accompany resistance to dietary-induced obesity and infertility in female C57BL/6J mice. Int J Obes (Lond) (2007) 31:395–402. doi: 10.1038/sj.ijo.0803392
33. Vahratian A. Prevalence of overweight and obesity among women of childbearing age: results from the 2002 National Survey of Family Growth. Matern Child Health J (2009) 13:268–73. doi: 10.1007/s10995-008-0340-6
34. van der Steeg JW, Steures P, Eijkemans MJ, Habbema JD, Hompes JG, Burggraaff JM, et al. Obesity affects spontaneous pregnancy chances in subfertile, ovulatory women. Hum Reprod (2008) 23:324–8. doi: 10.1093/humrep/dem371
35. Wise LA, Rothman KJ, Mikkelsen EM, Sørensen HT, Riis A, Hatch EE. An internet-based prospective study of body size and time-to-pregnancy. Hum Reprod (2010) 25:253–64. doi: 10.1093/humrep/dep360
36. Zeng X, Pang H, Li X, Luo S, Jin S, Li S. Impact of obesity on endometrial blood flow in women without polycystic ovarian syndrome during intracytoplasmic sperm injection. Reprod Biol Endocrinol (2013) 11:57. doi: 10.1186/1477-7827-11-57
Keywords: infertility, weight-adjusted-waist index, obesity, non-linear, NHANES
Citation: Wen Z and Li X (2023) Association between weight-adjusted-waist index and female infertility: a population-based study. Front. Endocrinol. 14:1175394. doi: 10.3389/fendo.2023.1175394
Received: 27 February 2023; Accepted: 21 July 2023;
Published: 08 August 2023.
Edited by:
Monica Marques Telles, Federal University of São Paulo, BrazilReviewed by:
Ali Abbara, Imperial College London, United KingdomTom Kelsey, University of St Andrews, United Kingdom
Sofia Christakoudi, Imperial College London, United Kingdom
Copyright © 2023 Wen and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiang Li, bHgxMzUzOTEyNzU4M0AxNjMuY29t
 Zujun Wen
Zujun Wen Xiang Li
Xiang Li